Abstract
Background:
Stroke is a major cause of adult disability, prompting the exploration of innovative rehabilitation methods. Virtual rehabilitation (VR), leveraging technological advances, has gained popularity as a treatment for stroke recovery.
Methodology:
The authors conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) published in English within the last decade, adhering to the PRISMA guidelines. The authors searched databases such as Medline/PubMed, and the Cochrane Library using specific search keywords and Medical Subject Headings (MeSH). The methodological quality was assessed using the PEDro scale, focusing on RCTs involving adult stroke patients undergoing VR rehabilitation, with outcomes related to motor function and quality of life.
Results:
The authors included 15 studies in our meta-analysis. VR rehabilitation offers several advantages over traditional therapy, such as enhanced feedback and increased patient motivation. Engaging VR environments helps improve focus during treatment, potentially boosting recovery from post-stroke impairments. VR therapies significantly benefit motor function, which can improve activities of daily living and overall quality of life.
Conclusion:
VR has demonstrated efficacy in improving motor function and quality of life for stroke survivors. Future research should explore patient variability and refine intervention methods. Incorporating VR into rehabilitation programs could optimize stroke recovery outcomes.
Keywords: exposure therapy, motor function, physical therapy, stroke, virtual rehabilitation
Introduction
Highlights
Stroke is a leading cause of adult disability, driving the exploration of novel rehabilitation methods. Virtual rehabilitation (VR) leverages technological advancements to offer innovative solutions for stroke recovery.
This study presents a comprehensive systematic review and meta-analysis of randomized controlled trials (RCTs) published in the last decade.
VR rehabilitation offers distinct advantages over traditional therapy, including enhanced feedback mechanisms and increased patient motivation. Engaging VR environments facilitate focused treatment sessions, potentially accelerating recovery from post-stroke impairments.
Enhanced motor function can translate into improved activities of daily living and overall quality of life for stroke survivors.
VR-based rehabilitation emerges as a promising intervention for stroke recovery, with demonstrated efficacy in enhancing motor function and quality of life.
Brain damage resulting from acute events like strokes often leads to disability and death1,2. Stroke is the primary cause of impairment and the second most common cause of death worldwide3,4. Even though physical therapy with aerobic exercise is believed to be the best approach to motor rehabilitation after a stroke, 15–30% of those who suffer from stroke are permanently disabled. Globally, it was the third leading cause of death and disability in 2019. Approximately 12.2 million new strokes are observed every year, with 25% of people aged over 25 years having a chance of stroke in their lifetime4. More than 50% of survivors have a disability in the form of reduced mobility following a stroke5. Numerous deficiencies have been noted, such as exhaustion, lassitude, fluctuations in mood, loss of sensory perception, deconditioning of the heart, nervousness, clumsiness, disorganized motions, inadequate equilibrium, and difficulties with walking6. In the case of a stroke, these deficits may impact the patient’s ability to perform functional tasks7,8.
Despite advancements in stroke care within clinical settings, which have greatly reduced the number of stroke-related mortality cases, stroke is the world’s leading cause of death and disability5,9,10. Concurrently, there is a discernible increase in the proportion of individuals with neurological abnormalities who experience substantial disability11. Although aerobic activities along with physical training are the gold standard for post-stroke motor rehabilitation, 15–30% of stroke patients experience lifelong impairment and only a few patients reported an improvement of their upper limbs (UL) function12,13. This significantly affects individuals’ ability to perform daily tasks independently and engage socially14.
It has been predicted that several motor rehabilitation programs utilizing motor learning frameworks will assist stroke victims in regaining the functional use of a damaged limb3,15,16. This is achieved by neural plasticity, which modifies the morphology and function of the nervous system17. International stroke rehabilitation research has recently focused on interventions for post-stroke motor and cognitive impairment, depression, and decreased functional independence. Novel therapies, such as virtual reality (VR), repetitive transcranial magnetic stimulation (RTMS), and robotic assistive therapies, have been demonstrated as potential future therapies18–20. Consequently, it has been demonstrated that enhanced neuronal plasticity has an important role in the rehabilitation of damaged limbs21,22. Recent research has led to the development of several stroke rehabilitation regimens aimed at improving post-stroke limb function, with evidence from the clinical trials of neuroplasticity-induced brain remodeling16,23–26.
The effectiveness of motor function improvement is examined and confirmed by several meta-analyses27,28. It is challenging to determine which program is better or which ones should be used consistently during rehabilitation, though, because of the intricacy of stroke recovery and the variations in the methods of research23–26.
It has been suggested that general exercises and a task-based approach with appropriate intensity be incorporated into stroke rehabilitation programs29,30. In stroke patients, passive stimulation techniques that use stimuli such as proprioception for movement of the body and visual input are employed to restore lost motor as well as sensory function30. These comprise a variety of electrical stimulation methods, including thermal stimulation (TS)31,32, periodic pneumatic compression28,33, neuromuscular stimulation, cutaneous electrical stimulation, transcutaneous electrical nerve stimulation (TENS), and peripheral stimulation with magnets28.
For stroke patients with severe disability, conventional therapies (CT) such as physical or occupational therapy are frequently used to improve their upper extremity motor function recovery34,35. Nevertheless, the results of this traditional strategy frequently rely on the skill and expertise of the medical staff, and it is frequently time-consuming with a low compliance rate. It has been shown, although, that the training incorporated into conventional therapy is still insufficient to result in a motor improvement of the damaged limb based on brain plasticity22.
The previously mentioned drawbacks prompted scientists to create and evaluate additional novel approaches, like virtual rehabilitation21,34, that would be more effective in helping stroke victims achieve functional recovery of their affected limbs.
Acknowledged as a cutting-edge approach, computer-simulated environment-based virtual rehabilitation enables users to engage in an array of situations and exercises within the designated virtual environment22, sometimes at higher levels of intensity than that found in traditional rehabilitation regimens for post-stroke patients36. This method has emerged as a viable option for stroke patients undergoing rehabilitation of motor function who have UL impairments34. Stroke survivors can engage in a goal-oriented program through virtual rehabilitation that supports and strengthens their functional limitations, activity restrictions, and limitations on their capacity to contribute to society37. Additionally, real-time visual feedback for motions is provided by virtual rehabilitation, which also boosts patient engagement in enjoyable rehabilitation programs38.
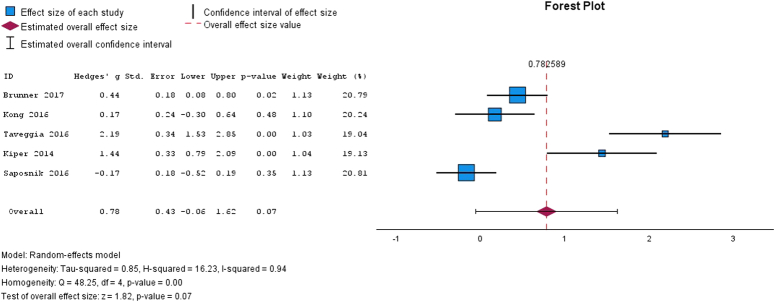
Although several VR interventions have been used with stroke survivors, the effectiveness of virtual rehabilitation interventions has not yet been significantly supported by high-quality research. VR-based therapy usually includes moving and acting within a virtual setting. Patients can use computer simulations to enhance their motor abilities by recognizing objects, following paths, and carrying out routine tasks in three-dimensional virtual environments (Fig. 1)39. VR technology in rehabilitation offers several benefits over previous rehabilitation techniques. Initially, it enables users to experience risky or unfeasible circumstances in real-world settings safely and efficiently. Second, patients do not have to worry about pressure, as they can work out at their own speed and skill level in a virtual setting. Third, virtual reality technology can assist patients in gaining self-assurance in handling challenging real-world circumstances. Significant alterations in healthcare provision, including rehabilitation services, have been observed due to the COVID-19 pandemic40.
