Abstract
Purpose
Pelvis tilting in sagittal plane influences the acetabular cup position. Majority of total hip arthroplasty (THA) are performed in lateral decubitus surgical position. This study is to assess whether there is any difference in sacral slope between standing and lateral decubitus position and influence of this variation in planning acetabular cup anteversion.
Materials and Methods
This is a prospective study including 50 patients operated between January 2020 to March 2022. Preoperative radiograph included lumbosacral spine lateral X-ray in standing, supine and lateral decubitus positions to calculate the sacral slope for assessment of anterior or posterior pelvic tilting. In our study, we determined the position of the acetabular cup based on changes in sacral slope between standing and lateral decubitus postures. For patients whose sacral slope increased from lateral decubitus to standing, we implanted the acetabular component with a higher degree of anteversion. Conversely, for patients with reverse phenomenon, the cup was inserted at lower anteversion.
Results
Twenty-four patients (48.0%) had increase in sacral slope from lateral decubitus to standing whereas 26 patients (52.0%) had decrease in sacral slope. There was linear correlation between difference in preoperative sacral slope and postoperative cross table lateral cup anteversion. Harris hip scores improved from 40.78 to 85.43. There was no subluxation or dislocation in any patient at minimum 2-year follow-up.
Conclusion
Individualized acetabular cup placement is important for better functional outcome in THA. Evaluation of pelvic tilting in lateral decubitus position is necessary for better positioning of acetabular cup and avoid postoperative complications.
Keywords: Total hip arthroplasty, Acetabular cup placement, Sacral slope, Lateral decubitus
INTRODUCTION
Total hip arthroplasty (THA) is a routinely performed surgical procedure for the management of hip joint arthritis. The outcomes depend on precise positioning of the implant, stability of the joint, restoration of patient-specific biomechanics, and achievement of more favorable clinical results1).
Improper positioning of the components has been considered as the primary reason for most postoperative complications which include impingement, fracture of the ceramic liner, increased surface wear, aseptic loosening of components, and prosthesis dislocation, subsequently leading to an increased need for revision surgeries2-5). This ultimately results in decreased functional outcomes and poor patient satisfaction in the long term. Positioning of the acetabular component is considered as the most inconsistent aspect of THA6).
The pelvis tilts anteriorly in supine position and posteriorly in sitting position7). This dynamic phenomenon of pelvis tilting causes a decrease and increase in the acetabulum anteversion, respectively8) and understanding of this spinopelvic kinematics that influence the stability of the body while in various positions is important for effective preoperative planning of THA. Thus, placement of acetabular components based on the static position of the pelvis intraoperatively can result in impingement despite the placement being in the Lewinnek safe zone8). Therefore, orientation of the cup in a functional safe zone based on spinopelvic spatial orientation is essential9,10). There is intersubject variance in pelvic tilt as well as intrasubject variance depending on the postural changes8).
The most commonly used approaches for a THA are posterior or postero-lateral and modified Hardinge approach which requires a lateral decubitus position. However, the literature does not explain or describe the sacral slope and cup version changes in lateral decubitus position, which is the most frequently encountered position during surgery11).
The objective of this study is to determine whether there is any difference in sacral slope between the standing and lateral decubitus position and how this variation in sacral slope can influence the planning for acetabular cup version during performance of THA.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board approval from Busan Bumin Hospital (IRB No. 202403-BM-021).
This is a prospective observational study that included patients who underwent THA surgery between January 2020 to March 2022 in a single tertiary care center. Preoperative radiograph series included a pelvis with both hips, hip lateral and lumbosacral spine lateral X-ray in standing, supine and lateral decubitus positions for calculating the sacral slope. Sacral slope in lateral decubitus position was calculated again after positioning the patient in the operating room under C-arm guidance. Postoperatively, acetabular cup version was calculated in standing lateral and cross table lateral hip views.
Fifty patients with involvement of the unilateral hip who underwent uncemented THA between January 2020 to March 2022 were included in this study. Exclusion criteria were (1) patients undergoing bilateral or revision THA, (2) patients with dysplastic hips, and (3) patients with spinal imbalance or severe spinal disorders (degenerative and congenital). All surgeries were performed under spinal anesthesia using a minimally invasive posterior approach by a single experienced senior surgeon.
