Abstract
Background
The Pain Understanding and Confidence Questionnaire (PUnCQ) comprises two parts: the first assesses clinical judgments based on contemporary pain knowledge, and the second consists of items querying confidence in pain management for the presented vignette. In contrast to existing measures, PUnCQ can evaluate a therapist’s capacity to make appropriate clinical decisions within a specific vignette. Thus, PUnCQ may be a promising measure to assess the clinical competence of physical therapists in pain management. This study evaluated the structural and construct validity of PUnCQ.
Methodology
Eligible participants were two cohorts of physical therapists managing patients with pain. PUnCQ and Knowledge and Attitudes of Pain (KNAP) data were collected using an anonymous survey. Confirmatory factor analysis was conducted for both parts of the PUnCQ, and an exploratory factor analysis was conducted when multidimensionality was suspected. Construct validity was assessed with the hypothesis that Pearson’s r values to KNAP scores, indicating knowledge about modern pain science and biopsychosocial attitudes toward pain, were expected to be 0.3-0.5 in part one and >0.5 in part two.
Results
Data from 112 participants were analyzed. PUnCQ part one fully satisfied the predetermined criteria for unidimensionality, but part two did not. Exploratory factor analysis for part two revealed a two-factor structure: a 14-item Factor 1 labeled “pain management” and a seven-item Factor 2 labeled “medication guidance and pain mechanism,” while Cronbach’s alpha was 0.98 across all items. Statistically significant correlations were detected with the KNAP in each part of the PUnCQ (r = 0.26 in part one and r = 0.41 in part two).
Conclusion
PUnCQ has structural validity and an aspect of construct validity.
Keywords: whiplash, pain neuroscience education, pain management, knowledge, chronic pain, unidimensionality
Introduction
Pain is the main reason patients seek musculoskeletal care. A comprehensive understanding of pain is essential for patient education, which is a core component of optimal musculoskeletal management [1] and whose effective administration is a recent research priority [2]. Research has focused on the attitudes and knowledge of physical therapists regarding pain, resulting in the development of assessment methods. For example, the Pain Attitudes and Beliefs Scale for Physiotherapists [3] evaluates the balance between the biological perspective, considering the extent of tissue damage in low back pain, and biopsychosocial factors that can exacerbate pain beyond tissue damage. Similarly, the Neurophysiology of Pain Questionnaire [4,5] was developed and modified to measure knowledge of neurophysiological pain mechanisms. While these measures contributed to evidence-based practice [6], the recent recognition of the effectiveness of pain neuroscience education [7,8] has led to the development of the Knowledge and Attitudes of Pain (KNAP), which assesses knowledge about modern pain science and biopsychosocial attitudes required for health care professionals [9]. However, these existing measures primarily assess general knowledge and attitudes, although clinical decision-making should be made by considering the patient’s biopsychosocial status, medical history, thoughts, and preferences as a whole. Therefore, they lack an evaluation of their ability to perform appropriate pain management in real clinical settings.
In response to these limitations, the Pain Understanding and Confidence Questionnaire (PUnCQ), introduced in 2020 [10,11], presents a clinical vignette featuring whiplash-associated disorders. PUnCQ probes 12 aspects of pain management. In contrast to the existing measures, PUnCQ surpasses general pain knowledge assessment, focusing on the competence of evidence-based clinical decision-making within a specific vignette. This unique approach positions PUnCQ as a promising tool for evaluating an aspect of the clinical competence of physical therapists in pain management. The PUnCQ has two parts: the first assesses the clinical competence of clinical decision-making based on contemporary knowledge of pain, and the second consists of 21 items querying confidence in pain management for the vignette. PUnCQ reflects the core curriculum of the International Association for the Study of Pain [12] and the British Pain Society [13]. Moreover, PUnCQ was developed by an expert panel including an anesthetist, a nurse, a pharmacist, a physical therapist, a psychologist, and an occupational therapist, indicating content validity. A previous study [10] investigated internal consistency for both parts among 133 undergraduate students and reported Cronbach’s alpha values of 0.58 for part one and 0.96 for part two. However, validation through factor analysis for construct validity, recommended by the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) initiative [14], has not been conducted. Therefore, PUnCQ, while showing some evidence of internal structure, requires further construct validity using factor analysis.
