Abstract
Background:
Bacillus cereus (B. cereus) is a Gram-positive, rod-shaped, motile organism, found in the environment and may exist in contaminated food sources such as reheated rice, vegetables and may lead to gastrointestinal symptoms after ingestion including diarrhea, nausea, and vomiting due to enterotoxigenic and emetic toxins. Non-gastrointestinal infections of Bacillus cereus have been reported in the literature, which include cutaneous and non-cutaneous infections in immunocompetent and immunocompromised individuals.
Case presentation:
A 38-year-old man presented with a one-week history of penile swelling and redness that started after an episode of severe diarrhea and vomiting, which soiled his genital region few hours after vigorous intercourse with his wife. This has led to infection of the penile skin by an unusual organism: Bacillus (B.) cereus. The patient was treated using fucidic acid ointment applications for 2 weeks achieving complete recovery.
Clinical discussion:
The recovery of B. cereus from the penile infection in our patient reveals the first case of such an unusual infection, though this pathogen has been reported to cause a wide range of non-GI tract infections, which include bacteremia, meningitis, endocarditis, endophthalmitis, pneumonia, and soft tissue diseases. Virulence factors allow this organism to induce diarrhea in addition to having dermonecrotic, cytotoxic, hemolytic properties resulting in a wide range of dermatologic presentations.
Conclusion:
The authors report a unique case of penile skin infection caused by B. cereus, an unusual culprit for an uncommon presentation successfully treated with fucidic acid ointment. This is the first case in literature describing such an entity.
Keywords: Bacillus cereus, bacteria, microbiology, penile infection, penis
Introduction
Highlights
Bacillus cereus is found in contaminated food and may lead to gastrointestinal symptoms including diarrhea, nausea, and vomiting.
Bacillus cereus causes a wide range of non-GI infections.
Treatment of Bacillus cereus includes vancomycin, gentamicin, chloramphenicol, ciprofloxacin, or carbapenems but can be treated with topical fucidic acid ointment in non-severe infections.
This is the first case in the literature of Bacillus cereus-induced penile infection.
Bacillus cereus (B. cereus) is a Gram-positive, rod-shaped, motile organism, exists in the environment, found in contaminated food including rice, beef, and vegetables and may lead to gastrointestinal symptoms including diarrhea, nausea, and vomiting. This is due to the production of enterotoxigenic and emetic toxins1,2. Non-gastrointestinal (GI) infection with B. cereus not only limited to cutaneous but includes a wide range of presentations3. Several etiologic agents have been reported to cause penile skin infection but not due to B. cereus 4,5.
Thus, in the absence of previous reports, we hereby present a case of an unusual penile infection caused by B. cereus.
Case presentation
The patient is a 38-year-old man, previously healthy, known heavy smoker (23 pack-years), circumcised since birth, married and sexually active in a monogamous relationship, with 2 children conceived naturally. He presented to the urology clinic with 1-week history of penile swelling and redness that started after an episode of severe diarrhea and vomiting 1 week prior to presentation. The patient reported having vigorous vaginal intercourse with his wife hours before the episode of diarrhea and vomiting and that his vomitus and stools had contaminated his genital area. The patient had eaten a meal with his family containing rice, one day prior to the onset of his GI symptoms, and his wife denied having any gastrointestinal symptoms.
On physical examination, the patient has normal penile length, with an area of redness and scaling noted over the glans penis and the sub-coronal area in addition to sloughed skin and purulent extravasation from the ventral aspect of the penile shaft lateral to the frenulum area as shown in Figure 1A. A swab culture was taken of these purulent excretions for diagnosis of his condition. The patient denied having any trauma to the penis or laceration, or any accidental bite during the intercourse time. The patient was advised not to have intercourse or perform masturbation and to apply fucidic acid ointment to the penis three times per day after washing properly and gently drying the area.
Figure 1.
(A1, A2) Infection of the ventral penile shaft and glans on presentation (yellow. arrow). (B) Follow-up image after 2 days of fucidic acid ointment application. (C) Follow-up after 1 week of fucidic acid application. (D1 and D2) Follow-up after 2 weeks of fucidic acid ointment application showing improvement notably on the glans penis (blue arrow).
The culture of the secretions on appropriate bacterial media after 24 h of incubation grew 3 organisms which were identified by Matrix-Assisted Laser Desorption/Ionization Time of Flight (MALDI-TOF) system, as Corynebacterium aurimocosum, Staphylococcus epidermitis (both of which constitute normal skin flora), and B. cereus. The antimicrobial susceptibility testing of B. cereus revealed susceptibility to chloramphenicol, ciprofloxacin, clindamycin, erythromycin, imipenem, teicoplanin and vancomycin, and resistance to amoxicillin/clavulanic acid and penicillin, as done based on the Clinical and Laboratory Standards Institute (CLSI, M45). The colony morphology and Gram stain features of the B. cerus are shown in Figures 2 and 3.
