Abstract
Tailgut cysts are rare congenital abnormalities that develop due to failure of embryologic tailgut to involute. This generally manifests as a presacral, retrorectal and multicystic mass. It has a high propensity in female patients including paediatric age group. The clinical presentation varies depending on the age of patient, location and size of the cyst. The symptoms are mostly due to mass effects and rarely complications such as malignancy. Being a rare entity, it is generally misdiagnosed. Differential diagnosis mostly includes rectal duplication cyst, sacrococcygeal teratoma and anterior meningocele. Radiological imaging such as computed tomography scan and magnetic resonance imaging is useful in the diagnosis. The treatment of choice is complete excision to prevent recurrence, infection and malignant degeneration. We have reviewed previous literature and given our valuable information regarding the same.
Keywords: Perineal lesion, presacral tumour, retrorectal tumour, tailgut cyst
INTRODUCTION
Tailgut cysts are rare congenital malformations that are embryologic remnants of the post-natal component of the hindgut.[1] The data available for tailgut cysts demonstrate a 5:1 predominance of these lesions in females. Tailgut cysts can present at any age. The majority of cysts remains asymptomatic, often missed on digital rectal exams. Most of the cases are seen in the 30–60 years of age group. Mass effect can lead to such symptoms as constipation, tenesmus, dysphasia, and/or polyuria; and lesion infection may manifest as a perianal fistula or a pelvic abscess.[1,2,3] Based on recent studies, the overall rate of malignant transformation of tailgut cysts is estimated to be as high as 26%.[4]
As the embryo folds during the 4th week of gestation, the cloacal membrane progresses ventrally and encloses a portion of the future gut that is distal to the eventual hindgut-a region known as the ‘tailgut’. Typically,[1] the tailgut involutes around the 6th week of gestation; however, when this process fails, a tailgut cyst remains.[1] Tailgut cysts arise in areas with complex anatomy and embryology. The retrorectal or presacral space is bounded anteriorly by the rectum, posteriorly by the sacrum, superiorly by the peritoneal reflection, inferiorly by the pelvic diaphragm muscles (levator ani and coccygeus), and laterally by the ureters and iliac arteries and veins.[2]
Tailgut cysts are congenital, retrorectal and multicystic lesions also known as postanal gut cysts. Only 20 cases have been reported in English literature in the paediatric age group.
CASE REPORT
A 4-year-old male patient presented to the paediatric surgery clinic with the complaint of vague lower abdominal pain for the past 4–5 months, which was non-radiating, increased after food intake and mild-to-moderate in intensity. It was associated with abdominal fullness after meals. Not associated with nausea, vomiting, diarrhoea, constipation, blood in urine/stool, pain while defecating, urinary complaints and fever. The patient had a history of left-sided inguinal herniotomy at the age of 7 months. The patient had a rotavirus infection at the age of 3 years (at that time patient had diarrhoea and vomiting for which he was admitted to the hospital for 8 days).
There was no family history of malignancy and the patient’s drug history was insignificant.
On examination, the abdomen was soft and non-tender.
Digital rectal examination demonstrated the presence of approximately 6 cm × 5 cm soft, cystic, non-tender, non-mobile swelling palpated at 6 o’clock position with no active bleeding or pus discharge at that time.
The examining finger was able to reach above the mass and feel the coccyx. Perianal examination revealed a normal resting tone and no perineal descent or prolapse furthermore, no skin tag, fissure, fistula or haemorrhoids were present. There was no gross perianal pathology. Apart from this, the rest of the physical exam was unremarkable. Laboratory studies were within normal limits, and there was no radiographic evidence of extra-pelvic disease.
The serum alpha-fetoprotein and beta-human chorionic gonadotropin were within normal limits.
Ultrasonography (USG) abdomen suggested a 41 mm × 33 mm sized well-defined cystic lesion with internal echoes and septations noted in the right mesorectal region adjacent to the rectum, with no evidence of internal vascularity.
Contrast-enhanced computed tomography (CT) scan of the abdomen showed a benign septate cystic lesion measuring 59 mm × 50 mm × 42 mm seen in the presacral region with retrorectal concavity and causing compression over the rectum [Figure 1a and b].
Figure 1.
