Summary
Nuclear pore complexes (NPCs) regulate nucleocytoplasmic transport and are anchored in the nuclear envelope by the transmembrane nucleoporin NDC1. NDC1 is essential for post-mitotic NPC assembly and the recruitment of ALADIN to the nuclear envelope. While no human disorder has been associated to one of the three transmembrane nucleoporins, biallelic variants in AAAS, encoding ALADIN, cause triple A syndrome (Allgrove syndrome). Triple A syndrome, characterized by alacrima, achalasia, and adrenal insufficiency, often includes progressive demyelinating polyneuropathy and other neurological complaints. In this report, diagnostic exome and/or RNA sequencing was performed in seven individuals from four unrelated consanguineous families with AAAS-negative triple A syndrome. Molecular and clinical studies followed to elucidate the pathogenic mechanism. The affected individuals presented with intellectual disability, motor impairment, severe demyelinating with secondary axonal polyneuropathy, alacrima, and achalasia. None of the affected individuals has adrenal insufficiency. All individuals presented with biallelic NDC1 in-frame deletions or missense variants that affect amino acids and protein domains required for ALADIN binding. No other significant variants associated with the phenotypic features were reported. Skin fibroblasts derived from affected individuals show decreased recruitment of ALADIN to the NE and decreased post-mitotic NPC insertion, confirming pathogenicity of the variants. Taken together, our results implicate biallelic NDC1 variants in the pathogenesis of polyneuropathy and a triple A-like disorder without adrenal insufficiency, by interfering with physiological NDC1 functions, including the recruitment of ALADIN to the NPC.
Keywords: NDC1, ALADIN, triple A syndrome, nuclear pore complex, peripheral neuropathy, alacrima, achalasia, neurodevelopmental disorder
This report describes the identification of biallelic NDC1 variants in children with a triple A-like syndrome, including intellectual disability, motor impairment, severe demyelinating with secondary axonal polyneuropathy, alacrima, and achalasia. The identified NDC1 variants interfere with physiological NDC1 functions, including the recruitment of ALADIN to the nuclear pore complex.
Introduction
The nuclear envelope (NE) is a specialized membrane that separates the nucleus from the cytoplasm. At sites where the inner and outer nuclear membrane fuse, nuclear pore complexes (NPCs) are embedded in the NE. The NPC consist of several multiprotein subcomplexes that are anchored in the membrane via three transmembrane nucleoporins: NDC1, POM121, and GP210.1 Altogether, the NPC subcomplexes form a cylindrical ring structure, which is essential for their most important functions: facilitating nucleocytoplasmic transport of proteins, RNAs, and other signaling molecules.2 In addition, transmembrane nucleoporins are involved in multiple other cellular processes such as transcriptional regulation, chromatin organization, and mitotic progression.3
Given their diverse functions, variants in genes encoding nucleoporins have been associated with a wide variety of disorders, including infantile bilateral striatal necrosis, nephrotic syndrome, and neurodevelopmental disorders.4,5,6 No disease-related variants have been described for the three essential transmembrane nucleoporins NDC1, POM121, and GP210. However, their upregulation is associated with various cancer types, including non-small cell lung cancer, cervical cancer, and esophageal squamous cell carcinoma.7,8,9 Increased NDC1 expression and mislocalization is also described in ventricular cardiac tissue of ischemic cardiomyopathy and dilated cardiomyopathy patients.10 In mice, a variant in NDC1 resulted in gametogenesis defects and skeletal malformations.11
NDC1 is a transmembrane nucleoporin that is essential for post-mitotic NE formation and NPC assembly.12,13 During the first steps of NE/NPC assembly, NDC1 is anchored in the NE via six transmembrane domains. Both its N and C termini face the NPC channel and facilitate the recruitment of other nucleoporins and membrane remodeling factors. The highly conserved large C-terminal tail of NDC1 recruits the nucleoporin ALADIN. At the NPC, ALADIN regulates selective nuclear import and is therefore essential for cellular homeostasis. Variants in AAAS, encoding for ALADIN, cause triple A syndrome, also known as Allgrove syndrome (OMIM: 231550). Triple A syndrome is an autosomal recessive disorder characterized by ACTH-resistant adrenal insufficiency, alacrima, achalasia, and a variety of neurological disturbances.14,15,16,17,18 In individuals with triple A syndrome, mislocalization of ALADIN is observed and is thought to be the main pathogenic mechanism underlying the disease.19,20,21
Here, we describe the first cohort of seven individuals, from four unrelated families, with biallelic variants in NDC1. The affected individuals present with alacrima, achalasia, and neurological features including developmental delay/intellectual disability, demyelinating and secondary axonal polyneuropathy, facial weakness, tongue fasciculation, and hypotonia, resembling the features observed in triple A syndrome. Cell biological studies were performed to provide insights into the molecular mechanisms contributing to disease pathogenesis.
Material and methods
Standard protocol approvals, registrations, and patient consents
The study was approved by the local ethics boards/IRBs. Clinical data from affected individuals were recruited through GeneMatcher.22 Written informed consent to participate in this study was obtained from all affected individuals or their parents/caretakers. Written informed consent for publication of photographs was obtained as applicable. Fibroblasts from affected individuals were obtained from skin biopsies previously sampled for routine diagnostics.
Exome sequencing
Exome sequencing was performed on DNA isolated from blood derived from probands and family members in different laboratories. Whole exome sequencing (WES) data are deposited internally in each medical institute, in respect to the privacy of the families. Details of sequencing and analysis pipelines are described in the supplemental methods.
RNA sequencing
The RNA sequencing pipeline used for family 1, individuals 1-I and 1-II, is described in Dekker et al.23 In short, skin biopsy-derived fibroblasts were cultured in Ham’s F10 medium containing 15% (v/v) fetal calf serum and 1% (v/v) penicillin/streptomycin. Fibroblast cultures for RNA sequencing were either untreated or treated with 100 μg/mL cycloheximide (Sigma-Aldrich) for 24 h. At a confluency of 70%–80%, RNA was isolated and RNA samples were enriched for polyadenylated RNA, followed by cDNA synthesis. Strand-specific sequencing was performed on an Illumina NovaSeq 6000 with 150 bp paired-end reads and unique molecular identifier-adaptors, generating a minimum of 40 million reads. Mapped RNA sequencing reads were visualized in the Integrative Genomics Viewer (IGV, v.2.14.5) using hg19 as reference genome.
Minigene assay
To confirm effects on splicing, a minigene exon-trapping assay was performed. NDC1 exon 9 and surrounding intronic sequences (∼100 bp upstream and downstream of splice donor and acceptor site) were amplified from genomic DNA and cloned into the pSPL3 vector (Thermo Fisher Scientific, Invitrogen) using Gibson assembly. HEK293T cells (70%–90% confluent) growing in a 12-well plate were transfected with 1 μg of the minigene constructed using 5 μg polyethyleneimine. After 24 and 48 h incubation, RNA was isolated using an RNeasy mini kit (QIAGEN, Venlo, the Netherlands), according to the manufacturer’s protocol, followed by cDNA synthesis using the iScript cDNA synthesis kit (Bio-Rad). Transcribed products from the vector were amplified using a standard set of primers. These RT-PCR products were visualized by agarose gel electrophoresis and confirmed by Sanger sequencing.
