Abstract
Background:
Bucket-handle meniscal tears are large longitudinal vertical meniscal tears that have an attached fragment flipped into the intercondylar notch. Meniscal repair attempts to restore the function of the meniscus and aims to preserve joint mechanics. Alternatively, meniscectomy results in quicker recovery but may lead to future degeneration.
Purposes:
To evaluate the long-term risk of subsequent ipsilateral knee surgery in patients who underwent a bucket-handle meniscal repair (BHMR) versus meniscectomy/bucket-handle meniscal debridement (BHMD) and assess risk factors associated with subsequent knee surgical intervention.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
An electronic health records search for all patients who underwent arthroscopic knee meniscal surgery (repair and meniscectomy) between 2011 and 2018 was performed. Natural language processing was used to search for terms of interest in the long operative notes to determine whether these surgeries were performed for bucket-handle meniscal tears. These patients comprised our initial cohort. Study patients were followed for at least 1 year and for up to 5 years (until December 31, 2019), with censoring at death or membership disenrollment. Baseline patient characteristics and outcomes were evaluated via a database review. The primary outcome was subsequent ipsilateral knee surgeries and secondary outcomes included contralateral knee surgeries, deep surgical site infections, and venous thrombotic events. Multivariable logistic regression analyses were used to model for subsequent surgical treatment of the ipsilateral knee. A subset analysis for patients aged 30 to 50 years was then performed.
Results:
The median follow-up time was 52.4 months (interquartile range [IQR], 33.5-60 months). A total of 1359 patients underwent BHMR and 1537 patients underwent BHMD. The median age was 24 years (IQR, 17-34 years) for the BHMR versus 38 years (IQR, 27-47 years) for the BHMD group (P < .001). Body mass index (BMI) was significantly lower in the BHMR group compared with the BHMD group (P < .001). BHMR was significantly more likely to be performed during a concomitant ipsilateral anterior cruciate ligament reconstruction (ACLR) than a BHMD (44.2% vs 30.1%, P < .001). During the follow-up period, a total of 656 subsequent ipsilateral procedures were performed in 393 (13.6%) patients. Patients who underwent initial BHMR were at a significantly higher risk of undergoing subsequent meniscal repair (4.3% vs 1%, P < .001), meniscectomy (12.1% vs 3.3%, P < .001), and ACLR (7.4% vs 2.9%, P < .001) compared with those who underwent BHMD. Multivariable analysis showed that BHMR, younger age, and lower BMI were risk factors for subsequent ipsilateral surgery. After adjusting for patient demographic and clinical characteristics, subset analysis showed that for patients aged 30 to 50 years, undergoing a BHMR versus a BHMD led to a 2.3-fold higher risk of subsequent surgery, a 5.3-fold higher risk of subsequent meniscal repair and a 3.2-fold higher risk of subsequent meniscectomy.
Conclusion:
BHMR was more often performed in younger patients with a lower BMI, especially during a concomitant ACLR. Patients treated with BHMR were more likely to undergo subsequent surgeries, with the likelihood decreasing with increasing age. Subset analyses showed increasing risk for subsequent surgeries with BHMR versus BHMD in the cohort consisting of patients aged 30 to 50 years.
Keywords: aging athlete, articular cartilage, knee, meniscus
Meniscal injuries are common in the general population and occur in a variety of morphologies, including horizontal, oblique, radial, longitudinal, and complex degenerative. 10 The meniscus has been proven to provide a number of biomechanical functions, including load dispersal, joint lubrication, and proprioception3,8; furthermore, meniscal loss may lead to accelerated cartilage degeneration and osteoarthritis. 24 Bucket-handle meniscal tears (BHMT), which comprise 10% of all meniscal tears, are large vertical longitudinal tears where a large attached fragment displaces from the remnant meniscus into the intercondylar notch. 33 This displacement phenomenon can result in mechanical locking of the knee joint and, depending on the size, effectively renders the meniscus incompetent, 16 which may result in significant meniscal degeneration and long-term joint dysfunction if not treated appropriately.
BHMTs are managed primarily surgically, with repair typically favored over resection to avoid the poorer postoperative outcomes associated with subtotal or total meniscectomy. 5 Although patients typically experience improvements in patient-reported outcomes after bucket-handle meniscal repair (BHMR),1,6 reoperation rates are consistently reported between 15% and 25%.18,25 While reoperation rates are a notable concern, it is important to also consider the long-term functional benefits and drawbacks of BHMR versus bucket-handle meniscal debridement (BHMD). Specifically, meniscal repair aims to preserve meniscal function, potentially offering better long-term joint health despite the higher risk for reoperation. Previous studies have identified a variety of factors affecting reoperation rates, including isolated meniscal pathology, concurrent anterior cruciate ligament (ACL) reconstruction (ACLR), sex, and age.2,25 However, many of these studies have small cohort sizes and short or intermediate follow-up periods, which may limit their conclusions and the general applicability of their results. In addition, there is a paucity of literature directly comparing outcomes after BHMR versus BHMD, also known as meniscectomy.
The purpose of this study was to evaluate the midterm risk of subsequent ipsilateral knee surgery in a large cohort of patients who underwent arthroscopic BHMR. Specifically, we aimed to determine the prevalence of subsequent surgery and to assess risk factors associated with subsequent ipsilateral knee surgical intervention in these patients.