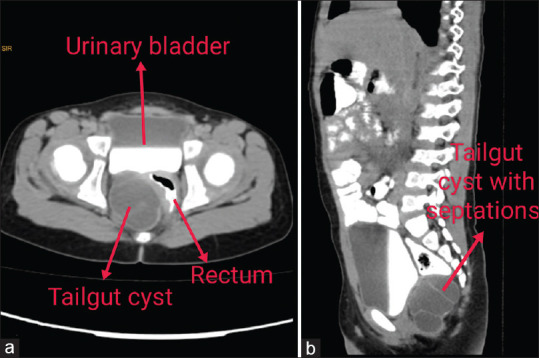
(a and b) Contrast computed tomography scan of abdomen and pelvis [red arrows indicate related structure in picture]
The patient underwent complete resection of the mass through a posterior (Kraske) approach. After positioning the patient, the cyst was rectally palpated and was found to be deviating towards the right side. Hence, an incision was made extending 3 cm from the coccyx superiorly. Sharp dissection was used to carry the incision down directly over the marked plane which extended bilaterally over the gluteal region. The subcutaneous tissue and fatty layer were divided bilaterally and the cyst was exposed after cutting the few gluteal muscle fibres. The mass had multiple tense and cystic loculations, one of which was inadvertently entered, releasing a thick, non-malodorous and purulent fluid consistent with sterile pus. The lesion was resected en bloc with its fibrous attachments to the distal coccyx but the coccyx was spared. The cyst was dissected taking all precautions not to enter the rectum. The levator ani was closed in the midline and gluteal muscle fibres were sutured to the respective position. A corrugated drain was brought out laterally from a separate incision. The remaining layers of the incision were re-approximated and closed. The patient tolerated the operation without any complications, and her post-operative course was uneventful. The drain was removed after 5 days. The patient returned to the clinic 2 weeks later for the removal of skin sutures and achieved a complete functional recovery soon thereafter.
Histopathology
Sections reveal cyst wall lined by stratified squamous epithelium, pseudostratified ciliated columnar and transitional lining. Subepithelial tissue shows a bundle of smooth muscle in the cyst wall. Many mixed inflammatory cells chiefly lymphocytes, polymorph and foamy macrophages are also seen [Figure 2].
Figure 2.
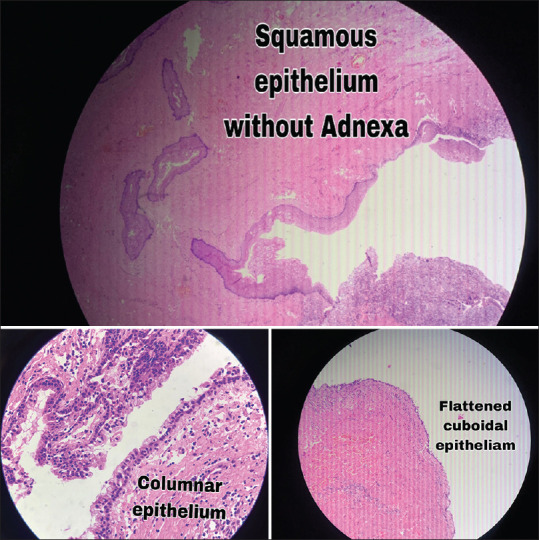
Histopathology slide
DISCUSSION
Tailgut cysts are typically located in presacral space and extend below the pelvic floor anterior to the coccyx and are therefore retroanal as well as retrorectal. The largest published series of 53 cases collected over four decades from the US Armed Forces Institute of Pathology noted that women outnumbered men by 3:1.[5] Tailgut cysts are more common in young and middle aged but quite rare in the paediatric group and hence make this review important.
Fewer than 100 adult cases have been reported in literature worldwide and only 18 cases in English literature in the paediatric group. Tailgut cysts can present in a variety of ways. Almost 50% of adult cases are asymptomatic and discovered incidentally.[5] The remainder present with symptoms of a pelvic mass (e.g. constipation, pelvic pain and urinary symptoms) or from cyst complications (recurrent perianal or retrorectal abscesses, cutaneous perianal sinuses or fistulae, rectal bleeding or malignant degeneration).[6]
Finally, malignant transformation into neuroendocrine tumours, adenocarcinoma and squamous cell carcinoma can occur; thus, accurate diagnosis and treatment are critical.[7]
In children, the cyst most commonly presents as an incidental finding on pre- or post-natal ultrasound scans or as a gluteal or perianal mass [Table 1]. There may be a postanal or sacral dimple,[8] as noted in some affected adults.[6] The cases till now had presented with pelvic or abdominal pain, gluteal cystic mass, renal symptoms, rectal prolapse, constipation, imperforate anus or stenosis. The tailgut cyst has been mostly incidentally diagnosed on USG.
Table 1.
