Version Changes
Revised. Amendments from Version 1
In this second version of the article, we have emphasized in the presentation of the case that it was a closed fracture of the thoraco-lumbar spine associated with dermabrasions on both lower limbs, thus supporting our theory of hematogenous infection. We also specified the method used to identify this bacterial species.
Abstract
Shewanella is an emerging human pathogen. It mostly causes skin and soft tissue infections. Osteosynthesis-associated infection involving Shewanella are rare and in most cases are secondary to direct contamination following open fractures in aquatic environments. Here, we present a rare case of hematogenous osteosynthesis-associated infection involving Shewanella algae affecting an 18-year-old patient who was operated on for 12 th thoracic vertebrae and 4th lumbar vertebrae fractures occurring in an aquatic environment. We performed surgical debridement with subsequent double course parenteral antibiotherapy that was then adapted to bacteria sensitivities for three weeks. After a follow-up of six months, the patient had no signs of recurrent infection. The presence of infected dermabrasions and the concordance between germs isolated in operative samples and in blood cultures presumes that the contamination was hematogenous.
Keywords: Shewanella, Osteosynthesis, Infection, Osteosynthesis-associated infection, Hematogenous
Background
Shewanella is an aquatic Gram-negative bacillus and is widely found throughout the environment. The most commonly reported clinical presentation is skin and soft tissue infection, 1 – 3 often preceded by exposure to seawater. 4 Bacteremia is often found in premature neonates with congenital pneumonia, patients with infections of the soft tissues of the lower limbs and with underlying health issues such as chemical esophagitis, cholangitis and liver abscess. 5 All the cases of osteosynthesis-associated infection involving Shewanella reported in the literature occurred after a direct contamination following open fractures, most often in aquatic environments. 6 – 9 We report the first case of osteosynthesis-associated infection caused by Shewanella algae via haemathogenic route.
Case presentation
An 18-year-old patient with no previous medical history of note was admitted to the intensive care unit after he fell into a well resulting in polytrauma. In addition to head and thoracic injuries, the whole body CT revealed a burst fracture of 12 th thoracic vertebra with section of the spinal cord and complete paraplegia, burst fracture of 4 th lumbar vertebra ( Figure 1). Both fractures were closed. In cutaneous clinical examination we found multiple water-soiled dermabrasions in both legs.
Figure 1. CT scan showing a burst fracture of 12 th thoracic vertebra and the 4 th lumbar vertebra.

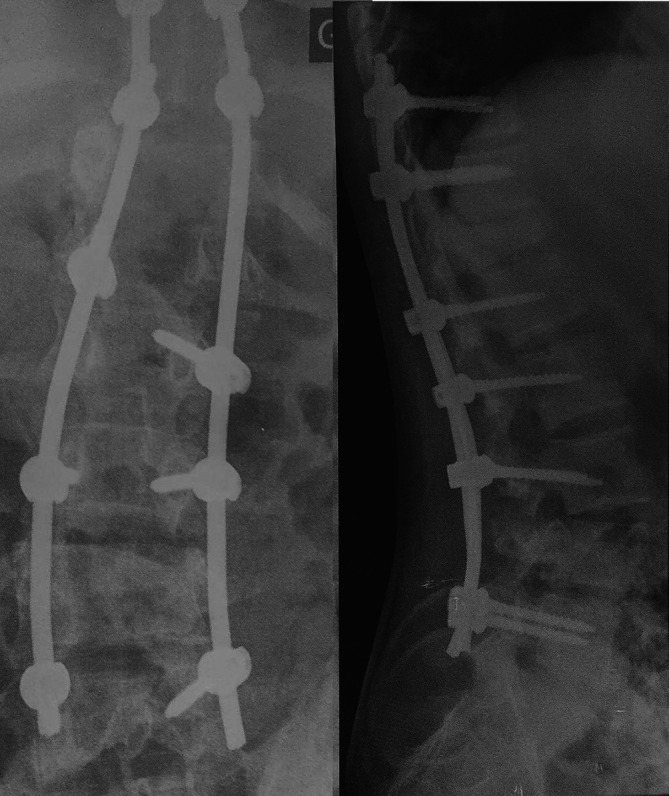
He was operated on in the orthopaedic surgery department, and postero-lateral fusion was performed from the 10 th thoracic vertebra to the 5 th lumbar vertebra ( Figure 2).