Methods
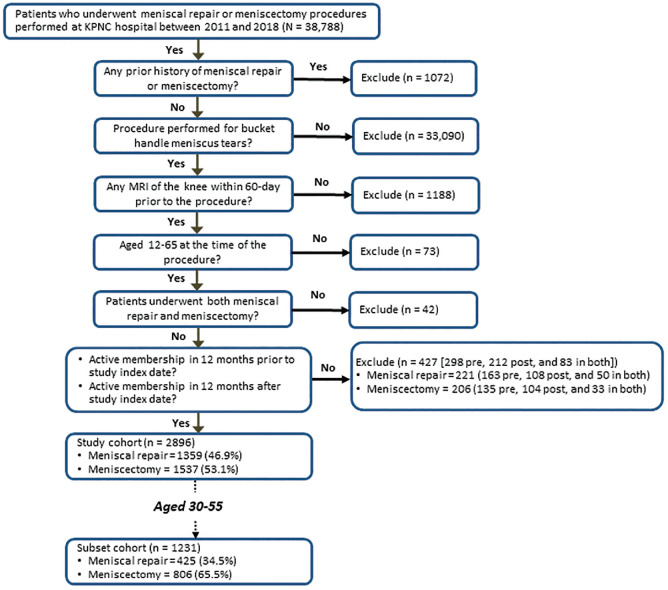
The Kaiser Foundation Research Institute's institutional review board approved our study with a waiver of consent. We performed an electronic health record search for all patients who underwent arthroscopic knee meniscal repair or meniscectomy between 2011 and 2018 (study entry period) at one of the Kaiser Permanente Northern California (KPNC) hospitals. KPNC, an integrated health care delivery system, serves >4 million members across 21 medical centers and hospitals and is representative of northern California's diverse population. 9 The study index date (or study entry) was defined as the first arthroscopic knee surgery during the study entry period. Patients who underwent ipsilateral meniscal repair or meniscectomy within 2 years before the study index date were excluded. The Current Procedural Terminology, fourth edition (CPT-4) codes and the International Classification of Disease, ninth and tenth revisions, Clinical Modification (ICD-9 and -10, respectively) procedure codes were used to identify knee meniscal repair and meniscectomy. Specifically, we used (1) CPT-4 codes 27403, 29882, and 29883, (2) ICD-9 code 81.47, and (3) ICD-10 codes 0SQC0ZZ, 0SQC3ZZ, 0SQC4ZZ, 0SXCXZZ, 0SQD0ZZ, 0SQD3ZZ, 0SQD4ZZ, and 0SQDXZZ for meniscal repair and (1) CPT-4 codes 27332, 27347, 29880, and 29881, (2) ICD-9 code 80.6, and (3) ICD-10 codes 0SBC0ZZ, 0SBC3ZZ, 0SBC4ZZ, 0SBD0ZZ, 0SBD3ZZ, and 0SBD4ZZ for meniscectomy. Natural language processing was used to search for terms of interest in the long operative notes to determine whether these surgeries were performed for BHMTs. The additional exclusion criteria included lacking magnetic resonance imaging confirming knee injury, aged younger than 12 years or older than 65 years at the time of the surgery, without active membership in the year before through the year after the index date, or had concomitant meniscectomy on study entry. A visual illustration of the study patient identification is shown in Figure 1. To ensure cohort selection accuracy, the study investigators conducted structured electronic health record review on all patients who had both meniscal repair and meniscectomy coded in their chart on study entry and a random sample of 3% of those with BHMR or BHMD only.
Figure 1.
Flowchart of the study cohort. KPNC, Kaiser Permanente Northern California; MRI, magnetic resonance imaging. Pre, no active membership in 12 months prior; Post, no active membership in 12 months after.
Patients were followed for outcomes of interest until December 31, 2019, with censoring at death or membership disenrollment (maximal study endpoint). Subsequent knee surgeries were defined as surgical interventions of the knee during follow-up including knee surgery of any type, repeat meniscal repair, and meniscectomy of the same knee (primary outcomes) or the opposite knee (secondary outcomes). Unrelated subsequent surgeries, such as microfracture, revision ACL surgery, and surgeries not related directly to the index meniscal surgery, were also included in the reoperation data to provide a comprehensive picture of patient outcomes. Additional secondary outcomes included ACLR, microfracture/chondroplasty, meniscal transplant and other interventions (eg, hardware removal, lysis of adhesions, loose body removal) of either knees, deep surgical site infections, and deep venous thrombosis or pulmonary embolism (VTE) within 30 days of study entry. Concomitant surgical interventions of interest performed at the time of index surgery included ACLR and non-ACLR (ie, microfracture/chondroplasty, meniscal transplant, and other). Patient characteristics at the study index date included age, sex, racial/ethnic groups (White, Asian [including Pacific Islanders and Native Hawaiian], Black, Hispanic/Latinx, and other), socioeconomic status, body mass index (BMI; including normal [18.5-24.9 kg/m2], overweight [25.0-29.9 kg/m2], obese [30.0-34.9 kg/m2], morbidly obese [35.0 and higher kg/m2], and unknown), Charlson Comorbidity Index score, and smoking status (current smoker or not). BMI value and smoking status closest to the index surgery and up to 1 year previously were utilized.
Descriptive statistics of patient characteristics were calculated and expressed as frequencies (proportions) or medians (interquartile range [IQR]), as appropriate. Time from surgery to (1) each of the 3 primary outcomes, (2) the first contralateral knee surgical intervention, and (3) the maximal study endpoint was calculated for each study patient. The crude rate of each outcome was calculated in (1) percentage of each study group and (2) rate per person-time (ie, per 100 person-years) for each study group; bivariate analyses were conducted using chi-square or Fisher exact tests for categorical variables (eg, sex, racial/ethnic groups, BMI groups) as appropriate, and Mann-Whitney U ([Wilcoxon rank-sum)] test for nonnormally distributed continuous variables (eg, age at study index date). P value adjustment was made using Bonferroni method when controlling for the multiple testing. Unadjusted analyses were performed to evaluate the association of each risk factor of interest with each primary outcome. To assess for risk factors associated with each primary outcome, we performed multivariable logistic regression analysis. Risk factors included in the multivariable regression analyses were either statistically significant in the unadjusted analyses or considered clinically relevant according to the study investigators’ clinical experiences. In the final regression analysis, continuous age at study index date was used instead of categorical groups.
