Abstract
Objective:
An expert panel made recommendations to optimize surgical education and training based on the effects of contemporary challenges.
Background:
The inaugural Blue Ribbon Committee (BRC I) proposed sweeping recommendations for surgical education and training in 2004. In light of those findings, a second BRC (BRC II) was convened to make recommendations to optimize surgical training considering the current landscape in medical education.
Methods:
BRC II was a panel of 67 experts selected on the basis of experience and leadership in surgical education and training. It was organized into subcommittees which met virtually over the course of a year. They developed recommendations, along with the Steering Committee, based on areas of focus and then presented them to the entire BRC II. The Delphi method was chosen to obtain consensus, defined as ≥80% agreement among the panel. Cronbach α was computed to assess the internal consistency of 3 Delphi rounds.
Results:
Of the 50 recommendations, 31 obtained consensus in the following aspects of surgical training (# of consensus recommendation/# of proposed): Workforce (1/5); Medical Student Education (3/8); Work Life Integration (4/6); Resident Education (5/7); Goals, Structure, and Financing of Training (5/8); Education Support and Faculty Development (5/6); Research Training (7/9); and Educational Technology and Assessment (1/1). The internal consistency was good in Rounds 1 and 2 and acceptable in Round 3.
Conclusions:
BRC II used the Delphi approach to identify and recommend 31 priorities for surgical education in 2024. We advise establishing a multidisciplinary surgical educational group to oversee, monitor, and facilitate implementation of these recommendations.
Keywords: educational technology and assessment, faculty development and educational support, medical student education, research training, residency education, structure and financing of surgical training, surgical education, surgical training, surgical workforce, work life integration
In June 2002, inspired by the Presidential Address of Dr Haile Debas at the 122nd meeting of the American Surgical Association (ASA), the ASA and the ASA Council in partnership with the American College of Surgeons (ACS), the American Board of Surgery (ABS), and the Resident Review Committee for Surgery (RRC-S) established a Blue Ribbon Committee on Surgical Education (BRC I). 1 The committee was charged with “examining the multitude of forces impacting health care and making recommendations regarding the changes needed in surgical education to enhance the training of surgeons to serve all the surgical needs of the nation, and to keep training and research in surgery at the cutting edge in the 21st Century.” 2 They published 34 recommendations in 2005 which included the following key elements: restructure general surgery residencies to include a modular format with continued specialization through fellowships and a focus on creating a training environment that reduces fatigue and promotes balanced lifestyles; study the impact of the 80-hour work week; broader application of simulation to teach and verify basic surgical skills; develop an optional research module with possibility for an advanced degree; and develop a new curricula for training. 2 A decade later a panel at the 132nd ASA meeting identified persistent issues in general surgery training and recommended the following actions: the need to define and continually update the curriculum, broader use of simulation, more structured teaching and assessment and earlier specialty focus during residency training. 3 Most recently on September 19, 2022, the ABS convened a summit on entrustable professional activities (EPAs) in surgery and competency-based medical education (CBME). At that meeting there was a discussion of the current status of surgical training in the United States. The attendees agreed that it was time for an updated and comprehensive look at surgical education and agreed that the ASA and the ACS would be the appropriate organizations to lead this effort. After consideration the ACS, ASA, and ABS agreed to sponsor the Blue Ribbon Committee II (BRC II) which first met in February 2023.
The charge to BRC II was to consider contemporary issues that affect surgical education and make recommendations to enhance training in general surgery and its related specialties today and in the future. Although the focus is on general surgery and its related specialties, advances in other surgical disciplines informed the conversation of the committee. Thus, we are hopeful that the observations and recommendations will apply to the training of surgeons across all surgical disciplines. It is important for all surgeons to realize that as a profession we are more effective when we work together.
BACKGROUND
Since the BRC I published its findings in 2005, the medical landscape has changed considerably. 2 Technical advances have transformed surgical practice, especially in abdominal and vascular surgery. Discoveries in molecular biology, genetics and immunology have changed our approach to cancer. New ways to organize surgical care have arisen as seen with acute care surgery and continued specialization. The delivery system has gradually merged, an electronic health care record has been developed and implemented, and the majority of surgeons are employed by hospitals, large multidisciplinary practices and even venture capital firms. A new generation of surgeons has assumed leadership in the profession with their own sensibilities about their role in the profession and its future. The COVID-19 pandemic put the spotlight on the tenuous balance of the competing priorities of patient care and surgical education exposing the dilemma posed by these dual professional obligations. 4
Some of the recommendations of BRC I have gained traction and been implemented. There is a well-organized national general surgery curriculum developed by the Surgical Council on Resident Education (SCORE) 5 and numerous educational offerings by national organizations representing all surgical specialties. There has been a greater emphasis on preparing faculty to teach and there are opportunities for professional advancement as an educator. The number of graduating residents has grown, although not at a pace to meet the country’s needs either by total number or geographic distribution. The number of women in the profession has increased considerably although racial diversity remains unchanged. The ABS and the RRC-S have provided increased flexibility in the training structure and a competency-based system is evolving.6,7
Importantly, surgical training is quite different than that of primary care or other medical specialties, due to the necessary portfolio of diagnostic and treatment options for surgical disorders as well as the development of surgical skills. Although we have adapted to an 80-hour work week, it has not been without major programmatic adjustments and the need for more training to develop the ability to provide high-quality surgical care.
Herein, we present the findings of this committee and its recommendations. Importantly, future manuscripts from each of the subcommittees will provide greater details of the issues and their recommendations.
METHODS
We used the key issues of focus for BRC I as a blueprint for BRC II. 2 To guide the process a Steering Committee was formed (Supplemental Digital Content 1, Table 1, http://links.lww.com/SLA/F128). This group purposely chose and invited a diverse group with experience in surgical education and training to join BRC II.
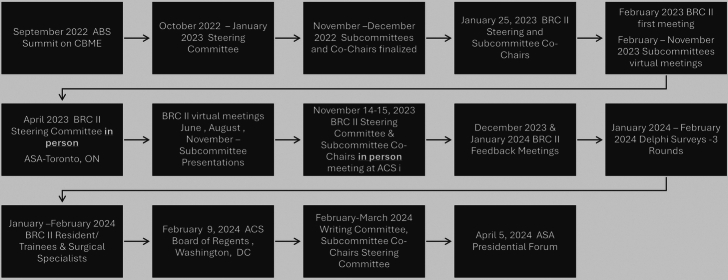
Eight working subcommittees were established (Table 1). We invited the authors of the BRC I paper to take part in one of the subcommittees to assess the impact of its recommendations and future opportunities. The above groups joined the Steering Committee to form BRC II, which made a total of 67 members. BRC II designed an orderly workflow (Fig. 1). The subcommittees formed expert panels in specified areas of focus and developed initial recommendations. The subcommittees were instructed to submit a report on their area of focus. The number of expected recommendations was not specified. In December 2023 and January 2024, BRC II held 2 meetings to further discuss each recommendation by the subcommittees. The Steering Committee processed and synthesized these, including feedback from the subcommittee co-chairs and other committee members. For more feedback, we presented the findings and recommendations of the subcommittees in separate virtual meetings to a sample of diverse general surgical trainees (January 2024) and education leaders representing all of the surgical disciplines (February 2024) (Supplemental Digital Content 1, Table 2, http://links.lww.com/SLA/F128). All subcommittees, including the BRC I members, were invited and participated in meetings of the BRC II and discussion of proposed recommendations as well as the Delphi process as outlined below.
TABLE 1.
