Abstract
Background:
Common carotid artery occlusion (CCAO) sometimes requires vascular reconstruction. Ipsilateral superficial temporal artery (STA)-middle cerebral artery (MCA) bypass is unsuitable due to insufficient blood flow to the external carotid artery. The bonnet bypass, one treatment option for CCAO, requires a long coronal incision and bone groove to prevent malposition and collapse of an interposition graft. However, this long incision might lead to skin complications and reduced collateral blood flow.
Methods:
A 60-year-old man who experienced recurrent ischemic stroke presented with the right internal carotid artery occlusion and left CCAO. The left STA was unavailable; however, both branches of his right STA were well-developed. Minimizing skin invasion was a priority because the patient had diabetes mellitus. We performed a right STA parietal branch – right MCA anastomosis, followed by a right STA frontal branch – left radial artery graft (RAG) – left MCA bonnet bypass using small intermittent skin incisions.
Results:
We drilled a bone groove extending across the entire length of the interposition graft through the small intermittent skin incisions. Furthermore, we applied a right STA-RAG end-to-side anastomosis instead of an endto-end anastomosis to preserve collateral skin anastomosis. Postoperatively, the bypass remained patent, and the patient was discharged without complications.
Conclusion:
The bonnet bypass is a potential treatment for CCAO, but the procedure is invasive. Our modified bonnet bypass method enables less invasive management, preventing collapse and malposition of the interposition graft and minimizing skin complications.
Keywords: Common carotid artery occlusion, Intermittent skin incision, Interposition graft, Modified bonnet bypass, Subcutaneous tunnel
INTRODUCTION
Common carotid artery occlusion (CCAO) can cause cerebral ischemic stroke and requires vascular reconstruction.[3] However, the ipsilateral superficial temporal artery (STA)-middle cerebral artery (MCA) bypass technique cannot be applied due to insufficient blood flow to the external carotid artery. The bonnet bypass has been identified as a revascularization technique for CCAO.[4,10] An interposition graft beneath the skin flap is needed, but it easily collapses under skin flap pressure or malposition. A bone groove corridor for interposition graft is protective; however, a long coronal skin incision is needed to drill the bone groove.[11] However, this coronal skin incision is invasive and may cause non-fusion of sutures or damage to skin collateral anastomosis. Here, we report a case of CCAO treated with a less invasive bonnet bypass technique.
CASE REPORT
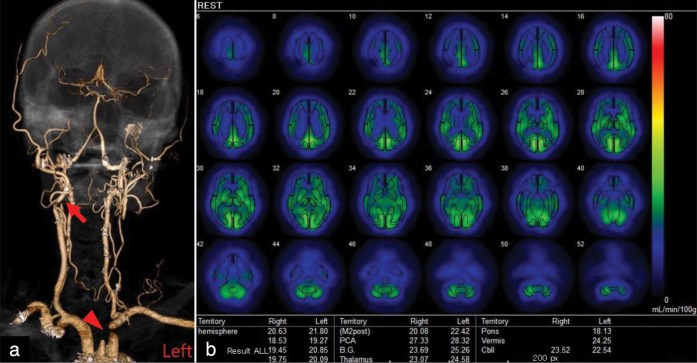
A 60-year-old man with bilateral carotid artery occlusion was admitted to our hospital for surgical treatment. He had experienced recurrent minor ischemic stroke and had undergone dual platelet drug therapy. Head-and-neck three-dimensional computed tomography angiography (3DCTA) showed right internal carotid artery occlusion and left CCAO [Figure 1a]. Head spectroscopy showed a general decrease in blood flow in the bilateral hemisphere [Figure 1b]. The patient had diabetes mellitus and was on antidiabetic medication. We decided to perform vascular reconstruction surgery, but the left STA was unavailable due to left CCAO. Fortunately, the frontal and parietal branches of the right STA were well-developed. An echograph showed the patency of the left radial artery, with a distal diameter of 2.4 mm. Allen’s test revealed no complications. We planned a two-staged surgery: First, we planned a right STA parietal branch-right MCA anastomosis. Subsequently, we planned a right STA frontal branch – left radial artery graft (RAG) – left MCA bonnet bypass.
Figure 1:
(a) Three-dimensional computed tomography angiography showed right internal carotid artery occlusion (arrow) and left common carotid artery occlusion (arrowheads). (b) Spectroscopy showed a general decrease in bilateral cerebral blood flow. The colored bar on the right side indicated the degree of cerebral blood flow.