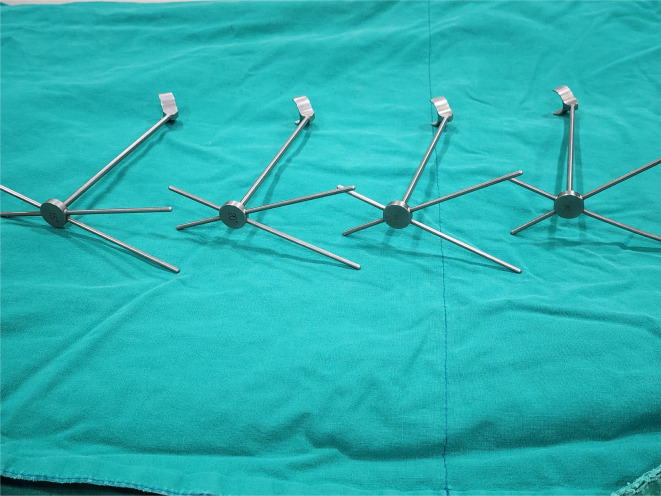
In our study, we planned the position of the acetabular cup based on the change in sacral slope from lateral decubitus posture (surgical position) to standing (functional position). In patients who showed an increase in the sacral slope from lateral decubitus to standing position, the acetabular component was implanted at a higher degree of anteversion to prevent anterior impingement of the component and posterior dislocation, whereas in those with the reverse phenomenon for the sacral slope, the cup was inserted at lower anteversion values to prevent posterior impingement and anterior dislocation while in the functional standing position. A change of one degree in sacral slope corresponded with 0.7° change in acetabulum cup version, with 30° being the mid reference value for cup version12). In such a case, the positioning of the implant would support better joint biomechanics and functional outcomes in terms of stability, mobility, and patient satisfaction. Acetabular component alignment guides from Corentec®, which are set at angles of 15°, 20°, 25°, and 30°, were used in the study (Fig. 1).
Fig. 1.
Acetabular component alignment guides from Corentec® (15°, 20°, 25°, and 30°).
The group included 24 males and 26 females with mean age of 56.33 years; the youngest patient was 24 years old and the eldest was 81 years of age. The indication for THA was primary osteoarthritis in nine patients, arthritis secondary to avascular necrosis of the femoral head in 39 patients, and post-traumatic arthritis of hip joint in two patients.
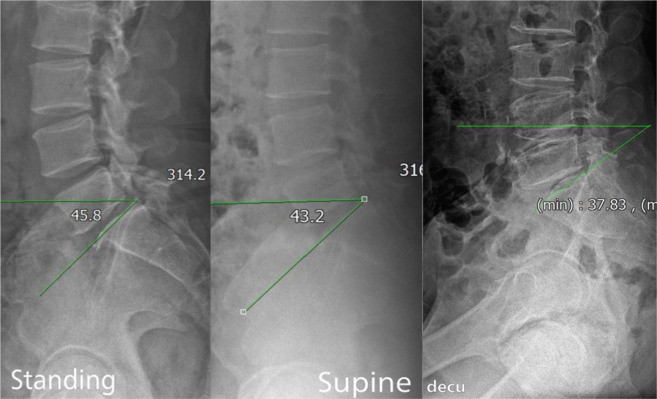
Written informed consent for inclusion in the study was obtained from all the patients. The parameters described by Lazennec et al.13) were used in the study. Sacral slope, which was measured in standing, supine, and lateral decubitus position, is defined as an angle formed between a line tangent to the upper end plate of S1 vertebra and the horizontal plane (Fig. 2).
Fig. 2.
Measuring sacral slope preoperatively in standing, supine, lateral decubitus.
True lateral radiographs of the lumbosacral spine were taken in standing, supine, and lateral decubitus position for each patient with the center of beam directed at the L4-L5 junction and the direction of the X-ray beam was kept vertical to the axial line of the patient. Keeping the same table, all radiographs were obtained at a focal film distance of 1.5 m. Reproducibility of the sagittal position has been previously validated, therefore, one standard radiograph was used for each patient14).
Lateral decubitus position was defined as a scenario where both the anterior superior iliac spine and both the shoulders are placed in the same vertical plane, in the same longitudinal axis as that of the operation bed and perpendicular to the floor with an X-ray taken aligning the mid coronal plane to that of the midline of the X-ray grid keeping both hips flexed to 20° and knees flexed to 30°. The pelvic sagittal plane should be parallel to the floor. The entire lumbar spine along with the sacro-coccygeal region should be visible in the radiograph.
Superimposition of the greater sciatic notches, the superior articulating facets and the superior and inferior endplates on a radiograph indicates achievement of a true lateral view.
