Abstract
Purpose
To undertake a global assessment of existing ultrasound practices, barriers to access, point-of-care ultrasound (POCUS) training pathways, and the perceived clinical utility of POCUS in Child Surgery.
Methods
An electronic survey was disseminated via the GICS (Global Initiative of Children’s Surgery) network. 247 anonymized responses from 48 countries were collated. 71.3% (176/247) worked in child surgery.
Results
Ultrasound was critical to practice with 84% (147/176) of requesting one daily or multiple times per week. Only 10% (17/176) could access emergency ultrasound < 1 h from request. The main barrier was a lack of trained personnel. HIC surgeons were more likely to have ultrasound training (24/29; 82.8%) compared with LMICs (74/147; 50.3%) (p = .001319; CI 95%). Self-perceived POCUS competence was associated with regularity of POCUS use (p < 0.001; CI 95%). Those who already practice POCUS most commonly use it for trauma, intussusception, and ultrasound-guided procedures. Majority (90%; 159/176) of child surgeons would attend formal POCUS training if available.
Conclusions
Ultrasound is critically important in children’s surgery globally, however, many surgeons experience barriers to timely access. There is a strong interest in learning POCUS for relevant pediatric surgical applications. Further research is needed to evaluate the best methods of training, accreditation, and governance.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00383-024-05797-8.
Keywords: POCUS, Point-of-care ultrasound, Pediatric surgery, Bedside ultrasound, Clinical ultrasound
Introduction
Point-of-care ultrasound (POCUS) or ‘clinician-led’ ultrasound refers to the use of ultrasound by non-radiologist clinicians at the patient’s bedside. Although for many years ultrasound has been the domain of radiologists and specialist sonographers, several critical developments have occurred that have altered the clinical landscape. Technological advances have facilitated the development of cheaper and increasingly smaller handheld devices that interface wirelessly with most screens [1]. The user-friendliness of ultrasound devices in part has contributed to the rapid expansion of POCUS into almost all areas of clinical medicine [2–7]. The specialists who have led the way include Emergency Physicians and Intensivists who have developed POCUS curricula, courses, and accredited training programs for their respective fields [8–10]. The value of POCUS to Anesthesia through facilitating vascular access, cardiovascular monitoring, and guiding regional anesthesia has also been demonstrated [8, 11]. Similarly, acute gynecological presentations and obstetric care have utilized POCUS in their diagnostic algorithms and have a large body of evidence to support its use [5, 12].
The field of Pediatric Surgery could stand to benefit from this technology, given the large proportion of pathologies amenable to ultrasound diagnosis, the conducive body habitus of children, and the importance of avoiding exposure to ionizing radiation. In emergency medicine in particular, many studies have shown equivalent diagnostic accuracy when emergency physicians have been trained to diagnose appendicitis, intussusception, and pyloric stenosis [13–15]. While there is evidence of some pediatric surgeons practicing POCUS in Europe [6], and sporadic reports from other regions [14, 16–19]; overall there is a paucity of published data regarding current POCUS practices in pediatric surgery worldwide.
While the majority of POCUS published literature exists in high-income countries (HICs), theoretically low-resourced healthcare settings also stand to benefit from the ‘task shifting’ and ‘capacity-building’ advantages POCUS offers. A particular challenge in LMICs is a critical lack of radiologists. Of 26 HICs evaluated, the average number of radiologists is 100 per million population [20–24]. Compared with studies evaluating countries in Africa, where the estimated number of radiologists is between 6.5 and 12 per million [20–24]. The practice of pediatric radiology is especially neglected, with only 4 of 54 countries in Africa offering sub-specialization in pediatric radiology (Ethiopia, Nigeria, South Africa, Tunisia) [25].
Using just one example, intussusception is a common emergency pediatric surgical condition for which there is a significant disparity in outcomes between high and low-income countries [26]. In LMICs, the mortality rate is greater than 10%, compared with < 0.2% in HICs [26]. The diagnosis of intussusception is time-critical and hinges on ultrasound use. Ultrasound can also be used to guide hydrostatic or pneumatic reduction in the treatment of intussusception. Focusing on even this single condition, there is the potential to help improve diagnostic and referral pathways for children with intussusception in LMICs through more ubiquitous access to ultrasound skills for clinicians.
Given the lack of data regarding POCUS use in children’s surgery, we developed a global survey to evaluate existing practices, barriers to ultrasound access, training pathways, and the perceived utility of POCUS in our field.
Methods
Following approval by the Global Initiative of Children’s Surgery (GICS) an electronic survey was disseminated via the GICS network and associated social media webpages in English language. Components of the survey were developed by pediatric surgeons with POCUS expertise. The term ‘POCUS’ was defined as the use of ultrasound by a (non-radiologist/non-sonographer) clinician in the assessment or treatment of a patient.
The survey assessed 4 areas:
Domain 1: Demographics—information about the respondent’s role and country of practice.
Domain 2: Ultrasound Services—information regarding ultrasound services, infrastructure, and barriers to access at the respondent’s institution.
