Abstract
Background
Eclampsia and pre-eclampsia rank as the third leading causes of maternal death in Ecuador, following pre-existing chronic diseases and postpartum haemorrhage, as reported by the Ecuadorian National Institute of Statistics and Census (INEC). In contrast, HELLP (Haemolysis, Elevated Liver enzymes, Low Platelet count) syndrome remains underexplored epidemiologically, not only in Latin America but globally. This study marks the first population-based investigation into HELLP syndrome incidence and mortality in Ecuador, examining geographical variations, altitude influences and ethnic backgrounds.
Methods
Conducted as a retrospective population-based cohort study from 2015 to 2017, this research delves into the incidence, risk factors and maternal mortality associated with HELLP syndrome in Ecuador. Utilising data from INEC and the Ecuadorian Ministry of Health, we identified HELLP syndrome cases through ICD-10 (International Classification of Diseases, tenth revision) coding in hospitalised individuals. Logistic regression analysis was employed to explore association, whilst geospatial statistical analysis focused on cantons to identify significant spatial clusters. Primary outcome measures include HELLP syndrome incidence and maternal mortality, supplying crucial insights into the syndrome’s impact on maternal health in Ecuador.
Results
The incidence of HELLP syndrome is 0.76 (0.69–0.84)/ 1000 deliveries. Afro-Ecuadorian communities have a higher risk (Odds Ratio (OR) = 2.18 (1.03–4.63)) compared to Indigenous Ecuadorian communities. Living at mid-level or high altitude is a significant risk factor OR of 2.79 (2.19–3.55) and an OR 3.61 (2.58–5.03), respectively. Being an older mother was also identified as a risk factor. Women living more than 20 km from the obstetric unit have an OR of 2.55 (2.05–3.18). Moreover, we found that cantons with higher crude HELLP syndrome incidence also have lower numbers of physicians (R = 0.503, p-value < 0.001). The mortality incidence of women with HELLP syndrome is 21.22 (12.05–20.59)/1000 deliveries with HELLP syndrome diagnoses.
Conclusions
High altitude, advanced maternal age and geographical distance between residence and health centres are risk factors for HELLP syndrome. Maternal mortality in women with HELLP syndrome is higher than pre-eclampsia and eclampsia but comparable with previous reports in other countries.
Keywords: Ethnic groups, Altitude, HELLP syndrome, Geographical distance, Medical attention
Introduction
HELLP (Haemolysis, Elevated Liver Enzymes, Low platelet count) syndrome is a rare pregnancy complication, considered a variant or a complication of pre-eclampsia [1]. It is characterised by the presence of haemolysis, elevated liver enzymes and a low platelet count, which can lead to liver and kidney failure, bleeding and even death for both the mother and the foetus. The pathophysiology of HELLP syndrome is not fully understood, but it is believed to involve abnormal activation of coagulation and complement systems, oxidative stress and inflammation [2]. Hypertensive disorders during pregnancy are a major cause of maternal and foetal mortality and morbidity worldwide [3]. According to the Ecuadorian National Institute of Statistics and Census (INEC), eclampsia and pre-eclampsia were identified as the third cause of maternal death in the country after pre-existing chronic diseases and postpartum haemorrhage [4]. However, HELLP syndrome has been less studied than these two conditions in epidemiological terms, not only in Latin American countries but worldwide. The main reason behind this lack of epidemiological studies is the low incidence of the disease [5], leading to the use of small datasets. There are several well-known risks associated with HELLP syndrome (e.g., history of hypertension and cardiovascular problems, maternal age, diabetes, obesity and null parity). A recent Canadian-based population study by Lisonkova et al. brought valuable information [6]. They pointed out that living in a rural area is a risk factor, which is consistent with previous studies, and that nulliparous women living more than 1 h from obstetric units have a 50% increased risk of HELLP syndrome [7].
Ecuador, like other Latin-American countries, has human communities living from 0 to more than 4,000 m above sea level (m.a.s.l.) and comprising a wide ethno-diversity across all these altitude changes. Therefore, the study of ethnicity and altitude, besides the geographical distances between residence and obstetrics units, is necessary. Regarding the potential impact of altitude, previous studies have shown that the incidence of HELLP syndrome could be greater at higher altitudes [8, 9]. This is because it has been demonstrated that women living at high altitudes have reduced uterine blood flow. The resulting hypoxia deteriorates arterial structure, leading to a decreased sensitivity to vasoconstriction during pregnancy [10]. These findings suggest that the increase in hypoxia could be the cause of a higher incidence of placental damage, which, in turn, would contribute to the elevated rates of pre-eclampsia and, consequently, HELLP syndrome in higher-altitude areas. However, regarding the influence of ethnicity, some contradictions were found in the literature. Oliveira et al. reported that HELLP syndrome is more frequent in Caucasian populations while pre-eclampsia without HELLP is more frequent in women of Afro-American origins [11]. Moreover, Williams et al. also indicated a higher risk of HELLP in White and Chinese populations compared to East Indian groups [12]. However, a recent study conducted by Chronock et al. showed that in terms of postpartum readmission, hypertensive disorders (including HELLP syndrome) are more frequent in older mothers and non-Hispanic Black women [13].
