Abstract
Background
The newborn and infant continuum of care such as essential newborn care, early initiation and exclusive breastfeeding, and immunisation are highly recommended for improving the quality of life and survival of infants. However, newborn and infant mortality remains high across Sub-Saharan African countries. While unintended pregnancies are associated with adverse newborn and infant health outcomes, there is inconclusive evidence on whether pregnancy intention influences newborn and infant continuum of care completion. Therefore, this review aimed to pool findings reported in the literature on the association between pregnancy intention and newborn and infant health care across the continuum of care in Sub-Saharan Africa.
Methods
We searched MEDLINE Complete, EMBASE, CINAHL Complete, and Global Health databases for studies potentially eligible for this systematic review and meta-analysis. Two researchers independently screened the identified articles by abstract and title, and then full-text using Covidence. We used the Newcastle–Ottawa Scale to assess the quality of the included studies. The Cochran’s Q test and I2 were executed to detect and quantify the presence of statistical heterogeneity in the studies. Meta-analysis was done for each outcome when more than one original study reported relevant data, using Stata statistical software version 18.
Results
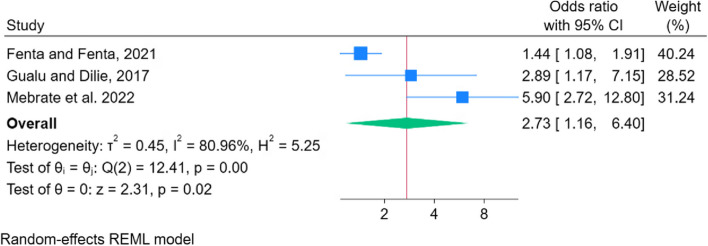
Eleven studies were included from a total of 235 articles identified by the search. The odds of completing essential newborn care (pooled odds ratio: 3.04, 95% CI: 1.56, 5.90), early initiation of breastfeeding (pooled odds ratio: 1.30, 95% CI: 1.13, 1.52), exclusive breastfeeding (pooled odds ratio: 2.21, 95% CI: 1.68, 2.89), and being fully immunised (pooled odds ratio: 2.73, 95% CI: 1.16, 6.40) were higher among infants born to women with intended pregnancies as compared to women with unintended pregnancies.
Conclusion
Intended pregnancy was positively associated with essential newborn care completion, early initiation and exclusive breastfeeding, and full immunisation of infants in SSA countries. Thus, policy-makers and stakeholders should strengthen the provision of quality family planning services to prevent unintended pregnancy. Furthermore, follow-up of women with unintended pregnancies is needed to increase women’s opportunity to access essential newborn health care services that further reduce the risk of newborn and infant morbidity and mortality.
Systematic review registration
PROSPERO registration number CRD42023409148.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12887-024-05036-y.
Keywords: Intended pregnancy, Unintended pregnancy, Essential newborn care, Breastfeeding, Immunisation, Sub-Saharan Africa, Systematic review
Introduction
Improving the quality of life and survival chances of newborns, and children remains an urgent global challenge [1]. Worldwide, considerable progress has been made to reduce neonatal mortality from 5 million in 1990 to 2.4 million in 2019 [2], and under-five mortality from 12.5 million in 1990 to 5.3 million in 2018 [2]. However, substantial differences in child mortality continue to exist across regions where Sub-Saharan Africa (SSA) holds the highest perinatal mortality rates of 34.7 deaths per 1,000 live births [3], infant mortality rate of 53 deaths per 1,000 live births [4], and under-five mortality rate of 78 deaths per 1,000 live births [2]. In addition, about 41% of children in SSA are highly affected by stunting, which possibly contributes to increasing child morbidity and mortality [5]. Many of these deaths are preventable or curable using interventions that are simple and cost-effective such as adequate nutrition, vaccination, and appropriate newborn and infant care [6, 7] as well as by improving access to maternal health care services [8].
Parental adherence to children’s preventive and curative health care sets children up for better long-term health and considerably reduces the risk for child morbidity and mortality [9–11]. Similarly, maternal pregnancy intention has a significant effect on parent–child attachment and bonding, with a potential impact on children’s long-term physical, developmental, and psychological health outcomes [12–14]. Women with unintended pregnancies face more difficulty in establishing a strong attachment with their babies, poor childcare practices, and breastfeeding difficulties [12, 15, 16]. Literature has shown that children born to mothers with unintended pregnancies had less secure mother-to-child attachment during infancy, poor preventive and curative care, and poor behavioural and educational outcomes than women with intended pregnancies [12, 16, 17]. In addition, unintended pregnancy was associated with childhood illness, stunting and underweight, and higher risks of infant and child mortality [16, 18]. Furthermore, adverse birth outcomes, such as congenital anomalies, preterm birth, and low birthweight were observed among children born from unintended pregnancies [18, 19]. Conversely, intended pregnancy was associated with a reduced risk of stillbirth compared to unintended pregnancies [14].
Mounting evidence has shown that women who experienced unintended pregnancy had lower likelihoods of timely initiation of breastfeeding, continuing to breastfeed, and exclusive breastfeeding than women with intended pregnancy [20, 21], resulting in poorer physical health of their children [13]. Furthermore, children born from unintended pregnancy were less likely to receive childhood immunisation [20, 22, 23]. These effects could be caused by maternal behaviours during pregnancy, and late initiation, or low use of antenatal care [24–27]. Hence, the prevention of unintended pregnancy and effective implementation of the maternity continuum of care are highly recommended to enhance the survival of newborns and infants through promoting preventive health care practices for children [28, 29]. A recent study has shown that completing the maternity continuum of care, which includes the use of antenatal care, birthing at health facility, and use of postnatal care can considerably improve the use of essential newborn care practices [30].
The World Health Organization and United Nations Children’s Fund [2, 31] strongly recommended strategies for the newborn and infant continuum of care, such as exclusive and timely initiation of breastfeeding, improving child nutrition, and child vaccination. This is anticipated to achieve the Sustainable Development Goal aimed to decrease the high rates of neonatal deaths to 12 per 1000 live births and under-five deaths to 25 per 1000 live births by 2030 [32, 33]. Though strong emphasis has been given to the newborn and infant continuum of care, in SSA, only 56.5% of children were fully vaccinated [34], 47% of infants were breastfed within one hour of birth and 35% of children received exclusive breastfeeding in the first six months of life [35]. However, none of these studies have analysed the association between maternal pregnancy intention and completion of the newborn and infant continuum of care including essential newborn care practices, exclusive and timely initiation of breastfeeding, and infant immunisation. Moreover, while unintended pregnancies are associated with adverse newborn and infant health outcomes, there is inconsistent and inconclusive evidence on whether pregnancy intention influences newborn and infant health care across the newborn and infant continuum of care.
