Abstract
Intraoperative acetabular fractures (IAFs), a complication seldomly encountered in total hip arthroplasty, are typically a result of the impact of insertion of a cementless press-fit cup. Factors that contribute to the risk of these types of fractures include poor bone quality, highly sclerotic bone, and the use of a press-fit cup that is excessively large. The approach to management of these fractures is dependent on when they are identified. Immediate stabilization measures should be implemented for management of fractures detected during surgery. When fractures are detected postoperatively, the decision regarding conservative treatment is dependent on the stability of the implant and the specific fracture pattern. In the majority of cases, effective treatment of an acetabular fracture detected intraoperatively can be administered using a multi-hole revision cup along with anchoring screws in the various regions of the acetabulum. Selection of plate osteosynthesis of the posterior column is recommended when there is a large posterior wall fragment or pelvic discontinuity. In cases where anatomical dimensions allow, cup-cage reconstruction may offer a promising alternative to a combined hip procedure. The number of reports addressing the management of IAFs is limited. This review focuses on outlining the strategies that are currently available for management of this seldomly encountered complication.
Keywords: Total hip arthroplasty, Intraoperative periprosthetic acetabular fracture, Cementless cup, Press-fit, Revision
INTRODUCTION
Intraoperative acetabular fracture (IAF) is a rare complication of total hip arthroplasty (THA). To date, only small case series from single centers have been published, with a reported incidence of 0.09%-0.4%1-6). A fracture that is not detected intraoperatively, which is not uncommon, can subsequently progress to a postoperative complication. It can be assumed that some IAF remain undetected7,8). A recent study reported a rate of occult fractures of 8.4%8). Thus, there is still uncertainty regarding the true prevalence and incidence of IAF in both primary and revision arthroplasty. Factors that increase the risk of IAF include insufficient acetabular reaming, imprecise reaming techniques, application of cementless monobloc or elliptical acetabular components, and prior pelvic irradiation1-6). Most patients reported in the literature were female patients with poor bone quality. Due to the low number of cases, variability in implant utilization, and differences in fracture patterns, there is a lack of consensus regarding the optimal treatment approach. Management of these fractures requires a substantial level of proficiency in performance of revision arthroplasty, as well as a profound understanding of acetabular osteosynthesis. Consequently, numerous orthopedic surgeons face challenges when confronted with such a complication. Referral to a high-volume revision THA center is recommended in the case of an IAF detected postoperatively in a low-volume center.
CLINICAL APPROACH
Intraoperative assessment of acetabular stability can be challenging. Indicators such as an abrupt shift in resistance during cup insertion, an insufficient press-fit, or failure to establish cup stability can be a strong indication of IAF. Thorough examination of the acetabular rim and floor, along with immediate intraoperative fluoroscopy is required for detection of such abnormalities. However, failure to detect IAF on radiographs is common, and the acetabular component may also appear stable. Therefore, meticulous stress testing for both the pelvis and the acetabular component becomes imperative. Use of fluoroscopy is critical, both with and without the presence of the acetabular component, for discernment of any differences in the radiographic appearance. Utilizing various imaging angles is recommended for a comprehensive assessment. In addition to an anteroposterior (AP) projection, oblique images of the hip, i.e., an ala and obturator projection (“Judet-views”), should be obtained. Use of the ala view can facilitate examination of the posterior column, encompassing the ilioischial line, anterior margin, medial wall, acetabular roof, and iliac crest. However, the obturator view is well-suited for examining the anterior column, including the iliopectineal line, posterior wall, and foramen obturatorum.
Postoperatively, clinical signs indicating the presence of IAF may manifest as diminished weight-bearing capacity, restricted range of motion, or persistent severe pain. Along with a routine clinical examination of the hip, a detailed pain history is required, including the localization, time of pain onset, and the impact of various therapeutic measures. Other causes of pain should be clarified (e.g., infection). Evaluation of the patient's ability to implement partial weight-bearing mobilization is also important.