A subset analysis was then performed isolating patients aged 30 to 50 years that was designed specifically to address an important clinical uncertainty that frequently challenges orthopaedic practitioners. The same analysis was performed in this subset including a multivariable logistic regression analysis to determine risk factors for subsequent surgeries. All statistical analyses were performed using SAS software version 9.4 (SAS) with the threshold of significance set at 2-sided P < .05.
Results
Patient Demographic and Clinical Characteristics
During the study entry period, a total of 1359 patients underwent meniscal repair surgery for a BHMT and 1537 patients for BHMD (Table 1). The median patient age for BHMR was significantly lower (24 years [IQR, 17-34 years]) compared with BHMD (38 years [IQR, 27-47 years]; P < .001). Most patients were White (52.9% total, 49.7% BHMR, and 55.7% BHMD). Median BMI was significantly lower in BHMR (25.8 kg/m2 [IQR, 23.1-29.5 kg/m2]) compared with BHMD (27.5 kg/m2 [IQR, 24.6-30.9 kg/m2]; P < .001). Smoking was more common in BHMD (12.3%) than BHMR (9.3%) (P = .01); 44.2% of BHMR had an ipsilateral ACLR at time of initial surgery compared with 30.1% of BHMD (P < .001).
Table 1.
Baseline Characteristic Comparisons a
| Characteristic | Entire Cohort (n = 2896, 100%) | Repair (n = 1359, 46.9%) | Meniscectomy (n = 1537, 53.1%) | P b |
|---|---|---|---|---|
| Age, years (median [IQR]) | 31 [21-43] | 24 [17-34] | 38 (27-47] | <.001 |
| Age groups, n (%) | <.001 | |||
| 12-29 years | 1351 (46.7) | 891 (65.6) | 460 (29.9) | |
| 30-50 years | 1231 (42.5) | 425 (31.3) | 806 (52.4) | |
| 51-65 years | 314 (10.8) | 43 (3.2) | 271 (17.3) | |
| Male, n (%) | 1940 (67.0) | 895 (65.9) | 1045 (68.0) | .22 |
| Race/ethnicity, n (%) c | .02 | |||
| White | 1531 (52.9) | 675 (49.7) | 856 (55.7) | |
| Black | 189 (6.5) | 95 (7.0) | 94 (6.1) | |
| Asian | 349 (12.1) | 183 (13.5) | 166 (10.8) | |
| Hispanic/Latinx | 665 (23.0) | 322 (23.7) | 343 (22.3) | |
| Other | 162 (5.6) | 84 (6.2) | 78 (5.1) | |
| Median household income, dollars, median [IQR] | 75,102 [54,450-100,357] | 75,769 [55,288-100,033] | 74,688 [54,288-100,481] | .70 |
| Low-income residence, n (%) d | 277 (9.6) | 123 (9.1) | 154 (10.0) | .38 |
| BMI, kg/m2, median [IQR] e | 26.6 [23.8-30.3] | 25.8 [23.1-29.5] | 27.5 [24.6-30.9] | <.001 |
| BMI, kg/m2, n (%) | <.001 | |||
| <25 | 972 (33.6) | 557 (41.0) | 415 (27.0) | |
| 25-29.9 | 1091 (37.7) | 462 (34.0) | 629 (40.9) | |
| >30 | 752 (26.0) | 280 (20.6) | 472 (30.7) | |
| Unknown | 81 (2.8) | 60 (4.4) | 21 (1.4) | |
| Charlson Comorbidity Index score ≥1, n (%) | 323 (11.2) | 135 (9.9) | 188 (12.2) | .0499 |
| Current smoker, n (%) | 315 (10.9) | 126 (9.3) | 189 (12.3) | .01 |
| Ipsilateral ACLR at time of initial surgery, n (%) | 1063 (36.7) | 600 (44.2) | 463 (30.1) | <.001 |
| Other ipsilateral knee procedure at time of initial surgery, n (%) | 501 (17.3) | 174 (12.8) | 327 (21.3) | <.001 |
ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; IQR, interquartile range.
Comparisons between 2 bucket-handle meniscal tears surgical treatment groups tested using χ2 tests for categorical variables and independent Mann-Whitney U (Wilcoxon rank-sum) test for nonnormally distributed continuous variables.
Race/ethnicity data were patient self-reported: White was defined as non-Hispanic/Latinx Caucasian; Black was defined as non-Hispanic/Latinx African Americans; Asian was defined as non-Hispanic/Latinx Asian including Pacific Islanders and Native Hawaiian; Hispanic/Latinx included any races; Other was defined as non-Hispanic/Latinx American Indians, Alaskan Natives, more than 1 race, and unknown (n = 45).
Low-income residence, address of residence in a census block with ≥20% households with income below the federal poverty level. 11
N = 2815 (1299 repair and 1516 meniscectomy).
