Abstract
The WATCHMAN™ atrial appendage closure device is designed to reduce the risk of stroke in patients with nonvalvular atrial fibrillation who are not suitable candidates for long-term oral anticoagulation therapy. However, the device also carries small risks, including procedural complications such as device migration, embolization, or pericardial effusion. We describe a case of WATCHMAN device migration requiring surgical retrieval.
Keywords: left atrial appendage closure, WATCHMAN device, atrial fibrillation, modified maze procedure, sternotomy
Introduction
The WATCHMAN™ FLX 35 mm atrial appendage closure device (Boston Scientific) is designed to reduce the risk of stroke in patients with nonvalvular atrial fibrillation who are not suitable candidates for long-term oral anticoagulation therapy. The WATCHMAN device is deployed into the left atrial appendage (LAA) under fluoroscopic guidance via a percutaneous technique. Transesophageal echocardiography (TEE) is performed to assess the morphology and size of the LAA and to identify any potential anatomical challenges for device implantation. Over time, heart tissue grows into the device and seals off the LAA, preventing the site from thrombus formation. This allows most patients to discontinue anticoagulation.
While the device offers the advantage of stroke prevention without the need for daily anticoagulation, it also carries risks, including complications such as device migration, embolization, or pericardial effusion. This case describes such a complication and discusses the literature and methods for device extraction.
Case Presentation
A 72-year-old female with past medical history of atrial fibrillation, pacemaker placement, hypertension, CHA2DS2-VASc score of 6, HAS-BLED score of 4, and two prior embolic occipital strokes despite therapeutic anticoagulation underwent placement of a WATCHMAN FLX 35 mm at an outside institution (Figure 1). The tug test was completed, no residual gap was noted, and measurement of the deployed device ranged from 26 to 29 mm with a compression ratio of 17% to 26%.
Figure 1.
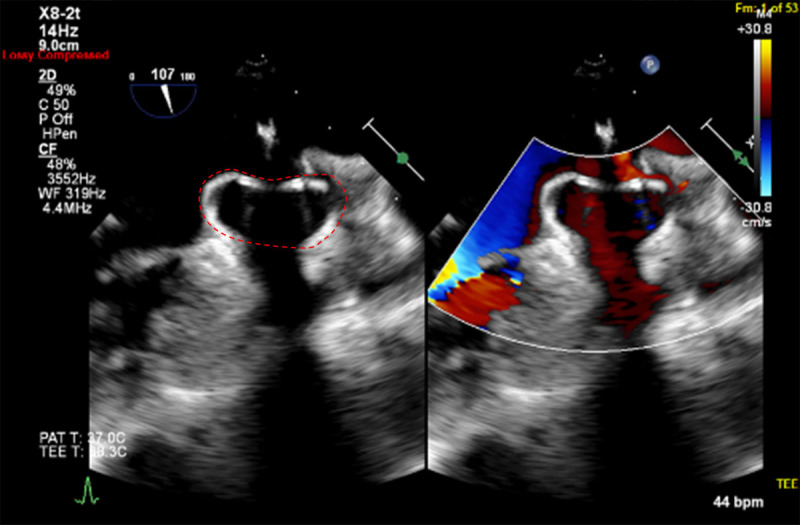
Transesophageal echocardiography post-WATCHMAN device implantation. Echocardiogram showing WATCHMAN device (red dotted line) in place after implantation.
On her 6-week post-WATCHMAN placement TEE, the device was noted to have migrated proximally. There was no apparent communication between the left atrium and LAA by color Doppler; however, it appeared to be anchored by only one superior anchor while encroaching into the left atrium and mitral apparatus (Figure 2, Video 1). An adjacent echodensity was concerning for a thrombus within the LAA. She was then referred for consultation at our surgery clinic for device extraction.
Figure 2.