When evaluating internal structure, internal consistency is an important but insufficient indicator, and unidimensionality is crucial for using a representative score for a certain concept. Despite content validity and satisfactory internal consistency across all items, a lack of unidimensionality may require scoring adjustments, such as summing averaged scores in each subscale to reach an overall score.
This study had two primary objectives: to evaluate the structural validity of the PUnCQ by assessing the unidimensionality of its two parts through factor analysis and to assess the construct validity of the PUnCQ by testing its correlation with the KNAP. These objectives aim to provide evidence for the validity of the PUnCQ as a tool for assessing pain management competence in physical therapists.
Materials and methods
Design
This cross-sectional study involved the data analysis of an anonymous paper-based survey administered to members of the Japanese Society of Allied Health and Rehabilitation and an anonymous online survey administered to members of the Japan Branch of the International McKenzie Institute. This study was an anonymous survey, and by completing the survey form, participants were exempted from submitting a written consent form for this study. The Ethics Committee of the Saitama Prefectural University approved the study (approval number 23100).
Participants
Following COSMIN guidelines [14], the sample size calculation indicated at least 105 participants to conduct a confirmatory factor analysis of the 21-item PUnCQ. Surveys were conducted among members of the Japanese Society of Allied Health and Rehabilitation (n = 263) and the Japan Branch of the International McKenzie Institute (n = 387), assuming a survey participation of approximately 20% based on previous studies [15-19].
The inclusion criterion was individuals registered as members of the respective organizations. Members of the Japan Branch of the International McKenzie Institute with registered email addresses were targeted.
The exclusion criteria were individuals not currently involved in treating patients with pain, those from professions other than physical therapy, and those with missing data. Duplicates across the two cohorts were excluded. The data collection period for each organization was two weeks.
Variables
The PUnCQ utilizes a clinical vignette featuring a whiplash-associated disorder. In part one, participants respond to 12 clinical judgments related to pain. Part two assesses confidence in 21 management skills. In part one, each of the five choices per clinical judgment is assigned a score of 1 for a correct response. Inappropriate choices, including “do not know,” receive a score of 0. The total score ranges from 0 to 12. In part two, participants rate their confidence in each management skill on an 11-point scale from 0 (not at all confident) to 10 (no problem). The mean score ranges from 0 to 10. This study used the Japanese PUnCQ [20].
The KNAP comprises 30 items that assess the participants’ knowledge of modern pain science and biopsychosocial attitudes toward pain. Respondents rate their agreement with statements on a 6-point scale. Following COSMIN guidelines, the KNAP underwent content validity verification [9]. Structural validity was assessed through exploratory factor and Rasch analysis, using data from 424 students in a four-year entry-level physical therapy education program [9]. In addition to internal consistency, hypothesis testing, test-retest reliability, and responsiveness were examined [9]. The internal consistency of KNAP, measured by Cronbach’s alpha, was 0.8 [9]. Scores were weighted for each item [9], resulting in a total score range of 0 to 150, where higher scores indicate greater knowledge of modern pain science and biopsychosocial attitudes toward pain. This study used the Japanese KNAP [21].
Analysis
IBM®SPSS® Amos™ 20.0 (IBM Corp., Armonk, NY, USA) was used for the confirmatory factor analysis. IBM SPSS Statistics for Windows, Version 28.0 (Released 2021; IBM Corp.) was used for other statistical analyses. The significance level was 5%.
