Abstract
The aim of this study was to evaluate the impact of COVID-19 on ocular diseases and changes in risk factors before and after the COVID-19 pandemic. This study was conducted using data from the Korea National Health and Nutrition Examination Survey (KNHANES) 2015–2021, a national cross-sectional health examination and survey. Associations between ocular diseases and risk factors were determined using the chi-squared test and logistic regression analysis. Bivariable adjusted logistic regression analysis was performed to examine the odds ratio (OR) and 95% confidence interval (CI) to evaluate of the impact of COVID-19 on ocular diseases. Individuals were divided into two age groups (< 60 and ≥ 60 years). A total of 50,158 people were diagnosed, of whom 7270 were diagnosed with cataract, 921 with glaucoma, and 439 with age-related macular degeneration (AMD). Risk factors for cataract were COVID-19 pandemic (OR 1.161), hypertension (OR 1.608), diabetes (OR 1.573), dyslipidemia (OR 1.167), stroke (OR 1.272), and depression (OR 1.567). Risk factors for AMD were COVID-19 pandemic (OR 1.600), dyslipidemia (OR 1.610), and depression (OR 1.466). Risk factors for glaucoma were hypertension (OR 1.234), dyslipidemia (OR 1.529), diabetes (OR 1.323), and depression (OR 1.830). The COVID-19 pandemic was a risk factor for cataracts and AMD, but not for glaucoma. Cataracts and AMD may be more influenced by the acquired health conditions or the environment.
Keywords: COVID-19 pandemic, Ocular diseases, Risk factor
Subject terms: Eye diseases, Risk factors
Introduction
COVID-19 is an infectious disease caused by a newly discovered coronavirus1. It is a novel strain of the virus that had not been previously identified in humans and has since spread throughout the world2. Symptoms of the disease include cough, fever, shortness of breath, and fatigue2. COVID-19 pandemic has had a major impact on daily activities around the world to help slow the spread of the virus and protect public health. Many countries have implemented social distancing measures, such as stay-at-home orders, travel restrictions, and business closures3. Schools and universities have been closed, and many people are now working from home. Changes in lifestyle patterns due to COVID-19 pandemic have affected nutritional status and physical activities4.
The most common ocular diseases were cataract, glaucoma, and age-related macular degeneration (AMD)5. The prevalence of cataract was the highest of all the ocular diseases studied, followed by glaucoma and AMD, with a marked increase in the prevalence of both glaucoma and AMD over time5. Although they are associated with a number of risk factors, it is not clear whether the COVID-19 pandemic has an impact on ocular disease such as cataract, glaucoma and AMD. However, the prevalence of risk factors such as obesity, dyslipidemia, hypertension, diabetes, smoking, reduction in physical activity and stroke, depression have increased with COVID-19 pandemic6,7. As COVID-19 has caused changes in the immune system and lifestyle habits8, it is possible that the prevalence of eye diseases has changed. Therefore, it was necessary to find out the changes in the prevalence of eye diseases and the differences in risk factors due to COVID-19. Investigating the impact of the COVID-19 pandemic on the prevalence of eye disease and the associated risk factors is essential to understanding the multiple ways in which this disease affects human health. Research into the impact of COVID-19 on ocular health may help to improve prevention and treatment methods, and to gain a better understanding of the long-term effects of this disease. The aim of this study was to evaluate the effect of COVID-19 on ocular disease in a Korean population.
Methods
The Korean National Health and Nutrition Examination Survey (KNHANES) was approved by the Institutional Review Board (IRB) of the Korean Centers for Disease Control and Prevention (2013-12EXP-03-5C, 2013-12EXP-03-5C, 2018-01-03-C-A, 2018-01-03-2C-A, 2018-01-03-5C-A, and 2018-01-03-4C-A). This study adhered to the tenets of the Declaration of Helsinki and was approved from IRB approval by the institutional review board of Hallym University Kangnam Sacred Heart Hospital (2024-04-011).