Initial radiological diagnostics include standard plain radiographs in two planes (AP pelvis and frog leg/crosstable lateral view). Computed tomography is warranted in cases where the cause of pain remains unclear and for assessment of the fracture morphology—particularly concerning the posterior wall involvement or pelvic discontinuity.
CLASSIFICATION
Several classification systems with varying complexity and suitability for categorizing periprosthetic acetabular fractures detected during surgery or postoperatively have been proposed in recent years. Essentially, all segments of the acetabulum (e.g., acetabular roof, quadrilateral surface, posterior wall) and the adjacent hemipelvis (os ilium, os pubis, os ischium) can be involved; however, involvement is most often detected along the medial border of the acetabulum9).
Acetabular fractures have traditionally been classified on the anatomical basis of the two-column concept according to Letournel10). However, this does not address the equally important prosthetic component in addition to a detailed description of the fracture. The first system for classification of periprosthetic acetabular fractures, described in 1996 by Peterson and Lewallen9), divides these fractures into two groups: type 1, fractures with a stable acetabular component and type 2, fractures with an unstable acetabular component. Callaghan11) first divided intraoperative fractures into four groups based on in vitro studies: type A, anterior wall fracture; type B, transverse fracture; type C, inferior acetabular fracture; type D, posterior wall fracture. The classification system proposed by Della Valle et al.12) is the system most commonly used for classification of periprosthetic acetabular fractures. This comprehensive classification system encompasses all possible variations—whether a fracture occurs intraoperatively during insertion or removal of a component, as a result of trauma, spontaneously, or with pelvic discontinuity—extending beyond the scope of only classifying fractures that are detected intraoperatively.
• Type 1: Intraoperatively during component insertion
a. Recognized, stable component, undisplaced fracture
b. Recognized, displaced fracture, cup unstable
c. Not recognized intraoperatively
• Type 2: Intraoperatively during component removal
a. Less than 50% bone stock loss
b. Greater than 50% bone stock loss
• Type 3: Traumatic
a. Component stable
b. Component unstable
• Type 4: Spontaneous
a. Less than 50% bone stock loss
b. Greater than 50% bone stock loss
• Type 5: Pelvic discontinuity
a. Less than 50% bone stock loss
b. Greater than 50% bone stock loss
c. Associated with pelvic radiation
A newer system for classification introduced in 2018 by Pascarella et al.13) also considers both the timing of the fracture and stability of the implant. It provides a straightforward method for implementation with establishment of a corresponding treatment strategy. Another classification system, the Unified Classification System (UCS), was introduced in 2014 following the well-known AO classification with the goal of universal applicability across all periprosthetic fractures14). The UCS considers factors including implant stability, fracture location, and the anatomical characteristics of the fracture site.
SURGICAL MANAGEMENT
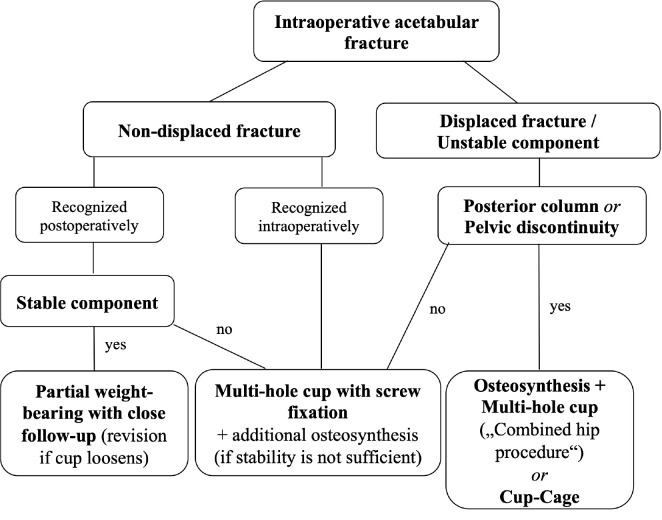
Fracture- and patient-related factors must be considered when making decisions regarding treatment and indications for surgical revision, including patient age, comorbidities, time of diagnosis, implant stability, bone quality, defect situation, and fracture pattern. A summary of the authors’ preferred treatment algorithm is shown in Fig. 1, which, however, cannot fully represent each individual case.