Blue Ribbon Committee II Focus Areas and Subcommittees
| Blue Ribbon Committee I Review: Findings and Impact |
| Medical Surgical Workforce |
| Medical Student Education |
| Work Life Integration, Wellness, and Resilience |
| Residency Education in Surgery |
| Goals, Structure, and Financing of Surgical Training |
| Faculty Development and Educational Support |
| Research Training |
| Educational Technology and Assessment |
FIGURE 1.
The process used for the work of Blue Ribbon Committee II. The goal from the beginning was to be as inclusive and transparent as possible with frequent virtual meetings of the subcommittees and the full panel. An in-person meeting was held on November 14 and 15, 2023 and allowed for discussion of all recommendations proposed by the subcommittees and the steering committee. Following this there were 2 additional virtual meeting designed to allow in depth discussion of the proposed recommendations before the Delphi analysis.
We chose the Delphi method to obtain consensus of the BRC II recommendations. The process followed previously published guidelines. 8 We used Research Electronic Data Capture (REDCap) to create an anonymous survey that included all subcommittee recommendations and several suggested by the Steering Committee. We sent 3 rounds of electronic surveys for Delphi assessment with frequent email reminders (Fig. 2).
FIGURE 2.
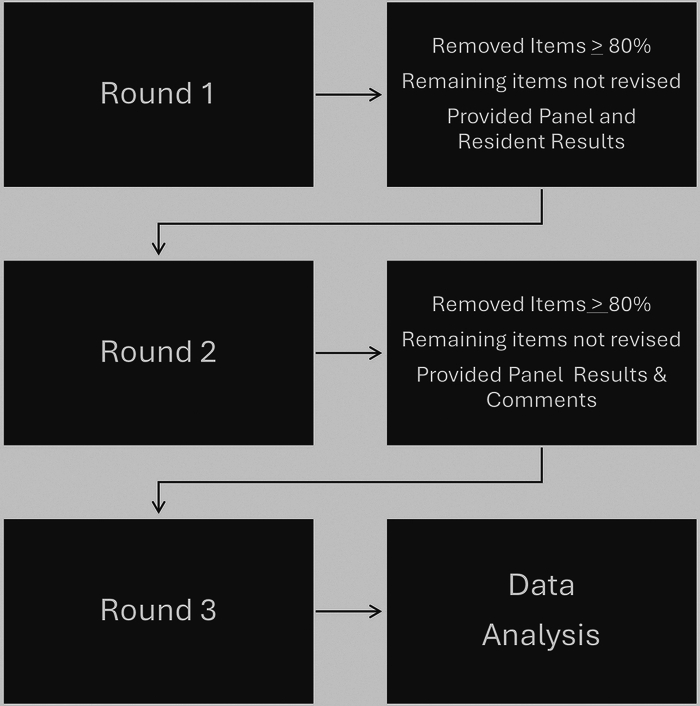
The Delphi method was chosen to obtain consensus defined as >80% agreement among panel members. Three rounds of voting occurred with frequent email reminders. After each round those recommendations reaching consensus were removed from the subsequent survey rounds, the statements were not modified,and additional information provided as indicated in the figure.
We emailed the first Delphi round survey as a link to all BRC II members (N=63, excluding the 2 BRC II Co-Chairs and the 2 Delphi Consultants) that made up the expert panel for this process. Each panelist was asked to assess each of the 50 proposed recommendations for the goal of advancing and optimizing surgical training. They were asked to answer, “Should the following subcommittee recommendation be included in the final BRC II recommendations and paper based on its anticipated impact and feasibility” using a rating scale of Yes, Don’t Know, and No. Panelists could also provide free text comments on the recommendations. We computed the percentage of “yes” choice and the Cronbach α for each individual recommendation to evaluate internal consistency (N=50). 9 The following definitions of Cronbach α were applied: where α is internal consistency: >0.9 excellent; >0.8 good; >0.7 acceptable; >0.6 questionable; >0.5 poor; and ≤0.5 unacceptable. The Consensus Rating (CR) was defined based on a proposed recommendation reaching a Cronbach α >0.70 and the percentage of “yes” choice wherein CR1; 80% to 100%, CR2; 60% to 79%, CR3; 21% to 59%, and CR4; 0% to 20%. Proposed and unmodified recommendations that did not reach CR1 (≥80%) a first round were included in the next Delphi round. In Round 2, panelists were also provided with the panel CR and the resident focus group CR from the initial survey. In Round 3, panelists were provided with the panel CR from Round 2 remaining items and the panelist comments from Round 1.
In addition, during the first Delphi round, each panelist was asked to evaluate the impact and implementation difficulty of each proposed recommendation using a 5-point Likert scale (5=major impact/very difficult, 4=high impact/difficult, 3=moderate impact/neutral difficulty, 2=low impact/easy implementation, 1=no impact/very easy implementation). Mean score and SD were computed for impact and implementation difficulty for each recommendation.
We used JMP software (JMP Pro 16; SAS Institute) to perform all statistical analysis.
As part of the process, we also engaged the voice of surgical trainees to assess the 50 proposed recommendations per the goal of advancing and optimizing surgical training. To obtain their perspectives, we sent the first round survey link to a group of residents and fellows (n=20) who were purposely chosen considering sex, race, ethnicity, region, and specialty by the BRC II subcommittee co-chairs or steering committee members. The survey sent to them did not request their evaluation of impact or implementation difficulty of the proposed recommendations. This group of trainees was not part of the expert panel, but as mentioned above, they formed an important focus group that met with the BRC II Committee in January 2024. We did not report the trainee qualitative feedback analysis in this manuscript.
This report is an overview of the recommendations. It is hoped that future manuscripts prepared by the subcommittees and surgical trainee focus group will more fully describe specific recommendations and considerations. We present priority recommendations that reached at least 80% consensus and the panel’s assessment of impact and implementation difficulty of each. Table 2 shows recommendations that did not reach consensus.
TABLE 2.
