Abstract
Persistent subretinal fluid (PSF) after scleral bucking of rhegmatogenous retinal detachment may delay recovery and affect the final visual quality, but with no effective treatment. This study firstly investigated the safety and efficacy of 577 nm yellow subthreshold micropulse laser (SML) on PSF after scleral bucking surgery. This double-masked randomized clinical trial was conducted from December 2020 to October 2022 at Chongqing Aier Eye Hospital. Participants with PSF last for 1 month after scleral bucking surgery with break closed and retina reattachment were recruitment. These participants were treated by 577 nm yellow SML or sham treatment. Funduscopy, optical coherence tomography (OCT) volume change, best corrected vision acuity (BCVA) and visual field test were evaluated for six mouths follow-up. A total of 24 participants were randomized into SML group or Sham group equally. Compared with Sham group, the OCT volume within 6 mm of macular fovea was significantly less in SML group 6 months after therapy (P = 0.048). There were no statistically significant differences of OCT volume at 1, 2 and 3 months from baseline between groups. BCVA of ETDRS letters had no statistically significant difference. Pattern Standard Deviation amelioration (P = 0.039) had statistically significance in SML group compared with Sham group. There were no complications in the 2 groups. These preliminary findings suggest that 577 nm yellow SML therapy could accelerate PSF absorption after scleral bucking surgery.
Trial registration: Chinese Clinical Trial Registry No. ChiCTR2000037838, 02/09/2020, https://www.chictr.org.cn/showproj.html?proj=51885.
Keywords: Subthreshold micropulse laser, Persistent subretinal fluid, Scleral bucking, Safety, Efficacy
Subject terms: Retinal diseases, Randomized controlled trials
Introduction
Persistent subretinal fluid (PSF) after scleral bucking (SB) of rhegmatogenous retinal detachment (RRD) was firstly observed by Robertson1. It was widely reported by the introduction of optical coherence tomography (OCT)2. The incidence rate of PSF varied because of different sample size, demographics and follow-up intervals3. The etiology and risk factors are multiple and unclear4. But PSF after RRD repair surgery may delay recovery and affect the final visual quality.
Subthreshold micropulse laser (SML), a modality of tissue-sparing therapy, specially targets on retina pigment epithelium (RPE) with its ON–OFF intervals5. Different than visible burned scar of traditional threshold laser, SML avoids the drawbacks of standard retinal laser by sparing energy and specific retinal targets6. A growing body of evidence showed that 577 nm yellow light was not absorbed by lutein and zeaxanthin, thus it is widely applied to treat retinal disorder such as central serous chorioretinopathy (CSC) and diabetic macular edema (DME) to reinforce drainage fluid under and inside retina.
In this study, it was evaluated the safety and efficacy of 577 nm yellow SML on fluid absorption and visual function recovery of PSF after RRD surgery.
Methods
This is a prospective study approved by the Ethics Committee of Chongqing Aier Eye Hospital (IRB2020004) and followed by Declaration of Helsinki, registered in the Chinese Clinical Trial Registry (ChiCTR2000037838). Informed consent was obtained from participants, whose PSF did not absorbed within 1 month after SB surgery, from December 2020 to October 2022 at Chongqing Aier Eye Hospital, Chongqing, China. Inclusion criteria: age over 18 years old; PSF lasts over 1 month after scleral bucking surgery with break closed and retina reattachment. And exclusion criteria: pregnancy; oculus fundus could not be seen clearly due to cloudy dioptric medium; Patients requiring treatment due to trauma, tumor, severe bleeding, endophthalmitis and other diseases during follow-up.
This study was designed as a non-inferiority double-masked randomized clinical trial. The main efficacy evaluation index was OCT volume within 6 mm of macular fovea. The target of SML group was set as 8.5 mm3, and 9 mm3 in Sham group, and standard deviation was set as 0.5 mm3. The non-inferiority margin was -0.1, α = 0.025, and the test power was 80%, dropout rate set as 10%, The ratio of the two groups was listed as 1:1. The minimal sample size was 12 eyes each group. Randomization number table was generated by an online random number generator to assign participants to either SML group or Sham group with block size of 4. Allocation codes were sealed in sequentially numbered opaque envelops. Two doctors who performed the laser therapy and the Supervision verified the group allocation. Participants were allocated into SML group and Sham group according to random number table. Two doctors applied SML or Sham treatment according to random number table over the follow-up. Participants and other researchers were blinded to patient groupings.