Fig. 1.
Proposed algorithm for treatment of intraoperative acetabular fractures.
Use of additional screws is recommended when IAF is detected during surgery. In such cases, a multi-hole revision cup is used as a plate, and multiple posterosuperior (ilium) and posteroinferior (ischium) bicortical screws are used to stabilize the component. While a study on undetected IAF (Della Valle and Paprosky type 1c) reported the same results as those for uncomplicated THA without further treatment15), another study reported a loosening rate of 100% for undetected IAF2). However, in a study reported by Yamamuro et al.15), screws were used primarily for fixation of the press-fit cup in the majority of patients. These divergent results can therefore be explained by the variety of possible fractures and implant types. We recommend additional screw fixation in any case of a suspected fracture, which can prevent early failure of the component in case of a fracture that cannot be confirmed with absolute certainty.
Conservative treatment of non-displaced intraoperative fractures with a stable acetabular component (Della Valle and Paprosky type 1a), only recognized postoperatively, with partial weight-bearing can be applied for several weeks. In such cases, a radiological assessment should be performed every 7-14 days. Fracture healing will occur in most cases, and loosening of the acetabular component can be an indication for acetabular revision (Fig. 2). However, early revision is indicated in the case of a posterior wall fracture with a large fragment (Fig. 3).
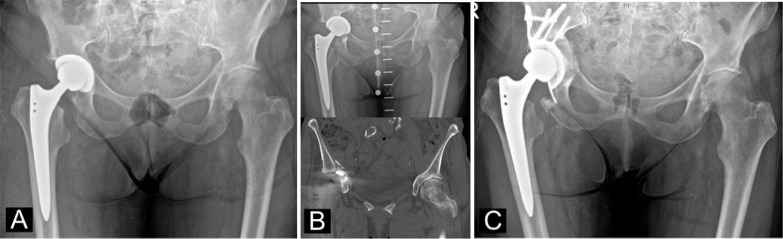
Fig. 2.
(A) Preoperative radiograph of a case of secondary osteoarthritis in Crowe IV dysplasia. (B) Total hip arthroplasty using a standard stem via a shortening osteotomy and a standard press-fit cup. A medialized acetabular component with a fracture of the quadrilateral surface can be observed. (C) After conservative treatment with six weeks of partial weight-bearing, a progressive acetabular protrusion was observed, thus revision was indicated.
Fig. 3.
(A) Postoperative radiograph of a total hip arthroplasty for treatment of primary osteoarthritis in a 52-year-old female patient. (B) Computed tomography eight weeks postoperatively for evaluation of persistent, severe pain showing a fracture of the posterior wall. (C) Immediate postoperative radiograph showing the acetabular revision with a multi-hole revision cup.
When managing a dislocated and/or unstable intraoperative fracture (Della Valle and Paprosky type 1b), removal of the component, visual registration of the fracture line, and acquisition of intraoperative images in different views (“Judet-views”) is initially required for assessing the integrity of the anterior and posterior column. Pelvic continuity is suspected in cases where significant displacement can be provoked at the fracture site. Thus, the use of a multihole cup as a plate may not be sufficient16). Likewise, it appears that in the case of a posterior wall fracture with a large fragment, the sole use of a multi-hole revision cup cannot be supported4,5). Osteosynthesis with reconstruction plates should be performed first in such cases. Repositioning the patient for additional posterior plating may be required when using an anterior or anterolateral approach. Osteosynthesis techniques may differ depending on the fracture type, and osteosynthesis of the posterior column is the most common. However, combined plating (anterior and posterior column – very rare) and anterograde or retrograde anterior or posterior column screw fixation are also an option. Selection of a suitable approach for the selected fixation is essential.
