Questions
How are acquired abdominal wall defects managed?
What are the reconstructive options for abdominal wall defects?
What are the advantages of free flaps in abdominal wall reconstruction?
Is the latissimus dorsi free flap a good option for abdominal wall reconstruction?
Case Description
A 34-year-old female patient with history of resection of an abdominal wall desmoid tumor and reconstruction with a component separation technique presented 12 months after surgery reporting pain adjacent to the surgical site, which was ultimately determined to be a local recurrence. The resection of the recurrence included the tumor (approximately 12 × 10 × 10 cm), skin, the cartilaginous sections of the seventh and eighth left costal arches, omentum left anterior leaflet of the diaphragm, and the medial half of the right rectus abdominis muscle (Figure 1). The abdominal wall defect was reconstructed by placing a 15 × 18-cm 2-component mesh fixed to the aponeurosis. In addition, a small defect was created at the superior edge of the mesh, through which a pedicled omentum flap was exteriorized. Four weeks later, the patient developed mesh exposure and peritoneal-cutaneous communication (Figure 2).
Figure 1.

Recurrent multilobed abdominal wall desmoid tumor. The resection included the tumor, the overlying skin anteriorly, the cartilaginous sections of the seventh and eighth left costal arches, partially the omentum and left anterior leaflet of the diaphragm, and the medial half of the right rectus abdominis muscle posteriorly.
Figure 2.
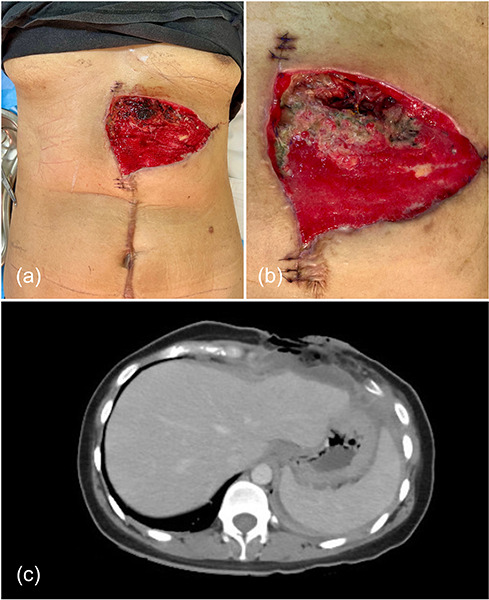
Three weeks after secondary reconstruction with a 2-component mesh fixed to the surrounding aponeurosis and an exteriorized pedicled omentum flap, the patient developed partial necrosis of the flap (A), with mesh exposure and, ultimately, peritoneal-cutaneous communication (B, C).
Salvage reconstruction with a vascularized latissimus dorsi (LD) myocutaneous free flap was performed using the left internal mammary vessels as recipient (Figure 3). Total hospitalization length was 18 days. Eight weeks after surgery, the patient exhibited a well-perfused flap with all the surgical wounds adequately healed. Computed tomography scan showed satisfactory restoration of the abdominal wall integrity (Figure 4).
Figure 3.
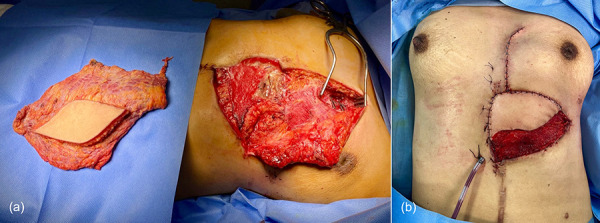
Vascularized latissimus dorsi free flap and recipient area, with the left internal mammary vessels exposed (A). Flap inset (B).
Figure 4.
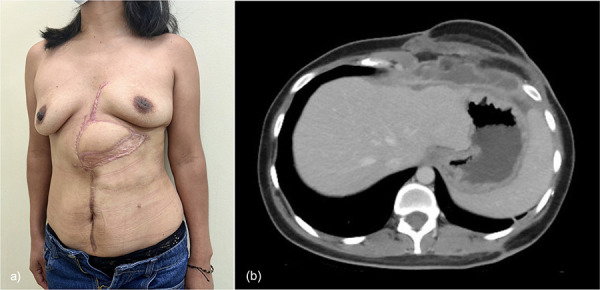
Six months after surgery, patient showing a well-perfused flap, with a totally incorporated skin graft, and all the surgical wounds adequately healed (A). Computed tomography scan showed satisfactory restoration of the abdominal wall integrity (B).