Structural Validity
Unidimensionality was assumed when one of the following criteria was satisfied: (1) chi-squared/degree of freedom <3; (2) comparative fit of index >0.95; (3) goodness-of-fit index >0.90; (4) adjusted goodness-of-fit index >0.85; (5) root mean square error of approximation <0.06; or (6) standardized root mean square residual <0.08 [14,22-24]. However, for the conservatory assessment of structural validity, when one of the criteria was not satisfied, exploratory factor analysis was conducted with the maximum likelihood method and direct oblimin rotation as recommended in a previous study [25]. Factor solutions with eigenvalues >1 were investigated. Additionally, the Kaiser-Meyer-Olkin measure was calculated, and Bartlett’s sphericity test was conducted with the acceptance criteria of a Kaiser-Meyer-Olkin measure >0.5 and a p-value <0.05. Subsequently, Cronbach’s alpha was calculated for each factor identified in the exploratory factor analysis and across all items. Acceptable internal consistency was deemed an alpha value ≥0.7 [14].
Hypothesis Testing for Construct Validity
Each part of the PUnCQ was expected to have a statistically significant correlation to KNAP. Furthermore, part two of the PUnCQ uses an 11-point numerical confidence rating scale, which was expected to be similar to KNAP. Therefore, Pearson’s r correlation to KNAP was expected to be >0.5 [14]. In contrast, part two of the PUnCQ uses binary variables and indicates the competence of evidence-based clinical decision-making within a specific vignette, which was expected to be dissimilar to KNAP. Therefore, Pearson’s r correlation to KNAP was expected to be 0.3-0.5 [14].
Results
Responses were obtained from 78 individuals (29.7%) in the Japanese Society of Allied Health and Rehabilitation cohort and 80 (20.1%) in the Japan Branch of the International McKenzie Institute cohort. Eighteen individuals in the Japanese Society of Allied Health and Rehabilitation cohort were excluded, yielding 60 valid responses. Similarly, 28 individuals from the Japan branch of the International McKenzie Institute cohort were excluded, yielding 52 valid responses. In total, there were 112 valid responses. The summary of participant demographics is presented in Table 1.
Table 1. Summary of the 112 participants.
| Variables | N = 112 |
| Age (years), mean (SD) | 36.7 (8.7) |
| Clinical experience (years), mean (SD) | 12.5 (7.5) |
| Sex | |
| n of men (%) | 89 (79.5%) |
| n of women (%) | 23 (20.5%) |
| Academic degree | |
| n of career college (%) | 48 (42.9%) |
| n of junior college or college (%) | 52 (46.4%) |
| n of master’s degree (%) | 10 (8.9%) |
| n of doctoral degree (%) | 2 (1.8%) |
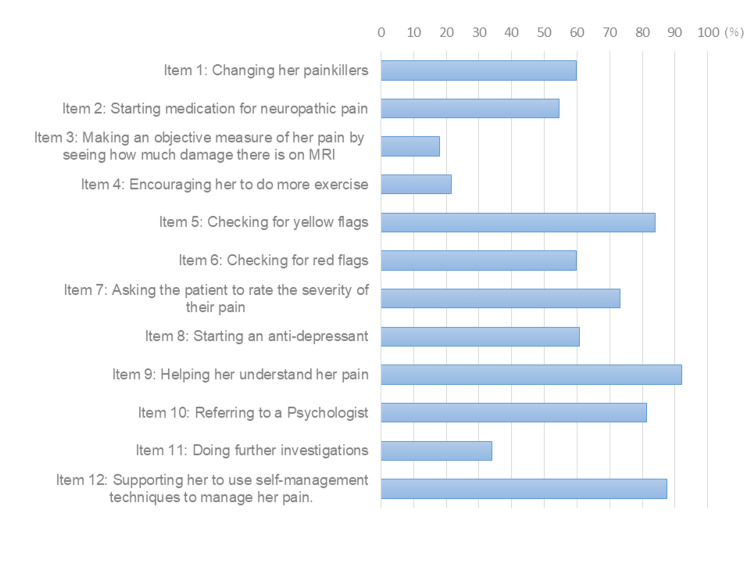
For the 112 participants, the mean (SD) for part one of the PUnCQ was 7.3 (1.6), and correct response rates are presented for each item in Figure 1. In particular, items 3, 4, and 11 had a correct response rate of less than 40%. The mean (SD) for part two of the PUnCQ was 5.2 (2.0). The mean (SD) for KNAP was 81.1 (6.3).
