Abstract
Air embolism is a rare cause of ischaemic stroke. It is known that air can enter the cerebral arterial circulation from pulmonary venous circulation through a bronchovenous fistula, or in cases of pulmonary barotrauma in deep-sea diving. We describe a case of spontaneous cerebral air embolism against a background of advanced interstitial lung disease (ILD). To our knowledge, this case demonstrates a mechanism of stroke in ILD patients that has not been previously described.
LEARNING POINTS
This case demonstrates a mechanism of stroke in patients with severe interstitial lung disease (ILD) that has not been previously described, and we suggest that in cases of advanced ILD, clinicians should consider this as a possible mechanism of stroke. The management of these patients should include transferring them to hyperbaric facilities to prevent further air emboli.
Keywords: Cerebral air embolism, stroke, interstitial lung disease, pneumomediastinum, pneumothorax
CASE DESCRIPTION
A patient in his 70s with a history of advanced idiopathic ILD was admitted with infective exacerbation of his chronic lung disease and was treated with oral antibiotics. He was a non-smoker and his past medical history included atrial fibrillation (AF) and bilateral pulmonary emboli – for which he was on lifelong rivaroxaban – gastritis, and a recent non-ST elevation myocardial infraction. He had a very limited exercise tolerance and was unable to leave the house. A chest X-ray on admission demonstrated a slight increase in the size of the chronic bilateral apical pneumothorax. However, the pneumothorax was small and not amenable to drainage. As the patient had a fall prior to admission, a computed tomography (CT) scan of his brain was performed, which showed no acute intracranial pathology.
On day 2 of admission, following loss of balance and a fall on the ward, the patient was found to have cerebellar signs – past pointing and dysdiadochokinesia in the right upper and lower limbs – and an unsteady gait. No repeat CT of the head was performed at the time. A magnetic resonance imaging (MRI) head scan on day 8 demonstrated multiple areas of restricted diffusion in the left posterior frontal lobe, bilateral parietal lobes, right lateral occipital lobes and bilateral cerebellar hemispheres. This was suggestive of subacute ischaemic infarcts of varying ages in multiple vascular territories (Fig. 1). He was transferred to the hyperacute stroke unit for monitoring and rehabilitation. A CT angiogram ruled out large-vessel stenosis; an echocardiogram ruled out any cardiac thrombus and no features to support patent foramen ovale were present, so it was assumed that these multiple infracts were AF induced. His anticoagulant was switched to apixaban. With daily therapy, he progressed well and was able to start mobilising with a walking frame under supervision. He was not on intravenous fluids.
Figure 1.
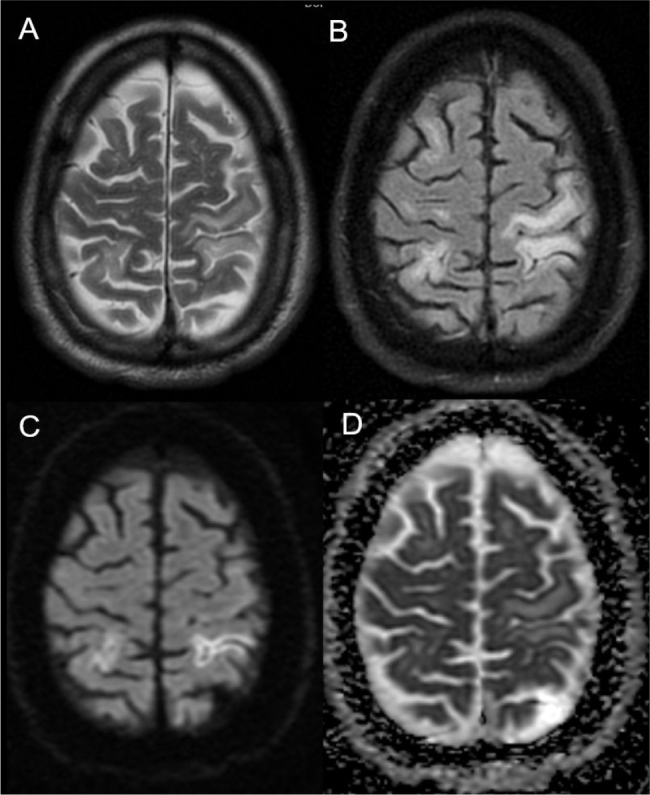
MRI at day 8 showing cortical T2 hyperintensity and swelling affecting bilateral frontal and parietal lobes (A), with commensurate changes on FLAIR (B). Cortical diffusion restriction in bilateral parietal cortices (C), confirmed on apparent diffusion coefficient maps (D), in keeping with ischaemia. There was further ischaemia affecting the left superior parietal lobe and bilateral cerebellar hemispheres (not shown).
