Abstract
Background
Post-COVID-19 conditions (PCCs), also known as long COVID, is persistently debilitating disorders that need investigation on their incidence, morbidity, and case-fatality rate.
Purpose
The objectives of this cohort study were to determine the incidence, characteristics, case-fatality, morbidity, and recovery of post-COVID-19 symptoms throughout a two-year period of observation.
Methods
This was a population-based cohort study of post-COVID-19 cases among 12,925 SARS-CoV-2 positive individuals in eight administrative districts of Bangladesh between July and December 2021–2023. PCC was diagnosed according to WHO clinical diagnostic criteria, and the screening procedure was completed through a household screening process.
Results
The incidence of PCC was 3.6%, the case-fatality rate was 1.92%, and the recovery rate was 9.0%. The significant predictors of PCC morbidity were geographical distribution, vaccination, comorbidities, and a longer duration of symptoms or multiple symptoms (p < 0.05).
Conclusion
Nearly 465 out of 522 people suffering from PCC are persistent and have a significant disability. However, the rate of recovery was 9.0%. It is necessary to investigate approaches to improve the recovery of PCC in Bangladesh.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-024-01358-6.
Keywords: Post-COVID-19 conditions, Cohort, Case-fatality, Recovery, Bangladesh
| Taxt box 1. Contributions to the literature |
|---|
| 1. More than 3% of SARS-CoV-2 cases in Bangladesh have post-COVID-19 Conditions (PCCs). In addition, this condition has a case-fatality rate of 1.92% and a recovery rate of 9.0%. |
| 2. The prominent symptoms of PCC attributes as fatigue, musculoskeletal pain, functional limitations, problems with memory and executive functions and psychological issues. |
| 3. The PCC can be introduced at any time during the lifespan with an episodic pattern. |
Introduction
Post-COVID-19 conditions (PCCs) can be referred to as “long COVID” [1] or post-acute COVID-19 condition (PACC) is characterized by the emergence of new or exacerbated symptoms after being infected with SARS-CoV-2 [2]. These symptoms are present for at least three months and persist for up to 8 weeks without a transparent and reportable diagnostic test [1]. Approximately, 5–10%, of people who have recovered from COVID-19 have reported experiencing Post-COVID Conditions (PCC), characterized by severe and incapacitating symptoms [3]. The global prevalence of PCC is 43%, with Asian people having a higher frequency of 51% [4]. During the first phase of the pandemic, a household survey conducted in Bangladesh revealed that 16.1% of persons had successfully recovered from COVID-19 [5], although another research indicated a proportion of 25.2% [6].
Understanding ongoing symptoms and risk factors associated with SARS-CoV-2 infection remains a challenge. The activation of an innate immune system component is the major cause of thrombo-inflammation and fitness loss [7]. Furthermore, the prevalence of PCC symptoms varies between 7% and 43% [8]. Patients with PCC often endure physical, mental, and social problems. The symptoms reported by individuals include fatigue (30.5%), insomnia (16.2%), cough (15.9%), myalgia (16.7%), joint pain (14.3%), anxiety (15%), depression (14.9%), social interaction disturbance (14.5%), headache (12.3%), problems with activities of daily living (12%), dizziness (10.8%), fever (9.8%), difficulties with brain fog (10.3%), and concentration problems (10%) [9]. Studies that have been published suggest that people with PCC and SARS-CoV-2 infection are more likely to have cardiovascular and metabolic problems, which may worsen their general health and cause death [10–16]. PCC etiology, nature, and associated risk factors must be thoroughly identified and understood in order to enhance PCC management. Professionals use a multidisciplinary method to define the clinical case and track the progression of PCC [17].
With so many people afflicted with SARS-CoV-2, it is essential for low- and middle-income country like Bangladesh [18] to ascertain the epidemiology and course of PCC. In order to negatively impact PCC incidence, related risks, and illness progression, PCC patients must be monitored [19] for a longer-term cohort study. There is a substantial research void in the determination of PCC symptom responses, absolute and relative risk calculations, incidence determination, case-fatality, and morbidity. Consequently, we plan to address these deficiencies through this cohort. The objectives of this study were as follows: (1) to evaluate the case-fatality and recovery rate of patients with PCC, (2) to assess the population proportion of patients with PCC in Bangladesh after a 2-year follow-up, (3) to examine the clinical characteristics of patients with PCC, and (4) to identify the predictive factors of PCC.
Methodology
Study design
This prospective epidemiological cohort study was conducted from July 2021 to December 2023. This study focused on individuals who had previously tested positive for COVID-19 using real-time polymerase chain reaction test (RT-PCR) between July and December 2021. The participants were selected from 24 COVID-19 testing centers in Bangladesh. According to previous research, it takes at least 2 months for PCC symptoms to manifest [9]. We performed telephone screenings between August 2021 and February 2022. For participants who consented to a home survey following the phone interview, we proceeded to perform the survey concurrently. A subsequent follow-up interview was conducted between September and December 2023.
Study population
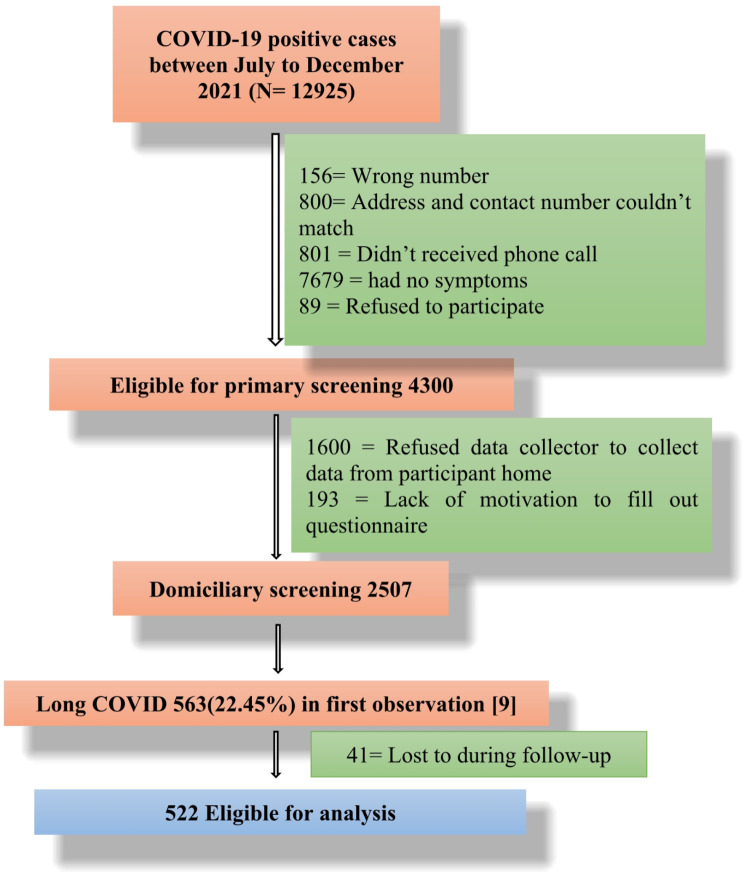
The population frame consisted of 12,925 individuals who tested positive by real-time reverse transcription–polymerase chain reaction (RT-PCR) for COVID-19 with a test date of at least 12 weeks in the past. Approximately 4300 out of 12,925 individuals satisfied the primary qualifying criterion. Prior to performing the home scanning, we performed a telephone interview to estimate the total number of samples for each division and identify potential participants. Among the 4300 individuals, 2507 agreed to participate in a face-to-face interview. During this interview, we identified 563 patients who exhibited symptoms of PCC between June and December 2021. The complete analysis included 522 participants (Fig. 1).
