Abstract
Background:
Diabetes mellitus is a chronic metabolic disorder with substantial implications for public health. Understanding the factors influencing blood sugar fluctuations is crucial for effective diabetes management and prevention. This study aimed to evaluate factors associated with blood sugar changes in diabetic patients and healthy individuals attending the Sabzevar Persian Cohort Center, employing the growth curve model.
Materials and Methods:
Data related to 589 diabetic patients and 589 non-diabetic patients participating in the Persian cohort study of Sabzevar were used. Due to the repetition of blood sugar measurements for each individual over time, we use the conditional latent growth curve model to examine intra-individual changes and variables that affect these changes over time.
Results:
The linear latent growth curve model, fitted with independent variables, exhibited a superior fit. The slope of the line for the diabetic group was measured at 1.78, while for the non-diabetic group, it was estimated to be -0.29. Within the diabetic group, the influence of age, the presence of fatty liver, and history of congenital heart disease (CHD) had a significant impact on the baseline (the intercept), and the effect of body mass index (BMI) on the changing trend of the response variable (slope) was also significant. In the non-diabetic group, significant effects were observed for age variables, BMI, family history of diabetes, and history of stroke in the family.
Conclusion:
Overall, the linear latent growth curve model showed good performance in the evaluation of the factors related to blood sugar changes in diabetic patients and healthy people.
Keywords: Adult, blood glucose, diabetes mellitus, non-linear dynamics
INTRODUCTION
Diabetes is a pressing global health concern, burdening healthcare systems, causing irreversible complications, and affecting the quality of life for millions of people.[1] This group of metabolic diseases is characterized by chronic hyperglycemia, which results from impaired insulin secretion, action, or a combination of both. It disrupts the metabolism of carbohydrates, lipids, and proteins.[2] Chronic hyperglycemia underlies both acute and long-term complications, impacting various organs like the heart, blood vessels, eyes, kidneys, and nerves. This has propelled diabetes into the spotlight as a twenty-first-century global health crisis.[3] Prolonged high blood glucose levels are closely linked to chronic complications.[4] The diabetes epidemic is fueled by a complex interplay of factors, including genetic predisposition, cultural shifts, population aging, urbanization, dietary changes, reduced physical activity, unhealthy lifestyles, and behavioral choices.[5] Key elements like age, gender, obesity, and blood pressure significantly influence diabetes development.[6,7] Inadequate control and management require substantial financial resources for diabetes treatment and complications.[8] Studies have shown that many patients, especially in Asian regions, do not achieve optimal control.[9,10]
Diabetes is often referred to as a “silent epidemic” and constitutes a significant public health challenge, accounting for 9% of global deaths.[10] This endocrine disorder affects over 100 million individuals annually, ranking as the seventh leading cause of death. The future is even more concerning, with the number of people living with diabetes expected to surge from 171 million in 2000 to 366 million by 2030.[11] In Iran, it's the most prevalent non-communicable disease, affecting over 3 million people with a prevalence rate of 7% for diagnosed diabetes and 13% for undiagnosed cases among adults, equating to nearly 20% of the population at risk.[12] In 2016, diabetes was responsible for approximately 2% of all deaths in Iran.[13] Managing diabetes is complex due to the lack of a definitive cure. Lifestyle modifications are essential, encompassing physical exercise, dietary changes, weight management, smoking cessation, medication adherence, blood sugar monitoring, and daily health-related planning. Effective communication with healthcare professionals plays a crucial role in managing this condition.[13] Diabetes can be asymptomatic in its early stages, with patients often diagnosed incidentally. As blood sugar levels rise, symptoms become more pronounced, including frequent urination, excessive thirst, increased appetite with unexplained weight loss, fatigue, and blurred vision. Many individuals live with undiagnosed diabetes for several years, risking the development of complications.[14] Thus, emphasizing self-care behaviors is vital as lapses can increase the risk of complications. Understanding the progression and treatment effectiveness of diseases requires a longitudinal approach in medical science. This approach involves repetitive measurements to investigate changes over time. For diabetes, a growth curve model is suitable for analyzing longitudinal data. It estimates the trajectory and extent of changes in the disease over time, considering factors influencing these changes.[15]
This study primarily focuses on utilizing longitudinal data and employs the growth curve model to scrutinize alterations in blood sugar levels among diabetic patients over time, while also measuring the risk factors involved. It's essential to underscore that previous research has primarily centered on the incidence and prevalence of diabetes, primarily relying on cross-sectional data. The main objective of this investigation is to model the changes in fasting blood sugar levels within diabetic patients as they evolve over time. As a consequence, this study is conducted with the overarching goal of probing into the dynamics of blood sugar variables, quantifying these changes, and identifying the factors that influence them. The outcomes of this research hold valuable insights for healthcare professionals and stakeholders involved in the provision of care, support, and treatment to diabetic patients. We aspire that this research will empower diabetic patients to gain a deeper understanding of the factors influencing their condition and aid healthcare and treatment researchers in designing targeted intervention programs for diabetic patients.