For this cross-sectional, population-based study, we used data from the KNHANES 2015–2021, a series of cross-sectional surveys of nationally representative samples of the Korean civilian population, conducted annually to assess the health and nutrition status of the South Korean population. To obtain representative samples, KNHANES uses a stratified, multistage, cluster probability sampling design by geographical area, age, and sex. For the health interview survey, a trained interviewer asked questions directly to individuals aged ≥ 19 years old. The inclusion criteria for this study were: (1) adults over 19 years of age, (2) those who completed a questionnaire on independent risk factors. Our exclusion criteria were aged < 19 years. Subjects were asked whether they had been diagnosed with cataracts by an ophthalmologist, in the same way as they were asked whether they had been diagnosed with cataract, glaucoma or AMD. Risk factors such as diabetes, hypertension, dyslipidemia, major depression disorder (MDD), and aerobic physical activity were questioned. Incorrect or untested responses (untested) were excluded (Fig. 1). The population was divided according to age: young (< 60 years) or older (≥ 60 years). The pre-COVID-19 period was 2015–2019, and the post-COVID-19 period was set at 2020–2021.
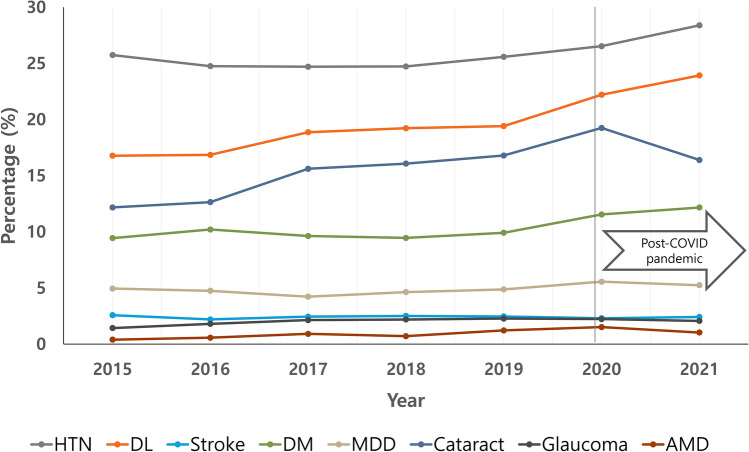
Fig. 1.
Disease prevalence by year.
Statistical analyses were performed using SPSS Version 27.0 (SPSS Inc., IBM Software, Portsmouth, UK), and two-tailed p-values less than 0.05 were considered statistically significant. To estimate the odds ratios (ORs) of cataract and potential factors, we performed binary logistic regression analyses using a generalized linear model for a complex survey design. The ORs measure the odds of an outcome occurring in the presence of various risk factors compared to the odds of the outcome occurring in their absence. ORs are presented with corresponding 95% confidence intervals (CIs). CIs provide a range of values that are believed to cover the true value of the ORs to a 95% level of confidence, thus giving an indication of the precision of our estimates.
Institutional review board statement
This study was approved by the Institutional Review Board of Kangnam Sacred Heart Hospital (Approval number: 2024-04-009).
