Abstract
Introduction
Older adults were critically vulnerable to disruptions in health care during the COVID-19 pandemic, but it is not known if changes in ED utilization varied based on patient characteristics. Using a cohort of older Veterans, we examined changes in ED visit rates based on four characteristics of interest: age, race, area deprivation index, and frailty.
Methods
Participants were aged ≥65, with ≥2 visits in primary or geriatric clinics between 02/02/2018–05/07/2019. An adjusted negative binomial regression model was constructed for each characteristic. We report mean counts of all ED visits by quarter for subgroups separately, and report rate ratios to compare ED visits in the first year of the COVID-19 pandemic to the year before.
Results
Patients with complete case data numbered 38,871. During the first two quarters, all subgroups had decreased ED visits, with more variation in the third and fourth quarters. The very highly frail, who had the highest mean estimated count of ED visits per person through both pre-COVID and COVID periods, also had a significant decrease in their ED visits during multiple quarters of the pandemic to a greater degree than other frailty subgroups.
Conclusion
Stratifying older adults by frailty identified patient subgroups with the greatest variation in ED visits during COVID. Very highly frail patients warrant special attention to understand how variation in ED utilization affects patient outcomes.
Keywords: acute care utilization, emergency medicine, Veteran Health Affairs, frailty, COVID-19
INTRODUCTION
In the Veteran Affairs Health Care System (VAHCS), almost half of Emergency Department (ED) visits are by people over 65 years of age.1 The VA has made a significant commitment to providing high-quality geriatric emergency care, with the goal of having all 111 VA EDs undergo Geriatric ED Accreditation.2 Achieving this goal will make the VA the single largest system of accredited EDs in the U.S. In a 2022 VA workgroup conference to advance the future of emergency care research in the VA, the top research priority identified for geriatric emergency care was to “examine the variation in care (referring to both care processes as well as other sources of variation) for older ED veterans and how variation affects outcomes.3”
One of the most notable sources of variation in ED care and utilization for older adults has been the COVID-19 pandemic. Older adults not only bore a disproportionately high burden of morbidity and mortality directly related to COVID, but they also suffered a high burden of poor health outcomes related to disruptions in their usual care. The reasons for delays in usual non-emergent care were multifactorial including various provider, health system, and patient-based factors.4–7
Prior literature looking at variation in ED use during the first year of the pandemic has demonstrated significant decreases in ED visits. This work has largely focused on changes in the types of ED visits (e.g. high acuity versus ambulatory care sensitive conditions,) and changes in specific clinical presentations (e.g. strokes or heart attacks.)8–11 However, less is known about the associations between decreased ED visits and individual patient-level characteristics among older adults. In two studies of all-age ED populations during the first four months of the pandemic, Yu et al. identified Medicaid use but not race as associated with decreased ED visits, while Lowe et al. identified Medicaid use, Hispanic ethnicity, and lower income as associated with decreased ED visits.12,13 In contrast, in a study of Medicare patients through the first 7 months of the pandemic by Smulowitz et al., patient-level characteristics did not explain changes in ED visits.14
A critical first step in understanding the impact of variation in ED utilization on outcomes during the pandemic is identifying which older adult patient populations were most vulnerable to disruptions in care. We aim to fill this knowledge gap by capitalizing on a previous study of 43,935 older Veterans receiving care in geriatrics or primary care clinics recruited from 57 VA medical centers. We examine subgroups based separately on age, race, frailty, and neighborhood deprivation because we expect these to help identify factors associated with differential risk. Additionally, whereas some of these characteristics are widely available to clinicians and health systems (age, race,) other factors are not routinely available to VAHCS clinicians such as neighborhood level effects (area deprivation index) and clinical measures (frailty). These results will help address the geriatric emergency care research priorities of the VA, including understanding variation within the VA ED system, and will inform future efforts to examine related outcomes.
METHODS
Study Design
This retrospective observational study was approved by the Durham Veterans Affairs Institutional Review Board.
Study Population
The study cohort met initial eligibility criteria for a prospective matched cohort study (IIR 15–379) comparing quality of life and quality of care outcomes for specialized geriatrics primary care (GeriPACT) clinics versus traditional primary care (PACT) at 57 VA medical centers.15 Briefly, GeriPACTs differ from traditional primary care in that they aim to provide comprehensive and coordinated primary care for high-risk older veterans, such as those with cognitive impairment or multiple chronic conditions.16 In previous work, we demonstrated that matching procedures generated excellent covariate balance between the patients included in the two groups, thus for the current analysis we considered the sample as a single cohort.15 Participants were identified through rolling quarterly electronic health record (EHR) data pulls conducted between 02/02/2018 and 05/07/2019. To be included, individuals had to be aged ≥65 and have had ≥2 visits in a PACT over the course of one year followed by 2 or more visits in a PACT or GeriPACT clinic in the subsequent year.
Outcome
The outcome was count of days with at least one ED visit per patient per quarter. Using March 1, 2020 as the date of pandemic onset, we examine ED visits in 8 quarterly intervals, comparing the 4 quarters before (Q1: March 2019–May 2019; Q2: June 2019–August 2019; Q3: September 2019–November 2019; Q4: December 2019–February 2020) to the seasonally equivalent 4 quarters during the COVID pandemic (Q5: March 2020–May 2020; Q6: June 2020–August 2020; Q7: September 2020–November 2020; Q8: December 2020–February 2021).
Identifying ED Visits
Days with an ED visit were extracted from three administrative data sources in the VA’s Corporate Data Warehouse (CDW).17 VA facility ED visits were identified from the CDW Outpatient domain file. VA-paid, community delivered ED visits were identified from the Program Integrity Tool (PIT) and Fee Basis domains. If multiple claims were found for the same date, these were counted as single day with an ED visit. ED observation stays were not used for counts of days with an ED visit unless otherwise captured by methods to identify ED visits.
Patient/Baseline Variables
Patient-level data was collected from CDW; January 1, 2019 was used as the index date to define covariates. We assessed demographic variables which would be expected to affect ED use, including age, race, ethnicity, sex, geocoded location (urban vs rural/highly rural), and the patient’s regional Veterans Integrated Services Network (VISN). To assess social support and other factors that impact access to care, we included marital status, VA priority level, service connection, and distance from patient’s residence to nearest VA primary care clinic.