Although the indications for the sole use of antiprotrusio cages (Fig. 4) or a cup-cage reconstruction (Fig. 5) cannot currently be conclusively determined, they likely represent an important treatment option. Higher variability of the implantation technique with regard to the previously selected surgical approach appears to be favorable, while the mostly poor reduction of the fracture is discussed critically; in general, remaining defects are filled with autogenous or allogenous cancellous bone.
Fig. 4.
(A) Postoperative radiograph of a total hip arthroplasty (THA) for treatment of primary osteoarthritis in an 85-year-old female patient. (B) Radiograph and computed tomography one week postoperatively showing protrusion of the acetabular component and intraoperative acetabular fracture involving the medial wall and acetabular roof. (C) Immediate postoperative radiograph showing the revision THA using an antiprotrusio cage with impaction bone grafting.
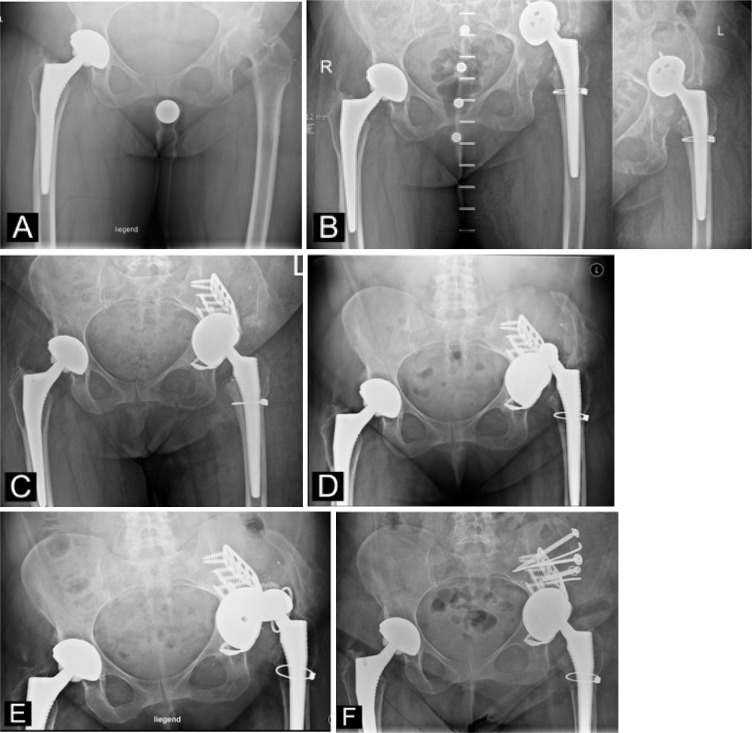
Fig. 5.
(A) Preoperative radiograph of a case of secondary osteoarthritis in a 55-year-old female patient. (B) Total hip arthroplasty (THA) was performed using a standard stem and cup. A cranialized acetabular component with a complex intraoperative acetabular fracture involving the anterior and posterior pillars can be observed. (C) Revision THA to a cup-cage construct with a dual-mobility cup was performed. (D) Early dislocation with revision to a constrained liner. (E) Re-dislocation with dislodgement of the constrained liner. (F) Revision with change to the dual mobility cup and bony refixation of the iliac crest with gluteus medius origin.
Appropriate revision implants can be used for treatment of an IAF in revision THA (Table 1). In our opinion, an additional plate osteosynthesis (so-called combined hip procedure) is only indicated in cases of interruption of the posterior column or a large posterior wall fragment. In cases of pelvic discontinuity, continuity of the hemipelvis must be restored to support stable cup anchorage with long-term osseointegration. The cup-cage technique may be a potential alternative to the “combined hip procedure” in such cases.
Table 1.
Implant Options for Management of Intraoperative Acetabular Fractures
| • Hemispherical (multi-hole) press-fit cup (jumbo cup if necessary) • Acetabular revision system (with augments if necessary) • Antiprotrusio cage (with augments if necessary) • Cup-cage-construct (for pelvic discontinuities) • Additional bone-grafting (autograft or allograft) • Additional plate osteosynthesis |
Partial to full weight-bearing on the operated leg may be allowed depending on the morphology of the fracture and the primary stability achieved. Mobilization is usually performed using a three-point gait with partial weight-bearing for six weeks. Weight-bearing can be increased after radiological follow-up.
