Abstract
Vaginal discharge is a common gynaecologic complaint in pre-menarchal girls. However, an intravaginal foreign body (FB) must be suspected when it is persistent. We report the case of a referred 4-year-old girl with a 5-month history of persistent foul-smelling vaginal discharge. Clinical examination confirmed purulent vaginal discharge, along with a vaginal granuloma. A hard, intravaginal object was felt through the anterior rectal wall on digital rectal examination. A plain pelvic X-ray revealed a radiopaque object whose intravaginal position was confirmed by ultrasonography. The patient underwent granuloma excision plus FB removal and antibiotic treatment. The 12-month follow-up was unremarkable.
Keywords: Foreign body, intravaginal, pre-menarchal girl, vaginal discharge, vulvovaginitis
INTRODUCTION
Vaginal discharge is a frequent complaint in pre-menarchal girls. Many aetiologies are described, but the most frequently evocated is the low oestrogen level, with its consequences on vaginal flora disturbance.[1] Intravaginal foreign body (IVFB) is a rare cause of vaginitis with vaginal discharge.[2,3] It occurs mainly in toddler girls, and symptoms depend on the shape, chemical composition and retention time.[3] Severe complications can occur due to delayed diagnosis.[4,5]
We report a case of a 4-year-old girl who was referred for persistent vaginal discharge due to an IVFB.
CASE REPORT
A 4-year-old girl was referred to our paediatric surgery department for persistent vaginal discharge, which started 5 months before the referral. The patient was seen in a district hospital where oestrogen cream and per-oral metronidazole were started, without any improvement after a month. Due to the persistence of foul-smelling vaginal discharge, the patient attended a referring hospital where vaginitis was diagnosed. Analysis of vaginal discharge identified methicillin-sensitive Staphylococcus aureus (MSSA), and then the patient underwent per-oral oxacillin without any change of the symptoms. Two months later, the patient was referred to us.
The mother complained of foul-smelling vaginal discharge. No history of sexual abuse or suspicion of child abuse was reported.
There were traces of purulent discharge on the vulva on clinical examination, which was taken on a swab for bacteriological examination. A granuloma was protruding through the vulva [Figure 1]. Further examination showed an intact hymen, an erythematous vaginal mucosa and an intravaginal granuloma. No intravaginal object was seen at this stage. On digital rectal examination (DRE), a solid object was felt in the vagina through the anterior rectal wall. No fistula was felt. A pelvic ultrasound was ordered, and a plain X-ray was to identify any foreign body (FB). The ultrasound revealed the presence of an IVFB, visible on the plain X-ray as a radiopaque, three-shaped object on the projection of the pubic symphysis [Figure 2]. During retrospective interrogation, after identifying an IVFB, the patient revealed an older female friend (7 years old) inserted an earring inside her genitals while playing some months ago. The full-blood count did not show any anomaly.
Figure 1.
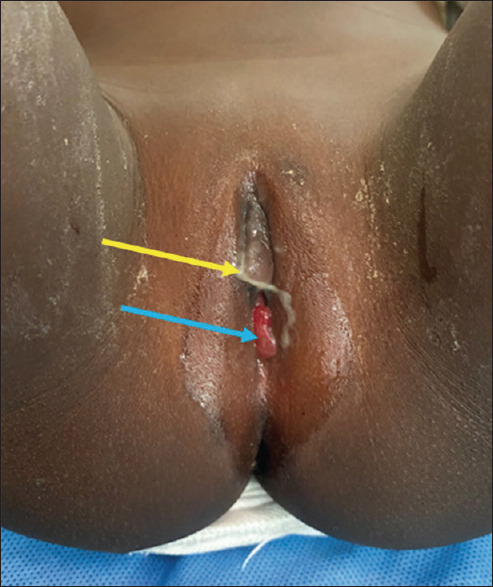
Genital examination. Purulent vaginal discharge on the vulva of the patient (yellow arrow) and a granuloma was protruding through the vulva (blue arrow)
Figure 2.