We assessed neighborhood disadvantage using the Neighborhood Atlas area deprivation index (ADI), a composite measurement tool used to quantify a veteran’s socioeconomic risk in single percentiles based on residential location.18 Similar to prior methods, we elected to analyze ADI by quartile rankings.19,20
To assess other health factors expected to influence ED use, we included data for presence (yes/no) and number of VA inpatient stays in the prior year, and the JEN Frailty Index (JFI). JFI is a claims-based measure of frailty, looking at 13 categories of conditions: minor ambulatory limitations, severe ambulatory limitations, chronic mental illness, chronic developmental disability, dementia, sensory disorders, self-care impairment, syncope, cancer, chronic medical disease, pneumonia, renal disorders, and other systemic disorders. It is available from the VA’s Geriatrics and Extended Care Data Analysis Center. JFI predicts institutional care and other home-based care and services, and ranges from 0 to 13, with higher scores reflecting higher risk of utilization.21 While the JFI algorithm is proprietary, limiting its widespread use, it is derived from readily available data from clinical encounters and claims (e.g. diagnosis code). It has been demonstrated to perform similarly to other claims-based measures of frailty.22
Analytic Methods
To examine the impact of the pandemic on ED visits, we constructed separate negative binomial regression models to assess changes across each of our four subgroups of interest. These were 1) Age: 65–74, 75–84, 85+; 2) Race: Black, White, Other (includes Asian, American Indian or Alaskan Native, Native Hawaiian or Pacific Islander, or had more than one race identified); 3) ADI percentile: quartiles of 0–25 (least disadvantage), 26–50, 51–75, 76–100 (most disadvantage); and 4) JFI: low frailty 0–3, moderate frailty 4–5, high frailty 6–7, very high frailty ≥8. These models were fit with generalized estimating equations (GEEs) with clustering by individual with an autoregressive structure, coupled with empirical sandwich standard errors to account for repeated observations per person over time. Patients were censored at the time of death via an offset in the quarter of their death, and then excluded from the analysis in subsequent quarters. Variables demonstrating high multicollinearity were removed. All models included continuous quarter, a post-COVID indicator, quarters since COVID (linear and squared), subgroup indicators and their interactions with the previous terms; adjusted models additionally included patient demographic, clinical, and geographic characteristics (see Supplemental Materials). Outcomes were reported as estimated mean counts of ED visits and 95% confidence intervals by quarter for each subgroup of interest. For reporting of results, quarters were standardized to 91 days for comparison. Additionally, mean estimate rate ratios with corresponding 95% confidence intervals were reported to compare the estimated mean rate of ED visits per person in each of the COVID-era quarters with their seasonally equivalent pre-COVID quarter, by each subgroup of interest. Rate ratios < 1.0 indicate fewer counts of ED visits in the COVID quarter compared to the corresponding pre-COVID quarter. Confidence intervals not including 1.0 and p-values < 0.05 indicate statistical significance.
Differential changes during the COVID pandemic time period were assessed via joint test of the difference in interaction terms between subgroup and a COVID quarter with the corresponding interactions with the seasonally equivalent pre-COVID quarter. If the joint test was significant, pairwise comparison tests identified specific levels within subgroups with differential change. Analyses were performed in SAS Enterprise Guide version 8.3 (SAS Institute, Cary, NC).
RESULTS
Patient Population
To summarize procedures for potentially eligible patient population identification in the parent study, we identified a total of 4,925 potentially eligible patients with qualifying GeriPACT visits from 6 rolling quarterly EHR data pulls. Of these, 647 were excluded because they lacked 5 or more suitable PACT patient matches. For the remaining 4,278 GeriPACT patients, we identified 58,144 PACT matches (limiting to the best 25 for those with >25 matches). After additional EHR data cleaning to identify patients ineligible due to death, duplications from previous quarterly data pulls, insufficient contact information, and then subsequent lack of sufficient matching individuals in the other group, a final cohort of 43,935 patients (3,229 GeriPACT and 40,706 PACT) was deemed eligible for consent in the parent study. For this secondary analysis, we grouped these patients as a single cohort, and additionally excluded patients who no longer had data available after VHA CDW data cleaning in March 2022 (n=6), those who were no longer documented as a Veteran (n=5), those who were deceased prior to study period start date of 1/1/2019 (n=1,702), and 3 who had geocoded location = “I” (insular Islands). Of the remaining 42,219 patients, we removed 3,348 who had missing data on variables included in the adjusted models, yielding an analyzed cohort of 38,871. For included patients, mean age in years was 80.3 (SD=7.3), 38,529 (99.1%) were male, 31,353 (80.7%) were White, and 24,205 (62.3%) were married (Table 1). Patients were distributed across the 23 regional VISNs, with the greatest number of patients (24.1%) in VISN 8 (Florida, South Georgia, and Puerto Rico).
Table 1.
