Abstract
Introduction
Adrenocortical carcinoma (ACC) is a rare and aggressive endocrine malignancy with a high recurrence rate. Approximately half of the patients are asymptomatic, while others experience symptoms due to the tumor's size or hormone secretion. Ro resection if possible is the best option for treatment of primary as well as locoregional recurrent ACC.
Case presentation
A 20-year-old female who previously underwent open left adrenalectomy for Stage III ACC presented with complaints of heaviness and vague discomfort in the left upper abdomen. Current hormonal assays were normal. Imaging revealed a lesion in the spleen suggestive of recurrence. She underwent elective surgery involving en bloc resection of the spleen, diaphragm, and associated structures. Postoperative recovery was uneventful, histopathology confirmed recurrence and subsequent PET-CT showed no recurrence. She is currently on mitotane and remains symptom-free with no signs of recurrence after initial surgery.
Clinical discussion
Complete resection (Ro) if possible, for recurrent and metastatic disease has been linked to long-term survival and offers significant palliative benefits, particularly in cases involving symptomatic steroid production.
Conclusion
ACC has a high frequency of local recurrence therefore management of recurrence should be considered from the initial diagnosis. Ro resection of recurrence is the best potential treatment. Follow-up protocols and improving integration between surgical, oncological, and supportive care departments are crucial for overcoming healthcare challenges in Nepal.
Keywords: Adrenocortical carcinoma, En bloc resection, Loco-regional recurrence
Highlights
-
•
ACC is an aggressive tumor with a high recurrence rate.
-
•
Half of the patients are asymptomatic, while others experience symptoms due to the tumor's size or hormone secretion
-
•
R0 resection if possible is the best option for treatment of primary as well as locoregional recurrent ACC.
1. Introduction
Adrenocortical carcinoma (ACC) is a rare and among the most aggressive endocrine malignancies [1]. There is global variation in annual incidence varying from 1 to 2 cases per million [2,3]. It has a bimodal distribution in the first and fourth decades of life with more prevalence in women [2]. About 50 % of patients are either asymptomatic and the rest experience mechanical symptoms due to the tumor's size or present with symptoms related to hormonal secretion [4]. Complete resection of tumor with integrity of capsule is the primary treatment for ACC. Complete tumor resection is a crucial prognostic factor, and invasive tumors should be excised en bloc with surrounding tissues or organs [5].
ACC can recur at any time, with most recurrences occurring in the first 2 years following surgery [6]. Approximately 25 % of patients have isolated locoregional recurrence. Locoregional recurrence can involve the pancreas, spleen, liver, diaphragm, and retroperitoneum [6]. Even after what seems to be a curative resection, most patients experience early tumor recurrence or distant metastasis. Following complete resection, over 50 % of patients will experience a recurrence within five years [6]. Mitotane is frequently employed as a chemotherapeutic agent in treating ACC. Its mechanism involves uptake by the adrenal cortex, where it induces necrosis, resulting in a specific cytotoxic effect. There are varying reports concerning the use of mitotane in ACC with some suggesting a significant improvement in survival while others do not [7].
There is paucity of literature on ACC and none on treatment for recurrence of ACC from Nepal. This case adhering to SCARE 2023 guidelines details successful management of local recurrence of left adrenal tumor to spleen after a year of adrenalectomy [8].
2. Case presentation
A 20-year-old female who had undergone open left adrenalectomy (Ro resection) for Stage III left adrenocortical carcinoma, European Network for the Study of Adrenal Tumors (ENSAT) one year back was referred to department of surgical gastroenterology with complaints of heaviness and vague discomfort in left upper abdomen for 3 months. At initial presentation, she had stage III ACC with proliferative index (Ki 67): 35 % and was advised and planned for adjuvant mitotane but she was lost to follow-up. She had facial puffiness and weakness for 2 months with hypertension, Cushingoid facies and central obesity prior to presentation. Laboratory investigations revealed high 8 am serum cortisol level 61.6 μg/dl (Normal <30 μg/dl); 24-h urine cortisol level 1980 μg/day (normal range 58–403 μg/day) and Adrenocorticotropic Hormone (ACTH) 144 pg/ml (Normal <46.0 pg/ml). Rest of the findings were normal.