Domain 3: POCUS Training – respondent’s experience of POCUS training (or lack thereof) and utilization of POCUS skills in their current clinical practice.
Domain 4: POCUS Applications – assessment of the respondent’s views on the clinical relevance of potential POCUS uses (‘applications’).
Twenty two potential POCUS applications were selected based on common pediatric conditions amenable to ultrasound diagnosis and the current use of POCUS in children’s healthcare as described in the literature. The survey was closed after 12 months. All responses were anonymous, and all respondents gave consent for publication of the survey findings.
There were 247 responses to the survey. These were collated in a secure electronic database. Of the 247 responders, 176 ([71.3%) were child surgeons; the remaining 71 worked in medical specialties. ‘Child surgeons’ were defined as those who identified as having specialized in ‘Pediatric Surgery’ or were from a different surgical specialty (i.e. general surgery, orthopedics, etc.) but routinely cared for children. Responses were compared between LMICs and HICs. Descriptive statistics were performed and chi-squared tests for statistical significance were used for categorical data. Statistical significance is indicated if p < 0.05 with a 95% confidence interval (CI).
Results
Domain 1—demographics
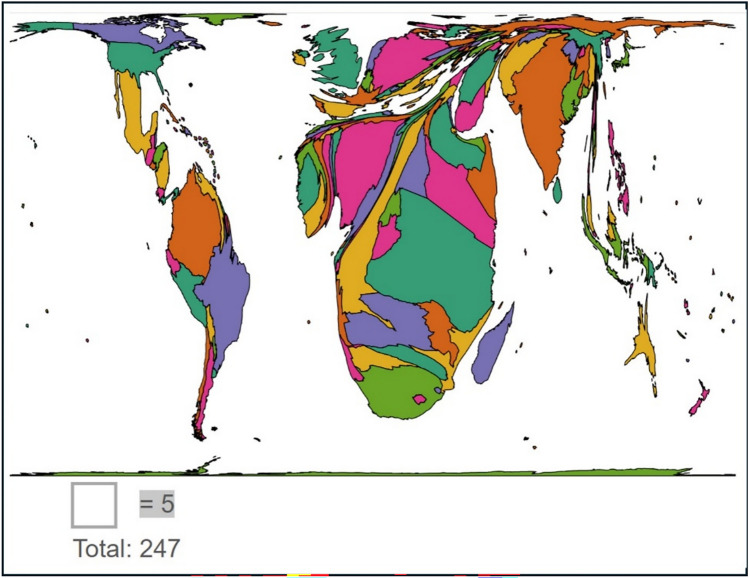
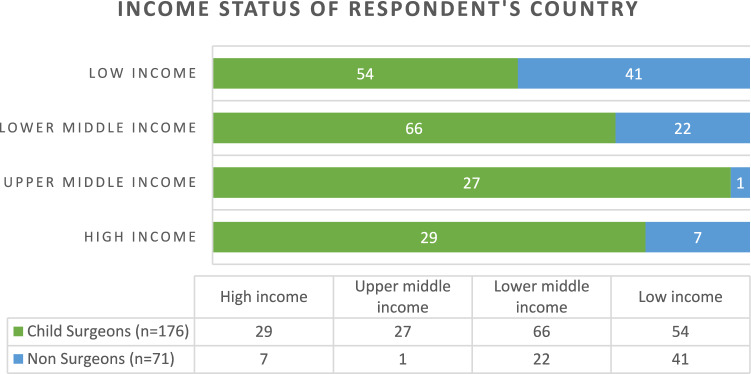
A total of 247 responses from 48 countries were received (additional data on a number of responses per country are given in Online Resource 1). These represented the continents of Africa, Asia, Europe, North and South America (Fig. 1). Countries were grouped by income level according to their official classification in the World Bank List of Economies [27] (Fig. 2). Most respondents were from LMICS 85.4% (211/247), with 14.6% (36/247) responses from HICs. Of the 176/247 child surgeons (n = 176), there was an almost equal split between consultant/attending level doctors 52.8% (93/176) and trainees/clinical officers 47.2% (83/176). Child surgeons predominantly worked in tertiary level institutions 83% (145/176); compared with secondary level 16% (28/176); and only 1% (3/176) from primary level healthcare facilities.
Fig. 1.
Cartogram showing the proportion of survey responses from different countries (Go-Cart program used to create cartogram)
Fig. 2.
Number of responses according to the income level of the country as defined by the Work Bank
Surgeons (n = 176) were mainly specialists in Pediatric Surgery 63% (110/176) or General Surgery 29% (30/176). The remaining responses were from 5 other surgical specialties (Fig. 3). All respondents routinely assessed or operated on children.
Fig. 3.
