Abstract
Splenic abscess is a life-threatening condition, which is very rare in children. There is usually an infective focus or pre-disposing factors such as immunodeficiencies towards developing splenic abscesses. Only one case of splenic abscess with brain abscesses in an adult has been reported in the English literature. We, therefore, report a case of an 11-year-old boy who was otherwise healthy, but presented with fever and weight loss for 2 months, right upper abdominal pain, vomiting, hypochondrial tenderness for 1 week and later on developed a left hemiplegia and right facioparesis 2 days before presentation. Diagnosis of splenic abscess and right intracerebral abscesses was confirmed with abdominopelvic ultrasound scan and abdominal and cranial computerised tomographic scans. He subsequently had percutaneous ultrasound-guided drainage of the splenic abscess which was not successful necessitating splenectomy with aggressive antibiotics treatment to which the patient responded with resolution of the brain abscesses and recovery of power in affected limbs. This report aimed to highlight the need for increased suspicion of splenic abscesses in children who are apparently immunocompetent and to add to the knowledge of management of this rare condition in children. We conclude that splenic abscess with intracerebral abscess is a rare but life-threatening condition which is amenable to treatment with drainage of abscess and aggressive guided antimicrobial therapy.
Keywords: Brain abscesses, children, immunocompetence, spleen
INTRODUCTION
Splenic abscess is very rare and could be life-threatening if not diagnosed and managed early. Most reports in the literature involve adults as splenic abscesses are rarer in children.[1,2,3] In autopsy-based studies, splenic abscesses are found in 0.14%–0.7% of the general population.[4] Splenic abscesses often occur as a result of haematogenous spread from a primary septic focus.[3] Other risk factors include immunosuppression and haemoglobinopathies such as sickle cell disease and trauma. The incidence of splenic abscesses is said to be on the increase recently due to immunosuppressive drugs and drug abuse.[2]
The common primary foci of infection coexisting with splenic abscesses include infective endocarditis, typhoid infections, urinary tract infections, osteomyelitis and pelvic infections. In some of the cases, however, there would not be any identifiable risk factor.[3] Quite often, the diagnosis of splenic abscess is often delayed owing to non-specific clinical features such as fever, abdominal pain vomiting and diarrhoea.[2] Delays in diagnosis and treatment contribute highly to the attendant mortality in this condition.[3]
Diagnosis is usually confirmed with the use of abdominopelvic ultrasound scans and abdominal computerised tomographic (CT) scans.[1,2,3,5] Treatment options are individualised and include conservative cares with antibiotics, percutaneous drainages and spleen-conserving surgeries such as partial splenectomy and splenectomy.[1,2,3,5,6,7]
The concomitant occurrence of splenic abscess and brain abscesses has only been reported once in the English literature and it was in an adult,[6] and none has been reported in a child. We then seek to report a case of splenic abscess with synchronous intracerebral abscess in an otherwise healthy child. We hope to highlight the need for increased index of suspicion and the challenges, techniques of treatment and outcome in this very rare scenario.
CASE REPORT
An 11-year-old boy was admitted to the children emergency room department with high-grade continuous fever and weight loss for 2 months. He also had a left upper abdominal pain for 1 week and developed sudden-onset inability to walk and weakness of both left upper and lower limbs 2 days before presentation.
There was occasional vomiting of recently ingested feeds, but no diarrhoea, constipation or cough. There was no history of antecedent trauma to the abdomen, and he was not a known sickle cell disease patient. There was no history suggestive of immunosuppression.
He was acute on chronically ill-looking, pale, anicteric, acyanosed, febrile (38.3°C), had significant tender lymphadenopathy in both axillae and inguinal regions, with a pulse of 104/min, respiratory rate of 42 cpm, blood pressure of 100/60 mmHg and weighed 22 kg.
The abdomen was tender with guarding on the left hypochondrium. The liver was enlarged by 5 cm below the costal margin. The spleen was tender and palpably enlarged 8 cm below the left costal margin. Bowel sounds were normal, and there was no ascites. He had a Glasgow consciousness scale of 15, however, had a right facioparesis. Power was zero in the left upper and lower limbs, but full[6] in the right upper and lower limbs.
He had a haemoglobin of 5.6 g/dl, total white cell count of 7900/m with neutrophilia (73%) and erythrocyte sedimentation rate (ESR) was 96 mm/h. The peripheral blood film showed severe hypochromic red blood cells and normal morphology of white blood cells and platelets. The Mantoux test was not significantly reactive, and human immunodeficiency virus assay by the enzyme-linked immunosorbent assay was non-reactive. Urinalysis showed protein (trace) bilirubin (++) and urobilinogen (+++). His liver and renal profiles were normal.
Radiographs of the chest and abdomen were also normal. Abdominal ultrasound revealed multiple hypoechoic areas of varying sizes in the spleen, largest pocket measuring about 6 ml of echo-rich content as well as hepatomegaly. The abdominal CT scan showed an enlarged spleen with multiple hypodense areas having contrast enhancement (suggestive of splenic abscesses) [Figure 1]. The cranial CT scan done same day on account of the neurological findings showed an ill-defined hypodense area in the right parietal lobe, which showed enhancing rim on post-contrast images suggestive of cerebritis [Figure 2a].