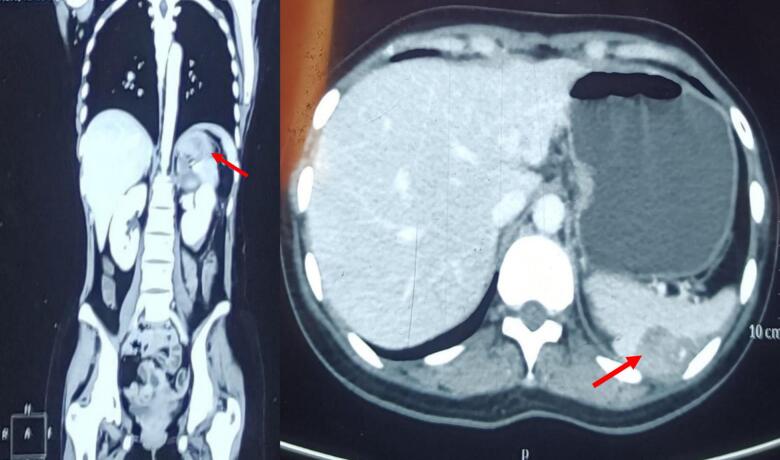
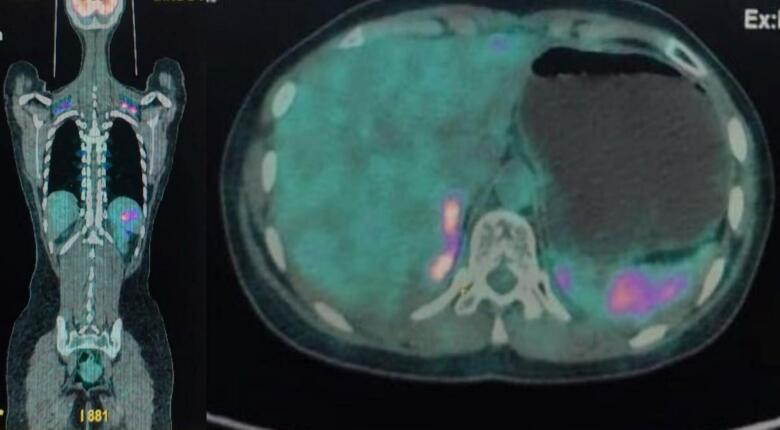
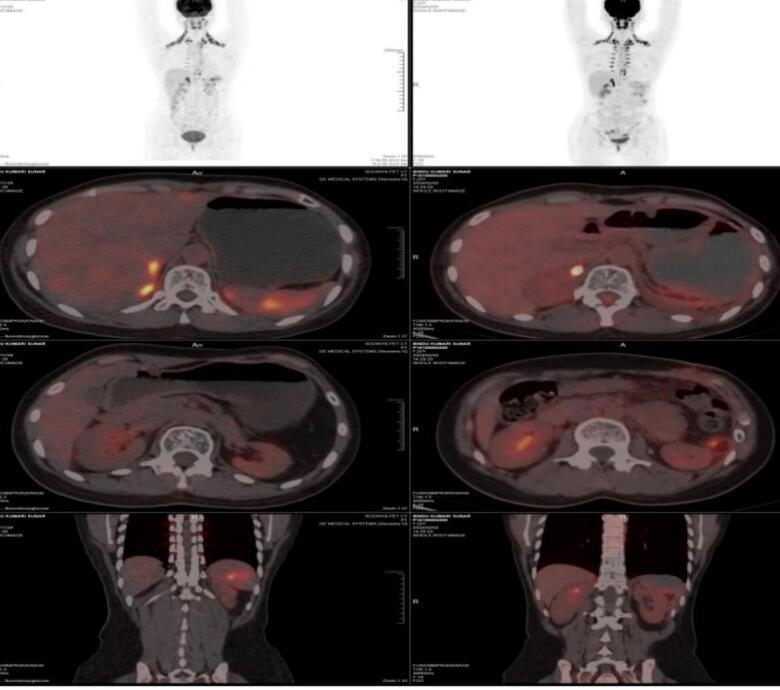
At the current presentation, the abdomen was not distended, non-tender and systemic examination was normal. Hormonal assay revealed normal cortisol, dehydroepiandrosterone and metanephrine, normetanephrine and aldosterone to renin ratio. Contrast enhanced Computed tomography (CECT) scan revealed well defined soft tissue density lesions measuring 4 × 3.1 × 2 cm in splenic parenchyma with heterogeneous enhancement in postcontrast phase with focal calcification (Fig. 1). The lesion abutted the left 10th, 11th intercostal muscle and left crus of diaphragm (Fig. 1). Positron emission tomography (PET) CT scan revealed metabolically active hypodense lesion with focal calcification in the spleen suggestive of metastasis without evidence of recurrent lesion at operated site (Fig. 2).