Up-to-date evidence with pooled estimates is required to understand whether developing interventions targeting preventing unintended pregnancies with the aim of child survival is required. Therefore, this study aimed to pool findings reported in literature on the association between pregnancy intention and essential newborn and infant health care across the newborn and infant continuum of care in SSA to contribute reliable evidence that would inform newborn and infant health policy and practice.
Methods
Registration and reporting
We used the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [36] to prepare and report this review (Supplementary File 1). After checking for a lack of other similar existing reviews and protocols, this systematic review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42023409148.
Information sources and search strategy
The search terms were prepared based on the following concepts: pregnancy intention, essential newborn care practice, early initiation of breastfeeding, exclusive breastfeeding, full immunisation status, and Sub-Saharan Africa. The search keywords included free text keywords and Medical Subject Headings (MeSH) using Boolean operators, truncation, wildcards, and phrases in various databases. A comprehensive literature search was done in major databases such as MEDLINE Complete (EBSCOhost platform), EMBASE, CINAHL Complete (EBSCOhost platform), and Global Health (EBSCOhost platform) on August 13, 2023. These databases were selected as they index health and medical-related research. Furthermore, bibliographies of reviews and the identified studies were reviewed in Google Scholar for potentially relevant studies. The EBSCOhost MEDLINE was used to develop the initial search strategy, which was then adapted for other databases. Details of search strategies for each database are provided in Supplementary File 2. A scholarly expert librarian reviewed the search plans and provided advice to improve the search.
Eligibility criteria
Inclusion criteria
We included observational studies that reported essential newborn care practice, or early initiation of breastfeeding, or exclusive breastfeeding, or child immunisation status as an outcome variable and pregnancy intention as an exposure variable. Furthermore, we included peer-reviewed studies published in the English language and conducted in SSA countries. Moreover, studies that reported the odds ratios (OR) with a 95% confidence interval (CI) or have raw data that allowed us to calculate the odds ratios with a 95% confidence interval were included.
Exclusion criteria
We excluded studies that did not report the associations of pregnancy intention with essential newborn care practice, or early initiation of breastfeeding, or exclusive breastfeeding, and full immunisation status. Review articles, qualitative studies, case reports, commentaries, case studies, conference abstracts, case series, and opinion pieces were excluded.
Study selection
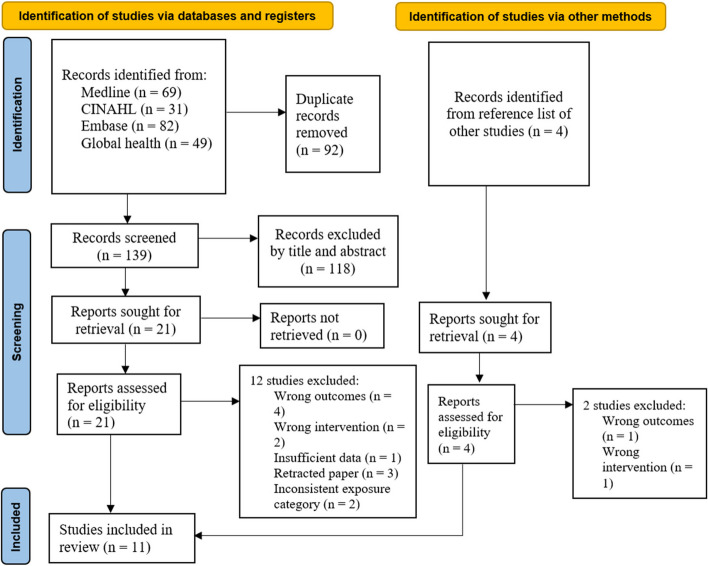
We used Covidence systematic review software to screen studies. Two researchers (BDM, VV) independently conducted title and abstract screening after removing duplicates. Similarly, potentially eligible studies for full-text review were retrieved and then systematically screened against the eligibility criteria. The third reviewer (AGB) resolved any conflicts during the screening process. The results of the search in each database, screening, and selection process are summarised in a PRISMA 2020 flow diagram (see Fig. 1).
Fig. 1.
PRISMA flow diagram of the studies screening process
Quality assessment
Two researchers (BDM, AGB) assessed the quality of each primary study using the Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomised studies [37], with no discrepancies observed. The NOS tool has selection, comparability, and outcome domains and rate articles with a maximum of ten stars. The selection domain focuses on sample size, representativeness of the target population, response rate, and ascertainment of risk factors with a maximum of five stars. The comparability domain focuses on controlling the confounding factors that potentially influence the outcome of the variable with a maximum of two stars. The outcome domain assesses the outcomes of interest and appropriateness of the statistical tests with a maximum of three stars. The quality of the studies was ranked based on the overall number of stars. Accordingly, studies with a star number of 9 or 10, 7 or 8, and 5 or 6 were deemed to be very-good quality, good quality, and satisfactory quality respectively (Suplementary file 3). Studies with four or less stars were deemed unsatisfactory quality and were to be excluded from the review due to poor quality. The NOS tool has been used in previous similar studies [38–40].
Data extraction
Two researchers (BDM, VV) independently extracted data in a Microsoft Excel spreadsheet. No discrepancies occurred during data extraction. All relevant data items such as author(s), study setting and design, sample size, study population, data collection methods, response rate, publication year, odds ratio with a 95% CI for the association of pregnancy intention with each of the four outcome variables (essential newborn care, early initiation of breastfeeding, exclusive breastfeeding, and full immunisation status), and the definition of all four outcome variables were extracted from each included study. The pregnancy intention of participants was also extracted for each outcome variable.
Outcome measurement
The association between pregnancy intention and newborn and infant health care across the continuum of care was the outcome of interest in this review. For this research, the newborn and infant health continuum of care includes essential newborn care, early initiation of breastfeeding, exclusive breastfeeding, and full immunisation status. Essential newborn care is defined in this research as the newborn has received all the recommended elements of the services, including safe cord care, initiating skin-to-skin contact, eye care, and delayed baby bathing for at least 24 h after birth [41]. Early initiation of breastfeeding is defined as the provision of mother’s breast milk to the baby within the first hour of birth [42]. Exclusive breastfeeding is defined as an infant receiving only breast milk from birth until six months of age without adding water or any other food except for mineral supplements, vitamins, or prescribed medicines [42]. Full immunisation is defined as a child who has received a single dose of Bacillus Calmette–Guérin (BCG) vaccine, four poliomyelitis vaccines, three doses of pentavalent vaccines (diphtheria, pertussis, tetanus, hepatitis B and Haemophilus influenza type B), three doses of pneumococcal conjugate vaccine (PCV), two doses of Rota vaccine, and one dose of measles vaccine before their first birthday [43].