Figure 1. Response distributions of the 112 participants in part one of the PUnCQ.
PUnCQ, Pain Understanding and Confidence Questionnaire
The results of the confirmatory factor analysis are summarized in Table 2. Part one of the PUnCQ met all six criteria for unidimensionality, while part two met only one. Consequently, an exploratory factor analysis was conducted for part two. The results revealed two-factor structures (Table 3) (Kaiser-Meyer-Olkin measure = 0.933 and p < 0.001 in Bartlett’s sphericity test). The first factor, comprising 14 items, was labeled “pain management,” and the second factor, comprising seven items, “medication guidance and pain mechanism.” Cronbach’s alpha for the first and second factors and all items was 0.98, 0.93, and 0.98, respectively, indicating acceptable internal consistency.
Table 2. Results of the confirmatory factor analysis.
* Satisfied with the predetermined unidimensionality criteria
ADFI, adjusted goodness-of-fit index; CFI, comparative fit of index; CMIN/df, chi-squared/degree of freedom; GFI, goodness-of-fit index; PUnCQ, Pain Understanding and Confidence Questionnaire; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual
| PUnCQ | CMIN/df | CFI | GFI | ADFI | RMSEA | SRMR |
| Part 1 | 0.868* | 1.000* | 0.935* | 0.906* | <0.001* | 0.070* |
| Part 2 | 4.516 | 0.778 | 0.545 | 0.444 | 0.178 | 0.068* |
Table 3. Factor loading in part two of the PUnCQ.
PUnCQ, Pain Understanding and Confidence Questionnaire
| Item description | Factor 1 | Factor 2 |
| Be able to help her understand that psychological factors influence an individual’s pain experience and pain behaviors in both acute and chronic pain. | 1.043 | -0.158 |
| Be able to help her understand that social factors influence an individual’s pain experience and pain behaviors in both acute and chronic pain. | 1.012 | -0.107 |
| In the absence of a clear diagnosis, provide useful information in a way that is helpful from her perspective and will allow her to move toward self-management. | 1 | -0.089 |
| Be able to help her understand that biological factors influence an individual’s pain experience and pain behaviors in both acute and chronic pain. | 1 | -0.088 |
| Signpost her with suitable information. | 0.843 | 0.071 |
| Explain the role of psychological interventions in pain management. | 0.825 | 0.11 |
| Know whether you should refer her for more specialist assessment. | 0.783 | 0.035 |
| Assess her understanding of pain and identify fears that may act as barriers to effective management. | 0.705 | 0.186 |
| Describe the role of pacing and activity management. | 0.687 | 0.167 |
| Discuss where self-management is a priority and should be encouraged and supported. | 0.675 | 0.254 |
| Conduct a comprehensive assessment of pain using valid and reliable tools. | 0.629 | 0.187 |
| List the common red flags associated with pain. | 0.529 | 0.349 |
| Describe the contribution of biological, psychological, and social factors to individual variation in pain perception, behavior, and expression. | 0.49 | 0.445 |
| Describe yellow flags and discuss their impact on the management of pain. | 0.485 | 0.436 |
| Differentiate between physical dependence, substance use disorder, misuse, tolerance, addiction, and nonadherence. | -0.062 | 0.859 |
| Explain the strengths and weaknesses of the World Health Organization analgesic ladder. | -0.064 | 0.78 |
| Explain the principles of gate control theory and the concepts of pain modulation and neuroplasticity. | 0.058 | 0.703 |
| Explain the main structures involved in pain and how they interact in the pain experience. | 0.224 | 0.701 |
| Diagnose the differences between nociceptive pain and neuropathic pain. | 0.227 | 0.639 |
| Explain analgesic effects, side effects, and their management. | 0.391 | 0.514 |
| Recognize commonly used definitions of pain and be able to describe the implications of these definitions for the patient, e.g., central sensitization, allodynia, and hyperalgesia. | 0.436 | 0.44 |
As hypothesized, the correlation between KNAP and part one of PUnCQ was significant (p = 0.006), with an r-value of 0.26 (95% CIs, 0.08-0.42). Similarly, the correlation between KNAP and part two of PUnCQ was significant (p < 0.001), with an r-value of 0.41 (95% CIs, 0.25-0.56).
