Abstract
Metastatic lateral pelvic lymph nodes (LPNs) in rectal cancer significantly impact the prognosis and treatment strategies. Western practices emphasize neoadjuvant chemoradiotherapy (CRT), whereas Eastern approaches often rely on LPN dissection (LPND). This review examines the evolving role of LPND in the context of modern treatments, including total neoadjuvant therapy (TNT), and the impact of CRT on the management of clinically suspicious LPNs. We comprehensively reviewed the key literature comparing the outcomes of LPND versus preoperative CRT for rectal cancer, focusing on recent advancements and ongoing debates. Key studies, including the JCOG0212 trial and recent multicenter trials, were analyzed to assess the efficacy of LPND, particularly in conjunction with preoperative CRT or TNT. Current evidence indicates that LPND can reduce local recurrence rates compared to total mesorectal excision alone in patients not receiving radiation therapy. However, the benefit of LPND in the context of neoadjuvant CRT is influenced by the size and pretreatment characteristics of LPNs. While CRT can effectively control smaller metastatic LPNs, larger or clinically suspicious LPNs may require LPND for optimal outcomes. Advances in surgical techniques, such as robotic-assisted LPND, offer potential benefits but also present challenges and complications. The role of TNT in controlling metastatic LPNs and improving patient outcomes is emerging but remains underexplored. The decision to perform LPND should be individualized based on patient-specific factors, including LPN size, response to neoadjuvant treatment, and surgeon expertise. Future research should focus on optimizing treatment protocols and further evaluating the role of TNT in managing metastatic LPNs.
Keywords: Lateral pelvic node dissection, Rectal neoplasms, Chemoradiation, Total neoadjuvant therapy, Local recurrence
INTRODUCTION
Lymph node (LN) metastasis is recognized as a critical prognostic factor in the treatment of colorectal cancer. Most surgical procedures aim to remove regional LNs along with the tumor. In rectal cancer, lymphatic spread primarily follows an "upward" route along the superior rectal artery and inferior mesenteric artery. However, a century ago, it was observed that there is also a "lateral spread" to the lateral pelvic wall via lymphatic channels along the midrectal vessels, particularly in advanced lower rectal cancer [1]. This phenomenon has been well-documented by both Japanese and Western surgeons [2].
Treatment strategies for lateral pelvic LNs (LPNs) have diverged, with the West adopting neoadjuvant chemoradiotherapy (CRT) and the East, particularly Japan, preferring surgical resection without CRT. According to the JCOG0212 trial, in cases of nonradiated lower rectal cancer where LPNs are either invisible or smaller than 1 cm, combined LPN dissection (LPND) revealed microscopic LPN involvement in 7.4% of cases [3]. This approach reduced local (pelvic sidewall) recurrence to 7.4%, compared to 12.6% in the group that underwent total mesorectal excision (TME) alone. These findings suggest that prophylactic LPND may be unnecessary in over 90% of these patients.
Conversely, on the other side of the world, a pooled analysis comparing TME alone to TME with additional LPND following neoadjuvant CRT demonstrated improved oncologic outcomes in the LPND group [4]. This was particularly evident in patients who had enlarged LPNs (≥7 mm) identified on pretreatment pelvic magnetic resonance imaging (MRI). These findings suggest that CCRT alone may not eradicate all microscopic LPN metastases, thereby supporting the inclusion of LPND in patients with suspicious LPNs even after CRT.
Recently, there has been a growing recognition in both Eastern and Western medical practices that LPND without CRT might result in overtreatment, while CRT alone may not always effectively eliminate all metastatic LNs. However, skepticism and reluctance to perform LPND persist among surgeons who are not familiar with this complex procedure. To address these concerns, it is essential to standardize LPND techniques based on surgical anatomy, particularly in the context of minimally invasive surgery, and to minimize potential complications during the learning phase.
Recent advancements, such as total neoadjuvant treatment (TNT), have been widely adopted for advanced rectal cancer. This approach aims to promote tumor regression, including metastatic LPNs, and improve disease-free survival (DFS). Additionally, surgical skills have improved due to a better understanding of pelvic anatomy and the adoption of more Intuitive Surgical platforms, such as robotics.
Despite these developments, debate continues regarding the indications, extent, and clinical benefits of LPND. This review examines the current management strategies for suspicious LPNs and the outcomes associated with different approaches.
ROUTE OF LPN SPREAD AND ESSENTIAL ANATOMY
Lateral lymphatic spread from the rectum primarily occurs through lymphatic channels along the midrectal vessels and some distal branches of the internal iliac vessels. The lymphatic flow then ascends along the branches and trunk of the internal iliac artery, eventually converging with lymphatics along the obturator vessels. This network further extends to connect with upstream lymphatics along the common iliac vessels and paraaortic channels.
Consequently, the most common sites for metastatic spread are around the distal branches of the internal iliac artery, followed by the proximal branches [5]. The obturator node group is the 2nd most common site for metastasis. As the spread moves further upstream, the frequency of metastasis decreases, and LN metastasis along the external iliac vessels becomes rare unless the lymphatic spread involves the inguinal nodes from very low-lying rectal cancers [5, 6]. The Japanese guidelines clearly define these LN groups, as illustrated in Fig. 1 [7]. Important vessels, nerves, and other structures are depicted in Fig. 2.
Fig. 1.
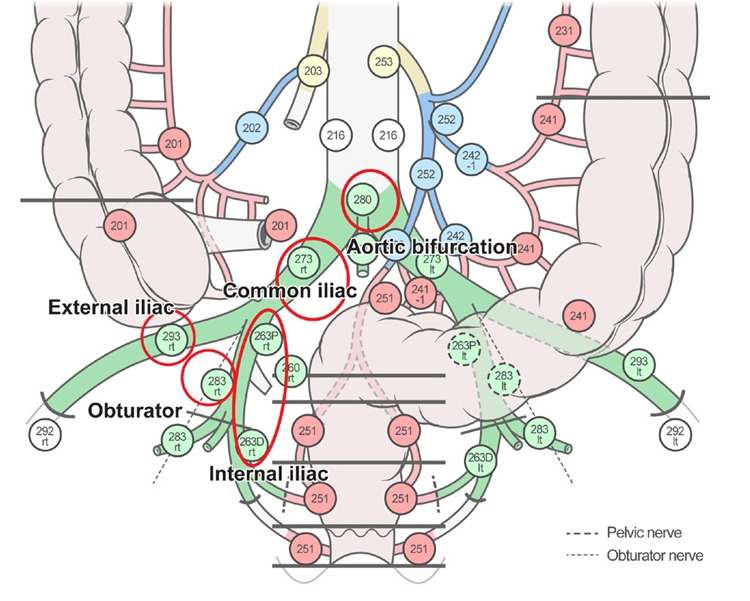
Schematic diagram of groups of lateral pelvic lymph nodes.
Fig. 2.
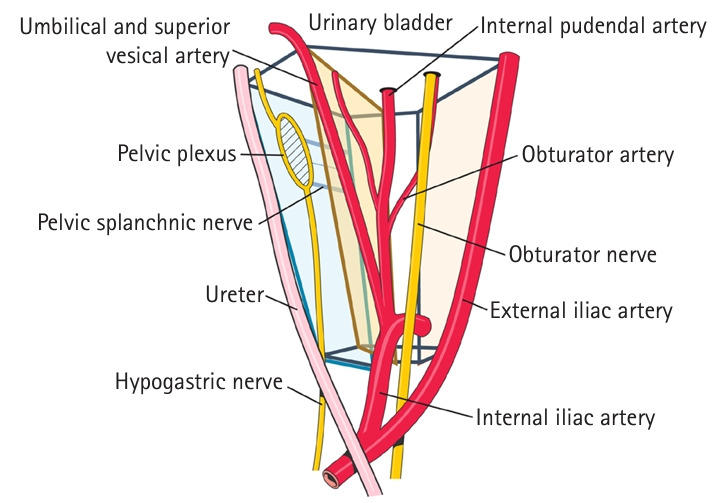
Fascial anatomy of pelvic side wall.