Pregnancy intention has been classified into intended and unintended [44]. For this study, intended pregnancy was when the woman reported that she planned or wanted her last pregnancy at the time of conception; otherwise, a pregnancy is considered an unintended pregnancy. Both unwanted pregnancies (no children are desired at all) and mistimed pregnancies (wanted at some time but occurred sooner than desired) were considered as unintended pregnancies [45].
Data analysis
The adjusted odds ratios (AOR) of the association between pregnancy intention and each outcome variable were extracted from each primary study as the measure of effect. For the outcome of early initiation of breastfeeding, the crude odds ratios (COR) and confidence intervals were calculated from the raw data. The COR was used for the outcome of early initiation of breastfeeding due to the lack of AOR data in the included studies. Since COR was calculated from all included studies for this outcome, this approach ensured that we did not mix AOR with COR in the same analysis. Logit transformations were made for the individual measure of effect before computing the pooled summary. When two or more studies reported relevant data, a quantitative meta-analysis was done for each outcome. Forest plots and tables are used to graphically display the summary of effect sizes with 95% CI and other results. The random-effects model was employed for the outcomes of essential newborn care, early initiation breastfeeding and child immunisation status. The random-effect model was employed to assume the variations or heterogeneity in the effect estimates across the studies [46, 47]. For the outcome of exclusive breastfeeding, the fixed effects model was used as the number of included studies was only two, which makes it inappropriate to perform the random-effects model because the precision in estimating variability in studies is limited [46, 48]. The weight of each study in the pooled estimates was calculated using the inverse of the variance. The potential variation between the primary studies was statistically estimated using Cochran’s Q test and quantified by I2 with significant heterogeneity to be deemed at p-value < 0.1 or I2 > 50% [49, 50]. Since very few studies were included in the meta-analysis of each outcome, publication bias, subgroup analysis, and sensitivity analysis were not conducted [48, 51]. In this analysis, early initiation of breastfeeding, while a component of essential newborn care, was analysed separately to better understand how pregnancy intention specifically influences this practice. The studies used for the early initiation of breastfeeding analysis differed from those included in the broader essential newborn care analysis, ensuring that our findings on early initiation are based on a unique set of data. Furthermore, unwanted and mistimed pregnancies were used interchangeably if the original studies had reported one of the two instead of unintended pregnancy. Likewise, wanted and planned pregnancy were used interchangeably if the original studies had reported one of the two instead of intended pregnancy. All statistical analyses were executed using Stata statistical software version 18.
Results
The database searches produced a total of 231 records, with a further 4 articles identified from manual searches of bibliographies of relevant studies. After a comprehensive screening, eleven studies met the inclusion criteria and retained for the review [52–62]. The steps and outcomes of the study selection process are shown in the PRISMA flow diagram (see Fig. 1).
Studies characteristics
All the studies included in the review used cross-sectional study designs and were published between 2016 and 2022. A total of 18,781 study participants were involved in the original studies. Many studies (n = 9) were set in Ethiopia [52–54, 56, 57, 59–62]. Eight studies collected the data via face-to-face surveys developed from literature reviews [52–54, 57–60, 62], two studies used the demographic and health survey [56, 61], and the remaining one study used data from multiple indicator cluster survey [55]. Of the included studies in the review, eight studies employed multistage random sampling [52–56, 58, 59, 61], two studies used systematic random sampling [60, 62], and one study used simple random sampling to collect data [57]. Almost all (n = 10) of the studies were of good quality methodological rigour (7 or 8 stars) on the NOS assessment. The summary of the 11 papers is shown in Table 1.
Table 1.
Characteristics of studies included in the review of the association between pregnancy intention and newborn and infant continuum of care in SSA, 2023
| Authors, year | Study country | Study design | Study population | Sample size | NOS score | Reported outcome type | Outcome prevalence (%) | Pregnancy intention | Association of outcome with pregnancy intention (OR) | Controlled confounding factors | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intended (%) | Unintended (%) | ||||||||||
| Alemu and Eshete, 2020 [53] | Ethiopia | Cross-sectional | Mothers who had infants under six months of age | 834 | 8 | Essential newborn care | 24.1 | 72.3 | 27.7 | 1.7 (1.2, 2.2) | Maternal education, employment, birth interval, and antenatal care |
| Chichiabellu et al. 2018 [54] | Ethiopia | Cross-sectional | Reproductive-age women who had given birth at home | 450 | 8 | Essential newborn care | 24 | 14.9 | 85.1 | 7.0 (3.73, 11.81) | Receive antenatal care, advice about essential newborn care, postnatal care visits, residence, birth preparedness, knowledge about newborn danger signs, and knowledge about newborn care |
| Habte et al. 2022 [52] | Ethiopia | Cross-sectional | Mothers who had infants under six months of age | 818 | 8 | Essential newborn care | 33.1 | 77.6 | 22.4 | 2.66 (1.56, 4.51) | Mother’s age, mother’s educational level, wealth index, family size, parity, birth preparedness and complication readiness plan, mode of delivery, timing of postnatal visits, knowledge on danger signs, time to reach nearby health facility, and attending monthly pregnant women conference |
| Apanga and Kumbeni, 2021 [55] | Ghana | Cross-sectional | Mothers of children aged less than two years | 3,466 | 7 | Early initiation of breastfeeding | 52.3 | 51 | 49 | 1.19 (1.04, 1.36) | Not adjusted |