Fig. 1.
(Left: coronal, right: axial) CECT Abdomen/pelvis showing well defined, heterogeneously enhancing soft tissue density lesion (red arrow), in splenic parenchyma. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
PET-CT Scan showing metabolically active hypodense lesion in spleen suggestive of metastasis.
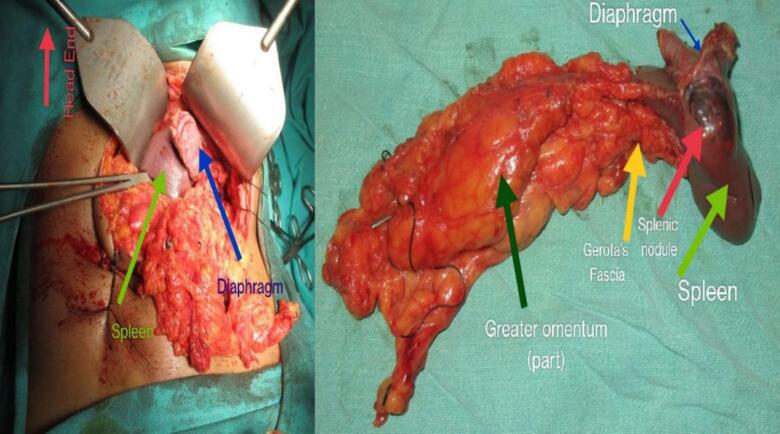
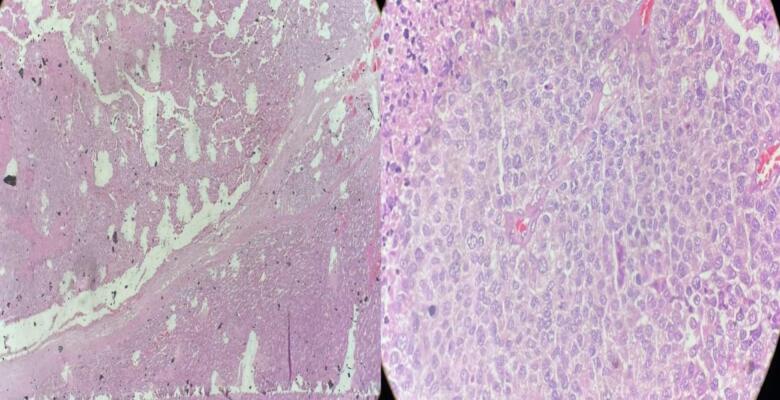
With diagnosis of locoregional recurrence of ACC, she was planned for elective surgery by team with expertise in oncologic surgery. Incision was made on the previous scar on the left subcostal region. Intraoperatively, there were no ascites, peritoneal and omental deposits or liver metastasis. A 3 × 4 cm soft to firm mass in the posterolateral surface of the spleen with invasion into the lateral dome of the diaphragm was noted (Fig. 3). In addition, a 1× 1 cm firm nodule in Gerota's fascia was identified. En bloc resection of spleen, gastrosplenic ligament, Gerota's fascia and left costal margin of the diaphragm was done followed by repair of diaphragm (Fig. 3). Perioperative course was uneventful and she was discharged on tenth post-operative day. Histopathology revealed tumor cells arranged in nests and large sheets infiltrating splenic parenchyma with fibrous capsule border with diaphragm margin being free of tumor (Fig. 4). PET CT done after 3 months of surgery revealed no FDG avid activity at the operated site or elsewhere (Fig. 5). She is currently on mitotane and on regular follow-up with no symptoms, signs, laboratory and imaging findings suggestive of tumor recurrence at two years.