Figure 2. Postoperative anteroposterior and profile radiography of the T10-L5 postero-lateral fusion.
At the 10 th post-operative day the patient presented fever (39.5°C), redness and swelling around the surgical wound with serous discharge ( Figure 3). Dermabrasions in lower limbs were infected. The vital signs included blood pressure, 120/60 mm Hg (NR: ≥ 90/60 mm Hg); respiration, 20 breaths per minute (NR: 12–18 breaths per minute); pulse, 95 beats per minute (NR: 60–100 beats per minute). Investigations showed a high white cell count (17.6 × 10 9/L) (NR: 4.5–11 × 10 9/L) and a raised C-reactive protein (176 mg/L) (NR: <0.3 mg/L). Three blood cultures were performed.
Figure 3. A clinical photograph of the surgical wound showing inflammatory signs with serous discharge.

The patient was reoperated on the 11 th post-operative day. Intraoperatively, we found abundant pus with infected necrotic tissues that were then cleaned and debrided. We took five deep bacteriological samples. The operative wound was closed on aspiratifs Redon drain. One of the blood cultures became positive, Gram staining performed from culture showed Gram-negative rods. They were identified as Shewenella algae by vitek 2. Intraoperative deep tissue specimens grew Shewanella algae and Klebsiella pneumoniae. Shewanella algae was resistant to amoxicillin, amoxicillin-clavulanic acid and levofloxacin, had intermediate susceptibility to trimethoprim-sulfamethoxazole and was sensitive to imipenem/cilastatin. Klebsiella pneumoniae was multi-resistant and was only sensitive to colistin. The patient had a double course of parenteral antibiotics (Imipenem/cilastatin at a dose of 500/500 mg/6 hours and colistin at a dose of 3 MUI/8 hours) for 25 days. The patient had minor adverse events such as epigastralgia and vomiting, which resolved with symptomatic treatment.
After three weeks of antibiotics, white cell count and C-reactive protein normalized. The surgical wound healed with no fistula. The patient was addressed to physical medicine and rehabilitation department. At eight months follow-up, the patient had no signs of recurrent infection.
Discussion
Shewanella has been regarded as an uncommon source of human infection. Despite being identified more than 70 years ago, 1 our understanding of the bacterium’s spread and the symptoms it causes comes primarily from a restricted set of individual case studies. Predominantly concentrated in tropical regions, the highest frequency of occurrences is noted within Southeast Asia, Southern Europe, and Africa. 10 They naturally exist in various environments like water of all types, raw fish, oily food, and soils. 2 , 5 Human infections involve Shewanella algae, putrefaciens, halitosis, and xiamenensis. However, the more offending species are Shewanella algae and putrefaciens accounting for more than 80% of cases. 1 Shewanella infections can be serious leading to life-threatening conditions such as necrotizing fasciitis and septic shock. 11 – 14 The route of infection is more likely cutaneous (wounds, leg ulcers, etc.), and, less frequently hepatobiliary or respiratory. 15 Malignancy, hepatobiliary disease, diabetes, immunodepression, dysregulated iron metabolism and chronic infections of lower limb have been reported to be risk factors for developing a Shewanella infection. 1 , 2 , 15 – 17 Although the patient received routine preoperative antibioprophylaxis based on 2 g of cefazolin and had no medical history, he developed infection.
In this case, Klebsiella pneumoniae was co-isolated in deep bacteriological samples. In fact, Shewanella algae are frequently identified in polymicrobial infections and the most common bacterial strains co-isolated are Enterobacteriaceae and marine flora bacteria. 2
Cases of osteosynthesis-associated infection caused by Shewanella are rare. In our review of the literature, all cases were secondary to open fractures of lower limbs occurring in an aquatic environment. 6 , 8 , 9 , 18 To the best of our knowledge, this is the first case in which osteosynthesis implant contamination was secondary to bacteremia. Shewanella algae have a significant ability to haematogenous diffusion. Indeed, Vignier 9 and Yousfi 19 observed that bacteremia occurred in respectively 28% and 18% of the cases they studied. Mortality rates were respectively 13 and eight per cent. Bacteremia can lead to severe secondary infection including instances of epidural spinal abscess, purulent pericarditis, acute gastroenteritis accompanied by bloody diarrhea, and meningoencephalitis, as reported in various studies. 20 – 23 The concordance between germs isolated in operative samples and in blood cultures presumes that the contamination was haematogenous, probably originating from infected dermabrasions in both legs.