Subsequent Ipsilateral Knee Surgery, Repeat Meniscal Repair, and Meniscectomy
The median time to the maximal study endpoint was 52.4 months (IQR, 33.5-60.0 months). During the follow-up period, a total of 656 subsequent ipsilateral procedures were performed in 393 (13.6%) patients. Significantly more subsequent surgeries were performed after BHMR (20.2%) compared with after BHMD (7.7%) (P < .001) (Table 2). The median time from study entry to subsequent surgery for BHMR was 10.6 months (IQR, 4.1-23.5 months) and for BHMD was 8.5 months (IQR, 4.0-24.5 months) (P = .55). BHMR had a significantly higher proportions of subsequent meniscal repair (4.3% vs 1%, P < .001), meniscectomy (12.1% vs 3.3%, P < .001), ACLR (7.4% vs 2.9%, P < .001), and microfracture (2.6% vs 0.9%, P = .001) while BHMD had a significantly higher proportion of arthroplasty (0.7% vs 0%, P = .001) (Table 2). Of note, 56 of the study patients had revision ACLRs (20 post-BHMD and 36 post-BHMR).
Table 2.
Subsequent Knee Surgeries Within 5 Years After Surgical Treatment a
| Entire Cohort (n = 2896, 100%) | Repair (n = 1359, 46.9%) | Meniscectomy (n = 1537, 53.1%) | P | |
|---|---|---|---|---|
| Crude rate, n (%) | ||||
| Ipsilateral knee surgery | 393 (13.6) | 274 (20.2) | 119 (7.7) | <.001 |
| Meniscal debridement/meniscectomy | 215 (7.4) | 165 (12.1) | 50 (3.3) | <.001 |
| Meniscal repair | 74 (2.6) | 59 (4.3) | 15 (1.0) | <.001 |
| Repeat index BHT repair | 109 (3.8) | 59 (4.3) | 50 (3.3) | .12 |
| Meniscal transplant | 5 (0.2) | 3 (0.2) | 2 (0.1) | .67 |
| ACLR | 145 (5.0) | 100 (7.4) | 45 (2.9) | <.001 |
| Cartilage transplant | 6 (0.2) | 4 (0.3) | 2 (0.1) | .43 |
| Microfracture/chondroplasty | 49 (1.7) | 35 (2.6) | 14 (0.9) | .001 |
| Arthroplasty | 11 (0.4) | 0 (0) | 11 (0.7) | .001 |
| Other | 151 (5.2) | 103 (7.6) | 48 (3.1) | <.001 |
| Contralateral knee surgery | 131 (4.5) | 57 (4.2) | 74 (4.8) | .42 |
| Crude rate per 100 person-years (95% CI) | ||||
| Ipsilateral knee surgery | 3.92 (3.53-4.31) | 6.24 (5.50-6.98) | 2.11 (1.73-2.49) | <.001 |
| Meniscal debridement | 2.03 (1.76-2.30) | 3.49 (2.96-4.03) | 0.85 (0.62-1.09) | <.001 |
| Meniscal repair | 0.68 (0.52-0.83) | 1.18 (0.88-1.48) | 0.25 (0.12-0.38) | .001 |
| Repeat index BHT repair | 1.00 (0.82-1.19) | 1.18 (0.88-1.48) | 0.85 (0.62-1.09) | .19 |
| Meniscal transplant | 0.05 (0.01-0.08) | 0.06 (0.00-0.12) | 0.03 (0.00-0.08) | .35 |
| ACLR | 1.36 (1.14-1.58) | 2.07 (1.66-2.47) | 0.77 (0.54-0.99) | .001 |
| Cartilage transplant | 0.05 (0.01-0.10) | 0.08 (0.00-0.15) | 0.03 (0.00-0.08) | .28 |
| Microfracture/chondroplasty | 0.45 (0.32-0.57) | 0.69 (0.46-0.92) | 0.24 (0.11-0.36) | .04 |
| Arthroplasty | 0.10 (0.04-0.16) | 0 | 0.18 (0.08-0.29) | .06 |
| Other | 1.41 (1.18-1.63) | 2.12 (1.71-2.53) | 0.82 (0.59-1.05) | .002 |
| Contralateral knee surgery | 1.21 (1.00-1.42) | 1.14 (0.84-1.43) | 1.28 (0.99-1.57) | .37 |
ACLR, anterior cruciate ligament reconstruction; BHT, bucket-handle tear; CI, confidence interval.
In the unadjusted analysis for subsequent ipsilateral knee surgery (Table 3), compared with patients aged 12 to 29 years, patients aged 30 to 50 years and 51 to 65 years had a significantly lower likelihood of subsequent surgeries. Patients with normal BMI were more likely to undergo subsequent ipsilateral knee surgery (odds ratio [OR]: 4.33, 95% confidence interval [CI]: 1.92-9.75 and OR: 2.48, 95% CI: 1.67-3.68 for meniscal repair and meniscectomy, respectively) compared with those who were obese; furthermore, overweight BMI was a significant risk factor for any ipsilateral knee surgery or for meniscal repair (OR: 1.45, 95% CI: 1.07-1.96 and OR: 2.5, 95% CI: 1.07-5.80, respectively) but not for meniscectomy (Table 3). Compared with patients treated with BHMD, patients in the BHMR group were more likely to undergo subsequent ipsilateral knee surgery of (1) any type (OR: 3.01, 95% CI: 2.39-3.78), (2) meniscal repair (OR: 4.61, 95% CI: 2.60-8.16), and (3) meniscectomy (OR: 4.11, 95% CI: 2.97-5.69). After adjusting for other risk factors, BHMR, age, and normal BMI remained significant risk factors for any subsequent ipsilateral surgery (BHMR: adjusted odds ratio [aOR]: 2.29, 95% CI: 1.79-2.93; age: aOR: 1.15, 95% CI: 1.09-2.21; normal BMI: aOR: 1.55, 95% CI: 1.13-2.12), meniscal repair (BHMR: aOR: 2.23, 95% CI: 1.27-3.93; age: aOR: 1.59, 95% CI: 1.36-1.86; normal BMI: aOR: 2.22, 95% CI: 1.01-4.85), and meniscectomy (BHMR: aOR: 2.96, 95% CI: 2.10-4.17; age: aOR: 1.18, 95% CI: 1.10-1.27; BMI: aOR: 1.73, 95% CI: 1.14-2.61).
