Questions
Q1. What are the options for breast reconstruction after successful oncologic treatment?
Q2. What are some of the consequences of mis-sizing breast implants?
Q3. What are the indications for intraoperative breast sizers?
Q4. What are the current options for intraoperative breast sizers?
Case Description
A 63-year-old female patient underwent a bilateral skin-sparing mastectomy (SSM) with bilateral tissue expander-to-implant breast reconstruction for a right-sided estrogen/progesterone-positive invasive lobular carcinoma of the breast. Following the SSM, the plastic surgery and reconstructive team (PRS) performed immediate reconstruction with 300-mL subpectoral tissue expanders, double-drape rearrangement of mastectomy skin, and double-donut nipple-areolar grafting (Figure 1).
Figure 1.
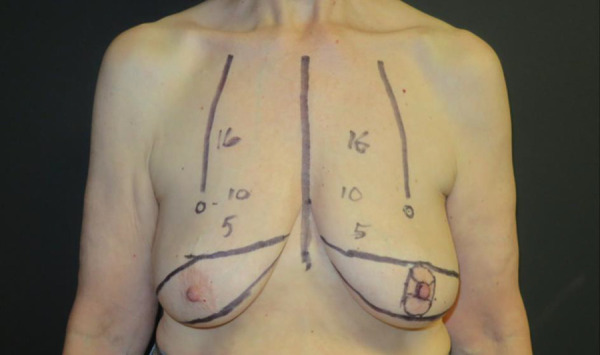
Preoperative measurements before bilateral skin-sparing mastectomy, 300-mL subpectoral tissue expander placement, double-drape rearrangement of mastectomy skin, and double-donut nipple-areolar grafting.
Subsequently, the patient would attend weekly or biweekly postoperative office visits, and at these visits she underwent serial expansion until each tissue expander reached 310 mL of saline. Three months after expander placement, the PRS performed expander-to-implant exchange with the corresponding preoperative markings (Figure 2).
Figure 2.
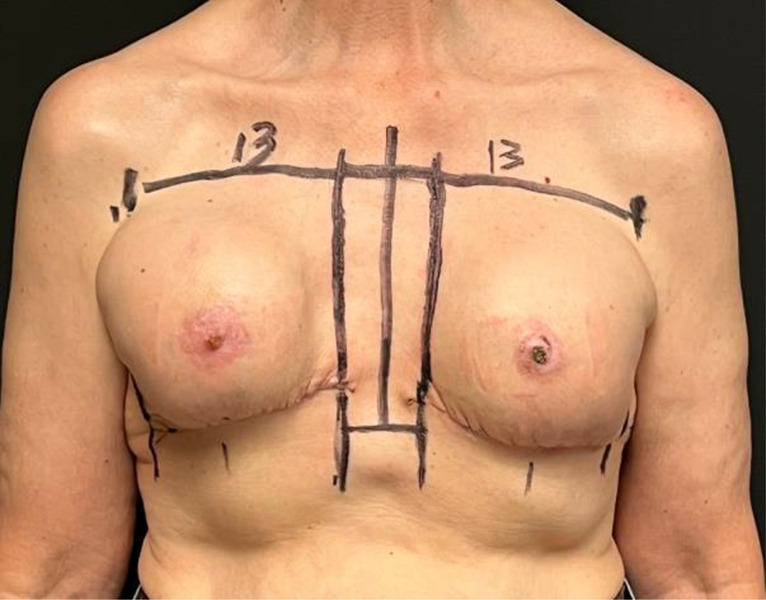
Preoperative measurements with tissue expanders before second stage.
The senior author uses 12 × 12-inch X-ray-detectable dry laparotomy pads (lap pads) as “implant sizers” to intraoperatively fill the breast pocket, assessing pocket volume to help select the appropriate size permanent implant. He found that 1 dry lap pad can approximate 100 mL. Therefore, in this case, 6 lap pads approximated a 600-mL implant. Following the insertion of 6 lap pads without the use of excess force, one can observe the symmetrical contour between the left and right breast and the edge of skin closure (Figure 3). The breast pocket was ultimately closed with 600-mL high-profile gel implants, (Figure 4), and the patient had no complications to date.
Figure 3.