Fig. 1.
Study flowchart and ensure all key variables are complete
Participant selection criteria
The primary eligibility criteria for participants were as follows: being 18 years of age or older, answering telephone calls, being COVID-19 positive through an RT-PCR test between July and December 2021, experiencing chronic PCC symptoms between July 2021 and December 2023, and providing consent for a household survey. Patients who were lost to follow-up at the initial follow-up screening were excluded.
Sample size and sampling method
All participants were included in a prospective cohort study of individuals who experienced post-COVID-19 symptoms [9] from July to December 2021.
Study procedure
The study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria for conducting a prospective cohort study. Figure 1 shows the flow chart that illustrates the study’s progress. Twelve senior physiotherapy students willingly participated as data collectors for the survey. They underwent training to gather household data using pretested and validated questionnaires.
Data collection tools
We collected a set of structured questions assessing the participant’s age, sex, marital status, occupation, education, blood group, living area, smoking habit, monthly family income, PCC severity, and vaccination status. This study also included patients with a history of clinical comorbidities, such as diabetes, hypertension, ischemic heart disease, chronic obstructive pulmonary disease, chronic kidney disease, hypothyroidism, urinary tract infection, osteoporosis, and high cholesterol.
C19-YRS questionnaire
The C19-YRS was used to assess the symptoms and severity of COVID-19 among the study participants. The C19 YRS is a valid and reliable tool for assessing symptom responses and severity and determining the scope of rehabilitation for patients with post-COVID-19 symptoms [20]. The C19-YRS consists of 22 items, each assessed on an 11-point numerical rating scale ranging from 0 (indicating the absence of symptoms) to 10 (indicating a very severe level or impact). These ratings capture the individual’s experience of symptoms both before and after contracting COVID-19. The questionnaire is divided into four subcategories, namely symptom severity score (ranging from 0 to 100), functional disability score (ranging from 0 to 50), extra symptoms (ranging from 0 to 60), and overall health (ranging from 0 to 10). This study only utilized the symptom severity scale. The initial questionnaire was in English and then translated into Bangla. Forward and backward translation was performed for the questionnaire. To ensure the internal consistency standards, Cronbach’s alpha was calculated, and the score was found to be 0.879.
Data analysis
Before the data analysis, the data underwent data management process for examining normality, excluding outliers, and ensuring internal consistency. Descriptive statistics was used to expressed as frequencies, percentages, mean and standard deviation. Analyzing big data is challenging and requires a multidisciplinary approach to transform data into knowledge for informed decision-making [21]. Pearson’s chi-square test or Fisher’s exact test (in the case of a value of 0 for any category or a 20% data value less than 5 in any category) was used to determine whether there was a relationship between the presence or absence of PCC symptoms among all the selected variables. A multiple logistic regression model was performed to estimate the associations of sociodemographic and clinical characteristics with the presence or absence of PCC symptoms (yes = presence of symptoms or no = absence of symptoms), using Odds Ratios (ORs) and 95% confidence interval (CI). The variables that significantly differed between the presence or absence of PCC symptoms in the bivariate analysis were controlled for in the adjusted analysis. The level of significance was set at p < 0.05 for all tests. All the data analyses were performed using version 25.00 of the IBM SPSS statistical software package.
Ethical consideration
Ethical approval
was obtained from the ethical review board of the Bangladesh Physiotherapy Association’s Institute of Physiotherapy Rehabilitation and Research with grant number (BPA-IPRR/IRB/19/01/2023/69). Prior to the telephone interview, the participants provided verbal informed consent, and written informed consent was obtained prior to participation in this study. During the household survey, if the participant was uneducated, an educated witness read and conveyed the message to the uneducated participants and gave consent as a witness; consequently, a thumbprint was taken from the participants. During the research, we ensured the preservation of confidentiality, ethics, and privacy by strictly following the principles outlined in the Declaration of Helsinki, revised in 2013. We acquired approval from the Directorate General of Health Services of the Government of the People’s Republic of Bangladesh to screen households in the future.
Results
Sociodemographic characteristics of participants
A total of 522 participants with or without PCC symptoms, both male (62.8%) and female (37.2%), initially participated in this study. After two years of being tested for COVID-19, 47 (9%) patients with PCC symptoms recovered fully, and 10 (1.92%) patients died. Among the study participants, 77.2% were married, 35.2% were service holders, and nearly half (47.7%) had a bachelor’s degree or above. Most participants were from urban areas (54.6%), and for 57.7% of the participants, had a monthly family income was < 35,000 BDT. Initially 38.1% of participants suffered mild, 35.2% moderate, and 26.6% severe PCC symptoms, and after two years, these symptoms diminished to mild (38.5%), moderate (33.8%) and severe (27.7%) PCC symptoms respectively. The number of recoveries (44.7%) and deaths (60.0%) were also greater for patients with moderate PCC symptoms. Initially, only 4% of participants were non-vaccinated, and 25.7% completed their booster dose. The recovery rate (59.6%) and death rate (80.0%) were also greater for those who completed their second vaccination dose. The details are presented in Table 1.
Table 1.
