Abstract
CONCERN AND AWARENESS IS GROWING about the health effects of exposures to environmental contaminants, including those found in food. Most primary care physicians lack knowledge and training in the clinical recognition and management of the health effects of environmental exposures. We have found that the use of a simple history-taking tool — the CH2OPD2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs) — can help physicians identify patients at risk of such health effects. We present an illustrative case of a mother who is concerned about eating fish and wild game because her 7-year-old son has been found to have learning difficulties and she is planning another pregnancy. Potential exposures to persistent organic pollutants (POPs) and mercury are considered. The neurodevelopmental effects of POPs on the fetus are reviewed. We provide advice to limit a patient's exposure to these contaminants and discuss the relevance of these exposures to the learning difficulties of the 7-year-old child and to the planning of future pregnancies.
Case
A 27-year-old woman who lives in a town on the shore of Lake Huron wants to have a second child but has concerns. Her 7-year-old son is being assessed by the school psychologist for a learning disorder. She tells her family physician that she saw something on television about contaminants in fish affecting children's intelligence. She is worried that her diet may have caused her son's learning disorder and wants advice on how to protect her second child against environmental contaminants that may cause learning problems. Her past medical history is unremarkable. She is taking no medications other than folate (0.4 mg/d). She has had only the one pregnancy. Her pregnancy and delivery of her son were uncomplicated, and the boy met the developmental milestones. The concern about a learning disorder is recent. There is no family history of congenital anomalies, early deafness or twins. Her maternal