Results
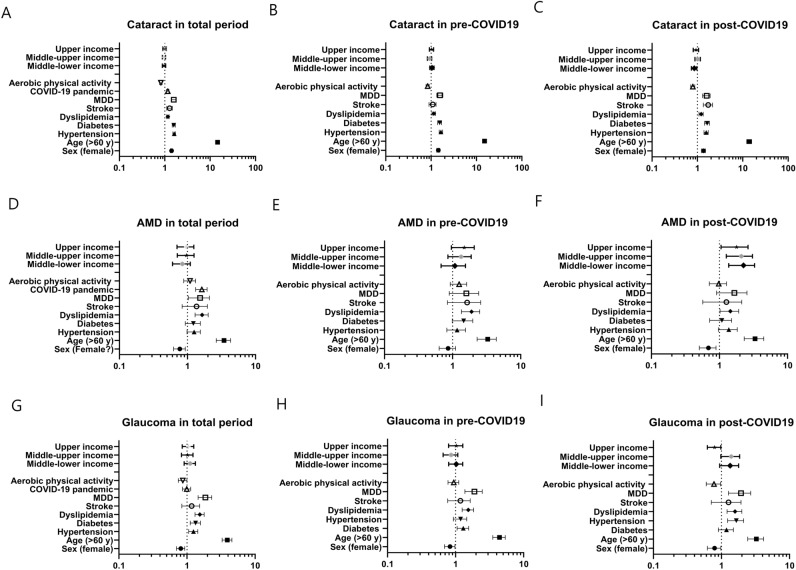
The characteristics of the study population are shown in Table 1. Of the 61,567 people in KHANES 2015–2021, 50,158 people (22,284 men and 27,874 women) over 19 years of age were included in this study, excluding 11,409 under 19 years of age. Of these, 33,073 were pre-COVID-19 and 17,085 were post-COVID-19. Of these, 7270 were diagnosed with cataracts, 921 with glaucoma and 439 with AMD. Mean age was 51.88 ± 17.09 years. Disease prevalence by year is shown in Table 1 and Fig. 1. We found the prevalences of cataract and AMD increased in post-COVID-19 compared to pre-COVID-19 Risk factors for cataract were COVID-19 pandemic (OR 1.161; 95% CI 1.091–1.235), hypertension (OR 1.608; 95% CI 1.506–1.717), diabetes (OR 1.573; 95% CI 1.455–1.701), dyslipidemia (OR 1.167; 95% CI 1.091–1.249), stroke (OR 1.272; 95% CI 1.105–1.463), and depression (OR 1.567; 95% CI 1.391–1.765) (Table 2 and Fig. 2A). Aerobic physical activity was the protective factor (OR 0.820; 95% CI 0.769–0.874). Before the COVID-19 pandemic, risk factors for cataract were sex (OR 1.437; 95% CI 1.327–1.557), age (OR 14.971; 95% CI 13.518–16.580), hypertension (OR 1.641; 95% CI 1.509–1.785), diabetes (OR 1.542; 95% CI 1.394–1.706), dyslipidemia (OR 1.144; 95% CI 1.048–1.249), and MDD (OR 1.558; 95% CI 1.337–1.815), not stroke (OR 1.075; 95% CI 0.900–1.284) (Table 2 and Fig. 2B). Aerobic physical activity was a protective factor (OR 0.837; 95% CI 0.772–0.909). However, stroke and personal income was not significant factor. After the start of the COVID-19 pandemic, stroke (OR 1.700; 95% CI 1.346–2.147) was found to be an important risk factor in addition to existing risk factors and middle-lower income to be a protective factor (Table 2 and Fig. 2C).
Table 1.
Demographic data.
| Total | Pre-COVID-19 | Post-COVID-19 | p-value | |
|---|---|---|---|---|
| N | 50,158 | 33,073 | 17,085 | |
| Period | 2015–2021 | 2015–2019 | 2020–2021 | |
| Age (year) | 51.88 ± 17.09 | 51.54 ± 16.90 | 52.53 ± 17.42 | < 0.001* |
| Sex (M:F) | 22,284:27,874 | 14,714:18,359 | 7570:9515 | 0.704 |
| Cataract | 7270 (16.0%) | 4477 (15.0%) | 2793 (18.1%) | < 0.001* |
| Glaucoma | 921 (2.0%) | 599 (2.0%) | 322 (2.1%) | 0.419 |
| AMD | 439 (1.0%) | 236 (0.8%) | 203 (1.3%) | < 0.001* |
AMD age-related macular degeneration. *p <0.05
Table 2.
The risk factors for cataract at pre- and post-COVID-19 pandemic.