Sociodemographic characteristics of participants
| Variables | Sub-category | Overall (N = 522) | 2nd Observation (N = 465) |
Recovery (n = 47; 9.0%) |
Death (10; 1.92%) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean/ Frequency | SD/Percentage | Mean/ Frequency | SD/Percentage | Median/ Frequency | IQR/Percentage | Median/ Frequency | IQR/Percentage | ||
| Age | 39.38 | ± 13.59 | 39.19 | ± 13.19 | 35 | (29.0, 47.0) | 41 | (32.75, 60.75) | |
| Age Category | 18–40 Years | 304 | (58.2%) | 268 | (57.6%) | 31 | (66.0%) | 05 | (50.0%) |
| 41–60 Years | 179 | (34.3%) | 167 | (35.9%) | 09 | (19.1%) | 03 | (30.0%) | |
| > 60 Years | 39 | (7.5%) | 30 | (6.5%) | 07 | (14.9%) | 02 | (20.0%) | |
| Gender | Male | 328 | (62.8%) | 293 | (63.0%) | 30 | (63.8%) | 05 | (50.0%) |
| Female | 194 | (37.2%) | 172 | (37.0%) | 17 | (36.2%) | 05 | (50.0%) | |
| Marital Status | Married | 403 | (77.2%) | 363 | (78.1%) | 32 | (68.1%) | 08 | (80.0%) |
| Unmarried | 117 | (22.4%) | 100 | (21.5%) | 15 | (31.9%) | 02 | (20.0%) | |
| Widow | 02 | (0.4%) | 02 | (0.4%) | 00 | (0%) | 00 | (0%) | |
| Occupation | Day labor | 45 | (8.6%) | 41 | (8.8%) | 03 | (6.4%) | 01 | (10.0%) |
| Service holder | 184 | (35.2%) | 162 | (34.8%) | 19 | (40.4%) | 03 | (30.0%) | |
| Health Professionals | 20 | (3.8%) | 17 | (3.7%) | 02 | (4.3%) | 01 | (10.0%) | |
| Law enforcement | 42 | (8.0%) | 38 | (8.2%) | 04 | (8.5%) | 00 | (0%) | |
| Housewife | 90 | (17.2%) | 81 | (17.4%) | 06 | (12.8%) | 03 | (30.0%) | |
| Student | 86 | (16.5%) | 77 | (16.6%) | 07 | (14.9%) | 02 | (20.0%) | |
| Unemployed | 17 | (3.3%) | 14 | (3.0%) | 03 | (6.4%) | 00 | (0%) | |
| Businessman | 38 | (7.3%) | 35 | (7.5%) | 03 | (6.4%) | 00 | (0%) | |
| Educational Status | No formal education | 13 | (2.5%) | 13 | (2.8%) | 00 | (0%) | 00 | (0%) |
| Primary education | 59 | (11.3%) | 53 | (11.4%) | 04 | (8.5%) | 02 | (20.0%) | |
| Secondary education | 92 | (17.6%) | 79 | (17.0%) | 10 | (21.3%) | 03 | (30.0%) | |
| Higher secondary education | 135 | (25.9%) | 122 | (26.2%) | 12 | (25.5%) | 01 | (10.0%) | |
| Bachelor or above | 223 | (47.7%) | 198 | (42.6%) | 21 | (44.7%) | 04 | (40.0%) | |
| Blood Group | A+ | 122 | (23.4%) | 108 | (23.2%) | 11 | (23.4%) | 03 | (30.0%) |
| A- | 05 | (1.0%) | 04 | (0.9%) | 01 | (2.1%) | 00 | (0%) | |
| B+ | 187 | (35.8%) | 162 | (36.8%) | 22 | (46.8%) | 03 | (30.0%) | |
| B- | 20 | (3.8%) | 18 | (3.9%) | 02 | (4.3%) | 00 | (0%) | |
| AB+ | 69 | (13.2%) | 63 | (13.5%) | 05 | (10.6%) | 01 | (10.0%) | |
| AB- | 04 | (0.8%) | 04 | (0.9%) | 00 | (0%) | 00 | (0%) | |
| O+ | 108 | (20.7%) | 99 | (21.3%) | 06 | (12.8%) | 03 | (30.0%) | |
| O- | 07 | (1.3%) | 07 | (1.5%) | 00 | (0%) | 00 | (0%) | |
| Living Area | Rural | 56 | (10.7%) | 52 | (11.2%) | 02 | (4.3%) | 02 | (20.0%) |
| Semi-urban | 181 | (34.7%) | 157 | (33.8%) | 22 | (46.8%) | 02 | (20.0%) | |
| Urban | 285 | (54.6%) | 256 | (55.1%) | 23 | (48.9%) | 06 | (60.0%) | |
| Monthly Family Income |
Below the poverty line < 10,200 (< 85 USD) |
20 | (3.8%) | 17 | (3.7%) | 03 | (6.4%) | 00 | (0%) |
| < 35,000 BDT (< 320 USD) | 301 | (57.7%) | 266 | (57.2%) | 28 | (59.6%) | 07 | (70.0%) | |
| > 35,000 BDT (> 320 USD) | 201 | (38.5%) | 182 | (39.1%) | 16 | (34.0%) | 03 | (30.0%) | |
| Post-COVID-19 condition severity | Mild | 199 | (38.1%) | 179 | (38.5%) | - | - | 02 | (20.0%) |
| Moderate | 184 | (35.2%) | 157 | (33.8%) | - | - | 06 | (60.0%) | |
| Severe | 139 | (26.6%) | 129 | (27.7%) | - | - | 02 | (20.0%) | |
| Vaccination | Non-Vaccinated | 21 | (4.0%) | 20 | (4.3%) | 01 | (2.1%) | 00 | (0%) |
| 1st dose | 60 | (11.5%) | 53 | (11.4%) | 07 | (14.9%) | 00 | (0%) | |
| 2nd dose | 307 | (58.8%) | 271 | (58.3%) | 28 | (59.6%) | 08 | (80.0%) | |
| Booster dose | 134 | (25.7%) | 121 | (26.0%) | 11 | (23.4%) | 02 | (20.0%) | |
| Smoking | Yes | 95 | (18.2%) | 84 | (18.1%) | 10 | (31.3%) | 01 | (10.0%) |
| No | 427 | (81.8%) | 381 | (81.9%) | 37 | (78.7%) | 09 | (90.0%) | |
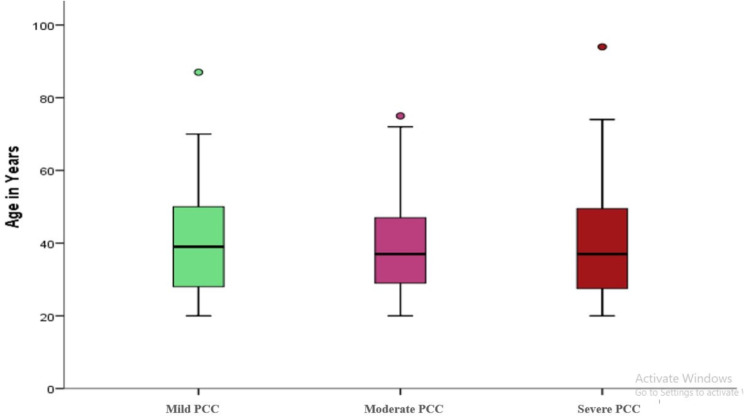
Representation of PCC symptoms
The study participants reported breathlessness (66.5%) as the most common PCC symptom during the first observation, followed by fatigue (45.0%), cough (17.8%), headache (13.9%), and myalgia (13.9%). Our second observation two years later, revealed that fatigue (89.2%) was the most prevalent PCC symptom, followed by breathlessness (79.4%), headache (74.2%), arthralgia (68.2%), myalgia (64.9%), and anxiety (69.7%). This study also revealed several novel symptoms in the respondents at the second observation, including taste alteration (52.0%), smell problems (43.2%), hair loss (39.6%), and diarrhea (36.6%). Table 2 includes the details of the symptoms. Most young adults suffer from mild PCC symptoms (Fig. 2).