grandmother had type 2 diabetes, and her father-in-law has hypertension; the rest of the family is healthy. Because the woman is worried about environmental exposures, you take an exposure history using the CH2OPD2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs)1 to identify possible sources of environmental contaminants (Table 1).
Table 1
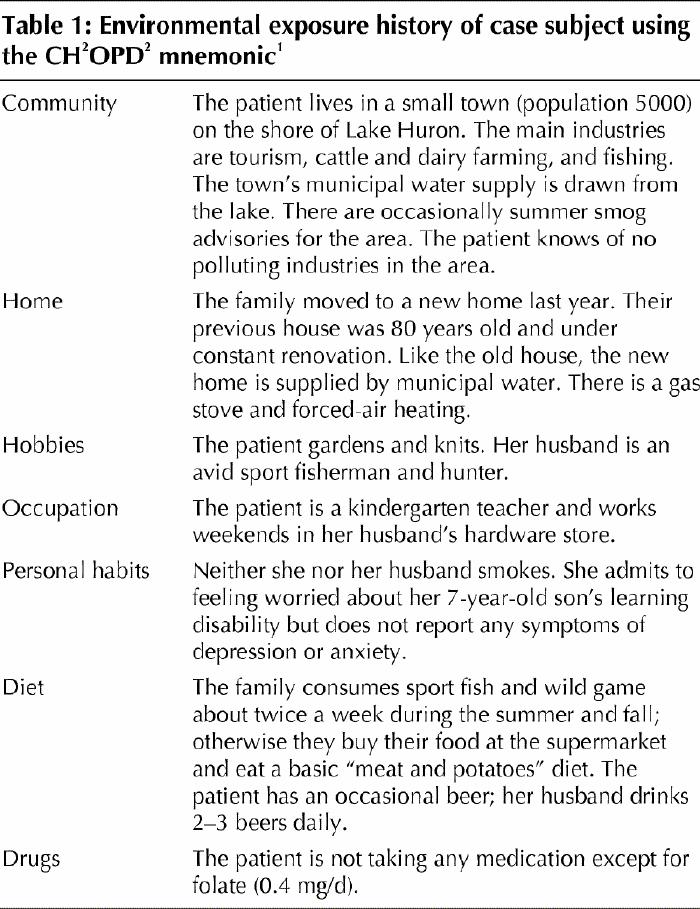
The environmental contaminants that can affect the neurobehavioural development of the fetus include metals (lead, mercury and manganese), nicotine, pesticides (e.g., organophosphates), dioxins, polychlorinated biphenyls (PCBs) and solvents (e.g., alcohol).2,3 In this article we focus on persistent organic pollutants (POPs) and mercury. These are the contaminants identified in the environmental exposure history of the case subject (Table 1). Although lead exposure was also noted in the exposure history (through renovating an 80-year-old home), it is discussed in an earlier article in this series.4
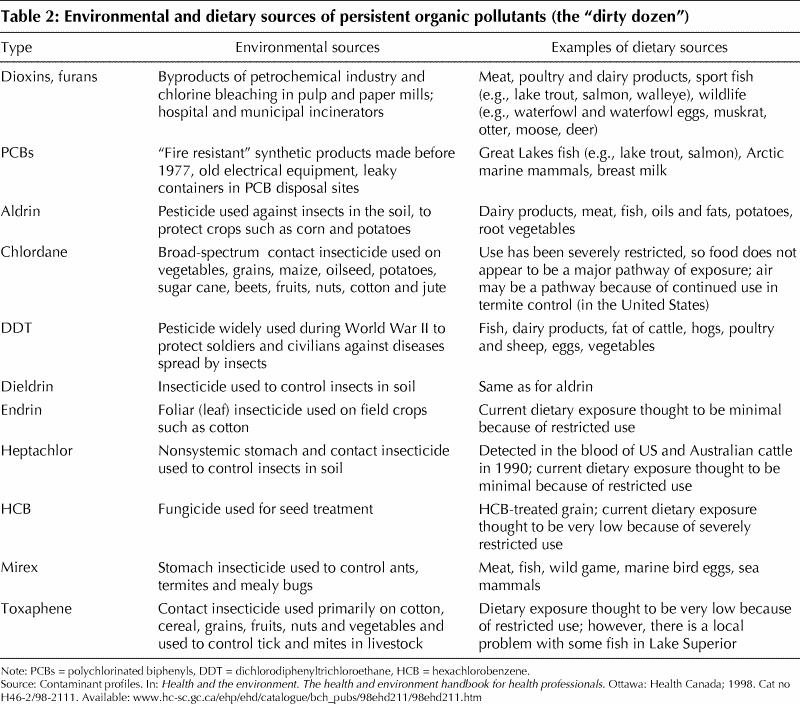
POPs are carbon-containing chemicals that share several properties. They are lipophilic, accumulating in the fat of living organisms, and increase in quantity up the food chain. Most are semivolatile, which means that they can travel in the air thousands of miles from their source before they settle. They resist photolytic, biological and chemical degradation and persist in the environment, taking as long as a century to degrade.5 Twelve POPs, including 9 pesticides, have been identified by the United Nations Environment Programme as powerful threats to the health of humans and wildlife and have been targeted for elimination (Table 2).6 In the 1970s many countries banned or severely restricted the use of the 9 pesticides and PCBs and implemented pollution control strategies to reduce the amount of dioxin and furan released in the environment. However, it is thought that all 9 pesticides and PCBs are still used in many countries today.