Immunofluorescence
Fibroblast cells were grown in Dulbecco’s modified Eagle’s medium supplemented with 10% (v/v) fetal calf serum and 1% (v/v) penicillin/streptomycin. Cells were regularly checked for mycoplasma infections. For immunostainings, fibroblast cells were grown on 24 mm coverslips (Thermo Fisher Scientific). Cells were fixed in 4% paraformaldehyde for 20 min on ice. After fixation, coverslips were blocked for 1.5 h on ice in blocking buffer containing 50 mM Tris-HCl (pH 7.4), 0.9% NaCl, 0.25% gelatin, 0.5% Triton X-100. Primary antibodies were diluted in blocking buffer and incubated overnight at 4°C. The next day, cells were incubated for 45 min with secondary antibodies and mounted on microscopy slides with ProLong Gold Antifade Reagent with DAPI (Thermo Fisher Scientific).
Antibodies
Primary antibodies: mouse anti-ALADIN (1:100, Santa Cruz, sc-374073), mouse anti-414 (MMS-120P, 1:500, BioLegend), and rabbit anti-CDT1 (D10F11, 1:200, Cell Signaling Technologies).
Secondary antibodies: goat anti-rabbit IgG (H + L) Alexa Fluor 488 (1:200, Thermo Fisher Scientific, A11088), Cy3 AffiniPure donkey anti-mouse IgG (H + L) (1:100, Jackson Laboratory, 715-165-150).
Confocal microscopy
Confocal fluorescent z stack images were acquired with the Broadband Leica TCS SP5, using Leica LAS AF application (Leica Microsystems). Lasers with 405, 488, and 561 nm excitation wavelength were used to visualize fluorescent secondary antibodies. Maximal projections of z stack images were processed with Fiji ImageJ software.
Super-resolution 3D-SIM microscopy was performed with the Elyra Zeiss PS1. Images were acquired using a 63× 1.4 NA oil objective, 405, 488, and 561 nm diode lasers with appropriate filters. The grating present in the light path was modulated in five phases and five rotations, and multiple z slices with an interval of 110 nm were recorded on an Andor iXon DU 885, 1002 × 1004 EMCCD camera. Raw images were reconstructed using the Zeiss Zen software and subsequently analyzed with Fiji ImageJ software.
Results
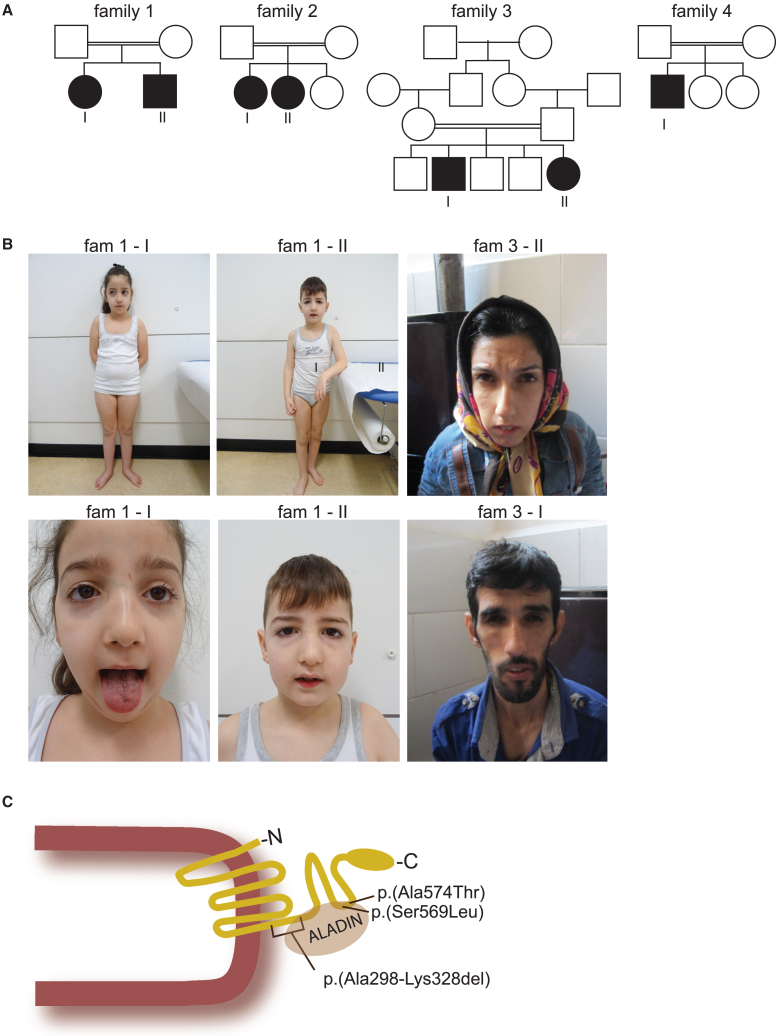
Genomic analysis, through WES or RNA sequencing, detected homozygous NDC1 variants in a cohort of seven individuals from four unrelated families (Figure 1A). Phenotypic features were very similar and are summarized in Table 1, while detailed clinical reports and additional information on the genomic alterations are provided in the supplemental information and Tables S1 and S2.
Figure 1.
Clinical features of affected individuals with NDC1 variants
(A) Pedigrees of four families with biallelic NDC1 variants. Affected individuals are depicted in black.
(B) Facial features of affected individuals 1-I, 1-II, 3-I, and 3-II. The lower panel in individual 1-I shows tongue fasciculations.
(C) Schematic drawing of the NDC1 protein in the nuclear envelope. The identified NDC1 variants and the interaction sites with ALADIN are depicted in the C-terminal NDC1 protein structure.
Table 1.
Summary of clinical features observed in individuals with biallelic NDC1 variants
| Ind 1-I | Ind 1-II | Ind 2-I | Ind 2-II | Ind 3-I | Ind 3-II | Ind 4 | % of individuals | |
|---|---|---|---|---|---|---|---|---|
| Variant in NDC1: NM_018087.5 | c.892-21G>A p.Ala298_Lys328del |
c.892-21G>A p.Ala298_Lys328del |
c.892-21G>A p.Ala298_Lys328del |
c.892-21G>A p.Ala298_Lys328del |
c.1706C>T p.Ser569Leu |
c.1706C>T p.Ser569Leu |
c.1720G>A p.Ala574Thr |
|
| Age at last investigation (years) | 12 | 10 | 13 | 10 | ±25 | 26 | 12 | |
| ID | borderline | borderline | mild | no | moderate | moderate | severe | 100 |
| Motor impairment | motor delay | motor delay | motor impairment | motor impairment | motor impairment | motor impairment | severe motor impairment | 100 |
| Clinical signs of polyneuropathy/EMG | yes (EMG confirmation) | yes (EMG confirmation) | yes (EMG confirmation) | yes, no EMG | yes, no EMG | yes, no EMG | no | 86 |
| Alacrima | yes | yes | yes | yes | not reported | yes | no | 71 |
| Dysphagia/achalasia | dysphagia, recurrent choking | suspect achalasia | no | no | achalasia | achalasia | dysphagia | 71 |
| Facial weakness | yes | yes | yes | not reported | yes | yes | not reported | 71 |
| Hypotonia | yes | yes | not reported | not reported | not reported | yes | yes | 57 |
| Tongue fasciculations | yes | yes | yes | yes | no | no | no | 57 |
| Growth delay | no | no | yes | yes | yes | yes | no | 57 |
| Epilepsy | no | no | no | no | no | yes | yes | 28 |
| Other autonomic features | no | no | yes | yes | no | no | no | 28 |
EMG, electromyography; ID, intellectual disability.