BRC II Recommendations That Did Not Meet 80% Consensus Threshold
| Recommendation | Delphi analysis results Consensus Rating (CR) 1-4; % Agreement; Impact (mean/SD); Difficulty (mean/SD) |
|---|---|
| Surgical Medical Workforce | |
| Streamline pathways for internationally trained surgeons to enter the surgical workforce while maintaining high standards for quality care | CR2; 75%; Impact 3.24/0.86, Difficulty 3.94/0.93 |
| Streamline pathways for International medical graduates to enter surgical training in the US while maintaining high standards for quality care | CR2; 67%; Impact 3.29/1.08; Difficulty 4.06/0.97 |
| Design a matching and support system for the selection of medical students with a commitment to working in underserved communities | CR3; 47%; Impact 3.33/0.91; Difficulty 3.67/0.97 |
| Design a matching and support system for the selection of medical students with a commitment to working in needed specialties, inclusive of true general surgery | CR3; 36%; Impact 3.35/0.89; Difficulty 3.73/0.92 |
| Medical Student Education | |
| The ACS in consultation with the House of Surgery should develop and establish a national curriculum for basic and modular surgical specialty focused surgical education to be required by students entering surgery, ideally reinforced before entering internship at their matched location | CR2; 67%; Impact 3.34/0.96; Difficulty 3.57/0.97 |
| To enhance the pipeline to surgery, develop national models required for medical school accreditation (LCME) for structured engagement programs targeting different educational levels (grade school, high school, college, etc.) and underserved and rural communities | CR3; 36%; Impact 3.25/1.08; Difficulty 3.86/0.95 |
| Develop models at the national level to be required by the medical school accrediting bodies (LCME) for mentorship, early exposure, and creation of an inclusive environment for all medical students interested in surgery with a special emphasis on the needs of those from diverse racial, ethnic, and social backgrounds | CR3; 36%; Impact 3.14/1.05; Difficulty 3.68/0.93 |
| Surgical leaders in collaboration with the Council of Deans and others, should develop a longitudinal surgical major to be recommended for all students planning to enter graduate surgical education | CR3; 36%; Impact 3.18/1.06; Difficulty 3.61/0.78 |
| To better reflect the practice of the surgical disciplines surgical education leaders at the national level develop disease oriented educational modules focusing on cross specialty collaboration and expectations (call, etc.) to train students in surgery, with modular approach to those not entering a surgical specialty (basic) and those applying into surgery (advanced) | CR3; 22%; Impact 2.93/1.04; Difficulty 3.68/0.98 |
| Work Life Integration, Wellness, and Resilience | |
| Codify national guidelines regarding resident trainees (surgery included), wages, and benefits | CR2; 75%; Impact 3.84/1.00; Difficulty 4.02/0.87 |
| Establish an intentional national framework for examining program culture, Department Chair leadership, and program leadership | CR2; 67%; Impact 3.11/1.23; Difficulty 3.67/1.02 |
| Residency Education in Surgery | |
| A digital literacy curriculum (teaching aimed at the learner’s ability to use information and communication technologies to find, evaluate, create, and communicate information) should be incorporated into SCORE and other national curricula for surgical training | CR2; 72%; Impact 3.11/1.01; Difficulty 2.57/0.85 |
| Transition from training to independent practice should be mentored, informed by competency assessment, and be the primary responsibility of terminal training | CR4; 20%; Impact 3.28/1.05; Difficulty 3.89/1.08 |
| Goals, Structure, and Financing of Surgical Training | |
| Reduce the training time for general surgery to a minimum of 4 yr if the trainee has met the required competencies | CR3; 56%; Impact 3.80/0.92; Difficulty 4.16/0.95 |
| Develop advanced 2-yr certificate programs in general surgery that define a period of required conditional independence (Promotion in Place) | CR4; 17%; Impact 3.42/1.12; Difficulty 4.02/0.75 |
| At the national level, define and include the successful attainment of a professional surgical identity as a goal of surgical training | CR4; 14%; Impact 2.58/0.99: Difficulty 3.47/0.99 |
| Faculty Development and Educational Support | |
| Establish a task force to define the levels of faculty appointment as surgical educators including education administration, providing lectures and didactic activities, or teaching clinical skills via an apprenticeship model | CR2; 69%; Impact 2.86/1.03; Difficulty 3.55/1.02 |
| Research Training | |
| For Track 3 (surgeon-scientist): Establish efforts to incorporate research training throughout residency/fellowship (instead of dedicated research years) and compress clinical training to not extend overall training time—similar to early specialization pilots | CR2; 72%; Impact 2.98/0.94; Difficulty 4.00/0.80 |
| Provide a suite of video-based education modules focused on foundational research training | CR3; 33%; Impact 2.78/0.82; Difficulty 2.62/1.09 |
RESULTS
Panel Demographics
The detailed demographic characteristics of the panel are shown in Supplemental Digital Content 1, Table 3, (http://links.lww.com/SLA/F128). Of the 43 panelists, 16 identified as women (37%) and 26 as men (61%). Eighty-six percent (37/43) of panelists were older than 45 years. Seventy percent identified as White or Caucasian, and 9% as Asian/Pacific Islander, Black or African American, or multiple ethnicity or other (4/43). Experience as a surgical educator varied with 57% reporting >20 years’ experience. The majority had multiple leadership roles in surgical education and over 95% were engaged in the education of both medical students and residents with 75% also engaged with fellows. Over 50% (23/44) of the panel reported 20 or more publications in surgical education, 25% (11/43) reported overseeing a research laboratory, and 84% (37/43) reported having a leadership role in a national surgical organization.
Delphi Analysis
The detailed Delphi analysis results are shown in Supplemental Digital Content 1, Table 4 (http://links.lww.com/SLA/F128). After 3 survey rounds, 31 recommendations met the criteria for CR1 with 23 occurring in Round 1, 4 in Round 2, and 4 in Round 3. Eight recommendations met the criteria for either CR2 or CR3 and 3 recommendations were in the CR4 category. The response rate by Delphi Round was as follows: Round 1 81% (51/63), Round 2 68% (43/63), and Round 3 57% (36/63). The Cronbach α was consistent with “good” internal consistency for Round 1 (0.833) and Round 2 (0.825). Internal consistency was “acceptable” for Round 3 (0.792).
Recommendations and Discussion
In this paper, we describe the surgical training priorities that were developed by a carefully selected group of experts in surgical education. We used a Delphi process to achieve consensus and the recommendations that met the criteria for CR1 are presented in rank order from highest level of consensus to lowest level of consensus for each area. Those recommendations that did not reach the predefined criteria for consensus are listed in Table 2. The organization below follows the issues that were considered by the subcommittees and/or BRC II. For reference, after each recommendation we provide the Consensus Rating (CR) 1 to 4; % Agreement; Impact and Difficulty (mean/SD).
Surgical Medical Workforce
The consideration of the surgical and medical workforce was not assigned to a subcommittee, but rather was a focus of the full committee and steering committee. Five recommendations were discussed and included in the Delphi analysis of which one reached consensus.
Recommendations
Meeting the demographic needs of the population served, as well as the sustainability needs of the surgical workforce is a priority for surgical training (CR1; 96%; Impact 3.51/0.92, Difficulty 3.90/0.76).
Discussion
There was a clear consensus that the demographic needs of the population served, as well as the sustainability needs of the surgical workforce is a priority for surgical training. In the past 20 years, there has been a 40% increase in medical school graduates and graduates of training programs in general surgery and its related specialties. Yet there are still shortages and maldistribution today which are predicted to grow in the future. 10 Alternative strategies are needed. The committee could not reach consensus on ways to channel US trainees to needed specialties or practice areas. Nor could the panel reach a strong consensus about methods to enhance the role of international medical graduates in fulfilling these needs. Continued discussion and development of new solutions along these lines is desperately needed and should be a priority for the future. This will need collaboration between surgical organizations, the government, regulatory groups, graduate medical institutions, and oversight bodies.
Medical Student Education
This subcommittee was charged with reviewing foundational curricula and newer approaches, including simulation and telemedicine in medical student surgical education. An important focus was on transition to residency. Of 8 recommendations included in the Delphi assessment, 3 reached consensus.
Recommendations
Develop models embraced by medical schools at the national level that programmatically and financially support surgical faculty and trainees engaged in surgical education and career development of students interested in the surgical disciplines (CR1; 84%; Impact 3.50/0.85, Difficulty 3.95/0.83).
The ACGME, LCME, APDS, and ASE, and specialty societies should work at the national level to develop an optimized residency selection process that adopts enhanced objective metrics in residency applications with a shift in focus from traditional cognitive tests to a holistic assessment approach that evaluates leadership, decision-making, ethics, technical skills, and standardized competency-based assessments of required skills (CR1; 82%; Impact 3.80/0.90, Difficulty 4.20/0.88).
At the surgery department level optimize availability of role models of diverse backgrounds to create a nurturing atmosphere and educational environment consistent with standards of the surgical profession (CR1; 82%; Impact 3.30/1.02, Difficulty 3.36/1.12).