Table 2.
Clinical presentation of post-COVID-19 condition symptoms
| Symptoms | 1st observation-2022 (n = 522) |
2nd observation-2024 (n = 465) |
||
|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |
| Common Symptoms | ||||
| Breathlessness or Dyspnea | 347 | (66.5%) | 369 | (79.4%) |
| Cough | 93 | (17.8%) | 63 | (13.5%) |
| Fatigue | 235 | (45.0%) | 415 | (89.2%) |
| Chest pain | 57 | (10.9%) | 203 | (43.7%) |
| Myalgia | 73 | (13.9%) | 302 | (64.9%) |
| Arthralgia | 63 | (12.1%) | 317 | (68.2%) |
| Headache | 73 | (13.9%) | 345 | (74.2%) |
| Abdominal Pain | 07 | (1.3%) | 80 | (17.2%) |
| Ear pain | 26 | (4.9%) | 07 | (1.5%) |
| Concentration | 26 | (4.9%) | 294 | (63.2%) |
| Memory Loss | 37 | (7.1%) | 275 | (59.1%) |
| Planning Problems | 18 | (3.4%) | 177 | (38.1%) |
| Anxiety | 54 | (10.3%) | 324 | (69.7%) |
| Depression | 61 | (11.7%) | 194 | (41.7%) |
| PTSD | 01 | (0.2%) | 269 | (57.8%) |
| Dizziness | 26 | (4.9%) | 141 | (30.3%) |
| Sleep Disturbance | 55 | (10.5%) | 163 | (35.1%) |
| Fever | 66 | (12.6%) | 213 | (45.8%) |
| Skin Rash | 06 | (1.1%) | 151 | (32.5%) |
| Novel Symptoms in Respondents | ||||
| Diarrhea | - | 170 | (36.6%) | |
| Smell Problems | - | 201 | (43.2%) | |
| Hair Loss | - | 184 | (39.6%) | |
| Taste Alteration | - | 242 | (52.0%) | |
| Weight Loss | - | 84 | (18.1%) | |
| Visual Problems | - | 127 | (27.3%) | |
| Sore Throat | - | 62 | (13.3%) | |
| Tinnitus | - | 89 | (19.1%) | |
| Brain Fog | - | 77 | (16.6%) | |
Fig. 2.
Severity of post-COVID-19 condition by age (years)
Comorbidity distribution of the respondents in the second observation
As shown in Tables 3 and 83.7% of participants with PCC symptoms in this study reported one or multiple comorbidities during our second observation, with diabetes (57.3%) and hypertension (56.0%) being the most prevalent comorbidities reported by the respondents. Osteoporosis (23.4%), COPD (21.6%), IHD (18.3%), and CKD (13.9%) were also most common among the study participants, as shown in Table 3.
Table 3.
Distribution of comorbidities among respondents in second observations
| Variable | Post-COVID-19 Conditions patients (n = 389) | Recovery (n = 40) | Death (n = 9) | |||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | |
| Diabetes | 223 | (57.3%) | 22 | (55.0%) | 04 | (44.4%) |
| Hypertension | 218 | (56.0%) | 21 | (52.5%) | 07 | (77.8%) |
| IHD | 71 | (18.3%) | 09 | (22.5%) | 02 | (22.2%) |
| COPD | 84 | (21.6%) | 11 | (27.5%) | 01 | (11.1%) |
| Chronic Kidney Disease | 54 | (13.9%) | 07 | (17.5%) | 01 | (11.1%) |
| Hypothyroidism | 41 | (10.5%) | 06 | (15.0%) | 01 | (11.1%) |
| UTI | 03 | (0.8%) | 00 | (0%) | 01 | (11.1%) |
| Osteoporosis | 91 | (23.4%) | 09 | (22.5%) | 02 | (22.2%) |
| High Cholesterol | 06 | (1.5%) | 02 | (5.0%) | 00 | (0%) |
IHD: Ischemic Heart Disease; COPD: Chronic Obstructive Pulmonary Disease; UTI: Urinary Tract Infection
Results from regression analysis
The participants’ marital status was significantly associated with PCC symptoms such as breathlessness and PTSD. The regression analysis suggested that being unmarried was a statistically significant predictor of PCC symptoms, breathlessness, and PTSD (odds ratio [OR] = 3.39, 95% CI = 1.51–7.64, p = 0.003; OR = 2.74, 95% CI = 1.25–5.97, p = 0.011). On the other hand, living in an urban area was significantly associated with PCC symptoms of breathlessness (OR = 3.15, 95% CI = 1.12–8.89, p = 0.030), fatigue (OR = 5.45, 95% CI = 1.15–19.52, p = 0 0.009), and problems with planning (OR = 2.92, 95% CI = 1.27–6.71, p = 0 0.011).