Abdominal X-ray. Note the three-shaped radio-opaque foreign body on the projection of the pubic symphysis (yellow arrow)
The patient underwent FB removal under general anaesthesia. We first proceeded to excision of the granuloma [Figure 3], which was sent to pathology. After that, with fine Kelly forceps, we extracted the IVFB, which was an earring [Figure 4]. Paracetamol was given as post-operative analgesia; empirical antibiotherapy was started with amoxicillin plus clavulanic acid, and daily sit baths using lukewarm water and Cytéal® for 5 days. Bacteriological results reported an MSSA, then amoxicillin plus clavulanic acid was continued for 10 days. The results of pathology confirmed that the removed tissue was a reactive granuloma.
Figure 3.
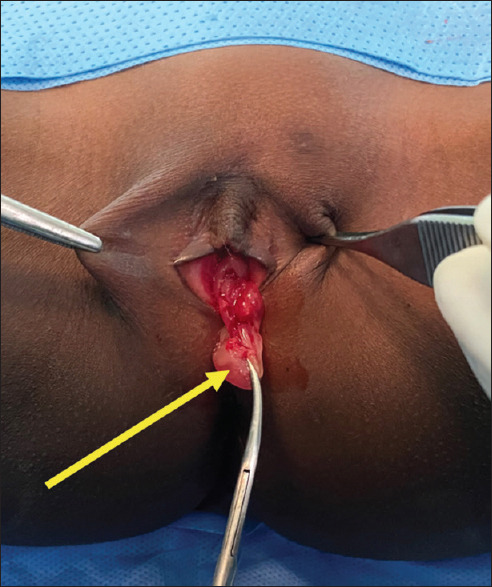
Intraoperative image. Excision of the granuloma arose from the vaginal mucosa (yellow arrow)
Figure 4.

The removed intravaginal foreign body, an earring
When reviewed on day 3 post-removal, no vaginal discharge was identified. No complaint was reported on the following appointments (week 2, 1 month, 3, 6 and 12 post-removal), and the physical examination was normal.
DISCUSSION
Vaginal discharge is a frequent complaint in pre-menarchal girls. In most patients, it is due to a lower level of oestrogen, which increases vaginal pH and leads to easy colonisation of the vaginal milieu by other non-commensal pathogens.[1] Other frequent causes are bacterial or fungal vulvovaginitis and diaper dermatitis.[3] In rare circumstances, vaginal discharge is due to IVFB, representing approximately 4% of pre-menarchal girls with gynaecologic complaints.[3] In children, it occurs mainly in patients younger than 8 years. However, older patients’ cases have been reported.[6]
This condition is challenging to diagnose due to the poor communication of the child, who does not always remember the insertion of a FB. In a 35-patient cohort, only 21 recalled the insertion of the FB, amongst whom two patients remembered insertion in hindsight after its removal.[3] This was the case with our patient. In children, insertion happens while playing several games, and in most cases (73%), the patients insert themselves into the FB.[3] While insertion by another person, sexual abuse or child abuse should be suspected.[1] Several objects can be inserted, and the most common are small hard objects (parts of toys, stones, coins or coin batteries), followed by toilet paper.[3]
In children, the reported duration of symptoms varies from 24 h to 9 years.[3,7] Delayed presentations lead to several complications, such as rectovaginal fistula or vaginal stenosis.[4] The most common presentation is vaginal bleeding or blood-stained vaginal discharge, followed by non-specific vaginal discharge, abdominal pain and foul-smelling vaginal discharge. Other rare presentations include genital itching, genital erythema and dysuria.[3] Our patients had a 5-month recurrent foul-smelling vaginal discharge until the diagnosis was made. The IVFB should be suspected in recurrent or persistent vaginal discharge in pre-menarchal girls. One of the six following elements is highly indicative of IVFB: reminding of insertion of a FB at admission, blood per vagina, blood-stained vaginal discharge, foul-smelling vaginal discharge, identification of a FB when inspecting genitalia and palpation of an IVFB during DRE.[3] Our patient had three of these elements. Most IVFB are not radiopaque. Hence, radiographs are not always helpful to identify FB. Ultrasonography is a good alternative and should be the first-line imaging in such cases. However, it depends on the ultrasonographer’s experience.[3] Some authors also reported the use of magnetic resonance imaging.[8]