Figure 1.
The different uses of virtual reality in the rehabilitation of stroke patients. VR, virtual rehabilitation.
The term “home-based VR” describes the use of virtual reality technology in patients’ rehabilitation in settings they are accustomed to, such as their own homes. Because treatment and exercise can be done remotely, patients no longer need to go often to hospitals or rehabilitation facilities. With the help of doctors and therapists, patients can receive their rehabilitation remotely, in the privacy and security of their own homes41–43. Promising results of VR therapy has been noted as the improvement of motor function, balance, and the ability to perform necessary daily tasks for patients with musculoskeletal and neurological disorders. For multiple sclerosis, severe brain damage, and stroke, it is a helpful therapeutic substitute44–46.
Methodology
Study searching and selection
The “Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)” criteria were followed in the conduct and reporting of this study. Medline/PubMed, and the Cochrane Library were the databases used in the literature search. The following search phrases were used: “physical therapy modalities,” “exposure therapy” “virtual rehabilitation,” and “stroke.” Medical Subject Heading (MeSH) descriptors were employed in the search strategy formation.
Types of records were determined by study design framework, contrasts, outcomes, interventions, and participants. Any patient with a persistent stroke that impacted their upper limbs was eligible to participate. The key result of interest was the treatment’s efficacy, with VR-based therapy serving as the intervention and traditional therapy serving as a comparison. The baseline values were compared to the most recent follow-up point, and a positive change was considered an indicator of effectiveness. In cases when many outcomes are recorded, the most pertinent result to other studies or the primary outcome is used when assessing a study’s efficacy in maintaining homogeneity.
Inclusion criteria
The subsequent inclusion standards were determined: (i) publications released between 2012 and 2022 to gather up-to-date and relevant research; (ii) The use of the English language; (iii) Randomized controlled trials (RCTs); (iv) adult stroke patients (age >18 years); (v) a VR game-based intervention that simulates virtual environments through the use of personal computers, electronic devices for video games and smartphone apps (vi) outcomes of motor function and quality of life assessed.
Exclusion criteria
A thorough verification procedure was used to ensure the papers in this systematic review fulfilled the eligibility requirements. Exclusions from this study included records or non-full texts about animal populations, non-randomized trials, and other research designs, including cohort, cross-sectional, case-control, and case studies. Those studies that did not disclose the data individually and merged participants with stroke in addition to those with other diseases were eliminated.
Each article that was part of this analysis had information available about the kind of treatment, the number of participants, the frequency of visits, the length of each session, the overall duration of therapy, the measuring instrument, and the outcome measures.
Evaluation of the bias risk
The methodological quality of the RCTs included in the meta-analysis was evaluated using the PEDro scale47. Eleven items in all address the topics of performance, attribution bases, information, detection, and selection48.
We utilized Cochrane’s updated quality assessment instrument (ROB-II) for randomized controlled trials49. Their internal validity must be critically assessed, which is made simpler by using ROB-II. This method aids in the transparent and uniform evaluation of bias, which enables researchers to make more informed decisions about which papers to include and which to omit from systematic reviews and meta-analyses49.
Statistical analyses
A meta-analysis was performed to assess the degree of effect changes between the control and intervention groups (IG) before and following treatments. The effectiveness of VR-based techniques was examined in the meta-analysis using the SPSS version 23 software. We performed subgroup analyses to minimize heterogeneity. To lessen the effects of study heterogeneity, a random-effects model was used to assess the pooled treatment effect of the various trials that were integrated50. Hedges’g, and the effect size (ES), Egger regression was used to measure publication bias, and Q statistics and I2 tests were used to evaluate heterogeneity. The trim-and-fill technique was utilized to incorporate absent studies, and meta-regression was employed to investigate the impact of time elapsed since the previous stroke on the efficacy of virtual reality.
Results
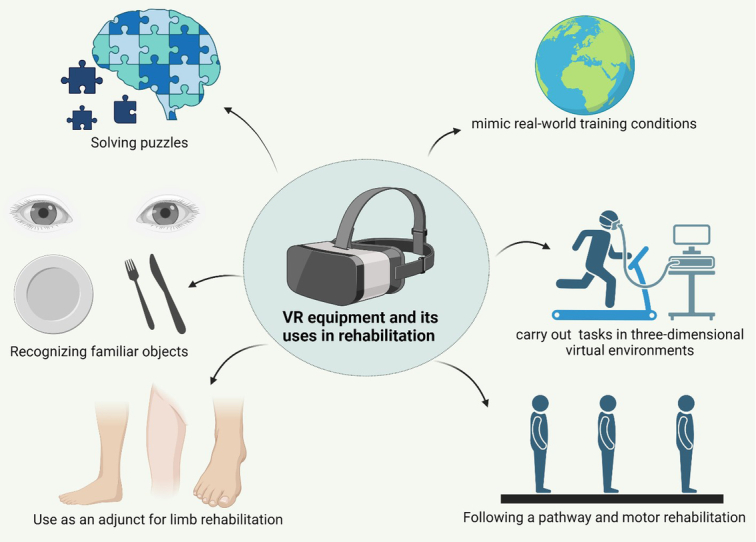
Overall, 165 articles were captured with the previously mentioned combination of keywords in the database searches, as shown in Figure 2. One hundred three articles underwent screening for eligibility check; after that, duplicates were removed. There were 20 articles in the review overall after the selection procedure; 15 of those were used in the meta-analysis of the statistical analysis. Figure 2 shows the whole selection process for each of the relevant operations. Table 1 displays the final score as well as the distinct features of each study (Appendix). Most of the studies that were selected for analysis showed excellent methodological quality (Table 2).
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Table 1.