MATERIALS AND METHODS
Study area and Persian cohort settings
In the current investigation, we have employed data pertaining to diabetic patients who are actively enrolled in the Persian cohort study within the city of Sabzevar. The Persian cohort study, in its essence, represents a forward-looking, long-term research initiative that targets a representative segment of the Iranian population. This extensive study encompasses a vast cohort of approximately 180,000 individuals falling within the age range of 35 to 70 years. It encompasses participants hailing from 19 geographically diverse regions across Iran.[16,17,18]
Initiated by the Ministry of Health in 2014, this extensive cohort study is a collaborative effort involving multiple medical sciences universities across various regions of Iran. The primary objective of this study is to assess the prevalence and incidence of non-communicable diseases, along with an exploration of the associated risk factors. Importantly, it takes into account the influence of various cultural practices and lifestyles, as well as environmental factors that can either positively or negatively impact disease development.[16,17] Notably, the Sabzevar cohort study represents a specific subset of the larger Persian cohort initiative, focusing on the region in the northeastern part of Iran, particularly within the confines of the Tawheed town situated in Sabzevar.[18,19]
The total population of Sabzevar for all age groups is 301,340 people, including 151,269 men and 150,071 women, and for the ages of 35 to 70, there are 112,165 people, including 56,424 men and 55,744 women. The total population living in Tawheed town for all age groups is 21,973 people, including 10,790 men and 11,183 women, and 8,960 people between the ages of 35 and 70, including 4,561 men and 4,390 women. This part of the city has been chosen because it has the lowest immigration rate and has the distribution of different ethnicities and races of Sabzevar, and it is possible to follow up the participants in the program for a long time. By sequential sampling method, 5174 people between the ages of 35 and 70 were invited to participate by telephone. In the first phase of the project, which started in February 2016, all these people have referred to the cohort center under the name of Persian Cohort, which was set up for this purpose. First, consent was obtained from the people, then personal, social and economic information, their status in terms of physical activity, personal habits, as well as information related to their diseases, all information related to their examinations has been recorded. In the second phase of the research, which started from February 2020, people were re-examined, and then in the third phase, which continued from February 2021 to February 2022, people were measured in terms of all research variables.[19]
Our study participants
This is a prospective cohort study that follows diabetics patients from 2016 to 2022 and their data is collected. In this investigation, all individuals diagnosed with diabetes who were participants in the Persian cohort study were selected through a comprehensive census. However, it was imperative to determine the minimum requisite sample size for this study, which was determined using the following methodology.
An initial sample of 99 individuals from the Persian cohort was utilized for preliminary data collection. The mean and variance of blood sugar levels in the first stage of this sample were computed as 170.52 and 71.5, respectively, while the corresponding figures for the second stage were 173.46 and 61.8. The estimation of the overall variance in blood sugar levels among the subjects was determined to be 66.65, assuming a constant correlation between repeated measurements. The correlation estimate between the first and second repetitions of blood sugar measurements within the sample was found to be 0.455. Subsequently, utilizing a statistical approach, the sample size was calculated with a 99% confidence level and 99% statistical power, yielding an approximate sample size of 240 individuals based on the specified criteria. In order to enhance the robustness and reliability of the study, all 589 diabetic patients were subjected to a comprehensive examination in a three-stage process.