PERIPROSTHETIC ACETABULAR FRACTURES WITH PELVIC DISCONTINUITY
To date, there is little evidence regarding the optimal treatment for IAF with pelvic discontinuity (Della Valle and Paprosky type 5). Achievement of primary stability of the acetabular component for long-term osseointegration is one of the challenges in management of acute acetabular fractures, particularly two-column fractures and T-shaped fractures with resulting pelvic discontinuity. There are three main surgical options: The combination of osteosynthesis and THA, the so-called combined hip procedure, endoprosthetic reconstruction using a conventional antiprotrusio cage (currently only recommended in geriatric cases), and the cup-cage construct.
Use of a cup-cage construct for acetabular fractures is described as follows.
Following exposure of the acetabulum and removal of the cup, the acetabulum may be prepared again by cup reaming down to the bottom of the fovea. A trial cup is used to determine the dimensions of the acetabular cavity. A cup that is 4-6 mm larger than the one corresponding to the acetabular defect without distraction should be selected. In general, a minimum outer diameter of 56 mm is required to facilitate a cup-cage construct. Additional holes are drilled ex situ at the edge of the tantalum cup using a drill or high-speed burr to maximize screw options for fixation of the cup to stable pelvic bone. Cancellous bone grafting can be performed at this site. The cup is usually placed in a vertical and retroverted position to maximize bone contact and allow for a good fit of the cage. The tantalum cup is screwed in the direction of the ilium, taking care to include both the stable parts of the pelvis as well as the anterior and posterior column, depending on the morphology of the fracture. In addition, screw fixation should be performed in the direction of the ischium and/or pubis for achievement of maximum anchorage.
The ring is then bent to obtain a suitable shape that matches the curvature of the ischium and ilium. Performing screw fixation in the direction that force is applied through the tantalum cup is important when fixing the ring to ensure a monolithic construct. Finally, cementing of the inlay is performed in the desired inclination and anteversion. Use of a dual-mobility cup is recommended to reduce the risk of dislocation.
OUTCOMES
Only small case series have been reported in the literature with various outcomes according to the anatomic location and severity of the IAF. Many IAFs are stable with stable implants and can thus be treated conservatively. Haidukewych et al.1) reported that the components were considered stable and no further treatment was required in 17 of 21 IAFs. In the four other cases, the unstable implant was replaced with a revision cup with a design allowing for additional screw fixation. Healing of fractures without revisions was reported in all cases. In the series reported by Sharkey et al.2), all IAF were initially considered stable. However, the press-fit of the cup was judged unsafe by the surgeon and the cup was fixed with additional screws in seven of nine cases where the fracture was detected intraoperatively. Healing of all intraoperatively diagnosed IAFs was reported, and no revisions were necessary. An association of the four undetected IAFs with secondary loosening was observed on the follow-up radiographs. The stability of the posterior column is an influential factor in the effort to achieve component stability4,5). Laflamme et al.5) reported a failure rate of 67% for IAF with an unstable posterior column, while safe osseointegration without further intervention was reported for patients with an intact posterior column. In the series reported by Brown et al.4), 69% of IAFs were not detected during surgery and revision was required for all fractures involving the posterior column.
IAFs rarely result in pelvic discontinuity requiring extensive cup revision. Only a few case series with short-term follow-up on patients treated using various reconstruction techniques have been reported in the literature6,16,17). The results were comparable to those reported for primary THA for treatment of acute acetabular fractures18-21) and acetabular revision for chronic pelvic discontinuity22-24), and are associated with a high risk of complications and revisions.