Presents the primary attributes of the research interventions
| Study | Group interventions | VR groups | No. participant | The average age of participants in years/SD | Frequency | Session duration (min/h) | Intervention duration (week) | Outcome measure | Measuring instrument | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Saposnik et al. 51 | Control group: Recreational activities intervention group: Conventional treatment + virtual rehabilitation along with Nintendo Wii | Commercial games based on Nintendo Wii | Total participants=121 Control group:62 Instrumental group:59 | 62 (12.0) 62 (13.0) | 5 | 60 min | 2 | 1. Motor function 2. Quality of life 3. Kinematics parameters |
1. WMFT, Box, and Block Test, SIS, dynamometer. 2. SIS, MBI, FIM, and Modified Rankin Scale 3. Kinematic analysis with RPSS |
Following the intervention, no statistically significant change was seen between the groups. |
| Kong et al. 52 | Control group: Conventional treatment IG: virtual rehabilitation with Nintendo Wii |
Commercial games created on Nintendo Wii | Participants=68 Control group:35 Intervention group:33 |
55.8 (11.5) 58.1 (9.1) | 4 | 60 | 3 | 1. Motor function 2. Quality of life |
1. FMA-UE, ARAT. 2. FIM, SIS |
Following the intervention, no statistically significant change was seen between the groups. |
| Choi et al. 53 | Control group: Conventional treatment Intervention group: virtual rehabilitation-based Mobile games | Mobile games using a smartphone and a Tablet or computer | Participants=24 Control group:12 Intervention group:12 |
72.1 (9.9) 61.0 (15.2) | 5 | 30 | 2 | 1. Motor function 2. Quality of life 3. Depression |
1. FMA-UE, Brunnstro¨m, MMT 2. MBI, EQ-5D 3. BDI |
There was a noticeable statistical difference between the FMA-UE, Brunnstro¨m, and MMT groups. |
| Brunner et al. 54 | Control group: Conventional treatment Intervention group; Conventional treatment + virtual rehabilitation system + bionic gloves (YouGrabber |
Games based on interacting with virtual environments and objects | N=102 CG:52 IG:50 | 62.0 (—) 62.0 (—) | 4 | 60 | 4 | 1. Motor function 2. Quality of life |
1. ARAT, Box, and Block Test 2. FIM |
Following the intervention, no statistically significant change was seen between the groups. |
| Shin et al. 55 | CG: Conventional treatment Intervention group; virtual rehabilitation with biofeedback bionic gloves (SmartGlove) |
Games based on interacting with virtual environments and objects | N=33 CG:14 IG:19 | 59.8 (13.0) 57.2 (10.3) | 3 | 30 | 4 | 1. Motor function 2. Quality of life |
1. FMA-UE, JTT, PPT (Purdue pegboard test) 2. SIS |
There was a discernible difference between the Fugl-Meyer Assessment for the Upper Extremities, SIS and JTT groups. |
| Taveggia et al. 56 | Control group: Conventional treatment Intervention group: Conventional treatment and virtual rehabilitation system with an exoskeleton (Armeo Spring) | Games based on performing virtual tasks in virtual environments | N=54 CG:27 IG:27 | 68.0 (13.0) 73.0 (10.0) | 5 | 30 | 6 | 1. Motricity 2.Spasticity 3. Pain 4. Quality of life |
1. MI 2. Ashworth 3. FIM 4. VAS |
Each measure showed a statistically significant difference between the two groups. |
| Rubio et al.,57 | Conventional treatment+ virtual rehabilitation system | Games based on interacting with virtual environments and objects | 10 | 59.50 (±11.43) years | 2 | 60 | 8 | 1. Motor function | 1. Action Research Arm Test (ARAT) 2. BBT 3. SF-36 |
There was a statistically significant variation in the UL motor function (BBT, ARAT, grip strength, and upper extremity muscle strength) in patients. |
| Mekbib et al.,58 | Conventional treatment Intervention group: virtual rehabilitation system | VR-based limb mirroring therapy | 21 | 57.13 (±4.45) | 4 | 60 | 2 | UE | Resting-state fMRI and FMA for UL | Exercises involving bilateral and unilateral limb mirroring in a fully immersive virtual setting have the potential to improve motor performance and cortical reorganization. |
| Sheehy et al.,59 | Conventional treatment occupational therapy rehabilitative exercise | Games based on interacting with virtual environments, arm and trunk movement | 69 | 64.7 (±16.2) | 5 | 30–45 min | 2 | UE | Jintronix software and a Kinect 2 three-dimensional motion-tracking camera | As sitting balance results were comparable for both groups, this study does not support the use of VRT-provided sitting balance exercises for the rehabilitation of sitting balance following a stroke. Though this is only the second study to look into virtual reality therapy (VRT) for sitting balance and post-stroke upper extremity function for sitting balance, more research employing more difficult exercises and more intense treatment is needed before definitive findings can be drawn. |
| Subramanian et al. 60 | CG: Similar real therapy Intervention group:: 3D immersive VR (CAREN) | Games based on interacting with virtual environments and object | N= 25 CG:13 IG:12 | 60.0 (11.0) 62.0 (9.7) | 3 | — | 4 | 1. Motor function 2. Arm use. 3. Kinematcs parameters |
1. Fugl-Meyer Assessment for the Upper Extremities, WMFT, RPSS (Reaching Performance Scale for Stroke) 2. MAL–AS 3. Kinematic 3D analysis |
No statistically significant difference was found between groups in kinematics, arm motor impairment, activity level, and arm us. |
| Cho & Jung,61 | Control group: Conventional treatment Intervention group: immersive VR (IREX) |
Games based on interacting with virtual environments and objects | N= 29 CG:14 IG:15 | 63.7 (8.8) 64.0 (7.1) | 5 | 60 | 4 | 1. Motor function 2. Visual perception and processing time |
1. WMFT 2. MVPT (Motor-free Visual Perception Test) |
No statistically significant difference was found between groups on WMFT. A statistically significant difference was found in MVPT between groups. |
| Kwon et al. 62 | Control group: Conventional therapy IG: Conventional therapy + Immersive VR (IREX) | Games based on interacting with virtual environments and objects | N= 26 CG:13 IG:13 | 57.9 (12.3) 57.1 (15.4) | 5 | 30 | 4 | 1. Motor function 2. Quality of life |
1. Fugl-Meyer Assessment for the Upper Extremities, MFT (Manual Function Test) 2. MBI |
Following the intervention, no statistically significant change was seen between the groups. |
| Sin et al. 63 | Control group: Conventional treatment Intervention group: Conventional therapy + semi-immersive VR with Xbox Kinect |
Commercial games based on Xbox Kinect | N= 35 CG:17 IG:18 | 75.5 (5.5) 71.7 (9.4) | 3 | 30 | 6 | 1. Motor function 2. Manual dexterity |
1. Active ROM, Fugl-Meyer Assessment for the Upper Extremities, 2. Box, and Block Test |
A statistically significant difference was found between active ROM, FMA-UE and BBT groups. |
| Rand et al. 64 | Control group: Conventional treatment Intervention group: Semi-immersive and non-immersive VR with Xbox Kinect, PlayStation 2&3 |
Commercial games based on Xbox Kinect, Sony Play Station 2 EyeToy, Sony Play Station 3 Move, and SeeMe VR system | N= 29 CG:14 IG:15 | 62.5 (—) 57.0 (—) | 2 | 60 | 12 | 1. Motor function | 1. Number of movements, acceleration, and movement intensity | A statistically significant difference was found between groups in the number of intentional movements |
| Thielbar et al. 65 | Control group: Intensive treatment IG: Intensive therapy with mechatronic VR (AVK) |