Fig. 3.
Left: intraoperative image, Right: resected pathological specimen.
Fig. 4.
Histopathology image left: 10× magnification, right: 100× magnification showing tumor cells arranged in sheets.
Fig. 5.
PET scan without increased uptake.
3. Discussion
The clinical presentation of ACC depends on their size and hormonal status. Excess production of steroids, androgens, and estrogens is more prevalent than mineralocorticoid excess. The most common and easily identifiable presentation of functional adrenocortical carcinomas is steroid excess (56 %). Patients presenting with steroid excess typically exhibit the classic signs of Cushing's syndrome, which include truncal obesity, rounded facies, buffalo hump, striae, hypertension, glucose intolerance, thinning of the skin, and osteoporosis [9]. Likewise, our patient on her initial presentation had complaints of facial puffiness due to higher cortisol level and on representation had symptoms probably due to mass effect.
ACC has a high frequency of local or systemic recurrence therefore management of recurrence should be considered from the initial diagnosis. Challenge in management of ACC is quantifying the risk of recurrence [10]. Patients with high risk of recurrence, defined by tumor size >8 cm, microscopic invasion of blood vessel/tumor capsule or a Ki-67 index >10 %, should be offered adjuvant mitotane routinely and considered for radiotherapy to adrenal bed [5]. Our patient, stage III ACC with proliferative index (Ki 67): 35 % was advised and planned for adjuvant mitotane but she was lost to follow-up and eventually presented with symptoms of locoregional recurrence after a year of surgery. Previous studies have documented the use of mitotane in both primary and adjuvant therapy settings for ACC concluding that the effectiveness of adjuvant mitotane following complete resection of ACC remains uncertain and complete surgical excision is the best modality for long-term survival [11,12]. However, we cannot ascertain the early recurrence in our case was due to tumor characteristic itself and/or lack of adjuvant mitotane therapy.
Modalities of complete resection, debulking surgery and palliative radiotherapy have been proposed to treat locoregional recurrence [5]. Complete resection (Ro) if possible, for recurrent and metastatic disease has been linked to long-term survival and offers significant palliative benefits, particularly in cases involving symptomatic steroid production [12]. Our patient had isolated locoregional recurrence treated with en bloc excision of involved organs. This approach aligns with that of prior studies which suggested repeat surgery in carefully chosen patients can enhance survival outcomes for isolated locoregional recurrence [6].
In Nepal, the geographical distribution of tertiary care centers poses a significant challenge for comprehensive cancer management. The concentration of such facilities in the capital poses the difficulties in maintaining a seamless continuum of care. This case highlights the urgent need for improved multidisciplinary coordination among healthcare providers across different regions to enhance patient outcomes. In this scenario, the patient initially underwent surgery by the Department of Urosurgery at a tertiary care center located 120 km from her home. Subsequently, she was scheduled for adjuvant mitotane therapy at a regional hospital but was lost to follow-up. This lapse in continuous care might have led to a locoregional recurrence of her condition. Eventually, she was referred to our hospital's Department of Surgical Gastroenterology, where a team of gastro surgeons performed the necessary surgery.
4. Conclusion
ACC has high locoregional recurrence rate and Ro resection of the recurrence is the best potential treatment offering long term survival. It should be performed in a specialized center and should be under close follow up adherence with mitotane therapy. Ensuring robust follow-up and facilitating better integration between surgical, oncological, and supportive care departments are essential steps toward addressing these challenges in the Nepalese healthcare setting.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal upon request.
Disclosure
None.
Declaration of generative AI in scientific writing
Chat GPT 3.5 was used to improve readability and language; however, we assure that the authors are ultimately responsible for and accountable for the contents of the work.
Declaration
All the authors declare that the information provided here is accurate to the best of our knowledge.
Ethical approval
Since this is a case report, our Institutional Review Board of Institute of Medicine, Tribhuvan University has waived the requirement for ethical approval.
Funding
This study received no funding.