Baseline Demographic and Clinical Characteristics (n=38,871)
| Age, mean (SD) | 80.3 (7.3) |
| Age, n (%) | |
| 65–75 | 10,366 (26.7) |
| 75–84 | 16,168 (41.6) |
| 85 or higher | 12,337 (31.7) |
| Male, n (%) | 38,529 (99.1%) |
| Race, n (%) | |
| Black race | 7,107 (18.3) |
| White race | 31,353 (80.7) |
| Other1 | 411 (1.1) |
| Ethnicity, n (%) | |
| Hispanic | 1,856 (4.8) |
| Non-Hispanic | 37,015 (95.2) |
| Marital status, n (%) | |
| Married | 24,205 (62.3) |
| Widowed/divorced/never married/separated | 14,666 (37.7) |
| Geocoded location, n (%) | |
| Rural/highly rural | 10,629 (27.3) |
| Urban | 28,242 (72.7) |
| Area deprivation index rank, n (%) | |
| 0–25% (least disadvantaged neighborhoods) | 6,727 (17.3) |
| 26–50% | 12,226 (31.5) |
| 51–75% | 11,243 (28.9) |
| 76–100% (most disadvantaged neighborhoods) | 8,675 (22.3) |
| Any inpatient stay in prior year, n (%) | 5,815 (15.0) |
| Number of inpatient stays prior year, mean (SD) | 0.3 (0.8) |
| Priority level, n (%) | |
| High disability (groups 1 and 4) | 12,216 (31.4) |
| Low/moderate disability (groups 2, 3, and 6) | 7,194 (18.5) |
| Low income (group 5) | 9,778 (25.2) |
| No disability (group 7 and 8) | 9,683 (24.9) |
| Service connection2, n (%) | |
| Not service connected | 20,609 (53.2) |
| Service connected 0–49% | 6,981 (18.0) |
| Service connected 50–99% | 6,858 (17.7) |
| Service connected 100% | 4,309 (11.1) |
| Aid and Attendance benefit2, n (%) | 1,022 (2.6) |
| Distance from nearest VA primary care clinic, mean (SD) | 14.8 (14.4) |
| Care Assessment Need (CAN) score, admission risk at 1 year ≥ 752,3, n (%) | 17,177 (44.2) |
| Multiple chronic conditions (2 or more, of 19 below), n (%) | 34,357 (88.4) |
| Anemia, n (%) | 9,204 (23.7) |
| Asthma, n (%) | 1,524 (3.9) |
| Prostatic hyperplasia, n (%) | 12,910 (33.2) |
| Cerebral vascular accident, n (%) | 4,155 (10.7) |
| Chronic renal failure, n (%) | 8,526 (21.9) |
| Chronic obstructive pulmonary disease, n (%) | 8,057 (20.7) |
| Congestive heart failure, n (%) | 5,010 (12.9) |
| Dementia or cognitive impairment, n (%) | 4,864 (12.5) |
| Depression, n (%) | 6,336 (16.3) |
| Diabetes, n (%) | 16,385 (42.2) |
| Gastro-esophageal reflux disease, n (%) | 11,641 (29.9) |
| Hypertension, n (%) | 32,405 (83.4) |
| Ischemic heart disease, n (%) | 13,416 (34.5) |
| Obesity, n (%) | 6,465 (16.6) |
| Osteoporosis, n (%) | 1,394 (3.6) |
| Peripheral vascular disease, n (%) | 4,174 (10.7) |
| Post-traumatic stress disorder, n (%) | 4,661 (12.0) |
| Spinal cord injury, n (%) | 68 (0.2) |
| Traumatic brain injury, n (%) | 489 (1.3) |
| Jen Frailty Index (JFI) score, n (%) | |
| Low frailty (score 0–3) | 18,648 (48.0) |
| Moderate frailty (4–5) | 12,271 (31.6) |
| High frailty (6–7) | 5,970 (15.4) |
| Very high frailty (≥8) | 1,982 (5.1) |
Includes Asian, American Indian or Alaskan Native, Native Hawaiian or Pacific Islander, or had more than one race identified.
Missing data: service connection (114), Aid and Attendance benefit (3), CAN score (31).
CAN scores predict hospitalization and mortality, and range from 0–99 where patients with larger values are more likely to experience hospitalization or death within a year.