Discussion
Departments of Surgery have traditionally focused on surgical care delivery, development of research programs, and the training of residents and fellows. Medical student education has sometimes taken a backseat to these missions and has often been overlooked or not appropriately prioritized. It is important that departments take a longitudinal approach to surgical training, recognizing that exposing students to surgery and surgeons early in the continuum will give students an understanding of the diverse options in a surgical career. This can begin with involvement in medical student curriculum design, providing didactic lectures in the preclinical years, and shadowing experiences before third year clerkships. It requires commitment of time by surgical faculty, and ideally would include role models that are diverse in subspecialty practice, clinical versus research focus, sex, and race/ethnicity. Increasingly, faculty compensation models that primarily rely on clinical productivity for faculty salaries diminish a department’s ability to support the education mission. Faculty and programmatic support is needed as are models of how to finance these efforts.
Successful transition from medical school to residency training relies upon adequate preparation and a fair selection process. While the fourth year of medical school is under the purview of each school, students interested in training in surgical specialties must be provided with meaningful experience during subinternships, including exposure to overnight call. Working with the Association of Program Directors in Surgery and the Association for Surgical Education, the ACS has developed a curriculum to prepare medical students for residency. 11 Implementation of standardized curricula during the core surgery clerkships merits thoughtful consideration as it should help in providing students a solid foundation for the next phase of their professional development.
The current selection process for students aspiring to match into a surgical specialty merits reevaluation. Although standardized tests are important measures of test taking abilities, a holistic review of applicants’ other attributes can allow selection of students for interview and eventual matching based on the program values, and specific program priorities, including research interests, commitment to caring the underserved, and racial/ethnic diversity.
Work Life Integration, Wellness, and Resilience
This subcommittee investigated the various needs of today’s trainees and recommended changes to meet those needs and improve work-life balance, physical as well as psychological safety, and program culture. Of 6 recommendations that were included in the Delphi assessment 4 reached consensus.
Recommendations
Create best practice recommendations for program and department leadership for creating a culture of belonging for surgical trainees (CR1; 87%; Impact 3.53/1.06, Difficulty 3.09/1.06).
Convene a multidisciplinary national group to achieve an equitable value-based and sustainable improvement in resident wages, taking into consideration the economic value (ROI) of a surgical trainee (CR1; 82%; Impact 3.69/1.04, Difficulty 3.89/0.96).
Develop a national framework defining workplace safety for surgical trainees (CR1; 82%; Impact 3.51/1.08, Difficulty 2.89/0.88).
Creating a just pathway for reporting of workplace mistreatment that provides an equitable investigation free of retaliation (CR1; 81%; Impact 3.29/1.01, Difficulty 3.76/1.03).
Discussion
The life of surgical trainees has dramatically changed in the last 20 years. Adoption of duty hour limits has not negatively affected patient care. 12 However, trainees work in an environment that is fast paced, and care for an increasing number of complex patients. Thus, the learning environment is pressured, focusing on patient care, often at the expense of wellness, personal and family priorities. The hierarchical relationship between trainees and surgical faculty may prevent honest reporting of concerns such as harassment, discrimination, and abuse. 13 This has possibly contributed to the alarming rates of burnout and suicidal ideation. 14 To help mitigate these concerns, Departments of Surgery are encouraged to create a culture of belonging for surgical trainees. Belonging can be defined as the feeling of security and support achieved when there is a sense of acceptance, inclusion, and identity for the trainee in the surgical department. This feeling of group acceptance helps protect the individual from the untoward effects of psychological stress.
While human resource policies and ACGME program requirements define avenues for reporting of mistreatment, they are often ineffective due to trainee reticence to report. The ACGME has 2 mechanisms for residents to report issues in the training program: an ombudsman whose job is to resolve issues outside of the accreditation system; and a formal complaint mechanism that goes directly to the ACGME. 15 A just pathway does exist; however, department and institutional practices need to be aligned with these national guidelines and best practices. A better understanding of what constitutes workplace safety standards for surgical trainees can lead to a safer environment for trainees as well as a greater sense of belonging. Standards for anonymous reporting concerns of harassment or abuse should be widely adopted.
While the cost of living, varies throughout the country, there are situations where the trainee salaries are barely adequate, despite the fact that the resident workforce, including those training in surgery provide immense value to hospitals and health systems for the direct patient care they provide. This complex issue affects all trainees, and data should be gathered on salary, benefits, and value of their work to inform national multidisciplinary discussions to address these financial concerns.
Residency Education in Surgery
This subcommittee reviewed current curricular efforts, including competency-based medical education. They considered simulation and newer modalities such as telemedicine and artificial intelligence. In addition, they examined trainee assessment in competency-based education and the use of EPAs. The transition from residency to practice was of particular interest. Of 7 recommendations considered in the Delphi analysis, 5 reached consensus.
Recommendations
National guidelines should be promulgated to support a comprehensive approach to competency-based reform, inclusive of curricular and assessment reforms, as well as faculty and trainee development (CR1; 96%; Impact 3.64/0.87, Difficulty 3.81/0.85).
Entrustable professional activities (EPAs) should be implemented as a competency-based assessment strategy for all surgical disciplines (CR1; 85%; Impact 3.11/1.01, Difficulty 2.57/0.85).
A mechanism for ongoing review and revision of SCORE should be implemented to ensure currency, including addition of updated content and elimination of nonessential or outdated elements (CR1; 85%; Impact 3.38/1.02, Difficulty 2.45/0.88).
A national research consortium should be established to critically review the effectiveness of competency-based reform, including a focus on implementation and correlation of educational and patient outcomes through data integration strategies (CR1; 81%; Impact 3.59/0.93, Difficulty 3.72/1.05).
Transition from training to independent practice should be mentored, informed by competency assessment, and be a shared responsibility between terminal training and index practice contexts (CR1; 80%; Impact 3.65/0.95, Difficulty 4.11/0.85).
Discussion
Competency-based medical education is an accepted method for medical students and residency training. An effective process to implement EPAs across all surgical disciplines needs to be developed. Surgical faculty will require training in assessment and evaluation, with the understanding that these activities must be integrated into the daily activities of busy clinicians who are essential to resident education. The success of competency-based education and adoption of EPAs have relevance to general surgery residency training, the surgical specialties, and fellowship training programs. National guidelines for CBME and EPA’s must be developed and will be most successful if proven for all surgical specialties. EPA’s are task oriented but specifically avoid being focused on surgical technique or judgment alone, rather they address multiple domains of the ACGME competencies including communication and professionalism among others. It is always a risk, however, that EPA’s will trend towards assessments of operative skill alone. This must be guarded against, or we may risk impeding the development of our trainees clinical thinking processes, curiosity, innovation, and development of effective and compassionate surgical care. Procedural training is crucial, but not sufficient. Thus, ongoing evaluation of these efforts will require critical review of the effectiveness of this reform, which might be best done as national research consortium aligned with intentional data integration to allow objective assessment of educational and patient outcomes.
After completion of terminal formal training (residency or fellowship), new graduates benefit from continued mentorship, and potentially competency assessment. The responsibility for transition to independence should be shared by the training program as well as the practice they enter and might be enhanced by communication between these entities.
SCORE has become the standard national curriculum for general surgery residency training, as well as vascular surgery, pediatric surgery, complex general surgical oncology, and surgical critical care. The available knowledge for surgical residents has expanded incredibly due to electronic information available to trainees. Other surgical specialties have developed similar online curricula. Currently reviewed and revised every 3 years, these online learning materials must continue ongoing review and evaluation with the intent of highlighting current material relevant to the surgical trainee, with addition of new essential information and of elimination of outdated or unnecessary content.