Author contribution
Conceptualization: Bikash Chandra Sah, Prajjwol Luitel, Sundar Shrestha, Mandesh Shrestha, Nirajan Subedi, Sharad Pokhrel.
Patient Management: Bikash Chandra Sah, Nirajan Subedi, Sharad Pokhrel.
Writing – original draft: Bikash Chandra Sah, Prajjwol Luitel, Sundar Shrestha, Mandesh Shrestha, Nirajan Subedi, Sharad Pokhrel.
Writing – review & editing: Bikash Chandra Sah, Prajjwol Luitel, Sundar Shrestha, Mandesh Shrestha, Nirajan Subedi, Sharad Pokhrel.
Visualization and Supervision: Bikash Chandra Sah, Prajjwol Luitel, Sundar Shrestha, Mandesh Shrestha, Nirajan Subedi, Sharad Pokhrel.
Guarantor
Prajjwol Luitel.
Research registration number
N/A.
Conflict of interest statement
No conflicts of interest were identified in the preparation of this case report.
Acknowledgements
None.
Data availability
The datasets used during this study will be available from the corresponding author upon reasonable request.
References
- 1.Datrice N.M., Langan R.C., Ripley R.T., et al. Operative management for recurrent and metastatic adrenocortical carcinoma. J. Surg. Oncol. 2012;105(7):709–713. doi: 10.1002/jso.23015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shariq O.A., McKenzie T.J. Adrenocortical carcinoma: current state of the art, ongoing controversies, and future directions in diagnosis and treatment. Ther. Adv. Chronic Dis. 2021 doi: 10.1177/20406223211033103. 12:20406223211033103. Published 2021 Jul 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kebebew E., Reiff E., Duh Q.Y., Clark O.H., McMillan A. Extent of disease at presentation and outcome for adrenocortical carcinoma: have we made progress? World J. Surg. 2006;30(5):872–878. doi: 10.1007/s00268-005-0329-x. [DOI] [PubMed] [Google Scholar]
- 4.Lam A.K. Update on adrenal tumours in 2017 World Health Organization (WHO) of endocrine tumours. Endocr. Pathol. 2017;28(3):213–227. doi: 10.1007/s12022-017-9484-5. [DOI] [PubMed] [Google Scholar]
- 5.Şişman P., Şahin A.B., Peynirci H., et al. Adrenocortical carcinoma: single center experience. Turk. J. Urol. 2017;43(4):462–469. doi: 10.5152/tud.2017.81598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glover A.R., Ip J.C., Zhao J.T., Soon P.S., Robinson B.G., Sidhu S.B. Current management options for recurrent adrenocortical carcinoma. Onco. Targets. Ther. 2013;6:635–643. doi: 10.2147/OTT.S34956. Published 2013 Jun 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paragliola R.M., Torino F., Papi G., Locantore P., Pontecorvi A., Corsello S.M. Role of Mitotane in adrenocortical carcinoma - review and state of the art. Eur. Endocrinol. 2018;14(2):62–66. doi: 10.17925/EE.2018.14.2.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sohrabi C., Mathew G., Maria N., et al. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. Published 2023 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sedlack A.J.H., Hatfield S.J., Kumar S., et al. Preclinical models of adrenocortical cancer. Cancers (Basel) 2023;15(11):2873. doi: 10.3390/cancers15112873. Published 2023 May 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schteingart D.E., Doherty G.M., Gauger P.G., et al. Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr. Relat. Cancer. 2005;12(3):667–680. doi: 10.1677/erc.1.01029. [DOI] [PubMed] [Google Scholar]
- 11.Al-Ward R., Zsembery C., Habra M.A. Adjuvant therapy in adrenocortical carcinoma: prognostic factors and treatment options. Endocr. Oncol. 2022;2(1) doi: 10.1530/EO-22-0050. R90-R101. Published 2022 Jul 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tran T.B., Maithel S.K., Pawlik T.M., et al. Clinical score predicting long-term survival after repeat resection for recurrent adrenocortical carcinoma. J. Am. Coll. Surg. 2016;223(6):794–803. doi: 10.1016/j.jamcollsurg.2016.08.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during this study will be available from the corresponding author upon reasonable request.