Although the semiconical anatomy of the lateral pelvic sidewall may appear complex, it has recently been more precisely defined through the identification of several key fascial planes (Fig. 2) [8]. The lateral plane of the pelvic sidewall comprises the external iliac vessels, the psoas muscle, and the obturator internus muscle. The most medial plane, referred to as the uretero-hypogastric nerve fascia, houses the ureter and the pelvic splanchnic nerves, which originate from sacral nerves 2–4. In surgical procedures, LPND involves the removal of all lymphoareolar tissues situated between these 2 planes.
The intermediate or middle plane, delineated by the vesico-hypogastric fascia, features the internal iliac artery and its branches, such as the superior and inferior vesical arteries and the internal pudendal artery. This plane demarcates the internal iliac LN group medially and the obturator LN group laterally.
At the bottom of the pelvic sidewall, the lumbosacral trunk and part of the pelvic floor muscles are located, while the roof is formed by the wall of the urinary bladder. Within the center of the obturator LN space, the obturator nerve and vessels pass through.
DIAGNOSIS AND PREVALENCE OF LPN METASTASIS
The natural prevalence of metastatic LPNs can only be estimated from Japanese studies, as preoperative CCRT is rarely used in Japan, where LPND is routinely performed. Within these studies, the prevalence varies widely, ranging from 13.8% to 36.8% (Table 1) [5, 9–20]. This variability is likely due to differences in patient characteristics such as tumor height, depth, and sex. The variability becomes even more pronounced when considering neoadjuvant treatments (Table 1) [21–32]. Currently, high-resolution pelvic MRI is the most commonly used method to achieve reliable results. Considerable efforts have been made to accurately distinguish metastatic LPNs from benign ones using criteria such as size, shape, configuration, signal characteristics, and fluorodeoxyglucose (FDG) uptake in positron emission tomography–computed tomography scans. Positive LNs are typically larger, round, or speculated in shape, exhibit mixed signals [33], and show increased FDG uptake [34]. However, identifying definitive features of metastatic LPNs remains challenging with a single classification system. Size criteria, particularly the maximum short-axis diameter (MSAD), have become widely accepted as reliable indicators for diagnosing metastatic LPNs. MRI evaluations of normal individuals indicate that an MSAD up to 4 mm is considered normal for common iliac and obturator nodes, while up to 5 mm is normal for internal and external iliac nodes [35]. The JCOG0212 study demonstrated positive rates for LPNs with MSAD ranging from 0 to 10 mm as follows: 7.4% for 0 to 10 mm, 5.2% for 0 to 5 mm, and 21.4% for 5 to 10 mm [36]. Additionally, Ogawa et al. [15] reported that a 5-mm cutoff showed a high area under the curve, with accuracy, sensitivity, and specificity values of 63.7%, 72.6%, and 54.7%, respectively.
Table 1.
Criteria and prevalence of LPN metastasis
| Study | Country | No. of patients | No. of CRT patients | Criteria of LPN metastasis | Pathologic positive rate (%) | |
|---|---|---|---|---|---|---|
| Fujita et al. [13] (2009) | Japan | 210 | 6 | >5 mm | 22.4 | |
| Ogawa et al. [15] (2016) | Japan | 272 | - | ≥5 mm in the SA | 17.0 | |
| Yamaoka et al. [16] (2017) | Japan | 19 | - | ≥5 mm in the SA | 36.8 | |
| Matsuda et al. [17] (2018) | Japan | 45 | - | ≥8 mm in the SA | 21.9 | |
| Dev et al. [18] (2018) | India | 43 | - | ≥8 mm in the SA | 20.9 | |
| Iwasa et al. [19] (2021) | Japan | 69 | - | >7 mm in the SA | 15.7 | |
| Abe et al. [20] (2022) | Japan | 67 | 7 | ≥5 mm in the SA | 26.9 | |
| Oh et al. [22] (2014) | Korea | 66 | 66 | >5 mm in the SA | 33.3 | |
| Akiyoshi et al. [23] (2015) | Japan | 77 | 77 | ≥7 mm in the LA | 40.3 | |
| Sinukumar et al. [24] (2015) | Japan | 8 | 8 | ≥8 mm in the SA | 25.0 | |
| Shin et al. [25] (2016) | USA | 18 | 18 | ≥7 mm in the LA | 61.1 | |
| Ishihara et al. [26] (2017) | Japan | 31 | 31 | ≥8 mm in the SA | 51.6 | |
| Kim et al. [27] (2017) | Korea | 53 | 53 | ≥5 mm in the SA | 37.7 | |
| Kim et al. [28] (2018) | Korea | 57 | 57 | ≥5 mm in the SA | 40.4 | |
| Hiyoshi et al. [29] (2020) | Japan | 78 | 26 | >5 mm | 11.5 | |
| Kawai et al. [30] (2021) | Japan | 42 | 42 | >8 mm | 52.4 | |
| Song et al. [31] (2021) | Korea | 99 | 99 | ≥5 mm in the SA | 30.3 | |
| Agger et al. [32] (2021) | Sweden | 344 | 309 | <5 mm in the SA with 3 malignant featuresa or 5–9 mm in the SA with 2 malignant featuresa | 8.7 |
LPN, lateral pelvic lymph node; CRT, chemoradiotherapy; SA, short axis; LA, long axis.
Malignant features of lymph nodes were defined as indistinct borders, heterogeneous signal, or attenuation and round shape.
In the context of CCRT, an analysis suggested that a pretreatment lateral LN size of ≥8 mm could serve as the optimal criterion for LPND, achieving sensitivity and specificity values of 92.3% and 78.7%, respectively [30]. This criterion could potentially spare 72.0% of patients from unnecessary lateral LN dissection. Malakorn et al. [37] discovered that all posttreatment LPNs smaller than 5 mm were negative, suggesting that such nodes might not require dissection. However, Kim et al. [27] proposed that the size of LPNs before treatment might be a more accurate predictor for LPND. Specifically, using a 5-mm cutoff for pretreatment LPNs, the positive rate was 16.7% among good responders (posttreatment LPN, <5 mm) and 62.5% among nonresponders (persistent posttreatment LPN, >5 mm). Similarly, Oh et al. [22] reported that among 66 irradiated cases of LPNs larger than 5 mm on pretreatment MRI, 22 (33.3%) were pathologically confirmed as positive.
Taken together, advanced lower rectal cancer, characterized by LNs larger than 5 to 8 mm (with or without neoadjuvant CRT), may necessitate LPND. These larger LNs are associated with an increased rate of metastasis, but they also pose a greater risk of undertreatment. Conversely, smaller LNs are associated with a lower rate of metastasis but carry a higher risk of overtreatment. Therefore, the decision to proceed with LPND should be carefully considered, taking into account the surgeon's expertise and the potential rate of complications.
LPN: REGIONAL OR SYSTEMIC?
Despite the anatomical proximity of LPNs to the primary tumor, some surgeons consider LPN metastasis to be systemic rather than regional due to the poor survival outcomes following resection [38]. This classification issue continues to be a point of contention in LPND. The TNM staging system in the American Joint Committee on Cancer (AJCC) Cancer Staging Manual, 8th edition, classifies internal iliac nodes as regional and obturator nodes as metastatic [39]. Consequently, many Western doctors regard obturator nodes as outside the regional chain. However, a Japanese multi-institutional study by Akiyoshi et al. [14] challenged this perspective. They classified internal iliac nodes as regional and pelvic sidewall nodes as external LPNs (Ext-LPNs). Their research on nonradiated patients showed that survival rates for internal iliac metastasis were comparable to those in the N2a category, while Ext-LPNs were similar to the N2b category, suggesting that both types of LPNs might be considered regional. The subsequent study by Akiyoshi et al. [40] revealed that patients with metastatic LPNs had survival rates that fell between those of ypN0 and ypN2 rectal cancer, indicating that LPN metastasis behaves more like a locoregional disease rather than a systemic one. Kim et al. [41] supported this finding by demonstrating that even irradiated patients with LPN metastasis had outcomes similar to those with mesorectal node metastasis. Specifically, metastasis in internal iliac LPNs was comparable to perirectal node metastasis, while Ext-LPN metastasis was akin to intermediate LN metastasis. These findings suggest that LPN metastasis can be considered locoregional, particularly with the modern standard of preoperative CRT plus TME and radical LPND (Fig. 3).