Table 3.
Risk Factors for Subsequent Ipsilateral Surgery After Bucket-Handle Surgery a
| Any Knee Surgery | Meniscal Repair | Meniscectomy | |
|---|---|---|---|
| Unadjusted | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Meniscal repair group (reference, meniscectomy) | 3.01 (2.39-3.78) | 4.61 (2.60-8.16) | 4.11 (2.97-5.69) |
| Age (5-year decrement) | 1.22 (1.17-1.28) | 1.27 (1.19-1.36) | 1.68 (1.45-1.96) |
| Age groups, years (reference, 12-29) | |||
| 30-50 | 0.47 (0.38-0.60) | 0.18 (0.10-0.35) | 0.42 (0.31-0.57) |
| 51-65 | 0.33 (0.21-0.52) | - d | 0.30 (0.16-0.57) |
| Male | 0.89 (0.71-1.11) | 1.25 (0.75-2.09) | 1.07 (0.79-1.44) |
| Race/ethnicity (reference, White) b | |||
| Black | 1.39 (0.93-2.07) | 1.40 (0.62-3.16) | 1.00 (0.57-1.74) |
| Asian | 0.73 (0.50-1.06) | 0.74 (0.33-1.67) | 0.48 (0.27-0.85) |
| Hispanic/Latinx | 0.90 (0.69-1.18) | 0.84 (0.46-1.53) | 0.86 (0.60-1.22) |
| Other | 1.50 (0.99-2.27) | 0.92 (0.33-2.60) | 1.44 (0.86-2.44) |
| BMI, kg/m2 (reference, ≥30) | |||
| <25 | 2.08 (1.55-2.81) | 4.33 (1.92-9.75) | 2.48 (1.67-3.68) |
| 25-29.9 | 1.45 (1.07-1.96) | 2.50 (1.07-5.80) | 1.32 (0.87-2.01) |
| Unknown | 2.44 (1.34-4.44) | 5.53 (1.58-19.31) | 2.56 (1.18-5.54) |
| Low-income residence c | 1.01 (0.71-1.45) | 1.15 (0.55-2.42) | 0.64 (0.37-1.12) |
| Charlson Comorbidity Index score ≥1 | 0.98 (0.69-1.37) | 0.70 (0.30-1.62) | 1.10 (0.72-1.69) |
| Current smoker | 1.07 (0.77-1.50) | 0.85 (0.39-1.87) | 1.14 (0.74-1.75) |
| Ipsilateral ACLR | 1.01 (0.81-1.26) | 1.11 (0.69-1.79) | 0.94 (0.70-1.26) |
| Multivariable modeling | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) |
| Meniscal repair group (reference, meniscectomy) | 2.29 (1.79-2.93) | 2.23 (1.27-3.93) | 2.96 (2.10-4.17) |
| Age (5-year decrement) | 1.15 (1.09-2.21) | 1.59 (1.36-1.86) | 1.18 (1.10-1.27) |
| Male | 0.86 (0.68-1.08) | 1.21 (0.73-2.02) | 1.06 (0.78-1.44) |
| Race/ethnicity (reference, White) | |||
| Black | 1.13 (0.75-1.72) | 0.85 (0.38-1.91) | 0.80 (0.45-1.41) |
| Asian | 0.64 (0.44-0.94) | 0.64 (0.29-1.39) | 0.43 (0.24-0.75) |
| Hispanic/Latinx | 0.81 (0.61-1.08) | 0.62 (0.34-1.14) | 0.80 (0.55-1.16) |
| Other | 1.33 (0.87-2.05) | 0.73 (0.27-1.96) | 1.29 (0.76-2.21) |
| BMI, kg/m2 (reference, ≥30) | |||
| <25 | 1.55 (1.13-2.12) | 2.22 (1.01-4.85) | 1.73 (1.14-2.61) |
| 25-29.9 | 1.37 (1.01-1.88) | 2.04 (0.92-4.55) | 1.19 (0.78-1.82) |
| Unknown | 1.35 (0.72-2.52) | 1.70 (0.50-5.74) | 1.28 (0.58-2.84) |
| Low-income residence | 1.05 (0.73-1.53) | 1.27 (0.61-2.64) | 0.68 (0.39-1.19) |
| Charlson Comorbidity Index score ≥1 | 1.11 (0.78-1.58) | 0.84 (0.38-1.89) | 1.28 (0.83-1.99) |
| Current smoker | 1.27 (0.90-1.80) | 1.26 (0.58-2.73) | 1.39 (0.90-2.17) |
| Ipsilateral ACLR | 0.82 (0.65-1.03) | 0.87 (0.54-1.40) | 0.78 (0.57-1.05) |
ACLR, anterior cruciate ligament reconstruction; aOR, adjusted odds ratio; BMI, body mass index; OR, odds ratio.
Race/ethnicity data were patient self-reported: White was defined as non-Hispanic/Latinx Caucasian; Black was defined as non-Hispanic/Latinx African Americans; Asian was defined as non-Hispanic/Latinx Asian including Pacific Islanders and Native Hawaiian; Hispanic/Latinx included any races; Other was defined as non-Hispanic/Latinx American Indians, Alaskan Natives, more than 1 race, and unknown (n = 45).
Low-income residence, address of residence in a census block with ≥20% households with income below the federal poverty level.
No cohort aged 51 to 65 years experienced meniscal repair of the same knee during follow-up.