Clinical description
All described individuals were born after uncomplicated pregnancies with growth measurements within the normal range. In all, symptoms started in the first year of life, characterized by delayed motor development in most individuals. The individuals from family 3 initially presented with vomiting and recurrent aspiration, but also experienced delayed motor development in early childhood. All individuals had intellectual disability, with variable severity. Speech development was affected and ranged between normal and non-verbal. Nasal speech was frequently described (4/7), and often associated with facial weakness (Figure 1B). Feeding difficulties were described for 5/7 affected individuals, and were characterized by dysphagia and near chocking. In one individual achalasia was radiologically confirmed and treated with surgery.
Physical examination showed the involvement of the peripheral, central, and autonomic nervous system. Clinical signs of peripheral neuropathy were observed in all but one individual, and were confirmed with EMG in three individuals. EMG recordings showed a motor demyelinating polyneuropathy with secondary axonal injury. The most frequently reported peripheral neurological features were hypotonia, muscle atrophy, decreased muscle strength, and decreased deep tendon reflexes. Other lower motor neuron signs included facial weakness (5/7), tongue atrophy, and tongue fasciculations (4/7). Exceptionally, individual 4-I presented with increased muscle tone, contractures of the knees, elbows, and ankles. He also developed epilepsy in the first year of life, characterized by atonic/tonic episodes or head drops. Epilepsy was also reported for individual 3-II. Dysfunction of the autonomic nervous system was seen in 5/7 individuals. Alacrima or hypolacrima was the most frequent autonomic feature and present in 5/7 individuals. In addition, limited heart rate variability was observed in two individuals.
The most frequently described facial features are related to facial muscle weakness, with downslant of the eyelids, a long thin nose, a high arched palate and a pre-auricular tag (Figure 1B). Examination of the hands and feet showed tapered fingers (3/7), hypotrophy of the muscles on the hands and feet (4/7), and hyperkeratosis (2/7). Remarkably, none of the affected individuals had adrenal insufficiency. Baseline cortisol levels were normal and normal responses to ACTH stimulation were observed. Brain MRI showed no major structural abnormalities except mild dilatation of the ventricles and prominent perivascular spaces in two individuals. Muscle CT in individual 1-I showed normal musculature of neck and shoulder, mild atrophy of the pelvis muscles, moderate atrophy of the hamstrings, and severe atrophy with fatty infiltration of the gastrocnemius and soleus muscles.
Genomic analysis
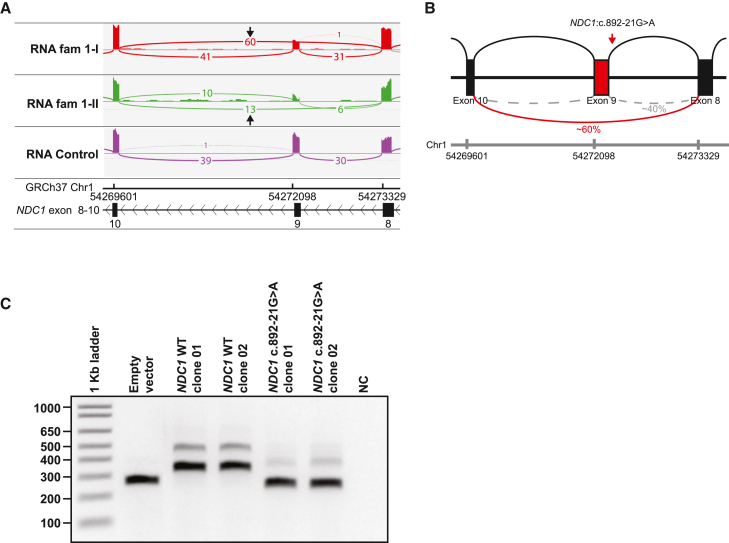
In family 1, diagnostic WES and SNP arrays did not identify pathogenic variants in both siblings, which could explain the phenotype (Table S3). SNP array showed multiple regions of homozygosity and a maternally inherited 215 kb duplication on chromosome 3q13, most likely unrelated to the phenotype. Diagnostic RNA sequencing analysis on both siblings of the overlapping ROH revealed reduced expression of exon 9 of NM_018087.4 (NDC1) (Figures 2A, S1A, and S1B). Skipping of exon 9 was observed in ∼60% of the reads. This exon 9 skip would result in an in-frame deletion of 30 amino acids (r.892_984del, p.Ala298_Lys328del) (Figures 1C and 2B). Re-analysis of WES data revealed an intronic homozygous variant in intron 8 of NDC1, c.892-21G>A, in both siblings. This variant is absent in gnomAD (v.2.1.1)24 and both parents were heterozygous carriers. Splice prediction software predicted that this variant results in a loss of the canonical splice acceptor site (SpliceAI: Δ score = 0.27; Δ score > 0.2 indicates potential effect on splicing, likely by creating an AG dinucleotide in the polypyrimidine tract between the splice acceptor and branchpoint, an alteration able to disrupt the canonical splice acceptor site) (Table S2; Figure S1C).25 A minigene assay confirmed that the c.892-21G>A variant indeed caused skipping of exon 9 (Figure 2C). In family 2, WES identified the same homozygous variant as identified in family 1 (NM_018087.4(NDC1):c.892-21G>A, r.892_984del, p.Ala298_Lys328del). Homozygosity for this variant was confirmed by segregation analysis of both parents and the healthy sister, who were all heterozygous.
Figure 2.
Functional analysis of the variant identified in family 1
(A) Sashimi plot showing partial skipping of exon 9 NDC1 in both affected individuals from family 1. These samples were not treated with cycloheximide (CHX–).
(B) Schematic representation of the effect of the homozygous NDC1:c.892-21G>A variant on splicing. In approximately 60% of the reads skipping of exon 9 is observed.
(C) Minigene assay confirming the effect of the NDC1:c.892-21G>A variant on splicing. HEK293T cells were transfected with plasmid DNA isolated from two independent clones containing NDC1 with the c.892-21G>A variant, two clones with WT NDC1 sequence, or an empty vector. RT-PCR of the transcribed minigene was performed showing that the NDC1:c.892-21G>A induces skipping of exon 9 not seen in WT samples. NC, negative control.
In families 3 and 4 homozygous missense variants were identified. In family 3, WES identified a homozygous missense variant in NDC1 (NM_018087.5(NDC1): c.1706C>T, p.Ser569Leu in both affected siblings within a large region of autozygosity (Figure 1C). The CADD (combined annotation-dependent depletion) score26 of this variant was 28.7 and the variant was predicted to be probably damaging by PolyPhen2,24 benign by MutationTaster, and tolerated by SIFT (Table S2). The variant is absent in gnomAD. In family 4, WES identified a homozygous missense variant in NDC1: NM_018087.5(NDC1): c.1720G>A, p.Ala574Thr (Figure 1C). The variant is absent in gnomAD27 and its CADD score is 27.1. The pathogenicity prediction program PolyPhen2 reports probably damaging effects, and SIFT classifies the variant as “tolerated” (Table S2).