As in other cases of osteosynthesis-associated infection reported in the literature, we performed surgical debridement with subsequent double course parenteral antibiotherapy that was then adapted to bacteria sensitivities. Colistin was selected because it was the only effective antibiotic against Klebsiella pneumonae. Imipenem/cilastatin was the only antibiotic available in the hospital to which Shewanella was sensitive. Typically, Shewanella displays susceptibility to erythromycin, fluoroquinolones, chloramphenicol, third and fourth generation cephalosporins, aminoglycosides, carbapenems, and to some degree, trimethoprim-sulfamethoxazole and tetracyclines. However, it exhibits resistance against first and second generation cephalosporins, penicillin, and colistin. 24 An emergence of resistance has been documented towards imipenem and piperacillin/tazobactam, which can be attributed to the presence of the class D beta-lactamase enzyme. 23 Hopefully, our microbial stain was sensitive to imipenem/cilastatin.
Currently, there are no established guidelines for the management of shewanella infections. However, certain reports have indicated that addressing Shewanella infections may necessitate a proactive approach involving both surgical debridement and administration of appropriate antimicrobial agents. This particular case underscores the importance of recognizing Shewanella algae as a potential offending pathogen in osteosynthesis-associated infection coming within the framework of secondary hematogenous infection even in patients without significant underlying medical conditions.
Consent
Written informed consent for publication of clinical details and clinical images was obtained from the patient.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; peer review: 2 approved]
Data availability
All data underlying the results are available as part of the article and no additional source data are required.
References
- 1. Holt HM, Gahrn-Hansen B, Bruun B: Shewanella algae and Shewanella putrefaciens: clinical and microbiological characteristics. Clin. Microbiol. Infect. 2005;11:347–352. 10.1111/j.1469-0691.2005.01108.x [DOI] [PubMed] [Google Scholar]
- 2. Chen YS, Liu YC, Yen MY, et al. : Skin and soft-tissue manifestations of Shewanella putrefaciens infection. Clin. Infect. Dis. 1997;25:225–229. 10.1086/514537 [DOI] [PubMed] [Google Scholar]
- 3. Tsai M-S, You H-L, Tang Y-F, et al. : Shewanella soft tissue infection: case report and literature review. Int. J. Infect. Dis. 2008;12:e119–e124. 10.1016/j.ijid.2008.03.020 [DOI] [PubMed] [Google Scholar]
- 4. Holt HM, Søgaard P, Gahrn-Hansen B: Ear infections with Shewanella alga: a bacteriologic, clinical and epidemiologic study of 67 cases. Clin. Microbiol. Infect. 1997;3:329–334. 10.1111/j.1469-0691.1997.tb00622.x [DOI] [PubMed] [Google Scholar]
- 5. Brink AJ, Straten A, Rensburg AJ: Shewanella (Pseudomonas) putrefaciens Bacteremia. Clin. Infect. Dis. 1995;20:1327–1332. 10.1093/clinids/20.5.1327 [DOI] [PubMed] [Google Scholar]
- 6. Prinja A, Singh J, Davis N, et al. : A rare cause of wound infection after an open fracture: Shewanella putrefaciens. Case Rep. 2013;2013:bcr2012008537–bcr2012008537. 10.1136/bcr-2012-008537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Prischl C, Bendtsen MM, Laursen M: Shewanella algae-infektion efter kirurgisk behandling af Haglunds deformitet og akillesseneruptur. n.d..