Fig. 3.
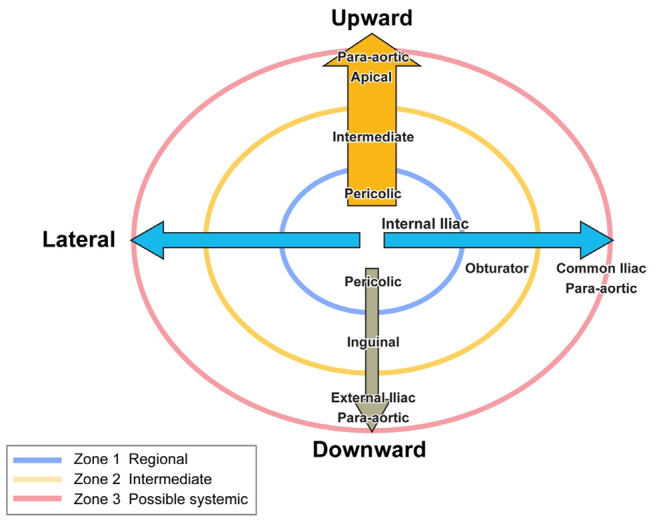
Possible classifications of lymph nodes spread according to survival.
Overall, these studies support the classification of LPN metastasis as locoregional, necessitating appropriate treatment that influences both staging and therapeutic approaches. However, the impact of LPND on local recurrence (LR) and overall survival (OS) remains unclear, especially in the context of preoperative CRT. Some research indicates that LPND may decrease LR and improve OS [11, 42]. A study from Korea by Kim et al. [43] demonstrated that clinically confirmed LPN metastasis is associated with locoregional recurrence, suggesting that it could be managed as a potentially curable regional disease. In contrast, other research has documented poor outcomes linked to high rates of distant metastasis [44]. A recent multicenter study by Ogura et al. [4, 42] revealed that LPND could lower rates of LR, lateral LR, and distant recurrence, while also improving 5-year cancer-specific survival, particularly in patients with a short-axis diameter of ≥7 mm on pretreatment MRI.
ROLE OF LPND IN PATIENTS WITHOUT CRT
LPND was originally developed in Japan, where radiation therapy has traditionally not been recommended for most locally advanced rectal cancers. As a result, this approach has not gained widespread acceptance outside Japan, where CCRT in conjunction with TME has become the standard for managing advanced rectal cancer. The only large-scale randomized clinical trial, JCOG0212, showed that adding LPND to TME was non-inferior to TME alone [3]. In this study, 7.4% of patients in the LPND group had pathologically positive LPNs for stage II/III rectal cancer, despite the LPNs being less than 10 mm in size on preoperative imaging. The inclusion of LPND resulted in an acceptable LR rate of 7.4%, compared to 12.6% in the group undergoing TME alone. This outcome supports the conclusion that the noninferiority of LPND to TME alone may justify its traditional use in Japan.
The perspective in Western countries differs. TME combined with preoperative CCRT for stage II/III lower rectal cancer has been shown to achieve similar or even lower LR rates compared to those observed with LPND. Additionally, more than 90% (specifically 92.6%) of patients undergoing nonselective (prophylactic) LPND may be receiving unnecessary treatment. A subgroup analysis revealed that 21.4% LPN positivity occurred in patients with enlarged LPNs greater than 5 mm, whereas only a 5.2% positivity rate was found in those with LPNs smaller than 5 mm [36]. For patients with invisible or LPNs smaller than 5 mm, nearly 95% could potentially avoid LPND. It is hypothesized that radiation may sterilize some of these metastatic LPNs, suggesting that TME alone could be sufficient for almost all patients without suspicious LPNs when CCRT is applied.
ROLE OF LPND VS. CRT ALONE
Tsukada et al. [45] compared the outcomes of 439 T3 rectal cancer patients treated with TME plus LPND in Japan to those treated with CRT plus TME in France. The estimated 5-year LR rate, DFS, and OS were 4.9%, 71%, and 82% in the CRT group, respectively, and 8.6%, 75%, and 90% in the LPND group. The rates of lateral LR versus nonlateral LR were 0.5% versus 4.2% in the CRT+TME group and 1.8% versus 6.2% in the TME+LPND group. The study concluded that LPND did not offer any survival benefits over CRT but was associated with a higher rate of complications.
Another study compared TME plus LPND without neoadjuvant treatment, as conducted by the Japanese National Cancer Center Hospital (NCCH) group [46], with TME alone and CCRT plus TME from a previous Dutch trial. The 5-year LR rates were 6.9% in the Japanese group, 5.8% in the Dutch group treated with CCRT and TME, and 12.1% in the Dutch group treated with TME alone. These results suggest that both LPND and CCRT are more effective than TME alone in reducing LR rates.
Among Japanese institutions, internal comparisons between CCRT combined with TME and TME with LPND for advanced rectal cancer without clinically suspicious LPNs have shown nearly equal survival outcomes in both groups [47, 48]. This suggests that TME alone, when accompanied by preoperative radiotherapy, can achieve favorable outcomes.
ROLE OF ADDITIONAL LPND EVEN AFTER CRT
As discussed in the previous section, LPND and CRT are equally effective in controlling LR for patients without clinically suspicious LPNs. This leads to an important question: can CRT effectively sterilize metastatic LPNs in patients who have clinically suspicious LPNs?
Kim et al. [43] reported intriguing findings from a study involving 366 patients undergoing CCRT with TME, where 82.7% of the 22 LRs occurred in the lateral pelvic area. These LRs were strongly correlated with the size of pretreatment LPN metastases, showing recurrence rates of 2.3%, 12.5%, and 68.8% for LPNs sized <5, 5 to 10, and >10 mm, respectively. A subsequent study with a larger sample size confirmed these findings, revealing an LR rate of 7.2%, with 64.6% of recurrences involving LPNs and 47.6% of these recurrences occurring without other metastases. Additionally, the pretreatment size of LPNs was significantly associated with 5-year LR-free survival, relapse-free survival, and OS in multivariate analysis. Kim et al. [27] observed similar outcomes in advanced rectal cancer cases with initially enlarged LPNs (>5 mm in short-axis diameter) that had reduced in size after CRT and were subsequently treated with TME alone. Among these patients, 11 out of 31 (35.5% ) experienced recurrence; this included 7 patients (22.6%) with LRs, 6 patients (19.4%) involving the lateral pelvic sidewall, and 5 patients (16.1%) who developed isolated pelvic node recurrence at the same site, in situ LPN recurrence, where LPN metastasis was suspected on pretreatment MRI. More recently, a Western international multicenter comparative study involving 159 patients with enlarged LPNs (>5 mm) compared outcomes between 2 groups: those who underwent CRT and TME alone (n=115) and those who received additional LPND alongside CRT and TME (n=44) [49]. The study found that the LR rate was 3% in the LPND group compared to 11% in the TME alone group. DFS and OS rates were similar between the 2 groups. However, multivariate analysis identified LPND as an independent prognostic factor for reduced LRs. Additionally, an international collaborative pooled analysis reported by Ogura et al. [4, 42] demonstrated the oncologic benefits of adding LPND compared to TME alone, particularly in the subgroup with enlarged LPNs (>7 mm in short-axis diameter) on pretreatment MRI. The study showed better outcomes for the LPND group in terms of 5-year lateral LR (5.7% vs. 19.5%), LR (5.7% vs. 25.6%), distant recurrence (13.5% vs. 30.8%), and cancer-specific survival (94.1% vs. 79.4%).