Table 2
Despite significant achievements in reducing the production and use of POPs, these pollutants remain ubiquitous, as evident by the global distribution of PCBs and organochlorine pesticides in butter samples from around the world.7 Most human exposure comes from dietary sources. POPs are ingested, stored in fatty tissue and excreted in feces and breast milk. The concentration of certain chemical contaminants in breast milk serves as an indicator of population exposure. From 1967 to 1992, there was a downward trend in the concentrations of organochlorine pesticides and PCB hydrocarbons in samples of Canadian breast milk during the phase-out of these chemicals.8 The estimated daily intake of PCBs from the current diet of the average Canadian is less than 1 μg/d.9
Although everyone is exposed to a background level of POPs, certain people may have higher levels of POPs exposure because of their eating habits. Some people eat more fish than the general population. Southeast Asian Canadians, Native Americans, sport anglers and hunters who regularly eat large amounts of Great Lakes fatty fish or wildlife from the top of the food chain, such as waterfowl and waterfowl eggs, turtles and turtle eggs, muskrat, otter, moose and deer, may be at risk of high exposure.10 Northern Aboriginals, such as the Inuit of Nunavik, who consume the fat of seals and beluga and narwhal whales, have been found to have higher body burdens of POPs.11,12
Health effects
Persistent organic pollutants
Concerns about the health effects of exposure to POPs arose initially from studies of wildlife communities that showed reproductive, developmental, endocrine, immunologic and carcinogenic effects.13,14,15 The wildlife in these communities had high rates of malformed genitalia, aberrant mating behaviour, sterility, cancer, and immune system and thyroid dysfunction. Toxicological and laboratory studies largely confirmed the links between POPs exposure and effects observed in these studies. There is growing evidence that some POPs act as endocrine disrupters, mimicking hormones by binding to or blocking hormone receptors.16,17,18,19
Neurodevelopmental, hematological, immunologic and reproductive effects have been found in animals at levels of exposure that overlap the range of exposures and body burdens found in humans.14 The health effects of POPs in humans is unclear, although available epidemiological evidence suggests they are similar to those in animals, affecting neurodevelopment,20,21,22 and thyroid,23 estrogen19 and immune function.15 The developing brain and nervous system may be most vulnerable. According to a landmark longitudinal study, babies whose mothers ate large amounts of highly contaminated fish (PCBs were measured) from Lake Michigan had lower birth weights, smaller head circumferences and shorter attention spans than babies whose mothers did not eat fish.24,25 Followed over 11 years, the exposed children have continued to do more poorly in a range of skills and development tests, including deficits in general intellectual functioning, short- and long-term memory, and attention span.26
A systematic review21 of the literature on the relation between neurological development in children and prenatal exposure to PCBs identified 7 studies, 2 of which evaluated children with high exposures. Abnormal reflexes were reported in all 4 studies that evaluated reflexes; delayed motor skills were identified in the first months of life among children in 4 of 5 studies that evaluated this area of development; and cognitive development was found to be affected in children at 4 years of age in 4 of 5 studies that looked at this aspect of development. The reviewers concluded that these studies suggested a subtle adverse effect of prenatal PCB exposure on child neurodevelopment. Because of limitations such as differences in study design, inconsistency in some results, a lack of comparable end points and the lack of adequate quantitative exposure data, the reviewers could not associate degree of risk with levels of exposure. Also, it is unclear to what extent postnatal exposure contributed to the children's outcomes, although the reviewers concluded that postnatal exposure to PCBs through breast-feeding was not clearly related to any effect on neurological development. This finding is consistent with the general recommendation that women should breast-feed even if they have chemical residues in their breast milk.27
Our understanding of the adverse health effects of exposure to POPs is limited by available research methods and measures of exposure and outcome. Methods of epidemiological studies to measure exposure may not be precise or valid.28 For example, contaminated fish contain a large number of putative neurotoxicants (methyl mercury, PCBs and pesticides), so it may not be possible to determine which contaminants might be responsible. PCB body burdens may simply reflect exposure to other fish-borne contaminants.29 A battery of tests have been developed to assess neurodevelopment and function, yet sensitive outcome measures for assessing neurobehavioural development in children relative to normative standards across a wide range of exposure levels are not currently available.30,31 Moreover, the nervous system develops in specific phases or stages, making it differentially vulnerable to chemical exposure. The conditions under which children are differentially sensitive are not well understood, although the weight of evidence suggests that exposure in utero has both transient and lasting effects.21,26,29
Methyl mercury
Mercury exists naturally in the environment, but levels have risen because of discharge from hydroelectric, mining, pulp and paper industries, incineration of municipal and medical waste, and from power plants, especially those using coal.32 Microbes in soils and in river and lake sediments convert elemental mercury into organic methyl mercury, which is more bioavailable. Methyl mercury concentrations increase in food chains, being highest in fish species at the top of the food chain, such as pike, walleye and bass in freshwater, and tuna, swordfish and shark in sea water.33 When ingested, almost all of the methyl mercury is absorbed. The half-life is about 44 days. Most methyl mercury is converted in inorganic mercury and excreted in feces.