Operation
First, a right STA frontal branch to the right MCA M4 branch anastomosis was performed. We created a short linear skin incision directly over the parietal branch distal to the junction of the frontal and parietal branches to prevent frontal branch injury. The first operation was performed without any complications. The clamp time for the MCA was 15 min. During outpatient follow-up, the patient developed bilateral chronic subdural hematomas. We performed burr-hole irrigation surgery twice, with maximum attention to preserve the STA frontal branch. Nine months after the first STA-MCA bypass surgery, we finally operated the right STA frontal branch – RAG – left MCA bonnet bypass.
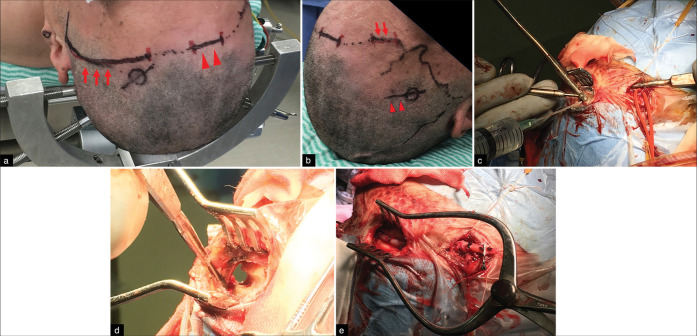
The head was fixed in a neutral position with the Sugita multipurpose head frame (Mizuho Medical Co. Ltd, Tokyo, Japan). This device enabled us to rotate the head approximately 30° in clockwise and counterclockwise directions [Figure 2a]. We rotated the head approximately 30° to the left from the neutral position to harvest the right STA frontal branch. We harvested the right STA frontal branch on the right forehead through an approximately 3 cm short linear skin incision to avoid skin complications [Figure 2b]. After harvesting the STA, we rotated the head frame in a reverse direction. Subsequently, a left frontotemporal craniotomy with a curved skin incision was performed. Before opening the dura mater, we drilled a bone groove extending across the entire length of the interposition graft to prevent collapse and malposition. Due to the long length of the subcutaneous bone groove, a reentry point was necessary to complete the drilling. We made another 3 cm skin incision midway between the foreheads, serving as a reentry point to drill the bone groove. During drilling, the skin flap was elevated using a muscle hook or spatula, and the subcutaneous frontal bone was horizontally drilled [Figure 2c and d].
Figure 2:
(a) The head is fixed with a rotatable head frame. The red arrow shows the planned skin incision line for the left frontotemporal craniotomy (arrows). The intermittent short skin incisions for creating the subcutaneous bone groove are visible on the median forehead (arrowheads). (b) The superficial temporal artery frontal branch on the right forehead was harvested through an approximately 3 cm linear skin incision. The planned harvest site is marked with a red line (arrows). The surgical wound from a previous burr-hole irrigation surgery for chronic subdural hematoma is visible in the center of the picture (arrowheads). (c) The procedure of bone groove drilling. The subcutaneous bone groove was drilled through intermittent short skin incisions. A spatula was used to elevate the skin during the drilling of the bone groove. (d) Magnified horizontal view of the subcutaneous bone groove. The bone groove extended over almost the entire length of the interposition graft, preventing graft collapse and malposition. (e) The radial artery graft (RAG) was pulled through the bone groove, fitting perfectly into the RAG.
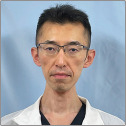
After completing the subcutaneous bone groove, we pulled the RAG through it. The bone groove seemed to fit perfectly to the RAG [Figure 2e]. After pressure distention with heparinized saline, we performed the RAG-left M4 end-to-side anastomosis [Figure 3a]. The total clamp time was 26 min. Subsequently, we conducted the RAG-right STA frontal branch end-to-side anastomosis to preserve the STA collateral flow to the skin [Figure 3b]. An indocyanine green video angiogram showed perfect patency of the bypass graft.
Figure 3:
(a) Intraoperative view of the radial artery graft (RAG) – left M4 end-to-side anastomosis. (b) Intraoperative view of the right superficial temporal artery (STA) frontal branch-RAG end-to-side anastomosis. The distal part of the STA frontal branch was preserved (Black arrow).
The postoperative course was uneventful, with 3DCTA showing excellent bypass patency [Figure 4a and b]. The patient was followed up at the outpatient clinic without additional neurological deficits. Figure 5 depicts the schematic image of the surgical field.