Note: Veterans Integrated Services Networks (VISNs) of nearest primary care clinic results removed for conciseness.
Mean Estimated ED Visit Counts
Within each model, mean estimated ED visits counts were consistently higher in all pre-COVID and COVID quarters for patients with older age, for Black patients, for patients living in higher ADI areas (indicating higher levels of neighborhood disadvantage), and for patients with higher frailty. We also noted a larger range of estimated mean counts of visits from the highest to lowest frailty groups (Figure 2D) compared to the age, race, and ADI models. In the model examining race (Figure 2B), we observed significant variation in the “Other” subgroup, which is likely related to having fewer patients in this sample. Results from unadjusted and adjusted models are presented in Supplemental Tables S1, S3, S5, S7.
Figure 2.
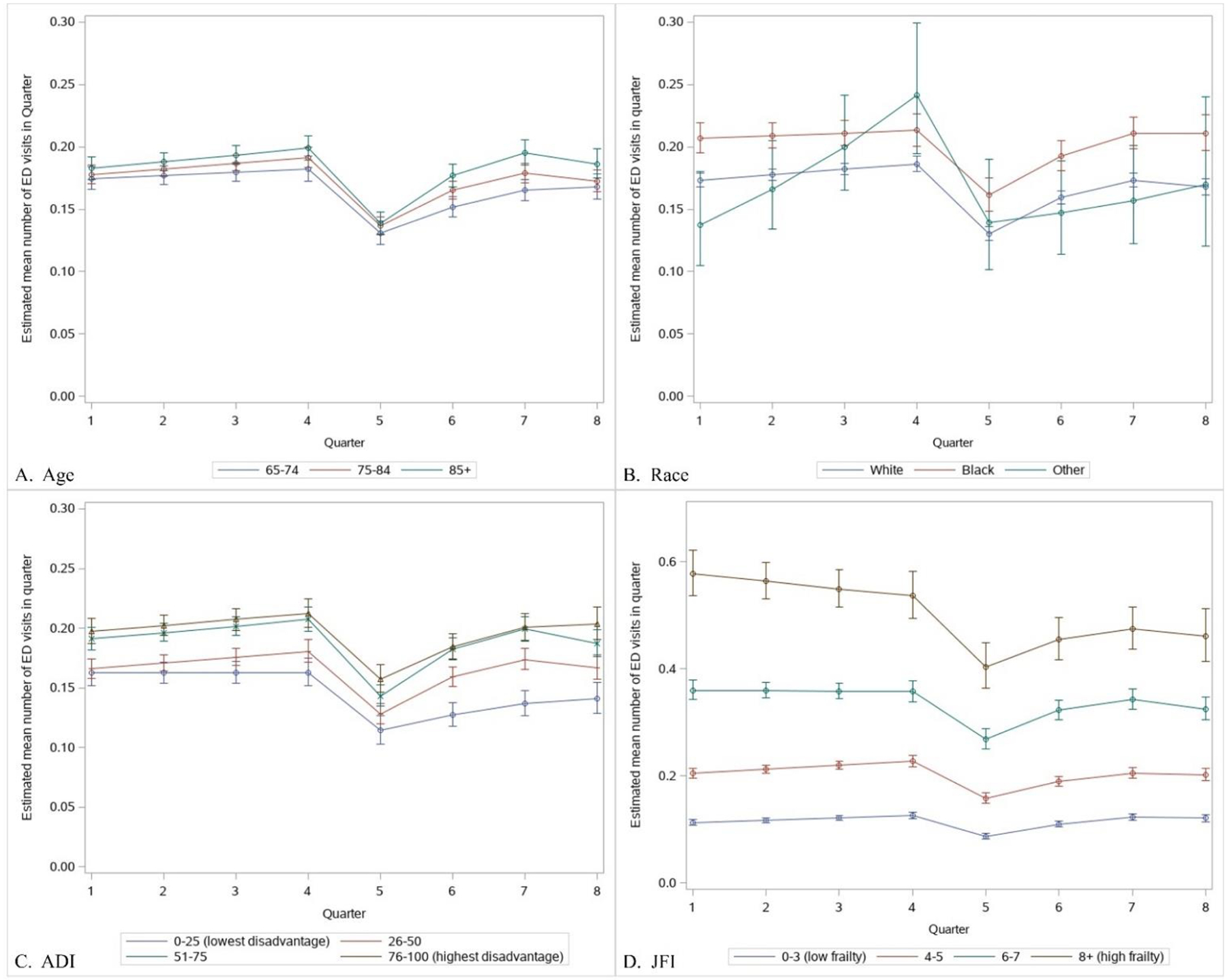
Mean Estimate ED Visit Counts and 95% Confidence Intervals by Subgroups and Quarter, Adjusted Models1
ED = emergency department, ADI = Area deprivation index, JFI = JEN Frailty Index
1 Standardized to 91 days in a quarter
2 Other race includes Asian, American Indian or Alaskan Native, Native Hawaiian or Pacific Islander, or had more than one race identified
3 JFI y-axis differs from other subgroups
Pre Covid-19: Q1=March-May 2019, Q2=June-August 2019, Q3=September-November 2019, Q4=December 2019-February 2020; Post Covid-19: Q5=March-May 2020, Q6=June-August 2020, Q7=September-November 2020, Q8=December 2020-February 2021
Mean Estimate Rate Ratios
With one exception, all subgroups across all models demonstrated statistically significant decreases in ED visits during the first two quarters of the pandemic period (Q5, Q6) compared to their pre-pandemic baselines (Q1, Q2). The “Other” subgroup in the model examining race was the exception, again likely related to the small sample size. Select subgroups continued to have statistically significant decreases in ED visits through the second half of the pandemic period (Q7, Q8) as well: Age 65–74, White patients, 0–25 ADI (those with the lowest neighborhood disadvantage), and those with very high frailty (JFI 8+) or moderate frailty (JFI 4–5). Results from both unadjusted and adjusted models for the rate ratios are presented in Supplemental Tables S2, S4, S6, S8.
Age:
In the age model (Figure 3A), the oldest subgroup (85+) did not have a significant decrease in total ED visits in either of the 2 later quarters of the pandemic. The intermediate age subgroup (75–84) had significantly fewer visits in Q8 (rate ratio 0.90, 0.85–0.96), but not in Q7 (0.96, 95% CI 0.91–1.00). In joint tests assessing differential changes over time by age group, there were no significant differential changes in ED visits by age subgroup in any quarter (Table S2).
Figure 3.
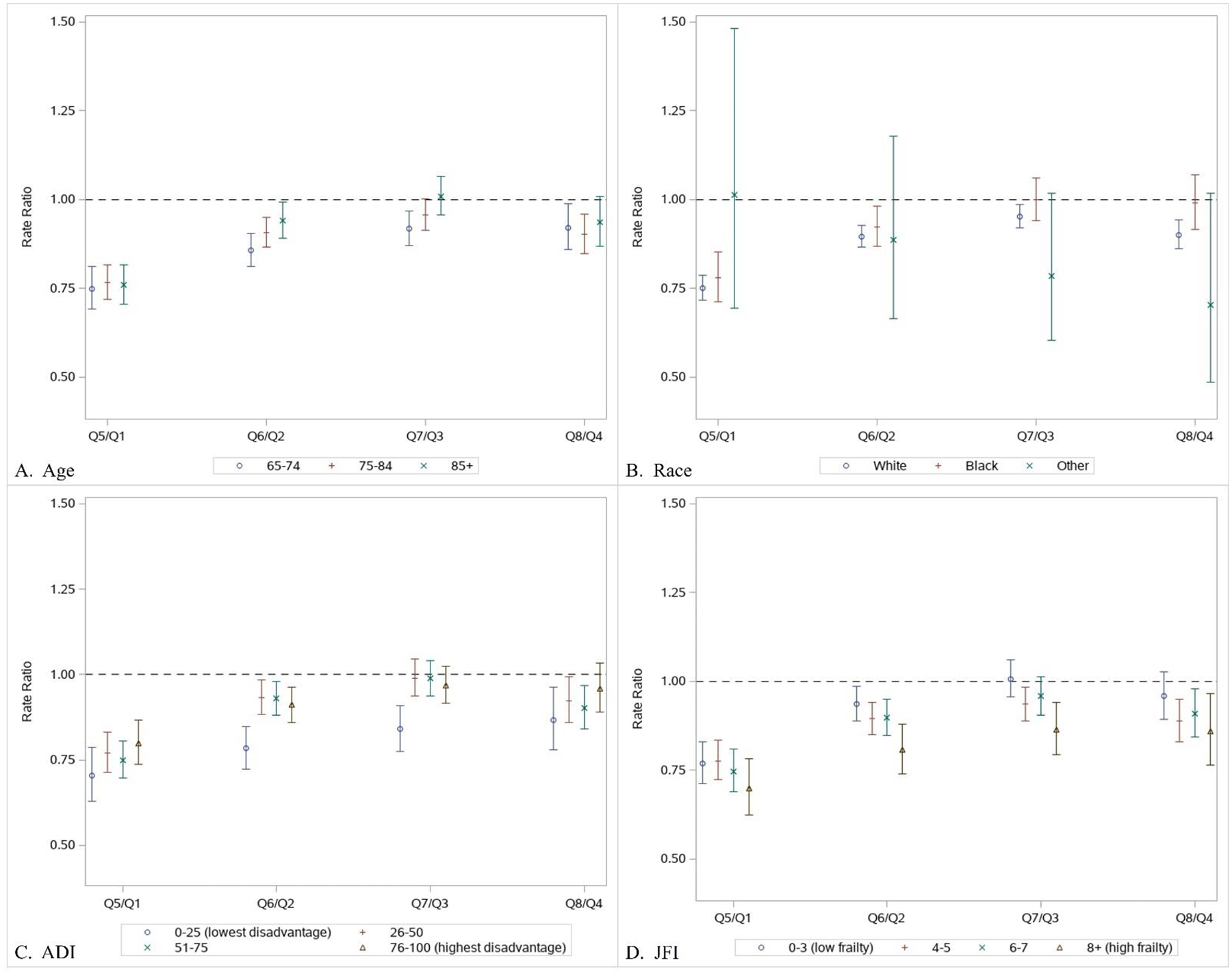
Estimated Rate Ratios and 95% Confidence Intervals by Subgroups and Quarter, Adjusted Models.1
ED = emergency department, ADI = Area deprivation index, JFI = JEN Frailty Index
1 Rate ratio = Mean estimate of number of ED visits in subgroup in Post Covid-19 quarter relative to the mean estimate of number of ED visits in the corresponding Pre Covid-19 quarter one year prior.