There is good evidence in animal studies that exposure to methyl mercury in utero has neurotoxic effects.14 There is also good evidence that high-dose exposure to methyl mercury in utero in humans is neurotoxic. In the 1950s, in Minimata Bay, Japan, 1422 infants who appeared healthy at birth were later found to have mental retardation, disturbances of gait, speech, sucking and swallowing, and abnormal reflexes. Mercury was discovered to have been discharged into the bay from a factory. Mothers, who were asymptomatic, were exposed to high does of methyl mercury by eating fish from the bay, and their babies were exposed in utero.34 However, the human epidemiologic studies related to low-level methyl mercury exposure in utero remain controversial with respect to a threshold for significant effects. Lower level exposures from maternal consumption of fish have not been consistently associated with adverse neurodevelopmental outcomes in children.35,36
Clinical management
Environmental exposure to low levels of POPs and mercury is ubiquitous. The clinical challenge lies in identifying which patients are exposed to higher than average levels of these substances and who might reduce their exposure by changing their diet and lifestyle habits. Use of the CH2OPD2 mnemonic1 when taking an environmental exposure history can help physicians direct questions about possible exposures from the patient's community, home, hobbies, occupation, personal habits, drugs and diet. Specific questions pertaining to the patient's hobbies (e.g., Do you hunt game?), diet (e.g., Do you eat sport fish?) and personal history (e.g., Have you lived in the Arctic or on a native reserve?) can be used to identify patients with possibly high exposures to POPs and mercury.
The environmental exposure history of the case subject (Table 1) identifies some exposure for both the mother and her son to POPs such as PCBs and dioxin-like compounds and to mercury through the consumption of sport fish and wild game. Information on mercury and PCB levels in Lake Huron fish can be found in the Guide to Eating Ontario Sport Fish.37 Most provinces issue similar guides. The possible exposure to lead from lead-based paint (mobilized during renovations), contaminated soil and lead shot in game meat should be investigated by measuring blood lead levels in both the mother and the son (see the article on lead exposure in this series4).
Testing the mother's hair or blood for mercury levels may be indicated if she had consumed fish with high mercury levels37 just before or during her pregnancy with her son. Laboratory tests to measure in vivo levels of PCBs and organochlorine pesticides are available, but they are quite expensive and not widely used. Testing the current PCB and pesticide levels in the son is not indicated or relevant, because the evidence indicates that the neurodevelopmental effects related to PCBs are the result of in utero exposure.
The mother should be informed about the available scientific evidence and about the uncertainties. Existing scientific evidence of ecological correlations observed in populations between loss of intellectual potential and exposure to specific PCBs cannot be extrapolated to individual cases. Of public health concern is the average shift in the distribution curve of intellectual capacity in the population as a whole.3,14 It is unlikely that the in utero exposure of the woman's son to PCBs and mercury from the mother's consumption of Great Lakes fish would have been large enough to produce clinically significant neurodevelopmental effects on its own. The effect, if any, would instead have been a subtle reduction in the son's learning potential. The onset of learning difficulties at age 7 suggests the involvement of other factors. A full case assessment should address other determinants of child development, including psychosocial, biological, genetic and nutritional.
Whether the patient should delay her second pregnancy should be discussed with the physician. A waiting period would not significantly reduce her PCB or dioxin body burdens, because of their persistence. She should be advised to follow the latest edition of the Guide to Eating Ontario Sport Fish.37 She should also reduce or avoid consumption of other wildlife, which can be contaminated with organochlorines, methyl mercury or lead from lead shot. However, waiting 3 to 6 months would significantly reduce her mercury body burden if further exposure is avoided, and therefore reduce the exposure of her fetus to mercury.