| General Characteristics | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Total | ||||
| Sex (female) | 1.404 | 1.319 | 1.494 | < 0.001* |
| Age (> 60 years) | 14.489 | 13.386 | 15.684 | < 0.001* |
| Hypertension | 1.608 | 1.506 | 1.717 | < 0.001* |
| Diabetes | 1.573 | 1.455 | 1.701 | < 0.001* |
| Dyslipidemia | 1.167 | 1.091 | 1.249 | < 0.001* |
| Stroke | 1.272 | 1.105 | 1.463 | < 0.001* |
| MDD | 1.567 | 1.391 | 1.765 | < 0.001* |
| COVID-19 pandemic | 1.161 | 1.091 | 1.235 | < 0.001* |
| Aerobic physical activity | 0.820 | 0.769 | 0.874 | < 0.001* |
| Income | ||||
| Lower | 0.732 | |||
| Middle-lower | 0.962 | 0.883 | 1.047 | 0.367 |
| Middle-upper | 0.958 | 0.880 | 1.043 | 0.323 |
| Upper | 0.983 | 0.903 | 1.071 | 0.699 |
| Pre-COVID-19 | ||||
| Sex (female) | 1.437 | 1.327 | 1.557 | < 0.001* |
| Age (> 60 years) | 14.971 | 13.518 | 16.580 | < 0.001* |
| Hypertension | 1.641 | 1.509 | 1.785 | < 0.001* |
| Diabetes | 1.542 | 1.394 | 1.706 | < 0.001* |
| Dyslipidemia | 1.144 | 1.048 | 1.249 | 0.003* |
| Stroke | 1.075 | 0.900 | 1.284 | 0.424 |
| MDD | 1.558 | 1.337 | 1.815 | < 0.001* |
| Aerobic physical activity | 0.837 | 0.772 | 0.909 | < 0.001* |
| Income | ||||
| Lower | 0.137 | |||
| Middle-lower | 1.042 | 0.936 | 1.161 | 0.452 |
| Middle-upper | 0.922 | 0.827 | 1.029 | 0.147 |
| Upper | 1.020 | 0.915 | 1.137 | 0.718 |
| Post-COVID-19 | ||||
| Sex (female) | 1.357 | 1.228 | 1.498 | < 0.001* |
| Age (> 60 years) | 13.816 | 12.183 | 15.668 | < 0.001* |
| Hypertension | 1.552 | 1.397 | 1.725 | < 0.001* |
| Diabetes | 1.626 | 1.436 | 1.841 | < 0.001* |
| Dyslipidemia | 1.203 | 1.081 | 1.340 | 0.001* |
| Stroke | 1.700 | 1.346 | 2.147 | < 0.001* |
| MDD | 1.577 | 1.303 | 1.909 | < 0.001* |
| Aerobic physical activity | 0.788 | 0.711 | 0.874 | < 0.001* |
| Income | 0.038* | |||
| Lower | 1 (ref) | |||
| Middle-lower | 0.845 | 0.736 | 0.970 | 0.017* |
| Middle-upper | 1.009 | 0.882 | 1.156 | 0.892 |
| Upper | 0.925 | 0.806 | 1.062 | 0.270 |
MDD Major depressive disorder, *p < 0.05.
Fig. 2.
Forest plots showing the odds ratio with 95% confidence interval. (A–C) The association between cataracts and risk factors in total study periods, pre-COVID-19 and post-COVID-19. (D–F) The association between AMD and risk factors in total study periods, pre-COVID-19 and post-COVID-19. (G–I) The association between glaucoma and risk factors in total study periods, pre-COVID-19 and post-COVID-19.
Risk factors for AMD were the COVID-19 pandemic (OR 1.600; 95% CI 1.318–1.943), age (OR 3.367; 95% CI 2.643–4.289), dyslipidemia (OR 1.610; 95% CI 1.291–2.008), and depression (OR 1.466; 95% CI 1.026–2.097) and sex was a protective factor (OR 0.761; 95% CI 0.624–0.928) (Table 3 and Fig. 2D). Before the COVID-19 pandemic, risk factors for AMD included age (OR 3.160; 95% CI 2.287–4.367), and dyslipidemia (OR 1.837; 95% CI 1.350–2.500) (Table 3 and Fig. 2E). After the start of the COVID-19 pandemic, income was a significant risk factor whereas sex was a protective factor (OR 0.670; 95% CI 0.505–0.889) (Table 3 and Fig. 2F).
Table 3.