2 Other race includes Asian, American Indian or Alaskan Native, Native Hawaiian or Pacific Islander, or had more than one race identified
Pre Covid-19: Q1=March-May 2019, Q2=June-August 2019, Q3=September-November 2019, Q4=December 2019-February 2020; Post Covid-19: Q5=March-May 2020, Q6=June-August 2020, Q7=September-November 2020, Q8=December 2020-February 2021
Race:
In the race model (Figure 3B), while White patients continued to have significantly fewer ED visits in the 2nd half of the pandemic period, Black patients did not have significantly fewer ED visits in either Q7 (1.0, 0.94–1.06) or Q8 (0.99, 0.92–1.07). The other/multiple groups of patients in the race model did not have significantly fewer ED visits in any quarter. In joint tests assessing differential changes over time followed by pairwise comparison tests for each quarter with a differential change, White patients had a significantly greater decrease in ED visits compared to Black patients in the 4th COVID quarter only (p = 0.042) (Table S4).
Area Deprivation Index:
In the ADI model (Figure 3C), for the second half of the pandemic period, the highest disadvantaged group (ADI 76–100) did not have significantly decreased visits in Q7 (0.97, 0.92–1.02) or Q8 (0.96, 0.89–1.03). The intermediate two groups with ADIs of 26–50 and 51–75 both had significantly fewer ED visits in Q8 compared to the seasonally equivalent pre-COVID quarter Q4, but not Q7 when compared to Q3 (26–50: 0.99, 0.94–1.05; 51–75: 0.99, 0.94–1.04). In joint tests assessing differential changes over time followed by pairwise comparison tests, the 0–25 ADI (lowest disadvantage) subgroup had a significantly greater decrease in ED visits compared to the decrease in each of the 3 other ADI groups in both the 2nd and 3rd COVID quarters (Table S6).
JEN Frailty Index:
For the frailty model (Figure 3B), the very high frailty subgroup continued to have significantly decreased ED visits in in Q7 (0.86, 0.79–0.94) and Q8 (0.86, 9.760 0.97), while the low frailty subgroup did not have significant decreases in either Q7 (1.00, 0.95–1.06) or Q8 (0.96, 0.79–1.03). Patterns were mixed for the high and moderate frailty subgroup. In joint tests assessing differential changes over time followed by pairwise comparison tests, the very high frailty JFI subgroup demonstrated a significantly greater decrease in ED visits compared to all other JFI subgroups in the 2nd quarter, and to the low and high frailty subgroups in Q3 (Table S8).
DISCUSSION
To optimally understand variation in ED utilization during the COVID-19 pandemic, we need to better understand which patient and clinical characteristics were associated with the greatest variation in ED visits. This study begins to fill a critical evidence gap by examining how ED use changed among a large cohort of older Veterans. While all subgroups across all models had significant decreases in ED visits in the first two COVID quarters compared to the pre-COVID baseline, both the lowest disadvantage ADI and highest frailty subgroups demonstrated significantly greater sustained decreases in their ED visits through subsequent quarters of the pandemic when compared to their respective other ADI and frailty subgroups.
Our results suggest that very highly frail patients may be especially vulnerable to disruptions in care. Compared to the other models, the JFI score subgroup demonstrated a much wider range of mean estimated total ED visits compared to the other examined subgroups. Most importantly, the very highly frail, who had the highest mean estimated count of ED visits per person through both pre-COVID and COVID periods, also had a significant decrease in their ED visits during multiple quarters of the pandemic to a greater degree than other JFI subgroups. The adjusted models demonstrate the association of very high frailty and decreased ED visits, even after controlling for other sociodemographic and clinical characteristics. This association is seen in unadjusted models as well (Supplemental Materials), which indicates that frailty could be used broadly by health systems as a straightforward way to identify populations at risk without requiring more complex modeling.
It is surprising that very highly frail patients were less likely to resume their usual emergency care in the latter half of the pandemic time period. Given their greater rates of co-morbidities and vulnerability to stressors,23 along with likely delays in outpatient care for their chronic conditions during COVID, it might be anticipated that this would lead to less change in need for acute care and ED visits compared to less frail patients. One possible explanation is that some of their pre-pandemic visits could be attributed as “avoidable” ED visits; however it seems unlikely that they had more avoidable visits compared to less frail patients in the pre-pandemic period given increased frailty is generally associated with higher rates of adverse post-ED outcomes.24–26 Another interpretation is that this population was recognized as more vulnerable to COVID and thus elected to stay away from ED and hospital settings, but even so, it is still possible that they then missed out on necessary acute care.
In administrative data studies, frailty has previously demonstrated important associations with health outcomes in multiple contexts. In prior VA work, using JFI in a model predicting long term institutionalization made it more accurate,27 and JFI has been used to predict hospitalization for Veterans in a home-based primary care program.28 In the ED setting, other frailty measures have demonstrated associations with higher ED utilization, as well as adverse 30-day outcomes, but not repeat ED visits.29,30 However, less is known about health outcomes associated with the use of bedside clinical assessments of frailty at the time of an ED visit.31 While some clinical measures, such as the Clinical Frailty Scale, are becoming more prevalent in the ED, little is known about how the use of a frailty assessment impacts subsequent ED care processes or clinical outcomes.32 Frailty may be best assessed as just one part of a comprehensive geriatric assessment in the ED, but the feasibility of providing these assessments to all older adults has not been established.33 Similar to other specialties, routine use of frailty assessments is limited by the heterogeneity of frailty measures available, and lack of consensus around how to manage frailty.34 Overall, this suggests that frailty metrics need to be made more routinely available to clinicians, researchers, administration, and policy-makers, but significant work is still needed to integrate it into research and clinical practice.