For the standing radiograph, the subject stood in erect position with hip and knees extended, bare feet held together with symmetrical loading on both the feet and the upper limbs folded across the chest to minimize variation due to the effect of trunk posture on the lumbosacral spine.
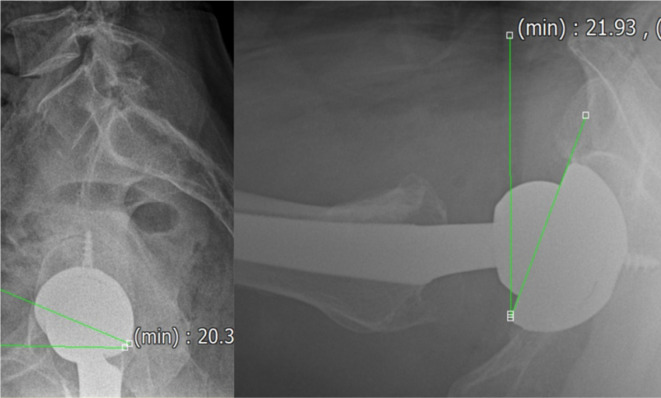
An angle formed by a horizontal line in the sagittal plane and a line tangent to the anterior and posterior edges of the acetabular cup is defined as surgical anteversion or acetabular tilt while in standing position. Acetabular anteversion was measured on the lateral radiographs in cross table lateral position using the Woo and Morrey method for measurement of acetabular version in the cross table lateral position15) (Fig. 3).
Fig. 3.
Measuring sacral slope preoperatively in standing, supine, lateral decubitus.
The cross table lateral projection for calculating acetabular cup version is taken with the patient in supine position and the limb is rotated internally by 15°-20°. The contralateral hip was flexed to 60° and the direction of the X-ray beam was parallel to the table, through the groin, directed 45° cephalad.
All values were measured by two observers, two times each, who worked independently. Measurements were performed using a digitized computer system PACS (picture archiving and communications system) version 5.1.3.2, Busan Bumin Hospital.
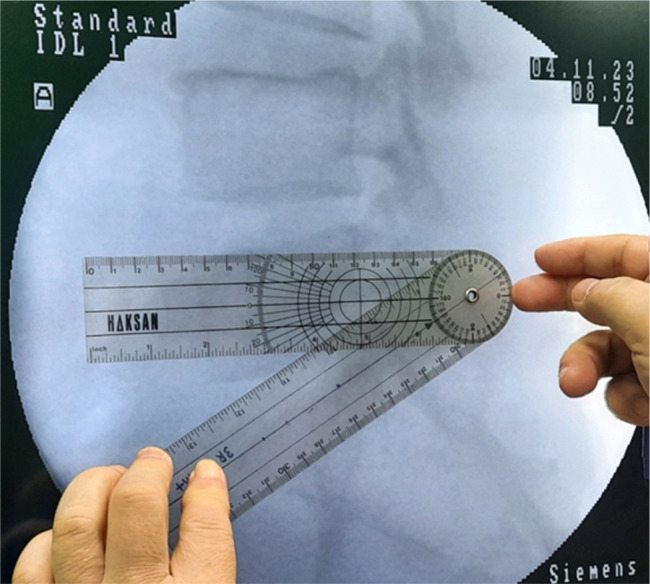
Spinal anesthesia was administered to all patients. After administration of anesthesia, the patient was positioned in lateral decubitus position as described above and supported anteriorly and posteriorly by well-padded posts (Fig. 4). Just before surgery, a lumbo-sacral spine lateral C-arm image was taken again in lateral decubitus position for assessment of the sacral slope and for planning final acetabular cup version (Fig. 5).
Fig. 4.
Patient is positioned in lateral decubitus position (surgical position).
Fig. 5.
Measuring the sacral slope of fluoroscopic image intraoperatively in lateral decubitus position.
Following standard prepping and draping, the incision was marked for the minimally invasive posterior approach, centering over the posterior edge of the greater trochanter and curving it supero-posteriorly and extending distally approximately 3 centimeters in each direction. In some obese patients the incision can be extended if necessary for adequate exposure of the acetabulum. Superficial and deep dissection was performed. Muscle fibers of the gluteus maximus were split in line with the skin incision, and the trochanteric bursa was excised. The piriformis tendon along with short external rotators was cut close to the point of insertion. A capsular incision was made and the hip joint was exposed and dislocated. The femoral neck cut was made. The acetabulum socket was prepared using serial successive reamers until punctate bleeding occurred.