The study's inclusion criteria were rigorously established, with age serving as the primary determinant, exclusively encompassing individuals aged between 35 and 70 years. This age range represented a fundamental prerequisite for prospective participants. Moreover, residential eligibility constituted another pivotal factor, mandating that individuals resided within the predefined geographic area to qualify for inclusion. Immigrants to this area were required to demonstrate a minimum one-year residency, while non-immigrants were expected to maintain a residency within the city for at least nine months annually. The criterion of Iranian nationality was strictly enforced, validated through the possession of both a national identification card and a birth certificate. Any individuals failing to meet these nationality prerequisites had their data expunged from the study's records. In contrast, the exclusion criteria encompassed individuals with communication impairments, which included individuals who were deaf, blind, mute, or afflicted with severe mobility limitations that impeded their ability to visit the cohort center. Furthermore, individuals with untreated mental retardation or acute psychiatric disorders such as psychosis were ineligible and subsequently excluded from our study. Finally, from 4260 people who participated in the Sabzeavr Persian cohort study, 589 diabetics, and 589 non-diabetic people were randomly selected for our study. The sample subjects in this study underwent three annual measurements, where the blood sugar variable was considered as the dependent variable, and the weight variable served as the independent variable. Additional qualitative variables, such as gender, the presence of fatty liver, and personal and family medical history, including stroke, brain conditions, diabetes, and heart diseases, were also incorporated into the analysis. Additionally, the height variable was included as a quantitative factor within the model. Data for this research were collected through a specifically designed questionnaire at the cohort center. The questionnaire is organized into three distinct sections:
Demographic Information: This first segment captures vital demographic data, encompassing gender, age, height, and weight, collected as quantitative variables. Gender is a qualitative variable.
Personal and Family Medical History: The second part of the questionnaire inquires about personal and familial medical history, including the presence of diabetes and heart diseases. These are measured qualitatively.
Clinical Test Results: The third and final segment focuses on clinical test results, particularly blood sugar levels measured in milligrams per deciliter. To perform blood sugar measurements, patients visit a specialized laboratory within the cohort center on a designated date, typically while in a fasting state. Subsequently, a 25 cc blood sample is obtained and analyzed in accordance with the blood sugar measurement protocol outlined in the Persian cohort guidelines.[19]
Conditional latent growth curve model
Due to the repetition of blood sugar measurements for each individual over time, we use the conditional latent growth curve model to examine intra-individual changes and variables that affect these changes over time. The first level of the equation of the growth curve model mathematically explains the relationship between the response variable and time as follows:
Y = β0 + β1t
In this equation, β0 is the constant value (value of the response variable at zero time); β1 is the linear coefficient of the model that expresses the average changes of the response variable over time. The response variable value (blood sugar) observed for sample i st at time t, yit is as follows:
yit = βoi + β1it + εit
εit represents the term of random error or the difference of the actual observed value yit from the predicted value. It is assumed that the error sentences are independent and have the same distribution. This means that all εits have the same distribution and each particular εit does not provide information about the values of other εits. Level 2 of the model is defined as follows for βoi and β1i coefficients.
βoi = ηoo + η01X + γoi
β1i = η10 + η11X + γ1i
The constant value of the response variable (βoi) is modeled in terms of the average constant value of the population (η00) and the coefficients ηo1 for the characteristics of X and the random error term at the individual level γoi. The annual changes of the response variable are expressed in terms β1i of This value is also modeled according to the fixed values of the population and independent variables and the error term γ1i.[20,21]
The conditional latent growth curve model (CLGM) offers advantages over other models for analyzing longitudinal data. It excels in accounting for individual differences in growth trajectories and enables the study of specific factors’ influence on changes over time. This flexibility goes beyond models that focus on average growth patterns across the entire sample, such as linear mixed-effect models (LMM) or hierarchical linear modeling (HLM). The CLGM extends the latent growth curve model (LGCM) by allowing the inclusion of predictors to explain individual differences in growth parameters. This helps researchers assess how various factors affect the rate of change over time. Additionally, the CLGM effectively handles missing data, making it a robust choice for studying dynamic changes while considering the influence of specific variables.[22,23]
To commence our analysis, we will first scrutinize the demographic information and conduct a comparative assessment between two distinct groups. Subsequently, the linear latent growth curve model will be deployed to juxtapose changes in the response variable within both groups: the diabetic and non-diabetic groups. The linear latent growth curve model entails the simultaneous fitting of a growth curve model for each of these groups, and through the application of the Wald test, we shall compare the constants and slopes of the models between the two groups. Upon this comparison, independent variables will be introduced into the model, allowing for the development of a conditional linear latent growth curve model. The model's adequacy will be evaluated based on specific fit indices. Values indicative of a well-fitting model include Root Mean Square Error of Approximation (RMSEA) <0.08, Tucker-Lewis Index (TLI) >0.90, Comparative Fit Index (CFI) >0.90, and Standardized Root Mean Square Residual (SRMR) <0.08. Furthermore, Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) criteria will be employed to compare the goodness of fit across different models. All analyses and modelling will be executed using Mplus software version 6.12. A significant level of 0.05 was performed for all analyses.