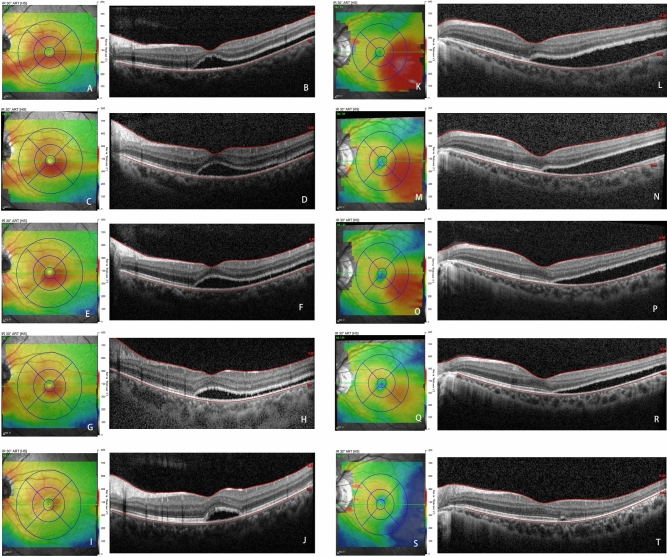
Supra Scan 577 nm micropulse laser (Quantel Medical, France) was applied to perform photocoagulation in SML group. Threshold of micropulse laser was titrated outside the vascular arch in each therapy. Initial parameter set as 50mW power value with 200 μm diameter spot and a pulse duration of 200 ms. The power was increased 10mW once emission, the spot moved aside simultaneously. A barely visible white spot was defined as the symbol of threshold value. Subthreshold micro pulse laser was switched the power to four times of the titrated threshold value and 5% duty cycle. Treatment performed on the area of subretinal fluid existing by multiple spot laser exposure with no space. Laser repeated if subretinal fluid existed persistent by OCT scan once a month up to 3 times (Fig. 1). Sham group did not receive SML with the laser switch-off or any other treatment.
Fig. 1.
Representative picture of SLO showed the hole was closed on the bucking ridge and retina reattachment (A). And OCT scan showed subretinal fluid existed in temporal area (C and D). The diagrammatic drawing showed subthreshold micropulse laser point shot in matrix pattern with no space (red points) in the SRF area (temporal of black line) (B).
All participants’ follow-up last for 6 months with one mouth interval for the first three mouth and three mouths for the last visit. Slit lamp funduscopy and Scanning Laser Ophthalmoscopy (SLO) to ensure break closed and retina reattachment. OCT (Heidelberg Engineering, Germany) of the retina was applied to survey the resolution of subretinal fluid. Macular volume within 6 mm of macular fovea were measured. And the patterns of PSF were recorded as shallow diffuse, multiple blebs and bleb-like loculated pattern7.Best corrected vision acuity (BCVA) was recorded as ETDRS letters every follow-up. Visual Field (VF) (Zeiss Humphrey Instruments, Germany) with 30–2 SITA Standard was test for the first and last visit.
Baseline characteristics were described as means and SDs for continuous variables with normal distribution and frequency for categorical variables. The normality of continuous data’s distribution was checked by Shapiro–Wilk test. All missing data were imputed by EM test with 25 copies of the data. Two sample t tests were conducted to estimate continuous variables, and frequency for categorical variables was analyzed by the χ2 test or Fisher exact test. Statistical analyses were performed using SPSS 22.0 software. Statistical significance was set at P < 0.05.