Discussion
This cross-cultural validity study investigated the structural and construct validity of the PUnCQ, which has the potential to assess an aspect of the clinical competence in pain management of Japanese physical therapists. The confirmatory factor analysis indicates that part one of the PUnCQ met all criteria for unidimensionality, indicating structural validity. However, doubts arose for part two regarding unidimensionality. Exploratory factor analysis for part two revealed a two-factor structure: a 14-item Factor 1 labeled “pain management” and a seven-item Factor 2 labeled “medication guidance and pain mechanism.” This finding may reflect that Japanese physical therapists do not receive pharmacology education. Although internal consistency for all items in part two was acceptable and the average of all items may be used for international comparisons, the average of both factors’ means may be reasonable when comparisons within the Japanese population are designed. Additionally, partial confirmation of the construct validity of PUnCQ was achieved.
Concerning PUnCQ scores, a study involving various professions, including students in Scottish physical therapy graduate programs and undergraduate nursing students (n = 2,238), reported a median of 4 for PUnCQ part one [11]. In contrast, a survey targeting undergraduate final-year physical therapy students in Scotland (n = 133) [10] reported that at least 50% of students selected the correct answer in almost all aspects. The mean score in this study for part one was 7.3, potentially aligning closely with the latter study’s data. However, items 3, 4, and 11 had a correct response rate of less than 40%, which may indicate a biomedical perspective on pain. These results may indicate the need to promote the education of Japanese physical therapists on the importance of the biopsychosocial perspective. For part two of the PUnCQ, the former previous study [11] reported average scores of 3.7 to 6.3, while the latter previous study [10] reported scores between 4 and 7. This study’s average score of 5.2 appears to approximate values from both previous studies. Although data suggest that the knowledge and understanding of pain among Japanese physical therapists may be lower than in advanced countries [26,27], this study includes a cohort of certified physical therapists in the McKenzie method, known for higher adherence to evidence-based practice [28], potentially contributing to the overall PUnCQ scores and resembling those in Scotland.
Regarding implications for physical therapy practice, this study enabled scoring PUnCQ, allowing us to move on to the final step of the questionnaire establishment process per the COSMIN. Thus, future research should verify the reliability and responsiveness of utilizing PUnCQ as a tool for assessing the effectiveness of educational interventions. Further, it is now possible to use the PUnCQ part one to identify relevant factors to enhance a certain competence in evidence-based clinical decision-making in relation to pain.
Several limitations exist in this study. First, the convenience sampling method introduces self-selection bias. However, since this is an anonymous survey, it is not assumed that only those who are confident in their pain management participated in this study, and therefore it is not believed that this limitation will significantly influence the results of this study. Second, the study used an adequate sample size according to COSMIN guidelines [14], but larger sample sizes would be desirable for a more accurate construct validity assessment. Third, the sample was limited to physical therapists, yet PUnCQ can be applied across various professions. Future research should consider larger multidisciplinary samples to assess the questionnaire’s validity. Fourth, the results of this study were obtained for Japanese physical therapists, and it is unclear whether similar internal structures are found among physical therapists in other countries. When using the PUnCQ in other countries, it would be necessary to confirm the internal structure, as in this study. Fifth, the clinical vignettes used in this study addressed disability related to whiplash injuries, and it is unclear whether the PUnCQ part 1 scores accurately reflect the competence of managing a variety of patients with pain, and further research is needed.