Figure 1.
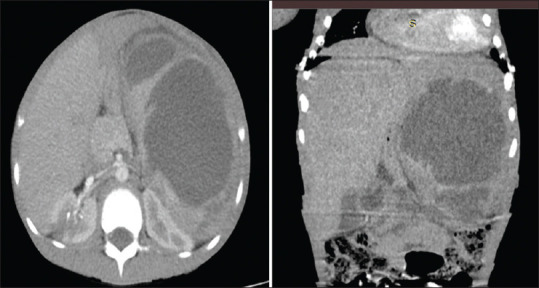
Contrast-enhanced abdominal CT scan (axial and coronal reconstructed images) at the level of the spleen showing multiloculated hypodense collection (HU: 7–29). CT: Computerised tomography
Figure 2.
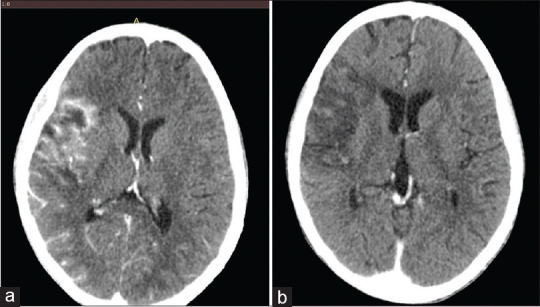
(a) Contrast-enhanced axial CT scans of the brain showing Irregular hypodense area in the right frontoparietal lobe with an enhancing rim. (b) Which resolved with time (3-week interval). CT: Computerised tomography
The child was commenced on intravenous ceftriaxone (150 mg/kg/day) and metronidazole (30 mg/kg/day) in divided doses. He was transfused serially with two units of blood to build the haematocrit to 11 g/dl. Ultrasound-guided percutaneous aspiration of the splenic abscess was done and yielded 150 ml of thick, foul-smelling pus which yielded a moderate growth of Escherichia coli on microscopy sensitive to meropenem. His antibiotic was converted to meropenem; however, the patient had worsening clinical condition, and a repeat abdominal scan showed an increase in the volume of the abscess collection in the spleen. He underwent exploratory laparotomy at which splenectomy was performed. Intraoperative findings included multiple splenic abscesses and adhesions, involving the spleen, stomach and greater omentum. In the post-operative period, the patient was continued on the intravenous meropenem of 100 mg/kg/day in divided doses for 2 weeks. Repeat cranial CT after wards also showed resolving cerebritis [Figure 2b]. He had physiotherapy with recovery of power in the left upper and lower limbs to 4 and now ambulates. He was discharged in a good condition 2 weeks after surgery and has been on follow-up for 1 year now.
DISCUSSION
Abscess rarely occurs in the spleen due to its efficient reticuloendothelial system phagocytic activity. It is also uncommon in the paediatric age group and life-threatening if untreated. Tung et al.[1] reported a median age of 59.9 years for splenic abscesses in their series. Most cases reported in the paediatric age group occur in pre-pubertal children, Rattan et al.[3] reported three cases of splenic abscesses in three children aged 9–12 years. It has also been found to be more common in males than females.[3,5] The index patient is a male who was aged 11 years.
Most cases of splenic abscesses arise as a metastasis from a primary infective focus or have such risk factors as immunodeficiency and haematological disorders such as sickle cell anaemia, trauma as well as splenic infarction.[3,5] This case is peculiar in that there was no primary infective focus identified, and the patient was otherwise healthy without any clinical or laboratory indices of immunodeficiency or preceding trauma before the illness. With symptoms dating for 2 months, it is possible there might have been a primary infective focus which probably would have been treated or resolved before presentation to us. The involvement of the spleen and the brain suggests an overwhelming infection perhaps due to delays in presentation for appropriate treatment.
The clinical presentation for splenic abscesses may be vague and non-specific, but fever and abdominal pain with left hypochondrial tenderness are usually present.[1,2,3,8] Other additional symptoms include nausea, vomiting and weight loss.[1,3,5,7] The index patient had all these symptoms; however, these are non-specific and are the reason why there are delays in diagnosis of splenic abscesses.[9,10] The additional symptoms of weakness of both left upper and lower limbs were pointers to the intracranial involvement. Examination findings in this patient included splenomegaly, left upper quadrant tenderness and diffuse abdominal tenderness, which are similar to what has been reported in other studies, with splenomegaly almost always being present.[2,3,5,9] Additional findings would depend on associated comorbidities; the index case had a right facioparesis and left hemiplegia confirming a likely right intracranial space-occupying lesion. Maliyil et al. had reported a case of splenic abscess with multiple brain abscesses in a 21-year-old man who presented with fever, left upper quadrant pain and seizures.[6] The index case appears to be the second in the literatures where there is concomitant splenic and intracerebral abscess in an otherwise healthy patient and the first to be reported in a child.
Leucocytosis, neutrophilia, anaemia and raised ESR are common haematological findings in abscesses; splenic and intracerebral inclusive.[1,2,3] The index patient had normal white cell count with neutrophilia, anaemia and raised ESR. It is possible that the protracted illness and treatments before presentation might explain the normal white cell count in this patient.