Results
A total of 24 eyes from 24 participants were randomized into SML group or Sham group (Fig. 2). The median age of these participants was 29.08 ± 10.50 and 31.67 ± 10.59 years old in SML group and Sham group. A total of 9 participants in SML group and 9 in Sham group were men. There were 7 right and 5 left eyes in SML group, 5 right and 7 left eyes in Sham group. Most of rhegmatogenous retinal detachment were macular fovea involvement (Table 1). Among all participants, 8 visits (6.67%) were missing due to COVID-19 epidemic restriction and 1 was lost the last follow-up (0.83%) owing to refusal.
Fig. 2.
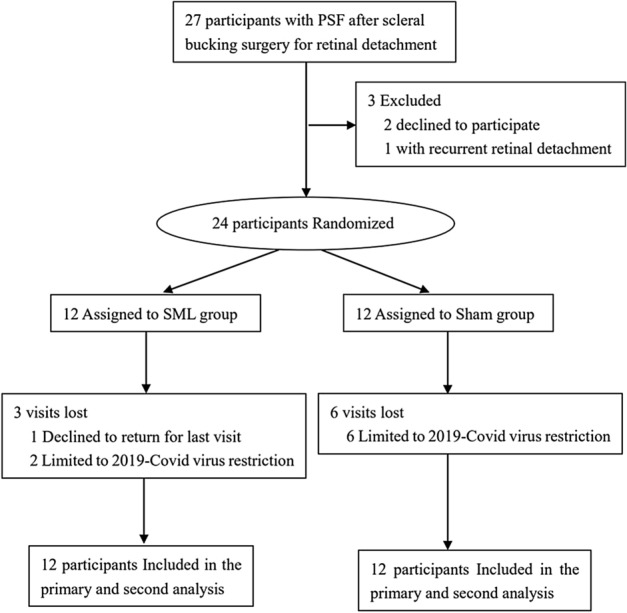
Participants Flow Diagram.
Table 1.
Demographic characteristics of participants.
| Variable | SML group(n = 12) | Sham group(n = 12) |
|---|---|---|
| Eye, No | 12 | 12 |
| Age, y | 29.08 ± 10.50 | 31.67 ± 10.59 |
| Sex, No. (%) | ||
|
Male Female |
7(37.5%) 5(12.5%) |
7(37.5%) 5(12.5%) |
| Laterality, No.(%) | ||
|
Right Left |
7(29.2%) 5(20.8%) |
5(20.8%) 7(29.2%) |
| Macular fovea involvement | ||
|
Yes No |
10(41.7%) 2(8.3%) |
11(45.8%) 1(4.2%) |
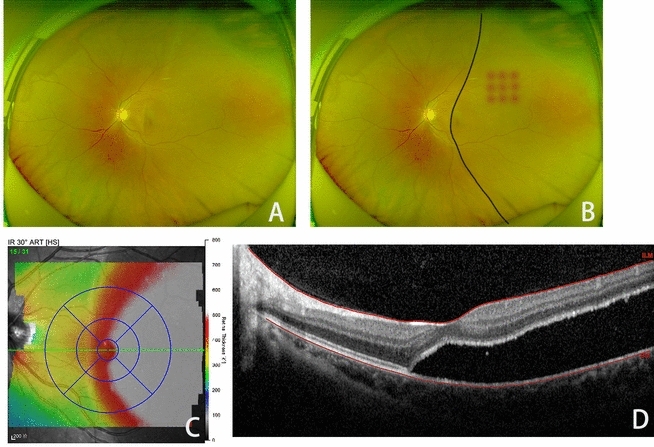
The baseline OCT volume within 6 mm of macular fovea was 10.44 ± 1.66 mm3 and 10.83 ± 1.90 mm3 in SML group and Sham group respectively (P = 0.598, 95%CI: − 1.90,11.12). Those volume were decreased 1, 2, 3 months after baseline visit respectively, with more decreased volume in SML group than Sham group but with no statistical significance. The volume in OCT of last visit, 6 months after baseline visit, was significantly less in SML group (8.27 ± 0.64 mm3) than Sham group (8.91 ± 0.84 mm3) (P = 0.048, 95%CI: − 1.27, − 0.01) (Table 2). At baseline PSF shew shallow diffuse pattern (11 for each group) or multiple blebs (One for each group). After 6 months for the last visit, 4 eyes (33.3%) in SML group and 5 eyes (41.7%) in Sham group have completed resolution of macular subretinal fluid, 3 in SML group and 1 in Sham group were multiple blebs, 2 in SML and 3 in Sham group were bleb-like loculated pattern, and there were 3 in each group showing shallow diffuse pattern (P > 0.05). In this study, there were 5 patients with average retinal thickness above 400um in OCT within Circle Diameters 1, 3, 6 mm ETDRS grids at baseline. Of these, there was each one patient in SML and Sham group with PSF absorption completely after 6 months follow-up. Until last visit, there was one in SML and 2 in Sham group with SRF absorption not completely (Fig. 3).