The acetabular cup was positioned according to the preoperative plan based on patient specific change in the sacral slope from standing to lateral decubitus position between the range of 20° to 35° of anteversion. A mechanical standard version guide was used to assess the position of the acetabular component intraoperatively. The resulting functional cup anteversion in standing position would be between 25° to 30°. Femoral preparation was performed using a standard technique, maintaining stem anteversion at approximately 15°. Combined anteversion was maintained between 40° to 50°, which was evaluated using a coplanar test16).
Following insertion of trial implants, stability was evaluated in all planes to ensure that there was no dislocation or impingement. Following confirmation, final implants were press-fitted.
Local anesthetic infiltration was applied around the capsule and muscles. Short external rotators were sutured along with the posterior capsule to the greater trochanter using the standard Ranawat technique. The incision was closed in layers over a drain, and a sterile dressing was applied.
Postoperative care and rehabilitation were administered according to standard protocols.
All data was recorded in an excel spreadsheet. Pearson’s correlation coefficient was used to determine the correlation of change in the sacral slope with acetabular cup version. The analysis was performed using IBM SPSS Statistics for Windows (ver. 20.0; IBM Corp.). A P-value less than 0.05 was considered significant.
RESULTS
There was no statistically significant inter-observer and intra-observer variability (Table 1).
Table 1.
Comparative Reliability of Preoperative Sacral Slope and Postoperative Cup Version Measurements in Different Positions
| Preoperative sacral slope | Postoperative cup version | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Standing | Supine | Lateral decubitus | Standing | Cross-table lateral | ||||||||||
| Reading 1 | Reading 2 | Reading 1 | Reading 2 | Reading 1 | Reading 2 | Reading 1 | Reading 2 | Reading 1 | Reading 2 | |||||
| Inter-observer reliability | 0.997 | 0.992 | 0.991 | 0993 | 0.995 | 0.994 | 0.995 | 0.991 | 0.98 | 0.976 | ||||
| Intra-observer reliability | 0.995, 0.994 | 0.995, 0.989 | 0.994, 0.996 | 0.992, 0.992 | 0.981, 0.972 | |||||||||
| P-value | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | ||||
The mean sacral slope was 35.57° (range, 15.78°-53.66°) in standing, 30.45° (range, 12.67°-48.75°) in supine, and 34.74° (range, 9.00°-53.01°) in lateral decubitus position preoperatively with a mean difference of 0.83° in sacral slope on change of position from lateral decubitus to standing and of 5.12° from standing to supine position. This difference in sacral slope from standing to supine position was statistically significant with a P<0.05 and change of posture from standing to lateral decubitus was not statistically significant with P-value of 0.66.
Twenty-six patients (52.0%) showed an increase in sacral slope with a minimum increase of 0.16° and a maximum increase of 13.84° from lateral decubitus to standing, while a decrease in the sacral slope was observed for 24 patients (48.0%), ranging from 0.44° to 10.02° for the same change of posture.
The difference in sacral slope between standing and lateral decubitus position was greater than 10° in 10 patients (20.0%), between 5° to 10° in 14 patients (28.0%), and less than 5° in 26 patients (52.0%) (Table 2).
Table 2.
Variability in Cup Version Based on Differences in Sacral Slope from Standing to Lateral Decubitus Position
| Difference in sacral slope from lateral decubitus to standing lateral position | |||||
|---|---|---|---|---|---|
| >10° | 5° to 10° | 5° to –5° | –5° to –10° | <–10° | |
| No. of patients | 8 | 6 | 26 | 8 | 2 |
| Mean cup version in cross-table lateral X-ray (°) | 35.33 | 31.90 | 29.26 | 25.60 | 21.94 |
| Mean cup version in standing X-ray (°) | 27.74 | 28.46 | 29.57 | 29.73 | 28.57 |
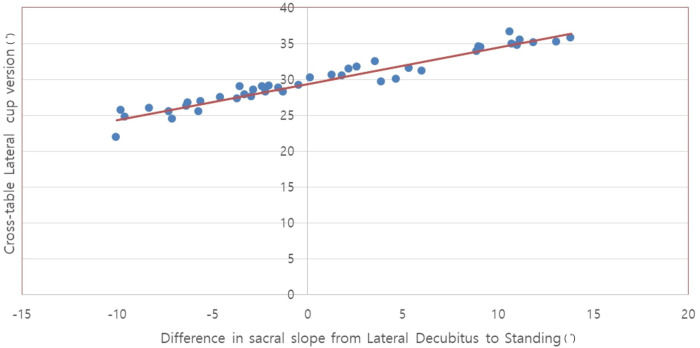
A linear correlation was observed between the difference in the preoperative sacral slope from lateral decubitus to standing position and postoperative acetabular cup version calculated in the cross-table lateral view of the hip with a correlation coefficient of 0.97 (Fig. 6). Clinically, this means that patients with more anterior pelvic tilting from lateral decubitus to standing position have shown a trend toward more postoperative acetabular cup anteversion calculated in cross table hip lateral view in our study.