The study also revealed that COVID-19 vaccination status is significantly associated with several PCC symptoms, such as, myalgia, concentration problems, anxiety, dizziness, and diarrhea. The results of regression analysis suggested that those who completed booster doses had a greater chance of developing myalgia (OR = 3.46, 95% CI = 1.03–11.59, p = 0 0.044), concentration problems (OR = 3.72, 95% CI = 1.11–12.41, p = 0 0.033), anxiety (OR = 3.78, 95% CI = 1.06–13.47, p = 0.040) and dizziness (OR = 2.95, 95% CI = 0.97–8.92, p = 0.056) than those who were not vaccinated. The details are presented in Table 4.
Table 4.
Predictors of post-COVID-19 symptoms by sociodemographic variables
| Independent Variable | Sub category | Unadjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value |
|---|---|---|---|---|---|
| Breathlessness | |||||
| Marital Status | Married | Reff. | Reff. | ||
| Unmarried | 1.55 (1.02, 2.39) | 0.049 | 3.39 (1.51, 7.64) | 0.003 | |
| Widow | 0.00 (0.00, 0.00) | 0.999 | 0.00 (0.00, 0.00) | 0.999 | |
| Living Area | Rural | Reff. | Reff. | ||
| Semi-urban | 2.90 (1.23, 6.81) | 0.015 | 2.91 (1.03, 8.22) | 0.044 | |
| Urban | 3.39 (1.48, 7.77) | 0.004 | 3.15 (1.12, 8.89) | 0.030 | |
| Fatigue | |||||
| Living Area | Rural | Reff. | Reff. | ||
| Semi-urban | 2.53 (0.94, 6.80) | 0.065 | 4.23 (1.18, 15.16) | 0.027 | |
| Urban | 3.07 (1.18, 8.02) | 0.022 | 5.45 (1.15, 19.52) | 0.009 | |
| Monthly Family Income |
Below the poverty line < 10,200 BDT (< 85 USD) |
Reff. | Reff. | ||
| < 35,000 BDT (< 320 USD) | 0.83 (0.29, 2.36) | 0.721 | 0.33 (0.08, 1.35) | 0.112 | |
| > 35,000 BDT (> 320 USD) | 0.68 (0.23, 1.98) | 0.476 | 0.21 (0.05, 0.92) | 0.038 | |
| Myalgia | |||||
| COVID-19 vaccine | Non-Vaccinated | Reff. | Reff. | ||
| 1st dose | 1.99 (0.64, 6.16) | 0.233 | 2.51 (0.71, 8.81) | 0.152 | |
| 2nd dose | 2.61 (0.93, 7.31) | 0.067 | 3.61 (1.14, 11.40) | 0.029 | |
| Booster dose | 2.16 (0.75, 6.25) | 0.155 | 3.46 (1.03, 11.59) | 0.044 | |
| Concentration Problem | |||||
| COVID-19 vaccine | Non-Vaccinated | Reff. | Reff. | ||
| 1st dose | 1.99 (0.64, 6.16) | 0.233 | 2.36 (0.66, 8.27) | 0.178 | |
| 2nd dose | 2.79 (0.99, 7.80) | 0.051 | 3.78 (1.20, 11.90) | 0.023 | |
| Booster dose | 2.37 (0.82, 6.84) | 0.111 | 3.72 (1.11, 12.41) | 0.033 | |
| Problems with Planning | |||||
| Living Area | Rural | Reff. | Reff. | ||
| Semi-urban | 1.41 (0.76, 2.60) | 0.279 | 2.64 (1.16, 6.03) | 0.021 | |
| Urban | 1.42 (0.79, 2.55) | 0.245 | 2.92 (1.27, 6.71) | 0.011 | |
| Occupation | Day labor | Reff. | Reff. | ||
| Service holder | 0.68 (0.33, 1.38) | 0.282 | 0.25 (0.09, 0.72) | 0.010 | |
| Health Professionals | 0.75 (0.25, 2.31) | 0.623 | 0.29 (0.07, 1.22) | 0.092 | |
| Law enforcement | 0.81 (0.33, 2.02) | 0.655 | 0.31 (0.09, 1.06) | 0.061 | |
| Housewife | 1.06 (0.48, 2.33) | 0.892 | 0.54 (0.18, 1.64) | 0.276 | |
| Student | 0.89 (0.40, 1.96) | 0.767 | 0.30 (0.08, 1.08) | 0.065 | |
| Unemployed | 0.58 (0.18, 1.85) | 0.358 | 0.18 (0.04, 0.83) | 0.029 | |
| Businessman | 0.62 (0.25, 1.56) | 0.311 | 0.26 (0.09, 0.84) | 0.025 | |
| Anxiety | |||||
| COVID-19 vaccine | Non-Vaccinated | Reff. | Reff. | ||
| 1st dose | 1.97 (0.58, 6.65) | 0.275 | 2.14 (0.57, 7.99) | 0.257 | |
| 2nd dose | 2.96 (0.97, 9.00) | 0.056 | 3.68 (1.10, 12.31) | 0.034 | |
| Booster dose | 2.45 (0.78, 7.70) | 0.125 | 3.78 (1.06, 13.47) | 0.040 | |
| Depression | |||||
| Age Category | 18–40 Years | Reff. | Reff. | ||
| 41–60 Years | 0.63 (0.43, 0.93) | 0.018 | 0.43 (0.19, 0.94) | 0.035 | |
| > 61 Years | 1.30 (0.62, 2.73) | 0.480 | 0.68 (0.14, 3.25) | 0.627 | |
| Smoking | Yes | Reff. | Reff. | ||
| No | 0.33 (0.19, 0.58) | < 0.001 | 0.31 (0.16, 0.58) | < 0.001 | |
| PTSD | |||||
| Marital Status | Married | Reff. | Reff. | ||
| Unmarried | 1.25 (0.83, 1.89) | 0.287 | 2.74 (1.25, 5.97) | 0.011 | |
| Widow | 0.00 (0.00, 0.00) | 0.999 | 0.00 (0.00–0.00) | 0.999 | |
| Dizziness | |||||
| COVID-19 vaccine | Non-Vaccinated | Reff. | Reff. | ||
| 1st dose | 2.30 (0.83, 6.40) | 0.111 | 2.03 (0.64, 6.51) | 0.232 | |
| 2nd dose | 2.76 (1.13, 6.76) | 0.026 | 2.93 (1.03, 8.29) | 0.042 | |
| Booster dose | 2.30 (0.90, 5.85) | 0.081 | 2.95 (0.97, 8.92) | 0.056 | |
| Sleep Disturbance | |||||
| Occupation | Day labor | Reff | Reff. | ||
| Service holder | 2.30 (1.18, 4.48) | 0.014 | 2.588 (1.011,6.63) | 0.047 | |
| Health Professionals | 18.17 (2.24, 147.54) | 0.007 | 20.923 (2.23, 196.09) | 0.008 | |
| Law enforcement | 1.91 (0.80, 4.56) | 0.143 | 1.664 (0.55, 5.05) | 0.369 | |
| Housewife | 2.36 (1.12, 4.94) | 0.024 | 3.238 (1.16, 9.02) | 0.025 | |
| Student | 1.88 (0.90, 3.92) | 0.093 | 1.417 (0.42, 4.80) | 0.575 | |