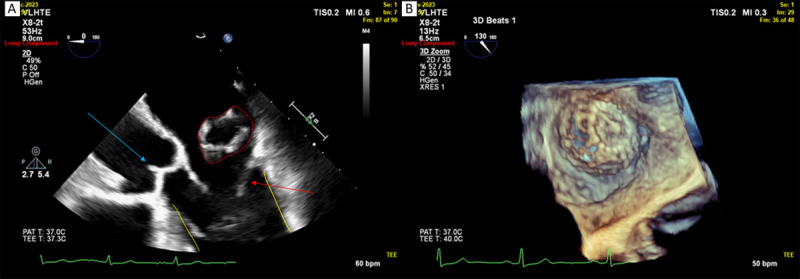
Transesophageal echocardiography (TEE) at 2-week follow-up post-WATCHMAN device implantation. (A) Echocardiogram showing the WATCHMAN device (red dotted line) encroaching onto the mitral apparatus (red arrow pointing to posterior mitral leaflet). Blue arrow points to semilunar valves of the aorta, and yellow lines outline the walls of the left ventricle. (B) TEE 3-dimensional reconstruction of the WATCHMAN device inside the left atrium.
Video 1.
Transesophageal echocardiography of WATCHMAN device appearing anchored by only one superior anchor while encroaching into the left atrium and mitral apparatus; see also at https://youtu.be/o-UXOjeJrzg.
Management
A multidisciplinary discussion involving cardiovascular surgery and interventional cardiology reviewed options for removal of the device. As the WATCHMAN was still partially lodged between the mitral apparatus and the LAA, it was deemed unsafe to attempt percutaneous retrieval. Given her history of atrial fibrillation and stroke, the decision was made to perform a maze procedure.
The patient was transferred to the operating room for open surgical removal of the WATCHMAN device. Her chest was opened through a median longitudinal sternotomy, and she was placed on cardiopulmonary bypass. Bilateral pulmonary vein isolation was performed using the AtriCure modified maze atrial fibrillation ablation system (AtriCure). The aorta was cross clamped and, after a warm induction of antegrade blood cardioplegia, the heart was arrested using antegrade cold blood cardioplegia.
The left atrium was incised, and the WATCHMAN device was identified emanating from the orifice of the left atrial appendage (Figure 3). It was mildly adherent to the left atrial appendage but was dissected free and removed intact (Figure 4). The orifice of the left atrial appendage was oversewn from the inside of the left atrium using two layers of 4–0 Prolene suture. The left atrial appendage was then stapled and excised from the outside using linear staples with pericardial strips. The left atrium was approximated using running 4–0 Prolene suture.
Figure 3.
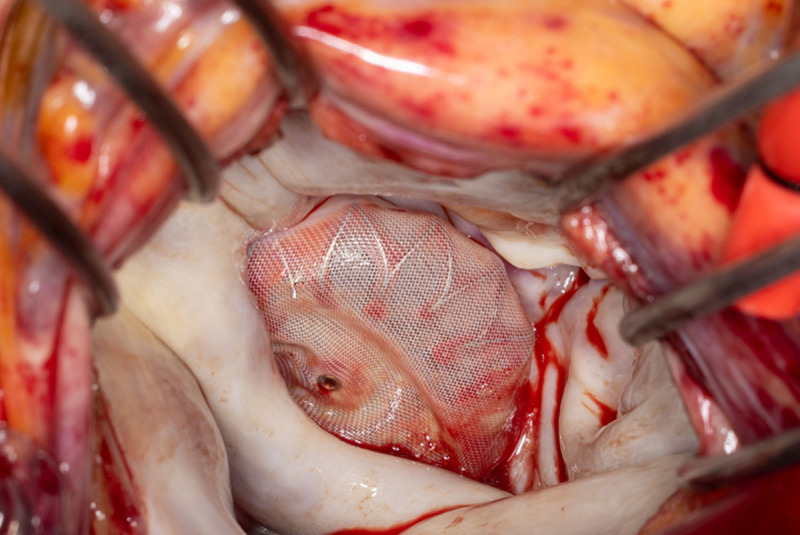
Intraoperative photograph of left atrium. WATCHMAN device visualized intraoperatively inside the open left atrium.
