Abstract
Introduction:
Open clavicle fractures are rare, and there are no current reported cases in the literature of a missed open clavicle with resultant fracture-related infection and osteomyelitis.
Case Report:
We present a 65-year-old female with no reported medical history, who presented to our institution with left clavicular pain and wound drainage 8 days after she was struck by a motor vehicle in her home country of Guyana. She was found to have a missed open clavicle fracture with an associated severe infection. She was subsequently treated with irrigation, debridement, and distal clavicle excision.
Conclusion:
We present this unique case with a potential procedure which could prove beneficial in cases of infection, trauma, or oncologic lesions in which the distal clavicle is deemed unsalvageable.
Keywords: Open clavicle fracture, missed open fracture, distal clavicle excision, osteomyelitis, clavicular osteomyelitis, neglected fracture, bone infection
Learning Point of the Article:
Open fractures of the clavicle are rare, and very little is reported on appropriate management, especially in the delayed setting with associated infection. In this article, we present resection of the distal clavicle as a potential procedure in the setting large segment of associated necrotic bone.
Introduction
Open clavicle fractures are rare, with a reported incidence of 1.8% of all clavicle fractures. These fractures are more common in the younger patients as a result of high-energy trauma, and very rare in the elderly population [1]. The general standard of care treatment of open fractures throughout the body is early antibiotics within 1 h, followed by irrigation and debridement within 6–12 h, and internal fixation [2, 3]. However, management becomes much less standardized when the patient presents in a delayed fashion.
There is a paucity of literature in orthopedics regarding appropriate management techniques of open clavicle in the setting of delayed presentation. To the best of our knowledge, no cases have been reported of a missed open clavicle fracture with an associated infection. Our patient presents a unique clinical conundrum due to the severe fracture-related infection and osteomyelitis with devitalized bone.
Open fractures are the most common cause of osteomyelitis in the adult population. Osteomyelitis after an open fracture is the result of direct traumatic inoculation. In the setting of an open fracture, bacteria are introduced into the bone and soft-tissue directly from the skin flora and outside contaminants. This initial inoculation has the potential of becoming osteomyelitis without appropriate irrigation, debridement, and antibiotic administration. These infections are often pyogenic and polymicrobial. Several factors contribute to the development of osteomyelitis after an open fracture, including the inoculum size, traumatized devitalized tissue, impaired vascularity, and potential foreign bodies [4].
We present such a case of osteomyelitis after an open fracture, with a potential procedure that could prove beneficial in cases of not only infection and trauma but also oncologic lesions or other conditions in which the distal clavicle is deemed unsalvageable. To the best of our knowledge, this is the only case reported in the literature.
Case Report
A 65-year-old right-hand dominant female with no reported past medical history or toxic habits, presented with left clavicular pain and wound drainage 8 days after she was struck by motor vehicle in her home country of Guyana. She reports initially had pain and abrasions about the left shoulder, as well as rib pain. However, she denied any bleeding, oozing, or a punctate wound at the time of injury. At the hospital in Guyana, she was diagnosed with a left distal-third clavicle fracture, and multiple rib fractures, and was discharged home with a sling. She denies receiving any antibiotics at the hospital or on discharge. At home, she developed a wound over the posterosuperior trapezial region over the subsequent week which began to drain purulent fluid. She was brought to the United States by her family who lives in Queens, New York to receive medical care. At the time of presentation to the emergency room, she was noted to have 5 cm by 2 cm ulceration and draining sinus and obvious purulence to the posterolateral shoulder near the trapezius, with associated surrounding erythema and exquisite tenderness (Fig. 1). Radiographs demonstrated a Neer IIA distal clavicle fracture with significant superior displacement of the medial fragment [5] (Fig. 2a and b). She was also found to have fractures to the third through fifth ribs, with a temperature of 100.2°F, tachycardia to 99 beats/min, and blood pressure of 115/74 mm/hg. Blood cultures were obtained in the ED which was negative.
Figure 1.

Clinical images of the posterior left shoulder demonstrating 5 cm × 2 cm ulceration and draining sinus with obvious purulence are shown.
Figure 2.