Games based on interacting with a virtual Keypad | N= 14 CG:7 IG:7 | 59.0 (7.0) 54.0 (7.0) | 3 | — | 6 | 1. Motor function | 1. JTT, ARAT, Fugl-Meyer Assessment for the Upper Extremities, finger function | A statistically significant difference was found between the FMA-UE, JTT, and finger function groups. |
| Zheng et al. 66 | CG: RTMS treatment + immersive VR IG: L-F RTMS treatment + immersive VR | Games based on interacting with virtual environments and objects | N= 108 CG:53 IG:55 | 66.2 (13.1) 65.4 (13.5) | 6 | — | 4 | 1. Motor function 2. Quality of life |
1. Fugl-Meyer Assessment for the Upper Extremities, WMFT 2. Modified Barthel Index 3. SF-36 |
A statistically significant difference was found between the FMA-UE, WMFT, and MBI groups. |
| Kiper et al. 67 | CG: Conventional treatment Intervention group: Conventional treatment + VR feedback gloves |
Games based on interacting with virtual environments and object | N= 44 CG:21 IG:23 | 65.5 (14.2) 63.1 (9.5) | 5 | 60 | 4 | 1. Motor function 2. Quality of life 3. Kinematic parameters |
1. Fugl-Meyer Assessment for the Upper Extremities 2. FIM 3. Kinematic 3D analysis |
There was a discernible variation between the groups in terms of FMA-UE, FIM, and kinematics characteristics. |
| Feng et al. 68 | Conventional treatment and physiotherapy +virtual rehabilitation | Games based on interacting with virtual environments and objects | N= 28 | IG: 67.47 ± 4.79 CG: 66.93 ± 4.64 |
5 | 45 min | 12 | Motor function | 1. BBS 2.FGA 3.TUGT |
The study’s findings suggest that, in comparison to traditional physical treatment, 12 weeks of VR rehabilitation improved the balance and gait of patients receiving physical therapy.. |
| Shin et al. 69 | Control group: Conventional treatment Intervention group: Conventional treatment and virtual rehabilitation system | Games based on interacting with virtual environments and objects | N= 32 CG:16 IG:16 | 54.6 (13.4) 53.3 (11.8) | 5 | 60 | 4 | 1. Quality of life 2.Depression 3. Motor function |
1. HRQOL and SF-36 2. Hamilton 3. Fugl-Meyer Assessment for the Upper Extremities |
Following the intervention, no statistically significant change was seen between the groups. |
| Lee et al. 70 | Control group: Conventional treatment Intervention group: Conventional treatment and virtual rehabilitation system | Games based on interacting with virtual environments and objects | N= 18 CG:8 IG:10 | 73.1 (8.9) 69.2 (5.5 | 3 | 30 | 6 | 1. Motor function | 1. JTHFT, BBT, GPT (Grooved pegboard test), dynamometer | There was a statistically significant variation in the UL motor function (JTHFT, BBT, GPT, grip strength, and upper extremity muscle strength) between the groups. |
BBS, Berg Balance Scale; BBT, Box and Block Test; CG, control group; FGA, Functional Gait Assessment; FIM, Functional Independence Measure; FMA-UE, Fugl-Meyer Assessment for Upper Extremity; GPT, Grooved Pegboard Test; HRQOL, Health-Related Quality of Life; IG, intervention group; JTHFT, Jebsen-Taylor Hand Function Test; JTT: Jebsen-Taylor Hand Function Test; MBI, Modified Barthel Index; MMT, Manual Muscle Testing; RPSS, Reaching Performance Scale for Stroke; RTMS, repetitive transcranial magnetic stimulation; SIS, Stroke Impact Scale; TUGT, Timed Up and Go Test; UL, upper limb; VAS, Visual Analog Scale; VR, virtual reality; WMFT, Wolf Motor Function Test.
Table 2.
Risk of bias ROB 2.
| Reference T | Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall bias |
|---|---|---|---|---|---|---|
| Saposnik et al., (2016)51 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kong et al., (2016)52 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Choi et al., (2016)53 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Brunner et al., (2017)54 | Some concerns | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Shin et al., (2016)55 | Some concerns | Low risk | High risk | Low risk | Low risk | High risk |
| Taveggia et al., (2016)56 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Rubio et al., (2022)57 | Some concerns | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Mekbib et al., (2020)58 | Some concerns | Low risk | High risk | Low risk | Low risk | High risk |
| Sheehy et al., (2020)59 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Subramanian et al., (2013)60 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cho & Jung, (2012)61 | Some concerns | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Kwon et al., (2012)62 | Some concerns | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Sin et al., (2013)63 | Some concerns | Low risk | High risk | Low risk | Low risk | High risk |
| Rand et al., (2014)64 | Some concerns | Low risk | High risk | Low risk | Low risk | High risk |
| Thielbar et al., (2014)65 | Some concerns | Low risk | High risk | Low risk | Low risk | High risk |
| Zheng et al., (2014)66 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kiper et al., (2014)67 | Some concerns | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Feng et al., (2019)68 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Shin et al., (2015)69 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Lee et al., (2016)70 | Some concerns | Low risk | Low risk | Low risk | Some concerns | Some concerns |
Risk of bias
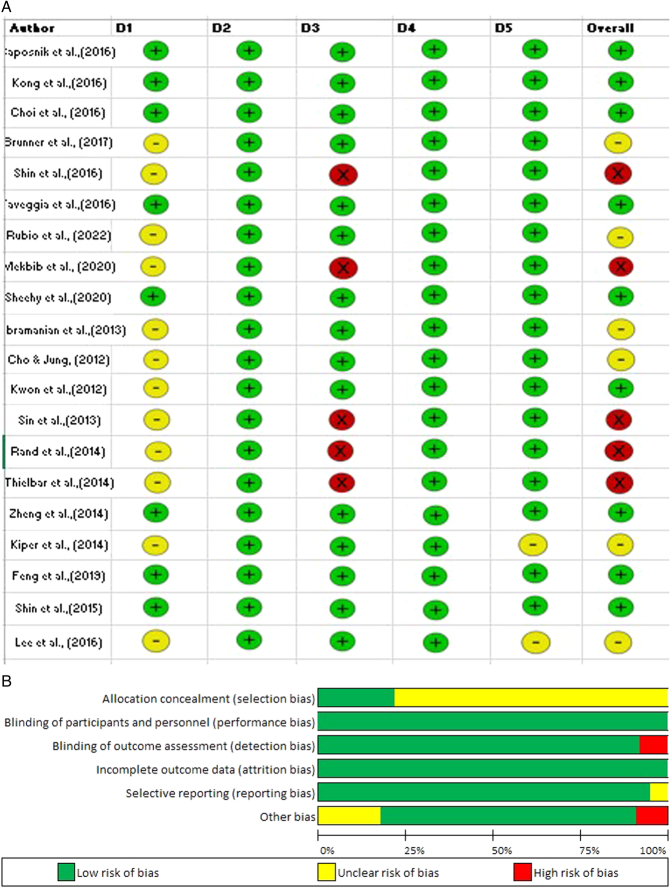
Table 2 and Figure 3 presents the RCTs that were included and their study quality. Three studies showed a high risk of bias, five had minor concerns, and nine had a low overall risk of bias. One of them had a low risk of bias while the other had a substantial risk of bias for non-randomized trials. The risk of bias in sequence generation, allocation concealment, outcome assessor blinding, selective outcome reporting, and other sources of bias was low in all of the studies (Saposnik et al.,51, Kong et al.,52, Choi et al.,53, Taveggia et al.,56, Subramanian et al.,60, Sheehy et al.,59, Rand et al.,64, Lee et al.,70, Shin et al. 69). The therapist and participant blinding in all trials (Brunner et al. 54, Rubio et al.,57; Kwon et al. 62; Sin et al. 63, Thielbar et al. 65, Feng et al. 68) was unclearly biased. There was a significant chance of bias in five studies (Zheng et al.,66, Shin et al.,55, Mekbib et al.,58, Cho & Jung,61, Kiper et al.,67) based on inadequate outcome data.
Figure 3.
(A) Selected studies are used to assess the risk of bias, (B) the graph and summary’s bias risk.
Viability of virtual rehabilitation treatment
Sixteen articles evaluating the viability of virtual reality treatment (pre-intervention versus post-mediation) were retrieved for the analysis. There was a notable improvement in subacute stroke patients receiving VR treatment as compared to their pre-intervention score. The analysis revealed that the post-stroke period (days) had no discernible impact on the therapeutic outcomes.
Key characteristics of various groups assembled for the meta-analysis are displayed in Table 3. These groups were formed considering the physical results examined in the investigations. As a result, two categories were created: quality of life and UL motor function. Furthermore, various subgroups were formed based on the instrument employed to quantify the outcomes. The quality of life group and the UL motor function group were subdivided into two subgroups.
Table 3.