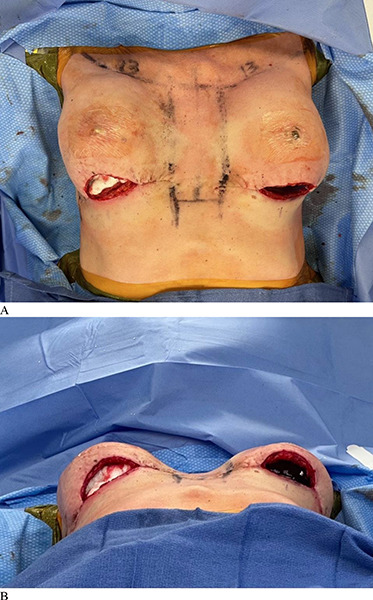
Intraoperative images comparing a 600-mL high-profile round gel implant (left breast) to 6 lap pads (right breast). (A) Birds eye view. (B) Inferior view.
Figure 4.
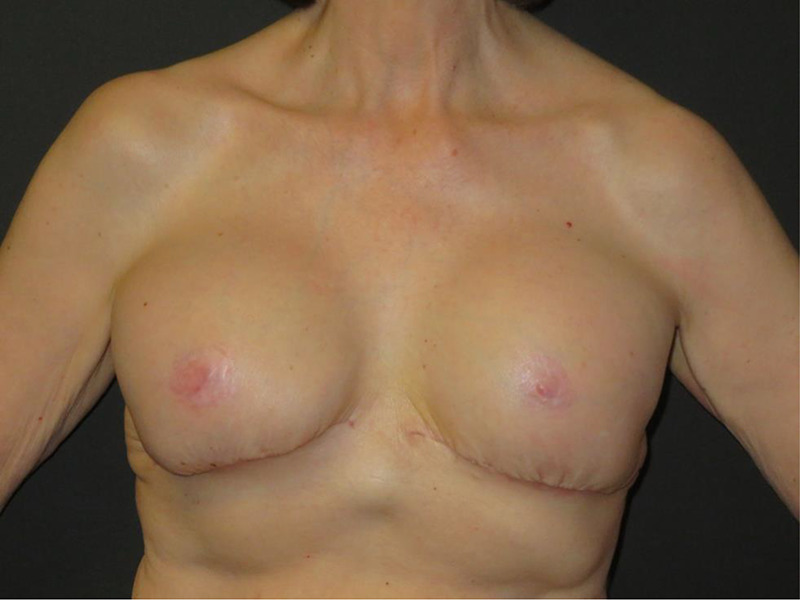
Postoperative view of breasts containing 2 600-mL high-profile round gel implants.
Q1. What are the options for breast reconstruction after successful oncologic treatment?
Breast cancer is the most common new cancer diagnoses and the second most common cause of cancer death among women in the US.1 Surgery is a standard of care for breast cancer treatment; thus, many women undergo either a lumpectomy or mastectomy with or without adjuvant radiation and chemotherapy. Additionally, over 40% of women in the US who undergo mastectomy for breast cancer opt for immediate implant-based breast reconstruction to improve their quality of life.2
Reconstruction consists of autologous or alloplastic techniques with implant-based techniques accounting for the vast majority (81%).2 Alloplastic reconstruction is traditionally performed in 2 stages. In the first stage, a tissue expander is inserted above or below the pectoralis muscle, followed by serial outpatient saline expansion.3 The tissue expander is removed in the second stage and exchanged with an implant. This staged method allows for patient feedback on their breast size in addition to any refinement procedures.3 Direct-to-implant is another alloplastic approach; it entails final implant insertion at the time of mastectomy. This presents with its own technical challenges and may still require a subsequent revision operation.3 Direct-to-implant reconstructions are best suited for patients who wish to maintain their current breast size, have undergone a nipple-sparing mastectomy, have thick mastectomy flaps, have no history of smoking, and have few medical comorbidities.4
Autologous reconstruction uses the patient's own tissue for reconstruction and is further broken down into pedicle versus free flap. Pedicle flaps originate from tissue adjacent to the breast using native blood supply.3 Examples of pedicle flaps include the transverse rectus abdominis musculocutaneous flap and latissimus dorsi flap.5 Alternatively, free flaps can be taken from adjacent or remote areas for breast reconstruction; they are disconnected from their native blood supply and reconnected in the breast area.3
As aforementioned, the patient presented in this publication underwent a double-donut, double-drape procedure immediately after tissue expander implantation. The senior author prefers this surgical technique in cases like this to enhance aesthetic outcomes in conjunction with neoadjuvant treatments. The double-drape technique involves using 2 drape flaps to close the breast wound. The inferior mastectomy flap is draped cephalically and repaired over the pectoralis muscle and subpectoral expander (air-filled by manufacturer). The inferior mastectomy flap is then de-epithelialized. Then, the upper mastectomy flap is draped caudally and repaired to the inframammary fold. One transverse scar in the inframammary fold avoids inverted dehiscence. The double-donut nipple-areolar reconstruction involves harvesting the nipple-areolar complex (NAC) from the non-cancer side at the outset of the operation. The shared NAC is then defatted aggressively under the areola. Two round, donut-shaped areolar grafts are constructed from the harvested larger NAC. The nipple graft is left thicker as a composite graft and split into 2 nipple composite grafts. The predetermined new NAC site is de-epithelialized for a 2 to 3-cm diameter in a round configuration, the half nipple composite grafts are sutured in the center, and donut areolar grafts are positioned and repaired circumferentially to de-epithelialized recipient sites and bolstered for 3 weeks.