We also note that patients in the 0–25 ADI subgroup (those living in the least disadvantaged neighborhoods) demonstrated significantly greater decreases in ED visits during the pandemic compared to other ADI subgroups. Given that residing in a low disadvantaged neighborhood is generally a protective factor in health, this decrease may be based on a different mechanism than the high frailty subgroups.35–37 One possibility is that patients living in low disadvantaged neighborhoods found other means to seek health care during the first year of the pandemic; previous work has demonstrated that lower ADI is associated with more willingness to use video visits among Veterans.38 However, even if willing, it is possible that highly frail patients were less able to use other means of outpatient health care due to other limitations. They also may have been less willing to present to the ED given concern for higher risk of COVID-19 infection. This also suggests an important focus for future work, looking at how variation in ED care driven by disparities in neighborhood disadvantage impacted clinical outcomes for geriatric patients during the pandemic.
Limitations: First, this cohort of patients is derived from the parent GeriPACT study and is not all-inclusive of VA ED patients. However, this was a unique opportunity to understand care for older patients, especially the oldest old, and to link to measures not widely available for a geriatric VA population such as the JFI. Additionally, the use of the ADI as a covariate is a composite measure of capturing social disadvantage and may need further exploration to find modifiable factors. Third, while comparing each quarter during COVID to their equivalent pre-pandemic quarter in terms of seasons is helpful to control for seasonal variation, this makes it difficult to capture other changes that might be related solely to subsequent COVID waves. Fourth, we limited our selection of subgroups of interest to the four included here as we believed they would impact ED utilization, but we acknowledge there are other patient-level characteristics that likely had a noteworthy impact on ED use. In particular, similar to community settings, dementia is well known to be associated with increased ED use in the VA.39 While dementia is one of the clinical diagnoses incorporated in the JFI, future work could be done to examine this as a specific patient-level characteristic. Fifth, we captured only VA provided or purchased ED visits, and did not include ED visits in the community paid for by Medicare or other means. This may limit the differential effects seen during COVID. Finally, this study cannot empirically address why visit counts changed, and explanations for these changes will require further investigation to suggest causality. However, we hope to find those areas of greatest change to suggest directions for this further work.
CONCLUSION
Our findings that very highly frail older Veterans had a differential decrease in ED visits in multiple quarters of the first year of the COVID-19 pandemic suggest targeted directions for future research on variations in ED care and outcomes. This work is particularly urgent given the growing population of older Veterans and significant resource allocation to enhancing geriatric-focused care in the ED setting and beyond.
Supplementary Material
Figure 1.
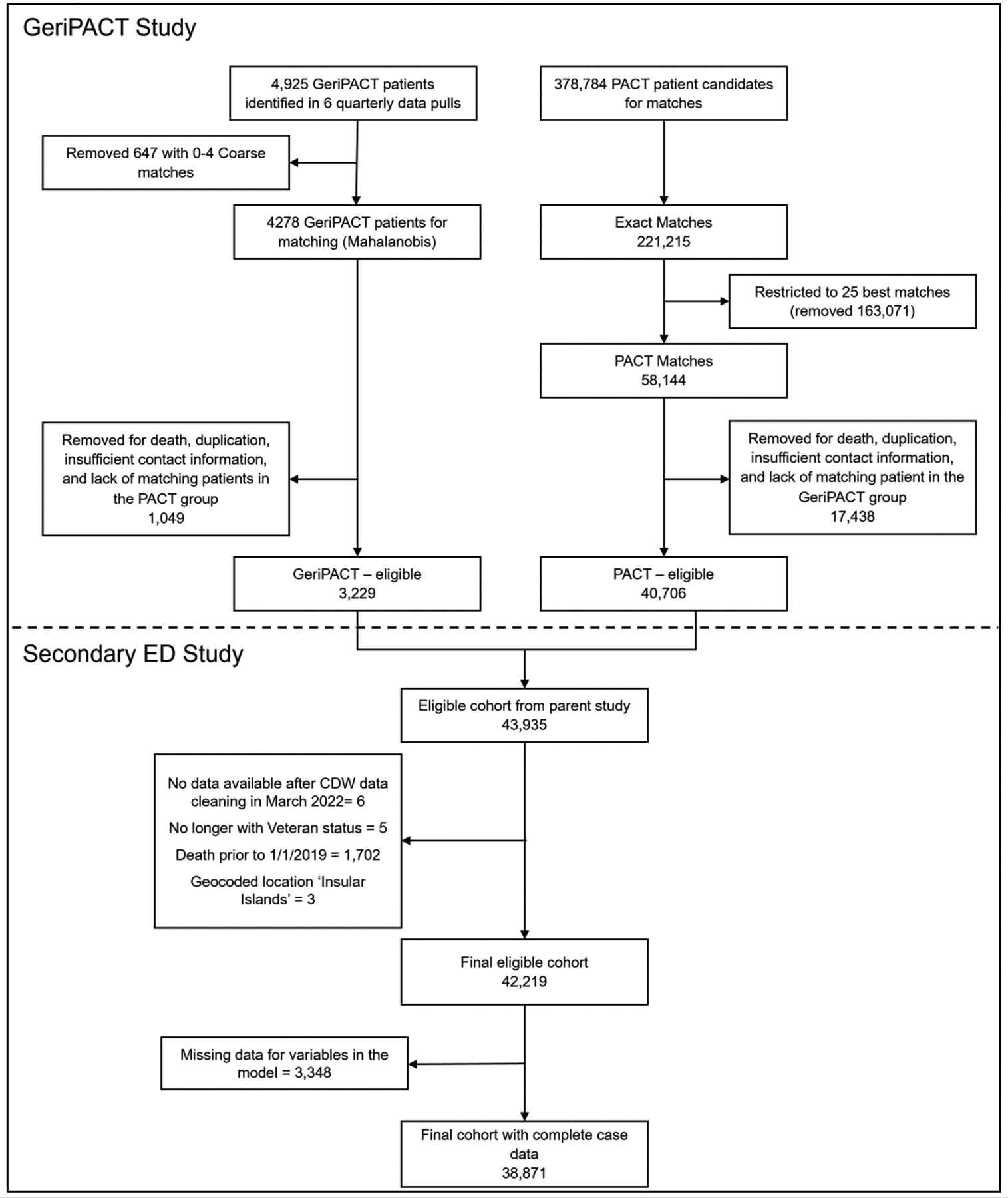
Study Flow Diagram.