These reports indicate that controlling LPN metastasis with CRT is not consistently effective in cases where LPN enlargement is suspected to be due to metastasis. Conversely, adding LPND has proven to be effective in managing CRT cases involving LPN enlargement and suspected metastasis.
SELECTIVE LPND
Optimal strategies for managing clinically suspicious LPNs have become clearer, with current evidence supporting the use of both CRT and LPND. Since neither LPND alone nor CRT alone can completely eliminate metastatic LPNs, particularly in patients with enlarged LPNs diagnosed by high-resolution MRI, a combined approach of CRT followed by TME and LPND on the affected side may be the most reasonable strategy.
In the author's own series [27], selective LPND for patients who responded favorably to preoperative CRT, especially those with initially suspicious lateral pelvic nodes (>5 mm in mean short-axis diameter), significantly reduced local recurrence from 23.1% to 0% at a median follow-up of 34 months and notably enhanced OS. This led us to revise our strategy to incorporate LPND even for patients who respond well to CRT.
Similarly, based on their earlier study, the Korean National Cancer Center group previously did not recommend LPND for good responders [50]. However, they have recently revised their approach following new evidence that LPND significantly reduces LR compared to TME alone in patients whose LPN size decreased from ≥5 to <5 mm. Additionally, in patients whose LPN size did not decrease to <5 mm, LPND has been shown to improve relapse-free survival compared to TME alone [51].
Despite these advances, there is ongoing debate about whether the indication for LPND should be based on MRI results before or after treatment for metastatic LPNs. Malakorn et al. [37] found that 20.3% of patients with posttreatment LPNs that had shrunk to <5 mm showed no signs of cancer in pathologic examinations. However, the remaining 79.7% of patients, whose LPNs remained >5 mm, exhibited metastatic rates of 64.7%. After a median follow-up of 39 months, no patients in the group with LPNs <5 mm died from cancer. Additionally, there were no recurrences in the lateral compartment across the entire cohort. Based on these findings, they recommend LPND only for LPNs >5 mm following CRT.
TECHNIQUES OF LPND
Japanese surgeons pioneered open extended LPND in the 1980s for treating advanced rectal cancer [52]. However, this procedure was associated with significant complications, including substantial bleeding and a high incidence of urinary and sexual dysfunction. To address these issues, nerve-preserving LPND was developed to maintain autonomic nerve function without compromising oncologic outcomes [53, 54].
In recent decades, laparoscopic surgery has become increasingly popular for treating rectal cancer, prompting efforts to adapt this technique for LPND. Laparoscopy provides a magnified view that allows surgeons to more easily identify small vessels, nerves, and fascial structures, which are less visible in conventional open surgery. Following several case series [21, 55, 56], recent studies have compared the outcomes of laparoscopic LPND with those of the open approach. One meta-analysis, which included 335 cases from 7 comparative studies, found that laparoscopic LPND was associated with lower postoperative morbidity, shorter hospital stays, and reduced urinary retention compared to open surgery, although some heterogeneity was noted among these studies [57]. Regarding long-term oncologic outcomes, several multicenter studies from Korea, Japan, and China have demonstrated that DFS and OS were similar between the laparoscopic and open LPND groups [58–60].
Robotic surgery, which offers enhanced precision through the EndoWrist function of instruments (Intuitive Surgical), surgeon control of most instruments, and a 3-dimensional (3D) magnified surgical view, has become a significant advancement in complex surgical procedures. This technology is especially advantageous for LPND, which involves the meticulous dissection of lymphoareolar tissues from complex neurovascular bundles in the narrow pelvic sidewall. Early case series on robotic LPND have confirmed its safety and feasibility [61, 62]. Further studies comparing robotic LPND with open and laparoscopic methods have shown that the robotic approach yields more favorable short-term outcomes. A recent meta-analysis of 567 patients (266 robotic and 301 laparoscopic LPND) across 5 studies found that robotic LPND resulted in fewer overall complications, notably reduced urinary retention, compared to the laparoscopic approach. Additionally, the robotic technique allows for the harvesting of a greater number of LPNs [63].
However, data on long-term oncologic outcomes remain limited. Yamaguchi et al. [64] reported a higher 5-year locoregional recurrence-free survival rate with robotic LPND compared to the open approach (98.0% vs. 90.9%, P=0.029), although there were no significant differences in 5-year DFS (P=0.157) and OS (P=0.106) rates. Similarly, Song et al. [31] compared long-term outcomes between robotic and laparoscopic LPND, finding better 5-year OS rates in the robotic LPND group (92.2% vs. 65.0%, P=0.017) during a median follow-up of 44.3 months. However, a meta-analysis including 292 patients from 3 Korean studies indicated no significant differences in overall recurrence and locoregional recurrence between the robotic and laparoscopic LPND groups [65]. These findings suggest potential advantages for the robotic approach in LPND, but further studies are needed to conclusively establish the benefits of robotic surgery for this procedure.
Despite these advancements, the complex neurovascular networks in the narrow pelvic sidewall pose technical challenges, increasing the risk of incomplete dissection of LPNs, even in cases involving metastatic LPNs. Kim et al. [66] developed a new protocol using fluorescence imaging (FI) for the intraoperative visualization of LPNs and lymphatic channels, which aids surgeons in minimizing the risk of incomplete LPND. In this study, the author injected 0.2 mL of a premixed indocyanine green solution (2.5 mg in 10 mL of saline) into the submucosa of the rectum, at the 3 and 9 o’clock positions, 1 to 2 cm above the dentate line, through the anus, 3 to 5 hours before surgery. FI provides landmarks that guide the dissection of LNs by visualizing them in real time. It is particularly helpful in identifying LNs obscured by complex structures, including vessels and nerves, under white light. The author also introduced a dual image–guided technique that combines FI with 3D reconstruction images to navigate suspicious LPNs in the relevant anatomy of the pelvic sidewall [67]. Using this technique, the author was able to identify suspicious LPNs among indocyanine green-bearing LNs under FI and then intraoperatively match each LPN with its corresponding 3D reconstruction image in real time, ensuring their complete and safe removal from the pelvic sidewall.
Additionally, studies have explored the learning curve associated with robotic LPND. Kim et al. [68] identified 4 learning phases and highlighted that the completeness of the LPND procedure improves with the surgeon's experience, as well as with the use of advanced imaging systems and standardized surgical techniques. These findings underscore the importance of continuous training and the adoption of new technologies in optimizing LPND outcomes.
COMPLICATIONS OF LPND
Considering the complexity of LPND, it is expected to have a higher rate of surgical complications compared to TME alone. The Chinese Lateral Node Collaborative Group’s multicenter analysis reported overall complication rates of 15.2% and severe complication rates of 7.8% following TME with LPND [69]. The only independent risk factor identified for both overall and severe morbidity was an operation duration of 260 minutes or more. A recent meta-analysis of 8 retrospective studies comparing TME alone with TME combined with LPND found that the addition of LPND significantly increased the incidence of overall complications, approximately 1.5 times higher than with TME alone [70]. In contrast, the JCOG0212 study [71], which involved nonradiated patients, showed that TME with LPND was associated only with significantly longer operation times and greater blood loss compared to TME alone, while the rates of overall grade 3 to 4 morbidities were similar between the groups.