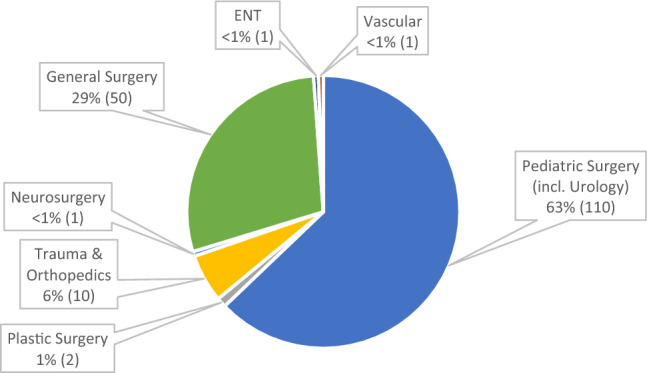
Breakdown of Child Surgeons specialties (n = 176)
Domain 2 – ultrasound services
We evaluated the availability of clinical investigations and ultrasound practices at the respondent’s hospital (Table 1). All had blood tests and ultrasound devices available at their institution (176/176). Cross-sectional imaging was available in all HIC settings (29/29) but only available in 65% (96/147) of LMICs. In terms of ‘normal’ ultrasound practices, in most respondent’s institutions ultrasound was typically performed by radiologists (or specialist sonographers) 64% (112/176). However, in almost a quarter of responses 24% (43/176), clinicians were the primary ultrasound operator, not radiologists. An equal mix of radiologists and clinician-led ultrasound was found in 11% (20/176). One respondent had access to ultrasound devices but no trained personnel to perform the skill. There was no statistically significant difference between LMICs and HICs in terms of who the principal ultrasound user was (P > 0.05; CI 95%).
Table 1.
Ultrasound infrastructure and access at the respondent’s institution
| Total (n = 176) | HIC (n = 29) | LMIC (n = 147) | |
|---|---|---|---|
| Available Investigations | |||
| Blood tests | 100% (176) | 100% (29) | 100% (147) |
| Radiographs | 100% (176) | 100% (29) | 100% (147) |
| Ultrasound device/s | 100% (176) | 100% (29) | 100% (147) |
| Cross-sectional imaging | 71% (125) | 100% (29) | 65% (96) |
| Who normally performs ultrasound? | |||
| Radiologist/sonographer only | 64% (112) | 48% (14) | 67% (98) |
| Non-radiologist (doctor or clinical officer) only | 24% (43) | 7% (2) | 12% (18) |
| Mix of both | 11% (20) | 45% (13) | 20% (30) |
| No ultrasound users available | < 1% (1) | 0% (0) | < 1% (1) |
| How often do you request an ultrasound? | |||
| Almost daily | 52% (91) | 55% (16) | 51% (75) |
| Multiple times per week | 32% (56) | 24% (7) | 33% (49) |
| Multiple times per month | 9% (15) | 3% (1) | 10% (14) |
| Rarely/never | 7% (12) | 7% (2) | 4% (6) |
| N/A | < 1% (1) | 7% (2) | 1% (2) |
| No response | < 1% (1) | 3% (1) | 0% (0) |
| Time to ultrasound from request? *(Radiology Department) | |||
| < 1 h | 10% (17) | 10% (3) | 10% (14) |
| 1–6 h | 52% (92) | 59% (17) | 51% (75) |
| 6–12 h | 13% (23) | 10% (3) | 14% (20) |
| 12–24 h | 9% (16) | 10% (3) | 9% (13) |
| > 24 h | 10% (17) | 0% (0) | 12% (17) |
| No guarantee it will be done | 5% (8) | 3% (1) | 5% (7) |
| No radiology department | < 1% (1) | 0% (0) | < 1% (1) |
| No response | 1% (2) | 7% (2) | 0% (0) |
In the clinical practice of child surgeons, ultrasound was a commonly used investigation, with 84% (147/176) requesting an ultrasound for a child either daily or multiple times per week—with no significant difference between LMIC and HIC groups (p > 0.05; CI 95%). In terms of ‘out of hours’ access to radiology-performed ultrasound, 19% (34/176) had no access, while 63% (111/176) could access these services but only in an emergency. We assessed the time for an emergency ultrasound from the request for an acute indication. In only 10% (17/176) of cases would emergency ultrasound be reliably performed < 1 h from request. For 40% (58/147) of LMIC respondents, an emergency ultrasound took more than 6 h to be performed; with 14% of these beyond 24 h from request (Table 1). No significant differences between LMIC and HIC were found across time intervals (p > 0.05).
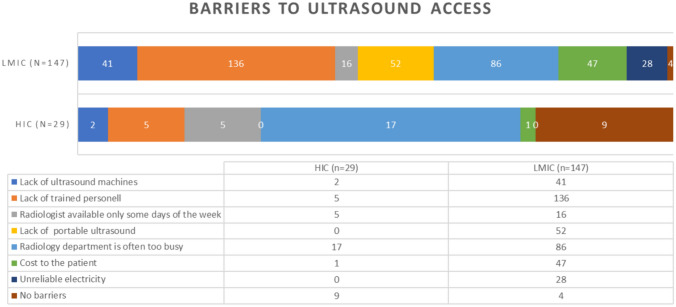
We also investigated barriers to ultrasound access that child surgeons encountered at their hospital (Fig. 4). A lack of ultrasound-trained personnel and the workload of the radiology department were the commonest issues. In LMICs compared with HICs the following barriers were found to be statistically significant (CI 95%) – lack of machines (p = 0.0162); lack of trained personnel (p = 0.0001); lack of portable machines (p = 0.0001); cost to the patient (p = 0.0016); reliability of electricity source (p = 0.0016). HICS were more likely to have no barriers (p = 0.0001).