| Gebremeskel et al. 2019 [57] | Ethiopia | Cross-sectional | Mothers of children aged less than 12 months | 809 | 7 | Early initiation of breastfeeding | 61.9 | 81 | 19 | 1.8 (1.25, 2.57) | Not adjusted |
| Gedefaw et al. 2020 [56] | Ethiopia | Cross-sectional | Mothers of children under five years of age | 7,115 | 8 | Early initiation of breastfeeding | 75 | 74 | 26 | 1.3 (1.15, 1.49) | Not adjusted |
| Duarte Lopes et al. 2022 [58] | Cape Verde | Cross-sectional | Mothers of children aged under two years | 1,765 | 8 | Exclusive breastfeeding | 32.5 | - | - | 1.06 (0.73, 1.54) | Maternal age, education, marital status, family income, residence, parity, prenatal care, number of prenatal visits, maternity leave, child’s birth weight, breastfeeding in the first hour after delivery |
| Mamo et al. 2020 [59] | Ethiopia | Cross-sectional | Mothers with infants aged 6–9 months | 725 | 8 | Exclusive breastfeeding | 65.4 | 61.3 | 38.7 | 4.73 (3.22, 6.95) | Marital status, residence, antenatal care, postnatal care attendance, mode of delivery, counselling on exclusive breastfeeding, sex of the child |
| Fenta and Fenta, 2021 [61] | Ethiopia | Cross-sectional | Women with children aged 12–23 months | 1,929 | 9 | Child’s immunisation status | 48.6 | 80.1 | 19.9 | 1.44 (1.08, 1.91) | Maternal education status, number of antenatal care visits, place of delivery, presence of vaccination card, maternal occupation, husband education status, husband occupational status, religion, wealth index, mother tetanus injections received, place of residence, community-level maternal education, community-level wealth index, community-level media exposure, the place of delivery, region |
| Gualu and Dilie, 2017 [62] | Ethiopia | Cross-sectional | Mothers with children aged 12–23 months | 298 | 8 | Child’s immunisation status | 91.7 | 78.8 | 21.2 | 2.89 (1.17, 7.17) | Mother’s occupational status, child’s sex, place of delivery, antenatal care, knowledge of time of vaccination schedule, and distance from the vaccination site |
| Mebrate et al. 2022 [60] | Ethiopia | Cross-sectional | Mothers with children aged 12–23 months | 664 | 8 | Child’s immunisation status | 72.6 | 93.3 | 6.7 | 5.9 (2.4, 11.3) | Mother’s age, educational status of the mother, district number of antenatal care visits, at least one postnatal care by a health care worker, number of children the mother has, child’s age in months, attitude to vaccination, knowledge of vaccination schedule |
Association between pregnancy intention and newborn and infant continuum of care
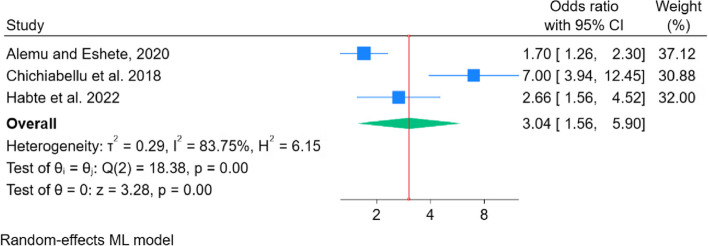
Three studies examined the association between pregnancy intention and essential newborn care practice [52–54]. The results of the meta-analysis showed that women whose pregnancy was intended were about three times (AOR: 3.04, 95% CI: 1.56, 5.90) more likely to practice essential newborn care as compared to women with unintended pregnancy (Fig. 2).
Fig. 2.
Pooled odds ratio of the association between essential newborn care and pregnancy intention
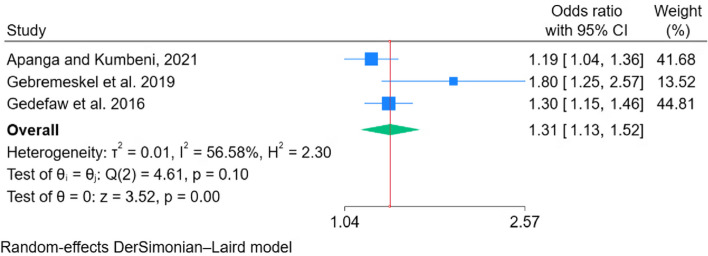
Three studies were included to estimate the association between pregnancy intention and early initiation of breastfeeding [55–57]. Meta-analysis of the three studies showed that women with intended pregnancy had 1.31 times (COR: 1.30, 95% CI: 1.13, 1.52) higher odds of early initiation of breastfeeding than women who had an unintended pregnancy (Fig. 3).
Fig. 3.
Pooled odds ratio of the association between early initiation of breastfeeding and pregnancy intention
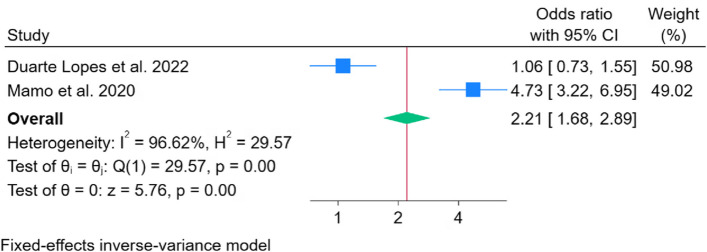
Two studies reported the association between pregnancy intention and exclusive breastfeeding [58, 59]. Meta-analysis of the two studies showed that women with an intended pregnancy had 2.21 times (AOR: 2.21, 95% CI: 1.68, 2.89) higher odds of exclusive breastfeeding than women who had an unintended pregnancy (Fig. 4).
Fig. 4.
Pooled odds ratio of the association between exclusive breastfeeding and pregnancy intention
Three studies reported the association between pregnancy intention and child immunisation status [60–62]. Accordingly, the pooled odds of being fully immunised was 2.73 times (AOR: 2.73, 95% CI: 1.16, 6.40) higher in children born from mothers with an intended pregnancy than children born from mothers with an unintended pregnancy (Fig. 5).
Fig. 5.
Pooled odds ratio of the association between child immunisation status and pregnancy intention
Discussion
Adjusted effect estimates were used to determine the association between pregnancy intention and newborn and infant continuum of care, including essential newborn care, early initiation and exclusive breastfeeding, and full immunisation. However, the studies did not control for the same mix of confounders. Furthermore, the association between pregnancy intention and early initiation of breastfeeding is likely to be affected by several other factors, as the analysis was executed based on an unadjusted effect measure. The results of the present meta-analyses did however suggest that intended pregnancy was associated with greater completion of essential newborn care practices, early initiation and exclusive of breastfeeding, and being fully immunised.
Women with intended pregnancy had higher odds of essential newborn care practice, early initiation and exclusive breastfeeding and fully immunised infants than women with unintended pregnancy. This could be explained by the fact that mothers with intended pregnancy may have greater psychological preparedness for providing care to their newborn infants [63]. Conversely, women experiencing an unintended pregnancy may not feel equipped to take on a maternal role, leading to poor mother-to-child attachment and low engagement with essential newborn practices [13, 64]. Previous studies have indicated that negligence, carelessness, aggression, and maltreatment of children were observed more often in mothers with unintended pregnancies [65, 66]. Furthermore, these women may have low health-seeking behaviour for themselves and their infants due to stress associated with unintended pregnancy, and less support from their partners or families [24, 67, 68]. Women who experience an unintended pregnancy may also receive little information and counselling regarding the benefit of appropriate newborn and infant feeding practices and care because of absent or delayed engagement with the continuum of perinatal health services [27, 69–72].