Lymphocele is a common complication following LPND, often asymptomatic and typically detected during follow-up appointments. Recent studies report an incidence rate ranging from 17.7% to 30.6% [72, 73]. These fluid collections usually appear between 3 to 8 weeks postoperatively, though they can occasionally emerge up to a year later. The clinical presentation of lymphoceles varies widely; many patients are asymptomatic and are diagnosed incidentally during routine imaging. Kim et al. [72] reported that 6.7% of patients developed symptomatic, infected lymphoceles, presenting with symptoms such as fever, pelvic pain, and leg edema, requiring intervention. Some patients required prolonged management with percutaneous nephrostomy catheters even after the lymphocele had resolved. Efforts to prevent lymphocele formation, including the use of hemostatic agents, tissue sealants, and intra-abdominal drains, have generally shown limited effectiveness, as noted in recent meta-analyses [74]. Additionally, a randomized controlled trial evaluating peritoneal flap techniques for lymphatic drainage found no significant advantage over traditional methods, although it did reduce the incidence of symptomatic lymphoceles [75]. This underscores the need for continued research into more effective preventive strategies and vigilant postoperative monitoring.
Urinary complications are a significant concern following preoperative CRT, particularly when it is combined with TME and LPND. Urinary retention is the most frequently observed complication, occurring in 7.2% of cases. Kim et al. [72] reported a slightly lower incidence rate of 5.5%. According to data from the JCOG0212 study, there was no difference in voiding function; however, it was noted that intraoperative blood loss, which was higher in the group undergoing TME with LPND, was significantly associated with postoperative urinary dysfunction [76]. Permanent catheterization due to neurogenic bladder was uncommon, with a reported incidence of 1.8% in the previous study.
There is limited literature on male sexual function following LPND. The JCOG0212 study investigated changes in male sexual dysfunction, defined by an International Index of Erectile Function score of 21 or greater, by comparing TME alone to TME with LPND [76]. Before surgery, only 14% of patients in the TME with LPND group and 12% in the TME alone group exhibited normal erectile function. Consequently, postoperative sexual dysfunction was observed in 79% of the TME with LPND group and 68% of the TME alone group, although this difference was not statistically significant. Similarly, there was no significant difference between the groups in the prevalence of mild erectile dysfunction (71% in the TME with LPND group vs. 59% in the TME alone group) or in the absence of erectile dysfunction (65% in the TME with LPND group vs. 53% in the TME alone group).
These findings underscore the necessity of meticulously weighing the potential risks and benefits of LPND in the management of rectal cancer, particularly concerning patient quality of life and postoperative recovery.
LPND IN THE ERA OF TNT
TNT is increasingly used in the treatment of locally advanced rectal cancer primarily for 2 reasons: to enhance DFS and OS, and to facilitate a clinical complete response that allows for organ preservation under the watch-and-wait approach [77, 78]. The practice of performing LPND following TNT has been infrequently reported, largely because TNT is predominantly utilized in Western countries where LPND is not commonly performed. Conversely, in Eastern countries, where TNT is only beginning to be adopted, LPND is performed more frequently.
Peacock et al. [79] reported 88 cases of LPND involving LPNs with a mean pretreatment diameter of 10 mm, which decreased to 6 mm posttreatment. In contrast, 70 non-LPND cases had LPNs with an average pretreatment diameter of 6 mm, reducing to 4 mm posttreatment. The positive rate of LPNs in the LPND group was 34.1%, suggesting that TNT alone may not completely sterilize all clinically suspicious LPNs in advanced rectal cancer. When LPND was added to TNT and TME, the recurrence rates were comparable: 3.4% versus 4.6% for lateral LR and 24.9% versus 28.2% for distant recurrence, 33.9% versus 36.7% for overall recurrence, and 12.2% versus 9.6% for LR rates in the LPND group versus the non-LPND group, respectively. Given the more aggressive metastatic characteristics associated with LPNs in the LPND group, surgical resection of these nodes may be beneficial in achieving better oncological outcomes. Clearly, further studies are necessary to validate the efficacy of LPND in the era of TNT.
CONCLUSION
In this review, we have examined the evolving landscape of managing LPN metastasis in rectal cancer, focusing on the interplay between LPND and CRT. Our findings highlight the complexity of treatment decisions in this area and the continuing debate over the optimal approach.
The evidence indicates that while LPND has shown benefits in certain situations, especially in non-irradiated cases with visibly enlarged LPNs, its widespread use may not be universally justified. Conversely, CRT alone might not eliminate all metastatic LPNs, which supports the idea that additional LPND could be necessary for patients with larger LPNs before treatment or for those whose LPNs remain enlarged despite undergoing CRT.
A comparison between Eastern and Western practices reveals divergent strategies: Japan traditionally favors LPND without CRT, while Western countries lean towards CRT with selective LPND. Recent advancements, such as the adoption of TNT and robotic-assisted surgeries, further complicate the landscape but also offer promising avenues for enhancing patient outcomes.
Our review also highlights the importance of balancing the risks and benefits of LPND. Although LPND can decrease LR rates and improve DFS, it is linked to increased complications such as lymphocele, urinary dysfunction, and potential effects on sexual health. Employing precise surgical techniques and selecting patients carefully are essential to minimize these risks.
Looking forward, further research is essential to refine the criteria for LPND, especially given the context of modern treatment regimens such as TNT. By integrating these insights, clinicians will be better equipped to tailor their approaches to the specific needs of individual patients, ultimately advancing the standard of care for rectal cancer patients with LPN involvement.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: GSC; Data curation: GSC, HJK; Investigation: GSC, HJK; Methodology: GSC, HJK; Project administration: GSC; Writing–original draft: GSC, HJK; Wrting–review & editing: GSC, HJK. All Authors read and approved the final manuscript.