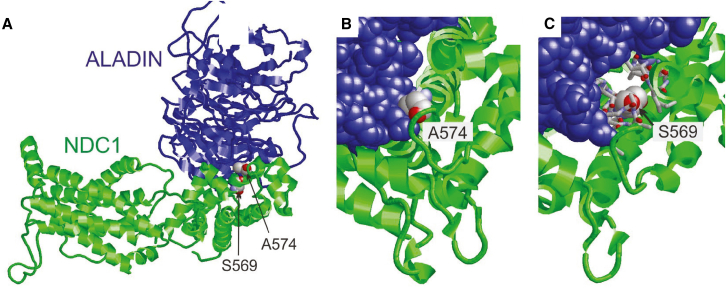
Pathogenic NDC1 variants affect interactions with ALADIN and NPC assembly
To verify the pathogenic effects of the missense variants identified in families 3 and 4, we modeled these variants into the in silico NDC1 protein structure. In addition, we modeled the interaction of NDC1 with ALADIN, NUP93, and NUP155 and evaluated the effects of the NDC1 variants on its interactors (Figure 3A). Interestingly, both missense variants p.Ser569Leu and p.Ala574Thr are located in the C-terminal domain of NDC1 that interacts with ALADIN (Figure S2).28,29,30 The p.Ala574 residue has been shown to directly interact with ALADIN. Replacement of the alanine residue with threonine is predicted to induce steric clashes with ALADIN, thereby decreasing heterodimer stability (Figure 3B). The p.Ser569 residue does not directly interact with ALADIN, but forms tight intramolecular interactions. Substitution with leucine is predicted to form steric clashes thereby decreasing NDC1 stability and consequently its ability to interact with ALADIN (Figure 3C). Overall, both variants are located in close proximity to the NDC1-ALADIN interface, suggesting that they have a negative effect on heterodimerization and anchoring of ALADIN in the NPC.
Figure 3.
Modeling structural effects of missense variants in NDC1
(A) View of the ALADIN-NDC1 heterodimers of the Xenopus laevis NPC. NDC1-ALADIN heterodimer showing that p.Ser569 and p.Ala574 are located close to the dimer interface. This panel is adapted from Huang et al.28
(B) Close-up of p.Ala574 showing that this residue forms direct contacts with the ALADIN subunit (shown in blue space-filled presentation). The bulkier substituted threonine side chain is predicted to cause steric clashes with ALADIN thereby decreasing heterodimer stability.
(C) Close-up of p.Ser569 showing that this residue forms tight intramolecular interactions (interacting residues shown in stick presentation). The bulkier substituted leucine side chain is anticipated to cause steric clashes thereby decreasing NDC1 stability and consequently its ability to interact with ALADIN. Overall, both variants are located in close proximity to the NDC1-ALADIN interface, suggesting that they have a negative effect on heterodimerization and on the anchoring of the NPC.
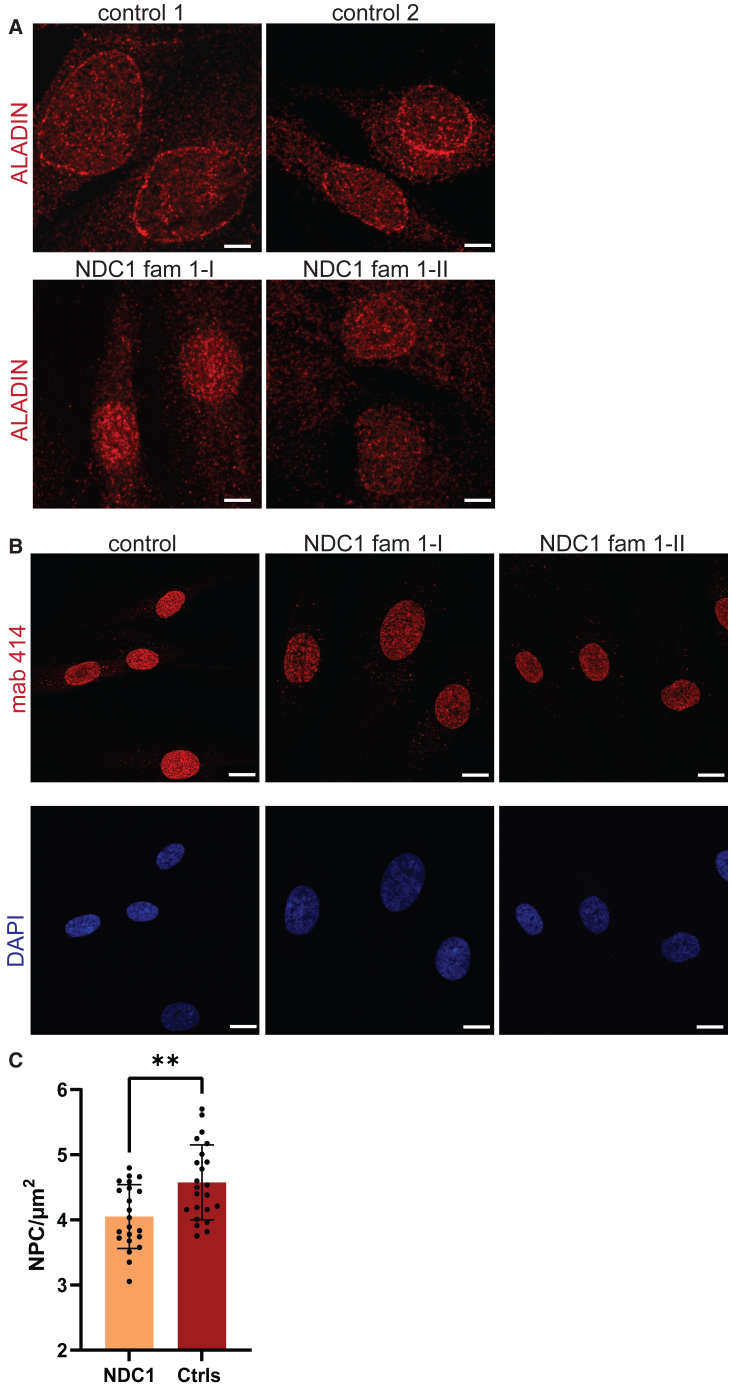
To investigate the effects of the p.Ala298_Lys328del variant on recruitment of ALADIN to the NPC, we assessed the localization of endogenous ALADIN in fibroblasts derived from affected individuals harboring this variant (individual 1-I + 1-II) by confocal microscopy and compared this with age-matched control fibroblast lines. Although, localization of ALADIN to the NE was observed in both control cell lines, fibroblasts containing the p.Ala298_Lys328del variant showed a decrease in ALADIN localization to the NE, indicative of recruitment defect (Figure 4A). These results support the pathogenicity of this variant as well as the importance of the NDC1 C terminus for ALADIN recruitment to the NE.
Figure 4.
NDC1 variants interfere with ALADIN recruitment and NPC insertion
(A) Cell lines were stained with anti-ALADIN antibodies (red) and its localization was evaluated with confocal microscopy. n = 2 independent experiments, >10 fields per cell line were evaluated, n = 2 NDC1 individuals; family 1-I and family 1-II.
(B) The number of NPCs was examined upon staining with the Mab-414 antibody (red). Nuclei were counterstained with DAPI. The structure of the NE and NPC localization were evaluated with confocal microscopy.
(C) Quantification of the number of NPCs in post mitotic cells (CDT1+) with 3D SIM microscopy after staining with the Mab-414 antibody (red). n = 3 experiments, n = 2 NDC1 individuals, n = 2 controls, two tailed unpaired t test, error bars represent the standard error of the mean (SEM)). ∗∗p < 0.01.