Reports of tailgut cysts in children
| Reference | Age | Sex | Largest dimension (s) (cm) | Presenting features |
|---|---|---|---|---|
| Raven | 2 months | Female | 5 | Intestinal obstruction |
| Hjermstad and Helwig | Neonate | Male | – | Prolapsing rectal lesion |
| Hjermstad and Helwig | Neonate | Female | – | |
| Rafindadi et al. | Neonate | Male | 25×20 | Cystic gluteal mass |
| Oh et al. | Neonate | Female | 9 | Prenatal US at 36 weeks gestation showed a sacrococcygeal mass |
| Al-Khuzaie et al. | Neonate | Female | 10×8 | Cystic gluteal mass |
| Sung et al. | 12 years | Male | 4×3 | Recurrent abdominal pain and vomiting |
| Antao et al. | 14 weeks | Male | 1.3×0.7 | Incidental finding on US scan in a neonate with anal stenosis |
| Podberesky et al. | 2 years | Female | 2.6×1.2 | Incidental finding on MRI scan for sacral vascular malformation |
| Jang et al. | 14 years | Male | 5×3 | Acute abdominal pain and dysuria |
| Galluzzo et al. | 12 years | Female | 12×11 | Lumbar pain |
| Kim and Park | Neonate | Female | 2.3×1.2 | Subcutaneous mobile postanal mass |
| Nakagawa et al. | Neonate | Female | 10.2×9.3 | Prenatal US at 23 weeks’ gestation showed a presacral cyst |
| Peter et al. | 19 months | Male | – | Large perianal swelling since birth |
| Garcia-Palacios et al. | 8 years | Female | – | Postanal retrorectal mass and constipation |
| Chung et al. | Neonate | Female | 5×4 | Prenatal US at 25 week’s gestation showed a presacral cyst |
| Hansen and Qvist | 4.5 years | Female | Not stated | Rectal prolapse (with a presacral mass) |
| Raisolsadat et al. | Neonate | Female | 4×3 | At posterior sagittal anorectoplasty for imperforate anus |
| Nadeem Haidar | 14 months | Female | 6.3×4.4 | Abdominal distension, urinary retention, renal failure |
| Nadeem Haidar | 7 months | Male | 5.7×4.3 | Cystic gluteal mass |
| Current case | 4 years | Male | 5.9×5 | Vague lower abdominal pain |
US: Ultrasound, MRI: Magnetic resonance imaging
In our case, the child had diarrhoea and was incidentally diagnosed with a cystic lesion in the presacral space but conservative management was decided initially in the peripheral hospital and now the child after a few years presented in our outpatient department with recurrent lower abdominal pain and on USG the size of cyst was found to be increased which was confirmed by CT scan.
Imaging, namely magnetic resonance imaging (MRI) and CT scans, is the principal method by which retrorectal masses can be diagnosed.[9] Other imaging modalities can be useful but are not diagnostic.[9] MRI is the optimum imaging technique. Cysts typically show a variable signal intensity on T1-weighted images (which depends on the protein content of the fluid) and are hyperintense on T2-weighted images.[8,10] The presence of a solid component in the lesion rules out the tailgut cyst.
Retrorectal cysts have various and different pathology. The cystic sacrococcygeal teratoma consists of all three germ layers and has solid components. Dermoid cysts are usually unilocular and lined by stratified squamous epithelium with dermal appendages. An anterior sacral meningocele communicates with the spinal subarachnoid space through a bony defect in the sacrum. The anorectal duplication cyst is unilocular and has a common wall with the rectum. The rare malignant tumour chordomas contain solid components.
In studies of the tailgut, it has been found that a lining of two to four layers of cuboidal cells is present with no definite muscular outer layer. A well-defined muscular wall with a myenteric plexus should be absent in a tailgut cyst to differentiate from a duplication cyst.[3] The pathological changes of tailgut cysts are distinctive. The lesions are usually multilocular and multicystic. Although a variety of epithelial types almost always line the cysts, the presence of some glandular or transitional epithelium is required to exclude epidermoid and dermoid cysts.[5]
Histopathology sections in our case revealed a cyst wall lined by stratified squamous epithelium, pseudostratified ciliated columnar and transitional lining. Subepithelial tissue shows a bundle of smooth muscle in the cyst wall. Many mixed inflammatory cells chiefly lymphocytes, polymorphs and foamy macrophages are also seen.
Tailgut cysts are considered to be remnants of the embryonic tailgut that normally regresses completely during normal development. In human embryos, the tailgut becomes visible at about 29 days (Carnegie stage 11), is fully developed by day 35 and has largely regressed by day 44 (Carnegie stage 18).[11] It is lined by stratified columnar epithelium. An alternative and less likely source of tailgut cysts is the neurenteric canal,[12] which is a transient communication between the yolk sac and the amniotic cavity in the embryo before the definitive notochord is formed.[5]
Surgical resection is the treatment of choice for both asymptomatic lesions (due to risks including infection, rupture, fistula formation and malignant transformation) and symptomatic tailgut cysts.[13,14,15] Approaches to tailgut cyst depend on the level of location of the lesion above or below the S3 level (may vary widely, from laparoscopic to transabdominal to transsacral to transanal).