Included research groups/subgroups in the meta-analysis.
| G | Studies | Outcome | Measuring strategy |
|---|---|---|---|
| 1 | Saposnik et al.,51, Rubio et al.,57, Mekbib et al.,58 Sheehy et al.,59 Kwon et al.,62 Sin et al.,63 Thielbar et al.,65 Kiper et al.,67 Lee et al.,70 Shin et al.,55 Kong et al.,52 Brunner et al.,54 | Motor functioning | Fugl-Meyer Assessment for Upper Extremity (FMA-UE), Box and Block Test (BBT) |
| 2 | Kwon et al.,62, Zheng et al.,66 Feng et al.,68 Saposnik et al.,51 Kiper et al.,67 Kong et al.,52 Taveggia et al.,56 Brunner et al.,54 | Standard of life | Barthel Scale, Functional Independence Measure (FIM) |
Graphical representation of the main outcome
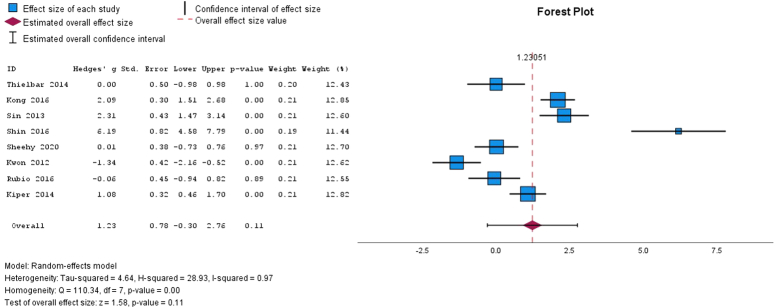
In the above figure, data are taken based on the frequency and intensity of exercise to determine how quickly the injured upper extremity recovers. Study evidence indicates that paretic extremities training has to be task-specific, repeated, and motivating. To help individuals in rehabilitation, motor training should also be customized for each person. Thus, physical exercises which improve sitting balance, and carry out daily tasks like holding utensils, turning knobs or locks, using a phone or computer, and writing are physical outcomes that are strongly related to the quality of life after a stroke (Fig. 4). The study’s findings show that effect sizes varied significantly amongst research, with an I-squared value of 0.97 indicating a high degree of heterogeneity. Large and significant physical outcomes of the groups on motor functioning were found by main outcome analyses utilizing a random-effects model (g=1.23; 95% CI=0.30–2.76; P=0.011; and I2=97%).
Figure 4.
Showing the analyzed physical outcomes of the groups.
Chance of predisposition
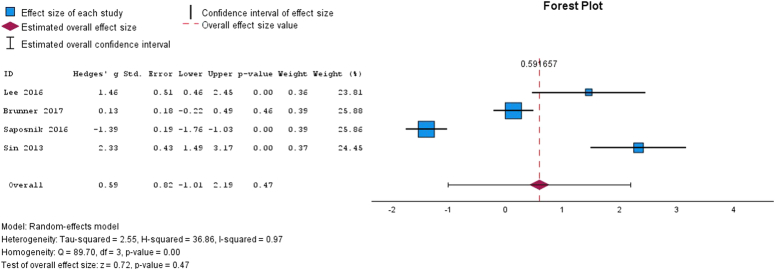
The results of VR interventions highlight that a mobile game-based VR rehabilitation program is both feasible and effective in supporting the recovery of the upper limb following an ischemic stroke. Moreover, stroke survivors who underwent additional virtual reality training using an Xbox Kinect demonstrated a significant improvement in upper extremity function (Fig. 5). The study shows strong heterogeneity in effect sizes across trials, as evidenced by a low homogeneity test P value and a high I2 value of 0.97. The main outcomes of the forest plot indicated that there’s a non-significant result was found for VR-based intervention in stroke patients of (g=0.59; 95% CI=1.01–2.19; P=0.047; I2=97%). The variability-causing elements do not add up to a statistically significant overall effect, as indicated by the non-statistically significant overall effect size (P=0.47). Understanding the results better may require more investigation of the origins of heterogeneity.
Figure 5.
Showing the virtual reality interventions in stroke patients.
Quality of life
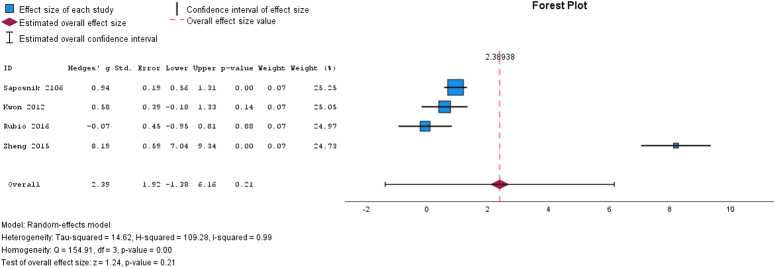
The study’s high I2 value of 0.99 indicates significant variation in impact sizes across studies (Fig. 6). There is substantial heterogeneity, as indicated by the low P value obtained from the homogeneity test. The results do not, however, appear to support a statistically significant overall effect, as indicated by the overall effect size test’s lack of statistical significance. To understand the cause of heterogeneity, more research needs to be conducted.
Figure 6.
Assessment of quality of life by using MBI and FIM.
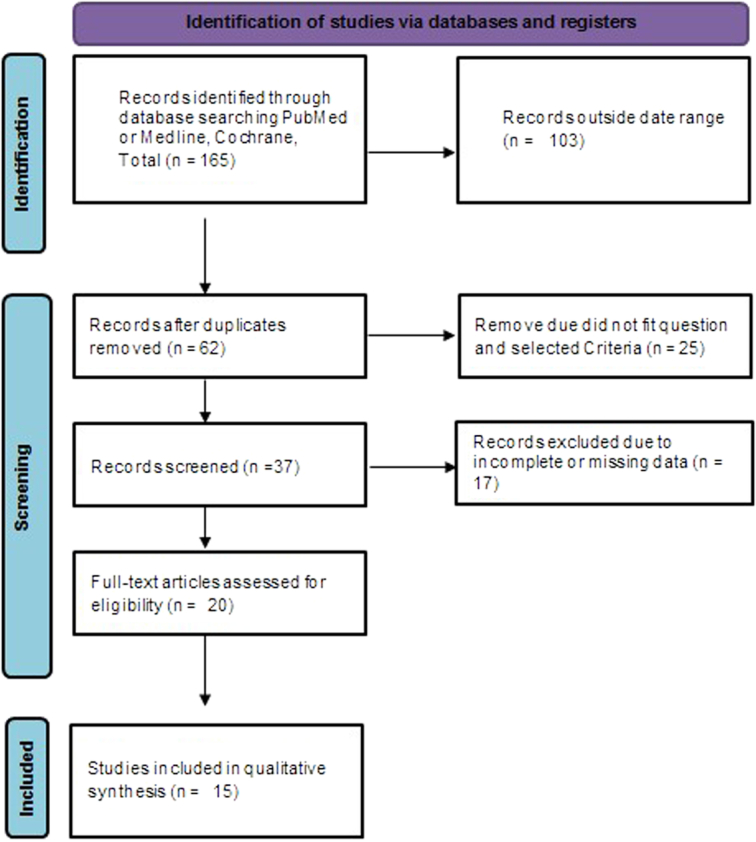
Treatment impacts of the post-stroke
The study’s high I2 value of 0.94 indicates substantial variation in impact sizes across studies (Fig. 7). Significant heterogeneity is present, as indicated by the low P value obtained from the homogeneity test. Nevertheless, the overall effect size test yields no statistically significant results, indicating that the data do not indicate a significant overall effect. To comprehend the underlying causes of heterogeneity, additional research is required.