ACKNOWLEDGMENTS
The authors would like to thank Jennifer Lindquist for her assistance in the acquisition of data included in this manuscript.
Funding:
The analysis was funded by the VA Health Services Research and Development (HSR&D) grant IIR 15–379 and was supported by the Center of Innovation to Accelerate Discovery and Practice Transformation at the Durham VA Health Care System (Grant No. CIN 13–410). Dr. Seidenfeld is funded by US Department of Veterans Affairs Health Services Research and Development Service Career Development Award 23–189 (IK2HX003673). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the United States government, or Duke University.
Footnotes
CONFLICTS OF INTEREST
Authors report no financial nor personal conflicts of interest.
Contributor Information
Justine Seidenfeld, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham VA Health Care System, Durham, NC, USA; Department of Emergency Medicine, Durham VA Health Care System, Durham, NC, USA; Department of Emergency Medicine, Duke University School of Medicine, Durham, NC, USA.
Karen M. Stechuchak, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham VA Health Care System, Durham, NC, USA; Department of Population Health Sciences, Duke University School of Medicine, Durham, NC, USA; Department of Medicine, Duke University School of Medicine, Durham, NC, USA.
Valerie A. Smith, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham VA Health Care System, Durham, NC, USA; Department of Population Health Sciences, Duke University School of Medicine, Durham, NC, USA; Department of Medicine, Duke University School of Medicine, Durham, NC, USA.
Catherine Stanwyck, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham VA Health Care System, Durham, NC, USA; Department of Medicine, Duke University School of Medicine, Durham, NC, USA.
Chelsea Perfect, Department of Medicine, Duke University School of Medicine, Durham, NC, USA.
Courtney Van Houtven, Center for the Study of Human Aging and Development, Duke University School of Medicine, Durham, NC, USA; Geriatric Research, Education, and Clinical Center, Durham VA Health Care System, Durham, NC, USA.
Susan Nicole Hastings, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham VA Health Care System, Durham, NC, USA; Department of Population Health Sciences, Duke University School of Medicine, Durham, NC, USA; Department of Medicine, Duke University School of Medicine, Durham, NC, USA; Center for the Study of Human Aging and Development, Duke University School of Medicine, Durham, NC, USA; Geriatric Research, Education, and Clinical Center, Durham VA Health Care System, Durham, NC, USA.
REFERENCES
- 1.Hwang U, Runels T, Han L, et al. Dissemination and implementation of age-friendly care and geriatric emergency department accreditation at Veterans Affairs hospitals. Acad Emerg Med. Apr 2023;30(4):270–277. doi: 10.1111/acem.14665 [DOI] [PubMed] [Google Scholar]
- 2.Kennedy M, Lesser A, Israni J, et al. Reach and Adoption of a Geriatric Emergency Department Accreditation Program in the United States. Ann Emerg Med. Apr 2022;79(4):367–373. doi: 10.1016/j.annemergmed.2021.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward MJ, Hwang U, Hastings SN, et al. Research and policy recommendations from the SOTA XVI: State of the Art Conference on VA Emergency Medicine. Acad Emerg Med. Apr 2023;30(4):240–251. doi: 10.1111/acem.14679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park S, Stimpson JP. Trends in self-reported forgone medical care among medicare beneficiaries during the COVID-19 pandemic. American Medical Association; 2021:e214299–e214299. doi: 10.1001/jamahealthforum.2021.4299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Callison K, Ward J. Associations Between Individual Demographic Characteristics And Involuntary Health Care Delays As A Result Of COVID-19. Health Aff (Millwood). May 2021;40(5):837–843. doi: 10.1377/hlthaff.2021.00101 [DOI] [PubMed] [Google Scholar]
- 6.Gale R, Eberlein S, Fuller G, Khalil C, Almario CV, Spiegel BMR. Public Perspectives on Decisions About Emergency Care Seeking for Care Unrelated to COVID-19 During the COVID-19 Pandemic. JAMA Netw Open. Aug 2 2021;4(8):e2120940. doi: 10.1001/jamanetworkopen.2021.20940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farina MP, Ailshire JA. Sociodemographic and health status differences in delaying medical care during the COVID-19 pandemic among older adults: findings from the Health and Retirement Study. BMC Public Health. Sep 10 2022;22(1):1720. doi: 10.1186/s12889-022-14118-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venkatesh AK, Janke AT, Shu-Xia L, et al. Emergency Department Utilization for Emergency Conditions During COVID-19. Ann Emerg Med. Jul 2021;78(1):84–91. doi: 10.1016/j.annemergmed.2021.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giannouchos TV, Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med. Feb 2021;40:20–26. doi: 10.1016/j.ajem.2020.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gutovitz S, Pangia J, Finer A, Rymer K, Johnson D. Emergency Department Utilization and Patient Outcomes During the COVID-19 Pandemic in America. J Emerg Med. Jun 2021;60(6):798–806. doi: 10.1016/j.jemermed.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rennert-May E, Leal J, Thanh NX, et al. The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS One. 2021;16(6):e0252441. doi: 10.1371/journal.pone.0252441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowe J, Brown I, Duriseti R, et al. Emergency Department Access During COVID-19: Disparities in Utilization by Race/Ethnicity, Insurance, and Income. West J Emerg Med. Apr 28 2021;22(3):552–560. doi: 10.5811/westjem.2021.1.49279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu J, Hammond G, Waken RJ, Fox D, Joynt Maddox KE. Changes In Non-COVID-19 Emergency Department Visits By Acuity And Insurance Status During The COVID-19 Pandemic. Health Aff (Millwood). Jun 2021;40(6):896–903. doi: 10.1377/hlthaff.2020.02464 [DOI] [PubMed] [Google Scholar]
- 14.Smulowitz PB, O’Malley AJ, Khidir H, Zaborski L, McWilliams JM, Landon BE. National Trends In ED Visits, Hospital Admissions, And Mortality For Medicare Patients During The COVID-19 Pandemic. Health Aff (Millwood). Sep 2021;40(9):1457–1464. doi: 10.1377/hlthaff.2021.00561 [DOI] [PubMed] [Google Scholar]