Retrorectal masses lying entirely below S3 can safely be accessed through a posterior, or Kraske, approach, while lesions lying above S3 can be excised through an anterior, or abdominal approach.[13] When lesions lie both above and below the level of S3, an integrated abdominosacral approach may be required.[13] During the posterior approach, a coccygectomy may provide better surgical exposure.[13] If the tailgut cyst is not resected entirely, there is a possibility for recurrence.[13]
Amongst the various treatment options, complete resection with clear margins is the most effective one and has the least incidence of recurrence and better patient outcomes.[13,16] Following excision, an annual digital rectal examination is recommended; furthermore, a CT scan is recommended in post-operative years 1 and 5.[13]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Haydar M, Griepentrog K. Tailgut cyst: A case report and literature review. Int J Surg Case Rep. 2015;10:166–8. doi: 10.1016/j.ijscr.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krivokapic Z, Dimitrijevic I, Barisic G, Markovic V, Krstic M. Adenosquamous carcinoma arising within a retrorectal tailgut cyst: Report of a case. World J Gastroenterol. 2005;11:6225–7. doi: 10.3748/wjg.v11.i39.6225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakr A, Kim HS, Han YD, Cho MS, Hur H, Min BS, et al. Single-center experience of 24 cases of tailgut cyst. Ann Coloproctol. 2019;35:268–74. doi: 10.3393/ac.2018.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicoll K, Bartrop C, Walsh S, Foster R, Duncan G, Payne C, et al. Malignant transformation of tailgut cysts is significantly higher than previously reported: Systematic review of cases in the literature. Colorectal Dis. 2019;21:869–78. doi: 10.1111/codi.14628. [DOI] [PubMed] [Google Scholar]
- 5.Hjermstad BM, Helwig EB. Tailgut cysts. Report of 53 cases. Am J Clin Pathol. 1988;89:139–47. doi: 10.1093/ajcp/89.2.139. [DOI] [PubMed] [Google Scholar]
- 6.Killingsworth C, Gadacz TR. Tailgut cyst (retrorectal cystic hamartoma): Report of a case and review of the literature. Am Surg. 2005;71:666–73. [PubMed] [Google Scholar]
- 7.Liang F, Li J, Yu K, Zhang K, Liu T, Li J. Tailgut cysts with malignant transformation: Features, diagnosis, and treatment. Med Sci Monit. 2020;26:e919803. doi: 10.12659/MSM.919803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Podberesky DJ, Falcone RA, Emery KH, Care MM, Anton CG, Miles L, et al. Tailgut cyst in a child. Pediatr Radiol. 2005;35:194–7. doi: 10.1007/s00247-004-1302-9. [DOI] [PubMed] [Google Scholar]
- 9.Shetty AS, Loch R, Yoo N, Mellnick V, Fowler K, Narra V. Imaging of tailgut cysts. Abdom Imaging. 2015;40:2783–95. doi: 10.1007/s00261-015-0463-3. [DOI] [PubMed] [Google Scholar]
- 10.Kim KR, Park WK. Radiologic features of a tailgut cyst in a neonate: A case report. J Korean Radiol Soc. 2008;58:177–80. [Google Scholar]
- 11.Hashimoto R. Development of the human tail bud and splanchnic mesenchyme. Congenit Anom (Kyoto) 2013;53:27–33. doi: 10.1111/j.1741-4520.2012.00387.x. [DOI] [PubMed] [Google Scholar]
- 12.Antao B, Lee AC, Gannon C, Arthur R, Sugarman ID. Tailgut cyst in a neonate with anal stenosis. Eur J Pediatr Surg. 2004;14:212–4. doi: 10.1055/s-2004-815872. [DOI] [PubMed] [Google Scholar]
- 13.Raven RW. Sacrococcygeal cysts and tumors. Br J Surg. 1935;23:337–61. [Google Scholar]
- 14.Oh JT, Son SW, Kim MJ, Kim L, Kim H, Hwang EH. Tailgut cyst in a neonate. J Pediatr Surg. 2000;35:1833–5. doi: 10.1053/jpsu.2000.19281. [DOI] [PubMed] [Google Scholar]
- 15.Sung MT, Ko SF, Niu CK, Hsieh CS, Huang HY. Perirenal tailgut cyst (cystic hamartoma) J Pediatr Surg. 2003;38:1404–6. doi: 10.1016/s0022-3468(03)00408-1. [DOI] [PubMed] [Google Scholar]
- 16.Jang SH, Jang KS, Song YS, Min KW, Han HX, Lee KG, et al. Unusual prerectal location of a tailgut cyst: A case report. World J Gastroenterol. 2006;12:5081–3. doi: 10.3748/wjg.v12.i31.5081. [DOI] [PMC free article] [PubMed] [Google Scholar]