NDC1 is known to be essential for post-mitotic NE formation and the assembly of new NPCs.13 To evaluate the effects of our variants on NPC assembly and NE formation we labeled all NPCs with the mAb414 antibody, which recognizes FG-repeat-containing NPCs. The NDC1 p.Ala298_Lys328del variant did not have major effects on NE morphology and NPC distribution during interphase (Figure 4B). The number of NPCs was additionally quantified with 3DSIM high-resolution microscopy. As NPC assembly can occur post-mitotically and during interphase, we used the post–mitotic marker CDT1 to discriminate between these two processes. Comparison of NDC1 p.Ala298_Lys328del cell lines with three unrelated age-matched controls showed an overall decrease of CDT1-positive NPCs in the NDC1 p.Ala298_Lys328del cell lines (Figure 4C, mean NDC1 p.Ala298_Lys328del = 4.05 pore/μm2; mean controls = 4.58 pore/μm2, p < 0.002, two-tailed unpaired t test). These results suggest that the C-terminal NDC1 p.Ala298_Lys328del variant affects both ALADIN recruitment and post-mitotic NPC formation.
Discussion
This report provides evidence that biallelic NDC1 variants can cause a neurological phenotype similar to triple A syndrome. In our series, individuals with homozygous NDC1 variants present with variable alacrima, achalasia, mild developmental delay/intellectual disability, and peripheral (motor) polyneuropathy, but without endocrine anomalies. We show that the variant identified in families 1 and 2 interferes with the physiological function of NDC1 as it decreases the recruitment of ALADIN to the nuclear rim and impairs post-mitotic NPC insertion.
Triple A syndrome is characterized by the triad of esophageal achalasia, alacrima, and adrenal insufficiency and is associated with biallelic AAAS variants. The disease phenotype is variable, the complete triad is observed in 70% of affected individuals, and disease onset is often in first decade of life.15,31,32 Adrenal failure is common and may be life threatening, but individuals without adrenal failure have also been described.33,34 In addition, various neurological symptoms are reported. Upper and lower motor neuron lesions can cause bulbar symptoms, spasticity, intellectual disability, cognitive decline, and cranial neuropathy.31,35 Progressive peripheral neuropathy of motor and sensory nerves, often demyelinating with secondary axonal degeneration, is one of the hallmarks, but its presence has not been systematically investigated in all subjects with AAAS variants.31,35,36 In contrast to the individuals reported in this paper, nearly all triple A syndrome patients present with the pathognomonic sign of marked hyperreflexia without other signs of spasticity. Additional autonomic dysfunction is observed in 33% of affected individuals, and is characterized by postural hypotension, abnormal cardiovascular responses, anisocoria, abnormal pupillary reflexes, impotence, and alacrima. The name “4A-syndrome” has been introduced for the clinical variant with autonomic dysfunction.37
Interestingly, the individuals with biallelic NDC1 variants showed high phenotypic overlap with those having variants in AAAS (Table 2). The majority of the examined individuals with NDC1 variants presented with alacrima and symptoms of achalasia or dysphagia, recurrent vomiting or inability to swallow hard texture food. The formal diagnosis of achalasia was made in two of the individuals (individuals 3-1 + 3-II). Progression of milder dysphagia into achalasia during adolescence should be considered in younger cases, as this is frequently seen in individuals with AAAS variants.38 Notably, signs of adrenal insufficiency were not observed in any of the individuals with NDC1 variants, while endocrine disorders are observed in about 80% of individuals with triple A syndrome.36,39 However, this percentage could reflect an ascertainment bias due to the age of onset and initial symptomatology.
Table 2.
Comparison of the clinical features observed in individuals with NDC1 and AAAS variants
| Clinical manifestations | NDC1 | AAAS |
|---|---|---|
| Adrenal insufficiency | – | + |
| Neurological features | ||
| Dysphagia/achalasia | + | + |
| Clinical signs of polyneuropathy | + | +/− |
| Hypotonia | +/− | +/− |
| Hyporeflexia | + | – |
| Muscular atrophy | + | +/− |
| Hypertonia | +/− | + |
| Tongue fasciculations/atrophy | +/− | +/− |
| Epilepsy | +/− | +/− |
| Facial weakness | +/− | +/− |
| Developmental delay | + | + |
| Dysautonomia | ||
| Alacrima | + | + |
| Postural hypotension | – | +/− |
| Abnormal heart responses | +/− | +/− |
| Sexual dysfunction | – | +/− |
| Dermatological manifestations | ||
| Hyperpigmentation | – | +/− |
| Hyperkeratosis | +/− | +/− |
| Cutis anserine | – | +/− |
Compared with individuals reported with AAAS variants, individuals with NDC1 variants presented with prominent neurological symptoms; however, this could be biased given that AAAS variant cases are often ascertained based on the endocrinological problems. All NDC1 individuals had neurological features from early childhood, while the neurological symptoms in AAAS-related triple A syndrome usually occur at the end of the first, or the beginning of the second decade of life.14,15,18 Like in triple A syndrome, the neurological defects observed in NDC1 cases affect the central, peripheral, and autonomic nervous system. The most commonly observed features were hypotonia, developmental delay/intellectual disability, demyelinating motor neuropathy with secondary axonal injury, alacrima, and tongue fasciculations.14,18,39 Alacrima was frequent, but no other autonomic disturbances were observed in the NDC1 cohort except for limited heart rate variability in one individual. Peripheral nerve involvement is described in many individuals with triple A syndrome, and is predominantly characterized as a motor axonal neuropathy, which frequently affects the ulnar nerve.16,40,41
The transmembrane nucleoporin NDC1 anchors various cytoplasmic nucleoporins in the NE with its N-terminal and C-terminal protein tails.12,29 All variants identified in the affected individuals are located in the C-terminal tail of NDC1, which binds ALADIN and NUP155. The identified missense variants (p.Ser569Leu and p.Ala574Thr) are located in a region that interacts with ALADIN, explaining their deleterious effects. The c.892-21G>A variant results in the frame loss of exon 9 (p.Ala298_Lys328del) in about 60% of NDC1 transcript. This deletion includes a known ALADIN binding site (Figure S2) and results in reduced ALADIN localization to the NE. This is reminiscent of experimental NDC1 knockdown, which also causes reduced ALADIN NE localization and being consistent with a loss of function mechanism of the human variants.29,30 Similarly, pathogenic missense variants in AAAS result in aberrant ALADIN localization. Therefore, decreased recruitment of ALADIN to the NE has been advocated as the main mechanism underlying AAAS-related triple A syndrome.19,29,42
NDC1 also has a well-established role in post-mitotic NPC assembly and NE formation.43 Both the N-terminal and C-terminal tails of NDC1 are indispensable for NPC insertion.13 Fibroblasts containing the C-terminal p.Ala298_Lys328del variant showed a lower number of post-mitotically inserted NPCs. Interestingly, we did not observe major anomalies in the structure of the NE in these cell lines during interphase, as previously seen upon siNDC1.43 These data support the involvement of C-terminal NDC1 in NPC assembly and show that the p.Ala298_Lys328del variant interferes with established NDC1 functions. This variant probably does not induce major structural NE anomalies during interphase since it does not directly affect the NDC1 transmembrane domains. This will enable the integration of NDC1 into the NPC membrane and could as well allow the establishment of physiological protein interactions required for membrane deforming capacities.13
The consequences of impaired ALADIN recruitment to the NPC on cellular homeostasis are unknown. Several studies indicate that NDC1-mediated anchoring of ALADIN at the NPC is essential for selective nuclear import of DNA repair proteins (ligase 1; APRATAXIN) and ferritin heavy chain 1, a protein that protects against nuclear oxidative stress.44,45 Consequently, ALADIN-depleted cells have an altered response to oxidative stress and increased levels of reactive oxygen species.20,44,45 Moreover, roles for ALADIN unrelated to the NPC have been described. ALADIN assists in mitotic spindle formation by altering the localization of Aurora A,46 and it interacts with progesterone receptor membrane component 2, which regulates the activity of cytochrome P450.47 Moreover, a recent report focusing on adrenal glands showed a role for ALADIN in the nucleocytoplasmatic transport of cyclic AMP-dependent protein kinase and subsequent dysregulation of the steroidogenic pathway.48 The overlap in phenotypes caused by NDC1 and AAAS variants suggests that impaired recruitment of ALADIN to the NPC contributes to the clinical features shared among the two groups of affected individuals, e.g., alacrima, achalasia, and neurological defects. Possibly, functions of ALADIN unrelated to the NPC could be contributing to distinguishing features such as adrenal insufficiency.