This review implies that preventing unplanned pregnancy may have an important role in improving essential newborn care, early initiation and exclusive breastfeeding, and completion of immunisation of infants in SSA and possibly other low-resource settings. The prevention of unintended pregnancy could be achieved through improving access to quality family planning services [73, 74]. Strengthening preconception services and information about the consequences of unintended pregnancy on newborn and infant health outcomes could improve newborn and infant health and survival [75]. Furthermore, counselling about maternal-child attachment in women with an unplanned pregnancy could contribute to better newborn and infant health outcomes [71].
Post-conception responses from partners, family and community members, and psychological consequences such as depression and anxiety following an unintended pregnancy possibly influence newborn and infant health care practices among women with unintended pregnancies [68, 76, 77]. Furthermore, women with unintended pregnancies may have several socioeconomic and cultural challenges to visiting health facilities [78, 79]. Previous studies in low- and middle-income countries reported that multiple visits to healthcare facilities, which require travel, money, and assistance from others, substantially deter women from using antenatal care, skilled birth attendance, and postnatal care following the occurrence of an unintended pregnancy [80–82]. Hence, encouraging perinatal service use and preventive and curative care of infants resulting from unintended pregnancies may require policies and practices that support identification of women with unintended pregnancies. Behavioural change approaches regarding unintended pregnancy also need to be considered at individual, family, and community levels [83–85]. This may reduce the humiliation of women from unsolicited post-conception responses from partner, family and community members following unintended pregnancies [86, 87].
This systematic review has the following limitations. In all the included studies, pregnancy intention was examined with other multiple determinants of newborn and infant continuum of care in cross-sectional studies for each outcome; it is thus not possible to establish causal effect relationships with certainty. Although there was significant heterogeneity among the included studies, addressing the sources of heterogeneity was not undertaken due to the limited number of studies included for each outcome. In addition, sensitivity analysis, publication bias and subgroup analyses were not conducted because of the limited number of studies included in each sub-topic. Furthermore, some studies were excluded due inconsistent categorisation of the exposure variable. Moreover, studies published in a language other than English and non-peer-reviewed articles may have been missed as only peer-reviewed articles published in English were included. While grey literature may exist on this topic, we included only peer-reviewed studies to ensure a robust approach and consistency across studies. Finally, the generalizability of this review may be limited because the included studies were not representative of all regions of SSA, with the majority of studies coming from Ethiopia. Nevertheless, this review used adjusted effect measures to quantitatively estimate the association between pregnancy intention on newborn and infant health across the continuum of care in SSA.
Conclusions
This review pinpointed that there were statistically significant positive associations between intended pregnancy and increased completion of essential newborn care practices, early initiation and exclusive breastfeeding and full immunisation of infants in SSA. There is a need for collaboration among stakeholders, policy-makers and health care providers to strengthen the provision of quality family planning services and enhancing preconception care services to prevent unintended pregnancy. Furthermore, strategies that help identify women with unintended pregnancies are needed to increase women’s access to essential maternal and neonatal/infant healthcare services that further reduce the risk of newborn and infant deaths. Moreover, further research with better design is needed to clearly understand the relationship between pregnancy intention and completion of newborn and infant health practices across the continuum of care.
Supplementary Information
Acknowledgements
The authors would like to thank Olivia Larobina (Scholarly Services Librarian at Deakin University) for her assistance in developing the systematic search strategy. We also would like to acknowledge Deakin University for providing PhD scholarship for the principal investigator of this research.
Abbreviations
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- NOS
Newcastle-Ottawa scale
- PROSPERO
International Prospective Register of Systematic Reviews
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SSA
Sub-Saharan African countries
Author’s contributions
All authors developed the conception of the review and study design. BDM conducted the literature review, study screening, data extraction, quality assessment, data analysis, interpretation of results, and drafting of the manuscript. VV, AGB and LS contributed to study screening, quality assessment, data extraction, assist data analysis, and critically reviewed the manuscript. All authors read and approved the final manuscript.
Funding
The first author is supported by Deakin University with a PhD research scholarship.
Availability of data and materials
All relevant data is included either in the manuscript or as supplementary files.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.USAID. Preventing Child and Maternal Deaths: A Framework for Action in a Changing World, 2023–2030: USAID; 2021 [Available from: Available at: https://www.usaid.gov/PreventingChildAndMaternalDeaths/framework. Accesed on April 2023.
- 2.WHO. Newborns: improving survival and well-being. 2020. Key facts Available at: https://www.whoint/news-room/fact-sheets/detail/newborns-reducing-mortality. 2021.
- 3.Akombi BJ, Renzaho AM. Perinatal mortality in sub-Saharan Africa: a meta-analysis of demographic and health surveys. Ann Glob Health. 2019;85(1):106. 10.5334/aogh.2348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World-Bank. World Bank. Mortality Rate, Infant (per 1000 Live Births) | Data. Available online: https://data.worldbank.org/indicator/SP.DYN.IMRT.IN. Accessed April 2023. 2018.
- 5.Quamme SH, Iversen PO. Prevalence of child stunting in Sub-Saharan Africa and its risk factors. Clin Nutr Open Sci. 2022;42:49–61. 10.1016/j.nutos.2022.01.009 [DOI] [Google Scholar]
- 6.Burstein R, Henry NJ, Collison ML, Marczak LB, Sligar A, Watson S, et al. Mapping 123 million neonatal, infant and child deaths between 2000 and 2017. Nature. 2019;574(7778):353–8. 10.1038/s41586-019-1545-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Bernis L, Kinney MV, Stones W, ten Hoope-Bender P, Vivio D, Leisher SH, et al. Stillbirths: ending preventable deaths by 2030. The lancet. 2016;387(10019):703–16. 10.1016/S0140-6736(15)00954-X [DOI] [PubMed] [Google Scholar]
- 8.UNICEF, WHO. Ending preventable newborn and stillbirths by 2030: moving faster towards high-quality universal health coverage in 2020–2025. UNICEF; World Health Organization; 2020.