Conclusions
This study confirmed the structural validity of the PUnCQ and partially supported its construct validity. While additional steps and further research are needed to establish the questionnaire according to COSMIN guidelines and to assess its applicability in other countries, the PUnCQ holds the potential for evaluating educational outcomes and the quality of Japanese physical therapists in the future.
Acknowledgments
This study used data that were collected as part of a research project conducted by the Japanese Society of Allied Health and Rehabilitation. The fee for the mail survey was covered by the Japanese Society of Allied Health and Rehabilitation. The author also acknowledges the McKenzie Institute International Japan branch for assistance in data collection.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Ethics Committee of the Saitama Prefectural University issued approval 23100. This study was approved by the Ethics Committee of Saitama Prefectural University on November 7, 2023.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Hiroshi Takasaki
Acquisition, analysis, or interpretation of data: Hiroshi Takasaki
Drafting of the manuscript: Hiroshi Takasaki
Critical review of the manuscript for important intellectual content: Hiroshi Takasaki
References
- 1.What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Lin I, Wiles L, Waller R, et al. Br J Sports Med. 2020;54:79–86. doi: 10.1136/bjsports-2018-099878. [DOI] [PubMed] [Google Scholar]
- 2.Research priorities in the mechanical diagnosis and therapy among diploma therapists: an international Delphi study. Chiba H, Handa Y, Kikkawa K, Takasaki H. Cureus. 2024;16:0. doi: 10.7759/cureus.62492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health care provider's attitudes and beliefs towards chronic low back pain: the development of a questionnaire. Ostelo RW, Stomp-van den Berg SG, Vlaeyen JW, Wolters PM, de Vet HC. Man Ther. 2003;8:214–222. doi: 10.1016/s1356-689x(03)00013-4. [DOI] [PubMed] [Google Scholar]
- 4.Unraveling the barriers to reconceptualization of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. Moseley L. J Pain. 2003;4:184–189. doi: 10.1016/s1526-5900(03)00488-7. [DOI] [PubMed] [Google Scholar]
- 5.How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. Catley MJ, O'Connell NE, Moseley GL. J Pain. 2013;14:818–827. doi: 10.1016/j.jpain.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Pain neurophysiology knowledge enhances attitudes toward biopsychosocial management of low back pain among Japanese physical therapists. Mikamo Y, Takasaki H. Prog Rehabil Med. 2021;6:20210039. doi: 10.2490/prm.20210039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Effectiveness of pain neurophysiology education on musculoskeletal pain: a systematic review and meta-analysis. Bülow K, Lindberg K, Vaegter HB, Juhl CB. Pain Med. 2021;22:891–904. doi: 10.1093/pm/pnaa484. [DOI] [PubMed] [Google Scholar]
- 8.A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: short-and long-term outcomes of pain and disability. Wood L, Hendrick PA. Eur J Pain. 2019;23:234–249. doi: 10.1002/ejp.1314. [DOI] [PubMed] [Google Scholar]
- 9.Assessing future health care practitioners' knowledge and attitudes of musculoskeletal pain; development and measurement properties of a new questionnaire. Beetsma AJ, Reezigt RR, Paap D, Reneman MF. Musculoskelet Sci Pract. 2020;50:102236. doi: 10.1016/j.msksp.2020.102236. [DOI] [PubMed] [Google Scholar]
- 10.National survey of knowledge and confidence related to pain management of final year physiotherapy students. Seenan C, Harrison H, McParland J, et al. Physiotherapy. 2017;103:135–136. [Google Scholar]
- 11.How do the attitudes, confidence, knowledge and understanding differ in pre-registration healthcare students towards treating people with chronic pain: an observational, cross-sectional study. Carroll SP, Augeard N, Tennant J, Seenan C. Eur J Physiother. 2021;23:1–8. [Google Scholar]