RESULTS
In this study, there were 589 diabetic patients and 589 non-diabetic patients. 45% of the diabetic patients and 42% of the non-diabetic patients were male, and the other samples were female. There was no significant difference between male and female ratio in two groups (P = 0.211). The average age and body mass index (BMI) of the diabetic group were significantly higher than the non-diabetic group (P < 0.001). The proportion of fatty liver in the diabetic group (25%) was higher than the non-diabetic group (14%), and this difference was statistically significant. Also, the ratio of family history of diabetes and family history of heart disease in the diabetic group was significantly higher than the non-diabetic group [Table 1].
Table 1.
Comparison of mean and ratio of studied variables using independent t-test and Chi-square
| Variable | Non-Diabetic | Diabetic | P |
|---|---|---|---|
| aAge | |||
| Average±SD | 47.39±8.49 | 7.75±54.54 | P<0.001 |
| aBody mass index | |||
| Average±SD | 28.15±4.46 | 29.25±4.74 | P<0.001 |
| bGender | |||
| Male (%) | 250 (7.41%) | 267 (3.45%) | P=0.211 |
| Female (%) | 349 (3.58%) | 322 (7.54%) | |
| bFatty liver | |||
| Has (%) | 84 (1.14%) | 147 (0.25%) | P<0.001 |
| No (%) | 510 (9.85%) | 442 (0.75%) | |
| bFamily history of diabetes | |||
| Has (%) | 232 (7.38%) | 385 (4.65%) | P<0.001 |
| No (%) | 367 (3.61%) | 204 (6.34%) | |
| bFamily history of heart disease | |||
| Has (%) | 250 (7.41%) | 281 (8.47%) | P=0.036 |
| No (%) | 349 (3.57%) | 307 (2.52%) | |
| bStroke in the family | |||
| Has (%) | 157 (2.26%) | 158 (8.26%) | P=0.810 |
| No (%) | 442 (8.73%) | 431 (2.73%) | |
aComparison of the mean of the two groups using the independent t-test.
bCompare the ratios of the two groups using the Chi-square test
In the next step, the linear latent growth curve model was fitted once without the effect of independent variables and then with independent variables. The goodness-of-fit indices of the two models in Table 2 were RMSEA <0.08, CFI >0.95, TLI >0.95, and SRMR <0.08, indicating that both models had an acceptable fit. However, considering that the values of AIC, BIC, and ABIC were reduced for the conditional model, it can be said that the conditional model had a better fit.
Table 2.
Goodness indices of linear latent growth curve model fit and conditional linear latent growth curve model
| Goodness indicators fit | Linear latent growth curve model | Conditional linear latent growth curve model |
|---|---|---|
| AIC | 34063.76 | 33741.91 |
| BIC | 34145.05 | 33944.81 |
| ABIC | 34094.23 | 3381.76 |
| RMSEA (90% CI) | 0.00 (0.00-0.045) | 0.00 (0.00-0.045) |
| CFI | 1 | 1 |
| TLI | 1 | 1 |
| SRMR | 0.005 | 0.015 |
The results of the linear latent growth curve model without the effect of independent variables are reported in Table 3. As can be seen, the intercept for diabetic and non-diabetic groups was 169.40 and 96.91, respectively, and was statistically significant. The constant value actually represents the average value of the response variable at the starting point. As can be seen, the two groups were significantly different in terms of blood sugar at the beginning of the study (constant value coefficient) and according to the result of the Wald test, this difference was statistically significant. The slope value of the line shows the trend of changes in the response variable over time. The slope of the line was 1.78 for the diabetic group and -0.29 for the non-diabetic group. The interpretation of these coefficients is that for the diabetic group it can be said that in each period the amount of blood sugar in the samples increases by an average of 1.78 units, and also, for the non-diabetic group, it can be said that in each period, the blood sugar level of the samples decreases by 0.29 units on average but the slope of the line was not significant for any of the groups. This means that according to the results of the latent linear growth curve model, the trend of blood sugar changes over time is not significant.