Q2. What are some of the consequences of mis-sizing breast implants?
The most common causes for breast implant revision include capsular contracture, ptosis of an aging breast, and implant malposition.6 The most devastating consequences of mis-sizing the implant include wound separation leading to implant explantation or delaying the adjuvant oncological treatment due to complications. Hence, accurately measuring the breast pocket prior to implant placement is crucial.
Implant malposition is one of the leading causes of revision following breast augmentation. Implant malposition rates can be as high as 5% in primary augmentation and 10% in secondary augmentation.7,9 Implant malposition is multifactorial, with one of its causes linked to implant selection.4 Thus, selection of the proper implant size and projection is imperative to further decrease the likelihood of implant malpositioning. If an implant is too large, the pocket will distort the breast parenchyma and skin, leading to suboptimal outcomes and implant malposition.6
Implant malposition also increases the financial burden for patients when revisions are necessary. If an implant is removed from its packaging but doesn't fit, the surgeon cannot repackage it and use it for another patient. In addition, other common breast augmentation complications, including implant infection and prosthetic exposure, may add an estimated $12,554 and $17,153, respectively, to the final cost.10 These financial burdens eventually fall on both the patient and healthcare system at large.
Q3. What are the indications for intraoperative breast sizers?
In order to achieve cosmetically reproducible breast reconstruction results, one must pay careful attention to both preoperative and intraoperative breast implant size planning. Effective intraoperative breast sizing implementation can aid in minimizing the reoperation rate, which for breast reconstruction can be as high as 40%.11 Surgeons utilize intraoperative breast sizers to establish the ideal volume for the implant after pocket dissection. Intraoperative breast sizers assess visually the 3-dimensional configuration and projection required to adequately fill the breast pocket. This technique lends itself to high utilization rates by residents and trainees to rapidly and effectively select implant size.12 Even for an experienced surgeon, measuring the pocket volume can prove to be difficult during a reconstruction surgery following mastectomy, particularly in the presence confounding variables. Surgeons may opt for a more precise method to measure breast pocket volume, such as purchasing an intraoperative breast sizer at a cost.
Q4. What are the current options for intraoperative breast sizers?
Numerous options for intraoperative breast sizers exist, and the method employed is largely up to the discretion of the surgeon. Many reconstructive surgeons use the widely available company-specific “implant sizers,” which come in various sizes and shapes. These sizers can either be prefilled with silicone and resterilizable for a preset number of uses, or they can be single-use disposable sizers filled with saline intraoperatively and discarded after use.13 These readily available implant sizers tend to be expensive and require intraoperative trial and error to achieve the desired result. Moreover, reusable implant sizers introduce sterility concerns potentially requiring revision due to infectious complications.14
Many surgeons will forgo purchasing implant sizers and instead opt for do-it-yourself (DIY) intraoperative sizers, which consist of readily available materials found in the operating room that can be used to assess the breast pocket volume. Some authors have described simple techniques such as filling a brassiere with rice preoperatively.15,16 However, these estimates cannot be changed during surgery, nor can they account for variations based on external estimates or submuscular implantation.12 Other DIY methods to size the pocket and estimate projection include temporally trapping air in the pocket or making use of simplified cotton sizers, a glove and luer lock system, and gauze swabs.12,17,20
Alternative imaging-focused, rather than medical device/DIY methods, for assessing breast volume include Grossman-Roudner cones and magnetic resonance imaging (MRI), the “High Five” process, anthropomorphic measurements, biostereometric analysis, and mammography. These methods usually have an additional associated cost and require additional personnel.21,26
In this case, we present the use of dry laparotomy pads as a safe, cost-effective, and easy-to-use method for measuring the breast pocket prior to expander-to-implant exchange. We describe our discovery of a reproducible way to estimate the breast pocket size using a common operating room object that is standardized and widely available. Introducing lap pads to the surgical field in a sterile manner at the beginning of each case ensures that excess packaging is not opened, as might happen when using packaged sizers, which could introduce unnecessary contamination. This approach allows for maximum patient satisfaction, effective complication control, and reduced costs for the patient.