Table 2.
OCT volume(mm3) within 6 mm of macular fovea.
| SML group(n = 12) | Sham group(n = 12) | P (95% CI)* | |
|---|---|---|---|
| Baseline visit | 10.44 ± 1.66 | 10.83 ± 1.90 | 0.598(− 1.90,1.12) |
| 1 month | 9.63 ± 1.35 | 9.63 ± 1.59 | 0.999(− 1.25,1.25) |
| 2 months | 9.34 ± 1.00 | 9.50 ± 1.25 | 0.730(− 1.12,0.80) |
| 3 months | 9.01 ± 0.77 | 9.35 ± 1.31 | 0.444(− 1.26,0.58) |
| 6 months | 8.27 ± 0.64 | 8.91 ± 0.84 | 0.048(− 1.28,− 0.01) |
* Two-sample t test was used.
Fig. 3.
Representative pictures of OCT scan showed baseline SRF in Sham group (A and B) and SML group (K and L). After once a mouth therapy, SRF was absorbed quickly (M-R) in SML group, and barely remained in the last visit of six months after baseline (S and T). But SRF absorption in Sham group was slower than SML group (C–H), and still remained a bled under macular (I and J).
BCVA was 66.83 ± 11.91 ETDRS letters in SML group and 64.92 ± 10.20 letters in Sham group at baseline visit (P = 0.676, 95%CI: -7.47,11.30). BCVA improved in each visit during the follow up, with more ETDRS letters in SML group than Sham group but no statistically significant difference. Six months after baseline, BCVA reached into 75.39 ± 10.49 and 72.50 ± 9.17 ETDRS letters in SML and Sham group, respectively (P = 0.4479, 95%CI: -5.45,11.24) (Table 3). Until last visit, there were 10 participants in SML group and 7 in Sham group with BCVA improving ≥ 5 letters (P > 0.05), and 4 in each group with BCVA improving ≥ 10 letters (P > 0.05) from baseline visit. All BCVA of SML group were improved in SML group. Only 1 participant in Sham group decreased 3 letters on last visit.
Table 3.
Follow-up BCVA (ETDRS letters) of Participants.
| SML group(n = 12) | Sham group(n = 12) | P (95% CI)* | |
|---|---|---|---|
| Baseline visit | 66.83 ± 11.91 | 64.92 ± 10.20 | 0.676(− 7.47,11.30) |
| 1 month | 71.50 ± 10.77 | 67.58 ± 9.72 | 0.359(− 4.77,12.61) |
| 2 months | 73.83 ± 9.09 | 68.27 ± 8.78 | 0.141(− 2.00,13.14) |
| 3 months | 74.60 ± 9.41 | 70.44 ± 8.68 | 0.272(− 3.50,11.84) |
| 6 months | 75.39 ± 10.49 | 72.50 ± 9.17 | 0.479(− 5.45,11.24) |
* Two-sample t test was used.
BCVA, Best-corrected visual acuity.