Fig. 4.
Barriers to ultrasound access described by respondent
Domain 3—ultrasound training
We asked respondents about their experience of ultrasound training, competence levels, and use of POCUS in their clinical management of children (Table 2). Approximately half of all respondents had received some kind of informal or formal ultrasound training (55%; 98/176). HIC surgeons were statistically more likely to be trained 24/29 (82.8%) compared with LMIC surgeons 74/147 (50.3%) (p = 0.001319; CI 95%). Of those who had received training (n = 98), most 46% (45/98) felt they had basic ultrasound competence; and almost half 47% (46/98) used POCUS daily or weekly in their practice. Self-perceived competence was associated with where the child surgeon used POCUS regularly in their clinical practice (p < 0.001; CI 95%). There were high levels of interest in attending a POCUS training course designed specifically for child surgeons, with 90% (159/176) saying they would be interested in attending such a course; 4% (7/176) had no interest; and 6% were unsure—no difference between LMIC and HIC groups (p > 0.05; CI 95%).
Table 2.
Child surgeons (n = 176) experience of POCUS training, self-perceived competency, and clinical
| POCUS Training | |
|---|---|
| Have you ever had any ultrasound training? (n = 176) | |
| No, I have never been trained | 44% (78) |
| Yes, I attended a training course | 27% (48) |
| Yes, I received informal training from colleagues | 28% (50) |
| If you have received training, how competent do you feel using ultrasound to assess patients? (n = 98) | |
| I do not feel competent | 32% (31) |
| I feel I have basic competence | 46% (45) |
| I feel competent and can teach others | 18% (18) |
| Non-response | 4% (4) |
| If you have received training, how often do you personally perform ultrasound on your patients? (n = 98) | |
| Daily | 26% (25) |
| At least once per week | 21% (21) |
| At least once per month | 24% (23) |
| Never | 25% (24) |
| Non-response | 5% (5) |
Domain 4—POCUS applications
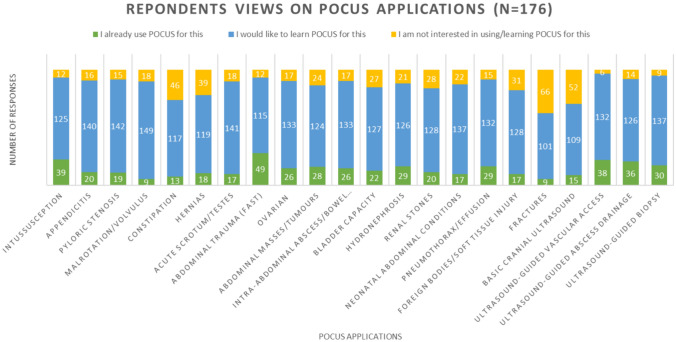
Respondents were asked to identify which of 22 potential POCUS applications they either already used POCUS for, would be interested in learning to use POCUS for, or had no interest in (Fig. 5). The top five most common uses of POCUS amongst child surgeons (n = 176) were FAST (focused assessment with sonography for trauma), intussusception, ultrasound-guided procedures, hydronephrosis, and pneumothorax detection. However, the most common applications respondents wanted to learn POCUS for were malrotation, pyloric stenosis, acute scrotum, appendicitis, and assessing the neonatal abdomen. The least useful applications included fractures, cranial ultrasound, constipation, hernias, and foreign bodies/soft tissue injury. Overall, there were high rates of interest in learning all of the 22 potential applications for POCUS, with a nadir of 57% (101/176) for fractures.
Fig. 5.
Response regarding applications of pocus, evaluating if respondents already used POCUS for this purpose or were interested or not interested in being trained to use POCUS for a particular condition/procedure
Discussion
Within the pediatric global health community, there is increasing recognition of the magnitude of the burden of surgical disease particularly in LMICs where almost half the population are children [26, 28]. The Lancet Commission on Global Surgery 2015 has been instrumental in defining this problem and highlights issues such as lack of diagnostics as contributory factors, and imploring solutions that are interdisciplinary, innovative, and technology-enabled [28]. Additionally, one of the biggest challenges LMICs face in healthcare provision is the low ratio of doctors per capita compared with HICs [29]. To help address this, the global health community has endorsed ‘task shifting’ in many clinical areas [30–32]. Given the critical lack of pediatric radiologists in many low-income settings [20], there is a strong rationale for ‘task-shifting’ some of the most basic ultrasound applications to doctors and surgeons. This is the first study to attempt to delineate global practices and the views of child surgeons on the value of POCUS to children’s surgical care.
Ultrasound use in child surgery
Our findings describe current norms and experiences of child surgeons concerning access to ultrasound services at their institution and the use of POCUS. We demonstrate that ultrasound in pediatric surgical care is critical in all settings, with child surgeons heavily reliant on this mode of imaging in their daily clinical practice (Table 1). Across both HIC and LMIC settings, the primary user of ultrasound (64%) was typically a radiologist or sonographer, as would be traditional. However, in almost a quarter of institutions surveyed, it was the norm for ultrasound to be clinician-led (POCUS) (Table 1). While the reason for this is unclear, it could reflect the general rise in POCUS use across the medical community in recent decades and an evolving status quo [33].