REFERENCES
- 1.Gerota D. Die lymphgefasse des rectums und des anus [The lymphatic vessels of the rectum and anus] Arch Anat Physiol. 1895;7:240–256. German. [Google Scholar]
- 2.Sauer I, Bacon HE. A new approach for excision of carcinoma of the lower portion of the rectum and anal canal. Surg Gynecol Obstet. 1952;95:229–42. [PubMed] [Google Scholar]
- 3.Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017;266:201–7. doi: 10.1097/SLA.0000000000002212. [DOI] [PubMed] [Google Scholar]
- 4.Ogura A, Konishi T, Beets GL, Cunningham C, Garcia-Aguilar J, Iversen H, et al. Lateral nodal features on restaging magnetic resonance imaging associated with lateral local recurrence in low rectal cancer after neoadjuvant chemoradiotherapy or radiotherapy. JAMA Surg. 2019;154:e192172. doi: 10.1001/jamasurg.2019.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kobayashi H, Mochizuki H, Kato T, Mori T, Kameoka S, Shirouzu K, et al. Outcomes of surgery alone for lower rectal cancer with and without pelvic sidewall dissection. Dis Colon Rectum. 2009;52:567–76. doi: 10.1007/DCR.0b013e3181a1d994. [DOI] [PubMed] [Google Scholar]
- 6.Yokoyama Y, Nozawa H, Sasaki K, Murono K, Emoto S, Matsuzaki H, et al. Essential anatomy for lateral lymph node dissection. Ann Coloproctol. 2023;39:457–66. doi: 10.3393/ac.2023.00164.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Japanese Society for Cancer of the Colon and Rectum . Japanese classification of colorectal, appendiceal, and anal carcinoma. 9th ed. Kanehara; 2018. Japanese. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi GS, Kim HJ, Park JS, Park SY. Minimally invasive approach for lateral pelvic node dissection: a standardization based on surgical anatomy. Dis Colon Rectum. 2019;62:1550. doi: 10.1097/DCR.0000000000001476. [DOI] [PubMed] [Google Scholar]
- 9.Fujita S, Yamamoto S, Akasu T, Moriya Y. Lateral pelvic lymph node dissection for advanced lower rectal cancer. Br J Surg. 2003;90:1580–5. doi: 10.1002/bjs.4350. [DOI] [PubMed] [Google Scholar]
- 10.Matsumoto T, Ohue M, Sekimoto M, Yamamoto H, Ikeda M, Monden M. Feasibility of autonomic nerve-preserving surgery for advanced rectal cancer based on analysis of micrometastases. Br J Surg. 2005;92:1444–8. doi: 10.1002/bjs.5141. [DOI] [PubMed] [Google Scholar]
- 11.Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, et al. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006;49:1663–72. doi: 10.1007/s10350-006-0714-z. [DOI] [PubMed] [Google Scholar]
- 12.Ueno H, Mochizuki H, Hashiguchi Y, Ishiguro M, Miyoshi M, Kajiwara Y, et al. Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg. 2007;245:80–7. doi: 10.1097/01.sla.0000225359.72553.8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fujita S, Yamamoto S, Akasu T, Moriya Y. Risk factors of lateral pelvic lymph node metastasis in advanced rectal cancer. Int J Colorectal Dis. 2009;24:1085–90. doi: 10.1007/s00384-009-0704-4. [DOI] [PubMed] [Google Scholar]
- 14.Akiyoshi T, Watanabe T, Miyata S, Kotake K, Muto T, Sugihara K, et al. Results of a Japanese nationwide multi-institutional study on lateral pelvic lymph node metastasis in low rectal cancer: is it regional or distant disease? Ann Surg. 2012;255:1129–34. doi: 10.1097/SLA.0b013e3182565d9d. [DOI] [PubMed] [Google Scholar]
- 15.Ogawa S, Hida J, Ike H, Kinugasa T, Ota M, Shinto E, et al. The important risk factor for lateral pelvic lymph node metastasis of lower rectal cancer is node-positive status on magnetic resonance imaging: study of the Lymph Node Committee of Japanese Society for Cancer of the Colon and Rectum. Int J Colorectal Dis. 2016;31:1719–28. doi: 10.1007/s00384-016-2641-3. [DOI] [PubMed] [Google Scholar]
- 16.Yamaoka Y, Kinugasa Y, Shiomi A, Yamaguchi T, Kagawa H, Yamakawa Y, et al. Preoperative chemoradiotherapy changes the size criterion for predicting lateral lymph node metastasis in lower rectal cancer. Int J Colorectal Dis. 2017;32:1631–7. doi: 10.1007/s00384-017-2873-x. [DOI] [PubMed] [Google Scholar]
- 17.Matsuda T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, et al. Outcomes and prognostic factors of selective lateral pelvic lymph node dissection with preoperative chemoradiotherapy for locally advanced rectal cancer. Int J Colorectal Dis. 2018;33:367–74. doi: 10.1007/s00384-018-2974-1. [DOI] [PubMed] [Google Scholar]
- 18.Dev K, Veerenderkumar KV, Krishnamurthy S. Incidence and predictive model for lateral pelvic lymph node metastasis in lower rectal cancer. Indian J Surg Oncol. 2018;9:150–6. doi: 10.1007/s13193-017-0719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iwasa Y, Koyama F, Marugami N, Kuge H, Nakamoto T, Obara S, et al. The middle rectal artery detected by contrast-enhanced magnetic resonance imaging predicts lateral lymph node metastasis in lower rectal cancer. Int J Colorectal Dis. 2021;36:1677–84. doi: 10.1007/s00384-021-03887-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abe T, Yasui M, Imamura H, Matsuda C, Nishimura J, Haraguchi N, et al. Combination of extramural venous invasion and lateral lymph node size detected with magnetic resonance imaging is a reliable biomarker for lateral lymph node metastasis in patients with rectal cancer. World J Surg Oncol. 2022;20:5. doi: 10.1186/s12957-021-02464-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang JT. Technical feasibility of laparoscopic lateral pelvic lymph node dissection for patients with low rectal cancer after concurrent chemoradiation therapy. Ann Surg Oncol. 2011;18:153–9. doi: 10.1245/s10434-010-1238-2. [DOI] [PubMed] [Google Scholar]
- 22.Oh HK, Kang SB, Lee SM, Lee SY, Ihn MH, Kim DW, et al. Neoadjuvant chemoradiotherapy affects the indications for lateral pelvic node dissection in mid/low rectal cancer with clinically suspected lateral node involvement: a multicenter retrospective cohort study. Ann Surg Oncol. 2014;21:2280–7. doi: 10.1245/s10434-014-3559-z. [DOI] [PubMed] [Google Scholar]
- 23.Akiyoshi T, Matsueda K, Hiratsuka M, Unno T, Nagata J, Nagasaki T, et al. Indications for lateral pelvic lymph node dissection based on magnetic resonance imaging before and after preoperative chemoradiotherapy in patients with advanced low-rectal cancer. Ann Surg Oncol. 2015;22 Suppl 3:S614–20. doi: 10.1245/s10434-015-4565-5. [DOI] [PubMed] [Google Scholar]
- 24.Sinukumar S, Engineer R, Saklani A. Preliminary experience with lateral pelvic lymph node dissection in locally advanced rectal cancer. Indian J Gastroenterol. 2015;34:320–4. doi: 10.1007/s12664-015-0589-9. [DOI] [PubMed] [Google Scholar]
- 25.Shin US, Nancy You Y, Nguyen AT, Bednarski BK, Messick C, Maru DM, et al. Oncologic outcomes of extended robotic resection for rectal cancer. Ann Surg Oncol. 2016;23:2249–57. doi: 10.1245/s10434-016-5117-3. [DOI] [PubMed] [Google Scholar]
- 26.Ishihara S, Kawai K, Tanaka T, Kiyomatsu T, Hata K, Nozawa H, et al. Oncological outcomes of lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Dis Colon Rectum. 2017;60:469–76. doi: 10.1097/DCR.0000000000000752. [DOI] [PubMed] [Google Scholar]
- 27.Kim HJ, Choi GS, Park JS, Park SY, Cho SH, Lee SJ, et al. Optimal treatment strategies for clinically suspicious lateral pelvic lymph node metastasis in rectal cancer. Oncotarget. 2017;8:100724–33. doi: 10.18632/oncotarget.20121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim MJ, Hur BY, Lee ES, Park B, Joo J, Kim MJ, et al. Prediction of lateral pelvic lymph node metastasis in patients with locally advanced rectal cancer with preoperative chemoradiotherapy: focus on MR imaging findings. PLoS One. 2018;13:e0195815. doi: 10.1371/journal.pone.0195815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hiyoshi Y, Miyamoto Y, Kiyozumi Y, Eto K, Nagai Y, Iwatsuki M, et al. Risk factors and prognostic significance of lateral pelvic lymph node metastasis in advanced rectal cancer. Int J Clin Oncol. 2020;25:110–7. doi: 10.1007/s10147-019-01523-w. [DOI] [PubMed] [Google Scholar]