The diagnostic investigation of choice for splenic abscess is abdominal ultrasonography and then characterised better with CT scans.[1,2,3,5,7,8] Ultrasonography reveals hypoechoic or anechoic lesions with hyperechoic debris in the spleen, which may be focal or multiple and varying in size with irregular margins. Our patient had multiple varying size pockets of abscesses as seen on ultrasonography, and the abdominal and cranial CT scans further elucidated the splenic and cerebral lesions, respectively [Figures 1 and 2]. Both imaging modalities remain gold standards in the diagnosis of splenic abscesses.[3]
Isolation of the exact causative organism is a key to guide antimicrobial therapy. The most common organisms implicated in splenic abscess are Gram-positive cocci such as Streptococci viridans and Streptococci intermedius, others are Gram-negative Enteric cocci such as E. coli and Klebsiella spp. and rarer organisms such as Salmonella spp. and Citrobacter freundis.[5,6,10] Gram-negative cocci, E. coli, were isolated in this particular patient and were sensitive to meropenem; this guided the antibiotic switch.
Treatment of splenic abscesses varies and could be conservative with the use of antibiotics alone, percutaneous drainage and antimicrobial therapy or with open operative approach with spleen-conserving surgeries or outright splenectomy.[1,2,3,4,5,6,7,8,9,10] These options are tailored to individual patients; however, some authors have suggested splenectomy with antimicrobial therapy to be the main stay of treatment with the best outcome.[1,2,10] Splenectomy is mostly indicated in settings of: multiple abscesses, multiloculated abscesses, debris-contained abscess, poorly defined abscess on CT or poor route of percutaneous drainage and in failed percutaneous drainage procedures.[8] The index patient first had ultrasound-guided drainage which failed and then subsequently had splenectomy. The intracerebral lesion responded to intensive antibiotic treatment according to sensitivity [Figure 2b]. Maliyil et al. employed percutaneous drainage of the splenic abscess and stereotactic drainage of the intracerebral abscesses in their own case.[6] We recommend that percutaneous drainage of the abscesses and antimicrobial therapy be deployed first with early recourse to open operative procedures if these fail.
CONCLUSION
To the best of our knowledge, this is the first reported case of splenic abscess coexisting with brain abscess in an immunocompetent child. Suspicion of splenic abscess should be raised in children presenting with left hypochondrial pain and pyrexia of uncertain origin. Efforts should be made to screen for other synchronous abscesses in other organ systems, particularly the brain, when there are associated lateralising signs. Early and appropriate treatment of infections from any focus could minimise the occurrence of splenic abscesses and other overwhelming infections, and we recommend individualised treatment modality with close surveillance to escalate treatments in splenic abscesses.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tung CC, Chen FC, Lo CJ. Splenic abscess: An easily overlooked disease? Am Surg. 2006;72:322–5. [PubMed] [Google Scholar]
- 2.Alonso Cohen MA, Galera MJ, Ruiz M, Puig la Calle J, Jr, Ruis X, Artigas V, et al. Splenic abscess. World J Surg. 1990;14:513–6. doi: 10.1007/BF01658678. [DOI] [PubMed] [Google Scholar]
- 3.Rattan KN, Kadian YS, Saroha V, Jindal N. Splenic abscess in children: A report of three patients. Afr J Paediatr Surg. 2009;6:106–9. doi: 10.4103/0189-6725.54774. [DOI] [PubMed] [Google Scholar]
- 4.Chun CH, Raff MJ, Contreras L, Varghese R, Waterman N, Daffner R, et al. Splenic abscess. Medicine (Baltimore) 1980;59:50–65. doi: 10.1097/00005792-198001000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Green BT. Splenic abscess: Report of six cases and review of the literature. Am Surg. 2001;67:80–5. [PubMed] [Google Scholar]
- 6.Maliyil J, Caire W, Nair R, Bridges D. Splenic abscess and multiple brain abscesses caused by Streptococcus intermedius in a young healthy man. Proc (Bayl Univ Med Cent) 2011;24:195–9. doi: 10.1080/08998280.2011.11928714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abiola AJ, Hassan S, Ameh E. Primary splenic abscess in children. J Pediatr Surg Case Rep. 2020;60:101552. [Google Scholar]
- 8.Bonares MJ, Ying T, Patel Y. Salmonella Thompson splenic abscess in a healthy female. BMJ Case Rep 2017. 2017 doi: 10.1136/bcr-2016-218595. r-218595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faruque AV, Qazi SH, Arshad M, Anwar N. Isolated splenic abscess in children, role of splenic preservation. Pediatr Surg Int. 2013;29:787–90. doi: 10.1007/s00383-013-3336-2. [DOI] [PubMed] [Google Scholar]
- 10.Lee WS, Choi ST, Kim KK. Splenic abscess: A single institution study and review of the literature. Yonsei Med J. 2011;52:288–92. doi: 10.3349/ymj.2011.52.2.288. [DOI] [PMC free article] [PubMed] [Google Scholar]