Prevention
The risks of eating contaminated fish must be balanced against the benefits. The health policy message is that most fish are highly nutritious and safe to eat.10 Fish are high in protein and unsaturated fatty acids. Women of child-bearing age and parents with young children should be advised to obtain a copy of their province's guide to eating sport fish.37,38 Mercury levels in fish are site-specific. Lake trout and salmon are the primary species with high concentrations of PCBs.
The tables in the Ontario guide to eating sport fish give size-specific consumption advice for each species of fish tested from many locations.37 This advice is based on health protection guidelines developed by Health Canada.39 The use of cleaning and cooking methods that can substantially reduce the exposure to fat-soluble contaminants in a fish meal should be used.10,37 Store-bought fish are routinely tested for contaminants to ensure that they meet Canadian standards. Health Canada recommends that women of child-bearing age and children should not consume more than 1 or 2 meals of shark, swordfish or fresh tuna (not canned tuna) per month, because these fish are known to contain higher levels of mercury.40 This exposure would be additive to potential mercury exposure from freshwater fish. US data indicate that people who are most at risk, especially women and minority groups, are the least informed about existing fish advisories.14,41 Physicians can play an important role in relaying information from advisories to their patients.
The long-term solution lies in pollution prevention and the virtual elimination of POPs and mercury from industrial processes. Although the actual burden of illness related to POPs is unknown, the weight of evidence from laboratory, animal and human epidemiological studies clearly indicates that there may be some impairment of children's intellectual function because of these exposures. The precautionary principle instructs us to take any reasonable measures that would prevent this harm. These measures will require changes to industrial processes and methods of waste incineration and power generation to virtually eliminate the release of these pollutants. Already contaminated sites and sediments need to be cleaned up.
Physicians may be interested in the work of the Canadian Association of Physicians for the Environment (www.cape.ca). This group is part of the Canadian Coalition for Green Health Care. The comparable group in the United States is Health Care Without Harm (www .hcwh.org). These groups are working to eliminate the use of mercury in the health care system and to bring in substitutes for products made from polyvinyl chloride, which generate dioxins when incinerated. In 1996 the Intergovernmental Forum on Chemical Safety agreed on a list of 12 POPs for virtual elimination from the environment. The Binding Convention on Persistent Organic Pollutants, sponsored by the United Nations Environment Programme, was formally adopted and signed in Stockholm in May 2001.42 It called for an immediate ban on 11 of the “dirty dozen”; a health-related exemption has been granted for DDT (dichlorodiphenyltrichloroethane), which is still needed in many countries to control malaria-transmitting mosquitoes.
Additional resources
· Information on endocrine disrupters: www.som.tulane.edu/ecme/eehome and www.ourstolenfuture.org
· In harms way. Toxic threats to child development: www.igc.org/psr/ihw.htm
· International Programme on Chemical Safety: www.who.int/pcs
· National Fish and Wildlife Contamination Program, Office of Water, US Environmental Protection Agency: www.epa.gov/ost/fish
· United Nations Environment Programme: www.chem.unep.ch/pops/default.html
Articles to date in this series .
Weir E. Identifying and managing adverse environmental health effects: a new series. CMAJ 2002;166(8):1041-3.
Marshall L, Weir E, Abelsohn A, Sanborn MD. Identifying and managing adverse environmental health effects: 1. Taking an exposure history. CMAJ 2002;166(8):1049-55.
Abelsohn A, Stieb D, Sanborn MD, Weir E. Identifying and managing adverse environmental health effects: 2. Outdoor air pollution. CMAJ 2002;166(9):1161-7.
Sanborn MD, Abelsohn A, Campbell M, Weir E. Identifying and managing adverse environmental health effects: 3. Lead exposure. CMAJ 2002;166(10):1287-92.