Table 3.
Results of fitting the linear latent growth curve model
| Groups | Intercept (Mean (standard error)) | Line slope (Mean (standard error)) | Covariance |
|---|---|---|---|
| Diabetic | 169.40 (2.65)* | 1.78 (1.87) | -402.46* |
| Non-diabetic | 96.91 (0.48)* | -0.29 (0.36) | 0.77 |
| Wald test result | 722.88* | 1.18 | ---- |
*Is significant at the 0.05 level
According to the results of the Wald test in Table 3, no significant difference was observed between the trends of blood sugar changes between the two groups. The covariance of the line slope and the constant value of the model in the diabetic group were negative and significant. This means that the trend of slope changes is negatively correlated with the initial value at the beginning of the study. As samples with higher blood sugar had less changes. Estimation of the trend of blood sugar changes in the two groups over time using the linear latent growth curve model is shown in Figure 1.
Figure 1.
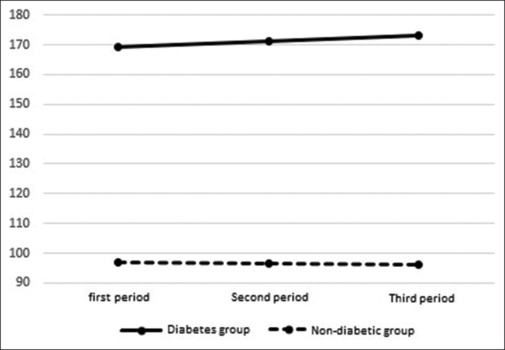
Estimation of changes in blood sugar in the two groups over time
Finally, the conditional linear latent growth curve model was fitted, the results of which are shown in Table 4. In this modified model, the trend of blood sugar changes in both groups (line slope) was significant over time. In the diabetic group, the effect of variables such as age, having fatty liver and family history of heart disease on a constant value and the effect of BMI on the trend of changes in the response variable (line slope) were significant. For interpretation, in the diabetic group, with an increase of one year of age, the amount of blood sugar at the beginning of the study decreases by an average of. 71 units. Also, with an increase of one unit in the BMI, the slope of the line increases by an average of 0.99 units.
Table 4.
Results of fitting the conditional latent growth curve model
| Groups | Auxiliary variable | Intercept (Mean (standard error)) | line slope (Mean (standard error)) |
|---|---|---|---|
| Diabetic | Model | 249.48 (26.64) | -58.16 (19.00)* |
| Age | -0.71 (0.35)* | 0.45 (0.25) | |
| Body mass index | -1.04 (0.56) | 0.99 (0.40)* | |
| Having fatty liver | -22.82 (6.15)* | 5.52 (4.40) | |
| Having a family history of diabetes | 0.67 (5.56) | 2.69 (3.97) | |
| Having a family history of heart disease | -12.10 (5.20)* | 6.77 (3.79) | |
| Having a family history of stroke | 0.94 (5.92) | 0.84 (4.22) | |
| Non-diabetic | Model | 59.21 (3.98)* | 19.51 (3.11)* |
| Age | 0.39 (0.05)* | -0.18 (0.04)* | |
| Body mass index | 0.68 (0.10)* | -0.39 (0.08)* | |
| Having fatty liver | -0.67 (1.31) | -0.36 (1.02) | |
| Having a family history of diabetes | 1.97 (0.94)* | -1.46 (0.74)* | |
| Having a family history of heart disease | -0.49 (0.93) | 0.43 (0.73) | |
| Having a family history of stroke | -3.00 (1.03)* | 1.95 (0.80)* |
* Is significant at the 0.05 level
In the non-diabetic group, the effects of age, BMI, family history of diabetes and family history of stroke on the constant value were significant. For example, the effect of a family history of diabetes on intercept was 1.97, Therefore, those with a family history of diabetes had an average of 1.97 units of blood sugar higher than the others at the beginning of the study. Also, the effect of family history of diabetes on the slope of -1.46 was estimated, which shows that the trend of blood sugar changes for samples with a history of diabetes is on average 1.46 units lower than others. The results can be seen in Table 4.