Although some similar studies have been conducted before in other Latin-American nations and using small samples [14, 15], this is the first Ecuadorian population-based study covering HELLP syndrome incidence and mortality while exploring geographical locations, the influence of altitude and ethnic background.
Methods
Study design
We conducted a population-based retrospective cohort study including all deliveries in Ecuadorian hospitals from 2015 to 2017. The main variables under study were altitude, self-identified ethnic group, geographic location and maternal age.
Dataset
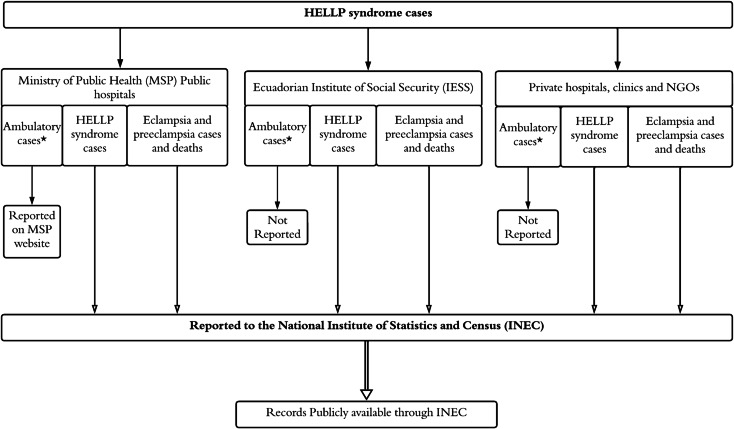
The data used in this study was obtained from the national registries of hospital discharges published by the INEC and the Ecuadorian Ministry of Health (MSP) for the period 2015–2017 [16] (Fig. 1). All cases were identified and HELLP syndrome was grouped according to the ICD-10 (International Classification of Diseases, tenth revision) identification code: O142. Similarly, for comparison regarding maternal mortality, we also included the number of cases (and deaths) for eclampsia and pre-eclampsia. The database comprises all hospitalised individuals and for this study, only Ecuadorian women with subsequent delivery were considered. All records are anonymous and comprise information regarding maternal age, location of residence, hospital location, hospitalisation date, clinical diagnosis, ethnic self-identification and delivery type. The demographic distribution is presented in Table 1. The total number of deliveries in 2015–2017 was 167,650, 159,435 and 166,960 respectively for a total of 494,045 across the three years.
Fig. 1.
Flowchart on data collection for the development of the study.
Source: authors’ own creation * Ambulatory cases: The information about ambulatory cases is not publicly accessible, which could lead to a potential loss of data due to this restriction. NGO: nongovernmental organizations
Table 1.
Sociodemographic characteristics of the population
| 2015 | 2016 | 2017 | |
|---|---|---|---|
| Maternal age (years) | # (%) | # (%) | # (%) |
| 10–14 | 1584 (0.94) | 1430 (0.9) | 1427 (0.85) |
| 15–19 | 35,596 (21.23) | 31,121 (19.52) | 31,756 (19.02) |
| 20–24 | 44,549 (26.57) | 41,535 (26.05) | 43,886 (26.29) |
| 25–29 | 38,051 (22.7) | 36,861 (23.12) | 39,380 (23.59) |
| 30–34 | 28,308 (16.89) | 28,395 (17.81) | 30,071 (18.01) |
| 35–39 | 14,902 (8.89) | 15,382 (9.65) | 15,922 (9.54) |
| 40–44 | 4231 (2.52) | 4259 (2.67) | 4096 (2.45) |
| 45–49 | 429 (0.26) | 440 (0.28) | 395 (0.24) |
| 50–55 | 0 (0) | 12 (0.01) | 27 (0.02) |
| Ethnicity (%) | |||
| Indigenous Ecuadorian | 7296 (4.35) | 7179 (4.5) | 7261 (4.35) |
| Afro-Ecuadorian | 2622 (1.56) | 1963 (1.23) | 1918 (1.15) |
| Montubio | 333 (0.2) | 380 (0.24) | 633 (0.38) |
| Mestizo | 144,569 (86.23) | 140,634 (88.21) | 146,213 (87.57) |
| Caucasian | 721 (0.43) | 483 (0.3) | 527 (0.32) |
| Other/not specified | 12,109 (7.22) | 8796 (5.52) | 10,408 (6.23) |
| Altitude (m) (%) | |||
| < 1500 | 98,777 (58.92) | 89,137 (55.91) | 101,486 (60.78) |
| 1500–3500 | 56,875 (33.92) | 57,162 (35.85) | 52,604 (31.51) |
| > 3500 | 11,627 (6.94) | 12,904 (8.09) | 12,574 (7.53) |
| Not specified | 371 (0.22) | 232 (0.15) | 296 (0.18) |
| Deliveries | 167,650 | 159,435 | 166,960 |
INEC classifies ethnic self-identification as Indigenous Ecuadorian, Afro-Ecuadorian, Black, Mulato, Montubio, Mestizo, Caucasian, Other and “not specified”. In this study, Afro-Ecuadorian, Black and Mulato people were grouped as “Afro-Ecuadorian” (Table 1), while the categories “not specified”, and Other were excluded from ethnic analysis. The Montubio population is a specific self-identified Mestizo sub-group geographically located in rural areas along the Ecuadorian coast and most of them work as farmers [17]. We decided to include them as a separate group and not as part of the Mestizo Ecuadorian population because they have a very well-defined geographical location significantly different from other groups.