Barriers
We also evaluated how easy it was for surgeons in their place of work to access traditional ultrasound services, with the majority (93%; 154/167) reporting some difficulty. The main barrier reported was not a lack of devices but rather a lack of ultrasound-skilled personnel (Fig. 4). Secondary to this was the workload pressure on local radiology departments (Fig. 4). Only 10% of respondents could reliably access emergency ultrasound within an hour from the time of request (Table 1). Our findings, therefore, demonstrate that the demand for ultrasound services in child surgery appears to outstrip the supply of trained ultrasound users. In LMIC institutions a significant additional barrier included the cost of ultrasound scans to families. In many institutions access to care requires payment ‘upfront’ which may render certain investigations inaccessible to poorer families. Equipping surgeons with POCUS skills to diagnose simple common pediatric conditions could help not only reduce the time to diagnosis and treatment of children but also improve the affordability of care.
Cultural sensitivity
We asked respondents to describe (in free text) any other issues they experienced with POCUS use in their setting. A HIC respondent described that their radiology department was “unwilling for anyone else to do ultrasound”. In some regions (i.e. Europe/North America), such issues have been formally addressed through directives and guidance from Radiology associations that have published their endorsement of POCUS and encourage radiologists to support doctors who which to integrate it into their practice [34, 35]. A further consideration highlighted by our survey is region-specific cultural barriers to clinician-led ultrasound. A respondent working in India described that the regulation of ultrasound was stringent because of concerns over prenatal sex selection [36, 37]. In their setting, it was not advisable for surgeons outside of large training institutes to venture into ultrasound practice for this reason. It is important, therefore, that POCUS initiatives developed for surgeons must be contextually appropriate and sensitive to local culture. Ideally, a collaborative approach should be taken in developing POCUS programs, through proactive engagement with local radiology services and relevant governance bodies [9, 10, 34, 38, 39].
Training
Our study indicates that most child surgeons (90%;159/176) would engage in formal POCUS training if a program with relevant content was made available. While a considerable proportion of surgeons already have some degree of ultrasound training, most have developed their skills informally. For those with training (formal or informal), the majority continued to practice their skills on a routine basis. However, we found that their perception of competence was associated with how frequently they practiced POCUS. Those who felt competent were more likely to use it regularly compared with those who did not. This finding is in keeping with published literature on POCUS training that emphasizes the importance of longitudinal training programs which over time build both competence and confidence in learners. This can be achieved through mentor-led learning and the use of simulation technology [40–42]. The latter, however, could be inaccessible to LMIC learners due to the large expense of current simulators. To better support LMIC POCUS learners there is a need to develop low-cost simulation technology.
POCUS Applications
Our evaluation of clinical applications of POCUS found that surgeons who already practice POCUS most commonly use it for trauma (FAST), intussusception, and ultrasound-guided procedures. This is consistent with published reports of the most common protocolized uses of POCUS relevant to our specialty [43–46]. While respondents had high rates of interest in learning all 22 potential applications, the most valued were the diagnosis of malrotation/volvulus, pyloric stenosis, and acute scrotum. The accepted ‘gold standard’ for diagnosis of malrotation is fluoroscopy, with the role of ultrasound still under debate [47]. The interest shown in learning POCUS to diagnose malrotation (with or without volvulus) may represent a lack of access to fluoroscopy services in many respondents’ institutions. However, the evidence for the role of ultrasound is growing. The largest published meta-analysis of the diagnostic accuracy of ultrasound in malrotation/volvulus indicates the superiority of ultrasound which has a sensitivity of 94% (range 89% 97%; 95% CI) and specificity of 100% (range 97%-100%; 95% CI); compared with fluoroscopy sensitivity 91% (range 84%-96%; 95% CI) and specificity 94% (range 72% -99%; 95% CI) [47]. However, it does not account for the individual ultrasound user's accrued experience and expertise which could impact diagnostic accuracy. The interest in learning POCUS for pyloric stenosis and the acute scrotum may be due to the frequency with which pediatric surgeons manage these conditions, where diagnostic uncertainty may lead to delayed care or negative operative findings. A curriculum that aims to accredit child surgeons with POCUS competencies should aim to distinguish between ‘basic’ and ‘advanced’ applications so that they are feasible and safe to teach.
Limitations
We acknowledge several limitations to this study. As with many surveys, there is likely to be a degree of selection bias given respondents, may be those who already have an interest in POCUS. The survey was circulated in the English language, which could have deterred non-English speakers from responding. However, of the 48 countries represented only 17 of these have English as an official language: with less than half 42% [103/247] of respondents working in an English-speaking country. Due to the low proportional response rate per country (range 1–17 responses per country), we cannot infer country-wide views on POCUS, our data instead likely reflects individual clinician views albeit within the area of child surgery.