Dysregulation of oxidative stress is one of the mechanisms that could contribute to the neurological features observed. While the pathophysiological mechanisms underlying the clinical features observed in triple A syndrome are not completely understood, oxidative stress is often causally related to peripheral neuropathy, and is implicated in several neurodegenerative and neurodevelopmental disorders.49,50 Previous studies have suggested that the triple A-related peripheral neuropathy might result from a defect of ACTH receptors on neurons or glia with secondary demyelination.17,36 However, our results, as well as several AAAS case descriptions, do not support this hypothesis as the subjects here reported did show demyelinating neuropathy without endocrine anomalies.
Although about 80% of individuals with triple A syndrome have an AAAS mutation, evidence for genetic heterogeneity has been reported for over two decades.35,38 A syndrome of alacrima, achalasia, and mental retardation (OMIM: 615510) has been linked to biallelic variants in the guanosine diphosphate-mannose pyrophosphorylase A (GMPPA) gene.51 The GMPPA protein inhibits guanosine diphosphate-mannose pyrophosphorylase B, which results in increased GDP-mannose levels and imbalanced glycosylation reactions.52 Moreover, variants in TRAPPC11 cause cerebral atrophy, intellectual disability and movement disorders, scoliosis, achalasia, and alacrima. The TRAPPC11 variants were also reported to influence protein glycosylation.53 Similar to individuals with pathogenic NDC1 variants, the distinguishing feature of the disorder related to these variants is the absence of adrenocortical dysfunction. Interestingly, the consequences of the variants in GMPPA and TRAPPC11 seem to be unrelated to the NPC structure, which suggests that the molecular mechanism causing the features observed in triple A-related disease are not only directly related to the NPC, but also to secondary defects, for example, alterations in selective nuclear trafficking.
Our observation shows that NDC1 variants should be considered in individuals with alacrima, achalasia, and neurological defects, mostly severe peripheral neuropathy. The variants identified here in the affected individuals all seem to have an effect on the interaction with ALADIN, explaining the high phenotypic overlap with AAAS-related triple A syndrome. The future description and evaluation of additional individuals with NDC1 variants is essential to better define the associated phenotype and gain more insight into the underlying disease mechanisms.
Statistics
Statistical analysis was performed using GraphPad Prism v.9.0. All datasets were checked for normality and outliers. All error bars represent the standard error of the mean. Details about the statistical tests are available in the figure legends.
Data and code availability
The WES and RNA sequencing data supporting the current study have not been deposited in a public repository out of respect for the patients' privacy, but data are available from the corresponding author on request.
Acknowledgments
We thank all patients and their caregivers for participation in this study. We thank the optical imaging center in the Erasmus University Medical Center for assistance with confocal microscopy and high-resolution microscopy. G.M.S.M. and D.J.S. are supported by ZonMw Top grant no. 91217045. K.K. and A.H. are supported by the Deutsche Forschungsgemeinschaft (DFG) (314061271-TRR/CRC 205).
Author contributions
Conceptualization: D.J.S., J.D.; R.S., G.M.S.M.; Methodology; D.J.S., J.D., R.S., G.M.S.M.; Formal analysis and investigation: D.J.S., J.D., H.D., R.S.; Resources: H.D., H.M., S.B., K.K., A.H., M.S., S.V., A.T., M.J., E.T., M.A.S., E.G.M.H., T.J.H., M.C.K.; Writing – original draft preparation: D.J.S., J.D., G.M.S.M.; Writing review and editing: H.D., R.S., H.M., S.B., K.K., A.H., M.S., S.V., A.T., M.J., E.T., M.A.S., E.G.M.H., T.J.H., M.C.K.. Supervision: G.M.S.M.
Declaration of interests
The authors declare no competing interests.
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.xhgg.2024.100327.
Web resources
OMIM: https://www.omim.org/
Genome Analysis Toolkit (GATK): http://www.broadinstitute.org/gatk/
Burrows-Wheeler Aligner: http://bio-bwa.sourceforge.net/
AlphaFold: https://alphafold.ebi.ac.uk/
GeneMatcher: https://genematcher.org/statistics/
Web browser application for RNA-seq analysis: https://github.com/KlinGenErasmusMC/rnaseq-voila
Supplemental information
References
- 1.Hampoelz B., Andres-Pons A., Kastritis P., Beck M. Structure and Assembly of the Nuclear Pore Complex. Annu. Rev. Biophys. 2019;48:515–536. doi: 10.1146/annurev-biophys-052118-115308. [DOI] [PubMed] [Google Scholar]
- 2.Sloan K.E., Gleizes P.E., Bohnsack M.T. Nucleocytoplasmic Transport of RNAs and RNA-Protein Complexes. J. Mol. Biol. 2016;428:2040–2059. doi: 10.1016/j.jmb.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 3.Ibarra A., Hetzer M.W. Nuclear pore proteins and the control of genome functions. Genes Dev. 2015;29:337–349. doi: 10.1101/gad.256495.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muir A.M., Cohen J.L., Sheppard S.E., Guttipatti P., Lo T.Y., Weed N., Doherty D., DeMarzo D., Fagerberg C.R., Kjærsgaard L., et al. Bi-allelic Loss-of-Function Variants in NUP188 Cause a Recognizable Syndrome Characterized by Neurologic, Ocular, and Cardiac Abnormalities. Am. J. Hum. Genet. 2020;106:623–631. doi: 10.1016/j.ajhg.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braun D.A., Lovric S., Schapiro D., Schneider R., Marquez J., Asif M., Hussain M.S., Daga A., Widmeier E., Rao J., et al. Mutations in multiple components of the nuclear pore complex cause nephrotic syndrome. J. Clin. Invest. 2018;128:4313–4328. doi: 10.1172/JCI98688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fichtman B., Harel T., Biran N., Zagairy F., Applegate C.D., Salzberg Y., Gilboa T., Salah S., Shaag A., Simanovsky N., et al. Pathogenic Variants in NUP214 Cause "Plugged" Nuclear Pore Channels and Acute Febrile Encephalopathy. Am. J. Hum. Genet. 2019;105:48–64. doi: 10.1016/j.ajhg.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bindra D., Mishra R.K. In Pursuit of Distinctiveness: Transmembrane Nucleoporins and Their Disease Associations. Front. Oncol. 2021;11 doi: 10.3389/fonc.2021.784319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang X.Y., Wang L., Liu Z.Y., Song W.X., Zhou M., Xi L. TMEM48 promotes cell proliferation and invasion in cervical cancer via activation of the Wnt/β-catenin pathway. J. Recept. Signal Transduct. Res. 2021;41:371–377. doi: 10.1080/10799893.2020.1813761. [DOI] [PubMed] [Google Scholar]