Altitude was extracted using the residential address of the patient and categorised into three groups: less than 1,500; between 1,500 and 3,500; and higher than 3,500 m.a.s.l.
Statistical analysis
The incidence for HELLP syndrome was calculated with respect to the total number of normal deliveries (natural and caesarean) using the Poisson distribution for confidence interval estimation using stats in R-package v 4.2.0 (The R foundation for Statistical Computing, Vienna, Austria) and represented as absolute frequency and percentages. Logistic regression analysis was used to study the association between the frequency of HELLP syndrome cases and demographic variables such as ethnicity, maternal age, altitude of the place of residence and distance from residence to obstetrics unit. The effect estimates are expressed as odds ratio (OR) and corresponding 95% confidence intervals (CI). Maternal age was not treated as a categorical variable in logistic regression analysis but as a continuous variable. Geographical distance was calculated using GeoPy Python library [18] and transformed to its natural logarithm. For the computation of distance, the GPS coordinates for each canton (secondary sub-division of Ecuador after provinces) were used, as provided by the INEC.
Geospatial statistical analysis
The spatial units for the analysis were the cantons. All HELLP syndrome cases were handled as new cases to obtain relative risk estimates. Geospatial statistical analysis was performed to identify statistically significant spatial clusters of HELLP syndrome cases. The spatial clusters were defined by the cantons with higher incidences of HELLP cases. Cases were distributed geographically by canton and by ICD-10 identification code. The spatial analysis was conducted in SATSCAN v 9.6 (Software for the spatial, temporal and space-time scan statistics, Boston, USA). The software tested for significance and identified approximate locations of areas with an increased risk for the occurrence of HELLP syndrome [19].
The geospatial analysis used: (1) the number of HELLP syndrome cases distributed geographically by canton, (2) the total population of each canton and (3) the spatial coordinates of each canton. A Poisson distribution was used to compare the number of cases in each geographical location. Space clustering was assessed by comparing the incidence rate ratio of HELLP syndrome cases in a specific geographical area with an expected incidence rate ratio of the cases of HELLP syndrome if their incidences were randomly distributed. The Likelihood ratio test was used to check the significance of identified space clusters. 999 Monte Carlo simulations were used to obtain the p-values of the test. A cluster was identified as significant when obtained p-values were inferior to 0.05 [20]. The Gini coefficient was used as an additional selection filter amongst the significant non-overlapping clusters, as described by Han et al. [21].
The spatial analysis was visualised using QGIS v 3.8 Zanzibar software (A Free and Open-Source Geographic Information System, Zurich, Switzerland). Shapefiles for all the maps in this article were obtained from the INEC portal following their licensing requirements [16]. All maps were created and designed by the authors of this manuscript.
Results
The socio-demographic data distribution according to the variables under study during the period 2015–2017 are presented in Table 1.
In addition to the information presented in Table 1, we should indicate that the women in our dataset are geographically distributed across 225 cantons. From these cantons, we computed the number of deliveries between 2015 and 2017 and the average number of doctors across the same period. This information will be used for further analysis. In addition to the information presented in Table 1, it is worth noting that the overall prevalence of eclampsia is 0.25 (0.23–0.26), while for pre-eclampsia it is 6.23 (6.16–6.30), as previously reported by Tejera et al. 2021 [22].