Fig. 6.
Relationship between difference in sacral slope (from lateral decubitus to standing) versus crosstable lateral cup version.
The mean acetabular anteversion postoperatively, in cross table lateral view was 29.78° with a standard deviation of 3.66°, while in standing position was 28.91° with a standard deviation of 8.38°. The difference in means of anteversion between the two positions was 0.86° and was not statistically significant with a P-value of 0.50.
Harris hip scores calculated preoperatively and postoperatively were 40.78 and 85.43 respectively, which was statistically significant. No subluxation or dislocation was observed in any of our patients at a minimum follow-up of two years.
DISCUSSION
Instability of the hip joint has been regarded as the most common reason for revision THA. Therefore, accurate implant positioning is regarded as a fundamental part of any arthroplasty procedure, to ensure restoration of the joint biomechanics and for achievement of favorable results. Poor positioning is associated with an increased risk of impingement, subluxation/dislocation, and suboptimal clinical outcomes. Currently, most surgeons tend to place the components according to standard recommended positions or anatomic landmarks intra-op and tend to ignore the dynamic nature of the hip joint and its adaptability while assuming various body postures.
Spino-pelvic balance, a dynamic and individualized phenomenon, maintains body equilibrium throughout the change in posture from supine to standing and from standing to sitting7). Co-ordinated movements occurring in the spine, pelvis, and hip joint are required for achievement of this sagittal balance of body posture. Variations in one parameter can have a synchronous effect on others and knowledge regarding the interplay of these factors is essential for planning of component positioning in THA.
Shon et al.17), in their study concluded that movements of the sagittal plane of the pelvis cannot be overlooked during the planning stage. Lee et al.18) emphasized the importance of considering spino-pelvic balance during cup placement to prevent dislocation in THA and recommended preoperative radiographs of the spine and hip, in both standing and sitting position for preoperative assessment of the parameters described above.
Most literature provide an explanation of safe ranges for positioning the component in supine position, while according to records, maximum dislocations occur while in functional positions. Abdel et al.19), who examined patients with hip dislocation, observed that the acetabular cups were placed within the Lewinnek safe zone in the majority of patients19,20). Therefore, knowledge of postural kinematics that predispose for such dislocations is critical. Based on this background knowledge, DiGioia et al.21) described the concept of functional cup positioning which explains placement of the cup based on dynamics of the body, rather than just anatomical placement. Shon et al.17) suggested spine-pelvis lateral view in standing and supine position for analyzing adaptation of the acetabular cup with pelvic dynamics preoperatively. In addition, he also emphasized the role of the sagittal position of the pelvis in impingement and dislocation after total hip replacement17).
As change in the sacral slope has an intimate association with acetabular version dynamics, it is the simplest parameter that can be used to estimate a safe zone for placement of the acetabular cup. Some studies have reported on these types of changes in supine, standing, and sitting positions. However, although the most common surgical position is the lateral decubitus, assessment of change in the sacral slope from lateral decubitus to standing or supine and its impact on cup version has not been reported in the literature.
Reliability of calculating the sacral slope on radiographs in various functional positions as a guide for assessing pelvic kinematics was highlighted in a study by Shon et al.8). Stefl et al.15) also regarded sacral slope as the most precise method of assessing dynamic change in spino-pelvic motion. According to Lazennec et al.13), although sacral slope in sitting position is more reliable for lumbosacral joint mechanics, standing measurements are also sufficient for assessment of the above described kinetics. Meermans et al.22) also emphasized the adequacy of standing position in providing substantial information in THA.
In our study, we calculated the difference in sacral slope between lateral decubitus and standing position and the cup anteversion was planned accordingly. Twenty-six patients had cup insertion at ≥28° (The median value obtained in our study.) as the sacral slope increased from lateral decubitus to standing position. In addition, in twenty-four patients with a decrease in the sacral slope from lateral decubitus to standing position, the cup version was maintained below 28°. We also propose that patients with greater cup version have a more stable hip joint with optimum mobility during performance of daily activity in the Asian lifestyle. None of our patients presented with signs of definitive impingement or subluxation/dislocation of the hip joint within a minimum follow-up period of two years. The Harris hip scores improved from a mean of 40.78 preoperatively to 85.43 postoperatively.