Risk factors for AMD at pre- and post- COVID-19 pandemic.
| General characteristics | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Total | ||||
| Sex (Female) | 0.761 | 0.624 | 0.928 | 0.007* |
| Age (> 60 years) | 3.367 | 2.643 | 4.289 | < 0.001* |
| Hypertension | 1.231 | 0.983 | 1.541 | 0.070 |
| Diabetes | 1.195 | 0.928 | 1.540 | 0.168 |
| Dyslipidemia | 1.610 | 1.291 | 2.008 | < 0.001* |
| Stroke | 1.278 | 0.833 | 1.961 | 0.261 |
| MDD | 1.466 | 1.026 | 2.097 | 0.036* |
| COVID-19 pandemic | 1.600 | 1.318 | 1.943 | < 0.001* |
| Aerobic physical activity | 1.076 | 0.880 | 1.315 | 0.477 |
| Income | 0.572 | |||
| Lower | 1 (ref) | |||
| Middle-lower | 0.814 | 0.603 | 1.098 | 0.178 |
| Middle-upper | 0.940 | 0.709 | 1.246 | 0.665 |
| Upper | 0.933 | 0.702 | 1.240 | 0.633 |
| Pre-COVID-19 | ||||
| Sex (female) | 0.837 | 0.634 | 1.105 | 0.209 |
| Age (> 60 years) | 3.160 | 2.287 | 4.367 | < 0.001* |
| Hypertension | 1.128 | 0.822 | 1.546 | 0.456 |
| Diabetes | 1.398 | 0.986 | 1.982 | 0.060 |
| Dyslipidemia | 1.837 | 1.350 | 2.500 | < 0.001* |
| Stroke | 1.472 | 0.839 | 2.583 | 0.178 |
| MDD | 1.468 | 0.892 | 2.415 | 0.131 |
| Aerobic physical activity | 1.217 | 0.921 | 1.608 | 0.167 |
| Income | ||||
| Lower | 0.221 | |||
| Middle-lower | 1.023 | 0.678 | 1.545 | 0.913 |
| Middle-upper | 1.263 | 0.852 | 1.874 | 0.245 |
| Upper | 1.412 | 0.960 | 2.078 | 0.080 |
| Post-COVID-19 | ||||
| Sex (female) | 0.670 | 0.505 | 0.889 | 0.005* |
| Age (> 60 years) | 3.215 | 2.309 | 4.476 | < 0.001* |
| Hypertension | 1.325 | 0.963 | 1.822 | 0.084 |
| Diabetes | 1.038 | 0.717 | 1.504 | 0.842 |
| Dyslipidemia | 1.397 | 1.019 | 1.915 | 0.038* |
| Stroke | 1.099 | 0.568 | 2.124 | 0.780 |
| MDD | 1.517 | 0.908 | 2.534 | 0.112 |
| Aerobic physical activity | 0.949 | 0.709 | 1.269 | 0.722 |
| Income | 0.006* | |||
| Lower | 1 (ref) | |||
| Middle-lower | 2.115 | 1.366 | 3.275 | 0.001* |
| Middle-upper | 1.960 | 1.260 | 3.050 | 0.003* |
| Upper | 1.663 | 1.052 | 2.629 | 0.030* |
MDD Major depressive disorder. *p <0.05
Risk factors for glaucoma were age (OR 3.864; 95% CI 3.272–4.563), hypertension (OR 1.234; 95% CI 1.056–1.441), diabetes (OR 1.323; 95% CI 1.113–1.572), dyslipidemia (OR 1.529; 95% CI 1.311–1.783), and MDD (OR 1.830; 95% CI 1.453–2.303), but not the COVID-19 pandemic. Protective factor for glaucoma was sex (OR 0.804; 95% CI 0.700–0.924) and aerobic physical activity (OR 0.861; 95% CI 0.745–0.996) (Table 4 and Fig. 2G). Before the COVID-19 pandemic, the risk factors were age (OR 4.343; 95% CI 3.512–5.372), hypertension (OR 1.280; 95% CI 1.052–1.558), dyslipidemia (OR 1.517; 95% CI 1.248–1.844), MDD (OR 1.838; 95% CI 1.372–2.461), and the protective factor was sex (OR 0.821; 95% CI 0.688–0.970) (Table 4 and Fig. 2H). Diabetes and aerobic physical activity were not significant factor. After the start of the COVID-19 pandemic, hypertension was not a risk factor and diabetes (OR 1.6129; 95% CI 1.231–2.111) was a risk factor. Aerobic physical activity was a protective factor (OR 0.760; 95% CI 0.597–0.968) (Table 4 and Fig. 2I).