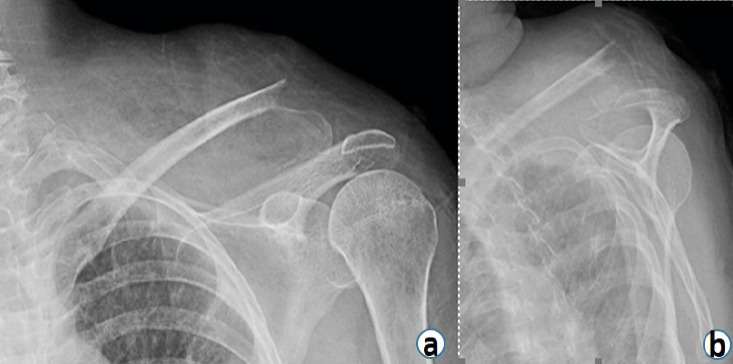
Anteroposterior (a) and scapular Y (b) shoulder radiographs at initial presentation are shown demonstrating a Neer 2A distal clavicle fracture with significant superior displacement of the medial fragment.
Given the delayed presentation and extensive infection with associated sepsis, the patient was indicated for immediate fluid resuscitation and intravenous antibiotic therapy with weight-based vancomycin (1000 mg every 12 h) and piperacillin and tazobactam (3.375 g every 6 h), and urgent irrigation and debridement, with excision of the distal clavicle.
The patient was brought to the operating room and placed supine on a radiolucent flat table. She was placed under general anesthesia, and the left upper extremity was prepped and draped in the usual sterile fashion. Intraoperatively, the patient was observed to have a 5 cm × 2 cm area of necrotic skin with an area of a draining sinus track in the middle of this overlying the clavicle. A surgical time-out was performed.
Sharp excision of necrotic skin was performed with 5 mm margins proximally and distally with a depth of 10 mm. A deep soft-tissue biopsy of the underlying trapezial muscle and subcutaneous tissue was obtained and sent for both tissue culture and pathology analysis. Multiple fluid swabs were sent for aerobic, anaerobic, fungal, and acid-fast bacilli testing as well. Deep open bone biopsy samples of the distal clavicle were obtained as well. Dissection was carried through the trapezial muscle, the pectoralis major muscle medial and deltoid laterally to expose the clavicle fracture site. The infection was found to have eroded through the trapezoidal fascia and subcutaneous tissue with obvious gross purulence and necrosis of the surrounding soft tissue. The lateral end of the medial clavicle fragment was found to be necrotic and moth-eaten secondary to the acute osteomyelitis.
All devitalized soft tissue was sharply excised with bovie cautery including subcutaneous tissue, trapezial myofascial tissue, the proximal aspect of the clavicular head of pectoralis major, and the proximal aspect of the anterior head of the deltoid. Approximately 5 cm of the main clavicle fragment was excised using a combination of rongeurs, curettes, and microsagittal saw. The lateral/distal clavicle fragment was completely removed up until the acromioclavicular joint as it was also found to be non-viable, and the coracoclavicular ligament attachments to the distal clavicle were excised. Of note, a communicating abscess was found anterior to the clavicle in the subcutaneous tissue and within the proximal biceps muscle and pectoralis muscle that is incised and decompressed. The muscle fibers of each were viable and, thus, were not debrided. The wound was irrigated with several liters of saline, betadine solution, and vancomycin powder, which was placed.
A medium hemovac drain was placed deep to the trapezial fascia. The pectoralis muscle medial and deltoid muscle lateral, and trapezium muscles proximal, were mobilized by dissection anterior and posterior to the muscles to allow for mobilization over the large 10 cm by 3 cm defect which remained after debridement. Suture was used to advance the muscle flaps over the defect and suture the muscles together in the space where the clavicle was previously. There was complete closure of the defect with the muscle flaps. A second medium hemovac drain was placed superficially. The skin and subcutaneous fashion were closed in a layered fashion. An incisional wound vacuum-assisted closure (VAC) was placed over the wound. The patient was awoken and returned to the recovery room in stable condition, with plans for possible repeat debridements depending on drainage, clinical stability, and wound appearance. Post-operative radiographs are demonstrated in Fig. 3a and b.
Figure 3.