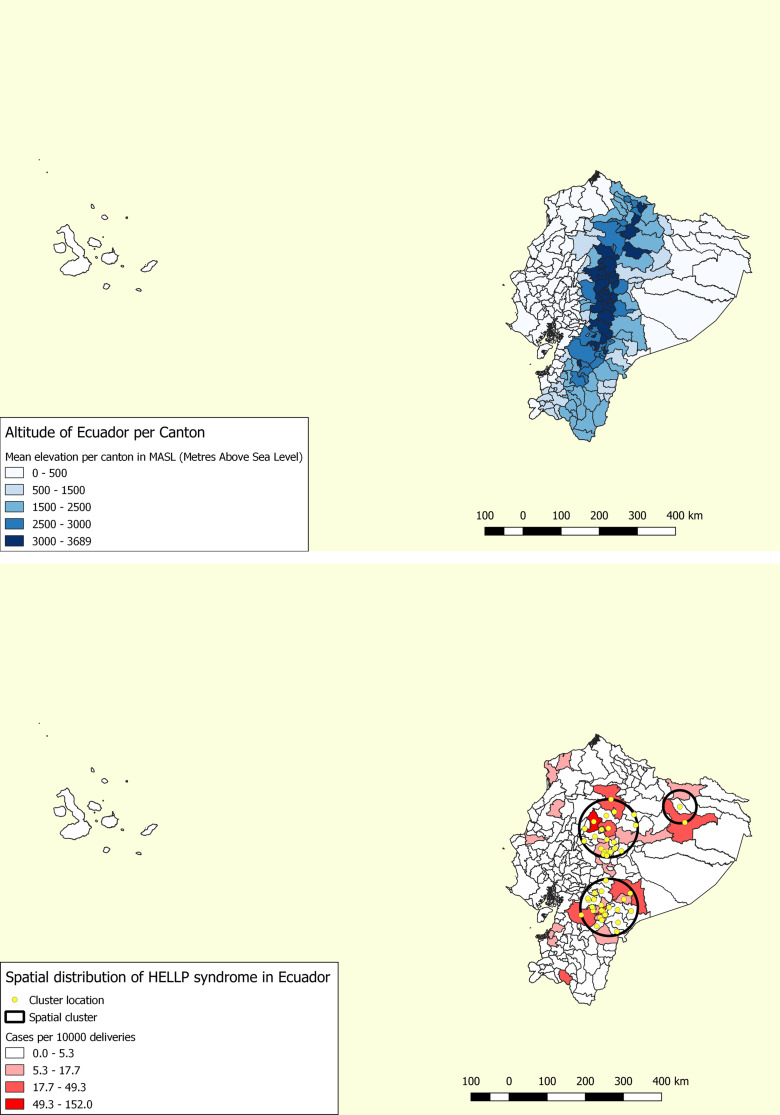
Moreover, the geographical distribution pattern focused on the mid-level and highest altitudes (except for the Amazon region) (Fig. 2). HELLP syndrome is clearly widespread, but several cantons did not show any cases in the period under study.
Fig. 2.
Above: Mean elevation in metres above sea level (m.a.s.l.) according to canton. Below: Geographical clusters indicating the areas with significantly higher incidences of HELLP syndrome
Relative risk (RR) for HELLP syndrome varied from 1.91 to 3.7 for the areas inside the three clusters when compared with the areas outside the clusters (Fig. 2, Right). In these areas, the cantons with the highest relative risk were: Francisco de Orellana, Quito, Latacunga, Sigchos and Morona. The influence of altitude, maternal age and distance between residence and obstetrics units showed a significant influence upon HELLP syndrome incidence (Table 2). High altitude is associated with a higher incidence of the disease as well as increased maternal age and increased geographical distance.
Table 2.
Influence of altitude, maternal age and geographical distance on HELLP syndrome incidence
| Variables | Independent variable analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| p-value | OR | 95% C.I. OR | p-value | OR | 95% C.I. OR | ||
| Ethnicity a | Afro-Ecuadorian | 0.969 | 0.99 | 0.47–2.07 | 0.043 | 2.18 | 1.03–4.63 |
| Montubio | 0.495 | 0.50 | 0.07–3.66 | 0.932 | 1.09 | 0.15–8.05 | |
| Mestizo | < 0.001 | 0.48 | 0.33–0.69 | 0.082 | 0.72 | 0.50–1.04 | |
| Caucasian | 0.988 | 0.00 | 0.00–0.00 | 0.989 | 0.00 | 0.00–0.00 | |
| Altitude b | 1500–3500 | < 0.001 | 2.92 | 2.32–3.66 | < 0.001 | 2.79 | 2.19–3.55 |
| > 3500 | < 0.001 | 3.72 | 2.71–5.12 | < 0.001 | 3.61 | 2.58–5.03 | |
|
Maternal Age |
< 0.001 | 1.04 | 1.02–1.05 | < 0.001 | 1.02 | 1.01–1.04 | |
|
Geographical Distance |
< 0.001 | 1.22 | 1.15–1.29 | < 0.001 | 1.27 | 1.20–1.35 | |
| Ratio of Doctors c | < 0.001 | 6.01 | 3.70–9.75 | < 0.001 | 6.82 | 4.00–11.65 | |
Notes (a) In these variables, Indigenous Ecuadorians were considered as a reference. (b) In altitude, the group of women living < 1500 m.a.s.l. were considered as a reference. (c) The ratio of doctors corresponds to the number of doctors per delivery by considering the women’s cantons. This variable was log-transformed after inclusion in the model. In the independent variable analysis, each OR was computed for each variable independently, while in the multivariate analysis, the OR comprised all of the variables’ effects
The areas under the curve (AUC) independently obtained for ethnicity, altitude, age, geographical distance and ratio of doctors were: 0.53, 0.64, 0.57, 0.57 and 0.62, respectively. On the other hand, for the multivariate model, the AUC was 0.73.
The incidence of HELLP syndrome is presented in Table 3. Moreover, the Chi-square test showed significant differences in the HELLP incidence across the time interval (X2 = 39.42, p-value < 0.001). The model including the years (used for OR computation in Table 3) showed a small AUC increment to 0.75. The data presented in Table 3 suggest that the incidence of HELLP syndrome increased from 2015 to 2017.
Table 3.