Sanborn MD, Cole D, Abelsohn A, Weir E. Identifying and managing adverse environmental health effects: 4. Pesticides. CMAJ 2002;166(11):1431-6.
Footnotes
[A detailed exposure history questionnaire is available on the Ontario College of Family Physicians Web site (www.cfpc.ca/ocfp/index.html — click on “Exposure History Sheets in MS Word” in the scrolling menu located in the middle of the page). The different components (Community, Home and Hobbies, Occupation, Personal habits, Diet and Drugs) can be printed on coloured paper for easy identification in patient charts. The questionnaire may be given to a patient to complete at home and bring to the next appointment for review and interpretation.]
This article has been peer reviewed.
Contributors: Dr. Abelsohn conceived of and drafted the article. Drs. Gibson, Sanborn and Weir contributed to the conception of the review. All of the authors contributed to the revising of the manuscript and approved the final version.
Competing interests: None declared.
Correspondence to: Dr. Alan Abelsohn, Department of Family and Community Medicine, University of Toronto, 1–1735 Bathurst St., Toronto ON M5P 2K4; fax 416 483-8182; alan.abelsohn@utoronto.ca
References
- 1.Marshall L, Weir E, Abelsohn A, Sanborn MD. Identifying and managing adverse environmental health effects: 1. Taking an exposure history. CMAJ 2002;166(8):1049-55. Available: www.cmaj.ca/cgi/content/full/166/8/1049 [PMC free article] [PubMed]
- 2.Greater Boston Physicians for Social Responsibility (GBPSR). Executive summary. In: In harms way. Toxic threats to child development. Boston: GBPSR; 2000. Available: www.igc.org/psr/ihw.htm (click on “Executive Summary” under Phase I in blue box at bottom of page) (accessed 2002 Apr 24).
- 3.Rice DC. Issues in developmental neurotoxicology: interpretation and implications of the data. Can J Public Health 1998;89(Suppl 1):S31-3. [PubMed]
- 4.Sanborn MD, Abelsohn A, Campbell M, Weir E. Identifying and managing adverse environmental health effects: 3. Lead exposure. CMAJ 2002;166 (10):1287-92. Available: www.cmaj.ca/cgi/content/full/166/10/1287 [PMC free article] [PubMed]
- 5.Fisher B. Most unwanted persistent organic pollutants. Environ Health Perspect 1999;107:A18-25. [DOI] [PMC free article] [PubMed]
- 6.Ritter L, Solomon KR, Forget J, Stemeroff M, O'Leary C. A review of the persistent organic pollutants: DDT, aldrin, dieldrin, endrin, chlordane, heptachlor, hexachlorobenzene, mirex, toxaphene, polychloirnated biphenyls, dioxin and furans. Geneva: International Programme on Chemical Safety; 1995. Available: www.chem.unep.ch/pops/indxhtms/asses0.html (accessed 2002 Apr 24).
- 7.Kalantzi O, Alcock E, Johnston P, Santillo D, Stringer R, Thomas G, et al. The global distribution of PCBs and organochlorine pesticides in butter. Environ Sci Technol 2001;35:1013-8. [DOI] [PubMed]
- 8.Craan AG, Haines DA. Twenty-five years of surveillance for contaminants in human breast milk. Arch Environ Contam Toxicol 1998;35:702-10. [DOI] [PubMed]
- 9.Contaminant profiles: polychlorinated biphenyls (PCBs). In: Health and the environment. The health and environment handbook for health professionals. Ottawa: Health Canada; 1998. Cat no H46-2/98-2111. Available: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/98ehd211/98ehd211.htm (accessed 2002 Apr 24).
- 10.Food quality. In: Health and the environment. The health and environment handbook for health professionals. Ottawa: Health Canada; 1998. Cat no H46-2/98-2111. Available: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/98ehd211/98ehd211.htm (accessed 2002 Apr 24).