DISCUSSION
In the realm of medical sciences, the dynamics of diseases over time necessitate close scrutiny to comprehend their evolving nature. This longitudinal study focused on predicting blood sugar changes over time, a crucial undertaking, particularly for diabetic patients when compared to their non-diabetic counterparts.[24] The use of longitudinal data, a hallmark of cohort studies, involves the repeated collection of variables over time. In investigating the factors influencing these variables, it is imperative to consider them as time-varying factors within the model.
The growth curve model, as employed in this study, is a valuable approach for utilizing longitudinal data to estimate the trajectory and magnitude of disease changes over time. Furthermore, it offers insights into the factors intricately linked to these changes, which are themselves subject to variation over time. Notably, it allows the examination of independent variables that also exhibit temporal fluctuations. This model, characterized by fewer assumptions and greater analytical power compared to analogous models, excels in addressing the correlation within observations and the variations between individuals, culminating in a more accurate estimation of model parameters.[25,26]
It is worth emphasizing that longitudinal studies on factors related to blood sugar changes are scarce on a global scale. Notably, there is a dearth of longitudinal research in Iran on the determinants of blood sugar changes. This study thus holds the distinction of being the inaugural investigation conducted on the Iranian population in this regard.[27]
The primary objective of this research was to unravel the intricacies of fasting blood sugar changes over time, discerning the disparities between diabetic and non-diabetic individuals. The employment of the growth curve model, featuring fixed and random values, was instrumental in scrutinizing the longitudinal data, taking into account the correlation within the patients’ blood sugar levels.[27,28]
Among the strengths of this study, the longitudinal design stands out, further enhanced by the application of the conditional linear latent growth curve model for data analysis. This statistical approach, developed to address the limitations of conventional longitudinal data analyses such as repeated measures variance analysis and multivariate variance analysis, provides the flexibility to handle missing data efficiently. Furthermore, it circumvents the need to make assumptions like the uniformity of variance and covariance between repeated measures, a condition known as the assumption of sphericity, which is pivotal in various univariate and multivariate methods. Recent years have seen the rise of growth curve models owing to their versatility in selecting different variance-covariance structures and other critical features, coupled with a lack of restrictive assumptions governing this type of data. Consequently, growth curve models offer an effective means to scrutinize and compare the factors influencing variable changes, all without the encumbrance of assumptions inherent in repeated measures variance analysis. In terms of sample size, this study demonstrates robustness. However, it is essential to acknowledge the study's limitations, which encompass the low number of repetitions (three repetitions for each individual) and the absence of data on the medications employed by diabetic patients as a potential confounding variable. Results revealed a marked difference in the average blood sugar levels between diabetic and non-diabetic individuals at the study's inception, with diabetic patients exhibiting a higher initial blood sugar level.[28] Over the course of the study, blood sugar increased marginally in diabetic patients, while it decreased among non-diabetic individuals. This downward trend is indicative of a linear decline in the average fasting blood sugar level over time. Further analysis considered the interplay of confounding variables, ultimately rendering both the constant value and the slope of the fitted line significant in both groups. This research underscores the preference for employing the linear conditional growth curve model to estimate changes in blood sugar levels throughout the research period, as it offers a more robust approach compared to the linear growth curve model. Within the group of diabetic patients, age, fatty liver, and a family history of heart disease demonstrated a negative relationship with blood sugar levels. This suggests that, as patients age, their blood sugar levels decrease, consistent with findings by Andishmand et al. However, age and fatty liver failed to exhibit a significant relationship with the slope of the fitted line, underscoring the need for a more extended observation period to capture the relationship between these variables and changes in blood sugar. It is crucial to note that the present study spans only a three-year period, which may account for the observed variations in outcomes compared to the research of Abdulahi et al.[27] Furthermore, having a fatty liver and a family history of heart disease correlated negatively with high blood sugar levels at the study's onset in diabetic patients. Conversely, the BMI variable exerted a positive influence on the fitted slope in these patients, indicating that a higher BMI correlated with a more pronounced upward trend in blood sugar levels. This observation aligns with previous studies by Bell et al. and Abdulahi et al.[24,29] In the group of healthy individuals, the variables of age, BMI, and having a family history of diabetes were identified as risk factors influencing the constant value of the fitted line. These findings are congruent with the outcomes of Monahan et al.'s study.[30]
CONCLUSION
In conclusion, this longitudinal study offers valuable insights into the dynamics of blood sugar changes over time in diabetic and non-diabetic individuals, addressing a critical gap in the current literature. The application of the conditional linear latent growth curve model has demonstrated its utility in capturing these changes and their determinants. While the study boasts several strengths, including its longitudinal design and sample size, certain limitations must be acknowledged. Future research endeavors should aim to extend the observation period, incorporate additional variables, and consider potential confounding factors to advance our understanding of blood sugar fluctuations in diverse populations. This study contributes to the body of knowledge surrounding blood sugar changes, providing a foundation for further research and supporting the development of targeted interventions for diabetic and non-diabetic individuals. Ultimately, it is hoped that these findings will empower healthcare professionals and researchers to devise more effective strategies for managing blood sugar levels and enhancing the overall well-being of patients.