Visual Field Index (VFI) of the baseline VF was 89.69 ± 8.48% in SML group and 86.33 ± 9.84% in Sham group. Mean Deviation (MD) of the baseline VF was − 6.11 ± 2.83 dB in SML group and − 7.55 ± 4.31 dB in Sham group. Pattern Standard Deviation (PSD) of the baseline VF was 4.62 ± 1.94 dB in SML group and 4.50 ± 1.79 dB in Sham group. Those indexes had no statistically difference between groups. But it was significant ameliorated in PSD (P = 0.039, 95%CI: − 2.29, − 0.06) for the difference between baseline and last visit in SML compared with Sham group (Table 4).
Table 4.
Visual field of participants.
| SML group(n = 12) | Sham group(n = 12) | P (95% CI)* | |
|---|---|---|---|
|
VFI baseline 6 months ΔVFI |
89.69 ± 8.48% 92.88 ± 4.60% 3.21 ± 4.87% |
86.33 ± 9.84% 90.60 ± 7.93% 4.26 ± 11.11% |
0.381(− 4.42,11.13) 0.398(− 3.21,7.77) 0.767(− 8.32,6.21) |
|
MD (dB) baseline 6 months ΔMD |
− 6.11 ± 2.83 − 4.94 ± 1.88 1.18 ± 1.88 |
− 7.55 ± 4.31 − 5.96 ± 3.79 1.59 ± 4.13 |
0.345(− 1.65,4.53) 0.411(− 1.51,3.56) 0.755(− 3.13,2.30) |
|
PSD (dB) baseline 6 months ΔPSD |
4.62 ± 1.94 3.44 ± 1.36 − 1.18 ± 1.38 |
4.50 ± 1.79 4.50 ± 1.74 − 0.00 ± 1.24 |
0.880(− 1.46,1.70) 0.110(− 2.38,0.26) 0.039(− 2.29, − 0.06) |
* Two-sample t test was used.
VFI: Visual field index. MD: Mean deviation. PSD: Pattern standard deviation.
Side effects and sequelae barely occurred. None of participants complained pain, but metamorphopsia and dimness ameliorated. No visible laser spots were seen in the slit lamp fundoscopy, SLO nor OCT after SML treatment.
Discussion
It is the fate of PSF complete resolution after RRD surgery, but the period of fluid absorption may be a long span. Unintentional retinal displacement and retinal folds, which are two complications of PSF after RRD surgery, may lead to metamorphopsia. Overextended progress contributes to financial burden of follow-up and negative emotion to patients, and display more rate of disruption of the outer retinal layers even if final absorption completely8.
PSF occurs due to many factors, such as age, dysfunctional RPE, macular involvement RRD, longstanding RRD prior to surgery8. PSF not only happens in pars plana vitrectomy (PPV) but also in SB, and the higher incidence rate of PSF after SB maybe more completely drainage of subretinal fluid in PPV. Subretinal fluid increases density by the limited capacity of RPE to remove the cellular and protein components9. And the assistant pachychoroidopathy may also contribute to PSF10.
Pachychoroidopathy always happen in CSC. Similarity, in chronic CSC, PSF can cause irreversible damage to the photoreceptors leading to visual loss11. Clinic study confirmed 577 nm yellow SML treatment of chronic CSC was effective and safe12. It was also as effective as PDT in treating acute CSC by the changes in SRF, CFT, BCVA and central retinal sensitivity13. Verteporfin was high cost and had several side effects before suspend production. In contrast SML prior low-cost and safe, though the effect seems a finger’s breadth. Other than subretinal fluid height and width, choroidal thickness14, here we focused on PSF volume change after SB succeed, depending on automatic identification and calibration calculation of macular volume by OCT scan itself. That’s an inadequacy of this report, for the width of subretinal fluid could not be detected and choroidal thickness did not measure nor calculate. Further study may monitor these indicators by ultra-wide field OCT or OCTA.
It is considered RPE is the target of SML, which forms the outer blood retinal barrier and transports nutrients, ions, oxygen, wans water between neuroretina and choroid15. That’s why we chose this therapy to treat PSF after SB surgery. In this study, the OCT volume within 6 mm of macular fovea dramatically decreased six months after 577 nm SML therapy, demonstrated its function on RPE transportation. Also, morphology of PSF changed gradually, consistent with previous reports3. Though BCVA amelioration had no statistic difference between two groups, the trend was clear. That may be limited by small sample and short follow-up time. It’s a pity we did not apply the M-chart or Amsler test to evaluate the metamorphopsia in this preliminary study16. But it may suggest that SML ameliorated visual function by the statistically PSD decrease in SML group compared with Sham group, which may be a better indicator of localized field defects than MD in visual field17.