Table 4.
Risk factors for glaucoma at pre- and post-COVID-19 pandemic.
| General characteristics | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Total | ||||
| Sex (female) | 0.804 | 0.700 | 0.924 | 0.002* |
| Age (> 60 years) | 3.864 | 3.272 | 4.563 | < 0.001* |
| Hypertension | 1.234 | 1.056 | 1.441 | 0.008* |
| Diabetes | 1.323 | 1.113 | 1.572 | 0.001* |
| Dyslipidemia | 1.529 | 1.311 | 1.783 | < 0.001* |
| Stroke | 1.134 | 0.838 | 1.535 | 0.416 |
| MDD | 1.830 | 1.453 | 2.303 | < 0.001* |
| COVID-19 pandemic | 0.985 | 0.856 | 1.133 | 0.832 |
| Aerobic physical activity | 0.861 | 0.745 | 0.996 | 0.044* |
| Income | ||||
| Lower | 0.763 | |||
| Middle-lower | 1.097 | 0.907 | 1.327 | 0.342 |
| Middle-upper | 1.006 | 0.828 | 1.222 | 0.952 |
| Upper | 1.032 | 0.849 | 1.255 | 0.750 |
| Pre-COVID-19 | ||||
| Sex (female) | 0.821 | 0.688 | 0.979 | 0.028* |
| Age (> 60 years) | 4.343 | 3.512 | 5.372 | < 0.001* |
| Hypertension | 1.280 | 1.052 | 1.558 | 0.014* |
| Diabetes | 1.163 | 0.928 | 1.457 | 0.190 |
| Dyslipidemia | 1.517 | 1.248 | 1.844 | < 0.001* |
| Stroke | 1.120 | 0.766 | 1.638 | 0.559 |
| MDD | 1.838 | 1.372 | 2.461 | < 0.001* |
| Aerobic physical activity | 0.928 | 0.774 | 1.114 | 0.424 |
| Income | ||||
| Lower | 0.432 | |||
| Middle-lower | 1.004 | 0.791 | 1.273 | 0.975 |
| Middle-upper | 0.841 | 0.656 | 1.079 | 0.174 |
| Upper | 1.003 | 0.789 | 1.274 | 0.983 |
| Post-COVID-19 | ||||
| Sex (female) | 0.779 | 0.621 | 0.977 | 0.030* |
| Age (> 60 years) | 3.178 | 2.432 | 4.153 | < 0.001* |
| Hypertension | 1.158 | 0.897 | 1.494 | 0.260 |
| Diabetes | 1.612 | 1.231 | 2.111 | 0.001* |
| Dyslipidemia | 1.549 | 1.206 | 1.990 | 0.001* |
| Stroke | 1.169 | 0.708 | 1.932 | 0.541 |
| MDD | 1.846 | 1.269 | 2.685 | 0.001* |
| Aerobic physical activity | 0.760 | 0.597 | 0.968 | 0.026* |
| Income | ||||
| Lower | 0.213 | |||
| Middle-lower | 1.294 | 0.939 | 1.782 | 0.116 |
| Middle-upper | 1.344 | 0.978 | 1.847 | 0.068 |
| Upper | 0.779 | 0.621 | 0.977 | 0.621 |
MDD Major depressive disorder. *p < 0.05
Discussion
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and rapidly evolved into a global health crisis9. It has led to widespread disease and significant mortality, with a profound impact on public health, economies, and daily life worldwide9. In this study, we investigated the effect of the COVID-19 pandemic on the prevalence and risk factors for ocular disease. This study found that COVID-19 pandemic was an important risk factor for cataract and AMD, but not for glaucoma. There may be several possible reasons why the prevalence of cataract and AMD has increased since the COVID-19 outbreak. First, changes in diet and lifestyle due to the COVID-19 pandemic. Changes in lifestyle due to the pandemic may affect nutritional status and daily activities, which may also affect the risk factors for ocular diseases such as diabetes, dyslipidemia and hypertension due to restrictions on outdoor activities10. Second, with immune system changes, COVID-19 affects the patient's immune system. This may worsen existing eye diseases or increase the risk of developing new eye diseases. COVID-19 causes epigenetic changes and hyperactivation in monocytes and permanent changes in stem cell gene expression, causing the immune system to produce more white blood cells11. The third is the postponement or cancellation of regular eye examinations due to COVID-19. Many people have been unable to access regular health care during the pandemic, including the postponement or cancellation of eye examinations. This may have the delayed early detection and treatment of some eye diseases. Fourth, social isolation and stress: prolonged social isolation can have a negative impact on mental