HELLP syndrome incidences for our entire cohort per 1000 deliveries
| Incidence (%) | 2015 (CI: 95%) | 2016 (CI: 95%) | 2017 (CI: 95%) | Overall (CI: 95%) |
|---|---|---|---|---|
| HELLP syndrome | 0.43 (0.34–0.54) | 0.90 (0.76–1.06) | 0.97 (0.83–1.13) | 0.76 (0.69–0.84) |
| OR (multivariate) | 2015 (OR CI: 95%) | 2016 (OR CI: 95%) | 2017 (OR CI: 95%) | |
| HELLP syndrome | (reference) | 2.10 (1.57–2.82) | 2.13 (1.58–2.86) |
Note The OR values were computed including the period as a categorical variable in the model presented in Table 2. We obtained a p-value < 0.001 for the period and for each of the years
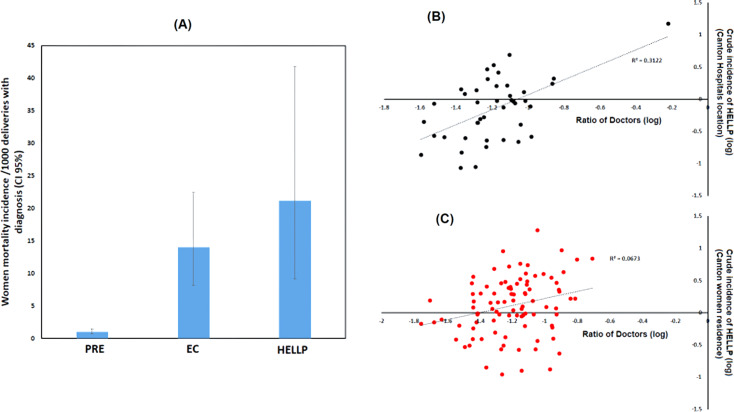
In the period from 2015 to 2017, we found a total of 377 Ecuadorian women with HELLP syndrome diagnoses and 8 deaths. This implies a mortality rate of 21.22 (9.17–41.81) per 1000 deliveries with HELLP syndrome diagnosis. For comparison, we calculated the same mortality rate for eclampsia and pre-eclampsia (Fig. 3A). The obtained mortality rate values are: 14.0 (8.16–22.42) and 1.05 (0.72–1.49) per 1000 deliveries for eclampsia and pre-eclampsia, respectively. Clearly, the mortality rate is higher for women with HELLP syndrome diagnosis. Because there were fewer cases of HELLP syndrome than pre-eclampsia, eclampsia, the confidence interval was lower (more conservative).
Fig. 3.
(A) Women’s mortality incidence/1000 deliveries with diagnoses of pre-eclampsia (PRE), eclampsia (EC) and HELLP syndrome (HELLP). (B) and (C) Variation between the number of doctors per delivery (ratio of doctors) and the crude incidence of HELLP syndrome according to cantons. In B, the cantons correspond to the hospital locations, while in C, the cantons correspond to the women’s locations
As presented in Table 2, geographical distance is an important risk associated with the development of HELLP syndrome. When exploring the association between crude incidence of HELLP syndrome across cantons and the number of doctors (divided by the number of deliveries), we found a different pattern. Regarding HELLP incidence based on the women’s canton of residence (the same used in the previous spatial analysis and in Table 2), a weak but significant association was found (R = 0.259, p-value = 0.021, Fig. 3C). This correlation increases if we consider not the women’s residence but the hospital location (R = 0.559, p-value < 0.001, Fig. 3B). In both cases, cantons with higher numbers of doctors/deliveries also had higher HELLP incidences, but this difference will be explored in our discussion. The correlation in Fig. 3 ignores the cantons with no cases of HELLP syndrome in the period under analysis. Moreover, the same model analysis presented in Table 2 was performed using geographical distance as a categorical variable. We found an OR = 2.55 (2.05–3.18, p-value < 0.001) for women living more than 20 km away from an obstetrics unit.
Discussion
We can notice an increase in the incidence of HELLP syndrome from 2015 to 2017. This increment can be associated with several factors, but we think it is more likely related to improvement in clinical diagnosis as well as database annotation. The incidence obtained is lower than the values previously reported in Canada (2.5/singleton deliveries) [6] but closer to values reported by Kongwattanaku et al. in Thailand [23] and Vigil-de Gracia et al. in Latin America [14, 15]. We think the differences are a consequence of parity/gravidity and maternal age considerations. We cannot separate nullipara from multigravida in our dataset and because the probability of HELLP is higher in nulliparous pregnancies [24], this could lead to an increase in the differences between both studies. Moreover, in our data, the highest percentage of deliveries occurred amongst women aged 20–29, while Lisonkova et al. found the highest percentage in the 25–34 age bracket [6]. The cantons with the highest relative risk (darkest colours in Fig. 2) were: Francisco de Orellana, Quito, Latacunga, Sigchos and Morona. Cantons like Quito (where the capital of Ecuador is located) receive severe cases from other locations with fewer medical resources and, consequently, the HELLP incidence can be affected. These mobility issues, the possible implication of medical resources and the previous work of Lisonkova et al. [6] were the main motivators to include variables like the ratio of doctors and geographical distance in our models. However, other variables related to social and economic impacts could improve the analysis of the geographical incidence distribution.