Standard retinal laser has been widely used for chorioretinal diseases such as DME, RVO, retina hole, neoplasm and some exudative diseases, by its photothermy and photocoagulation. But it was denounced of the visual field loss caused by chorioretinal scarring and progressive retinal atrophy. Subthreshold micropulse laser emits trains of repetitive ultrashort laser pulses so photocoagulation leaves the retinal cells intact while minimizing thermal effects on the neuroretina and choroid18,19. That’s why participants and researchers (except the two doctors applied SML and the supervision) were blinded to patient groupings, for no pain during micropulse working and no laser scar in ocular examination.
810 nm micropulse diode laser to create subthreshold lesion in pigmented rabbit retina, RPE cell heterogeneity with cell repair and growth limited collateral damage20. 577 nm subthreshold micropulse yellow laser can reduce flow deficit areas to promote choriocapillaris flow recovery in sCSC21. And it also has therapy on treatment of diabetic macular edema in ameliorating BCVA and CMT, as well as parafoveal vessel density and foveal avascular zone (FAZ) area15. The report about SML approach on adult Coat’s disease demonstrates its effective in resolution of macular oedema and modality for exudative22. 577 nm yellow subthreshold micropulse laser emerged a slight advantage in diabetic macular edema than 810 infrared light23.Yellow light is not absorbed by lutein and zeaxanthin, thus 577 nm laser can treat foveal without damage. So, it is safe and effective to apply 577 nm SML in retinal disorders with no complications15,24. Also in this study, 577 nm SML therapy in PSF after RRD surgery has no damage to the retina, VF and BCVA amelioration were consistent with metamorphopsia improved. Corresponding, morphology change of retina and structure of ellipsoid in OCT was restored as well as volume decrease.
The main mechanism of subthreshold micropulse laser is being studied. One theory is that SML stimulates RPE to product HSP, which could immunomodulate metabolism and function25. And AQP3, one of the aquaporin family, upregulated by subthreshold micropulse laser irradiation may retinal edema by drainage of subretinal fluid to choroidal26. Other cytokines such as VEGF down regulation and PEDF upregulation play anti-inflammatory effect as well as restoration the Muller cells and microglial cell function6,27. But it is unclear why the effecting of micropulse working on PSF absorption after SB surgery. It needs further studies in vivo and in vitro to test the microenvironment change and RPE function amelioration in the future.
This study was limited to sample size, short follow-up period and follow-up loss by 2019-Covid virus epidemic restriction. But the noninvasive safety of 577 nm SML brought out repeatable and economic therapy of PSF after SB succeed. This preliminary study was so sketchy. In further study, we’d like to recruit more patients, divide groups according to retinal thickness, and apply more tools to analyze the visual function amelioration about SML management PSF.
Conclusion
This preliminary report showed that the persistent subretinal fluid after scleral bucking absorption was accelerated by 577 nm SML treatment, corresponding with visual function ameliorated. Thus, this study documented the safety and efficacy of subthreshold micropulse yellow laser treatment for persistent subretinal fluid after scleral bucking.
Supplementary Information
Acknowledgements
With many thanks to Pro Xiangge He and Hongru Chen as scientific advisors during this research.
Author contributions
Z. Chen had full access to the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Z. Chen, Y. Wang, G. Wang, L. Liu. Administrative, technical, or material support: Y. Wang, G. Wang, L. Liu. Subthreshold micropulse laser therapy: J. Xie, Q. Wang. Acquisition and analysis of data: Z. Liu, Y. Wu, Y. Ma. Drafting of the manuscript: Z. Chen, Z. Liu. Supervision: M. Chen.