In contrast to the Lewinnec safe zone proposition for positioning of the acetabular cup between 15°±10°, Mccollum and Gray23) proposed that the hip is most stable when allowing a physiological range of motion when the cup is positioned at 30°-50° abduction and 20°-40° of flexion. They did not observe any subluxation or dislocation in their patients during a six-year follow-up period15,23).
No outlier was observed in terms of implant positioning despite use of a minimally invasive postero-lateral approach in all patients. This could be due to the surgeon’s experience in the field of hip arthroplasty. According to Callanan et al.24), the results of analysis showed that the surgical approach was the only surgeon-related factor associated with cup malrotation and a minimally invasive approach was the least accurate.
According to a study reported by Brown et al.11), even use of intraoperative radiographs for assessment of component position was not reliable and beneficial, thus, its routine use is not recommended during performance of THA. Otero et al.6) observed wide fluctuations in pelvic alignment between preoperative anteroposterior and intraoperative lateral decubitus position X-rays. However, the limitations of their study were that they did not perform testing of inter-observer reliability of the method of measurement or even attempt to isolate the source of error as X-rays were not taken at the time of patient positioning before surgery6). These limitations were addressed in our study through testing of interobserver variability and taking X-rays prior to start of surgery after positioning the patient on the operating table.
Lazennec et al.25) observed bidirectional variations in sacral tilt from change in position from standing to supine position, which was also observed in our study.
Uemura et al.26), who also analyzed pelvic sagittal inclination in 422 patients, reported change up to 36.9° from change in supine to standing position. Similar to their results, fluctuation less than 10° was also observed for 40 patients (80.0%) in our study26). Comparative analysis was performed to observe the variations of sacral slope in different functional positions including standing, sitting, and supine as described in previously reported literature; lateral decubitus position was used as a reference position in our study8,27-32) (Table 3). Another study by Hepinstall et al.33) using robotic technology reported that consideration of preoperative functional pelvic position may result in improved postoperative placement of a functional acetabular component in THA. The fact that positioning of the patient during surgery can cause changes in rotation of the pelvis is a limitation of our study. However, this limitation can be controlled by proper fixing of the anterior and posterior preoperatively, asking the assistant to examine and correct pelvic rotation during surgery or by use of C-arm guidance. Despite obtaining good intra-observer and inter-observer reliability, some errors in measurement that could not be excluded could have occurred. Another limitation was the small sample size and short-term follow-up.
Table 3.
Comparison of Sacral Slope in Various Positions in Previous Studies
| Study | Sacral slope | |||
|---|---|---|---|---|
| Standing (°) | Sitting (°) | Supine (°) | Lateral (°) | |
| Our study | 35.57±8.31 | - | - | 34.74±10.41 |
| Shon et al.8) (2008) | 35.3 (13.4 to 50.5) | 14.9 (–25.6 to 40.1) | 40.9 (11.4 to 52.6) | 30.2 (15.5 to 51.2) |
| Chevillotte et al.27) (2018) | 37.1±6.3 | 11.3±10.8 | 41±7.2 | - |
| Watanabe et al.28) (2021) | 38±8.7 | 15±14 | - | - |
| Sun et al.29) (2022) | 34.8±7.1 (13.5 to 52.3) | 19.9±8.5 (0.9 to 42) | - | - |
| Philippot et al.30) (2009) | 42.4±12.6 | 21.2±11.6 | 43.9±11.1 | - |
| Sari-Ali et al.31) (2005) | 39.4 | 18.7 | - | - |
| Eddine et al.32) (2001) | 41.7 | - | 45.7 | - |
Values are presented as mean±standard deviation, mean (range), mean±standard deviation (range), or mean only.
CONCLUSION
Precise and individualized acetabular cup version is important for achievement of more favorable functional outcomes in THA and to minimize postoperative complications of variance in pelvic tilt between standing, supine, and lateral decubitus position. Therefore, evaluation of pelvic tilting in lateral decubitus position is required preoperatively, particularly for patients undergoing THA using a posterior or postero-lateral approach and a modified Hardinge’s approach.
To examine the dynamics in pelvic tilt described above, we recommend obtaining standing, supine, and lateral decubitus sagittal views preoperatively and obtaining another lateral decubitus radiograph after positioning the patient, prior to surgery intraoperatively under C-arm guidance to determine the difference in sacral slope and to minimize intra and inter-subjective variability.