Figure 4:
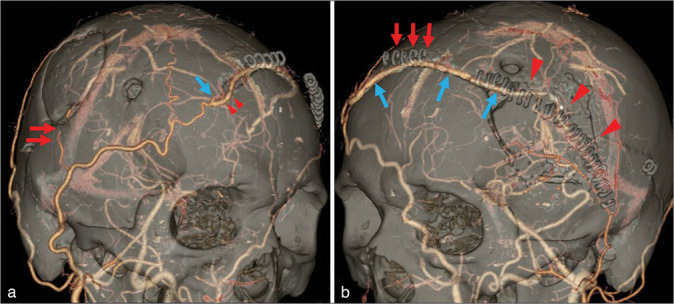
(a) Postoperative three-dimensional computed tomography angiography (3DCTA) right oblique view. The right superficial temporal artery (STA) parietal branch-M4 bypass of the first operation was patent (red arrows). The right STA frontal branch – radial artery interposition graft end-to-side anastomosis was also patent (arrowheads). The distal part of the right STA frontal branch was preserved due to the end-to-side anastomosis (blue arrow). (b) The left anterior oblique view of the postoperative 3DCTA. Residual skin staples on the medial forehead show the intermittent small skin incision for the reentry point (arrows). Residual skin staples on the left frontotemporal head show the skin incision for the left frontotemporal craniotomy (arrowheads). The bonnet bypass is perfectly patent (blue arrows).
Figure 5:
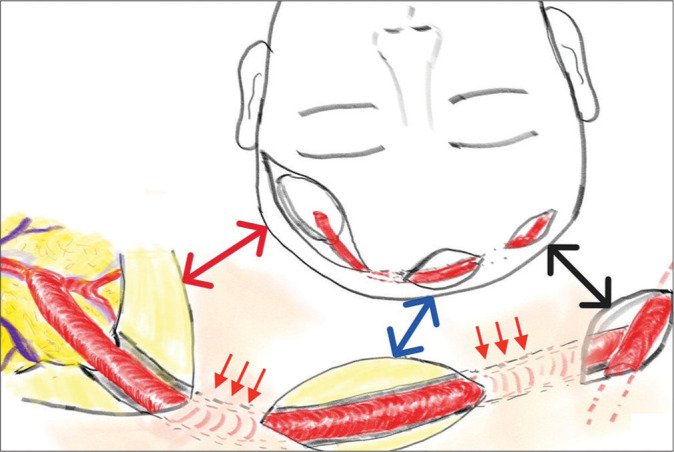
Schematic representation of our modified bonnet bypass. The red left-right arrow shows the left frontotemporal craniotomy and radial artery graft (RAG)-left M4 anastomosed part. The blue left-right arrow shows the intermittent skin incision for the reentry point. The black left-right arrow shows the right superficial temporal artery frontal branch-RAG end-to-side anastomosed part. Red arrows show the subcutaneous tunnel part.
DISCUSSION
CCAO is relatively rare, and standard revascularization is not applicable due to STA unavailability.[2] Various treatment options, including the bonnet bypass, have been reported.[6,10] When employing an interposition graft, caution must be exercised to prevent malposition, skin flap pressure, and graft injury.[5] Previous studies have reported the effectiveness of fixing and protecting bypass grafts with a bone groove in the skull and microplates.[11] Another study also reported that a bone groove was used as a conduit for saphenous vein grafts.[9] In these studies, bilateral coronal skin incision was performed. In contrast, we used a subcutaneous tunnel and small linear skin incisions instead of bilateral coronal skin incisions. The use of ring-reinforced artificial vascular graft tunnels might prevent an interposition graft from collapsing under the skin flap, although it may cause infection or thinning of the skin flap.[8] We implemented a subcutaneous bone groove extending the entire length of the interposition graft to mitigate the risk of graft collapse and malposition.
Utilizing intermittent short skin incisions as reentry points enabled the drilling of the entire length of the bone groove without resorting to a long coronal skin incision. Our method, which aids in fixing and protecting the interposition graft, is less invasive than conventional bonnet bypass procedures. Moreover, we opted for end-to-side anastomosis between the donor STA and RAG to preserve blood flow to the skin flap instead of end-to-end anastomosis. Our method enables the preservation of collateral blood flow from the donor STA to the orbit or skin flap, potentially reducing skin complications and ischemic oculopathy.[1,7]
The bonnet bypass procedure is complicated. The previous studies have described the position of the patient as supine lateral, with the head fixed on the horse-shoe headrest and rotated in the opposite direction during the operation.[11] This positioning allows for a horizontal surgical field, facilitating easier anastomosis. However, another draping might be needed after rotating the head, raising concerns about infection risks. In our case, the patient was positioned supine, with the head fixed in a neutral position, using a rotatable frame. This frame simplifies the rotation of the head in clockwise and counterclockwise directions. However, the surgical field was steeply sloped; hence, we performed anastomosis on a nearly perpendicular plane. Therefore, the procedure used in our study might pose difficultly compared with those used in previous studies.[11]
CONCLUSION
The conventional bonnet bypass is a potential treatment for CCAO, but the procedure is complicated and invasive. Our modified bonnet bypass procedure, utilizing an intermittent tunneling method, allows for a less invasive approach while preventing the collapse and malposition of the interposition graft. Furthermore, this approach preserves collateral anastomosis in the skin.