Conclusion
Our findings demonstrate the critical importance of ultrasound as a diagnostic tool in children’s surgery globally. Despite this, many child surgeons experience significant barriers to timely access to local ultrasound services for their patients. While approximately half of the respondents had some form of ultrasound training, the continued use of their skills was associated with self-perceived competence. Overall, we found high levels of interest amongst child surgeons in learning POCUS for relevant pediatric surgical applications. Training child surgeons in basic applications of POCUS could serve to improve access to diagnostics and reduce time to definitive care for children. Central to this intervention is linking this skill (POCUS) to the surgical care provider, thereby reinforcing the crucial link between the imaging and clinical findings. Further research is needed to evaluate the best training methods, mentorship, accreditation, and governance mechanisms for child surgeons learning POCUS.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the Global Initiative for Children’s Surgery (GICS) for supporting this work by circulating this survey to its members.
Author contribution
GN—conceptualization, survey tool development, methodology, data analysis & write-up. MS—survey tool development, survey dissemination, review & edit of the manuscript. AJ—survey tool development, survey dissemination, review & edit of the manuscript. AH—supervision of the work including review & edit of the manuscript. KL— supervision of the work including survey tool development, survey dissemination, & contribution to the manuscript. JL—conceptualization, survey tool development, methodology, survey dissemination, data analysis, write up, review & edit of manuscript.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baribeau Y, Sharkey A, Chaudhary O, Krumm S, Fatima H, Mahmood F et al (2020) Handheld Point-of-Care Ultrasound Probes: the new generation of POCUS. J Cardiothorac Vasc Anesth 34(11):3139–3145. 10.1053/j.jvca.2020.07.004 10.1053/j.jvca.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raimondi F, Yousef N, Migliaro F, Capasso L, De Luca D (2021) Point-of-care lung ultrasound in neonatology: classification into descriptive and functional applications. Pediatr Res 90(3):524–531. 10.1038/s41390-018-0114-9 10.1038/s41390-018-0114-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alzayedi AS, Azizalrahman AA, AlMadi HA, Althekair AM, Blaivas M, Karakitsos D (2017) Use and Education of Point-of-Care Ultrasound in pediatric emergency medicine in Saudi Arabia. J Ultrasound Med 36(11):2219–2225. 10.1002/jum.14254 10.1002/jum.14254 [DOI] [PubMed] [Google Scholar]
- 4.Arnold MJ, Jonas CE, Carter RE (2020) Point-of-Care Ultrasonography. Am Fam Physician 101(5):275–285 [PubMed] [Google Scholar]
- 5.Collins K, Collins C, Kothari A (2019) Point-of-care ultrasound in obstetrics. Australas J Ultrasound Med 1:32–39. 10.1002/ajum.12133 10.1002/ajum.12133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller LE, Stoller JZ, Fraga MV (2020) Point-of-care ultrasound in the neonatal ICU. Curr Opin Pediatr 32(2):216–227. 10.1097/mop.0000000000000863 10.1097/mop.0000000000000863 [DOI] [PubMed] [Google Scholar]
- 7.Lin J, Bellinger R, Shedd A, Wolfshohl J, Walker J, Healy J et al (2023) Point-of-care ultrasound in airway evaluation and management: a comprehensive review. Diagnostics (Basel). 10.3390/diagnostics13091541 10.3390/diagnostics13091541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fagley RE, Haney MF, Beraud AS, Comfere T, Kohl BA, Merkel MJ et al (2015) Critical care basic ultrasound learning goals for american anesthesiology critical care trainees: recommendations from an expert group. Anesth Analg 120(5):1041–1053. 10.1213/ane.0000000000000652 10.1213/ane.0000000000000652 [DOI] [PubMed] [Google Scholar]
- 9.Gold D, Levine M, Hsu D, Way DP, Shefrin AE, Lam SHF et al (2021) Design of a point-of-care ultrasound curriculum for pediatric emergency medicine fellows: a delphi study. AEM Education and Training 5(4):e10700. 10.1002/aet2.10700 10.1002/aet2.10700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramgobin D, Gupta V, Mittal R, Su L, Patel MA, Shaheen N et al (2022) POCUS in Internal medicine curriculum: quest for the holy-grail of modern medicine. J Community Hosp Intern Med Perspect. 10.55729/2000-9666.1112 10.55729/2000-9666.1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li L, Yong RJ, Kaye AD, Urman RD (2020) Perioperative Point of Care Ultrasound (POCUS) for Anesthesiologists: an overview. Curr Pain Headache Rep 24(5):20. 10.1007/s11916-020-0847-0 10.1007/s11916-020-0847-0 [DOI] [PubMed] [Google Scholar]