Funding Statement
Funding No funding to declare.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Weber M, Grifka J, Renkawitz T. Patient-specific restoration of biomechanics in total hip arthroplasty. Z Orthop Unfall. 2019;157:292–9. doi: 10.1055/a-0725-8527. https://doi.org/10.1055/a-0725-8527. [DOI] [PubMed] [Google Scholar]
- 2.D'Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW., Jr The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–21. doi: 10.2106/00004623-200003000-00003. https://doi.org/10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–4. doi: 10.1016/S0883-5403(98)90052-3. https://doi.org/10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 4.Kummer FJ, Shah S, Iyer S, DiCesare PE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty. 1999;14:509–13. doi: 10.1016/S0883-5403(99)90110-9. https://doi.org/10.1016/s0883-5403(99)90110-9. [DOI] [PubMed] [Google Scholar]
- 5.Patil S, Bergula A, Chen PC, Colwell CW, Jr, D'Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85-A Suppl 4:56–63. doi: 10.2106/00004623-200300004-00007. https://doi.org/10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 6.Otero JE, Fehring KA, Martin JR, Odum SM, Fehring TK. Variability of pelvic orientation in the lateral decubitus position: are external alignment guides trustworthy? J Arthroplasty. 2018;33:3496–501. doi: 10.1016/j.arth.2018.07.021. https://doi.org/10.1016/j.arth.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 7.Aguilera-Bohórquez B, Corea P, Sigüenza C, Gerstner-Saucedo J, Carvajal A, Cantor E. Relationship between spinopelvic parameters and hip function in patients with femoroacetabular impingement at diagnosis: a cross-sectional study. Hip Pelvis. 2023;35:6–14. doi: 10.5371/hp.2023.35.1.6. https://doi.org/10.5371/hp.2023.35.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shon WY, Gupta S, Biswal S, et al. Validation of a simple radiographic method to determine variations in pelvic and acetabular cup sagittal plane alignment after total hip arthroplasty. Skeletal Radiol. 2008;37:1119–27. doi: 10.1007/s00256-008-0550-4. https://doi.org/10.1007/s00256-008-0550-4. [DOI] [PubMed] [Google Scholar]
- 9.Tezuka T, Heckmann ND, Bodner RJ, Dorr LD. Functional safe zone is superior to the Lewinnek safe zone for total hip arthroplasty: why the Lewinnek safe zone is not always predictive of stability. J Arthroplasty. 2019;34:3–8. doi: 10.1016/j.arth.2018.10.034. https://doi.org/10.1016/j.arth.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Dorr LD, Callaghan JJ. Death of the Lewinnek "Safe Zone". J Arthroplasty. 2019;34:1–2. doi: 10.1016/j.arth.2018.10.035. https://doi.org/10.1016/j.arth.2018.10.035. [DOI] [PubMed] [Google Scholar]
- 11.Brown NM, McDonald JF, 3rd, Sershon RA, Hopper RH., Jr The effect of intraoperative radiographs on component position and leg length during routine posterior approach total hip arthroplasty. Hip Pelvis. 2021;33:128–39. doi: 10.5371/hp.2021.33.3.128. https://doi.org/10.5371/hp.2021.33.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Niemeier TE, Wills BW, Theiss SM, Strom SF. Sagittal pelvic kinematics in hip arthroplasty. Curr Rev Musculoskelet Med. 2020;13:240–6. doi: 10.1007/s12178-020-09628-w. https://doi.org/10.1007/s12178-020-09628-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazennec JY, Charlot N, Gorin M, et al. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004;26:136–44. doi: 10.1007/s00276-003-0195-x. https://doi.org/10.1007/s00276-003-0195-x. [DOI] [PubMed] [Google Scholar]
- 14.Mayr E, Kessler O, Prassl A, Rachbauer F, Krismer M, Nogler M. The frontal pelvic plane provides a valid reference system for implantation of the acetabular cup: spatial orientation of the pelvis in different positions. Acta Orthop. 2005;76:848–53. doi: 10.1080/17453670510045471. https://doi.org/10.1080/17453670510045471. [DOI] [PubMed] [Google Scholar]
- 15.Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017;99-B(1 Supple A):37–45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0415.R1. [DOI] [PubMed] [Google Scholar]
- 16.Kittanakere SR, Kohli R, Shah HM, Shetty N, Bhonsle RP, Sivakanthan A. Factors affecting demonstration of intra-operative Co-planar test in Total Hip Arthoplasty. J Kar Orth Assoc. 2018;6:35–8. [Google Scholar]