- 9.Guan L., Zhang L., Wang T., Jia L., Zhang N., Yan H., Zhao K. POM121 promotes proliferation and metastasis in non-small-cell lung cancer through TGF-β/SMAD and PI3K/AKT pathways. Cancer Biomark. 2021;32:293–302. doi: 10.3233/CBM-210001. [DOI] [PubMed] [Google Scholar]
- 10.Tarazon E., Rivera M., Rosello-Lleti E., Molina-Navarro M.M., Sánchez-Lázaro I.J., España F., Montero J.A., Lago F., González-Juanatey J.R., Portolés M. Heart failure induces significant changes in nuclear pore complex of human cardiomyocytes. PLoS One. 2012;7 doi: 10.1371/journal.pone.0048957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akiyama K., Noguchi J., Hirose M., Kajita S., Katayama K., Khalaj M., Tsuji T., Fairfield H., Byers C., Reinholdt L., et al. A mutation in the nuclear pore complex gene Tmem48 causes gametogenesis defects in skeletal fusions with sterility (sks) mice. J. Biol. Chem. 2013;288:31830–31841. doi: 10.1074/jbc.M113.492306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stavru F., Hulsmann B.B., Spang A., Hartmann E., Cordes V.C., Gorlich D. NDC1: a crucial membrane-integral nucleoporin of metazoan nuclear pore complexes. J. Cell Biol. 2006;173:509–519. doi: 10.1083/jcb.200601001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eisenhardt N., Redolfi J., Antonin W. Interaction of Nup53 with Ndc1 and Nup155 is required for nuclear pore complex assembly. J. Cell Sci. 2014;127:908–921. doi: 10.1242/jcs.141739. [DOI] [PubMed] [Google Scholar]
- 14.Dixit A., Chow G., Sarkar A. Neurologic presentation of triple A syndrome. Pediatr. Neurol. 2011;45:347–349. doi: 10.1016/j.pediatrneurol.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Flokas M.E., Tomani M., Agdere L., Brown B. Triple A syndrome (Allgrove syndrome): improving outcomes with a multidisciplinary approach. Pediatric Health Med. Ther. 2019;10:99–106. doi: 10.2147/PHMT.S173081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koehler K., Brockmann K., Krumbholz M., Kind B., Bönnemann C., Gärtner J., Huebner A. Axonal neuropathy with unusual pattern of amyotrophy and alacrima associated with a novel AAAS mutation p.Leu430Phe. Eur. J. Hum. Genet. 2008;16:1499–1506. doi: 10.1038/ejhg.2008.132. [DOI] [PubMed] [Google Scholar]
- 17.Stuckey B.G., Mastaglia F.L., Reed W.D., Pullan P.T. Glucocorticoid insufficiency, achalasia, alacrima with autonomic motor neuropathy. Ann. Intern. Med. 1987;106:61–63. doi: 10.7326/0003-4819-106-1-62. [DOI] [PubMed] [Google Scholar]
- 18.Vallet A.E., Verschueren A., Petiot P., Vandenberghe N., Nicolino M., Roman S., Pouget J., Vial C. Neurological features in adult Triple-A (Allgrove) syndrome. J. Neurol. 2012;259:39–46. doi: 10.1007/s00415-011-6115-9. [DOI] [PubMed] [Google Scholar]
- 19.Cronshaw J.M., Matunis M.J. The nuclear pore complex protein ALADIN is mislocalized in triple A syndrome. Proc. Natl. Acad. Sci. USA. 2003;100:5823–5827. doi: 10.1073/pnas.1031047100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kind B., Koehler K., Krumbholz M., Landgraf D., Huebner A. Intracellular ROS level is increased in fibroblasts of triple A syndrome patients. J. Mol. Med. 2010;88:1233–1242. doi: 10.1007/s00109-010-0661-y. [DOI] [PubMed] [Google Scholar]
- 21.Krumbholz M., Koehler K., Huebner A. Cellular localization of 17 natural mutant variants of ALADIN protein in triple A syndrome - shedding light on an unexpected splice mutation. Biochem. Cell. Biol. 2006;84:243–249. doi: 10.1139/o05-198. [DOI] [PubMed] [Google Scholar]
- 22.Sobreira N., Schiettecatte F., Valle D., Hamosh A. GeneMatcher: a matching tool for connecting investigators with an interest in the same gene. Hum. Mutat. 2015;36:928–930. doi: 10.1002/humu.22844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dekker J., Schot R., Bongaerts M., de Valk W.G., van Veghel-Plandsoen M.M., Monfils K., Douben H., Elfferich P., Kasteleijn E., van Unen L.M.A., et al. Web-accessible application for identifying pathogenic transcripts with RNA-seq: Increased sensitivity in diagnosis of neurodevelopmental disorders. Am. J. Hum. Genet. 2023;110:251–272. doi: 10.1016/j.ajhg.2022.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adzhubei I.A., Schmidt S., Peshkin L., Ramensky V.E., Gerasimova A., Bork P., Kondrashov A.S., Sunyaev S.R. A method and server for predicting damaging missense mutations. Nat. Methods. 2010;7:248–249. doi: 10.1038/nmeth0410-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bryen S.J., Yuen M., Joshi H., Dawes R., Zhang K., Lu J.K., Jones K.J., Liang C., Wong W.K., Peduto A.J., et al. Prevalence, parameters, and pathogenic mechanisms for splice-altering acceptor variants that disrupt the AG exclusion zone. HGG Adv. 2022;3 doi: 10.1016/j.xhgg.2022.100125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rentzsch P., Schubach M., Shendure J., Kircher M. CADD-Splice-improving genome-wide variant effect prediction using deep learning-derived splice scores. Genome Med. 2021;13:31. doi: 10.1186/s13073-021-00835-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karczewski K.J., Francioli L.C., Tiao G., Cummings B.B., Alföldi J., Wang Q., Collins R.L., Laricchia K.M., Ganna A., Birnbaum D.P., et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–443. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang G., Zhan X., Zeng C., Zhu X., Liang K., Zhao Y., Wang P., Wang Q., Zhou Q., Tao Q., et al. Cryo-EM structure of the nuclear ring from Xenopus laevis nuclear pore complex. Cell Res. 2022;32:349–358. doi: 10.1038/s41422-021-00610-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kind B., Koehler K., Lorenz M., Huebner A. The nuclear pore complex protein ALADIN is anchored via NDC1 but not via POM121 and GP210 in the nuclear envelope. Biochem. Biophys. Res. Commun. 2009;390:205–210. doi: 10.1016/j.bbrc.2009.09.080. [DOI] [PubMed] [Google Scholar]
- 30.Yamazumi Y., Kamiya A., Nishida A., Nishihara A., Iemura S.I., Natsume T., Akiyama T. The transmembrane nucleoporin NDC1 is required for targeting of ALADIN to nuclear pore complexes. Biochem. Biophys. Res. Commun. 2009;389:100–104. doi: 10.1016/j.bbrc.2009.08.096. [DOI] [PubMed] [Google Scholar]
- 31.Houlden H., Smith S., De Carvalho M., Blake J., Mathias C., Wood N.W., Reilly M.M. Clinical and genetic characterization of families with triple A (Allgrove) syndrome. Brain. 2002;125:2681–2690. doi: 10.1093/brain/awf270. [DOI] [PubMed] [Google Scholar]