| Unemployed | 1.75 (0.55, 5.56) | 0.340 | 1.377 (0.32, 5.96) | 0.669 | |
| Businessman | 2.35 (0.94, 5.85) | 0.067 | 2.632 (0.86, 8.05) | 0.090 | |
| Diarrhea | |||||
| COVID-19 vaccine | Non-Vaccinated | Reff. | Reff. | ||
| 1st dose | 2.73 (0.97, 7.69) | 0.058 | 3.83 (1.19, 12.28) | 0.024 | |
| 2nd dose | 1.88 (0.77, 4.58) | 0.163 | 2.13 (0.78, 5.85) | 0.142 | |
| Booster dose | 1.80 (0.71, 4.55) | 0.216 | 2.09 (0.71, 6.12) | 0.182 | |
| Weight Loss | |||||
| Educational Background | No formal education | Reff. | Reff. | ||
| Primary education | 2.76 (0.79, 9.56) | 0.110 | 2.70 (0.62, 11.66) | 0.184 | |
| Secondary education | 5.21 (1.51, 17.96) | 0.009 | 6.16 (1.37, 27.73) | 0.018 | |
| Higher secondary education | 7.41 (2.18, 25.16) | 0.001 | 6.93 (1.49, 32.15) | 0.013 | |
| Bachelor or above | 4.31 (1.37, 13.56) | 0.012 | 3.64 (0.76, 17.34) | 0.105 | |
| Smoking | Yes | Reff. | Reff. | ||
| No | 0.43 (0.20, 0.91) | 0.028 | 0.32 (0.13, 0.79) | 0.014 | |
| Visual Problems | |||||
| Age | 1.00 (0.99, 1.02) | 0.638 | 1.05 (1.00, 1.09) | 0.039 | |
| Sore Throat | |||||
| Occupation | Day labor | Reff. | Reff. | ||
| Service holder | 1.84 (0.78, 4.33) | 0.162 | 5.00 (1.43, 17.45) | 0.012 | |
| Health Professionals | 4.04 (0.00, 9.23) | 0.998 | 9.91 (0.00, 14.39) | 0.998 | |
| Law enforcement | 3.25 (0.82, 12.96) | 0.095 | 8.35 (1.57, 44.56) | 0.013 | |
| Housewife | 2.25 (0.83, 6.14) | 0.113 | 4.48 (1.10, 18.23) | 0.036 | |
| Student | 1.09 (0.44, 2.72) | 0.847 | 1.10 (0.18, 6.86) | 0.918 | |
| Unemployed | 4.04 (0.00, 9.23) | 0.998 | 1.38 (0.00, 3.45) | 0.998 | |
| Businessman | 2.92 (0.73, 11.68) | 0.130 | 7.79 (1.49, 40.64) | 0.015 | |
OR: ODDs Ratio; CI: Confidence Interval; *p < 0.05; **p < 0.01; ***p < 0.001; Binary Logistic
The presence of comorbid UTIs and cholesterol was a significant predictor of PCC symptom cough (OR = 18.35, 95% CI = 1.86–181.35, p = 0 0.013; OR = 9.06, 95% CI = 1.78–46.03, p = 0.008). Having a history of cholesterol was associated with a six-times greater chance of developing fever (OR = 6.67, 95% CI = 1.22–36.59, p = 0 0.029) and CKD was associated with a two-times greater chance of developing diarrhea (OR = 1.84, 95% CI = 1.03–3.29, p = 0.041) as presented in Table 5.
Table 5.
Predictors of post-COVID-19 symptoms by comorbidities
| Independent variable | Sub category | Unadjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value |
|---|---|---|---|---|---|
| Cough | |||||
| UTI | No | Reff. | Reff. | ||
| Yes | 7.49 (1.04, 54.16) | 0.460 | 18.35 (1.86, 181.35) | 0.013 | |
| Cholesterol | No | Reff. | Reff. | ||
| Yes | 4.54 (1.06, 19.48) | 0.421 | 9.06 (1.78, 46.03) | 0.008 | |
| Fever | |||||
| Cholesterol | No | Reff. | Reff. | ||
| Yes | 4.45 (0.89, 22.26) | 0.069 | 6.67 (1.22, 36.59) | 0.029 | |
| Skin Rash | |||||
| IHD | No | Reff. | Reff. | ||
| Yes | 0.59 (0.31, 0.98) | 0.043 | 0.46 (0.24, 0.88) | 0.020 | |
| Diarrhea | |||||
| CKD | No | Reff. | Reff. | ||
| Yes | 1.84 (1.07, 3.16) | 0.026 | 1.84 (1.03, 3.29) | 0.041 | |
OR: ODDs Ratio; CI: Confidence Interval; *P < 0.05; **P < 0.01; ***P < 0.001; UTI: Urinary Tract Infection; IHD: Ischemic Heart Disease; CKD: Chronic Kidney Disease; Binary Logistic
Discussion
The study’s objective was to estimate the population proportion of post-COVID-19 conditions (PCCs) in Bangladesh with a two-year follow-up study and to determine the case-fatality and morbidity rates of PCC. Furthermore, this study aimed to identify the predictive factors for PCC morbidity in Bangladesh. The study’s key results included 465 (89.27%) patients out of 522 who had consistent PCCs two years after follow-up. The case-fatality rate was 1.92% (10 out of 522), and the recovery rate was 9.0% (47 out of 522). The clinical characteristics of PCC patients were mostly similar to those in previous studies conducted in Bangladesh. The significant symptoms included fatigue at 89.2%, chest pain at 43.7%, muscle pain at 64.9%, cognitive problems at 63.2%, musculoskeletal problems at 68.2%, headache at 74.2%, and anxiety at 69.7%. The regression analysis revealed that the factors significantly associated with PCC were geographical distribution, vaccination status, comorbidities, and a longer duration of symptoms or having multiple symptoms. The PCC documented a prevalence of post-COVID-19 conditions at a rate of 3.6%. A systematic review and meta-analysis study found that the prevalence rate ranged from 43 to 51% [4], while prior studies conducted in Bangladesh revealed a prevalence rate ranging from 16.1 to 25.2% [5, 6]. The incidence of PCC is declining; however, the pace of recovery remains low. The study found a recovery rate of 9.0%. Other studies have reported comparable outcomes [22].