Figure 4.

WATCHMAN device after extraction, bottom view (left) and top view (right).
The patient was rewarmed and weaned from cardiopulmonary bypass. Cardiopulmonary bypass time was 55 minutes, and cross-clamp time was 32 minutes.
The patient was extubated in the operating room and transferred to the intensive care unit on vasopressin overnight. Her hospital course was uncomplicated, and she was discharged home on postoperative day 5. She was in normal sinus rhythm, and no anticoagulation was initiated. At her 2-week follow-up, she was doing well without further incidence of arrhythmia on electrocardiogram. At the 2-month follow-up with her cardiologist, her electrocardiogram remained normal and continued to monitor her hypertension, prediabetes, and dyslipidemia.
Discussion
The WATCHMAN device is an attractive option for patients who want to avoid blood thinners and are worried about stroke. While it has low complications, device migration can occur post-insertion, though it is rarely discussed. The current literature reveals only six case reports describing WATCHMAN device migration/embolization during implantation1,2,3,4,5,6 and another 15 postoperatively with their subsequent removal (7 were surgical and 8 were percutaneous removal).7,8,9,10,11,12,13,14,15,16,17,18,19,20,21 There is a steady increase of WATCHMAN device utilization, jumping from 1,195 in 2015 to 11,165 devices in 2017.22 WATCHMAN manufacturer Boston Scientific reports over 90,000 implants globally as of 2019. As per US Food and Drug Administration labeling, four clinical trials reported the incidence of device embolization ranging from 0% to 0.6%, while device migration was reported as 0.2% in only one study and 0% in the other three studies.23
A National Cardiovascular Data Registry (NCDR) showed that device migration or embolization was more common in lower annual median volume centers, with the use of WATCHMAN 2.5 device versus WATCHMAN FLX, in patients with larger LAA ostia (median 23 vs 21 mm, P = .04), and in cases with a smaller difference between LAA ostia and WATCHMAN size (median 4 mm vs 5 mm, P = .04).24 Additionally, an NCDR left atrial appendage occlusion registry study reports that, compared to manufacturer recommended sizing, the odds of device migration or embolization at 45 days were similar if undersized devices were used and favorable if oversized devices were used. They also reported that the selection of oversized devices increased significantly over the study period.
Proper sizing of the device based on the atrial appendage is therefore very important in preventing device migration, and experience with the device improves the choice in sizing. Abnormalities in atrial appendage structure, such as the chicken wing shape, may also present risks. This was demonstrated in a previous case report in which a WATCHMAN device migrated into the left ventricular outflow tract in a patient with this anatomical feature.11
When a WATCHMAN device does migrate, it poses the challenge of determining whether a surgical or percutaneous approach should be used for retrieval since there is limited comparative data between the two methods. Advantages of open-heart surgical extraction include reducing the risk of thromboembolism during the procedure and providing a robust treatment of atrial fibrillation through modified maze and LAA excision, although complications with open-heart surgery can be high and patient recovery is longer.
It is worth noting that percutaneous removal entails simultaneous placement of a new device, which may pose challenges as abnormal atrial appendage anatomy may be the primary cause of device migration in this population, and therefore the risk of migration may persist. Open removal allows direct visualization of the device and removing it intact, while percutaneous removal typically involves using a Raptor or Snare device to pull it through a French sheath.7,12,13,18 Theoretically, this may cause parts of the WATCHMAN’s metal frame to break off and embolize since the device needs to be crushed for extraction.13
One case report mentions that the unfolded anchoring barbs remained hooked into the LAA orifice during removal.9 Aortic injury during percutaneous removal has been previously reported, leading to dissection in one case and pseudoaneurysm in another.8,17 Percutaneous endovascular extraction, however, does come with advantages such as the avoidance of sternotomy, having a shorter hospital stay, and avoiding complications related to cardiopulmonary bypass. Moreover, it may offer the only solution for poor surgical candidates.