- 32.Patt H., Koehler K., Lodha S., Jadhav S., Yerawar C., Huebner A., Thakkar K., Arya S., Nair S., Goroshi M., et al. Phenotype-genotype spectrum of AAA syndrome from Western India and systematic review of literature. Endocr. Connect. 2017;6:901–913. doi: 10.1530/EC-17-0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luigetti M., Pizzuti A., Bartoletti S., Houlden H., Pirro C., Bottillo I., Madia F., Conte A., Tonali P.A., Sabatelli M. Triple A syndrome: a novel compound heterozygous mutation in the AAAS gene in an Italian patient without adrenal insufficiency. J. Neurol. Sci. 2010;290:150–152. doi: 10.1016/j.jns.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Rivera-Suazo Y., Espriu-Ramirez M.X., Trauernicht-Mendieta S.A., Rodriguez L. Allgrove syndrome in a toddler: Alacrima and achalasia, with no adrenal insufficiency. Rev. Gastroenterol. Mex. (Engl Ed) 2020;86:441–443. doi: 10.1016/j.rgmx.2020.09.003. S0375--0906. [DOI] [PubMed] [Google Scholar]
- 35.Weiman D.I., Gillespie M.K., Hartley T., Osmond M., Ito Y., Care4Rare Canada Consortium. Boycott K.M., Kernohan K.D., Lines M., McMillan H.J. Neurophysiological Characteristics of Allgrove (Triple A) Syndrome: Case Report and Literature Review. Child Neurol. Open. 2021;8 doi: 10.1177/2329048X211031059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kimber J., McLean B.N., Prevett M., Hammans S.R. Allgrove or 4 "A" syndrome: an autosomal recessive syndrome causing multisystem neurological disease. J. Neurol. Neurosurg. Psychiatry. 2003;74:654–657. doi: 10.1136/jnnp.74.5.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gazarian M., Cowell C.T., Bonney M., Grigor W.G. The "4A" syndrome: adrenocortical insufficiency associated with achalasia, alacrima, autonomic and other neurological abnormalities. Eur. J. Pediatr. 1995;154:18–23. doi: 10.1007/BF01972967. [DOI] [PubMed] [Google Scholar]
- 38.Tibussek D., Ghosh S., Huebner A., Schaper J., Mayatepek E., Koehler K. "Crying without tears" as an early diagnostic sign-post of triple A (Allgrove) syndrome: two case reports. BMC Pediatr. 2018;18:6. doi: 10.1186/s12887-017-0973-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roucher-Boulez F., Brac de la Perriere A., Jacquez A., Chau D., Guignat L., Vial C., Morel Y., Nicolino M., Raverot G., Pugeat M. Triple-A syndrome: a wide spectrum of adrenal dysfunction. Eur. J. Endocrinol. 2018;178:199–207. doi: 10.1530/EJE-17-0642. [DOI] [PubMed] [Google Scholar]
- 40.Dumic M., Barisic N., Rojnic-Putarek N., Kušec V., Stanimirović A., Koehler K., Huebner A. Two siblings with triple A syndrome and novel mutation presenting as hereditary polyneuropathy. Eur. J. Pediatr. 2011;170:393–396. doi: 10.1007/s00431-010-1314-4. [DOI] [PubMed] [Google Scholar]
- 41.Frasquet M., Rojas-Garcia R., Argente-Escrig H., Vázquez-Costa J.F., Muelas N., Vílchez J.J., Sivera R., Millet E., Barreiro M., Díaz-Manera J., et al. Distal hereditary motor neuropathies: Mutation spectrum and genotype-phenotype correlation. Eur. J. Neurol. 2021;28:1334–1343. doi: 10.1111/ene.14700. [DOI] [PubMed] [Google Scholar]
- 42.Cho A.R., Yang K.J., Bae Y., Bahk Y.Y., Kim E., Lee H., Kim J.K., Park W., Rhim H., Choi S.Y., et al. Tissue-specific expression and subcellular localization of ALADIN, the absence of which causes human triple A syndrome. Exp. Mol. Med. 2009;41:381–386. doi: 10.3858/emm.2009.41.6.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mansfeld J., Guttinger S., Hawryluk-Gara L.A., Panté N., Mall M., Galy V., Haselmann U., Mühlhäusser P., Wozniak R.W., Mattaj I.W., et al. The conserved transmembrane nucleoporin NDC1 is required for nuclear pore complex assembly in vertebrate cells. Mol. Cell. 2006;22:93–103. doi: 10.1016/j.molcel.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 44.Storr H.L., Kind B., Parfitt D.A., Chapple J.P., Lorenz M., Koehler K., Huebner A., Clark A.J.L. Deficiency of ferritin heavy-chain nuclear import in triple a syndrome implies nuclear oxidative damage as the primary disease mechanism. Mol. Endocrinol. 2009;23:2086–2094. doi: 10.1210/me.2009-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Juhlen R., Idkowiak J., Taylor A.E., Kind B., Arlt W., Huebner A., Koehler K. Role of ALADIN in human adrenocortical cells for oxidative stress response and steroidogenesis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0124582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carvalhal S., Ribeiro S.A., Arocena M., Kasciukovic T., Temme A., Koehler K., Huebner A., Griffis E.R. The nucleoporin ALADIN regulates Aurora A localization to ensure robust mitotic spindle formation. Mol. Biol. Cell. 2015;26:3424–3438. doi: 10.1091/mbc.E15-02-0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Juhlen R., Landgraf D., Huebner A., Koehler K. Identification of a novel putative interaction partner of the nucleoporin ALADIN. Biol. Open. 2016;5:1697–1705. doi: 10.1242/bio.021162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bitetto G., Lopez G., Ronchi D., Pittaro A., Melzi V., Peverelli E., Cribiù F.M., Comi G.P., Mantovani G., Di Fonzo A. SCARB1 downregulation in adrenal insufficiency with Allgrove syndrome. Orphanet J. Rare Dis. 2023;18:152. doi: 10.1186/s13023-023-02763-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mallet M.L., Hadjivassiliou M., Sarrigiannis P.G., Zis P. The Role of Oxidative Stress in Peripheral Neuropathy. J. Mol. Neurosci. 2020;70:1009–1017. doi: 10.1007/s12031-020-01495-x. [DOI] [PubMed] [Google Scholar]
- 50.Nishimura Y., Kanda Y., Sone H., Aoyama H. Oxidative Stress as a Common Key Event in Developmental Neurotoxicity. Oxid. Med. Cell. Longev. 2021;2021 doi: 10.1155/2021/6685204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Koehler K., Malik M., Mahmood S., Gießelmann S., Beetz C., Hennings J.C., Huebner A.K., Grahn A., Reunert J., Nürnberg G., et al. Mutations in GMPPA cause a glycosylation disorder characterized by intellectual disability and autonomic dysfunction. Am. J. Hum. Genet. 2013;93:727–734. doi: 10.1016/j.ajhg.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Franzka P., Henze H., Jung M.J., Schüler S.C., Mittag S., Biskup K., Liebmann L., Kentache T., Morales J., Martínez B., et al. GMPPA defects cause a neuromuscular disorder with alpha-dystroglycan hyperglycosylation. J. Clin. Invest. 2021;131 doi: 10.1172/JCI139076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Koehler K., Milev M.P., Prematilake K., Reschke F., Kutzner S., Jühlen R., Landgraf D., Utine E., Hazan F., Diniz G., et al. A novel TRAPPC11 mutation in two Turkish families associated with cerebral atrophy, global retardation, scoliosis, achalasia and alacrima. J. Med. Genet. 2017;54:176–185. doi: 10.1136/jmedgenet-2016-104108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The WES and RNA sequencing data supporting the current study have not been deposited in a public repository out of respect for the patients' privacy, but data are available from the corresponding author on request.