Q1. How are acquired abdominal wall defects managed?
Acquired abdominal wall defects resulting from previous surgeries, tumor resection, infection, or trauma present a significant challenge for both general and reconstructive surgeons. Traditionally, partial-thickness defects and/or limited tissue loss are addressed with local skin, muscle, and/or aponeurotic flaps, often requiring component separation of the abdominal wall layers to provide fascial apposition. Alternatively, regional flaps (including muscle, myocutaneous, and omental flaps) offer viable options for autologous coverage of larger defects. Additionally, the use of a tailored mesh placed in a preperitoneal or preaponeurotic plane has proven to provide lasting reinforcement to the weakened abdominal wall.
Previously, the selection of the “suitable option” followed the reconstructive ladder, an algorithmic approach aimed at achieving the best defect coverage through the simplest means.1 However, the current management of abdominal wall defects places a greater emphasis of adhering to the “like-with-like” reconstruction principle, regardless of the complexity of the reconstructive technique, aiming to restore functional stability, structural integrity, protection and retention of internal organs, and, ideally, physiologic muscle contraction.2 Furthermore, decision-making in specific scenarios should not solely focus on achieving primary wound coverage but should also consider effectively preventing the potential need for subsequent reconstruction. In light of these considerations, free flaps have emerged as an important tool in the reconstructive surgeon's armamentarium, as advancements in microsurgical techniques have facilitated their widespread use in an effective and safe manner.
Q2. What are the reconstructive options for abdominal wall defects?
Prosthetic materials: The use of synthetic mesh for reinforcing the abdominal wall is deemed suitable for aseptic cases. Regardless of the technique, careful deliberation should be given to selection of mesh material and method of mesh fixation to the abdominal wall.
Skin grafts: Primarily employed in cases of significant abdominal trauma and cutaneous-only defects. Once the wound achieves stability, grafts can be removed through dermabrasion or excision methods.
Local flaps: Skin and subcutaneous flaps can be based laterally on the intercostal vessels, on perforators from the deep circumflex iliac artery, or on axial vessels from the superficial circumflex iliac, superior epigastric, or superficial external pudendal arteries. The external oblique can be used as either a medially based musculofascial turnover flap or a laterally based musculocutaneous flap. The rectus muscle, based on either the superior epigastric or the deep inferior epigastric vessels, can be used as a muscle or musculocutaneous flap.
Regional flaps: The omentum, the tensor fascia latae, and the rectus femoris muscles are most commonly used, while the gracilis muscle has more limited applications.
Free flaps: Free tissue transfer may be necessary when dealing with a large defect and when no adequate local or regional flaps are available. Various flap options are available, among which the anterolateral thigh, tensor fasciae latae, gracilis, and LD flaps are the most frequently employed choices.
Q3. What are the advantages of free flaps in abdominal wall reconstruction?
The transfer of vascularized free flaps offers significant advantages by mobilizing healthy tissue with a rich blood supply, which improves the healing process, enhances resistance to infection, and enables high-quality reconstruction.3,5 As aforementioned, these flaps are indicated for extensive defects and situations where reliable pedicled options are not available, such as in patients with previous abdominal procedures. In such cases, the risk of compromising the tissue vascularity and the low reliability of the vascular pedicle-angiosome relation can jeopardize the success rate and, therefore, the trustworthiness of regional/pedicled reconstructive techniques.3
Moreover, when transferred as functional free flaps, they allow for the mobilization of sizable muscles with sufficient contractile capacity and strength to replace the motor function of the abdominal wall when it is significantly impaired. This is particularly relevant when both rectus abdominis muscles are missing or when one hemiabdomen of oblique muscles, combined with the ipsilateral rectus muscle, are absent.
A variety of flap options are available, with some of the most common being the LD, anterolateral thigh, tensor fasciae latae, and gracilis flaps. The LD muscle offers a large surface area flap that can be used with a small skin paddle or as a muscle- only flap with a skin graft directly over the flap. Both the anterolateral thigh and tensor fascia latae provide skin coverage and a robust fascial supportive layer. On the other hand, the gracilis muscle or myocutaneous flap is smaller in comparison and should be preserved for specific small defect scenarios.
Q4. Is the latissimus dorsi free flap a good option for abdominal wall reconstruction?