Conclusion
WATCHMAN device migration is a rare but major complication that may be asymptomatic and only discovered on follow-up echocardiographic imaging. The decision to remove via open surgery or percutaneous extraction should be made with input from both interventional cardiology and cardiovascular surgery and should include a discussion of thromboembolization and aortic injury risks versus the benefits of avoiding sternotomy and cardiopulmonary bypass.
Shared decision-making between the patient and the healthcare team is essential to ensure that the patient is appropriately informed of the possible risks of each procedure and their preferences are considered.
Competing Interests
The authors have no competing interests to declare.
References
- 1.Al Rameni D, de Armas IS, Al Rameeni A, Gupta S, Gregoric ID. Case Report: WATCHMAN Procedure Complicated By Atrial Perforation and Device Dislodgement. Cardiovasc Revasc Med. 2023. Aug;53S:S188–S190. doi: [DOI] [PubMed] [Google Scholar]
- 2.Fastner C, Lehmann R, Behnes M, Sartorius B, Borggrefe M, Akin I. Veno-venous double lasso pull-and-push technique for transseptal retrieval of an embolized Watchman occluder. Cardiovasc Revasc Med. 2016. Apr-May;17(3):206–8. doi: [DOI] [PubMed] [Google Scholar]
- 3.Li HY, Wu XL, Xiao FY, Zhou XD, Chen Y, Huang WJ. Successful Percutaneous Retrieval of a 33-mm Watchman Left Atrial Appendage Occlusion Device From the Left Atrium. JACC Cardiovasc Interv. 2018. Apr 23;11(8):e65–e67. doi: [DOI] [PubMed] [Google Scholar]
- 4.Lubis AC, Iqbal M, Munawar DA, Hartono B, Munawar M. A Simple Percutaneous Retrieval Technique for an Embolized Watchman Left Atrial Appendage Closure Device in the Thoracic Aorta Using a Homemade Snare. Int Heart J. 2021. Sep 30;62(5):1153–1155. doi: [DOI] [PubMed] [Google Scholar]
- 5.Roberts A, Mach S, Goebel J, Palomino H, Horstemeyer D. Watchman Device Dislodgement Creating a Left Ventricular Outflow Tract Obstruction Requiring Emergency Cardiopulmonary Bypass. Case Rep Anesthesiol. 2022. Feb 23;2022(1):3215334. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stöllberger C, Schneider B, Finsterer J. Serious complications from dislocation of a Watchman left atrial appendage occluder. J Cardiovasc Electrophysiol. 2007. Aug;18(8):880–1. doi: [DOI] [PubMed] [Google Scholar]
- 7.Deng H, Liao H, Liu Y, et al. Acute Heart Failure Caused by Dislocation of a WATCHMAN Left Atrial Appendage Occluder. JACC Cardiovasc Interv. 2016. May 23;9(10):e97–9. doi: [DOI] [PubMed] [Google Scholar]
- 8.Manosalbas Rubio IM, Martín Cañuelo JJ, Galera Martinez MC, García Turrillo E, Rodríguez Piñero M. Aortic Extraction of a Migrated Watchman® Device. Cir Esp (Engl Ed). 2021. Mar;99(3):243–245. doi: [DOI] [PubMed] [Google Scholar]
- 9.Takayuki G, Grimmig O, Sören J, Dirk F. Asymptomatic dislocation of a Watchman left atrial appendage occluder. Asian Cardiovasc Thorac Ann. 2019. Jun;27(5):394–395. doi: [DOI] [PubMed] [Google Scholar]
- 10.Moradi N, Tosonian S, Askari A, Sontz EM. Delayed dislodgment of a watchman device: A rare complication manifesting as a transient ischemic event. J Cardiovasc Electrophysiol. 2020. Jul;31(7):1848–1850. doi: [DOI] [PubMed] [Google Scholar]