- 15.Smith VA, Van Houtven CH, Lindquist JH, Hastings SN. Evaluation of a geriatrics primary care model using prospective matching to guide enrollment. BMC Med Res Methodol. Aug 16 2021;21(1):167. doi: 10.1186/s12874-021-01360-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sullivan JL, Shin MH, Adjognon OL, et al. Geriatric patient-aligned care teams in Department of Veterans Affairs: how are they structured? Geriatrics. 2018;3(3):46. doi: 10.3390/geriatrics3030046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). Jul 2014;33(7):1203–11. doi: 10.1377/hlthaff.2014.0054 [DOI] [PubMed] [Google Scholar]
- 18.Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med. Jun 28 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michaels AD, Meneveau MO, Hawkins RB, Charles EJ, Mehaffey JH. Socioeconomic risk-adjustment with the Area Deprivation Index predicts surgical morbidity and cost. Surgery. Nov 2021;170(5):1495–1500. doi: 10.1016/j.surg.2021.02.016 [DOI] [PubMed] [Google Scholar]
- 20.Luningham JM, Seth G, Saini G, et al. Association of Race and Area Deprivation With Breast Cancer Survival Among Black and White Women in the State of Georgia. JAMA Netw Open. Oct 3 2022;5(10):e2238183. doi: 10.1001/jamanetworkopen.2022.38183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kinosian B, Wieland D, Gu X, Stallard E, Phibbs CS, Intrator O. Validation of the JEN frailty index in the National Long-Term Care Survey community population: identifying functionally impaired older adults from claims data. BMC Health Serv Res. Nov 29 2018;18(1):908. doi: 10.1186/s12913-018-3689-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Orkaby AR, Huan T, Intrator O, et al. Comparison of Claims-Based Frailty Indices in US Veterans 65 and Older for Prediction of Long-Term Institutionalization and Mortality. The Journals of Gerontology: Series A. 2023;78(11):2136–2144. doi: 10.1093/gerona/glad157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. Mar 2 2013;381(9868):752–62. doi: 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elliott A, Taub N, Banerjee J, et al. Does the Clinical Frailty Scale at Triage Predict Outcomes From Emergency Care for Older People? Ann Emerg Med. Jun 2021;77(6):620–627. doi: 10.1016/j.annemergmed.2020.09.006 [DOI] [PubMed] [Google Scholar]
- 25.Rueegg M, Nissen SK, Brabrand M, et al. The clinical frailty scale predicts 1-year mortality in emergency department patients aged 65 years and older. Acad Emerg Med. May 2022;29(5):572–580. doi: 10.1111/acem.14460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dev S, Gonzalez AA, Coffing J, et al. Validating administratively derived frailty scores for use in Veterans Health Administration emergency departments. Acad Emerg Med. Apr 2023;30(4):349–358. doi: 10.1111/acem.14705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jacobs JC, Maciejewski ML, Wagner TH, et al. Improving Prediction of Long-Term Care Utilization Through Patient-Reported Measures: Cross-Sectional Analysis of High-Need U.S. Veterans Affairs Patients. Med Care Res Rev. Oct 2022;79(5):676–686. doi: 10.1177/10775587211062403 [DOI] [PubMed] [Google Scholar]
- 28.Gillespie SM, Li J, Karuza J, et al. Factors Associated With Hospitalization by Veterans in Home-Based Primary Care. J Am Med Dir Assoc. May 2021;22(5):1043–1051 e1. doi: 10.1016/j.jamda.2020.12.033 [DOI] [PubMed] [Google Scholar]
- 29.Hastings SN, Purser JL, Johnson KS, Sloane RJ, Whitson HE. Frailty predicts some but not all adverse outcomes in older adults discharged from the emergency department. J Am Geriatr Soc. Sep 2008;56(9):1651–7. doi: 10.1111/j.1532-5415.2008.01840.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kojima G Frailty as a Predictor of Emergency Department Utilization among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. Jan 2019;20(1):103–105. doi: 10.1016/j.jamda.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 31.Lo AX, Heinemann AW, Gray E, et al. Inter-rater Reliability of Clinical Frailty Scores for Older Patients in the Emergency Department. Acad Emerg Med. Jan 2021;28(1):110–113. doi: 10.1111/acem.13953 [DOI] [PubMed] [Google Scholar]
- 32.Selman K, Shenvi C. What’s in a Name? Understanding Failure to Thrive and Frailty in the Emergency Department. Journal of Geriatric Emergency Medicine. 2022;3(1):2. doi: 10.17294/2694-4715.1021 [DOI] [Google Scholar]
- 33.Hogervorst VM, Buurman BM, De Jonghe A, et al. Emergency department management of older people living with frailty: a guide for emergency practitioners. Emerg Med J. Sep 2021;38(9):724–729. doi: 10.1136/emermed-2020-210014 [DOI] [PubMed] [Google Scholar]
- 34.Walston J, Robinson TN, Zieman S, et al. Integrating Frailty Research into the Medical Specialties-Report from a U13 Conference. J Am Geriatr Soc. Oct 2017;65(10):2134–2139. doi: 10.1111/jgs.14902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trinidad S, Brokamp C, Mor Huertas A, et al. Use Of Area-Based Socioeconomic Deprivation Indices: A Scoping Review And Qualitative Analysis. Health Aff (Millwood). Dec 2022;41(12):1804–1811. doi: 10.1377/hlthaff.2022.00482 [DOI] [PubMed] [Google Scholar]
- 36.Markey C, Bello O, Hanley M, Loehrer AP. The Use of Area-Level Socioeconomic Indices in Evaluating Cancer Care Delivery: A Scoping Review. Ann Surg Oncol. May 2023;30(5):2620–2628. doi: 10.1245/s10434-023-13099-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Foster HME, Celis-Morales CA, Nicholl BI, et al. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. Lancet Public Health. Dec 2018;3(12):e576–e585. doi: 10.1016/S2468-2667(18)30200-7 [DOI] [PubMed] [Google Scholar]
- 38.Dang S, Muralidhar K, Li S, et al. Gap in Willingness and Access to Video Visit Use Among Older High-risk Veterans: Cross-sectional Study. J Med Internet Res. Apr 8 2022;24(4):e32570. doi: 10.2196/32570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seidenfeld J, Dalton A, Vashi AA. Emergency department utilization and presenting chief complaints by Veterans living with dementia. Acad Emerg Med. Apr 2023;30(4):331–339. doi: 10.1111/acem.14686 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