Funding
This study was supported by Science-Health Joint Medical Scientific Research Project of Chongqing (2021MSXM292) and Aier Eye Hospital Group Scientific Research Fund (AF2001D15).
Data availability
All data supporting the findings of this study are available within the paper and Supplementary Information.
Competing interests
The authors declare no competing interests.
Ethical approval
This is a prospective study approved by the Ethics Committee of Chongqing Aier Eye Hospital (IRB2020004) and followed by Declaration of Helsinki, registered in the Chinese Clinical Trial Registry (ChiCTR2000037838). Informed consent of participate and data publish without identifying information was obtained from participants.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-71528-7.
References
- 1.Veckeneer, M. et al. Persistent subretinal fluid after surgery for rhegmatogenous retinal detachment: hypothesis and review. Graefes Arch. Clin. Exp. Ophthalmol.250, 795–802 (2012). 10.1007/s00417-011-1870-y [DOI] [PubMed] [Google Scholar]
- 2.Hagimura, N., Iida, T., Suto, K. & Kishi, S. Persistent foveal retinal detachment after successful rhegmatogenous retinal detachment surgery. Am. J. Ophthalmol.133, 516–520 (2002). 10.1016/S0002-9394(01)01427-1 [DOI] [PubMed] [Google Scholar]
- 3.Fu, Y. et al. Natural history of persistent subretinal fluid following the successful repair of rhegmatogenous retinal detachment. Int. J. Ophthalmol.13, 1621–1628 (2020). 10.18240/ijo.2020.10.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kobayashi, M. et al. Influence of submacular fluid on recovery of retinal function and structure after successful rhegmatogenous retinal reattachment. PLoS ONE14, e0218216 (2019). 10.1371/journal.pone.0218216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frizziero, L. et al. Subthreshold micropulse laser modulates retinal neuroinflammatory biomarkers in diabetic macular edema. JCM10, 3134 (2021). 10.3390/jcm10143134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Midena, E. et al. Changes of aqueous humor müller cells’ biomarkers in human patients affected by diabetic macular edema after subthreshold micropulse laser treatment. Retina40, 126–134 (2020). 10.1097/IAE.0000000000002356 [DOI] [PubMed] [Google Scholar]
- 7.Fouad, Y. A., Habib, A. M., Sanders, R. N. & Sallam, A. B. Persistent subretinal fluid following successful rhegmatogenous retinal detachment surgery. Seminars Ophthalmol.37, 724–729 (2022). 10.1080/08820538.2022.2085516 [DOI] [PubMed] [Google Scholar]
- 8.Mimouni, M. et al. Persistent loculated subretinal fluid after rhegmatogenous retinal detachment surgery. Retina40, 1153–1159 (2020). 10.1097/IAE.0000000000002565 [DOI] [PubMed] [Google Scholar]
- 9.Long, K., Meng, Y., Chen, J. & Luo, J. Multifactor analysis of delayed absorption of subretinal fluid after scleral buckling surgery. BMC Ophthalmol.21, 86 (2021). 10.1186/s12886-021-01853-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chantarasorn, Y., Oellers, P. & Eliott, D. Choroidal thickness is associated with delayed subretinal fluid absorption after rhegmatogenous retinal detachment surgery. Ophthalmol. Retina3, 947–955 (2019). 10.1016/j.oret.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 11.Kertes, P. J. Retinal atrophy in idiopathic central serous chorioretinopathy. Evidence-Based Ophthalmol.4(1), 42–43 (2003). [Google Scholar]