Footnotes
How to cite this article: Sakamoto Y, Okamoto S, Saito R. Less invasive bonnet bypass with subcutaneous tunneling method for common carotid artery occlusion – A technical note. Surg Neurol Int. 2024;15:300. doi: 10.25259/SNI_528_2024
Contributor Information
Yusuke Sakamoto, Email: usakamoto420@gmail.com.
Sho Okamoto, Email: okamoto88kun@yahoo.co.jp.
Ryuta Saito, Email: ryuta@med.nagoya-u.ac.jp.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Alizai AM, Trobe JD, Thompson BG, Izer JD, Cornblath WT, Deveikis JP. Ocular ischemic syndrome after occlusion of both external carotid arteries. J Neuroophthalmol. 2005;25:268–72. doi: 10.1097/01.wno.0000189831.92504.2d. [DOI] [PubMed] [Google Scholar]
- 2.Belczak S, Mulatti GC, Abrão SR, da Silva ES, Aun R, Puech-Leão P, et al. Common carotid artery occlusion: A single-center experience in 40 cases. Int J Angiol. 2016;25:39–43. doi: 10.1055/s-0035-1547340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belkin M, Mackey WC, Pessin MS, Caplan LR, O’Donnell TF. Common carotid artery occlusion with patent internal and external carotid arteries: Diagnosis and surgical management. J Vasc Surg. 1993;17:1019–27. discussion 1027-8. [PubMed] [Google Scholar]
- 4.Deshmukh VR, Porter RW, Spetzler RF. Use of. “bonnet” bypass with radial artery interposition graft in a patient with recurrent cranial base carcinoma: Technical report of two cases and review of the literature. Neurosurgery. 2005;56:E202. doi: 10.1227/01.neu.0000144492.42325.34. [DOI] [PubMed] [Google Scholar]
- 5.Garrido E, Freed MH. Fatal complication of the “bonnet bypass”: Case report. Neurosurgery. 1983;13:320–1. doi: 10.1227/00006123-198309000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Hecht N, Wessels L, Fekonja L, von Weitzel-Mudersbach P, Vajkoczy P. Bypass strategies for common carotid artery occlusion. Acta Neurochir (Wien) 2019;161:1993–2002. doi: 10.1007/s00701-019-04001-4. [DOI] [PubMed] [Google Scholar]
- 7.Kawaguchi S, Iida JI, Uchiyama Y. Ocular circulation and chronic ocular ischemic syndrome before and after carotid artery revascularization surgery. J Ophthalmol. 2012;2012:350475. doi: 10.1155/2012/350475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kazumata K, Asaoka K, Yokoyama Y, Sugiyama T, Kaneko S, Itamoto K. “Isolated carotid bifurcation” and vertebral-carotid artery bypass for common carotid artery occlusion. Neurol Med Chir (Tokyo) 2013;53:179–82. doi: 10.2176/nmc.53.179. [DOI] [PubMed] [Google Scholar]
- 9.Morgan MK, Brennan J, Day MJ. Interposition saphenous vein bypass graft between the common and intracranial internal carotid arteries. J Clin Neurosci. 1996;3:272–80. doi: 10.1016/s0967-5868(96)90065-x. [DOI] [PubMed] [Google Scholar]
- 10.Spetzler RF, Roski RA, Rhodes RS, Modic MT The. “bonnet bypass”. Case report. J Neurosurg. 1980;53:707–9. doi: 10.3171/jns.1980.53.5.0707. [DOI] [PubMed] [Google Scholar]
- 11.Toyota S, Iwaisako K, Wakayama A, Yoshimine T. Fixation and protective method for the interposition graft in bonnet bypass--technical note. Neurol Med Chir (Tokyo) 2010;50:263–6. doi: 10.2176/nmc.50.263. [DOI] [PubMed] [Google Scholar]