Secondary Outcomes
Before the maximal study endpoint, 4.5% of the study patients (n = 131, 57 BHMR and 74 BHMD) underwent subsequent surgery of the opposite knee and the median time from the index BHMT surgical treatment to their contralateral knee surgery was 23.9 months (IQR, 12.3-34.3 months) in the BHMR group and 17.1 months (IQR, 7.1-30.9 months) in the BHMD group (P = .11). Very few patients (n = 21, 0.7%) had either deep surgical site infections or VTE within 30 days of study index date, including 6 (0.2%) with infection and 15 (0.5%) with VTE.
30- to 50-Year-Old Subgroup Analysis
When isolating only to 1231 patients aged 30 to 50 years at time of index procedure (425 [34.5%] in the BHMR group and 806 [65.5%] in the BHMD group), median age in the BHMR group (38 years [IQR, 33-43 years]) remained significantly lower compared with the BHMD group (40 years [IQR, 35-45 years]) (P < .001). A significantly higher proportion of BHMR had normal BMI (33.7%) versus BHMD (21.1%) (P < .001) as well as higher proportion of ipsilateral ACLR at time of index surgery (40.5% BHMR vs 28% BHMD, P < .001). Multivariable analysis results showed the BHMR group was more likely to experience a subsequent ipsilateral knee surgery than the BHMD group (aOR: 2.34, 95% CI: 1.60-3.50). Furthermore, there was a significantly higher likelihood of subsequent meniscal repair (aOR: 5.33, 95% CI: 1.67-17.04) or meniscectomy (aOR: 3.17, 95% CI: 1.84-5.46).
Discussion
In this large retrospective cohort study, we demonstrated that, without controlling for other covariates, ipsilateral subsequent knee surgeries occurred 3 times as often in patients undergoing BHMR compared with BHMD. Patients aged 12 to 29 years and normal and overweight BMI were associated with increased odds of any ipsilateral reoperation.
Our rate of subsequent surgery after BHMR (20.2%) was similar to rates reported in other studies.26,31 In a recent meta-analysis looking at all-cause meniscal repairs, Schweizer et al 26 found a 19% risk of failure with minimum 5-year follow-up but found a significantly lower failure rate with inside-out repair compared with all-inside repair (5.6% vs 22.3%, P = .009). Another recent study showed that, despite a BHMR failure rate of 33% at a median time of 19 months (IQR, 6-39 months), successful repairs had higher patient-reported outcomes and significantly less osteoarthritis in comparison with failed repairs. 12 This is in contrast to Shelbourne et al, 27 who found no significant difference between BHMR and BHMD. Our study showed a much greater rate of subsequent surgeries if a BHMR was performed as the index surgery. This may be a point to include when counseling patients, as outcomes after BHMD may not be significantly or clinically better than BHMR, but there is a significantly higher risk of reoperation after BHMR.
Our study identified younger age at time of index surgery as a risk factor for undergoing initial BHMR versus BHMD. This may be due to surgeon preference to repair a meniscus in a younger person who may have more healing potential. 34 Another possible explanation is an evolving body of evidence documenting the deleterious long-term effects of meniscectomy in younger patients. A recent meta-analysis by Mosich et al 19 found that all included studies regarding meniscectomy demonstrated unsatisfactory outcomes in terms of pain, stiffness, range of motion, and rate of subsequent osteoarthritis. In addition, the meniscus becomes more degenerative as we age, which may lead to difficulties with a repair as the patient ages. Interestingly, while the trend is to attempt BHMR for younger patients, age is also a risk factor for increase in subsequent surgery for both BHMR and BHMD. We speculate that this is likely secondary to overall higher activity levels in younger patients, 17 in addition to their disproportionate participation in higher demand activities involving rapid acceleration/deceleration, jumping, or changes in direction, leaving them vulnerable to sustaining a recurrent meniscal injury after undergoing meniscal surgery. 23 Furthermore, we performed a subset analysis on patients between the ages of 30 and 50 years. Whereas the treatment pathways for younger and older patients are generally well established—favoring meniscal repair in younger patients due to their higher regenerative capacity and partial meniscectomy in older patients owing to their increased likelihood of coexisting degenerative changes—the optimal strategy for middle-aged patients remains ambiguous. Unlike the 66% of younger (aged 18-29 years) patients who underwent BHMR, only 31% underwent BHMR in the 30- to 50-year-old subset. After adjusting for all risk factors, only BHMR was a significant risk factor for any subsequent surgery (2.3 times), subsequent meniscal repair (5.3 times), and subsequent meniscectomy (3.2 times).
In our study, BMI was a significant risk factor as we noted a 2.2 times (BHMR) and 1.7 times (BHMD) risk of subsequent surgery in patients with normal BMI compared with obese BMI. The effects of BMI on reoperation rates are poorly reported in the literature, with few studies available describing either increased or decreased risk of reoperation after meniscal repair.14,29 In addition, Shieh et al 28 and Patel et al 22 did not find BMI to have a significant association with revision meniscal surgery in pediatric populations, and Saltzman et al 25 had similar findings in an adult population of BHMTs. These studies had significantly fewer reported patients undergoing reoperation compared with our study, which may have left them underpowered to detect differences based on patient BMI. While BMI was identified as a significant risk factor for subsequent surgery in our dataset, the relationship could be influenced by confounding variables. Increased activity levels and physical demands, typically associated with a normal BMI, could be risk factors that account for difference in reoperation.