- 12.Knights S, Prasad S, Kalafat E, Dadali A, Sizer P, Harlow F et al (2023) Impact of point-of-care ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: An observational multicentre cohort study. PLoS Med 20(4):e1004192. 10.1371/journal.pmed.1004192 10.1371/journal.pmed.1004192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doniger SJ, Kornblith A (2018) Point-of-care ultrasound integrated into a staged diagnostic algorithm for pediatric appendicitis. Pediatr Emerg Care 34(2):109–115. 10.1097/pec.0000000000000773 10.1097/pec.0000000000000773 [DOI] [PubMed] [Google Scholar]
- 14.McVay MR, Copeland DR, McMahon LE, Cosper GH, McCallie TG, Kokoska ER et al (2009) Surgeon-performed ultrasound for diagnosis of pyloric stenosis is accurate, reproducible, and clinically valuable. J Pediatr Surg. 10.1016/j.jpedsurg.2008.10.028 10.1016/j.jpedsurg.2008.10.028 [DOI] [PubMed] [Google Scholar]
- 15.Arroyo AC, Zerzan J, Vazquez H, Dickman E, Likourezos A, Hossain R et al (2021) Diagnostic accuracy of point-of-care ultrasound for intussusception performed by pediatric emergency medicine physicians. J Emerg Med 60(5):626–632. 10.1016/j.jemermed.2020.11.030 10.1016/j.jemermed.2020.11.030 [DOI] [PubMed] [Google Scholar]
- 16.Lindert J, Rolle U, Naidoo G (2024) Point of care ultrasound in pediatric surgery across the european region—European pediatric surgery association endorsed survey. Eur J Pediatr Surg 34(01):020–027. 10.1055/a-2185-8963 10.1055/a-2185-8963 [DOI] [PubMed] [Google Scholar]
- 17.Ballard RB, Rozycki GS, Knudson MM, Pennington SD (1988) The surgeon’s use of ultrasound in the acute setting. Surg Clin North Am 78(2):337–364. 10.1016/s0039-6109(05)70316-9 10.1016/s0039-6109(05)70316-9 [DOI] [PubMed] [Google Scholar]
- 18.Allemann F, Cassina P, Röthlin M, Largiadèr F (1999) Ultrasound scans done by surgeons for patients with acute abdominal pain: a prospective study. Eur J Surg 165(10):966–970. 10.1080/110241599750008099 10.1080/110241599750008099 [DOI] [PubMed] [Google Scholar]
- 19.Avinadav E, Almog A, Kravarusic D, Seguier E, Samuk I, Nika A et al (2016) Point-of-care ultrasound in a department of pediatric and adolescent surgery. Isr Med Assoc J 18(11):677–679 [PubMed] [Google Scholar]
- 20.Nakajima Y, Yamada K, Imamura K, Kobayashi K (2008) Radiologist supply and workload: international comparison–working group of japanese college of radiology. Radiat Med 26:455–465. 10.1007/s11604-008-0259-2 10.1007/s11604-008-0259-2 [DOI] [PubMed] [Google Scholar]
- 21.Staff W (2015). Shortage of radiologists in SA requires Innovative Solution. Tech Smart South Africa website. http://www.techsmart.co.za/business/Shortage-of-radiologists-in-SA-requires-innovative-solution.html. Accessed 28 March 2023.
- 22.Kawooya MG (2012) Training for rural radiology and Imaging in Sub-Saharan Africa: addressing the mismatch between services and population. J Clin Imaging Sci 29(2):37. 10.4103/2156-7514.97747 10.4103/2156-7514.97747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rad-Aid Org (2020). Tanzania Radiology. Radiology Aid Organization website. https://rad-aid.org/countries/africa/tanzania/. Accessed 28 March 2024.
- 24.Andronikou S, McHugh K, Abdurahman N, Khoury B, Mngomezulu V, Brant WE et al (2011) Paediatric radiology seen from Africa Part I: providing diagnostic imaging to a young population. Pediatr Radiol. 10.1007/s00247-011-2081-8 10.1007/s00247-011-2081-8 [DOI] [PubMed] [Google Scholar]
- 25.Iyawe EP, Idowu BM, Omoleye OJ (2021) Radiology subspecialisation in Africa: a review of the current status. SA J Radiol 25(1):2168. 10.4102/sajr.v25i1.2168 10.4102/sajr.v25i1.2168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Collaboration PAR (2021) Paediatric surgical outcomes in sub-Saharan Africa: a multicentre, international, prospective cohort study. BMJ Glob Health 6(9):e004406. 10.1136/bmjgh-2020-004406 10.1136/bmjgh-2020-004406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The World Bank (2022) World Bank List of Economies 2021–2022. The World Bank website. https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html. Accessed 28 March 2024.
- 28.Meara JG, Greenberg SL (2025) The lancet commission on global surgery global surgery 2030: evidence and solutions for achieving health, welfare and economic development. Surgery 157(5):834–835. 10.1016/j.surg.2015.02.009 10.1016/j.surg.2015.02.009 [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization (2024) Medical doctors per 10 000 population. WHO website. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/medical-doctors-(per-10-000-population). Accessed 25 April 2024.