On day 11, he vomited a large amount of food matter and 15 minutes later was found unresponsive in his chair with fixed right gaze deviation, a Glasgow coma scale of 6 (E3, M1, V2), a sudden drop from 15. He was haemodynamically stable with no respiratory compromise. An urgent CT head scan demonstrated air emboli in bilateral frontal sulci and the left parietal lobe (Fig. 2A), as well as in the left cerebellum (Fig. 2B). A CT scan of thorax and abdomen demonstrated bilateral pneumothorax and pneumomediastinum tracking inferiorly adjacent to the oesophagus and anterior to the great vessels, with no evidence of malignancy (Fig. 2C). As twitching activity was noted in his limbs on the right side, he was started on levetiracetam intravenously. No venous air emboli were demonstrated on a CT venogram. A repeat CT head scan 24 hours later showed bilateral diffuse vasogenic oedema and sulci effacement with evolving infarcts in bilateral frontoparietal lobes and bilateral cerebellar hemispheres (Fig. 3).
Figure 2.
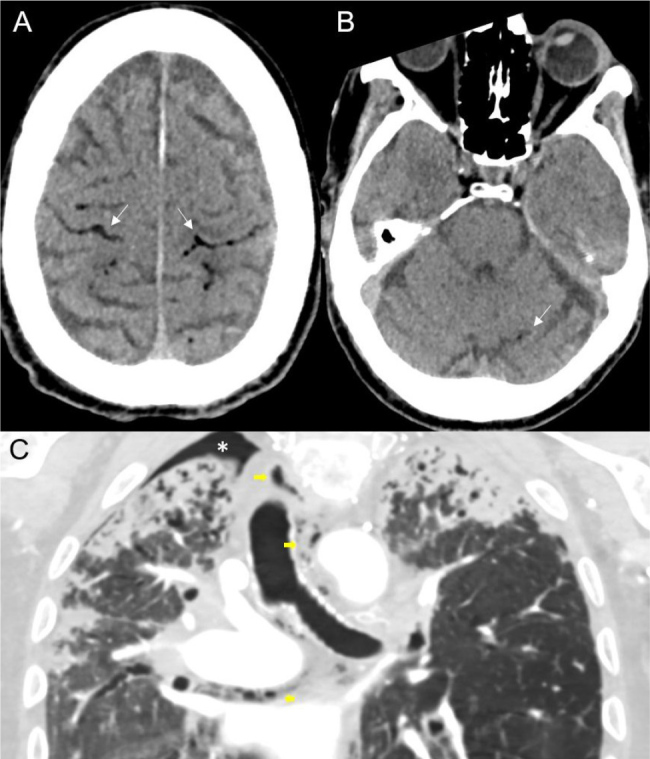
CT at day 11 showing intracranial gas at the bilateral frontal and parietal cortical-sulcal interface (arrows, A) and in left cerebellar hemisphere (arrows, B). CT scan of thorax and abdomen demonstrated bilateral pneumothorax and pneumomediastinum tracking inferiorly adjacent to the oesophagus and anterior to the great vessels (C).
Figure 3.
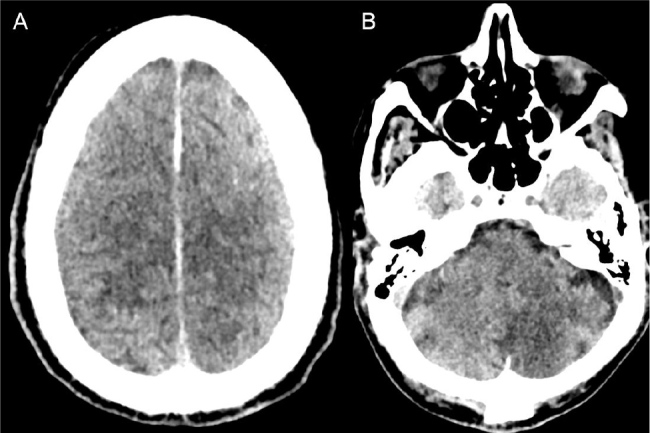
CT at day 12 showing resolution/resorption of intracranial gas, with rapid progression in ischaemia oedema and brain swelling at the vertex (A), and ischaemia in left cerebellar hemisphere (B).