Figure 7.
Treatment impacts of the post-stroke term between experiment and control groups.
Discussion
The primary goal of this meta-analysis and systematic review of RCTs was to examine the impact of different VR modalities on post-stroke physical capacities and living standards. Virtual rehabilitation systems are a promising technique for physical intervention because they have several advantages over traditional therapies. These benefits include the potential to utilize games to directly offer feedback to patients and increase participant motivation; moreover, they are affordable, easy to use, and compatible with a variety of systems71.
Moreover, virtual reality therapy administered at home may help stroke patients recover72. Regarding the particular technology employed in the several experiments that produced positive outcomes, all these technologies have certain things in common, like allowing individuals to use games to engage with virtual surroundings; based on the degree of immersion applied, subjects behave in manners that are similar to reality. In this approach, the user’s attention is enhanced as the involvement increases and subjects have less interaction with the outer surroundings. Considering that attention disorders are the most common cognitive condition following a stroke, it is crucial to recognize their detrimental effects73.
As a result, the application of immersive virtual reality systems, facilitating complete focus on the tasks, may offer significant benefits for deficit rehabilitation. The statistical analysis conducted for this evaluation showed that virtual rehabilitation intervention had a beneficial impact on motor function, particularly in the entire FMA-UE. Findings are under the evaluation of Laver et al. 74; researchers suggested that virtual reality therapies are comparable to traditional therapy to enhance activities of daily living (ADL) and UL motor performance following a stroke. It would be interesting to examine the precise elements of therapy that enable the achievement of these beneficial outcomes. Thus, intensive therapy, stimulating therapy using exercise games, motor learning stimulation, along beneficial interaction between the reaction and the stimuli are four components of VR therapy that may cooperate to guarantee success75.
The results regarding quality of life illustrate the possible advantages of virtual rehabilitation interventions after a stroke. As per The International System of Classification of Health, Disability and Functioning (ICF)76, limitations on participation may arise from activity restrictions that are impacted by impairment in terms of both physical structural and functional levels. However, these three areas are not usually directly related to one another77. There is a suggestion that the development in UL function that this analysis has uncovered may enhance ADL participation, which in turn may enhance quality of life. Considering that there is a recognized association between the two instruments, it is also possible that the improvements observed in the FIM scale, and the FMA-UE scales are related. Researchers were encouraged to indicate which ICF scale domains they expected to improve with the intervention, in keeping with the research direction suggested by Lohse et al. 78.
Finally, Pietrzak et al. 79 stated that to simplify the use of the services for virtual interventions and treatment facilities, emphasis should be placed on the necessity of integrating VR-based video games into stroke rehabilitation. Additionally, by modifying the length, intensity, and difficulty level of the VR games, as well as by offering various forms of feedback and encouraging reinforcement, therapists may develop customized games based on the medical characteristics of the patients72.
Limitations
While the outcomes presented in this review are valuable, it should be noted that it has certain limitations. One limitation concerned the large range of VR treatments, each of which is categorized under one word or term. Moreover, a separate analysis of acute and chronic strokes was not conducted. Some studies53,60,69 did not offer data gathered before or after the intervention, so they were excluded from the meta-analysis. An additional limitation was the use of various measurement tools. Due to this, it was not possible to compare the research statistically.
Also, while the PRISMA guidelines were followed, restricting the search to a limited number of databases and only articles published in English, which might miss relevant studies, especially those in other languages or other studies that contain negative findings. This could tilt the results towards positive outcomes. Furthermore, the limited focus on measuring improvement outcomes of motor function and quality of life overlooks other aspects that could be assessed such as cost-effectiveness and long-term sustainability. The patient’s experience is also a factor that should be assessed. The limitations affect the ability to form a holistic evaluation of VR therapy’s potential.
Conclusion
The outcomes suggest that virtual rehabilitation could be useful for enhancing the quality of life following a stroke and motor functioning. By using video games developed for virtual reality platforms, this study can be useful in clinical treatment. It can also serve as a foundation for the development of further research on the topic and offer valuable feedback for future interventions for improvements in methodology. Data with larger sample sizes and more consistency regarding the kind of instrument used, length of treatment sessions, and the effect of the intervention strategy will be needed for clinical research. Determining which specific therapeutic components are more crucial to a successful outcome will also be crucial.
Ethical approval
Ethical approval was not required for this review.
Consent
Informed consent was not required for this review.
Source of funding
No funding obtained.
Author contribution
P.P.: conceptualization, methodology, validation, writing—original draft preparation, writing—review and editing. K.K.C.: methodology, validation, writing—original draft preparation, writing—review and editing. P.B.: conceptualization, writing—original draft preparation, writing—review and editing. E.G.: validation, writing—original draft preparation, writing—review and editing. M.O.A.: methodology, writing—original draft preparation, writing—review and editing. P.I.: writing—original draft preparation, writing—review and editing, data curation. A.S.A.: writing—original draft preparation, writing—review and editing. A.D.: writing—original draft preparation, writing—review and editing. Y.T.: writing—original draft preparation, writing—review and editing. M.D.M.M.: writing—original draft preparation, writing—review and editing. M.M.R.: writing—original draft preparation, writing—review and editing. S.M.: writing—original draft preparation, writing—review and editing. H.B.: writing—original draft preparation, writing—review and editing. G.S.: writing—original draft preparation, writing—review and editing. H.J.: writing—original draft preparation, writing—review and editing. S.G.: writing—original draft preparation, writing—review and editing, validation, supervision. O.A.H.: writing—original draft preparation, writing—review and editing.
Conflicts of interest disclosure
All authors do not have any conflict of interest.
Research registration unique identifying number (UIN)
1. Name of the registry: PROSPERO.
2.Unique identifying number or registration ID: CRD42024542963.
3.Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=542963.
Guarantor
Srikanth Gadam.
Data availability statement
The data that support the findings of this study are available in the supplementary material of this article.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Priyadarshi Prajjwal, Email: priyadarshiprajwal@gmail.com.
Kiran Kishor Chandrasekar, Email: kirankishor96@gmail.com.
Pavani Battula, Email: pavani.b3@gmail.com.
Elizabeth Gaviria, Email: gaviria.elizabeth00@gmail.com.
Mishael Oluwadamilola Awe, Email: awemishael01@gmail.com.
Pugazhendi Inban, Email: inban.pugaz@gmail.com.
Adel S. Almutairi, Email: AdelAlmutairi247@gmail.com.
Arpan Das, Email: dr.arpand@gmail.com.
Yogesh Tekuru, Email: tekuruyogesh@gmail.com.
Mohammed Dheyaa Marsool Marsool, Email: mohamadalansa438@gmail.com.
Murali Mohan Reddy, Email: murali.mohan2@learner.Manipal.edu.
Spandana Mitra, Email: spandana.mitra@icloud.com.
Hyma Bamba, Email: Hymabambagmch@gmail.com.
Gurmehar Singh, Email: Gurmehar281@gmail.com.
Hritvik Jain, Email: hritvikjain2001@gmail.com.
Srikanth Gadam, Email: drsrikanthgadam@gmail.com.
Omniat Amir Hussin, Email: omniatamir123@gmail.com.