- 11.Sandau CD, Ayotte P, Dewailly D, Duffe J, Norstrom RJ. Analysis of hydroxylated metabolites of PCBs and other chlorinated phenolic compounds in whole blood from Canadian Inuit. Environ Health Perspect 2000;108:611-6. [DOI] [PMC free article] [PubMed]
- 12.Muckle G, Dewailly E, Ayotte P. Prenatal exposure of Canadian children to polychlorinated biphenyls and mercury. Can J Public Health 1998;89(Suppl 1):S22-7. [PubMed]
- 13.Colborn T, vom Saal FS, Soto A. Developmental effects of endocrine-disrupting chemicals in wildlife and humans. Environ Health Perspect 1993;101 (5):378-84. [DOI] [PMC free article] [PubMed]
- 14.Johnson BL, Hicks H, Jones D, Cibulas W,Wargo A, De Rosa C. Public health implications of persistent toxic substances in the Great Lakes and St. Lawrence basins. J Great Lakes Res 1998;24(2):698-722.
- 15.Tryphonas H. The impact of PCBs and dioxins on children's health: immunologic considerations. Can J Public Health 1998;89(Suppl 1):S49-52. [PubMed]
- 16.Solomon GM, Schetter T. Environment and health: 6. Endocrine disruption and potential human health implications. CMAJ 2000;163(11):1471-6. Available: www.cmaj.ca/cgi/content/full/163/11/1471 [PMC free article] [PubMed]
- 17.Tilson H. Developmental neurotoxicology of endocrine disruptors and pesticides: identification of information gaps and research needs. Environ Health Perspect 1998;106(Suppl 3):807-11. [DOI] [PMC free article] [PubMed]
- 18.Endocrine Disrupter Screening and Testing Advisory Council final report. Office of Prevention, Pesticides, and Toxic Substances, US Environmental Protection Agency; 1998. Available: www.epa.gov/oscpmont/oscpendo/history/finalrpt.htm (accessed 2002 Apr 24).
- 19.Wade M. Human health and exposure to chemicals which disrupt estrogen, androgen and thyroid hormone physiology. Ottawa: Environmental and Occupational Toxicology Division, Environmental Health Directorate, Health Protection Branch, Health Canada. Available: www.hc-sc.gc.ca/ehp/ehd/bch/env_contaminants/endocrine.pdf (accessed 2002 May 13).
- 20.Lai TJ, Guo YL, Yu ML, Ko HC, Hsu CC. Cognitive development in Yucheng children. Chemosphere 1994;29:2405-11. [DOI] [PubMed]
- 21.Ribas-Fito N, Sala M, Kogevinas M, Sunyer J. Polychlorinated biphenyls (PCBs) and neurological development in children: a systematic review. J Epidemiol Community Health 2001;55:537-46. [DOI] [PMC free article] [PubMed]
- 22.Lai T, Guo Y, Guo N, Hsu C. Effect of prenatal exposure to polychlorinated biphenyls on cognitive development in children: a longitudinal study in Taiwan. Br J Psychiatry Suppl 2001;178(Suppl 40):S49-52. [DOI] [PubMed]
- 23.Brouwer A, Morse DC, Lans MC, Schuur AG, Murk AJ, Klasson-Wehler E, et al. Interactions of persistent environmental organohalogens with the thyroid hormone system: mechanisms and possible consequences for animal and human health. Toxicol Ind Health 1998;14:59-84. [DOI] [PubMed]
- 24.Jacobson J, Jacobson S, Humphrey H. Effects of in utero exposure to polychlorinated biphenyls and related contaminants on cognitive function in young children. J Pediatr 1990;116:38-45. [DOI] [PubMed]
- 25.Jacobson J, Jacobson S, Humphrey H. Effects of exposure to PCBs and related compounds on growth and activity in children. Neurotoxicol Teratol 1990;12:319-26. [DOI] [PubMed]