First described for abdominal wall reconstruction by Houston et al in 1988,6 the free vascularized LD flap has demonstrated its efficacy in restoring the integrity of the anatomical area, intra-abdominal organ retention, and functional stability.2,4,7 By coapting the thoracodorsal nerve to the intercostal nerves, a physiological reinnervation of the LD is provided and, therefore, a dynamic contraction of the abdominal wall is reestablished. Moreover, voluntary synergistic contractility of the abdominal wall is restored, which represents a functionally and esthetically superior result compared with any other muscles transferred from the thigh.2
However, valid concerns have been raised with regard the impact of LD flap harvest on the functionality of the upper extremity. Patients requiring abdominal wall reconstruction often rely on upper extremity strength and range of motion to perform daily activities. While this consideration might incline the reconstructive plan toward using thigh-based fasciocutaneous flaps, such as the anterolateral thigh or the tensor fasciae latae flaps, in cases of infected defects, muscle or myocutaneous flaps offer advantages for infection control over fasciocutaneous flaps, especially when thorough debridement is challenging due to the risk of exposure of intraabdominal organs.8,9 Furthermore, the LD flap has proven to be an effective option in severely infected abdominal defects, improving wound healing, and overcoming local infections or spreading of bacterial inoculation.10
Overall, the LD flap fulfills the requirements of anatomic and dynamic function in reconstruction of complex abdominal wall defects, establishing it as a first-line microsurgical option in numerous institutions, including our own.
Acknowledgments
Disclosures: None of the authors declare any conflict of interest. The authors alone are responsible for the content and writing of this paper. This study was funded entirely by its authors.
References
- 1.Rohrich RJ, Lowe JB, Hackney FL, Hobar PC. An algorithm for abdominal wall reconstruction. Plast Reconstr Surg. 2000; 105:202-216. 10.1097/00006534-200001000-00036 [DOI] [PubMed] [Google Scholar]
- 2.Ninkovic M, Ninkovic M, Öfner D, Ninkovic M. Reconstruction of large full-thickness abdominal wall defects using a free functional latissimus dorsi muscle. Front Surg. 2022. Mar 17;9:853639. 10.3389/fsurg.2022.853639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasconez HC, Sengezer M, McGrath PC. Flap coverage of a large defect after excision of a massive dermatofibrosarcoma protuberans. Plast Reconstr Surg. 1995;95:136-141. doi: 10.1097/00006534-199501000-00023 10.1097/00006534-199501000-00023 [DOI] [PubMed] [Google Scholar]
- 4.Ninkovic M, Kronberger P, Harpf C, Rumer A, Anderl H. Free innervated latissimus dorsi muscle flap reconstruction of full-thickness abdominal wall defects. 1998;101:971-978. [DOI] [PubMed] [Google Scholar]
- 5.Ninkovic M, Schoeller T, Benedetto K-P, Anderl H. Emergency free flap cover in complex injuries of the lower extremities. Scand J Plast Reconstr Surg Hand Surg. 1996;30:37-47. 10.3109/02844319609072403 [DOI] [PubMed] [Google Scholar]
- 6.Houston GC, Drew GS, Vazquez B, Given KS. The extended latissimus dorsi flap in repair of anterior abdominal wall defects. Plast Reconstr Surg. 1988;81:917-924. 10.1097/00006534-198806000-00015 [DOI] [PubMed] [Google Scholar]
- 7.Sharma RK, Verma GR, Biswas G. Reconstruction of a major abdominal and chest wall defect using latissimus dorsi and extended deep inferior epigastric artery flap. Ann Plast Surg. 1992;28:366-369. 10.1097/00000637-199204000-00012 [DOI] [PubMed] [Google Scholar]
- 8.Gosain A, Chang N, Mathes S, Hunt TK, Vasconez L. A study of the relationship between blood flow and bacterial inoculation in musculocutaneous and fasciocutaneous flaps. Plast Reconstr Surg. 1990;86:1152-1163. 10.1097/00006534-199012000-00019 [DOI] [PubMed] [Google Scholar]
- 9.Calderon W, Chang N, Mathes SJ. Comparison of the effect of bacterial inoculation in musculocutaneous and fasciocutaneous flaps. Plast Reconstr Surg. 1986;77:785-794. 10.1097/00006534-198605000-00016 [DOI] [PubMed] [Google Scholar]
- 10.Kim SW, Han SC, Hwang KT, Ahn BK, Kim JT, Kim YH. Reconstruction of infected abdominal wall defects using latissimus dorsi free flap. ANZ J Surg. 2013. Dec;83(12):948-953. 10.1111/j.1445-2197.2012.06286.x [DOI] [PubMed] [Google Scholar]