In order to ascertain the fatality of a condition, it is essential to determine the case-fatality rate. The case fatality rate of PCC in Bangladesh was 1.92% in this cohort study. A case-control study utilized a comprehensive commercial insurance database to identify a PCC cohort’s higher incidence of adverse effects over a one-year period. The study found a case-fatality rate of 2.8% for PCC in the USA. [23]. The case fatality rate of various COVID-19 variants was reported in a systematic review and meta-analysis (Alpha: 2.62%, Beta: 4.19%, Gamma: 3.60%, Delta: 2.01%, Omicron: 0.70%). Additionally, disparities in case fatality rates were observed among continents. In general, the case fatality rate of COVID-19 in Europe and Oceania was marginally lower than that of other continents [24]. Another study found, individuals who contracted SARS-CoV-2 were at a case-fatality rate that was more than three times that of those who did not contract the virus in the subsequent year [25]. The lack of evaluation of autopsy results makes it difficult to determine whether post-COVID-19 conditions or any other comorbid conditions were the primary cause of case-fatality.
Strengths and limitations
This pioneering study aimed to investigate the prevalence of PCC in Bangladesh over a two-year period. This article contributes valuable insights into the recovery and death rates, as well as the predicted indicators of morbidity, associated with PCC in Bangladesh. This report also presented a clear indication of the attributable risk of PCC for the population under study. Employing a questionnaire administered through interviews, this research sought to enhance data precision. The results may have wider applicability due to the utilization of a random sampling approach that includes the whole population, hence minimizing selection bias. Including the whole population of the country might improve the generalizability of the findings. Nevertheless, there are some limitations to this study. The sample size calculation data were derived by considering an inter-cluster correlation of 1.3, on the assumption that there would be no significant differences among the demographic cohorts in different districts. Actually, the districts in Dhaka had a greater number of respondents, but there was an imbalance in the distribution of respondents among the divisions. To overcome this constraint, we determined the least required sample size and then conducted the study with a sample size that exceeded this minimum requirement. We were unable to reach a significant number of potential participants over the phone because they refused to participate, either because they were too sick or because their careers were too busy to respond, some of whom may have had symptoms. However, we could not addressed minimize potential factors that could influence the correlation between the observed PCC and COVID-19 for example, the number of vaccine doses received, or any interventions. An autopsy could have determined the exact cause of death in cases where people were claiming that death was due to post-COVID symptoms, which is another limitation of the present study. With specific information, the case-fatality rate of patients with PCC could be determined more precisely.
Implications of the study
This study has significant potential in implicating in healthcare services, policies and further research programs. This study fills the research gap on incidence, case-fatality and recovery of post-COVID-19 conditions (PCC) in Bangladesh. This will support the necessity of future epidemiological research, healthcare policy making and estimating healthcare costs. This study revealed the persistent symptoms that may lead to a greater disease burden and potential healthcare crisis. Managing long-term PCC symptoms requires symptom response tracking, and our study will support the determination of the clinical management of PCC. According to this study attributable risk of PCC, the episodic pattern is well understood in promoting the health of individuals with PCC in Bangladesh.
Recommendations
Therefore, it is important to perform future research that examines the primary cluster of PCC, including its neurological or neurophysiological effects, as well as its impact on chronic fatigue syndrome and other debilitating disorders.
Conclusions
This study comprehensively analyses the epidemiology of post-COVID-19 conditions in Bangladesh. The occurrence, death, illness, and recovery rates from July to December 2021–2023. By utilizing the clinical diagnostic criteria established by the World Health Organization (WHO) for PCC and performing screenings in households across eight districts, this study determined that the incidence of PCC was 3.6%, the death rate was 1.92%, and the recovery rate was 9.0%. This study identified important factors that strongly influence the occurrence of PCC morbidity, such as geographical distribution, vaccination status, the presence of other medical conditions, and the duration of symptoms. This groundbreaking study, representing Bangladesh’s first comprehensive investigation into the effects of PCC, highlights the urgent need for continuous monitoring of PCC patients over time and additional research to improve recovery methods. This study provides valuable knowledge for public health strategies addressing the enduring consequences of COVID-19.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- PCC
Post COVID-19 conditions
- C19-YRS
Yorkshire Rehabilitation Scale
- PTSD
Post-traumatic stress disorder
- DM
Diabetes Mellitus
- HTN
Hypertension
- CKD
Chronic Kidney Disease
- STROBE
Strengthening the reporting of observational studies in epidemiology
Author contributions
Conceptualisation: AHS, MFK, KMAH, TH, SA, RA, MWI & IKJ, Funding acquisition: KMAH, SJ, MZH, TH & IKJ, Methodology: AHS, MFK, MZH, TH, SA, RA, MWI & IKJ, Project administration: AHS, MFK, KMAH, SJ, MZH, TH, SA, RA, MWI, IKJ, Supervision: KMAH, SJ & IKJ, Validation: AHS, KMAH, SJ, MZH, TH, RA & IKJ, writing – original draft: AHS, MFK, KMAH, SJ, MZH, TH, SA, RA, MWI & IKJ, Writing – review & editing: AHS, MFK, KMAH, SJ, MZH, TH, SA, RA, MWI & IKJ.
Funding
This study obtained partial funding for data collection from Jashore University of Science and Technology through the University Grants Commission (UGC) of the People’s Republic of Bangladesh as part of a doctoral project (Grant No.: 23-FoBST-06).
Data availability
The data was available on an electronic data site. [Hossain, Altaf (2024), “PCC cohort”, Mendeley Data, V1, doi: 10.17632/jdks6ym88v.1]
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization: WHO. Post COVID-19 condition (Long COVID) [Internet]. 2022. https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition.
- 2.Coronavirus disease (COVID-19). Post COVID-19 condition [Internet]. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition.