Our results regarding the influence of maternal age and altitude are consistent with previous findings [6, 9]. Women with a higher maternal age have an increased risk of developing HELLP syndrome. Furthermore, altitude, which has been better explored in pre-eclampsia and eclampsia, showed a similar pattern regarding HELLP syndrome. This means, as previously reported by other authors [8, 9], that high altitude is associated with an increased risk of HELLP syndrome incidence. From the cantons previously presented, Orellana is almost the only one at a lower altitude. The association between altitude and eclampsia or pre-eclampsia is well known [25] and mediated by hypoxia (or at least is one of their possible causes) [26]. However, HELLP syndrome has been explored less and few reports are available in Latin American countries. An important problem regarding altitude is “adaptability” [27]. The populations in cantons with the highest altitudes. like Latacunga (one of the cantons with the highest incidence), are mainly Mestizo or Indigenous and have been living there for generations with an expected adaptation to those environments. However, another canton with a similar altitude, such as Ambato, has a much lower HELLP incidence. These results suggest that the risk that altitude poses could be mediated by other factors. In fact, the OR values obtained in Table 2 are lower in the multivariable model compared to the individual effects.
Even when we obtained a higher OR for the Afro-Ecuadorian population compared to Indigenous Ecuadorians (OR = 2.18 (1.03–4.63)), we should be cautious about this effect. The distribution of HELLP syndrome cases across ethnic groups is sparse, no cases were found in the Caucasian population and only 1 case in the Montubio community. This result could indicate that those ethnic groups are somehow protected, but those groups live at different altitudes and have different socio-economic conditions. Including these variables (as in Table 2) leads to an even more sparse distribution, which makes ethnicity analysis difficult, but the OR values change considerably when compared to the independent effect. We know that in general Afro-Ecuadorians have an increased risk of developing pre-eclampsia and eclampsia, which could justify the increased risk of HELLP syndrome [15]. However, the change in OR of the ethnic groups after including the remaining variables is an indication of the complex associations regarding HELLP incidence. The Montubio group inhabits a low altitude; however, there is a group of Afro-Ecuadorians who reside at mid-level altitude, though the majority live at low altitude. Between these regions, we could find a significant change in medical resources as well as travelling distances to hospitals. Moreover, increasing the number of years considered in the population analysis may be needed to further explore the possible effect of ethnicity whilst considering the wide variation in altitude and geographical conditions.
Whereas pre-eclampsia can be identified at antenatal visits, some women experience a sudden and rapid progression to eclampsia or even HELLP syndrome [7, 28]. A recent study found that nulliparous women living more than 1 h from obstetrics units have a 50% increased risk of eclampsia [7]. Here, we also found a similar pattern regarding HELLP syndrome incidence, in that women who live further away from a health centre are more likely to develop HELLP syndrome (Table 3). In several cantons in Ecuador, a patient requiring hospital care is moved to another canton with better hospital resources (and usually a higher number of medical personnel). This movement not only increases the distance (as previously discussed) but also strengthens the association between the HELLP incidence and the increment in the number of doctors, as presented in Fig. 2B and C. This finding (also supported by the OR obtained in Table 2) could be explained by several reasons. The incremental increase in the risk of developing HELLP syndrome in cantons with a higher proportion of doctors can be associated with cases of rapid progression but also because patients with severe obstetric complications might be transferred to specialised hospitals, usually located in urban areas. This movement increases the geographical distance and might be more of a reflection of the absence of specialised obstetric hospitals in rural areas. Moreover, we cannot reject the idea that cantons with a higher number of doctors are better able to achieve an early diagnosis of HELLP, which could also increase this correlation.
On the other hand, it is evident that maternal mortality is higher in HELLP syndrome than in eclampsia or pre-eclampsia. The mortality rate we found (21.22/1000 HELLP cases or 2.12%) is consistent with those found by other authors in several countries [6, 14, 29]. Because of the low number of deaths, it is difficult to reliably study other variables that could be related to this finding. Many years are required to accomplish this type of analysis. However, as HELLP syndrome is a further aggravation of eclampsia and pre-eclampsia, it is plausible to expect higher mortality, as presented in our results.
Strengths and limitations
We should keep in mind that the connection between HELLP and the studied risk factors cannot be demonstrated, but these findings suggest that there is a significant association that should be further analysed to bring evidence to the causality of HELLP syndrome.
Moreover, the public data used does not have information regarding the women’s number of gestations and/or parity and we have ignored the foetal sex, perinatal mortality, women’s clinical history and gestational age at the time of delivery, another limitation in our study was the absence of data from ambulatory cases, as depicted in Fig. 1. These variables could be relevant to HELLP syndrome epidemiology [6]. However, this is the first countrywide population-based study in Ecuador. The study comprises information from the entire country and could provide guidance for Public Health management.