- 26.Jacobson J, Jacobson S. Intellectual impairment in children exposed to polychlorinated biphenyls in utero. N Engl J Med 1996;335:783-9. [DOI] [PubMed]
- 27.Walter JR. Pollutants in breast milk. Arch Pediatr Adolesc Med 1996;150:981-90. [DOI] [PubMed]
- 28.Schell J, Budinsky R, Wernke M. PCBs and neurodevelopmental effects in Michigan children: an evaluation of exposure and dose characterization. Regul Toxicol Pharmacol 2001;33(3):300-12. [DOI] [PubMed]
- 29.Seegal RF. Can epidemiological studies discern subtle neurological effects due to perinatal exposure to PCBs? Neurotoxicol Teratol 1996;18:251-4. [DOI] [PubMed]
- 30.Fielder N, Feldman RG, Jacobson J, Rahill A, Wetherell A. The assessment of neurobehavioral toxicity: SGOMSEC joint report [review]. Environ Health Perspect 1996;104(Suppl 2):179-91. [DOI] [PMC free article] [PubMed]
- 31.Davidson P, Weiss B, Myers G, Cory-Slechta D, Brockel B, Carter Young E, et al. Evaluation of techniques for assessing neurobehavioural development in children. Neurotoxicology 2000;21:957-72. [PubMed]
- 32.Mercury study report to Congress. Washington: Office of Air Quality Planning and Standards and Office of Research and Development, US Environmental Protection Agency; 1997. Available: www.epa.gov/oar/mercury.html (updated 2002 Mar 29; accessed 2002 May 13).
- 33.Contaminant profiles: mercury. In: Health and the environment. The health and environment handbook for health professionals. Ottawa: Health Canada; 1998. Cat no H46-2/98-2111. Available: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/98ehd211/98ehd211.htm (accessed 2002 Apr 24).
- 34.Harada H. Congenital Minimata disease: intrauterine methylmercury poisoning [review]. Teratology 1978;18:285-8. [DOI] [PubMed]
- 35.Myers G, Davidson P, Shamlaye C. A review of methylmercury and child development. Neurotoxicology 1998;19:313-28. [PubMed]
- 36.Myers G, Davidson P. Prenatal methylmercury exposure and children: neurologic, developmental and behavioural research. Environ Health Perspect 1998;106(Suppl 3):841-7. [DOI] [PMC free article] [PubMed]
- 37.Guide to eating Ontario sport fish, 2001–2002. 21st ed, rev. Toronto: Ontario Ministry of the Environment; 2001. Avaialable: www.ene.gov.on.ca/envision/guide (accessed 2002 Apr 24).
- 38.Guide de consommation du poisson de pêche sportive en eau douce. Québec: Ministère de l'Environnement and Ministère de la Santé et des Services sociaux du Québec; 2000. www.menv.gouv.qc.ca/eau/guide (accessed 2002 Apr 24).
- 39.Dose and response for chemicals: tolerable daily intake. In: Health and the environment. The health and environment handbook for health professionals. Ottawa: Health Canada; 1998. Cat no H46-2/98-2111. Available: www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/98ehd211/98ehd211.htm (accessed 2002 May 13).
- 40.Advisory: Information on mercury levels in fish. Ottawa: Health Canada; 2001. Available: www.hc-sc.gc.ca/english/protection/warnings/2001/2001_60e.htm (accessed 2002 Apr 24).
- 41.Fact sheet: Update: national listing of fish and wildlife advisories. Washington: Office of Water, US Environmental Protection Agency; 2001. Available (pdf format): www.epa.gov/waterscience/fish/advisories/factsheet.pdf (accessed 2002 Apr 24).
- 42.Stockholm Convention on persistent organic pollutants (POPs). Geneva: United Nations Environment Programme; 2001. Available: www.chem.unep.ch/sc (acessed 2002 May 13).