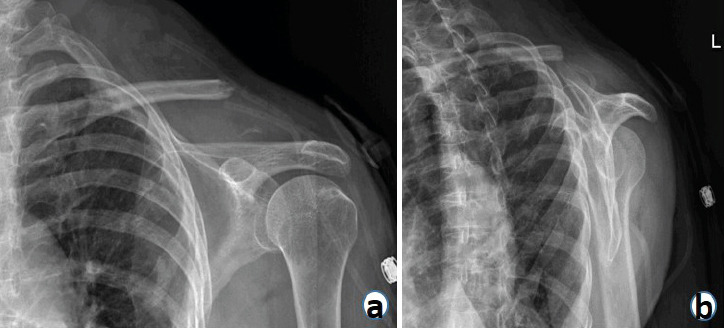
Anteroposterior (a) and scapular Y (b) shoulder radiographs taken on post-operative day 1 are shown demonstrating the status post-lateral clavicle resection.
Postoperatively, the patient was maintained in a regular sling with range of motion (ROM) as tolerated, without lifting restrictions for 4 weeks. Infectious disease (ID) was consulted and the patient was placed on empiric antibiotics of vancomycin (1000 mg every 12 h) and piperacillin and tazobactam (3.375 g every 6 h) until cultures were finalized. Hemovac drains were removed after 5 days when output was zero. Cultures subsequently grew Methicillin-resistant Staphylococcus aureus. Intravenous (IV) vancomycin was administered for 2 weeks while the patient remained in the hospital and participated in daily occupational therapy. The incisional wound VAC was removed after 7 days with excellent appearance of the surgical site, and the decision was made at that time to continue with IV antibiotic therapy. After 2 weeks, the patient was transitioned to oral linezolid (400 mg every 12 h) for 4 weeks based on ID recommendations. The post-operative course was complicated medically by the patient developing influenza and pneumonia, which was treated with piperacillin and tazobactam (3.375 g every 6 h) during the hospital stay. The Nylon sutures were removed post-operative day 18 with excellent wound healing, no erythema or drainage, and the patient was discharged home on day 19 after being medically stable. At 4 weeks postoperatively, the patient followed up in the outpatient office. Her wound was noted to have healed well without any signs of infection, her pain was well controlled, and her shoulder ROM was noted to be 175° of forward flexion, 75° of external rotation, internal rotation to L1 vertebrae, and abduction to 100° (Fig. 4a, b, c, d). Radiographs obtained at the time demonstrated maintained osseous alignment of the remaining medial clavicle without interval displacement from post-operative radiographs, and she was able to perform the vast majority of her activities of daily living (Figs. 5a, b and 6).
Figure 4.
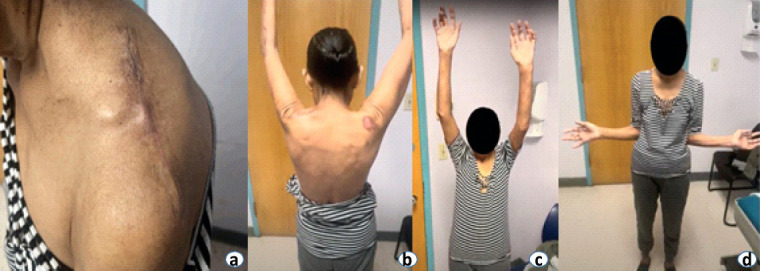
Clinical images taken during patient’s 4-week post-operative visit demonstrating a well-healed posterior left shoulder incision (a) and excellent range of motion (b, c, d) are shown.
Figure 5.
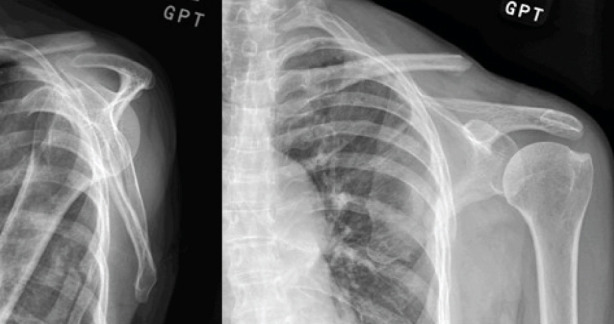
Anteroposterior (a) and scapular Y (b) shoulder radiographs taken on 4 weeks postoperatively are shown demonstrating status post-lateral clavicle resection with maintained osseous alignment of the remaining medial clavicle without interval displacement.