Figure 2.

B. cereus colonies growing on chocolate agar media.
Figure 3.
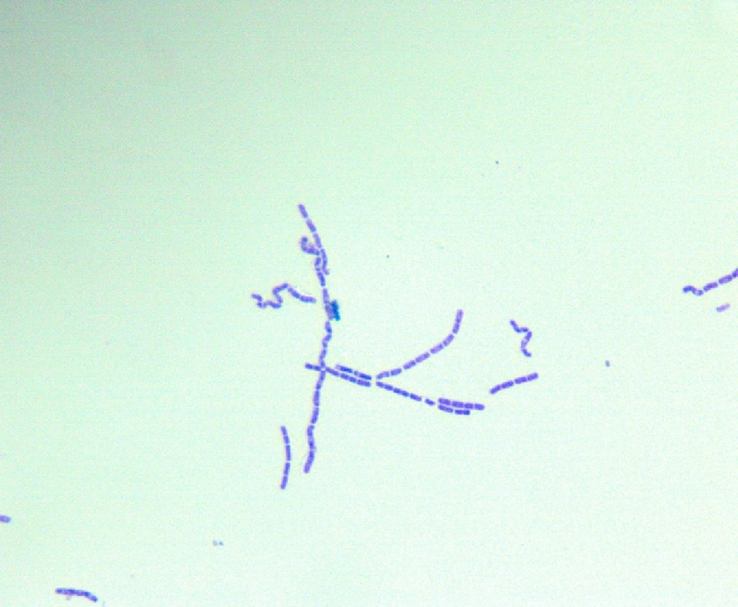
B. cereus on Gram staining showing Gram-positive spore forming rod-shaped bacteria under oil. immersion lens (100×).
The patient was not started on ciprofloxacin because of the significant improvement of symptoms after the application of fucidic acid ointment for 2 days as shown in Figure 1B. He was then instructed to continue the fucidic acid course and follow-up in 1 week shown in Figure 1C. The results of improvement after 2 weeks are shown in Figure 1 D1 and D2.
On follow-up after 1 month, the patient was satisfied with the recovery from his condition and no complications had occurred requiring subsequent follow-up in the clinic. He had no pain, burning, or discomfort in the genital area and no recurrence of the infection occurred.
Written consent was obtained from the patient prior to writing of this manuscript.
Discussion
Penile infections of the skin generally occur secondary to penetrating injuries, and mostly caused by penetrating injuries mostly due to group A streptococcus, Staphylococcus (S.) aureus, anaerobes, and sexually transmitted pathogens. Though the skin involvement can be self-limited, extension to cellulitis of the penis and scrotum can occur4,5.
The recovery of B. cereus from the penile infection in our patient revealed the first case of such an unusual infection, though this pathogen has been reported to cause a wide range of non-GI tract infections.
Non-gastrointestinal infections caused by B. cereus, although rare, reported in the literature, include serious conditions such as bacteremia, meningitis, endocarditis, endophthalmitis, pneumonia, and soft tissue diseases6. Skin infections, rarely reported in the literature, can present in patients without any underlying diseases, as shown in a case report of a patient with a cutaneous ulcer caused by B. cereus; this was the first study to report such an infection in an immunocompetent individual7. Furthermore, necrotic cutaneous infections have been observed in patients with type 2 diabetes mellitus8. Additionally, a rare case of B. cereus endocarditis was reported in a patient without typical risk factors, who experienced good clinical outcomes without the need for valve replacement9. Another case report showed that this bacterium caused septic arthritis in a pediatric patient who was fully immunized; this was the first recorded case of septic arthritis by this bacterium10.
The pathogenicity of this bacteria whether inside GI tract or externally depends on pore-forming enterotoxins produced by bacterium. These include nod-like receptor protein-3 (NLRP3) are hemolysin BL (HBL), nonhemolytic enterotoxin (NHE), and cytotoxin which are produced by vegetative cells growing in small intestine, mimic diarrheal syndrome11. Notably, symptoms typically appear 6–15 h after the ingestion of contaminated food that has been left for more than 2 h. These symptoms include profuse watery diarrhea, abdominal pain, cramping and vomiting. A comparable situation occurring in our current case.
Additionally, emetic toxins mimic symptoms like those caused by S. aureus, including nausea and vomiting, manifesting within 30 min–6 h after ingesting contaminated food, even if it has been reheated. These toxins are pH- stable, resistant to heat and proteases due to the presence of cereulide, an ionophoric low-molecular-weight dodecadepsipeptide3.
In this current case, it is plausible that diarrhea and vomitus which contaminated the penis post-intercourse is likely the source of the skin infection.