Concomitant ACLR has been reported to reduce the risk of subsequent surgery after meniscal repairs.2,6,13,15,20,21,25,35 In a population study by Wasserstein et al 32 from a universal healthcare system, 1332 patients who underwent meniscal repair and ACLR were matched with 1239 patients who underwent isolated meniscal repair. They found that the rate of meniscal reoperation was approximately twice as high for the meniscal repair alone cohort as compared with the combined procedure cohort (16.7% vs 9.7%, respectively) with ACLR independently associated with lower rates of reoperation on regression analysis (OR: 0.57, P < .0001). Several factors may lead to this, including a longer rehabilitation period in patients with ACLR promoting a prolonged low-stress intra-articular environment, biologic augmentation gained through drilling bone tunnels for graft placement, 4 and improved anterior-posterior rotatory stability gained after ACLR.30,36 While our study did not show a significant reduction in subsequent surgery after concomitant ACLR, further investigation into how a variety of factors influence BHMT repair success in the setting of concomitant ACLR is warranted.
BHMR can be performed via several different methods (inside-out repair, outside-in repair, and all-inside repair) with the gold standard being inside-out repair.20,25 Our study was limited in that we were not able to capture the method of fixation for BHMR. However, recent studies have been unable to show a significant difference in failure rates, functional outcome scores, or complication rates when comparing modern all-inside devices with inside-out repair.2,7
Limitations
Although this study represents one of the largest comparative studies on BHMR versus BHMD, our study had several limitations. Given the retrospective nature of the study, we were not able to collect patient-reported outcomes or other data not accessible by electronic chart review. While these data were generated from a closed, high-retention health care system, some patients may have left the system before undergoing a subsequent surgery. In addition, we were not able to comment on certain factors that may affect the success of BHMT repair, including medial versus lateral tear, tear chronicity, tear size, repair device utilized, number of sutures, and repair technique. We recognize that the observational design of our study limits our ability to draw causal conclusions. We believe that future research, including potentially randomized controlled trials incorporating modern repair techniques and long-term rehabilitation strategies, would provide a more comprehensive understanding of the risks and benefits associated with BHMR and BHMD. Despite these limitations, this study aids physicians in counseling middle-aged patients who are considering repair versus debridement for BHMT. It is worth discussing that our study included all subsequent reoperations, not necessarily those related directly to the meniscal surgery itself. This could potentially inflate the reoperation rates reported and may include surgeries influenced by other independent factors. Therefore, while our study offers valuable data on reoperation rates, these should be interpreted cautiously, especially when counseling patients on the long-term outcomes of either BHMR or BHMD.
It is important to note that reoperation rates are just one facet of the larger picture. The long-term risks associated with meniscal insufficiency after BHMD, such as the potential for accelerated cartilage degeneration and osteoarthritis, are significant considerations that were not captured in this study. In addition, patient-reported outcomes become crucial when comparing quality of life, pain management, and functional status in the long term for both treatment options. Such patient-reported outcomes would provide a more comprehensive comparison of the advantages and disadvantages associated with BHMR and BHMD, beyond reoperation rates.
Conclusion
To our knowledge, this is the largest reported contained patient cohort study on outcomes after BHMR versus BHMD. BHMR was more often performed in younger patients with a lower BMI, especially during a concomitant ACLR. Patients after BHMR were more likely to undergo subsequent surgeries, with the likelihood decreasing with increasing age. Subset analyses showed increasing risk for subsequent surgeries with BHMR versus BHMD in the 30- to 50-year-old cohort.
Footnotes
Final revision submitted February 7, 2024; accepted March 4, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research support was received from Kaiser Foundation Community Benefits Grant. M.W.H. has received education payments from Evolution Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Kaiser Permanente Northern California (ref No. 00001045).
ORCID iD: David Y. Ding  https://orcid.org/0000-0002-8423-7245
https://orcid.org/0000-0002-8423-7245
References
- 1. Ahn JH, Kim KI, Wang JH, Kyung BS, Seo MC, Lee SH. Arthroscopic repair of bucket-handle tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):205-210. [DOI] [PubMed] [Google Scholar]
- 2. Ardizzone CA, Houck DA, McCartney DW, Vidal AF, Frank RM. All-inside repair of bucket-handle meniscal tears: clinical outcomes and prognostic factors. Am J Sports Med. 2020;48(13):3386-3393. [DOI] [PubMed] [Google Scholar]
- 3. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14(4):270-275. [DOI] [PubMed] [Google Scholar]
- 4. de Girolamo L, Galliera E, Volpi P, et al. Why menisci show higher healing rate when repaired during ACL reconstruction? Growth factors release can be the explanation. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):90-96. [DOI] [PubMed] [Google Scholar]
- 5. Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford). 2001;40(6):631-639. [DOI] [PubMed] [Google Scholar]
- 6. Espejo-Reina A, Serrano-Fernandez JM, Martin-Castilla B, Estades-Rubio FJ, Briggs KK, Espejo-Baena A. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy. 2014;30(4):492-496. [DOI] [PubMed] [Google Scholar]
- 7. Fillingham YA, Riboh JC, Erickson BJ, Bach BR, Jr, Yanke AB. Inside-out versus all-inside repair of isolated meniscal tears: an updated systematic review. Am J Sports Med. 2017;45(1):234-242. [DOI] [PubMed] [Google Scholar]