- 12.Kim, Y. J. et al. Short-duration multiple-session subthreshold micropulse yellow laser (577 nm) for chronic central serous chorioretinopathy: results at 3 years. Eye (Lond)33, 819–825 (2019). 10.1038/s41433-018-0309-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeng, M., Chen, X., Song, Y. & Cai, C. Subthreshold micropulse laser photocoagulation versus half-dose photodynamic therapy for acute central serous chorioretinopathy. BMC Ophthalmol.22, 110 (2022). 10.1186/s12886-022-02331-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kayhan, B., Demir, N., Sevincli, S. & Sonmez, M. Electrophysiological and anatomical outcomes of subthreshold micropulse laser therapy in chronic central serous chorioretinopathy. Photodiagnosis Photodynamic Therapy41, 103221 (2023). 10.1016/j.pdpdt.2022.103221 [DOI] [PubMed] [Google Scholar]
- 15.Bonfiglio, V. et al. Efficacy and safety of subthreshold micropulse yellow laser for persistent diabetic macular edema after vitrectomy: a pilot study. Front. Pharmacol.13, 832448 (2022). 10.3389/fphar.2022.832448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nowomiejska, K. et al. M-charts as a tool for quantifying metamorphopsia in age-related macular degeneration treated with the bevacizumab injections. BMC Ophthalmol.13, 13 (2013). 10.1186/1471-2415-13-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park, K. H., Tomita, G., Liou, S. Y. & Kitazawa, Y. Correlation between peripapillary atrophy and optic nerve damage in normal-tension glaucoma. Ophthalmology103(11), 1899–1906 (1996). 10.1016/S0161-6420(96)30409-0 [DOI] [PubMed] [Google Scholar]
- 18.Chen, S.-N., Hwang, J.-F., Tseng, L.-F. & Lin, C.-J. Subthreshold diode micropulse photocoagulation for the treatment of chronic central serous chorioretinopathy with juxtafoveal leakage. Ophthalmology115, 2229–2234 (2008). 10.1016/j.ophtha.2008.08.026 [DOI] [PubMed] [Google Scholar]
- 19.Sivaprasad, S., Elagouz, M., McHugh, D., Shona, O. & Dorin, G. Micropulsed diode laser therapy: evolution and clinical applications. Surv. Ophthalmol.55, 516–530 (2010). 10.1016/j.survophthal.2010.02.005 [DOI] [PubMed] [Google Scholar]
- 20.Pollack, J. S., Kim, J. E., Pulido, J. S. & Burke, J. M. Tissue effects of subclinical diode laser treatment of the retina. Arch. Ophthalmol.116, 1633–1639 (1998). 10.1001/archopht.116.12.1633 [DOI] [PubMed] [Google Scholar]
- 21.Ho, M. et al. Analysis of choriocapillaris perfusion and choroidal layer changes in patients with chronic central serous chorioretinopathy randomised to micropulse laser or photodynamic therapy. Br. J. Ophthalmol.105, 555–560 (2021). 10.1136/bjophthalmol-2020-316076 [DOI] [PubMed] [Google Scholar]
- 22.Kumar, A., Kumar, P., Ambiya, V. & Mishra, S. K. Subthreshold micropulse laser for adult onset Coats’ associated exudative maculopathy. Eur. J. Ophthalmol.32(5), 29–31. 10.1177/11206721211005691 (2022). 10.1177/11206721211005691 [DOI] [PubMed] [Google Scholar]
- 23.Vujosevic, S. et al. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: morphologic and functional safety. Retina35, 1594–1603 (2015). 10.1097/IAE.0000000000000521 [DOI] [PubMed] [Google Scholar]
- 24.Gawęcki, M. Micropulse laser treatment of retinal diseases. J. Clin. Med.8, 242 (2019). 10.3390/jcm8020242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inagaki, K. et al. Sublethal photothermal stimulation with a micropulse laser induces heat shock protein expression in ARPE-19 cells. J. Ophthalmol.2015, 729792 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hirabayashi, K., Kakihara, S., Tanaka, M., Shindo, T. & Murata, T. Investigation of the therapeutic mechanism of subthreshold micropulse laser irradiation in retina. Graefes Arch. Clin. Exp. Ophthalmol.258, 1039–1047 (2020). 10.1007/s00417-020-04638-3 [DOI] [PubMed] [Google Scholar]
- 27.Midena, E. et al. Sub-threshold micropulse laser treatment reduces inflammatory biomarkers in aqueous humour of diabetic patients with macular edema. Sci. Rep.9, 10034 (2019). 10.1038/s41598-019-46515-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data supporting the findings of this study are available within the paper and Supplementary Information.