health, which can also affect physical health, especially eye health. Stress is known to be a risk factor for several eye diseases12. In addition, with many people spending more time at home due to social isolation, screen time on computers, smartphones and other devices has increased. This can lead to increased vision problems and eye fatigue13. Furthermore, oxidative stress, which is a main pathogenesis of cataract and AMD, is increased by COVID-19 infection and damages the lens and retinal pigment epithelium14,15. However, the COVID-19 pandemic is not a risk factor for glaucoma. Glaucoma is thought to be caused more by endogenous factors rather than exogenous factors. COVID-19 is caused by the SARS-CoV-2 virus, which primarily affects the respiratory system but can also impact other organs due to its inflammatory and vascular effects16. Glaucoma, on the other hand, is a group of eye conditions that primarily involve the degeneration of the optic nerve, often associated with increased intraocular pressure17. The etiology of glaucoma is complex, involving genetic, vascular, and mechanical components that are not directly influenced by viral infections like COVID-1917.
This study showed that risk factors have changed since the COVID-19 pandemic. Stroke was not a risk factor for cataract, but after the COVID-19 pandemic, it became an important risk factor. In AMD, dyslipidemia was a major risk factor rather than sex, but this was reversed after the COVID-19 pandemic. These changes in risk factors may be due to changes in the immune system caused by coronavirus infection. COVID-19 may trigger stronger inflammatory responses in men18,19. Glaucoma was not associated with diabetes and aerobic physical activity before the COVID-19 pandemic, but became associated after the COVID-19 pandemic. Lifestyle factors may become important in the management and reduction of glaucoma risk factors.
Surprisingly, household income had an effect on the change of risk factors. For cataracts, income was not a risk factor in pre-COVID-19, but upper-middle income was a protective factor for low income in post-COVID-19. For AMD, income was not a risk factor in pre-COVID-19, but an increase in income was a risk factor for low income in post-COVID-19. This is likely to have been influenced by the increase in home offices, long-time computer use, decline in outdoor physical activities, and social isolation among the upper-middle income class post-COVID-19 during the pandemic.
In conclusion, the COVID-19 pandemic was a risk factor for cataract and AMD, but not for glaucoma. Cataract and AMD may be more affected by the external factors than glaucoma. The indirect effects of the pandemic, such as stress, changes in immune system, changes in access to healthcare, and lifestyle changes, are likely to play a significant role in these observed trends.
Acknowledgements
This study was supported by the National Research Foundation (NRF) grant (NRF-2023R1A2C2002674) funded by the Korea government and Hallym University Research Fund funded by Hallym University.
Author contributions
Y.J.S. planned the study, performed and analyzed the data, supervised the project and drafed the manuscript. H.J.K. performed and analyzed the data, and drafed the manuscript. Y.K.R. conducted and analyzed the data, and drafed the manuscript. All authors commented on and revised the manuscript.
Funding
The authors have no financial interest regarding the subject matter of this manuscript.
Data availability
All the data utilized in this study are publicly available through the KNHANES website (http://knhanes.cdc.go.kr, accessed on 14 July 2022).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hyeon Jung Kim and Yun Kyoung Ryu.