Tissue expander fill volume often underpredicts the final pocket volume because the expander may not be filling the entire diameter of the pocket circumferentially. Therefore, the use of lap pad sizers becomes a valuable tool for selecting the final implant. This case demonstrates how inserting dry lap pads into the breast pocket to assess volume and projection to the nearest 100 mL highlights a reliable and readily reproducible method to select the appropriate implant for a patient.
Acknowledgments
Ethics: The patient described in this document has been provided informed consent on the use of their images, and granted the use of their images for scientific publications.
Disclosure: The authors disclose no financial or other conflicts of interest.
References
- 1.Broyles JM, Balk EM, Adam GP, et al. Implant-based versus autologous reconstruction after mastectomy for breast cancer: a systematic review and meta-analysis. Plast Reconstr Surg Glob Open. 2022;10(3):e4180. doi:10.1097/GOX.0000000000004180 10.1097/GOX.0000000000004180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saldanha IJ, Broyles JM, Adam GP, et al. Implant-based breast reconstruction after mastectomy for breast cancer: a systematic review and meta-analysis. Plast Reconstr Surg Glob Open. 2022;10(3):e4179. doi:10.1097/GOX.0000000000004179 10.1097/GOX.0000000000004179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Somogyi RB, Ziolkowski N, Osman F, Ginty A, Brown M. Breast reconstruction: updated overview for primary care physicians. Can Fam Physician. 2018;64(6):424-432. [PMC free article] [PubMed] [Google Scholar]
- 4.Brown MH, Somogyi RB, Aggarwal S. Secondary breast augmentation. Plast Reconstr Surg. 2016;138(1):119e-135e. doi:10.1097/PRS.0000000000002280 10.1097/PRS.0000000000002280 [DOI] [PubMed] [Google Scholar]
- 5.Regan JP, Casaubon JT. Breast Reconstruction. In: StatPearls. Updated 2023. Jul 23. https://www.ncbi.nlm.nih.gov/books/NBK470317/ [PubMed] [Google Scholar]
- 6.Denney BD, Cohn AB, Bosworth JW, Kumbla PA. Revision breast augmentation. Semin Plast Surg. 2021;35(2):98-109. doi:10.1055/s-0041-1727272 10.1055/s-0041-1727272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spear SL, Murphy DK, Slicton A, Walker PS, Inamed silicone breast implant U.S. study group . Inamed silicone breast implant core study results at 6 years. Plast Reconstr Surg. 2007;120(7 Suppl 1):8S-16S. doi:10.1097/01.prs.0000286580.93214.df 10.1097/01.prs.0000286580.93214.df [DOI] [PubMed] [Google Scholar]
- 8.Maxwell GP, Van Natta BW, Bengtson BP, Murphy DK. Ten-year results from the Natrelle 410 anatomical form-stable silicone breast implant core study. [published correction appears in Aesthet Surg J. 2015 Nov;35(8):1044].. Aesthet Surg J. 2015;35(2):145-55. doi:10.1093/asj/sju084 10.1093/asj/sju084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGuire P, Reisman NR, Murphy DK. Risk factor analysis for capsular contracture, malposition, and late seroma in subjects receiving Natrelle 410 form-stable silicone breast implants. Plast Reconstr Surg. 2017;139(1):1-9. doi:10.1097/PRS.0000000000002837 10.1097/PRS.0000000000002837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yan C, Fischer JP, Wes AM, et al. The cost of major complications associated with immediate two-stage expander/implant-based breast reconstruction. J Plast Surg Hand Surg. 2015;49(3):166-71. doi:10.3109/2000656X.2014.970639 10.3109/2000656X.2014.970639 [DOI] [PubMed] [Google Scholar]
- 11.Nelson JA, Voineskos SH, Qi J, et al. Elective revisions after breast reconstruction: results from the mastectomy reconstruction outcomes consortium. Plast Reconstr Surg. 2019;144(6):1280-1290. doi:10.1097/PRS.0000000000006225 10.1097/PRS.0000000000006225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caulfield RH, Niranjan NS. Innovative techniques: a novel technique for intraoperative estimation of breast implant size in aesthetic and reconstructive breast surgery. Aesthetic Plast Surg. 2008;32(1):126-129. doi:10.1007/s00266-007-9045-2 10.1007/s00266-007-9045-2 [DOI] [PubMed] [Google Scholar]