- 11.Bhagat A, Gier C, Kim P, Diggs P, Gursoy E. Delayed embolization of next-generation left atrial appendage closure device in an asymptomatic patient. HeartRhythm Case Rep. 2023. May 31;9(9):598–601. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han Y, Wang F, Xiaokereti J, et al. Dislodged Watchman Device Retrieved Using Double Transseptal Sheaths Technique and Reinstalled with LAmbre Device. Anatol J Cardiol. 2022. May;26(5):407–410. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabriels J, Beldner S, Khan M, Zeitlin J, Jadonath R, Patel A. Embolization of Watchman Device Following a Hybrid Radiofrequency Ablation of Atrial Fibrillation and Watchman Implantation Procedure. J Cardiovasc Electrophysiol. 2017. Jul;28(7):835–6. doi: [DOI] [PubMed] [Google Scholar]
- 14.El-Gabry M, Shehada SE, Wendt D, Mourad F. Emergent surgical removal of a migrated left atrial appendage occluder. Eur J Cardiothorac Surg. 2018. Jul 1;54(1):191–192. doi: [DOI] [PubMed] [Google Scholar]
- 15.Mansour MJ, Bénic C, Didier R, Noel A, Gilard M, Mansourati J. Late discovery of left atrial appendage occluder device embolization: a case report. BMC Cardiovasc Disord. 2020. Jun 22;20(1):305. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sasko B, Ritter O, Bramlage P, Riediger F. Late left atrial appendage closure device displacement and massive thrombus formation: a case report. Eur Heart J Case Rep. 2020. Feb 20;4(2):1–5. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Afzal MR, Ellis CR, Gabriels J, et al. Percutaneous approaches for retrieval of an embolized or malpositioned left atrial appendage closure device: A multicenter experience. Heart Rhythm. 2020. Sep;17(9):1545–1553. doi: [DOI] [PubMed] [Google Scholar]
- 18.Maan A, Turagam MK, Dukkipati SR, Reddy VY. Percutaneous Extraction of a Migrated WATCHMAN™ Device After Seven Months. J Innov Card Rhythm Manag. 2021. Jul 15;12(7):4572–4574. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turagam MK, Neuzil P, Dukkipati SR, et al. Percutaneous Retrieval of Left Atrial Appendage Closure Devices With an Endoscopic Grasping Tool. JACC Clin Electrophysiol. 2020. Apr;6(4):404–413. doi: [DOI] [PubMed] [Google Scholar]
- 20.Fanari Z, Goel S, Goldstein JA. Successful percutaneous retrieval of embolized transcatheter left atrial appendage closure device (Watchman) using a modified vascular retrieval forceps. Cardiovasc Revasc Med. 2017. Dec;18(8):616–618. doi: [DOI] [PubMed] [Google Scholar]
- 21.Blanchard T, Hacker K, Grill J, Betcher J. Who watches the WATCHMAN? A rare case of lower extremity paralysis. J Am Coll Emerg Physicians Open. 2023. Oct 7;4(5):e13052. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Munir MB, Khan MZ, Darden D, et al. Contemporary procedural trends of Watchman percutaneous left atrial appendage occlusion in the United States. J Cardiovasc Electrophysiol. 2021. Jan;32(1):83–92. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.FDA.gov [Internet]. Silver Spring, MD: US Food and Drug Administration; c2024. Premarket Approval (PMA); 2018. Sep 27 [cited 2024 Aug 13]. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf13/P130013S035C.pdf. [Google Scholar]
- 24.Lin A. Early and late Watchman device migration and embolization: Insights from the NCDR LAAO registry. J Cardiovasc Electrophysiol. 2023. Jun;34(6):1499–1501. doi: [DOI] [PubMed] [Google Scholar]