- 9.Yee AZ, Lwin MO, Ho SS. The influence of parental practices on child promotive and preventive food consumption behaviors: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):1–14. 10.1186/s12966-017-0501-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker S, Morawska A, Mitchell AE. Do Australian children carry out recommended preventive child health behaviours? Insights from an online parent survey. J Paediatr Child Health. 2020;56(6):900–7. 10.1111/jpc.14773 [DOI] [PubMed] [Google Scholar]
- 11.Jensen SK, Bouhouch RR, Walson JL, Daelmans B, Bahl R, Darmstadt GL, et al. Enhancing the child survival agenda to promote, protect, and support early child development. In: Seminars in perinatology. Elsevier; 2015. [DOI] [PubMed] [Google Scholar]
- 12.Singh A, Upadhyay AK, Singh A, Kumar K. The association between unintended births and poor child development in India: evidence from a longitudinal study. Stud Fam Plann. 2017;48(1):55–71. 10.1111/sifp.12017 [DOI] [PubMed] [Google Scholar]
- 13.Pakseresht S, Rasekh P, Leili EK. Physical health and maternal-fetal attachment among women: Planned versus unplanned pregnancy. INternational Journal of Womens Health and Reproduction Sciences. 2018;6(3):335–41. 10.15296/ijwhr.2018.55 [DOI] [Google Scholar]
- 14.Hall JA, Barrett G, Copas A, Phiri T, Malata A, Stephenson J. Reassessing pregnancy intention and its relation to maternal, perinatal and neonatal outcomes in a low-income setting: a cohort study. PLoS ONE. 2018;13(10): e0205487. 10.1371/journal.pone.0205487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawhill IV, Guyot K. Preventing unplanned pregnancy: lessons from the states. Economic studies at brookings. 2019. p. 1–18.
- 16.Chowdhury P, Garg MK, Sk MIK. Does mothers’ pregnancy intention affect their children’s preventive and curative care in India? Evidence from a longitudinal survey. BMJ Open. 2021;11(4): e042615. 10.1136/bmjopen-2020-042615 [DOI] [Google Scholar]
- 17.Foster DG, Biggs MA, Raifman S, Gipson J, Kimport K, Rocca CH. Comparison of health, development, maternal bonding, and poverty among children born after denial of abortion vs after pregnancies subsequent to an abortion. JAMA Pediatr. 2018;172(11):1053–60. 10.1001/jamapediatrics.2018.1785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson EL, Burke AE, Wang A, Pennell PB. Unintended pregnancy, prenatal care, newborn outcomes, and breastfeeding in women with epilepsy. Neurology. 2018;91(11):e1031–9. 10.1212/WNL.0000000000006173 [DOI] [PubMed] [Google Scholar]
- 19.Hall JA, Benton L, Copas A, Stephenson J. Pregnancy intention and pregnancy outcome: systematic review and meta-analysis. Matern Child Health J. 2017;21:670–704. 10.1007/s10995-016-2237-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chatterjee E, Sennott C. Fertility intentions and child health in India: Women’s use of health services, breastfeeding, and official birth documentation following an unwanted birth. PLoS ONE. 2021;16(11): e0259311. 10.1371/journal.pone.0259311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lindberg L, Maddow-Zimet I, Kost K, Lincoln A. Pregnancy intentions and maternal and child health: an analysis of longitudinal data in Oklahoma. Matern Child Health J. 2015;19:1087–96. 10.1007/s10995-014-1609-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh A, Singh A, Thapa S. Adverse consequences of unintended pregnancy for maternal and child health in Nepal. Asia Pac J Public Health. 2015;27(2):NP1481–91. 10.1177/1010539513498769 [DOI] [PubMed] [Google Scholar]
- 23.Sharrow D, Hug L, You D, Alkema L, Black R, Cousens S, et al. Global, regional, and national trends in under-5 mortality between 1990 and 2019 with scenario-based projections until 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet Glob Health. 2022;10(2):e195–206. 10.1016/S2214-109X(21)00515-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography. 2015;52(1):83–111. 10.1007/s13524-014-0359-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abajobir AA, Maravilla JC, Alati R, Najman JM. A systematic review and meta-analysis of the association between unintended pregnancy and perinatal depression. J Affect Disord. 2016;192:56–63. 10.1016/j.jad.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 26.Tolossa T, Turi E, Fetensa G, Fekadu G, Kebede F. Association between pregnancy intention and late initiation of antenatal care among pregnant women in Ethiopia: a systematic review and meta-analysis. Syst Rev. 2020;9:1–10. 10.1186/s13643-020-01449-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ranatunga IDJC, Jayaratne K. Proportion of unplanned pregnancies, their determinants and health outcomes of women delivering at a teaching hospital in Sri Lanka. BMC Pregnancy Childbirth. 2020;20(1):1–15. 10.1186/s12884-020-03259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Owili PO, Muga MA, Chou Y-J, Hsu Y-HE, Huang N, Chien L-Y. Associations in the continuum of care for maternal, newborn and child health: a population-based study of 12 sub-Saharan Africa countries. BMC Public Health. 2016;16(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phway P, Kyaw AT, Mon AS, Mya KS. Continuum of care of mothers and immunization status of their children: A secondary analysis of 2015–2016 Myanmar Demographic and Health Survey. Public Health in Practice. 2022;4: 100335. 10.1016/j.puhip.2022.100335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zelka MA, Yalew AW, Debelew GT. Effects of continuity of maternal health services on immediate newborn care practices, Northwestern Ethiopia: multilevel and propensity score matching (PSM) modeling. Heliyon. 2022;8(12): e12020. 10.1016/j.heliyon.2022.e12020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.UNICEF D. Improving maternal, infant and young child nutrition expands opportunities for every child to reach his or her full potential. United Nations Children’s Fund 2023 [Available from: Available from: https://data.unicef.org/topic/nutrition/child-nutrition/.
- 32.UN. Department of Economic Social Affairs. Transforming our world: the 2030 Agenda for Sustainable Development. United Nations General Assembly. Cited 2023. Available at: https://sdgs.un.org/2030agenda; 2015.
- 33.UNICEF D. Analytics Section. Progress for every child in the SDG era: are we on track to achieve the SDGs for children? UNICEF Division of Data. Research and Policy: New York Cited 2023 Available from: https://www.uniceforg/media/56516/file. 2018.
- 34.Bobo FT, Asante A, Woldie M, Dawson A, Hayen A. Child vaccination in sub-Saharan Africa: Increasing coverage addresses inequalities. Vaccine. 2022;40(1):141–50. 10.1016/j.vaccine.2021.11.005 [DOI] [PubMed] [Google Scholar]
- 35.Pretorius CE, Asare H, Genuneit J, Kruger HS, Ricci C. Impact of breastfeeding on mortality in sub-Saharan Africa: a systematic review, meta-analysis, and cost-evaluation. Eur J Pediatr. 2020;179:1213–25. 10.1007/s00431-020-03721-5 [DOI] [PubMed] [Google Scholar]
- 36.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88: 105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 37.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. p. 1–12.