Financial support and sponsorship
This study was supported by the Tehran University of Medical Sciences, Tehran, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This article is taken from the epidemiology doctoral thesis in the Department of Epidemiology and Biostatistics, Faculty of Health, Tehran University of Medical Sciences. We hereby thank all the professors of the Epidemiology and Biostatistics Department for their scientific advice. Also, all the employees and officials of Sabzevar Cohort Center who have cooperated in the implementation of this plan are also appreciated.
REFERENCES
- 1.Koo M, Lee M-H, Chang Y-Y, Huang C-F, Chen S-C, Yeh Y-C. Factors associated with self-care behaviors in middle-aged adults and elderly with diabetes mellitus. Hu li za zhi. 2011;58:43–52. [PubMed] [Google Scholar]
- 2.Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. Mcgraw-hill; New York, NY, USA: 2015. Harrison's principles of internal medicine, 19e. [Google Scholar]
- 3.Organization WH Country profiles for diabetes. https://scholar.googleusercontent.com/scholar.enw?q=info:yrYw CWgXKUYJ:scholar.googlecom/&output=citation&scisdr=ClG1gdcB EN7dpgsbNsY:AFWwaeYAAAAAZaEdLsbPFND8VZ_keFpMiq8NhU4&scisig=AFWwaeYAAAAAZaEdLjgD5vNhatf FLOMxfp8TAXE&scisf=3&ct=citation&cd=0&hl=en 2016 [Google Scholar]
- 4.Gomez-Perez FJ, Aguilar-Salinas CA, Almeda-Valdes P, Cuevas-Ramos D, Garber IL, Rull JA. HbA1c for the diagnosis of diabetes mellitus in a developing country. A position article. Arch Med Res. 2010;41:302–8. doi: 10.1016/j.arcmed.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 5.Garg P, Duggal N. Type 2 diabetes mellitus, its impact on quality of life and how the disease can be managed-a review. Obesity Medicine. 2022;35:100459.. [Google Scholar]
- 6.Ciarambino T, Crispino P, Leto G, Mastrolorenzo E, Para O, Giordano M. Influence of gender in diabetes mellitus and its complication. Int J Mol Sci. 2022;23:8850.. doi: 10.3390/ijms23168850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ismail L, Materwala H, Al Kaabi J. Association of risk factors with type 2 diabetes: A systematic review. Comput Struct Biotechnol J. 2021;19:1759–85. doi: 10.1016/j.csbj.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel MR, Resnicow K, Lang I, Kraus K, Heisler M. Solutions to address diabetes-related financial burden and cost-related nonadherence: Results from a pilot study. Health Educ Behav. 2018;45:101–11. doi: 10.1177/1090198117704683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goh CC, Koh KH, Goh S, Koh Y, Tan NC. Achieving triple treatment goals in multi-ethnic Asian patients with type 2 diabetes mellitus in primary care. Malays Fam Physician. 2018;13:10–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Mohan V, Khunti K, Chan SP, Filho FF, Tran NQ, Ramaiya K, et al. Management of type 2 diabetes in developing countries: Balancing optimal glycaemic control and outcomes with affordability and accessibility to treatment. Diabetes Ther. 2020;11:15–35. doi: 10.1007/s13300-019-00733-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 12.Shirinzadeh M, Shakerhosseini R. Nutritional value assessment and adequacy of dietary intake in type 2 diabetic patients. Iranian Journal of Endocrinology and Metabolism. 2009;11:25–32. [Google Scholar]