Goals, Structure, and Financing of Surgical Training
In this category, we considered the financial models supporting residency training and how current and future goals could be conducted and needs met within a changing paradigm. Specific considerations included: selection of candidates for surgical training; the importance of diversity alignment with workforce needs; the desired end product; essential resources (human, infrastructure, and finances); and sustainable financing. Eight recommendations were included in the Delphi analysis including 3 proposed by the Steering Committee. Of these, 5 reach consensus.
Recommendations
Convene a summit of national surgical organizations to address funding shortfalls for surgical graduate medical education, to include stakeholders such as policymakers, government representatives, insurance company representatives, philanthropic development experts, and others (CR1; 91%; Impact 3.91/1.06, Difficulty 3.78/1.11).
Convene a summit of national surgical organizations including AAMC Representation (ie, Council of Deans and others) to define pathways to introduce medical students to the surgical disciplines in the first 2 years of medical school (CR1; 86%; Impact 3.18/0.98, Difficulty 3.24/0.98).
Convene a summit of national surgical organizations including AAMC Representation (ie, Council of Deans and others) to define best practices in providing financial support for surgeons involved with undergraduate and graduate surgical education (CR1; 84%; Impact 3.53/1.08, Difficulty 3.42/1.14).
Define the competencies for initial board eligibility in general surgery while simultaneously requiring a minimum of 4 years of training (CR1; 83%; Impact 3.53/1.06, Difficulty 3.53/1.10).
Move towards initial board eligibility for general surgery to occur when the trainee has met the required competencies (CR1; 82%; Impact 3.91/0.90, Difficulty 4.00/0.95).
Discussion
Primary training in general surgery has been mostly unchanged for decades. Over the last 20 years, there have been developments in subspecialty training, including integrated residencies in vascular surgery, thoracic surgery, and plastic surgery. In addition, flexible pathways have been successful in terms of providing residents with an opportunity to have practice specific or fellowship specific training during residency. As surgical training moves toward a competency-based paradigm, EPA’s hold promise of an even more efficient training system that allows individuals to meet their professional goals. If there is a shift from time-based training to a truly competency-based education, the competencies for completion of training need to be proven. Once these are reached (at a minimum of 4 years), board eligibility could be possible, which could create an opportunity for increased autonomy and even “promotion in place.” There are potential barriers concerning implementation of EPAs including tradition and inertia as well as the need for added funding for a trainee that does not meet the expectations defined in the EPAs and will take longer to finish training.
The current method for financing graduate medical education relies primarily on funding from Medicare. As training programs have expanded, there is often inadequate funding for the number of training positions in hospitals. Given ongoing physician shortages including nearly all surgical specialties, we urge the federal government to find ways to invest more in graduate medical education. At the same time, it would be worthwhile to investigate alternate sources of funding. A meeting of surgical organizations should be planned and include broad stakeholder input.
Added financial concerns exist for funding of surgical educators. Engagement with the Association of American Medical Colleges (AAMC) is a reasonable starting point to explore options for financial support for surgical education and increased involvement of surgeons in the preclinical years of medical school.
Faculty Development and Educational Support
This subcommittee investigated the demands on surgical faculty and proposed recommendations to promote and sustain that work into the future. Of the 6 recommendations included in the Delphi analysis, 5 reached consensus.
Recommendations
Work across surgical disciplines to develop a national curriculum for faculty training in surgical education principles, including: teaching in the OR and the use of EPAs; coaching, mentorship, and sponsorship; creating a learning environment devoid of bias and a culture that supports surgical education (CR1; 91%; Impact 3.55/0.93, Difficulty; 3.57/1.11).
Establish a multidisciplinary surgical task force to develop a faculty teaching performance assessment tool based on the best available evidence (CR1; 84%; Impact 3.36/0.99, Difficulty 3.32/1.05).
Surgery RRC to work with APDS to define minimal faculty FTE requirements for program accreditation in the areas of teaching learners, including using simulation, for quality assessment and improvement, and database and portfolio development (CR1; 83%; Impact 3.18/0.97, Difficulty 3.70/0.95).
Establish a task force of leaders from all surgical disciplines, hospitals, and medical schools to define and validate a system to pay surgeons for their efforts in graduate and undergraduate surgical education (CR1; 82%; Impact 3.82/1.06, Difficulty 4.09/0.94).
Establish a task force of leaders from all surgical disciplines and hospitals to accurately define the economic value of a surgical trainee (ie, resident, or fellow) for the purposes of negotiating hospital payment for their work (CR1; 81%; Impact 3.66/1.12; Difficulty 3.91/0.86).
Discussion
Professional development for faculty is necessary to improve teaching skills, and training in evaluation and assessment is needed for successful implementation of competency-based medical education. As we improve our teaching skills, a tool to assess the quality of the teaching will be useful. A national teaching curriculum for faculty should be developed that involves all surgical specialties, including a focus on how to effectively implement EPAs and CBME in surgery. The issue of compensation for surgeons teaching time to offset lost clinical productivity is real and needs to be addressed with solutions found and implemented. To provide livable wages for trainees, it is essential that we define the economic value of all trainees to the hospitals including those in surgery. Strategic initiatives should be undertaken by surgical education leaders and colleges of medicine and osteopathy in collaboration with the AAMC and other oversight groups with regular meetings and monitoring of the progress.
Research Training
This subcommittee was asked to review current efforts to train surgeon-scientists and how those efforts could be perfected to provide a universal minimum standard of research education simultaneously creating a research track for those pursuing an academic surgery career path (basic science research, education, quality outcomes, etc.). Specifically, they considered the best timing of research training in residency, curriculum, and advanced degrees. Of the 9 recommendations considered in the Delphi analysis, 7 reached consensus.
Recommendations
Create a national research curriculum using a competency-based medical education (CBME) framework to meet the needs of the proposed tracks (CR1; 89%; Impact 3.11/0.98, Difficulty 3.58/0.92).
Update SCORE content for foundational research training (CR1; 89%; Impact 2.76/0.88, Difficulty 2.58/0.94).
Change the selection process for competitive surgical fellowships so that they do not hinge on a certain type of research experience but rather provide alternative ways to expose trainees to subspecialty disciplines and to reduce the barriers for surgical trainees to access fellowship training positions (CR1; 89%; Impact 3.64/0.88, Difficulty 3.47/1.06).
Establish nationally required research tracks as specified by the ACGME: foundational (Track 1), flexible (Track 2), and surgeon-scientist (Track 3) (CR1; 82%; Impact 3.76/1.03, Difficulty 3.98/1.06).
Establish national processes to evaluate the impact of the proposed changes in research training on resident wellness, fellowship matching, career trajectories, research discoveries and innovations, and other outcomes (CR1; 82%; Impact 3.07/0.78, Difficulty 3.18/1.01)
Implement the Track 2 (flexible) research pathway to enhance research training, scholarship, and professional development to meet the future needs of academic programs and health care delivery systems (CR1; 80%; Impact 3.11/0.75, Difficulty 3.60/0.96).
For Track 3 (surgeon-scientist): Develop a research track to prepare surgeon scientists to enhance competitiveness for extramural funding and allows board subspecialty certification. These programs will require a well-developed training program infrastructure (including dedicated program leadership, staff, and mentors), institutional commitment, and high-quality research environment (CR1; 80%; Impact 3.53/0.99, Difficulty 4.04/0.85).
Discussion
Surgical research has led to transformational advances in the treatment of human disease, from the development of antisepsis, anesthesia, blood transfusion, nutritional support, and organ transplantation to the discovery of insulin and the targeted treatment of cancer. Yet the accelerating pace and deepening complexity of scientific discovery pose significant challenges to the ongoing role of surgeons, from the creation of new knowledge to its thoughtful translational application in the clinical setting.