- 38.Biset G, Woday A, Mihret S, Tsihay M. Full immunization coverage and associated factors among children age 12–23 months in Ethiopia: systematic review and meta-analysis of observational studies. Hum Vaccin Immunother. 2021;17(7):2326–35. 10.1080/21645515.2020.1870392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Awoh AB, Plugge E. Immunisation coverage in rural–urban migrant children in low and middle-income countries (LMICs): a systematic review and meta-analysis. J Epidemiol Community Health. 2016;70(3):305–11. 10.1136/jech-2015-205652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alamneh Y, Adane F, Yirga T, Desta M. Essential newborn care utilization and associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20:1–9. 10.1186/s12884-020-2804-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Organization WH. WHO recommendations on maternal and newborn care for a positive postnatal experience: World Health Organization; 2022. Available at: https://www.who.int/publications/i/item/9789240045989. Accessed Apr 2023. [PubMed]
- 42.Wojcieszek AM, Bonet M, Portela A, Althabe F, Bahl R, Chowdhary N, et al. WHO recommendations on maternal and newborn care for a positive postnatal experience: strengthening the maternal and newborn care continuum. BMJ Glob Health. 2023;8(Suppl 2): e010992. 10.1136/bmjgh-2022-010992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.WHO. WHO recommendations for routine immunization-summary tables. WHO Geneva, Switzerland; 2014. Available at: https://www.who.int/teams/immunization-vaccines-andbiologicals/policies/who-recommendations-forroutine-immunization---summary-tables. Accessed Apr 2023.
- 44.Stanford JB, Hobbs R, Jameson P, DeWitt MJ, Fischer RC. Defining dimensions of pregnancy intendedness. Matern Child Health J. 2000;4:183–9. 10.1023/A:1009575514205 [DOI] [PubMed] [Google Scholar]
- 45.Santelli J, Rochat R, Hatfield-Timajchy K, Gilbert BC, Curtis K, Cabral R, et al. The measurement and meaning of unintended pregnancy. Perspect Sex Reprod Health. 2003;35(2):94–101. 10.1363/3509403 [DOI] [PubMed] [Google Scholar]
- 46.Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. JBI Evidence Implementation. 2015;13(3):196–207. [DOI] [PubMed] [Google Scholar]
- 47.Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of effectiveness. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. JBI; 2020. [cited August 2023]. Available from: https://synthesismanual.jbi.global. 10.46658/JBIMES-20-04.
- 48.Cooper H. Research synthesis and meta-analysis: A step-by-step approach. 5th ed. Thousand Oaks (CA): Sage Publications; 2015. p. 1–364.
- 49.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193. 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- 50.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 51.Chandler J, Cumpston M, Li T, Page MJ, Welch V. Cochrane handbook for systematic reviews of interventions. Hoboken: Wiley; 2019. [Google Scholar]
- 52.Habte A, Lukas K, Tamirat T. The level of Community-Based Essential Newborn Care utilization and associated factors among rural women in Southern Ethiopia, 2020: Based on the updated Community-Based Essential Newborn Care guideline. SAGE open medicine. 2022;10:20503121211067690. 10.1177/20503121211067690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alemu A, Eshete A. Newborn care practices and associated factors among lactating mothers at home in the rural districts of Gedeo Zone, southern Ethiopia. Pediatric Health Med Ther. 2020;11:47–54. 10.2147/PHMT.S232860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chichiabellu TY, Mekonnen B, Astawesegn FH, Demissie BW, Anjulo AA. Essential newborn care practices and associated factors among home delivered mothers in Damot pulasa Woreda, southern Ethiopia. Reprod Health. 2018;15(1):1–11. 10.1186/s12978-018-0609-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Apanga PA, Kumbeni MT. Prevalence and predictors of timely initiation of breastfeeding in Ghana: an analysis of 2017–2018 multiple indicator cluster survey. Int Breastfeed J. 2021;16:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gedefaw G, Goedert MH, Abebe E, Demis A. Effect of cesarean section on initiation of breast feeding: Findings from 2016 Ethiopian Demographic and Health Survey. PLoS ONE. 2020;15(12): e0244229. 10.1371/journal.pone.0244229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gebremeskel SG, Gebru TT, Gebrehiwot BG, Meles HN, Tafere BB, Gebreslassie GW, et al. Early initiation of breastfeeding and associated factors among mothers of aged less than 12 months children in rural eastern zone, Tigray, Ethiopia: cross-sectional study. BMC Res Notes. 2019;12(1):1–6. 10.1186/s13104-019-4718-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Duarte Lopes E, Monteiro AMRL, Varela DOBFC, Trigueiros DELR, Monteiro Spencer Maia I, de Jesus Xavier Soares J, et al. The prevalence of exclusive breastfeeding and its associated factors in Cape Verde. BMC Nutr. 2022;8(1):1–7. 10.1186/s40795-022-00554-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mamo K, Dengia T, Abubeker A, Girmaye E. Assessment of exclusive breastfeeding practice and associated factors among mothers in west Shoa zone, Oromia. Ethiopia Obstet Gynecol Int. 2020;2020:3965873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mebrate M, Workicho A, Alemu S, Gelan E. Vaccination Status and Its Determinants Among Children Aged 12 to 23 Months in Mettu and Sinana Districts, Oromia Region, Ethiopia: A Comparative Cross Sectional Study. Pediatric Health Med Ther. 2022;13:335–48. 10.2147/PHMT.S380303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fenta SM, Fenta HM. Individual and community-level determinants of childhood vaccination in Ethiopia. Archives of Public Health. 2021;79(1):1–11. 10.1186/s13690-021-00581-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gualu T, Dilie A. Vaccination coverage and associated factors among children aged 12–23 months in debre markos town, Amhara regional state, Ethiopia. Adv Pub Health. 2017;2017(1):5352847. [Google Scholar]
- 63.Tsegaw HZ, Cherkos EA, Badi MB, Mihret MS. Intended pregnancy as a predictor of good knowledge on birth preparedness and complication readiness: the case of northern Ethiopia pregnant mothers. Int J Reprod Med. 2019;2019:9653526. 10.1155/2019/9653526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abajobir AA, Kisely S, Najman JM. A systematic review of unintended pregnancy in cross-cultural settings: Does it have adverse consequences for children? Ethiopian Journal of Health Development. 2017;31(3):138–54. [Google Scholar]