- 17.Shon WY, Sharma V, Keon OJ, Moon JG, Suh DH. Can pelvic tilting be ignored in total hip arthroplasty? Int J Surg Case Rep. 2014;5:633–6. doi: 10.1016/j.ijscr.2014.07.015. https://doi.org/10.1016/j.ijscr.2014.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee SH, Lim CW, Choi KY, Jo S. Effect of spine-pelvis relationship in total hip arthroplasty. Hip Pelvis. 2019;31:4–10. doi: 10.5371/hp.2019.31.1.4. https://doi.org/10.5371/hp.2019.31.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res. 2016;474:386–91. doi: 10.1007/s11999-015-4432-5. https://doi.org/10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCarthy TF, Alipit V, Nevelos J, Elmallah RK, Mont MA. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplasty. 2016;31(9 Suppl):264–8. doi: 10.1016/j.arth.2016.01.067. https://doi.org/10.1016/j.arth.2016.01.067. [DOI] [PubMed] [Google Scholar]
- 21.DiGioia AM, Jaramaz B, Blackwell M, et al. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998;(355):8–22. doi: 10.1097/00003086-199810000-00003. https://doi.org/10.1097/00003086-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Meermans G, Grammatopoulos G, Innmann M, Beverland D. Cup placement in primary total hip arthroplasty: how to get it right without navigation or robotics. EFORT Open Rev. 2022;7:365–74. doi: 10.1530/EOR-22-0025. https://doi.org/10.1530/EOR-22-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;(261):159–70. doi: 10.1097/00003086-199012000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Callanan MC, Jarrett B, Bragdon CR, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–29. doi: 10.1007/s11999-010-1487-1. https://doi.org/10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lazennec JY, Brusson A, Rousseau MA. Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthop Traumatol Surg Res. 2013;99(1 Suppl):S87–103. doi: 10.1016/j.otsr.2012.12.003. https://doi.org/10.1016/j.otsr.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Uemura K, Takao M, Otake Y, et al. Change in pelvic sagittal inclination from supine to standing position before hip arthroplasty. J Arthroplasty. 2017;32:2568–73. doi: 10.1016/j.arth.2017.03.015. https://doi.org/10.1016/j.arth.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 27.Chevillotte T, Coudert P, Cawley D, et al. Influence of posture on relationships between pelvic parameters and lumbar lordosis: comparison of the standing, seated, and supine positions. A preliminary study. Orthop Traumatol Surg Res. 2018;104:565–8. doi: 10.1016/j.otsr.2018.06.005. https://doi.org/10.1016/j.otsr.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 28.Watanabe S, Choe H, Kobayashi N, Ike H, Kobayashi D, Inaba Y. Prediction of pelvic mobility using whole-spinal and pelvic alignment in standing and sitting position in total hip arthroplasty patients. J Orthop Surg (Hong Kong) 2021;29:23094990211019099. doi: 10.1177/23094990211019099. https://doi.org/10.1177/23094990211019099. [DOI] [PubMed] [Google Scholar]
- 29.Sun Z, Zhou S, Jiang S, Zou D, Yu M, Li W. Variations of sagittal alignment in standing versus sitting positions under the Roussouly classification in asymptomatic subjects. Global Spine J. 2022;12:772–9. doi: 10.1177/2192568220962436. https://doi.org/10.1177/2192568220962436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Philippot R, Wegrzyn J, Farizon F, Fessy MH. Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Orthop Traumatol Surg Res. 2009;95:70–6. doi: 10.1016/j.otsr.2008.01.001. https://doi.org/10.1016/j.otsr.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Sari-Ali E, Lazennec J, Morin M, Saillant G. [Comparative study of sagittal lumbo-pelvic balance values between the standing and seated positions. The lumbo-pelvic complex] Sauramps; 2005. pp. 35–46. French. [Google Scholar]
- 32.Eddine TA, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup. Surg Radiol Anat. 2001;23:105–10. doi: 10.1007/s00276-001-0105-z. https://doi.org/10.1007/s00276-001-0105-z. [DOI] [PubMed] [Google Scholar]
- 33.Hepinstall MS, Coden G, Salem HS, Naylor B, Matzko C, Mont MA. Consideration of pelvic tilt at the time of preoperative planning improves standing acetabular position after robotic-arm assisted total hip arthroplasty. Hip Int. 2023;33:47–52. doi: 10.1177/11207000211038670. https://doi.org/10.1177/11207000211038670. [DOI] [PubMed] [Google Scholar]