All surgeons by the completion of their training should gain a fundamental appreciation for research that prepares them to ethically apply future scientific breakthroughs and technological advances to their clinical practice over the course of a career. To this end, a competency-based curriculum should be developed that includes interpretation of evidence, implementation, innovation, statistical approaches, bioinformatics, and scientific communication. This should apply to most trainees (Track 1). All programs regardless of setting or size should be able to readily access common resources for this curriculum through platforms such as SCORE.
Although some surgical scientists have been successful with a 2-year concentrated research experience during residency, it is becoming more widely appreciated that this limited research experience during residency is insufficient preparation for a career as an independent investigator. In fact, most trainees do not pursue such experiences with the goal of becoming a surgeon-scientist. Extension of research time beyond 2 years for the resolute few is usually impractical and may excessively disrupt clinical training. Because of the time needed to later complete residency and fellowship, a research hiatus of 4 to 6 years places the budding surgical investigator at considerable disadvantage. Individuals with advanced research credentials (eg, MD, PhD) may be discouraged from entering surgical training because of the total length of clinical training, during which their ability to conduct research is effectively on hold. To encourage the pursuit of careers as surgeon-scientists, it is important to set up a more efficient and effective pathway (Track 3) that better integrates research and clinical training, extending through subspecialty fellowship. Similar physician-scientist training pathways already exist within other clinical specialties such as Neurosurgery and Pediatrics and may serve as a useful blueprint. Because Track 3 requires substantial infrastructure, investment, and the availability of surgeon-scientists to serve as role models and mentors, it is predicted to be available in only a handful of programs and to apply to <10% of trainees. The Track 3 strategy may maximize chances for the aspiring surgeon-scientist to achieve extramural funding and other metrics of success.
For trainees, dedicated time during residency for research and other professional development activities is still a valuable experience that may provide skills and perspectives that further their individual academic, personal, and career goals as surgeons. However, some feel obliged to undertake these experiences during residency primarily to increase their perceived competitiveness for coveted subspecialty fellowship positions. Thus, a flexible approach to research and professional development time (“Track 2”) should continue to be available to develop future leaders and meet the diverse needs of academic programs, but this should ideally be dissociated from the selection process for subspecialty fellowship.
Educational Technology and Assessment
This subcommittee reviewed the technological advances in education since BRC I. They constructed a framework for applying these technologies to improve the effectiveness and efficiency of surgical education and assessment. They considered the implications of innovative technologies, including artificial intelligence, on learner-centered surgical education. They recommended a framework for applying these in surgical education. Five recommendations were made. After discussion with the full BRC II committee, these were combined into a single recommendation which reached consensus.
Recommendations
Given the rapidly changing landscape in surgical education and evolving technology, it is recommended that a Multidisciplinary Surgical Educational Council be established with the collaborative efforts of the ACS, ABS, ACGME, ASE, APDS, and the parallel surgical specialty boards and oversight groups to serve as an oversight body and convene subcommittees to: (1) monitor and facilitate implementation of BRC II recommendations, (2) establish, assess and maintain an up to date toolbox of new recommended educational technologies, and (3) develop consensus and road maps on best practices for technology implementation and prospective assessment (CR1; 93%; Impact 3.93/1.00, Difficulty 3.93/1.00).
Discussion
This subcommittee found innumerable technologies available for surgical education, and included simulation, telementoring, artificial intelligence, video, and haptic sensors for assessment of technical skills. While these products and services have provided value to the end users, a comprehensive warehouse of educational technologies does not exist. An important work product was creating a toolbox of new educational technologies with guidelines for implementation. Further advances and evaluation of existing products would receive help from the establishment of Multidisciplinary Surgical Educational Council to coordinate efforts of the ACS, ABS, and surgical education societies in advancing educational technology and assessment as well to monitor and facilitate the implementation of the recommendations made by BRC II.
LIMITATIONS
The findings of this report must be considered within the context of its limitations. Although we tried to include in a diverse panel of experts in surgical education, an unanticipated shortcoming is that the demographics of the panel was not balanced with most members being White or Caucasian and older than 45 years. Thus, they were limited by their unique perspectives and lacked the potential diversity of opinions necessary for a robust discussion. This may be in part the consequence of including the BRC I panel from 20 years ago. That said the work was primarily performed by the subcommittees focused on current issues. These groups were younger, gender diverse with more balance in racial and ethnic makeup. Furthermore, the panel sought input from residents and fellows through a focused group meeting as well as non-general surgery specialists who may be directly affected or interested in the statements. The majority of panelists were surgeons and hence there is an unavoidable bias in that sense. There were no patients on the panel, however, a member of the steering committee was a public member with board service on the American Board of Surgery and an understanding of the financing graduate medical education. The recommendations will require annual review to monitor implementation. We defined consensus as achieving >80% agreement to include proposed recommendations. It could be argued that the bar for consensus was too high. Many of the proposed recommendations have merit and may warrant consideration as well. Regarding the Delphi survey process there was a falloff in the response rate over the 3 rounds. This could have negatively affected the final overall consensus ratings. Despite this, the internal consistency was good in Rounds 1 and 2 and acceptable in Round 3. The priority recommendations will require annual review to monitor implementation.
SUMMARY
It is clear from this contemporary assessment that the landscape of surgical education and training is rapidly changing with countless challenges and opportunities. The progress following the report by BRC I took 2 decades and was made primarily in areas controlled directly by surgeons in collaboration with the ABS, ACS, and RRC-S combined with the organic need-based expansion of medical schools and then post graduate surgical training programs. In this report, several key recommendations emerged as shown in Table 3. These will be further amplified by forthcoming reports from each of the subcommittees. It is clear that there is much more work to do.
TABLE 3.
BRC II Key Recommendations
| Prioritizing the sustainability of the surgical workforce in training programs |
| Optimizing the preparation of medical students for a possible surgical career |
| Selecting surgical trainees through a more holistic process |
| Establishing a culture of belonging and safety for our trainees |
| Implementing competency-based training for all surgical specialties |
| Providing trainees a mentored transition to practice |
| Solving the financial underfunding of surgical education |
| Developing a national curriculum for faculty development in education, EPAs, and assessment |
| Developing a surgeon-scientist training pathway |
| Providing a framework for change implementation and oversight by a Multidisciplinary Surgical Education Council |
We must realize that the pace of change in medicine is greater today than it was in the days when one was limited to practice by the knowledge that you could carry around with you. 16 What our residents and fellows are trained in today is not likely to be what they will be doing in 20 years. For our patients sake, we cannot wait another 20 years let alone 5 years. We must act now with ongoing review and oversight to bring these recommendations to reality in a maximum of the next 5 years. Implementation will require dedication and meaningful collaboration of surgeon educators and leaders collaborating with like-minded partners in government, as well as regulatory and oversight organizations. Although we did not provide a description of implementation pathways, we have proposed a framework for successful change. This includes establishing a multidisciplinary surgical educational group to oversee, monitor and facilitate implementation of these recommendations. It is now up to our profession.
CONCLUSIONS
The members of BRC II are motivated by our commitment and dedication to providing the highest quality surgical care to all while we continually earn the trust of our patients. In this report, we propose recommendations to optimize surgical education and training. In the broader sense, as surgical educators, we must keep focus on our overall goal which is to prepare the current and future generations of surgeons to meet the ever-changing health care needs of society while keeping the trust of those we serve. Our trainees must be competent in essential skills but also learn how to think through the complexities of surgical disease and to be inspired by an unrelenting commitment to quality keeping the patient at the forefront at all times. The scope of our initiative is broader than general surgery and broader than the current portfolio of procedures in our toolbox. We must be prepared to safely integrate advances in surgical care in our educational programs and practice. Although, we believe the proposed changes in surgical education and training will need to be driven by surgeons, we also appreciate that for these to be successfully implemented will require help and collaboration of organizations overseeing undergraduate and graduate medical education as well as the certifying boards. It is imperative that we must act with a real sense of urgency lest we lose valuable time in the face of unrelenting change.