SUMMARY
Delayed diagnosis and treatment of IAFs, a rare complication of THA, can lead to complex revision scenarios. Management of an IAF can be challenging in terms of indication determination, surgical approach selection, implant choice, and technical execution. Accurate assessment of the fracture pattern and implant stability, along with a substantial background in performance of revision arthroplasty and fixation of acetabular fractures are essential for successful treatment. Fractures detected intraoperatively without involvement of the posterior column can be managed using a multi-hole cup with additional screw fixation. Conservative treatment with partial weight-bearing is a viable approach for management of fractures detected postoperatively without dislocation and posterior column involvement. Close radiographic monitoring should continue until fracture healing has been achieved. A combination of osteosynthesis with a revision cup or, alternatively, a cup-cage reconstruction is indicated in cases of pelvic discontinuity or fractures affecting the posterior column.
Funding Statement
Funding No funding to declare.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Haidukewych GJ, Jacofsky DJ, Hanssen AD, Lewallen DG. Intraoperative fractures of the acetabulum during primary total hip arthroplasty. J Bone Joint Surg Am. 2006;88:1952–6. doi: 10.2106/00004623-200609000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Sharkey PF, Hozack WJ, Callaghan JJ, et al. Acetabular fracture associated with cementless acetabular component insertion: a report of 13 cases. J Arthroplasty. 1999;14:426–31. doi: 10.1016/S0883-5403(99)90097-9. https://doi.org/10.1016/s0883-5403(99)90097-9. [DOI] [PubMed] [Google Scholar]
- 3.Kim YS, Callaghan JJ, Ahn PB, Brown TD. Fracture of the acetabulum during insertion of an oversized hemispherical component. J Bone Joint Surg Am. 1995;77:111–7. doi: 10.2106/00004623-199501000-00013. https://doi.org/10.2106/00004623-199501000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Brown JM, Borchard KS, Robbins CE, Ward DM, Talmo CT, Bono JV. Management and prevention of intraoperative acetabular fracture in primary total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2017;46:232–7. [PubMed] [Google Scholar]
- 5.Laflamme GY, Belzile EL, Fernandes JC, Vendittoli PA, Hébert-Davies J. Periprosthetic fractures of the acetabulum during cup insertion: posterior column stability is crucial. J Arthroplasty. 2015;30:265–9. doi: 10.1016/j.arth.2014.09.013. https://doi.org/10.1016/j.arth.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Desai G, Ries MD. Early postoperative acetabular discontinuity after total hip arthroplasty. J Arthroplasty. 2011;26:1570.e17–9. doi: 10.1016/j.arth.2010.12.021. https://doi.org/10.1016/j.arth.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 7.Dammerer D, Putzer D, Glodny B, et al. Occult intra-operative periprosthetic fractures of the acetabulum may affect implant survival. Int Orthop. 2019;43:1583–90. doi: 10.1007/s00264-018-4084-7. https://doi.org/10.1007/s00264-018-4084-7. [DOI] [PubMed] [Google Scholar]
- 8.Hasegawa K, Kabata T, Kajino Y, Inoue D, Tsuchiya H. Periprosthetic occult fractures of the acetabulum occur frequently during primary THA. Clin Orthop Relat Res. 2017;475:484–94. doi: 10.1007/s11999-016-5138-z. https://doi.org/10.1007/s11999-016-5138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson CA, Lewallen DG. Periprosthetic fracture of the acetabulum after total hip arthroplasty. J Bone Joint Surg Am. 1996;78:1206–13. doi: 10.2106/00004623-199608000-00011. https://doi.org/10.2106/00004623-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;(151):81–106. doi: 10.1097/00003086-198009000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Callaghan JJ. Periprosthetic fractures of the acetabulum during and following total hip arthroplasty. Instr Course Lect. 1998;47:231–5. doi: 10.2106/00004623-199709000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Della Valle CJ, Momberger NG, Paprosky WG. Periprosthetic fractures of the acetabulum associated with a total hip arthroplasty. Instr Course Lect. 2003;52:281–90. [PubMed] [Google Scholar]