- 65.Guterman K. Unintended pregnancy as a predictor of child maltreatment. Child Abuse Negl. 2015;48:160–9. 10.1016/j.chiabu.2015.05.014 [DOI] [PubMed] [Google Scholar]
- 66.Isumi A, Fujiwara T. Synergistic effects of unintended pregnancy and young motherhood on shaking and smothering of infants among caregivers in Nagoya City. Japan Frontiers in public health. 2017;5:245. 10.3389/fpubh.2017.00245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Faisal-Cury A, Menezes PR, Quayle J, Matijasevich A. Unplanned pregnancy and risk of maternal depression: secondary data analysis from a prospective pregnancy cohort. Psychol Health Med. 2017;22(1):65–74. 10.1080/13548506.2016.1153678 [DOI] [PubMed] [Google Scholar]
- 68.Barton K, Redshaw M, Quigley MA, Carson C. Unplanned pregnancy and subsequent psychological distress in partnered women: a cross-sectional study of the role of relationship quality and wider social support. BMC Pregnancy Childbirth. 2017;17:1–9. 10.1186/s12884-017-1223-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ochako R, Gichuhi W. Pregnancy wantedness, frequency and timing of antenatal care visit among women of childbearing age in Kenya. Reprod Health. 2016;13:1–8. 10.1186/s12978-016-0168-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Amo-Adjei J, Anamaale TD. Effects of planned, mistimed and unwanted pregnancies on the use of prenatal health services in sub-Saharan Africa: a multicountry analysis of demographic and health survey data. Tropical Med Int Health. 2016;21(12):1552–61. 10.1111/tmi.12788 [DOI] [PubMed] [Google Scholar]
- 71.Ekrami F, Mohammad-Alizadeh Charandabi S, Babapour Kheiroddin J, Mirghafourvand M. Effect of counseling on maternal-fetal attachment in women with unplanned pregnancy: a randomized controlled trial. J Reprod Infant Psychol. 2020;38(2):151–65. 10.1080/02646838.2019.1636943 [DOI] [PubMed] [Google Scholar]
- 72.Khan MN, Harris ML, Shifti DM, Laar AS, Loxton D. Effects of unintended pregnancy on maternal healthcare services utilization in low-and lower-middle-income countries: systematic review and meta-analysis. Int J Public Health. 2019;64:743–54. 10.1007/s00038-019-01238-9 [DOI] [PubMed] [Google Scholar]
- 73.Norton M, Chandra-Mouli V, Lane C. Interventions for preventing unintended, rapid repeat pregnancy among adolescents: a review of the evidence and lessons from high-quality evaluations. Global Health: Science and Practice. 2017;5(4):547–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rees H, Pillay Y, Mullick S, Chersich M. Strengthening implant provision and acceptance in South Africa with the ‘Any woman, any place, any time’approach: An essential step towards reducing unintended pregnancies. S Afr Med J. 2017;107(11):939–44. 10.7196/SAMJ.2017.v107i11.12903 [DOI] [PubMed] [Google Scholar]
- 75.Goodfellow A, Frank J, McAteer J, Rankin J. Improving preconception health and care: a situation analysis. BMC Health Serv Res. 2017;17:1–8. 10.1186/s12913-017-2544-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McNamara J, Risi A, Bird AL, Townsend ML, Herbert JS. The role of pregnancy acceptability in maternal mental health and bonding during pregnancy. BMC Pregnancy Childbirth. 2022;22(1):1–10. 10.1186/s12884-022-04558-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yong MQY, Yeo Y, Shorey S. Factors affecting unintended pregnancy resolution from the perspectives of pregnant women and people: A systematic review of qualitative evidence. Midwifery. 2023;127: 103866. 10.1016/j.midw.2023.103866 [DOI] [PubMed] [Google Scholar]
- 78.Hajizadeh M, Nghiem S. Does unwanted pregnancy lead to adverse health and healthcare utilization for mother and child? Evidence from low-and middle-income countries. Int J Public Health. 2020;65:457–68. 10.1007/s00038-020-01358-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Klann EM, Wong YJ. A pregnancy decision-making model: psychological, relational, and cultural factors affecting unintended pregnancy. Psychol Women Q. 2020;44(2):170–86. 10.1177/0361684320904321 [DOI] [Google Scholar]
- 80.Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-Saharan Africa and Latin America. Health Policy Plan. 2014;29(5):589–602. 10.1093/heapol/czt045 [DOI] [PubMed] [Google Scholar]
- 81.Khan MN, Harris ML, Loxton D. Assessing the effect of pregnancy intention at conception on the continuum of care in maternal healthcare services use in Bangladesh: Evidence from a nationally representative cross-sectional survey. PLoS ONE. 2020;15(11): e0242729. 10.1371/journal.pone.0242729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rahman MM, Rahman MM, Tareque MI, Ferdos J, Jesmin SS. Maternal pregnancy intention and professional antenatal care utilization in Bangladesh: a nationwide population-based survey. PLoS ONE. 2016;11(6): e0157760. 10.1371/journal.pone.0157760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Uthaphan P, Mueaithaisong A, Phanphoon A, Karsapone S, Sopajorn S, Neadpuckdee R, et al. Using an Integrated Training Course with Family, Community, and Buddhism in Solving Unintended Pregnancies among Vulnerable Thai Youth. High Educ Stud. 2022;12(4):137–42. 10.5539/hes.v12n4p137 [DOI] [Google Scholar]
- 84.Moseson H, Mahanaimy M, Dehlendorf C, Gerdts C. “… Society is, at the end of the day, still going to stigmatize you no matter which way”: A qualitative study of the impact of stigma on social support during unintended pregnancy in early adulthood. PLoS ONE. 2019;14(5): e0217308. 10.1371/journal.pone.0217308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Feld H, Barnhart S, Wiggins AT, Ashford K. Social support reduces the risk of unintended pregnancy in a low-income population. Public Health Nurs. 2021;38(5):801–9. 10.1111/phn.12920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Crowley JL, High AC, Thomas LJ. Desired, expected, and received support: How support gaps impact affect improvement and perceived stigma in the context of unintended pregnancy. Health Commun. 2019;34(12):1441–53. 10.1080/10410236.2018.1495162 [DOI] [PubMed] [Google Scholar]
- 87.Smith W, Turan JM, White K, Stringer KL, Helova A, Simpson T, et al. Social norms and stigma regarding unintended pregnancy and pregnancy decisions: a qualitative study of young women in Alabama. Perspect Sex Reprod Health. 2016;48(2):73–81. 10.1363/48e9016 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data is included either in the manuscript or as supplementary files.
No datasets were generated or analysed during the current study.