As for next steps, as the highest priority, we recommend establishing a Multidisciplinary Surgical Educational Council to work with current organizations and regulatory bodies to design a plan for implementation including monitoring. One might consider the following prioritization framework based on the CR category derived from the Delphi analysis of 50 recommendations: CR1 (≥80%) (N=31) may be considered as high priority items and implementation should proceed; CR2 (60% to 79%) (N=8) may be considered as a moderate priority and warrant thoughtful consideration; CR3 (21% to 59%) (N=8) may be considered a low priority and at some time in the future may need additional investigation; and CR4 (14% to 20%) (N=3) would be considered a very low priority and may not need further investigation at this time.
Supplementary Material
Acknowledgments
Acknowledgment of Collaborative Group
Blue Ribbon Committee II: Blue Ribbon Committee I Review: Findings and Impact: Chair—Timothy C. Flynn MD; Barbara L. Bass, MD—George Washington School of Medicine and Health Sciences; Murray F. Brennan, MD—Memorial Sloan Kettering Cancer Center; Haile T. Debas, MD—University of California, San Francisco; Julie A. Freischlag, MD—Wake Forest School of Medicine; R. Scott Jones, MD, MS—University of Virginia; Mark A. Malangoni, MD—Cleveland, Ohio; Carlos A. Pellegrini, MD—University of Washington; Ajit K. Sachdeva MD—American College of Surgeons; Patricia L. Turner, MD, MBA—American College of Surgeons; Andrew L. Warshaw, MD—Massachusetts General Hospital; Richard E. Welling, MD; Michael J. Zinner, MD—Miami Cancer Institute and Baptist Health Cancer Center. Medical Student Education: Co-Chairs—Adnan A. Alseidi, MD, EdM—University of California, San Francisco and Henri R. Ford, MD, MHA—University of Miami Miller School of Medicine; H. William Craver, DO—American Association of Colleges of Osteopathic Medicine; Andrew J. Dennis, DO—Midwestern University College of Osteopathic Medicine; Abbey Fingeret, MD, MS, MHPTT—University of Nebraska Medical Center; Gerald M. Fried, MD, CM—McGill University; Bonnie Simpson Mason, MD—American College of Surgeons; Ranjan Sudan, MD, MBBS—Duke University School of Medicine; Stephen C. Yang, MD—Johns Hopkins Medical Institutions. Work Life Integration, Wellness, and Resilience: Co-Chairs—Kristen Conrad-Schnetz, DO—Cleveland Clinic and Kyla P. Terhune, MD, MBA—Vanderbilt University Medical Center; Wali R. Johnson, MD, MPH—Vanderbilt University Medical Center; Megan E. Jenkins Turner, DO—Franciscan Health St. James General Surgery Residency; Ajita S. Prabhu, MD—Cleveland Clinic Lerner College of Medicine through Case Western Reserve University; Bonnie Simpson Mason, MD—American College of Surgeons. Residency Education in Surgery: Co-Chairs—Karen J. Brasel, MD, MPH—Oregon Health and Science University and John D. Mellinger, MD, MS—American Board of Surgery; Eric A. Elster, MD—Uniformed Services University; Gerald M. Fried, MD, CM,—McGill University; Daniel A. Hashimoto, MD, MTR—Hospital of the University of Pennsylvania; Benjamin T. Jarman, MD—Gunderson Health System; Amit R.T. Joshi, MD—Cooper Medical School of Rowan University; Rachel R. Kelz, MD, MSCE, MBA—Hospitals of the University of Pennsylvania; Brenessa M. Lindeman, MD, MEHP—University of Alabama at Birmingham; Carla M. Pugh, MD, PhD—Stanford University; Richard K. Reznick, MD—Royal College of Physicians and Surgeons of Canada. Goals, Structure, and Financing of Surgical Training: Co-Chairs—Julie A. Freischlag, MD—Wake Forest School of Medicine and Mary E. Klingensmith, MD—Accreditation Council for Graduate Medical Education; Cherisse D. Berry, MD—NYU Grossman School of Medicine; David T. Cooke, MD—University of California Davis Health; Karen Fisher, JD—Public Member, Washington, DC; Rebecca M. Minter, MD—University of Wisconsin School of Medicine and Public Health; Linda G. Phillips, MD—University of Texas Medical Branch, Galveston; Anton N. Sidawy, MD, MPH—George Washington University. Faculty Development and Educational Support: Co-Chairs—Diana L. Farmer, MD—University of California Davis Health and Richard B. Damewood, MD—WellSpan York Hospital; Julie A. Freischlag, MD—Wake Forest School of Medicine; M. Ashraf Mansour, MB, BCH—American Board of Surgery; Fabrizio Michelassi, MD—Weill Cornell Medical College; Mohsen M. Shabahang, MD, PhD—WellSpan Surgical Specialists; Kenneth Sharp, MD—Vanderbilt University Medical Center. Research Training: Co-Chairs—Mary T. Hawn, MD—Stanford University and Jeffrey B. Matthews, MD—The University of Chicago Medicine & Biological Sciences; Ginny L. Bumgardner, MD, PhD—The Ohio State University, College of Medicine; James S. Economou, MD, PhD—University of California, Los Angeles; Kamal M.F. Itani, MD—Veterans Affairs Boston Health Care System; Rachel R. Kelz, MD, MSCE, MBA—Hospitals of the University of Pennsylvania; Thomas F. Tracy, Jr, MD, MBA—American Pediatric Surgical Association; Martha A. Zeiger, MD—National Institutes of Health, National Cancer Institute. Educational Technology and Assessment: Co-Chairs—Gerald M. Fried, MD, CM—McGill University and Carla M. Pugh, MD, PhD—Stanford University; Caprice C. Greenberg, MD, MPH—University of North Carolina at Chapel Hill School of Medicine; Daniel A. Hashimoto, MD, MS—Hospital of the University of Pennsylvania; John T. Paige, MD—LSU Health New Orleans School of Medicine; Dana A. Telem, MD, MPH—University of Michigan; Julian E. Varas, MD, MS—Pontificia Universidad Catolica de Chile. Delphi analysis: Xiaodong Chen, PhD, MSc, BEng—The Ohio State University College of Medicine and Dimitrios Stefanidis, MD, PhD—Indiana University School of Medicine. Steering Committee: Co-Chairs—E. Christopher Ellison, MD—The Ohio State University College of Medicine and Steven C. Stain, MD—Lahey Hospital and Medical Center; L.D. Britt, MD, MPH—Eastern Virginia Medical School; Jo Buyske, MD—American Board of Surgery; Karen Fisher, JD—Public Member, Washington, DC; Ajit K. Sachdeva, MD—American College of Surgeons; Patricia L. Turner, MD, MBA—American College of Surgeons. American College of Surgeons Staff Collaboration: Patrice Gabler Blair, DrPH, MPH; Connie Bura; Linda K. Lupi, MBA; Deirdre M. McGory, JD; Rachel Williams Newman, MS; Peter J. Schmitt, MA, Chicago, IL.
Footnotes
S.C.S. and E.C.E. are joint first authors.