- 30.World Health Organization (2024) Optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. WHO website. https://www.who.int/publications-detail-redirect/9789241504843. Accessed 25 April 2024. [PubMed]
- 31.Bognini MS, Oko CI, Kebede MA, Ifeanyichi MI, Singh D, Hargest R et al (2023) Assessing the impact of anaesthetic and surgical task-shifting globally: a systematic literature review. Health Policy Plan 38(8):960–994. 10.1093/heapol/czad059 10.1093/heapol/czad059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okoroafor SC, Christmals CD (2023) Task shifting and task sharing implementation in Africa: a scoping review on rationale and scope. Healthcare (Basel) 11(8):1200. 10.3390/healthcare11081200 10.3390/healthcare11081200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smallwood N, Dachsel M (2018) Point-of-care ultrasound (POCUS): unnecessary gadgetry or evidence-based medicine? Clin Med (Lond) 18(3):219–224. 10.7861/clinmedicine.18-3-219 10.7861/clinmedicine.18-3-219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andronikou S, Otero HJ, Belard S, Heuvelings CC, Ruby LC, Grobusch MP (2022) Radiologists should support non-radiologist point-of-care ultrasonography in children: a case for involvement and collaboration. Pediatr Radiol 52(3):604–607. 10.1007/s00247-021-05185-7 10.1007/s00247-021-05185-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Györgyi Z, de Luca D, Singh Y (2022) The European society of paediatric radiology’s position statement on point-of-care ultrasound. Pediatr Radiol 52(3):608–609. 10.1007/s00247-021-05184-8 10.1007/s00247-021-05184-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhaktwani A (2012) The PC-PNDT act in a nutshell. Indian J Radiol Imaging 22(2):133–134. 10.4103/0971-3026.101114 10.4103/0971-3026.101114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith M, Krishnan SV, Leamon A, Galwankar S, Sinha TP, Kumar VA et al (2023) Removing barriers to emergency medicine point-of-care ultrasound: illustrated by a roadmap for emergency medicine point-of-care ultrasound expansion in India. J Emerg Trauma Shock 16(3):116–126. 10.4103/jets.jets_50_23 10.4103/jets.jets_50_23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith M, Innes S, Wildman S, Baker D (2023) A proposed framework for point of care musculoskeletal ultrasound and ultrasound image-guided interventions by physiotherapists: scope of practice, education and governance. Ultrasound J 15:15. 10.1186/s13089-023-00311-y 10.1186/s13089-023-00311-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Rijn RR, Stafrace S, Arthurs OJ, Rosendahl K (2021) Non-radiologist-performed point-of-care ultrasonography in paediatrics — European Society of Paediatric Radiology position paper. Pediatr Radiol 51(1):161–167. 10.1007/s00247-020-04843-6 10.1007/s00247-020-04843-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rajamani A, Shetty K, Parmar J, Huang S, Ng J, Gunawan S et al (2020) Longitudinal competence programs for basic point-of-care ultrasound in critical care: a systematic review. Chest 158(3):1079–1089. 10.1016/j.chest.2020.03.071 10.1016/j.chest.2020.03.071 [DOI] [PubMed] [Google Scholar]
- 41.Brant JA, Orsborn J, Good R, Greenwald E, Mickley M, Toney AG (2021) Evaluating a longitudinal point-of-care-ultrasound (POCUS) curriculum for pediatric residents. BMC Med Educ 21(1):64. 10.1186/s12909-021-02488-z 10.1186/s12909-021-02488-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dietrich CF et al (2023) The ultrasound use of simulators, current view, and perspectives: requirements and technical aspects (WFUMB state of the art paper). Endosc Ultrasound 12(1):38–49. 10.4103/eus-d-22-00197 10.4103/eus-d-22-00197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coley BD, Mutabagani KH, Martin LC, Zumberge N, Cooney DR, Caniano DA et al (2000) Focused abdominal sonography for trauma (FAST) in children with blunt abdominal trauma. J Trauma 48(5):902–906. 10.1097/00005373-200005000-00014 10.1097/00005373-200005000-00014 [DOI] [PubMed] [Google Scholar]
- 44.Corbett SW, Andrews HG, Baker EM, Jones WG (2000) ED evaluation of the pediatric trauma patient by ultrasonography. Am J Emerg Med 18(3):244–249. 10.1016/s0735-6757(00)90113-x 10.1016/s0735-6757(00)90113-x [DOI] [PubMed] [Google Scholar]
- 45.Sivitz AB, Tejani C, Cohen SG (2013) Evaluation of hypertrophic pyloric stenosis by pediatric emergency physician sonography. Acad Emerg Med 20(7):646–651. 10.1111/acem.12163 10.1111/acem.12163 [DOI] [PubMed] [Google Scholar]
- 46.Chang YJ, Hsia SH, Chao HC (2013) Emergency medicine physicians performed ultrasound for pediatric intussusceptions. Biomed J 36(4):175–178. 10.4103/2319-4170.112739 10.4103/2319-4170.112739 [DOI] [PubMed] [Google Scholar]
- 47.Nguyen HN, Kulkarni M, Jose J, Sisson A, Brandt ML, Sammer MBK et al (2021) Ultrasound for the diagnosis of malrotation and volvulus in children and adolescents: a systematic review and meta-analysis. Arch Dis Child 106(12):1171–1178. 10.1136/archdischild-2020-321082 10.1136/archdischild-2020-321082 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.