- 30.Kawai K, Shiratori H, Hata K, Nozawa H, Tanaka T, Nishikawa T, et al. Optimal size criteria for lateral lymph node dissection after neoadjuvant chemoradiotherapy for rectal cancer. Dis Colon Rectum. 2021;64:274–83. doi: 10.1097/DCR.0000000000001866. [DOI] [PubMed] [Google Scholar]
- 31.Song SH, Choi GS, Kim HJ, Park JS, Park SY, Lee SM, et al. Long-term clinical outcomes of total mesorectal excision and selective lateral pelvic lymph node dissection for advanced low rectal cancer: a comparative study of a robotic versus laparoscopic approach. Tech Coloproctol. 2021;25:413–23. doi: 10.1007/s10151-020-02383-7. [DOI] [PubMed] [Google Scholar]
- 32.Agger E, Åkerlund V, Ekberg O, Jörgren F, Lydrup ML, Buchwald P. Management, treatment and prognostic significance of lateral lymph node metastases in rectal cancer: a regional cohort study. Int J Colorectal Dis. 2021;36:2707–14. doi: 10.1007/s00384-021-04018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, et al. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003;227:371–7. doi: 10.1148/radiol.2272011747. [DOI] [PubMed] [Google Scholar]
- 34.Dahmarde H, Parooie F, Salarzaei M. Is 18F-FDG PET/CT an accurate way to detect lymph node metastasis in colorectal cancer: a systematic review and meta-analysis. Contrast Media Mol Imaging. 2020;2020:5439378. doi: 10.1155/2020/5439378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ishibe A, Ota M, Watanabe J, Suwa Y, Suzuki S, Kanazawa A, et al. Prediction of lateral pelvic lymph-node metastasis in low rectal cancer by magnetic resonance imaging. World J Surg. 2016;40:995–1001. doi: 10.1007/s00268-015-3299-7. [DOI] [PubMed] [Google Scholar]
- 36.Komori K, Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Shiomi A, et al. Predictive factors of pathological lateral pelvic lymph node metastasis in patients without clinical lateral pelvic lymph node metastasis (clinical stage II/III): the analysis of data from the clinical trial (JCOG0212) Eur J Surg Oncol. 2019;45:336–40. doi: 10.1016/j.ejso.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 37.Malakorn S, Yang Y, Bednarski BK, Kaur H, You YN, Holliday EB, et al. Who should get lateral pelvic lymph node dissection after neoadjuvant chemoradiation? Dis Colon Rectum. 2019;62:1158–66. doi: 10.1097/DCR.0000000000001465. [DOI] [PubMed] [Google Scholar]
- 38.Enker WE, Pilipshen SJ, Heilweil ML, Stearns MW, Jr, Janov AJ, Hertz RE, et al. En bloc pelvic lymphadenectomy and sphincter preservation in the surgical management of rectal cancer. Ann Surg. 1986;203:426–33. doi: 10.1097/00000658-198604000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. Springer; 2017. [Google Scholar]
- 40.Akiyoshi T, Toda S, Tominaga T, Oba K, Tomizawa K, Hanaoka Y, et al. Prognostic impact of residual lateral lymph node metastasis after neoadjuvant (chemo)radiotherapy in patients with advanced low rectal cancer. BJS Open. 2019;3:822–9. doi: 10.1002/bjs5.50194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim HJ, Choi GS, Cho SH, Kang MK, Park JS, Park SY, et al. Sequential lateral lymphatic metastasis shows similar oncologic outcomes to upward spread in advanced rectal cancer after preoperative chemoradiotherapy. Dis Colon Rectum. 2024;67:359–68. doi: 10.1097/DCR.0000000000002989. [DOI] [PubMed] [Google Scholar]
- 42.Ogura A, Konishi T, Cunningham C, Garcia-Aguilar J, Iversen H, Toda S, et al. Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low cT3/4 rectal cancer. J Clin Oncol. 2019;37:33–43. doi: 10.1200/JCO.18.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim TH, Jeong SY, Choi DH, Kim DY, Jung KH, Moon SH, et al. Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol. 2008;15:729–37. doi: 10.1245/s10434-007-9696-x. [DOI] [PubMed] [Google Scholar]
- 44.Kim YI, Jang JK, Park IJ, Park SH, Kim JB, Park JH, et al. Lateral lymph node and its association with distant recurrence in rectal cancer: a clue of systemic disease. Surg Oncol. 2020;35:174–81. doi: 10.1016/j.suronc.2020.08.013. [DOI] [PubMed] [Google Scholar]
- 45.Tsukada Y, Rullier E, Shiraishi T, Capdepont M, Sasaki T, Celerier B, et al. Comparison between preoperative chemoradiotherapy and lateral pelvic lymph node dissection in clinical T3 low rectal cancer without enlarged lateral lymph nodes. Colorectal Dis. 2023;25:1153–62. doi: 10.1111/codi.16535. [DOI] [PubMed] [Google Scholar]
- 46.Kusters M, Beets GL, van de Velde CJ, Beets-Tan RG, Marijnen CA, Rutten HJ, et al. A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg. 2009;249:229–35. doi: 10.1097/SLA.0b013e318190a664. [DOI] [PubMed] [Google Scholar]
- 47.Nagawa H, Muto T, Sunouchi K, Higuchi Y, Tsurita G, Watanabe T, et al. Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum. 2001;44:1274–80. doi: 10.1007/BF02234784. [DOI] [PubMed] [Google Scholar]
- 48.Watanabe T, Tsurita G, Muto T, Sawada T, Sunouchi K, Higuchi Y, et al. Extended lymphadenectomy and preoperative radiotherapy for lower rectal cancers. Surgery. 2002;132:27–33. doi: 10.1067/msy.2002.125357. [DOI] [PubMed] [Google Scholar]
- 49.Kroon HM, Malakorn S, Dudi-Venkata NN, Bedrikovetski S, Liu J, Kenyon-Smith T, et al. Local recurrences in western low rectal cancer patients treated with or without lateral lymph node dissection after neoadjuvant (chemo)radiotherapy: an international multi-centre comparative study. Eur J Surg Oncol. 2021;47:2441–9. doi: 10.1016/j.ejso.2021.06.004. [DOI] [PubMed] [Google Scholar]
- 50.Kim MJ, Chan Park S, Kim TH, Kim DY, Kim SY, Baek JY, et al. Is lateral pelvic node dissection necessary after preoperative chemoradiotherapy for rectal cancer patients with initially suspected lateral pelvic node? Surgery. 2016;160:366–76. doi: 10.1016/j.surg.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 51.Kim MJ, Chang GJ, Lim HK, Song MK, Park SC, Sohn DK, et al. Oncological impact of lateral lymph node dissection after preoperative chemoradiotherapy in patients with rectal cancer. Ann Surg Oncol. 2020;27:3525–33. doi: 10.1245/s10434-020-08481-y. [DOI] [PubMed] [Google Scholar]
- 52.Moriya Y, Hojo K, Sawada T, Koyama Y. Significance of lateral node dissection for advanced rectal carcinoma at or below the peritoneal reflection. Dis Colon Rectum. 1989;32:307–15. doi: 10.1007/BF02553486. [DOI] [PubMed] [Google Scholar]
- 53.Moriya Y. Pelvic node dissection with autonomic nerve sparing for invasive lower rectal cancer. In: Wanebo HJ, editor. Colorectal cancer. Mosby; 1993. p. 274–89. [Google Scholar]
- 54.Hojo K, Koyama Y, Moriya Y. Lymphatic spread and its prognostic value in patients with rectal cancer. Am J Surg. 1982;144:350–4. doi: 10.1016/0002-9610(82)90018-6. [DOI] [PubMed] [Google Scholar]
- 55.Konishi T, Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Akiyoshi T, et al. Lateral lymph node dissection with preoperative chemoradiation for locally advanced lower rectal cancer through a laparoscopic approach. Surg Endosc. 2011;25:2358–9. doi: 10.1007/s00464-010-1531-y. [DOI] [PubMed] [Google Scholar]