- 8. Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health. 2012;4(4):340-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gordon NC. Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2011 California Health Interview Survey. https://memberhealthsurvey.kaiser.org/Documents/chis_non_kp_2011.pdf
- 10. Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168-176. [DOI] [PubMed] [Google Scholar]
- 11. Holmen JE, Kim L, Cikesh B, et al. Relationship between neighborhood census-tract level socioeconomic status and respiratory syncytial virus-associated hospitalizations in U.S. adults, 2015-2017. BMC Infect Dis. 2021;21(1):293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kalifis G, Raoulis V, Panteliadou F, Liantsis A, D’Ambrosi R, Hantes M. Long-term follow-up of bucket-handle meniscal repairs: chondroprotective effect outweighs high failure risk. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2209-2214. [DOI] [PubMed] [Google Scholar]
- 13. Kimura M, Shirakura K, Hasegawa A, Kobuna Y, Niijima M. Second look arthroscopy after meniscal repair. Factors affecting the healing rate. Clin Orthop Relat Res. 1995;(314):185-191. [PubMed] [Google Scholar]
- 14. Laurendon L, Neri T, Farizon F, Philippot R. Prognostic factors for all-inside meniscal repair. A 87-case series. Orthop Traumatol Surg Res. 2017;103(7):1017-1020. [DOI] [PubMed] [Google Scholar]
- 15. Majeed H, Karuppiah S, Sigamoney KV, Geutjens G, Straw RG. All-inside meniscal repair surgery: factors affecting the outcome. J Orthop Traumatol. 2015;16(3):245-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Marchetti DC, Phelps BM, Dahl KD, et al. A contact pressure analysis comparing an all-inside and inside-out surgical repair technique for bucket-handle medial meniscus tears. Arthroscopy. 2017;33(10):1840-1848. [DOI] [PubMed] [Google Scholar]
- 17. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213-218. [DOI] [PubMed] [Google Scholar]
- 18. Moses MJ, Wang DE, Weinberg M, Strauss EJ. Clinical outcomes following surgically repaired bucket-handle meniscus tears. Phys Sportsmed. 2017;45(3):329-336. [DOI] [PubMed] [Google Scholar]
- 19. Mosich GM, Lieu V, Ebramzadeh E, Beck JJ. Operative treatment of isolated meniscus injuries in adolescent patients: a meta-analysis and review. Sports Health. 2018;10(4):311-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nobile F, Condello V, Madonna V, et al. All-inside repair of meniscal bucket handle tears: a retrospective study at mean 4-years follow-up evaluation. J Biol Regul Homeost Agents. 2020;34(4)(suppl 3):183-190. [PubMed] [Google Scholar]
- 21. Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16(8):822-829. [DOI] [PubMed] [Google Scholar]
- 22. Patel NM, Mundluru SN, Beck NA, Ganley TJ. Which factors increase the risk of reoperation after meniscal surgery in children? Orthop J Sports Med. 2019;7(5):2325967119842885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34(4):252-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roos H, Lauren M, Adalberth T, Roos EM, Jonsson K, Lohmander LS. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41(4):687-693. [DOI] [PubMed] [Google Scholar]
- 25. Saltzman BM, Cotter EJ, Wang KC, et al. Arthroscopically repaired bucket-handle meniscus tears: patient demographics, postoperative outcomes, and a comparison of success and failure cases. Cartilage. 2020;11(1):77-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schweizer C, Hanreich C, Tscholl PM, et al. Nineteen percent of meniscus repairs are being revised and failures frequently occur after the second postoperative year: a systematic review and meta-analysis with a minimum follow-up of 5 years. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2267-2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shelbourne KD, Dersam MD. Comparison of partial meniscectomy versus meniscus repair for bucket-handle lateral meniscus tears in anterior cruciate ligament reconstructed knees. Arthroscopy. 2004;20(6):581-585. [DOI] [PubMed] [Google Scholar]
- 28. Shieh AK, Edmonds EW, Pennock AT. Revision meniscal surgery in children and adolescents: risk factors and mechanisms for failure and subsequent management. Am J Sports Med. 2016;44(4):838-843. [DOI] [PubMed] [Google Scholar]
- 29. Sommerfeldt MF, Magnussen RA, Randall KL, et al. The relationship between body mass index and risk of failure following meniscus repair. J Knee Surg. 2016;29(8):645-648. [DOI] [PubMed] [Google Scholar]
- 30. Sonnery-Cottet B, Saithna A, Blakeney WG, et al. Anterolateral ligament reconstruction protects the repaired medial meniscus: a comparative study of 383 anterior cruciate ligament reconstructions from the SANTI study group with a minimum follow-up of 2 years. Am J Sports Med. 2018;46(8):1819-1826. [DOI] [PubMed] [Google Scholar]
- 31. Thaunat M, Fournier G, O’Loughlin P, et al. Clinical outcome and failure analysis of medial meniscus bucket-handle tear repair: a series of 96 patients with a minimum 2 year follow-up. Arch Orthop Trauma Surg. 2020;140(11):1649-1654. [DOI] [PubMed] [Google Scholar]
- 32. Wasserstein D, Dwyer T, Gandhi R, Austin PC, Mahomed N, Ogilvie-Harris D. A matched-cohort population study of reoperation after meniscal repair with and without concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(2):349-355. [DOI] [PubMed] [Google Scholar]
- 33. Wright DH, De Smet AA, Norris M. Bucket-handle tears of the medial and lateral menisci of the knee: value of MR imaging in detecting displaced fragments. AJR Am J Roentgenol. 1995;165(3):621-625. [DOI] [PubMed] [Google Scholar]
- 34. Yang BW, Liotta ES, Paschos N. Outcomes of meniscus repair in children and adolescents. Curr Rev Musculoskelet Med. 2019;12(2):233-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yeo DYT, Suhaimi F, Parker DA. Factors predicting failure rates and patient-reported outcome measures after arthroscopic meniscal repair. Arthroscopy. 2019;35(11):3146-3164.e2. [DOI] [PubMed] [Google Scholar]
- 36. Zaffagnini S, Signorelli C, Bonanzinga T, et al. Does meniscus removal affect ACL-deficient knee laxity? An in vivo study. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3599-3604. [DOI] [PubMed] [Google Scholar]