- 3.Mateu L, Tebé C, Loste C, Santos JR, Lladós G, López CR et al. Determinants of the onset and prognosis of the post-COVID-19 condition: a 2-year prospective observational cohort study. The Lancet Regional Health - Europe [Internet]. 2023;33:100724. 10.1016/j.lanepe.2023.100724. [DOI] [PMC free article] [PubMed]
- 4.Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long covid: a meta-analysis and systematic review. J Infect Dis. 2022;226(9):1593–607. 10.1093/infdis/jiac136. 10.1093/infdis/jiac136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hossain MA, Hossain KM, Saunders K, et al. Prevalence of long covid symptoms in Bangladesh: a prospective inception cohort study of covid-19 survivors. BMJ Global Health. 2021;6(12). 10.1136/bmjgh-2021-006838. [DOI] [PMC free article] [PubMed]
- 6.Chakrovorty SK, Hossain KM, Hossain MA, Ahammad S, Kabir MF, Shafin R, et al. Predictors of and factors associated with novel post covid symptoms in the musculoskeletal, functional, and cognitive domains for vaccinated delta-variant survivors: a descriptive survey of a nationwide prospective inception cohort in Bangladesh. SSRN Electron J. 2022. 10.2139/ssrn.4249920. 10.2139/ssrn.4249920 [DOI] [Google Scholar]
- 7.Ruf W. Immune damage in Long Covid. Science [Internet]. 2024;383(6680):262–3. 10.1126/science.adn1077. [DOI] [PubMed]
- 8.Kabir MF, Yin KN, Jeffree MS, Ahmedy FB, Zainudin MF, Htwe O, Jahan S, Hossain MZ, Hossain KA. Al Mukit10 MA, Hossain11 T. comparing effectiveness of telerehabilitation versus institution-based adapted physical activity and therapeutic exercise program on fatigue, physical functioning, and episodic disability for chronic fatigue syndrome in long covid-19: protocol for a randomized control trial. Chelonian Res Foundation. 2023;18(2):1380–95. 10.18011/2023.11(2).1380.1395. 10.18011/2023.11(2).1380.1395 [DOI] [Google Scholar]
- 9.Kabir MF, Yin KN, Jeffree MS, Ahmedy FB, Jahan S, Islam MW, Jahid IK, Sivan M, Chakrovorty SK, Hossain KA. Profile of long COVID symptoms needing rehabilitation: a cross-sectional household survey of 12,925 SARS-CoV-2 cases between July and December 2021 in Bangladesh. Archives Public Health. 2023;81(1):132. 10.1186/s13690-023-01140-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front Microbiol. 2021;12:1494. 10.3389/fmicb.2021.698169. 10.3389/fmicb.2021.698169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar A, Arora A, Sharma P, Anikhindi SA, Bansal N, Singla V, et al. Is diabetes mellitus associated with case-fatality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2020;14:535–45. 10.1016/j.dsx.2020.04.044. 10.1016/j.dsx.2020.04.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–38. 10.1007/s00392-020-01626-9. 10.1007/s00392-020-01626-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–10. 10.1001/jamacardio.2020.0950. 10.1001/jamacardio.2020.0950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharif N, Ahmed SN, Opu RR, Tani MR, Dewan D, Daullah MU, et al. Prevalence and impact of diabetes and cardiovascular disease on clinical outcome among patients with COVID-19 in Bangladesh. Diabetes Metab Syndr: Clin Res Rev. 2021;15:1009–16. 10.1016/j.dsx.2021.05.005. 10.1016/j.dsx.2021.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:811–2. 10.1001/jamacardio.2020.1017. 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cuschieri S, Grech S. COVID-19 and diabetes: the why, the what and the how. J Diabetes Complications. 2020;34:107637. 10.1016/j.jdiacomp.2020.107637. 10.1016/j.jdiacomp.2020.107637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stengel S, Gölz L, Kolb JF, Tarbet K, Völler S, Koetsenruijter J et al. First insights into multidisciplinary and multispecialty long COVID networks—a SWOT analysis from the perspective of ambulatory health care professionals. Frontiers in Medicine [Internet]. 2023;10. 10.3389/fmed.2023.1251915. [DOI] [PMC free article] [PubMed]
- 18.Bangladesh population (live) accessed via Worldometer. 2021. Available: https://www.worldometers.info/world-population/bangladesh-population/.
- 19.Carson G. Research priorities for Long Covid: refined through an international multi-stakeholder forum. BMC Medicine [Internet]. 2021;19(1). 10.1186/s12916-021-01947-0. [DOI] [PMC free article] [PubMed]
- 20.O’Connor RJ, Preston N, Parkin A, Makower S, Ross D, Gee J, Halpin SJ, Horton M, Sivan M. The COVID-19 Yorkshire Rehabilitation Scale (C19‐YRS): application and psychometric analysis in a post‐COVID‐19 syndrome cohort. J Med Virol. 2022;94(3):1027–34. 10.1002/jmv.27415. 10.1002/jmv.27415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fei Z, Ryeznik Y, Sverdlov O, Tan CW, Wong WK. An overview of healthcare data analytics with applications to the COVID-19 pandemic. IEEE Transactions on Big Data [Internet]. 2021;1. 10.1109/tbdata.2021.3103458.
- 22.Ballouz T, Menges D, Anagnostopoulos A, Domenghino A, Aschmann HE, Frei A, Fehr JS, Puhan MA. Recovery and symptom trajectories up to two years after SARS-CoV-2 infection: population based, longitudinal cohort study. BMJ. 2023;381. 10.1136/bmj-2022-074425. [DOI] [PMC free article] [PubMed]
- 23.DeVries A, Shambhu S, Sloop S, Overhage JM. One-Year Adverse Outcomes Among US Adults with Post–COVID-19 Condition vs Those Without COVID-19 in a Large Commercial Insurance Database. InJAMA Health Forum 2023 Mar 3 (Vol. 4, No. 3, pp. e230010-e230010). American Medical Association. 10.1001/jamahealthforum.2023.0010. [DOI] [PMC free article] [PubMed]
- 24.Xia Q, Yang Y, Wang F, Huang Z, Qiu W, Mao A. Case fatality rates of COVID-19 during epidemic periods of variants of concern: A meta-analysis by continents. International Journal of Infectious Diseases [Internet]. 2024;141:106950. 10.1016/j.ijid.2024.01.017. [DOI] [PubMed]
- 25.Uusküla A, Jürgenson T, Pisarev H, Kolde R, Meister T, Tisler A et al. Long-term mortality following SARS-CoV-2 infection: A national cohort study from Estonia. the Lancet Regional Health Europe [Internet]. 2022;18:100394. 10.1016/j.lanepe.2022.100394. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data was available on an electronic data site. [Hossain, Altaf (2024), “PCC cohort”, Mendeley Data, V1, doi: 10.17632/jdks6ym88v.1]