Conclusions
HELLP syndrome is distributed across several cantons of Ecuador with an increase from 2015 to 2017. However, there is a higher prevalence in cantons located at mid-level and high altitudes, except for the Amazon region. We found that Afro-Ecuadorian groups could have a higher incidence of the disease compared to Indigenous Ecuadorians, but more data is needed to clearly resolve the ethnic variation when altitude and other variables are also considered. Moreover, we confirm that increased maternal age and altitude are relevant risk factors for HELLP syndrome incidence. The maternal mortality for women with HELLP syndrome is higher than those with eclampsia or pre-eclampsia but but to which is similar the ratios reported by other authors in different countries.
Our results demonstrate that cantons with a higher density of doctors also have the highest crude incidence of HELLP syndrome. We also found an increased risk of HELLP syndrome in women living more than 20 km from an obstetrics unit. This is consistent with the density of doctors and the relocation of women to cantons with better medical resources and conditions. These results together could guide governmental strategies to reduce the HELLP incidence and/or improve the management of the disease in cantons with higher disease incidence or reduced personnel.
Acknowledgements
Not applicable.
Author contributions
Marco Coral-Almeida: Conceived and designed the analysis, Performed the analysis, data curation, writing of original draft.Aquiles R. Henríquez-Trujillo: Contributed data and analysis tools, Conceived and designed the analysis, Performed the analysis, writing and review of the manuscript, writing of original draft.Eduardo Tejera: Contributed data and analysis tools, Conceived and designed the analysis, Performed the analysis, writing and review of the manuscript, writing of original draft.María Eugenia Sánchez: Conceived and designed the analysis, Collected the data, writing of original draft.María Barriga-Burgos: Writing and review of the manuscript, data curation.Evelyn Alarcón-Moyano: Writing and review of the manuscript, data curation.
Funding
The study was funded by Universidad de Las Américas, Quito. Ecuador. Fund reference: VET.MCA.21.01. The founding body does not have any role in the design of the study, collection, analysis, and interpretation of data.
Data availability
All the data used in this manuscript is publicly available through the Ecuadorian National Institute of Statistics and Census (INEC) and the Ecuadorian Ministry of Health (MSP) at: https://www.ecuadorencifras.gob.ec/camas-y-egresos-hospitalarios/.
Declarations
Ethics approval and consent to participate
This study uses public retrospective anonymised data from the INEC and MSP with no specific ethical issue to be considered. Additionally, a local ethics committee ruled that no formal ethics approval was required in this case. The letter from the ethical committee can be provided upon request.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Marco Coral-Almeida, Email: marco.coral@udla.edu.ec.
Eduardo Tejera, Email: eduardo.tejera@udla.edu.ec.
References
- 1.Adorno M, Maher-Griffiths C, Grush Abadie HR. HELLP syndrome. Crit Care Nurs Clin North Am. 2022;34:277–88. 10.1016/j.cnc.2022.04.009 [DOI] [PubMed] [Google Scholar]
- 2.Lewandowska M, Englert-Golon M, Krasiński Z, Jagodziński PP, Sajdak S. A rare case of HELLP syndrome with hematomas of spleen and liver, Eclampsia, severe hypertension and prolonged Coagulopathy-A Case Report. Int J Environ Res Public Health. 2022;19. [DOI] [PMC free article] [PubMed]
- 3.Sutton ALM, Harper LM, Tita ATN. Hypertensive disorders in pregnancy. Obstet Gynecol Clin North Am. 2018;45:333–47. 10.1016/j.ogc.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 4.Rectificación. Los índices de la mortalidad materna |Noticias | El Universo. https://www.eluniverso.com/noticias/2015/10/08/nota/5172101/indices-mortalidad-materna/
- 5.Cecatti J. Powerful evidence on HELLP syndrome from a routine health database. BJOG. 2020;1471–0528. 16312. [DOI] [PubMed]
- 6.Lisonkova S, Razaz N, Sabr Y, Muraca G, Boutin A, Mayer C, et al. Maternal risk factors and adverse birth outcomes associated with HELLP syndrome: a population-based study. BJOG. 2020. 10.1111/1471-0528.16225. 10.1111/1471-0528.16225 [DOI] [PubMed] [Google Scholar]
- 7.Engjom HM, Morken N-H, Høydahl E, Norheim OF, Klungsøyr K. Risk of eclampsia or HELLP-syndrome by institution availability and place of delivery – a population-based cohort study. Pregnancy Hypertens. 2018;14:1–8. 10.1016/j.preghy.2018.05.005 [DOI] [PubMed] [Google Scholar]