Means used to remove the IVFB depend on its location: Distal ones can be easily removed with small surgical instruments, while proximal ones require vaginoscopy.[1,3] In our case, there was a granuloma around the FB, which needed to be removed before extraction of the FB with fine Kelly forceps. Some authors suggest vaginal irrigation with povidone-iodine after removal and do not initiate any additional treatment or sit baths.[3] Given the extent of vaginitis, we started antibiotics and sit baths as recommended by other authors.[9] After removing the FB, the prognosis is good if no previous complication was present,[3] as seen with the unremarkable 12-month follow-up in our patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s parent(s) has given her consent for her images and other clinical information to be reported in the journal. The patient’s parents understand that her names and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The author FTAZ is grateful to the NGO Förderverein Uni Kinshasa e.V., fUNIKIN through the excellence scholarship program BEBUC, which funds his specialisation in paediatric surgery.
REFERENCES
- 1.Smith YR, Berman DR, Quint EH. Premenarchal vaginal discharge: Findings of procedures to rule out foreign bodies. J Pediatr Adolesc Gynecol. 2002;15:227–30. doi: 10.1016/s1083-3188(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 2.Someshwar J, Lutfi R, Nield LS. The missing “Bratz” doll: A case of vaginal foreign body. Pediatr Emerg Care. 2007;23:897–8. doi: 10.1097/pec.0b013e31815c9dd2. [DOI] [PubMed] [Google Scholar]
- 3.Stricker T, Navratil F, Sennhauser FH. Vaginal foreign bodies. J Paediatr Child Health. 2004;40:205–7. doi: 10.1111/j.1440-1754.2004.00338.x. [DOI] [PubMed] [Google Scholar]
- 4.Nakib G, Calcaterra V, Pelizzo G. Longstanding presence of a vaginal foreign body (Battery): Severe stenosis in a 13-year-old girl. J Pediatr Adolesc Gynecol. 2017;30:e15–8. doi: 10.1016/j.jpag.2016.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Shiryazdi SM, Heiranizadeh N, Soltani HR. Rectorrhagia and vaginal discharge caused by a vaginal foreign body –A case report and review of literature. J Pediatr Adolesc Gynecol. 2013;26:e73–5. doi: 10.1016/j.jpag.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Dahiya P, Sangwan K, Khosla A, Seth N. Foreign body in vagina –An uncommon cause of vaginitis in children. Indian J Pediatr. 1999;66:466–7. doi: 10.1007/BF02845543. [DOI] [PubMed] [Google Scholar]
- 7.Simon DA, Berry S, Brannian J, Hansen K. Recurrent, purulent vaginal discharge associated with longstanding presence of a foreign body and vaginal stenosis. J Pediatr Adolesc Gynecol. 2003;16:361–3. doi: 10.1016/j.jpag.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Dahiya P, Agarwal U, Sangwan K, Chauhan M. Long retained intravaginal foreign body: A case report. Arch Gynecol Obstet. 2003;268:323–4. doi: 10.1007/s00404-002-0321-8. [DOI] [PubMed] [Google Scholar]
- 9.Chinawa J, Obu H, Uwaezuoke S. Foreign body in vagina: An uncommon cause of vaginitis in children. Ann Med Health Sci Res. 2013;3:102–4. doi: 10.4103/2141-9248.109463. [DOI] [PMC free article] [PubMed] [Google Scholar]