The pneumocephalus had dissipated but a small amount of gas was found within the carotid sheath. In view of extensive cerebral damage and as the patient’s clinical status remained unchanged, a palliative approach was agreed; he passed away a few days later. Throughout this admission and in the preceding few months, the patient experienced no haemoptysis or haematemesis, there was no history of positive airway pressure ventilation and he had received no iatrogenic puncture wounds in the neck or thorax.
DISCUSSION
In the majority of cases of cerebral air embolism in the literature, the air finds its way into the venous circulation following a trauma or an iatrogenic method. It can also result from a neurosurgical, orthopaedic or laparoscopic procedure, a vascular procedure for example central line insertion or haemodialysis, or as a complication of mechanical ventilation[1].
The most common reason for spontaneous non-iatrogenic air embolism is deep-sea diving, in particular when a diver surfaces too quickly or holds their breath while swimming to the surface, causing pulmonary barotrauma. This also can occur during an aircraft flight, caused by external decompression during ascent[2]. Adelowo et al. reported a case of pulmonary air leak syndrome secondary to inflammatory polyarthritis-related ILD, in which the patient eventually developed widespread subcutaneous emphysema[3].
To our knowledge, a case of spontaneous (non-traumatic, non-iatrogenic) cerebral air embolism in advanced ILD is rarely reported in the literature. A systematic search was undertaken to find relevant articles on spontaneous cerebral air embolism, using the following search strategies: ‘(spontaneous cerebral air embolus OR cerebral air embolism OR cerebral gas embolus) AND (interstitial lung disease OR pneumothorax OR chronic lung disease)’. Our search resulted in only three articles of similar cases.
Alagha et al. described a case where a patient experienced transient ischaemic attack symptoms with expressive aphasia and right-hand weakness; he was later found to have spontaneous pneumothorax, but also a patent foramen ovale. His symptoms lasted only five minutes and were presumed to be due to cerebral air embolism secondary to paradoxical embolism[4]. Gardner et al. described a case of spontaneous cerebral air embolism four years after resection of a non-small cell lung cancer tumour[5].
Our patient had no history of trauma, or surgical or vascular procedures. On review of his scans, no intracardiac or intravascular gas was demonstrated on CT studies prior to cerebral air embolism. Spontaneous pneumomediastinum occurs in ILD due to the Macklin effect, which describes alveolar rupture following an increase in intrathoracic pressure, resulting in air dissection through the bronchovascular sheath into the mediastinum[6]. We hypothesise that advanced fibrosis damaged the structural integrity of our patient’s lungs, and the air entered his pulmonary venous vasculature at the level of alveoli, facilitated by sudden increase in intrathoracic pressure during vomiting. The air in the pulmonary veins then entered the left atrium, subsequently into the left ventricle, resulting in recurrent cerebral air emboli and extensive ischaemic strokes.
CONCLUSION
This case demonstrates a mechanism of stroke in ILD that has not been previously described and we suggest that in cases of advanced ILD, clinicians should consider this as a possible mechanism of stroke. If initial imaging demonstrates cerebral air embolism, supportive measures such as administration of 100% oxygen and transporting the patient to a hyperbaric facility may be considered to prevent further emboli, however, their effectiveness has not been proved in the literature.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
Patient Consent: A written consent was obtained from the patient’s next of kin.
REFERENCES
- 1.Squitieri M, Poggesi A, Cecchi A, Di Lascio G, Gadda D, Lombardo I, et al. Cerebral air embolism: a non-thrombotic cause of acute stroke. Arch Clin Med Case Rep. 2020;4:1071–1077. [Google Scholar]
- 2.Brennan D, Brennan P, O’Rourke J, Looby S. Cerebral air embolism during air flight-neuroimaging and management. Can J Neurol Sci. 2016;43:841–842. doi: 10.1017/cjn.2016.288. [DOI] [PubMed] [Google Scholar]
- 3.Adelowo O, Akintayo RO, Olaosebikan H, Oba R. Recurrent spontaneous subcutaneous emphysema in a patient with rheumatoid arthritis. BMJ Case Rep. 2015;2015:bcr2015210802. doi: 10.1136/bcr-2015-210802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alagha Z, Al-Astal A. A rare case of spontaneous pneumothorax leading to cerebral air embolism. Cureus. 2024;16:e52277. doi: 10.7759/cureus.52277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardner R, Wang LH, Ford A, Keyrouz SG. Spontaneous cerebral air embolism associated with remote lung surgery. Neurocrit Care. 2008;8:434–436. doi: 10.1007/s12028-008-9073-z. [DOI] [PubMed] [Google Scholar]
- 6.Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiments. Medicine (Baltimore) 1944;23:281–358. [Google Scholar]