- 8.Kumtepe Y, Dündar O, Çetinkaya K, Ingeç M. Pre-eclampsia and eclampsia incidence in the eastern Anatolia region of Turkey: the effects of high altitude. J Turkish German Gynecol Association. 2011;12:26–30. 10.5152/jtgga.2011.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey B, Euser AG, Bol KA, Julian CG, Moore LG. High-altitude residence alters blood-pressure course and increases hypertensive disorders of pregnancy. J Maternal-Fetal Neonatal Med. 2020. 10.1080/14767058.2020.1745181. 10.1080/14767058.2020.1745181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Genbacev O, Zhou Y, Ludlow JW, Fisher SJ. Regulation of human placental development by oxygen tension. Science. 1997;277:1669–72. 10.1126/science.277.5332.1669 [DOI] [PubMed] [Google Scholar]
- 11.Oliveira N, Poon LC, Nicolaides KH, Baschat AA. First trimester prediction of HELLP syndrome. Prenat Diagn. 2016;36:29–33. 10.1002/pd.4694 [DOI] [PubMed] [Google Scholar]
- 12.Williams KP, Wilson S. Ethnic variation in the incidence of HELLP syndrome in a hypertensive pregnant population. J Perinat Med. 1997;25:498–501. 10.1515/jpme.1997.25.6.498 [DOI] [PubMed] [Google Scholar]
- 13.Chornock R, Iqbal SN, Kawakita T. Racial disparity in Postpartum Readmission due to hypertension among women with pregnancy-Associated Hypertension. Am J Perinatol. 2020. 10.1055/s-0040-1712530. 10.1055/s-0040-1712530 [DOI] [PubMed] [Google Scholar]
- 14.Vigil-De Gracia P, Rojas-Suarez J, Ramos E, Reyes O, Collantes J, Quintero A, et al. Incidence of eclampsia with HELLP syndrome and associated mortality in Latin America. Int J Gynecol Obstet. 2015;129:219–22. 10.1016/j.ijgo.2014.11.024 [DOI] [PubMed] [Google Scholar]
- 15.Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel J, et al. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization Multicountry Survey on maternal and Newborn Health. BJOG. 2014;121:14–24. 10.1111/1471-0528.12629 [DOI] [PubMed] [Google Scholar]
- 16.Instituto Nacional de Estadísticas y Censos. http://www.inec.gob.ec
- 17.Roitman K. Hybridity, Mestizaje, and Montubios in Ecuador. Queen Elizabeth House, University of Oxford, QEH Working Papers. 2008.
- 18.GeoPy. https://github.com/geopy/geopy
- 19.Kulldorff M. A spatial scan statistic. Commun Stat Theory Methods. 1997;26:1481–96. 10.1080/03610929708831995 [DOI] [Google Scholar]
- 20.Ron-Garrido L, Coral-Almeida M, Gabriël S, Benitez-Ortiz W, Saegerman C, Dorny P, et al. Distribution and potential indicators of hospitalised cases of Neurocysticercosis and Epilepsy in Ecuador from 1996 to 2008. PLoS Negl Trop Dis. 2015;9:e0004236. 10.1371/journal.pntd.0004236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han J, Zhu L, Kulldorff M, Hostovich S, Stinchcomb DG, Tatalovich Z et al. Using Gini coefficient to determining optimal cluster reporting sizes for spatial scan statistics. Int J Health Geogr. 2016;15. [DOI] [PMC free article] [PubMed]
- 22.Tejera E, Sánchez ME, Henríquez-Trujillo AR, Pérez-Castillo Y, Coral-Almeida M. A population-based study of pre-eclampsia and eclampsia in Ecuador: ethnic, geographical and altitudes differences. BMC Pregnancy Childbirth. 2021;21. [DOI] [PMC free article] [PubMed]
- 23.Kongwattanakul K, Saksiriwuttho P, Chaiyarach S, Thepsuthammarat K. Incidence, characteristics, maternal complications, and perinatal outcomes associated with pre-eclampsia with severe features and HELLP syndrome. Int J Womens Health. 2018;10:371–7. 10.2147/IJWH.S168569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malmström O, Håberg SE, Morken N. Probability and outcomes of second pregnancy after HELLP syndrome in the first: a population-based registry study. Acta Obstet Gynecol Scand. 2020;:aogs13859. [DOI] [PubMed]
- 25.Zhou J, Xiao D, Hu Y, Wang Z, Paradis A, Mata-Greenwood E, et al. Gestational hypoxia induces pre-eclampsia-like symptoms via heightened endothelin-1 signaling in pregnant rats. Hypertension. 2013;62:599–607. 10.1161/HYPERTENSIONAHA.113.01449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zamudio S. High-altitude hypoxia and pre-eclampsia. Front Biosci. 2007;12:2967. 10.2741/2286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmed SIY, Ibrahim ME, Khalil EAG. High altitude and pre-eclampsia: adaptation or protection. Med Hypotheses. 2017;104:128–32. 10.1016/j.mehy.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 28.Andersgaard AB, Herbst A, Johansen M, Ivarsson A, Ingemarsson I, Langhoff-Roos J, et al. Eclampsia in Scandinavia: incidence, substandard care, and potentially preventable cases. Acta Obstet Gynecol Scand. 2006;85:929–36. 10.1080/00016340600607149 [DOI] [PubMed] [Google Scholar]
- 29.Yıldırım G, Güngördük K, Aslan H, Gül A, Bayraktar M, Ceylan Y. Comparison of perinatal and maternal outcomes of severe pre-eclampsia, eclampsia, and HELLP syndrome. J Turk Ger Gynecol Assoc. 2011;12:90–6. 10.5152/jtgga.2011.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data used in this manuscript is publicly available through the Ecuadorian National Institute of Statistics and Census (INEC) and the Ecuadorian Ministry of Health (MSP) at: https://www.ecuadorencifras.gob.ec/camas-y-egresos-hospitalarios/.