- 13.Henderson PW, Nash D, Laskowski M, Grant RT. Objective comparison of commercially available breast implant devices. Aesthetic Plast Surg. 2015;39(5):724-732. doi:10.1007/s00266-015-0537-1 10.1007/s00266-015-0537-1 [DOI] [PubMed] [Google Scholar]
- 14.Khoo LS, Radwanski HN, Senna-Fernandes V, Antônio NN, Fellet LLF, Pitanguy I. Does the use of intraoperative breast sizers increase complication rates in primary breast augmentation? a retrospective analysis of 416 consecutive cases in a single institution. Plast Surg Int. 2016;2016:6584810. doi:10.1155/2016/6584810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.James JH. What size prosthesis for augmentation mammaplasty? Ann Plast Surg. 1987;19(3):294-296. doi:10.1097/00000637-198709000-00017 10.1097/00000637-198709000-00017 [DOI] [PubMed] [Google Scholar]
- 16.Dionyssiou DD, Demiri EC, Davison JA. A simple method for determining the breast implant size in augmentation mammaplasty. Aesthetic Plast Surg. 2005;29(6):571-573. doi:10.1007/s00266-005-0103-3 10.1007/s00266-005-0103-3 [DOI] [PubMed] [Google Scholar]
- 17.Duscher D, Wenny R, Somma F, Huemer GM. A novel method for intraoperative breast implant pocket assessment: air augmentation. Arch Plast Surg. 2017;44(4):354-355. doi:10.5999/aps.2017.44.4.354 10.5999/aps.2017.44.4.354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ishii N, Tani Y, Kiuchi T, Uno T, Ando J, Kishi K. Optimal intraoperative selection of the projection of silicone breast implant using simplified cotton sizers. Gland Surg. 2019;8(5):537-541. doi:10.21037/gs.2019.10.01 10.21037/gs.2019.10.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choudhary S, Curnier A. An intraoperative DIY breast sizer. Br J Plast Surg. 2002;55(7):592-593. doi:10.1054/bjps.2002.3926 10.1054/bjps.2002.3926 [DOI] [PubMed] [Google Scholar]
- 20.Cerqueiro J, Mallucci P. The surgical glove as a breast sizer of adjustable volume: a cost-effective tool in aesthetic augmentation and reconstruction of the breast. Plast Reconstr Surg. 2002;110(2):704-705. doi:10.1097/00006534-200208000-00060 10.1097/00006534-200208000-00061 [DOI] [PubMed] [Google Scholar]
- 21.Caruso MK, Guillot TS, Nguyen T, Greenway FL. The cost effectiveness of three different measures of breast volume. Aesthetic Plast Surg. 2006;30(1):16-20. doi:10.1007/s00266-004-0105-6 10.1007/s00266-004-0105-6 [DOI] [PubMed] [Google Scholar]
- 22.Palin WE Jr, von Fraunhofer JA, Smith DJ Jr. Measurement of breast volume: comparison of techniques. Plast Reconstr Surg. 1986;77(2):253-255. doi:10.1097/00006534-198602000-00013 10.1097/00006534-198602000-00013 [DOI] [PubMed] [Google Scholar]
- 23.Adams WP. The High Five Process: tissue-based planning for breast augmentation. Plast Surg Nurs. 2007;27(4):197-201. doi:10.1097/01.PSN.0000306185.95812.c3 10.1097/01.PSN.0000306185.95812.c3 [DOI] [PubMed] [Google Scholar]
- 24.Kalbhen CL, McGill JJ, Fendley PM, Corrigan KW, Angelats J. Mammographic determination of breast volume: comparing different methods. AJR Am J Roentgenol. 1999;173(6):1643-1649. doi:10.2214/ajr.173.6.10584814 10.2214/ajr.173.6.10584814 [DOI] [PubMed] [Google Scholar]
- 25.Loughry CW, Sheffer DB, Price TE, et al. Breast volume measurement of 598 women using biostereometric analysis. Ann Plast Surg. 1989;22(5):380-385. doi:10.1097/00000637-198905000-00002 10.1097/00000637-198905000-00002 [DOI] [PubMed] [Google Scholar]
- 26.Sigurdson LJ, Kirkland SA. Breast volume determination in breast hypertrophy: an accurate method using two anthropomorphic measurements. Plast Reconstr Surg. 2006;118(2):313-320. doi:10.1097/01.prs.0000227627.75771.5c 10.1097/01.prs.0000227627.75771.5c [DOI] [PubMed] [Google Scholar]