- 12.Core competencies for pain management: results of an interprofessional consensus summit. Fishman SM, Young HM, Lucas Arwood E, et al. Pain Med. 2013;14:971–981. doi: 10.1111/pme.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.London: British Pain Society; [ Feb; 2024 ]. 2018. A Practical Guide to Incorporating Pain Education into Pre-registration Curricula for Healthcare Professionals in the UK. [Google Scholar]
- 14.Mokkink LB, Prinsen C, Patrick DL, et al. COSMIN methodology for systematic reviews of patient-reported outcome measures (PROMs) [ Feb; 2024 ]. 2018. https://cosmin.nl/wp-content/uploads/COSMIN-syst-review-for-PROMs-manual_version-1_feb-2018.pdf. https://cosmin.nl/wp-content/uploads/COSMIN-syst-review-for-PROMs-manual_version-1_feb-2018.pdf [DOI] [PMC free article] [PubMed]
- 15.A Japanese version of the Patient Attitudes and Beliefs Scale for patients with musculoskeletal disorders. Takasaki H, Hall T. Physiother Theory Pract. 2020;36:1438–1446. doi: 10.1080/09593985.2019.1571143. [DOI] [PubMed] [Google Scholar]
- 16.Cross-cultural adaptation of the 12-item Örebro musculoskeletal screening questionnaire to Japanese (ÖMSQ-12-J), reliability and clinicians' impressions for practicality. Takasaki H, Gabel CP. J Phys Ther Sci. 2017;29:1409–1415. doi: 10.1589/jpts.29.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Possible solutions to enhance evidence-based practice proposed by rehabilitation professionals in Japan: a Delphi study. Takasaki H, Ueno T. J Phys Ther Sci. 2023;35:31–39. doi: 10.1589/jpts.35.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rasch analysis of self-reported adherence to patient-centered physical therapy scale among Japanese physical therapists: cross-sectional study. Takasaki H. Int J Environ Res Public Health. 2021;18:10282. doi: 10.3390/ijerph181910282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Development and validity assessment of a Japanese version of the Exercise Adherence Rating Scale in participants with musculoskeletal disorders. Takasaki H, Kawazoe S, Miki T, Chiba H, Godfrey E. Health Qual Life Outcomes. 2021;19:169. doi: 10.1186/s12955-021-01804-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cross-cultural adaptation of the pain understanding and confidence questionnaire into Japanese. Takeuchi R, Sugiura S, Miki T, Chiba H, Handa Y, Takasaki H. J Phys Ther Sci. 2023;35:624–627. doi: 10.1589/jpts.35.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cross-cultural adaptation of the knowledge and attitude of pain into Japanese and test-retest reliability in undergraduate students. Tanuma T, Takasaki H. Prog Rehabil Med. 2022;7:20220030. doi: 10.2490/prm.20220030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Schermelleh-Engel K, Moosbrugger H, Müller H. Method Psych Res. 2003;8:23–74. [Google Scholar]
- 23.Confirmatory factor analysis of the Japanese Health Locus of Control scales among people with musculoskeletal disorders. Nemoto S, Miki T, Kondo Y, Takasaki H. J Phys Ther Sci. 2023;35:7–11. doi: 10.1589/jpts.35.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Confirmation of the unidimensionality of the satisfaction and recovery index among those with various musculoskeletal disorders. Takasaki H, Ishida S. Cureus. 2024;16:0. doi: 10.7759/cureus.62501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Costello A, Osborne JW. Pract Assess Res Evaluation. 2005;10:1–9. [Google Scholar]
- 26.Research activities contributing to evidence-based practice implementation in Japanese rehabilitation professionals. Mizuno H, Ueno T, Takasaki H. J Phys Ther Sci. 2023;35:340–345. doi: 10.1589/jpts.35.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Use of the Physiotherapy Evidence Database (PEDro) in Japan. Takasaki H PhD, Elkins MR PhD, Moseley AM PhD. Phys Ther Res. 2016;19:58–66. doi: 10.1298/ptr.e9881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKenzie therapists adhere more to evidence-based guidelines and have a more biopsychosocial perspective on the management of patients with low back pain than general physical therapists in Japan. Takasaki H, Saiki T, Iwasada Y. Open J The Rehab. 2014;2:173–181. [Google Scholar]