Blue Ribbon II Committee was sponsored by the American College of Surgeons, Chicago, IL; American Board of Surgery, Philadelphia, PA; The American Surgical Association, Boston, MA. No funding received for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); or others.
Authors' contribution: All authors meet the following requirements: (1) authors made substantial contributions to conception and design, and/or acquisition of data, and/or analysis and interpretation of data; (2) authors participated in drafting the article or revising it critically for important intellectual content; and (3) authors gave final approval of the version to be published. In addition, they participated in BRC II subcommittee and committee meetings. S.C.S. and E.C.E.: member of the writing committee, presents at ASA Forum, co-principal author and co-chair of the BRC II responsible for process, design, and oversight of the BRC II and corresponding author. E.C.E.: member of the writing committee, presents at ASA Forum, co-principal author and co-chair of BRC II responsible for process, design, and oversight of the BRC II and corresponding author. D.L.F.: member of the writing committee, Co-chair Faculty Development and Educational Support. T.C.F.: member of the writing committee and chaired the BRC I Review Committee. J.A.F.: co-chair goals, structure and financing subcommittee, presented at ASA Forum. J.B.M.: member of the writing committee, Co-chair Residency Research Subcommittee. R.W.N.: member of writing committee and lead administrative support for project. X.C. and D.S.: consultant for Delphi analysis, reviewed/wrote methods. L.D.B., J.B., K.F., A.K.S., and P.L.T.: members of the steering committee guided the BRC II process and contributed critical review of the manuscript. Blue Ribbon Committee II: as indicated in the submission letter, the entire BRC II committee contributed to the content of this manuscript through participation in hours of virtual meetings and discussions in subcommittee meetings and BRC II meetings.
E.C.E. receives royalties from McGraw Hill and Wolters-Kluwer unrelated to this manuscript. The remaining authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.annalsofsurgery.com.
Contributor Information
Steven C. Stain, Email: steven.c.stain@lahey.org.
E. Christopher Ellison, Email: christopher.ellison@osumc.edu.
Diana L. Farmer, Email: dlfarmer@ucdavis.edu.
Timothy C. Flynn, Email: timothy.flynn@surgery.ufl.edu.
Julie A. Freischlag, Email: jfreisch@wakehealth.edu.
Jeffrey B. Matthews, Email: jmatthews@uchicago.edu.
Rachel W. Newman, Email: rnewman@facs.org.
Xiaodong Chen, Email: Xiaodong.Chen@osumc.edu.
Dimitrios Stefanidis, Email: dimstefa@iu.edu.
L.D. Britt, Email: brittld@evms.edu.
Jo Buyske, Email: jbuyske@absurgery.org.
Karen Fisher, Email: KSFisher1776@gmail.com.
Ajit K. Sachdeva, Email: asachdeva@facs.org.
Patricia L. Turner, Email: pturner@facs.org.
Collaborators: Timothy C. Flynn, Barbara L. Bass, Murray F. Brennan, Haile T. Debas, Julie A. Freischlag, R. Scott Jones, Mark A. Malangoni, Carlos A. Pellegrini, Ajit K. Sachdeva, Patricia L. Turner, Andrew L. Warshaw, Richard E. Welling, Michael J. Zinner, Adnan A. Alseidi, Henri R. Ford, H. William Craver, Andrew J. Dennis, Abbey Fingeret, Gerald M. Fried, Bonnie Simpson Mason, Ranjan Sudan, Stephen C. Yang, Kristen Conrad-Schnetz, Kyla P. Terhune, Wali R. Johnson, Megan E. Jenkins Turner, Ajita S. Prabhu, Bonnie Simpson Mason, Karen J. Brasel, John D. Mellinger, Eric A. Elster, Gerald M. Fried, Daniel A. Hashimoto, Benjamin T. Jarman, Amit R. T. Joshi, Rachel R. Kelz, Brenessa M. Lindeman, Carla M. Pugh, Richard K. Reznick, Julie A. Freischlag, Mary E. Klingensmith, Cherisse D. Berry, David T. Cooke, Karen Fisher, Rebecca M. Minter, Linda G. Phillips, Anton N. Sidawy, Diana L. Farmer, Richard B. Damewood, Julie A. Freischlag, M. Ashraf Mansour, Fabrizio Michelassi, Mohsen M. Shabahang, Kenneth Sharp, Mary T. Hawn, Jeffrey B. Matthews, Ginny L. Bumgardner, James S. Economou, Kamal M. F. Itani, Rachel R. Kelz, Thomas F. Tracy, Jr, Martha A. Zeiger, Gerald M. Fried, Carla M. Pugh, Caprice C. Greenberg, Daniel A. Hashimoto, John T. Paige, Dana A. Telem, Julian E. Varas, Xiaodong Chen, Dimitrios Stefanidis, E. Christopher Ellison, Steven C. Stain, L.D. Britt, Jo Buyske, JD Karen Fisher, Ajit K. Sachdeva, Patricia L. Turner, Patrice Gabler Blair, Connie Bura, Linda K. Lupi, Deirdre M. McGory, Rachel Williams Newman, and Peter J. Schmitt
REFERENCES
- 1. Debas HT. Surgery: a noble profession in a changing world. Ann Surg. 2002;236:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Debas HT, Bass BL, Brennan MF, et al. American Surgical Association Blue Ribbon Committee . American Surgical Association Blue Ribbon Committee Report on Surgical Education: 2004. Ann Surg. 2005;241:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lewis F, Klingensmith M. Issues in general surgery residency training—2012. Ann Surg. 2012;256:553–559. [DOI] [PubMed] [Google Scholar]
- 4. Rosenbaum L. Not otherwise specified: the quiet revolution in medical training. N Engl J Med. 2024;390:e19.38381672 [Google Scholar]
- 5. SCORE. The Score Portal from the Surgical Council of Resident Education. Accessed March 2, 2024. http://www.surgicalcore.org/
- 6. Dagnone D, Stockley D, Flynn L, et al. Delivering on the promise of competency based medical education—an institutional approach. Can Med Educ J. 2019;10:e28–e38 [PMC free article] [PubMed] [Google Scholar]
- 7. Atkinson RB, Khubchandani JA, Chun MBJ, et al. Cultural competency curricula in US graduate medical education: a scoping review. J Grad Med Educ. 2022;14:37–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jünger S, Payne SA, Brine J, et al. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med. 2017;31:684–706. [DOI] [PubMed] [Google Scholar]
- 9. Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oslock WM, Satiani B, Way DP, et al. A contemporary reassessment of the US Surgical Workforce through 2050 predicts continued shortages and increased productivity demand. Am J Surg. 2022;223:28–35 [DOI] [PubMed] [Google Scholar]
- 11. American College of Surgeons. ACS/APDS/ASE Resident Prep Curriculum. Accessed March 12, 2024. http://www.facs.org/for-medical-professionals/education/programs/acsapdsase-resident-prep-curriculum/
- 12. Rajaram R, Chung JW, Jones AT, et al. Association of the 2011 ACGME resident duty hour reform with general surgery patient outcomes and with resident examination performance. JAMA. 2014;312:2374–2384. [DOI] [PubMed] [Google Scholar]
- 13. Hu YY, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381:1741–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80–90. [DOI] [PubMed] [Google Scholar]
- 15. Accreditation Council for Graduate Medical Education . Report an issue. Accessed March 28, 2024. https://www.acgme.org/residents-and-fellows/report-an-issue/ [Google Scholar]
- 16. Rubin R. It takes an average of 17 years for evidence to change practice—the burgeoning field of implementation science seeks to speed things up. JAMA. 2023;329:1333–1336. [DOI] [PubMed] [Google Scholar]