References
- 1.Zeb, A., Alzahrani, E., Erturk, V. S. & Zaman, G. Mathematical model for coronavirus disease 2019 (COVID-19) containing isolation class. Biomed. Res. Int.2020, 3452402 (2020). 10.1155/2020/3452402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pal, M., Berhanu, G., Desalegn, C. & Kandi, V. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): An update. Cureus12, e7423 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahmoudi, J. & Xiong, C. How social distancing, mobility, and preventive policies affect COVID-19 outcomes: Big data-driven evidence from the District of Columbia-Maryland-Virginia (DMV) megaregion. PLoS One17, e0263820 (2022). 10.1371/journal.pone.0263820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coskun, M. G., Ozturk, R. I., Tak, A. Y., Sanlier, N. Working from home during the COVID-19 pandemic and its effects on diet, sedentary lifestyle, and stress. Nutrients. 14 (2022). [DOI] [PMC free article] [PubMed]
- 5.Lau, J. T., Lee, V., Fan, D., Lau, M. & Michon, J. Knowledge about cataract, glaucoma, and age related macular degeneration in the Hong Kong Chinese population. Br. J. Ophthalmol.86, 1080–1084 (2002). 10.1136/bjo.86.10.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma, L. P. et al. Long-term impact of the COVID-19 pandemic on obsessive-compulsive disorder. Psychiatry Res.331, 115625 (2023). 10.1016/j.psychres.2023.115625 [DOI] [PubMed] [Google Scholar]
- 7.Goldman, N., Park, S. S., Beltran-Sanchez, H. Life expectancy among native Americans during the COVID-19 pandemic: Estimates, uncertainty and obstacles. Am. J. Epidemiol. (2023). [DOI] [PMC free article] [PubMed]
- 8.Pandey, V., Mohan, R., Kumar, A., Gangadevi, P. & Kurien, N. The impact of the COVID-19 outbreak on lifestyle-related behavior among the general population. Cureus15, e45756 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pollard, C. A., Morran, M. P. & Nestor-Kalinoski, A. L. The COVID-19 pandemic: A global health crisis. Physiol. Genom.52, 549–557 (2020). 10.1152/physiolgenomics.00089.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sohn, M. et al. Impact of COVID-19 and associated preventive measures on cardiometabolic risk factors in South Korea. J. Obes. Metab. Syndr.30, 248–260 (2021). 10.7570/jomes21046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheong, J. G. et al. Epigenetic memory of coronavirus infection in innate immune cells and their progenitors. Cell186, 3882-3902 e24 (2023). 10.1016/j.cell.2023.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabel, B. A., Wang, J., Cardenas-Morales, L., Faiq, M. & Heim, C. Mental stress as consequence and cause of vision loss: The dawn of psychosomatic ophthalmology for preventive and personalized medicine. EPMA J.9, 133–160 (2018). 10.1007/s13167-018-0136-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chu, G. C. H. et al. Association between time spent on smartphones and digital eye strain: A 1-year prospective observational study among Hong Kong children and adolescents. Environ. Sci. Pollut. Res. Int.30, 58428–58435 (2023). 10.1007/s11356-023-26258-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maurya, M. et al. Oxidative stress in retinal pigment epithelium degeneration: From pathogenesis to therapeutic targets in dry age-related macular degeneration. Neural Regen. Res.18, 2173–2181 (2023). 10.4103/1673-5374.369098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsueh, Y. J. et al. The pathomechanism, antioxidant biomarkers, and treatment of oxidative stress-related eye diseases. Int. J. Mol. Sci.23, 1255 (2022). 10.3390/ijms23031255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kopanska, M. et al. Effects of SARS-CoV-2 inflammation on selected organ systems of the human body. Int. J. Mol. Sci.23, 4178 (2022). 10.3390/ijms23084178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Esposito, F. et al. Epigenetics in Glaucoma. Medicina (Kaunas)60, 905 (2024). 10.3390/medicina60060905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sher, E. K. et al. Covid-19 a triggering factor of autoimmune and multi-inflammatory diseases. Life Sci.319, 121531 (2023). 10.1016/j.lfs.2023.121531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manjili, R. H., Zarei, M., Habibi, M. & Manjili, M. H. COVID-19 as an acute inflammatory disease. J. Immunol.205, 12–19 (2020). 10.4049/jimmunol.2000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data utilized in this study are publicly available through the KNHANES website (http://knhanes.cdc.go.kr, accessed on 14 July 2022).