References
- 1.Sabut SK, Sikdar C, Mondal R, et al. Restoration of gait and motor recovery by functional electrical stimulation therapy in persons with stroke. Disabil Rehabil 2010;32:1594–1603. [DOI] [PubMed] [Google Scholar]
- 2.Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:2064–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011;377:1693–1702. [DOI] [PubMed] [Google Scholar]
- 4.Feigin VL, Brainin M, Norrving B, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022 [published correction appears in Int J Stroke. 2022 Apr;17(4):478]. Int J Stroke 2022;17:18–29. [DOI] [PubMed] [Google Scholar]
- 5.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association [published correction appears in Circulation. 2023 Feb 21;147(8):e622] [published correction appears in Circulation. 2023 Jul 25;148(4):e4]. Circulation 2023;147:e93–e621. [DOI] [PubMed] [Google Scholar]
- 6.Al Khathaami AM, Algahtani H, Alwabel A, et al. The status of acute stroke care in Saudi Arabia: an urgent call for action!. Int J Stroke 2011;6:75–76. [DOI] [PubMed] [Google Scholar]
- 7.Guy S, Clarke L, Bryant H, et al. An interdisciplinary team approach to acute stroke rehabilitation. Neurol Rehabil Stroke 2004:26–56. [Google Scholar]
- 8.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol 2009;8:741–754. [DOI] [PubMed] [Google Scholar]
- 9.Johnson CO, Nguyen M, Roth GA, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18:439–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simpkins AN, Janowski M, Oz HS, et al. Biomarker application for precision medicine in stroke. Transl Stroke Res 2020;11:615–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baumann M, Lurbe-Puerto K. Increased residual disability among post-stroke survivors, and differences in the repercussions between informal caregivers. Top Stroke Rehabil 2011;18:162–171. [DOI] [PubMed] [Google Scholar]
- 12.Choo PL, Gallagher HL, Morris J, et al. Correlations between arm motor behavior and brain function following bilateral arm training after stroke: a systematic review. Brain Behav 2015;5:e00411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Writing Group Members. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012;125:e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bailey RR, Klaesner JW, Lang CE. Quantifying real-world upper-limb activity in nondisabled adults and adults with chronic stroke. Neurorehabil Neural Repair 2015;29:969–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arya KN, Pandian S, Verma R, et al. Movement therapy induced neural reorganisation and motor recovery in stroke: a review. J Bodywork Movement Ther 2011;15:528–537. [DOI] [PubMed] [Google Scholar]
- 16.Brewer L, Horgan F, Hickey A, et al. Stroke rehabilitation: recent advances and future therapies. QJM 2013;106:11–25. [DOI] [PubMed] [Google Scholar]
- 17.Hosp JA, Luft AR. Cortical plasticity during motor learning and recovery after ischemic stroke. Neural Plast 2011;2011:871296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johansson BB. Current trends in stroke rehabilitation. A review with focus on brain plasticity. Acta Neurol Scand 2011;123:147–159. [DOI] [PubMed] [Google Scholar]
- 19.Kleim JA, & Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. 2008.. [DOI] [PubMed]
- 20.Talelli P, Greenwood RJ, Rothwell JC. Arm function after stroke: neurophysiological correlates and recovery mechanisms assessed by transcranial magnetic stimulation. Clin Neurophysiol 2006;117:1641–1659. [DOI] [PubMed] [Google Scholar]
- 21.da Silva Cameirão M, Bermúdez I, Badia S, et al. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: a randomised controlled pilot study in the acute phase of stroke using the rehabilitation gaming system. Restor Neurol Neurosci 2011;29:287–298. [DOI] [PubMed] [Google Scholar]
- 22.Saposnik G, Levin M, Stroke Outcome Research Canada (SORCan) Working Group . Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke 2011;42:1380–1386. [DOI] [PubMed] [Google Scholar]
- 23.Chen JC, Shaw FZ. Progress in sensorimotor rehabilitative physical therapy programs for stroke patients. World J Clin Cases: WJCC 2014;2:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dobkin BH, Dorsch A. New evidence for therapies in stroke rehabilitation. Curr Atheroscler Rep 2013;15:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pollock A, Baer G, Langhorne P, et al. Physiotherapy treatment approaches for the recovery of postural control and lower limb function following stroke: a systematic review. Clin Rehabil 2007;21:395–410. [DOI] [PubMed] [Google Scholar]
- 26.Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014;9:e87987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu WY, Cheng CH, Liao KK, et al. Effects of repetitive transcranial magnetic stimulation on motor functions in patients with stroke: a meta-analysis. Stroke 2012;43:1849–1857. [DOI] [PubMed] [Google Scholar]
- 28.Laver K. Virtual reality for stroke rehabilitation. Virtual Reality in Health and Rehabilitation. CRC Press; 2020:19–28. [Google Scholar]
- 29.French B, Thomas LH, Leathley MJ, et al. Repetitive task training for improving functional ability after stroke. Stroke 2009;40:e98–e99. [DOI] [PubMed] [Google Scholar]
- 30.Kita K, Otaka Y, Takeda K, et al. A pilot study of sensory feedback by transcutaneous electrical nerve stimulation to improve manipulation deficit caused by severe sensory loss after stroke. J Neuroeng Rehabil 2013;10:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen JC, Liang CC, Shaw FZ. Facilitation of sensory and motor recovery by thermal intervention for the hemiplegic upper limb in acute stroke patients: a single-blind randomised clinical trial. Stroke 2005;36:2665–2669. [DOI] [PubMed] [Google Scholar]
- 32.Wu HC, Lin YC, Hsu MJ, et al. Effect of thermal stimulation on upper extremity motor recovery 3 months after stroke. Stroke 2010;41:2378–2380. [DOI] [PubMed] [Google Scholar]
- 33.Cambier DC, De Corte E, Danneels LA, et al. Treating sensory impairments in the post-stroke upper limb with intermittent pneumatic compression. Results of a preliminary trial. Clin Rehabil 2003;17:14–20. [DOI] [PubMed] [Google Scholar]
- 34.Ackerley SJ, Byblow WD, Barber PA, et al. Primed physical therapy enhances recovery of upper limb function in chronic stroke patients. Neurorehabil Neural Repair 2016;30:339–348. [DOI] [PubMed] [Google Scholar]
- 35.Jarvis K, Reid G, Edelstyn N, et al. Development of the occupational therapy stroke arm and hand record: an upper limb treatment schedule. Br J Occup Ther 2014;77:126–133. [Google Scholar]
- 36.Chen L, Lo WLA, Mao YR, et al. Effect of virtual reality on postural and balance control in patients with stroke: a systematic literature review. Biomed Res Int 2016;2016:7309272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Merians AS, Jack D, Boian R, et al. Virtual reality–augmented rehabilitation for patients following stroke. Phys Ther 2002;82:898–915. [PubMed] [Google Scholar]
- 38.Levin MF, Weiss PL, Keshner EA. Emergence of virtual reality as a tool for upper limb rehabilitation: incorporation of motor control and motor learning principles. Phys Ther 2015;95:415–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levac DE, Huber ME, Sternad D. Learning and transfer of complex motor skills in virtual reality: a perspective review. J Neuroeng Rehabil 2019;16:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 2021;11:e045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Appel L, Appel E, Bogler O, et al. Older adults with cognitive and/or physical impairments can benefit from immersive virtual reality experiences: a feasibility study. Front Med (Lausanne) 2020;6:329; Published 2020 Jan 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smits M, Staal JB, van Goor H. Could Virtual Reality play a role in the rehabilitation after COVID-19 infection? BMJ Open Sport—Exercise Med 2020;6:e000943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wade DT. Rehabilitation after COVID-19: an evidence-based approach. Clin Med (Northfield Il) 2020;20:359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee HS, Park YJ, Park SW. The effects of virtual reality training on function in chronic stroke patients: a systematic review and meta-analysis. Biomed Res Int 2019;2019:7595639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maggio MG, Russo M, Cuzzola MF, et al. Virtual reality in multiple sclerosis rehabilitation: a review on cognitive and motor outcomes. J Clin Neurosci 2019;65:106–111. [DOI] [PubMed] [Google Scholar]