- 56.Park JS, Choi GS, Lim KH, Jang YS, Kim HJ, Park SY, et al. Laparoscopic extended lateral pelvic node dissection following total mesorectal excision for advanced rectal cancer: initial clinical experience. Surg Endosc. 2011;25:3322–9. doi: 10.1007/s00464-011-1719-9. [DOI] [PubMed] [Google Scholar]
- 57.Du R, Zhou J, Li D, Zhang Q, Liu J, Ma C, et al. Postoperative morbidity and mortality after mesorectal excision with laparoscopic versus conventional open lateral lymph node dissection for advanced rectal cancer: a meta-analysis. Asian J Surg. 2021;44:26–35. doi: 10.1016/j.asjsur.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 58.Yamaguchi T, Konishi T, Kinugasa Y, Yamamoto S, Akiyoshi T, Okamura R, et al. Laparoscopic versus open lateral lymph node dissection for locally advanced low rectal cancer: a subgroup analysis of a large multicenter cohort study in Japan. Dis Colon Rectum. 2017;60:954–64. doi: 10.1097/DCR.0000000000000843. [DOI] [PubMed] [Google Scholar]
- 59.Lim HK, Kim M, Park JW, Ryoo SB, Park KJ, Oh HK, et al. Laparoscopic versus open lateral pelvic lymph node dissection in locally advanced rectal cancer: multicentre retrospective cohort study. BJS Open. 2022;6:zrac068. doi: 10.1093/bjsopen/zrac068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tang J, Zhou S, Zhao W, Lou Z, Liang J, Feng B, et al. Short- and long-term outcomes of laparoscopic versus open selective lateral pelvic lymph node dissection for locally advanced middle-low rectal cancer: Results of a multicentre lateral node study in China. Colorectal Dis. 2022;24:1325–34. doi: 10.1111/codi.16223. [DOI] [PubMed] [Google Scholar]
- 61.Park JA, Choi GS, Park JS, Park SY. Initial clinical experience with robotic lateral pelvic lymph node dissection for advanced rectal cancer. J Korean Soc Coloproctol. 2012;28:265–70. doi: 10.3393/jksc.2012.28.5.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kagawa H, Kinugasa Y, Shiomi A, Yamaguchi T, Tsukamoto S, Tomioka H, et al. Robotic-assisted lateral lymph node dissection for lower rectal cancer: short-term outcomes in 50 consecutive patients. Surg Endosc. 2015;29:995–1000. doi: 10.1007/s00464-014-3760-y. [DOI] [PubMed] [Google Scholar]
- 63.Chen YC, Tsai YY, Ke TW, Shen MY, Fingerhut A, Chen WT. Robotic versus laparoscopic pelvic lateral lymph node dissection in locally advanced rectal cancer: a systemic review and meta-analysis. Surg Endosc. 2024;38:3520–30. doi: 10.1007/s00464-024-10901-z. [DOI] [PubMed] [Google Scholar]
- 64.Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, Furutani A, et al. Oncological outcomes of robotic-assisted laparoscopic versus open lateral lymph node dissection for locally advanced low rectal cancer. Surg Endosc. 2018;32:4498–505. doi: 10.1007/s00464-018-6197-x. [DOI] [PubMed] [Google Scholar]
- 65.Chaouch MA, Hussain MI, Carneiro da Costa A, Mazzotta A, Krimi B, Gouader A, et al. Robotic versus laparoscopic total mesorectal excision with lateral lymph node dissection for advanced rectal cancer: a systematic review and meta-analysis. PLoS One. 2024;19:e0304031. doi: 10.1371/journal.pone.0304031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim HJ, Park JS, Choi GS, Park SY, Lee HJ. Fluorescence-guided robotic total mesorectal excision with lateral pelvic lymph node dissection in locally advanced rectal cancer: a video presentation. Dis Colon Rectum. 2017;60:1332–3. doi: 10.1097/DCR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 67.Kim HJ, Choi GS, Park JS, Park SY, Cho SH, Seo AN, et al. S122: impact of fluorescence and 3D images to completeness of lateral pelvic node dissection. Surg Endosc. 2020;34:469–76. doi: 10.1007/s00464-019-06830-x. [DOI] [PubMed] [Google Scholar]
- 68.Kim HJ, Choi GS, Park JS, Park SY, Lee SM, Song SH. Stepwise improvement of surgical quality in robotic lateral pelvic node dissection: lessons from 100 consecutive patients with locally advanced rectal cancer. Dis Colon Rectum. 2022;65:599–607. doi: 10.1097/DCR.0000000000002329. [DOI] [PubMed] [Google Scholar]
- 69.Zhou S, Tang J, Mei S, Lou Z, Fu W, Feng B, et al. Risk factors and prognostic significance of postoperative complications following lateral pelvic lymph node dissection for rectal cancer: results of the multicenter lateral node study in China. Jpn J Clin Oncol. 2022;52:1150–8. doi: 10.1093/jjco/hyac109. [DOI] [PubMed] [Google Scholar]
- 70.Hajibandeh S, Hajibandeh S, Matthews J, Palmer L, Maw A. Meta-analysis of survival and functional outcomes after total mesorectal excision with or without lateral pelvic lymph node dissection in rectal cancer surgery. Surgery. 2020;168:486–96. doi: 10.1016/j.surg.2020.04.063. [DOI] [PubMed] [Google Scholar]
- 71.Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012;13:616–21. doi: 10.1016/S1470-2045(12)70158-4. [DOI] [PubMed] [Google Scholar]
- 72.Kim HJ, Choi GS, Park JS, Park SY, Song SH, Lee SM, et al. Long-term complications of laparoscopic or robotic lateral pelvic node dissection after preoperative chemoradiotherapy for locally advanced rectal cancer. Dis Colon Rectum. 2024;67:505–13. doi: 10.1097/DCR.0000000000003183. [DOI] [PubMed] [Google Scholar]
- 73.Ochiai K, Kaneko M, Nozawa H, Kawai K, Hata K, Tanaka T, et al. Incidence of and risk factors for lymphocele formation after lateral pelvic lymph node dissection for rectal cancer: a retrospective study. Colorectal Dis. 2020;22:161–9. doi: 10.1111/codi.14831. [DOI] [PubMed] [Google Scholar]
- 74.Gerken AL, Dobroschke J, Reißfelder C, Hetjens S, Braun V, Di Monta G, et al. Tissue sealants for the prevention of lymphoceles after radical inguinal lymph node dissection in patients with melanoma: a systematic review and individual patient data meta-analysis. J Surg Oncol. 2019;119:728–36. doi: 10.1002/jso.25366. [DOI] [PubMed] [Google Scholar]
- 75.Student V, Jr, Tudos Z, Studentova Z, Cesak O, Studentova H, Repa V, et al. Effect of peritoneal fixation (PerFix) on lymphocele formation in robot-assisted radical prostatectomy with pelvic lymphadenectomy: results of a randomized prospective trial. Eur Urol. 2023;83:154–62. doi: 10.1016/j.eururo.2022.07.027. [DOI] [PubMed] [Google Scholar]
- 76.Saito S, Fujita S, Mizusawa J, Kanemitsu Y, Saito N, Kinugasa Y, et al. Male sexual dysfunction after rectal cancer surgery: results of a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for patients with lower rectal cancer: Japan Clinical Oncology Group Study JCOG0212. Eur J Surg Oncol. 2016;42:1851–8. doi: 10.1016/j.ejso.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 77.Conroy T, Castan F, Etienne PL, Rio E, Mesgouez-Nebout N, Evesque L, et al. Total neoadjuvant therapy with mFOLFIRINOX versus preoperative chemoradiotherapy in patients with locally advanced rectal cancer: long-term results of the UNICANCER-PRODIGE 23 trial. Ann Oncol. 2024 Jul 8; doi: 10.1016/j.annonc.2024.06.019. [Epub]. [DOI] [PubMed] [Google Scholar]
- 78.Verheij FS, Omer DM, Williams H, Lin ST, Qin LX, Buckley JT, et al. Long-term results of organ preservation in patients with rectal adenocarcinoma treated with total neoadjuvant therapy: the randomized phase II OPRA trial. J Clin Oncol. 2024;42:500–6. doi: 10.1200/JCO.23.01208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Peacock O, Manisundaram N, Dibrito SR, Kim Y, Hu CY, Bednarski BK, et al. Magnetic resonance imaging directed surgical decision making for lateral pelvic lymph node dissection in rectal cancer after total neoadjuvant therapy (TNT) Ann Surg. 2022;276:654–64. doi: 10.1097/SLA.0000000000005589. [DOI] [PMC free article] [PubMed] [Google Scholar]