- 13.Pascarella R, Sangiovanni P, Cerbasi S, et al. Periprosthetic acetabular fractures: a new classification proposal. Injury. 2018;49 Suppl 3:S65–73. doi: 10.1016/j.injury.2018.09.061. https://doi.org/10.1016/j.injury.2018.09.061. [DOI] [PubMed] [Google Scholar]
- 14.Duncan CP, Haddad FS. The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone Joint J. 2014;96-B:713–6. doi: 10.1302/0301-620X.96B6.34040. https://doi.org/10.1302/0301-620X.96B6.34040. [DOI] [PubMed] [Google Scholar]
- 15.Yamamuro Y, Kabata T, Kajino Y, Inoue D, Hasegawa K, Tsuchiya H. Does intraoperative periprosthetic occult fracture of the acetabulum affect clinical outcomes after primary total hip arthroplasty? Arch Orthop Trauma Surg. 2022;142:3497–504. doi: 10.1007/s00402-021-04226-y. https://doi.org/10.1007/s00402-021-04226-y. [DOI] [PubMed] [Google Scholar]
- 16.Rogers BA, Whittingham-Jones PM, Mitchell PA, Safir OA, Bircher MD, Gross AE. The reconstruction of periprosthetic pelvic discontinuity. J Arthroplasty. 2012;27:1499–506.e1. doi: 10.1016/j.arth.2011.12.017. https://doi.org/10.1016/j.arth.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 17.Takigami I, Ito Y, Mizoguchi T, Shimizu K. Pelvic discontinuity caused by acetabular overreaming during primary total hip arthroplasty. Case Rep Orthop. 2011;2011:939202. doi: 10.1155/2011/939202. https://doi.org/10.1155/2011/939202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin C, Caron J, Schmidt AH, Torchia M, Templeman D. Functional outcomes after total hip arthroplasty for the acute management of acetabular fractures: 1- to 14-year follow-up. J Orthop Trauma. 2015;29:151–9. doi: 10.1097/BOT.0000000000000164. https://doi.org/10.1097/BOT.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 19.De Bellis UG, Legnani C, Calori GM. Acute total hip replacement for acetabular fractures: a systematic review of the literature. Injury. 2014;45:356–61. doi: 10.1016/j.injury.2013.09.018. https://doi.org/10.1016/j.injury.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Borg T, Hernefalk B, Hailer NP. Acute total hip arthroplasty combined with internal fixation for displaced acetabular fractures in the elderly: a short-term comparison with internal fixation alone after a minimum of two years. Bone Joint J. 2019;101-B:478–83. doi: 10.1302/0301-620X.101B4.BJJ-2018-1027.R2. https://doi.org/10.1302/0301-620X.101B4.BJJ-2018-1027.R2. [DOI] [PubMed] [Google Scholar]
- 21.Malhotra R, Gautam D. Cup-cage construct using porous cup with Burch-Schneider cage in the management of complex acetabular fractures. Hip Pelvis. 2019;31:87–94. doi: 10.5371/hp.2019.31.2.87. https://doi.org/10.5371/hp.2019.31.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Konan S, Duncan CP, Masri BA, Garbuz DS. The cup-cage reconstruction for pelvic discontinuity has encouraging patient satisfaction and functional outcome at median 6-year follow-up. Hip Int. 2017;27:509–13. doi: 10.5301/hipint.5000480. https://doi.org/10.5301/hipint.5000480. [DOI] [PubMed] [Google Scholar]
- 23.Abolghasemian M, Tangsaraporn S, Drexler M, et al. The challenge of pelvic discontinuity: cup-cage reconstruction does better than conventional cages in mid-term. Bone Joint J. 2014;96-B:195–200. doi: 10.1302/0301-620X.96B2.31907. https://doi.org/10.1302/0301-620X.96B2.31907. [DOI] [PubMed] [Google Scholar]
- 24.Hipfl C, Janz V, Löchel J, Perka C, Wassilew GI. Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Joint J. 2018;100-B:1442–8. doi: 10.1302/0301-620X.100B11.BJJ-2018-0481.R1. https://doi.org/10.1302/0301-620X.100B11.BJJ-2018-0481.R1. [DOI] [PubMed] [Google Scholar]