The pathogenesis behind the development of such an infection by this organism may be related to the presence of a range of virulence factors including HBL, Nhe or cytotoxin K (CytK). These factors possess dermonecrotic, cytotoxic, hemolytic, and may alter the vascular permeability in the animal models described in the literature. This would result in a wide range of dermatologic presentations from superficial necrosis to necrotizing fasciitis and myonecrosis as reported in a few cases in the literature8.
The treatment of B. cereus infection varies depending on the site and severity of the infection. Infections of the GI system is often self-limited and require supportive care only. However, in case of focal or systemic infection, rapid intervention with antibiotics is crucial. The first-line antibiotics for this more severe infection include vancomycin, gentamicin, chloramphenicol, ciprofloxacin, or carbapenems12. Non-complicated penile skin infections occurring secondary to penetrating injuries are usually self-limited and may be treated with topical or oral antibiotics4. In the current case, Fucidic acid ointment was sufficient to resolve the penile skin infection with B. cereus.
In conclusion, we report a unique case of penile skin infection caused by B. cereus, an unusual culprit for an uncommon presentation that was successfully treated with fucidic acid ointment. This is the first case in literature describing such an entity.
Ethical approval
This manuscript does not contain personal and/or medical information about an identifiable individual. Consent to write and publish this article was obtained from the patient.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Source of funding
None.
Author contribution
B.B.: conceptualization, review and editing, supervision. O.N.: resources, writing—original draft, supervision, review and editing. J.M.: writing—original draft, review and editing. G.A.: resources, writing—original draft, review and editing. A.E.Z.: resources, writing—original draft, review and editing. N.E.S.: resources, writing—original draft.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
The article is a case report and does not need to be registered.
Guarantor
Bassel Bachir.
Data availability statement
The images provided and chart reported in the article are available upon request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
O.G.N., J.H.M. contributed equally to this manuscript and are first authors.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Oussama G. Nasrallah, Email: on10@aub.edu.lb.
Jana H. Mahdi, Email: janaamahdi@icloud.com.
George F. Araj, Email: garaj@aub.edu.lb.
Noura El Sayegh, Email: ne121@aub.edu.lb.
Aline El Zakhem, Email: az51@aub.edu.lb.
Bassel G. Bachir, Email: bb12@aub.edu.lb.
References
- 1.Guinebretière MH, Thompson FL, Sorokin A, et al. Ecological diversification in the Bacillus cereus Group. Environ Microbiol 2008;10:851–865. [DOI] [PubMed] [Google Scholar]
- 2.Kimura 木村 啓太郎 K, Yokoyama 横山 智 S. Trends in the application of Bacillus in fermented foods. Curr Opin Biotechnol 2019;56:36–42. [DOI] [PubMed] [Google Scholar]
- 3.McDowell RH, Sands EM, Friedman H. Bacillus Cereus. StatPearls StatPearls Publishing Copyright © 2024. StatPearls Publishing LLC.; 2024. [Google Scholar]
- 4.Cree GE, Willis AT, Phillips KD, et al. Anaerobic balanoposthitis. Br Med J (Clin Res Ed) 1982;284:859–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards SK, Bunker CB, van der Snoek EM, et al. 2022 European guideline for the management of balanoposthitis. J Eur Acad Dermatol Venereol 2023;37:1104–1117. [DOI] [PubMed] [Google Scholar]
- 6.Aygun FD, Aygun F, Cam H. Successful treatment of Bacillus cereus bacteremia in a patient with propionic acidemia. Case Rep Pediatr 2016;2016:6380929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esmkhani M, Shams S. Cutaneous infection due to Bacillus cereus: a case report. BMC Infect Dis 2022;22:393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michelotti F, Bodansky HJ. Bacillus cereus causing widespread necrotising skin infection in a diabetic person. Pract Diabetes 2015;32:169–70a. [Google Scholar]
- 9.Soudet S, Becquart C, Dezoteux F, et al. Bacillus cereus endocarditis and a probable cutaneous gateway. Ann Dermatol Venereol 2017;144:45–48. [DOI] [PubMed] [Google Scholar]
- 10.Newman P, Garcia M, Ward R, et al. A rare case of Bacillus cereus septic arthritis. Cureus 2022;14:e33148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beecher DJ, Wong AC. Improved purification and characterization of hemolysin BL, a hemolytic dermonecrotic vascular permeability factor from Bacillus cereus. Infect Immun 1994;62:980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luna VA, King DS, Gulledge J, et al. Susceptibility of Bacillus anthracis, Bacillus cereus, Bacillus mycoides, Bacillus pseudomycoides and Bacillus thuringiensis to 24 antimicrobials using Sensititre automated microbroth dilution and Etest agar gradient diffusion methods. J Antimicrob Chemother 2007;60:555–567. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The images provided and chart reported in the article are available upon request.