- 13.Khodakarami R, Abdi Z, Ahmadnezhad E, Sheidaei A, Asadi-Lari M. Prevalence, awareness, treatment and control of diabetes among Iranian population: Results of four national cross-sectional STEPwise approach to surveillance surveys. BMC Public Health. 2022;22:1216.. doi: 10.1186/s12889-022-13627-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diagnosis and classification of diabetes mellitus. https://diabetesjournals.org/care/article-abstract/33/Supplement_1/S62/25777. Diabetes Care. 2010;32(Suppl 1(Suppl 1)):S62–7. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12:14.. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poustchi H, Eghtesad S, Kamangar F, Etemadi A, Keshtkar A-A, Hekmatdoost A, et al. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): Rationale, objectives, and design. American journal of epidemiology. 2018;187:647–55. doi: 10.1093/aje/kwx314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eghtesad S, Mohammadi Z, Shayanrad A, Faramarzi E, Joukar F, Hamzeh B, et al. The PERSIAN cohort: Providing the evidence needed for healthcare reform. Arch Iran Med. 2017;20:691–5. [PubMed] [Google Scholar]
- 18.Ahmadi A, Shirani M, Khaledifar A, Hashemzadeh M, Solati K, Kheiri S, et al. Non-communicable diseases in the southwest of Iran: Profile and baseline data from the Shahrekord PERSIAN Cohort Study. BMC Public Health. 2021;21:2275.. doi: 10.1186/s12889-021-12326-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bakhshimoghaddam F, Jafarirad S, Maraghi E, Ghorat F. Association of dietary and lifestyle inflammation score with type 2 diabetes mellitus and cardiometabolic risk factors in Iranian adults: Sabzevar Persian Cohort Study. Br J Nutr. 2023:1–10. doi: 10.1017/S0007114523001903. [DOI] [PubMed] [Google Scholar]
- 20.Preacher KJ. Latent growth curve modeling. Sage. 2008 [Google Scholar]
- 21.Voelkle MC. Latent growth curve modeling as an integrative approach to the analysis of change. Psychology Science. 2007;49:375.. [Google Scholar]
- 22.Duncan TE, Duncan SC, Strycker LA. An introduction to latent variable growth curve modeling: Concepts, issues, and application. Routledge. 2013 [Google Scholar]
- 23.Little RJ, Rubin DB. Statistical analysis with missing data. John Wiley & Sons. 2019 [Google Scholar]
- 24.Kesavadev J, Misra A, Saboo B, Aravind SR, Hussain A, Czupryniak L, et al. Blood glucose levels should be considered as a new vital sign indicative of prognosis during hospitalization. Diabetes Metab Syndr. 2021;15:221–7. doi: 10.1016/j.dsx.2020.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burant CJ. Latent growth curve models: Tracking changes over time. Int J Aging Hum Dev. 2016;82:336–50. doi: 10.1177/0091415016641692. [DOI] [PubMed] [Google Scholar]
- 26.Wake SK, Zewotir T, Muluneh EK. Analysis of heterogeneous growth changes in longitudinal height of children. J Health Popul Nutr. 2023;42:78.. doi: 10.1186/s41043-023-00425-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdulahi AM, Aguade AE, Yohannis HK. Longitudinal modeling of fasting blood sugar with diabetes: A case study of Adama Hospital Medical College, Ethiopia. Health Sci Rep. 2022;5:e951.. doi: 10.1002/hsr2.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu Y, Zheng X, Li Y, Ye X, Cheng H, Wang H, et al. Exploring patient medication adherence and data mining methods in clinical big data: A contemporary review. J Evid Based Med. 2023;16:342–75. doi: 10.1111/jebm.12548. [DOI] [PubMed] [Google Scholar]
- 29.Bell RA, Arcury TA, Snively BM, Smith SL, Stafford JM, Dohanish R, et al. Diabetes foot self-care practices in a rural, triethnic population. Diabetes Educ. 2005;31:75–83. doi: 10.1177/0145721704272859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeWit SC, Stromberg H, Dallred C. Medical-surgical nursing: Concepts & practice. Elsevier Health Sciences. 2016 [Google Scholar]