- 46.Zanier ER, Zoerle T, Di Lernia D, et al. Virtual reality for traumatic brain injury. Front Neurol 2018;9:345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bhogal SK, Teasell RW, Foley NC, et al. The PEDro scale provides a more comprehensive measure of methodological quality than the Jadad scale in stroke rehabilitation literature. J Clin Epidemiol 2005;58:668–673. [DOI] [PubMed] [Google Scholar]
- 48.Verhagen AP, De Vet HC, De Bie RA, et al. The Delphi list: a criteria list for quality assessment of randomised clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 1998;51:1235–1241. [DOI] [PubMed] [Google Scholar]
- 49.Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 50.Brydges CR. Effect Size Guidelines, Sample Size Calculations, and Statistical Power in Gerontology. Sands LP, editor. Innovation in Aging. 2019 Aug 1;3(4). [DOI] [PMC free article] [PubMed]
- 51.Saposnik G, Cohen LG, Mamdani M, et al. Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): a randomised, multicentre, single-blind, controlled trial. Lancet Neurol 2016;15:1019–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kong KH, Loh YJ, Thia E, et al. Efficacy of a virtual reality commercial gaming device in upper limb recovery after stroke: a randomised, controlled study. Top Stroke Rehabil 2016;23:333–340. [DOI] [PubMed] [Google Scholar]
- 53.Choi YH, Ku J, Lim H, et al. Mobile game-based virtual reality rehabilitation program for upper limb dysfunction after ischemic stroke. Restor Neurol Neurosci 2016;34:455–463. [DOI] [PubMed] [Google Scholar]
- 54.Brunner I, Skouen JS, Hofstad H, et al. Virtual reality training for upper extremity in subacute stroke (VIRTUES) a multicenter RCT. Neurology 2017;89:2413–2421. [DOI] [PubMed] [Google Scholar]
- 55.Shin JH, Kim MY, Lee JY, et al. Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: a single-blinded, randomised controlled trial. J Neuroeng Rehabil 2016;13:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Taveggia G, Borboni A, Salvi L, et al. Efficacy of t-assisted rehabilitation for the functional recovery of the upper limb in post-stroke patients: a randomised controlled study. Eur J Phys Rehabil Med 2016;52:767–773. [PubMed] [Google Scholar]
- 57.Aguilera-Rubio Á, Cuesta-Gómez A, Mallo-López A, et al. Feasibility and Efficacy of a virtual reality game-based upper extremity motor function rehabilitation therapy in patients with chronic stroke: a pilot study. Int J Environ Res Public Health 2022;19:3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mekbib DB, Zhao Z, Wang J, et al. Proactive motor functional recovery following immersive virtual reality–based limb mirroring therapy in patients with subacute stroke. Neurotherapeutics 2020;17:1919–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sheehy L, Taillon‐Hobson A, Sveistrup H, et al. Sitting balance exercise performed using virtual reality training on a stroke rehabilitation inpatient service: a randomized controlled study. Pm&r 2020;12:754–765. [DOI] [PubMed] [Google Scholar]
- 60.Subramanian SK, Lourenço CB, Chilingaryan G, et al. Arm motor recovery using a virtual reality intervention in chronic stroke: randomised control trial. Neurorehabil Neural Repair 2013;27:13–23. [DOI] [PubMed] [Google Scholar]
- 61.Cho K, Yu J, Jung J. Effects of virtual reality-based rehabilitation on upper extremity function and visual perception in stroke patients: a randomised control trial. J Phys Ther Sci 2012;24:1205–1208. [Google Scholar]
- 62.Kwon JS, Park MJ, Yoon IJ, et al. Effects of virtual reality on upper extremity function and activities of daily living performance in acute stroke: a double-blind randomised clinical trial. NeuroRehabilitation 2012;31:379–385. [DOI] [PubMed] [Google Scholar]
- 63.Sin H, Lee G. Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil 2013;92:871–880. [DOI] [PubMed] [Google Scholar]
- 64.Rand D, Givon N, Weingarden H, et al. Eliciting upper extremity purposeful movements using video games: a comparison with traditional therapy for stroke rehabilitation. Neurorehabil Neural Repair 2014;28:733–739. [DOI] [PubMed] [Google Scholar]
- 65.Thielbar KO, Lord TJ, Fischer HC, et al. Training finger individuation with a mechatronic-virtual reality system leads to improved fine motor control post-stroke. J Neuroeng Rehabil 2014;11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zheng CJ, Liao WJ, Xia WG. Effect of combined low-frequency repetitive transcranial magnetic stimulation and virtual reality training on upper limb function in subacute stroke: a double-blind randomised controlled trail. J Huazhong Univ Sci Technol [Med Sci] 2015;35:248–254. [DOI] [PubMed] [Google Scholar]
- 67.Kiper P, Agostini M, Luque-Moreno C, et al. Reinforced feedback in virtual environment for rehabilitation of upper extremity dysfunction after stroke: preliminary data from a randomised controlled trial. Biomed Res Int 2014;2014:752128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Feng H, Li C, Liu J, et al. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: a randomized controlled trial. Med Sci Monitor 2019;25:4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shin JH, Park SB, Jang SH. Effects of game-based virtual reality on health-related quality of life in chronic stroke patients: a randomised, controlled study. Comput Biol Med 2015;63:92–98. [DOI] [PubMed] [Google Scholar]
- 70.Lee S, Kim Y, Lee BH. Effect of virtual reality‐based bilateral upper extremity training on upper extremity function after stroke: a randomised controlled clinical trial. Occup Ther Int 2016;23:357–368. [DOI] [PubMed] [Google Scholar]
- 71.Ruiz‐González L, Lucena‐Antón D, Salazar A, et al. Physical therapy in Down syndrome: systematic review and meta‐analysis. J Intellect Disabil Res 2019;63:1041–1067. [DOI] [PubMed] [Google Scholar]
- 72.Lin J, Kelleher CL, Engsberg JR. Developing home-based virtual reality therapy interventions. Games Health 2013;2:34–38. [DOI] [PubMed] [Google Scholar]
- 73.Hochstenbach J, Mulder T, van Limbeek J, et al. Cognitive decline following stroke: a comprehensive study of cognitive decline following stroke. J Clin Exp Neuropsychol 1998;20:503–517. [DOI] [PubMed] [Google Scholar]
- 74.Laver KE, Lange B, George S, et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 2017;11:CD008349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Holden MK. Virtual environments for motor rehabilitation. Cyberpsychol Behav 2005;8:187–211. [DOI] [PubMed] [Google Scholar]
- 76.World Health Organization . Towards a common language for functioning, disability, and health: ICF. Int Classific Funct Disabil Health 2002. [Google Scholar]
- 77.Sullivan KJ, Cen SY. Model of disablement and recovery: knowledge translation in rehabilitation research and practice. Phys Ther 2011;91:1892–1904. [DOI] [PubMed] [Google Scholar]
- 78.Lohse KR, Hilderman CG, Cheung KL, et al. Virtual reality therapy for adults post-stroke: a systematic review and meta-analysis exploring virtual environments and commercial games in therapy. PLoS ONE 2014;9:e93318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pietrzak E, Pullman S, McGuire A. Using virtual reality and videogames for traumatic brain injury rehabilitation: a structured literature review. Games Health 2014;3:2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available in the supplementary material of this article.