- 8. Lee GC, Lee J-Y, Kim D-M, et al. : A Fatal Shewanella algae Infection After an Open Tibial Fracture Following a Tropical Storm: A Case Report. JBJS Case Connect. 2013;3:e92. 10.2106/JBJS.CC.M.00062 [DOI] [PubMed] [Google Scholar]
- 9. Vignier N, Théodose R, Barreau M, et al. : Human Infection with Shewanella putrefaciens and S. algae: Report of 16 Cases in Martinique and Review of the Literature. Am. J. Trop. Med. Hyg. 2013;89:151–156. 10.4269/ajtmh.13-0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Finkelstein R, Oren I: Soft Tissue Infections Caused by Marine Bacterial Pathogens: Epidemiology, Diagnosis, and Management. Curr. Infect. Dis. Rep. 2011;13:470–477. 10.1007/s11908-011-0199-3 [DOI] [PubMed] [Google Scholar]
- 11. Giroux P-A, Sinna R, Mercut R, et al. : Shewanella putrefaciens necrotizing fasciitis of the lower limb. Med. Mal. Infect. 2017;47:436–438. 10.1016/j.medmal.2017.06.005 [DOI] [PubMed] [Google Scholar]
- 12. Ananth AL, Nassiri N, Pamoukian VN: Shewanella algae: A Rare Cause of Necrotizing Fasciitis. Surg. Infect. 2014;15:336–338. 10.1089/sur.2012.208 [DOI] [PubMed] [Google Scholar]
- 13. Brugnaro P, Morelli E, Ebo F, et al. : The first Italian case report of leg ulcer and sepsis caused by Shewanella algae in a immunocompetent patient. n.d.. [PubMed]
- 14. Latif A, Kapoor V, Vivekanandan R, et al. : A rare case of Shewanella septicemia: risk factors, environmental associations and management. BMJ Case Rep. 2019;12:e230252. 10.1136/bcr-2019-230252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. To KKW, Wong SSY, Cheng VCC, et al. : Epidemiology and clinical features of Shewanella infection over an eight-year period. Scand. J. Infect. Dis. 2010;42:757–762. 10.3109/00365548.2010.490562 [DOI] [PubMed] [Google Scholar]
- 16. Pagani L, Lang A, Vedovelli C, et al. : Soft Tissue Infection and Bacteremia Caused by Shewanella putrefaciens. J. Clin. Microbiol. 2003;41:2240–2241. 10.1128/JCM.41.5.2240-2241.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Takata T, Chikumi H, Morishita S, et al. : Shewanella algae Bacteremia in an End-stage Renal Disease Patient: A Case Report and Review of the Literature. Intern. Med. 2017;56:729–732. 10.2169/internalmedicine.56.7616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smith JRO, Morgan M, Palmer JH: Shewanella algae infection complicating an open lower limb fracture. J. Plast. Reconstr. Aesthet. Surg. 2014;67:e99–e100. 10.1016/j.bjps.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 19. Yousfi K, Bekal S, Usongo V, et al. : Current trends of human infections and antibiotic resistance of the genus Shewanella. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36:1353–1362. 10.1007/s10096-017-2962-3 [DOI] [PubMed] [Google Scholar]
- 20. Tan C-K, Lai C-C, Kuar W-K, et al. : Purulent Pericarditis with Greenish Pericardial Effusion Caused by Shewanella algae. J. Clin. Microbiol. 2008;46:2817–2819. 10.1128/JCM.01018-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dey S, Bhattacharya D, Roy S, et al. : Shewanella algae in acute gastroenteritis. Indian J. Med. Microbiol. 2015;33:172–175. 10.4103/0255-0857.148442 [DOI] [PubMed] [Google Scholar]
- 22. Brulliard C, Traversier N, Allyn J, et al. : Case Report: Disseminated Shewanella algae Infection with Meningoencephalitis in a Traveler Secondary to Marine Injury in Madagascar. Am. J. Trop. Med. Hyg. 2017;97:1043–1044. 10.4269/ajtmh.17-0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim D-M, Kang C-I, Lee CS, et al. : Treatment Failure Due to Emergence of Resistance to Carbapenem during Therapy for Shewanella algae Bacteremia. J. Clin. Microbiol. 2006;44:1172–1174. 10.1128/jcm.44.3.1172-1174.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cimmino T, Olaitan AO, Rolain J-M: Whole genome sequence to decipher the resistome of Shewanella algae, a multidrug-resistant bacterium responsible for pneumonia, Marseille, France. Expert Rev. Anti-Infect. Ther. 2016;14:269–275. 10.1586/14787210.2016.1106936 [DOI] [PubMed] [Google Scholar]