Figure 6.

Clinical images taken during patient’s 4-week post-operative visit demonstrating the patient’s ability to perform activities of daily living without issue are shown. Source: Kevin M Lehane, DO.
Discussion
Clavicle fractures are common injuries, representing 44% of all shoulder girdle fractures and 2.6–3.3% of all orthopedic fractures [1, 2, 6, 7, 8]. However, open clavicle fractures are rare, with a reported incidence of 1.8% of all clavicle fractures, and our more common in the younger population and a result of high-energy trauma [1]. Fractures of the distal third clavicle are less common than midshaft fractures and account for only 10–30% of all clavicle fractures. Distal clavicle fractures may be treated conservatively or surgically, however, there is a lack of consensus on the gold standard of treatment [5, 9]. Although rare, when open clavicle fractures occur, they are more often associated with serious concomitant injury [8]. The general standard of care treatment of open fractures throughout the body is early antibiotics within 1 h, followed by irrigation and debridement within 6–12 h, and internal fixation [2, 3]. However, there is a paucity of information in the orthopedic literature regarding appropriate management techniques of open clavicle fractures and treatment outcomes, especially in the delayed presentation with associated infection.
The most common complications of clavicle fractures vary by treatment, with hardware prominence most common for operative and malunion/non-union as most common for non-operative [9]. Infection after clavicle fractures is reported at approximately 0.4–3.5%, and almost always associated with operative treatment [11, 12]. In a study by Sliepen et al. reviewing all clavicle fractures treated at their institution, of their 630 clavicle fractures, only three patients suffered an open fracture, none of them developed a fracture-related infection [13]. Delay in debridement of open fractures has been cited in numerous studies as a risk factor for deep infection, including the study by Hull et al., which demonstrated a 3% increased risk of infection for every hour of delay [14].
The only case of clavicle fracture-related infection before surgical intervention in literature we were able to find is a case report by Strauss et al., whom described a closed distal clavicle fracture which was complicated by the breakdown of skin over the fracture site and the subsequent development of infection. The patient was treated with irrigation and debridement and external fixation [15]. To the best of our knowledge, this is the first described case of fracture-related infection of the distal clavicle treated with distal clavicle resection. Given the delayed presentation and resultant necrotic bone, operative repair of the clavicle was deemed futile, due to the resultant bone loss and morbidity of subsequent procedures needed to address such. Short-term follow-up has been great, with eradication of the infection, and satisfactory clinical outcomes and ROM. Outcomes of distal clavicle resection in literature have been positive, but are generally indicated for acromioclavicular pathology. In a study by Novak et al. looking at open distal clavicle resections, they noted no significant differences in the strength of the affected shoulder compared with the opposite shoulder, as well as no cephalad migration of the lateral clavicle [16].
Conclusion
Our patient presents a unique clinical conundrum in a patient who presented late after a missed open clavicle fracture, with resultant severe fracture-related infection and osteomyelitis with devitalized bone. After treatment with the resection of a large portion of the distal clavicle, the short-term outcomes of both range and motion and function have been very positive in our patient. Our procedure could prove beneficial in cases of infection, trauma, or oncologic lesions in which the distal clavicle is deemed unsalvageable.
Clinical Message.
Open fractures of the clavicle are rare, and very little is reported on appropriate management, especially in the delayed setting with associated infection. Resection of the distal clavicle may be an appropriate procedure if there is a large amount of associated necrotic bone. Short-term ROM and clinical outcomes after the procedure are very good. As mentioned previously, given outcomes, our procedure could prove beneficial in cases of infection, trauma, or oncologic lesions in which the distal clavicle is deemed unsalvageable.
Biography






Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Amer KM, Congiusta DV, Suri P, Choudhry A, Otero K, Adams M. Clavicle fractures:Associated trauma and morbidity. J Clin Orthop Trauma. 2020;13:53–6. doi: 10.1016/j.jcot.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sagi HC, Patzakis MJ. Evolution in the acute management of open fracture treatment?Part 1. J Orthop Trauma. 2021;35:449–56. doi: 10.1097/BOT.0000000000002094. [DOI] [PubMed] [Google Scholar]
- 3.Sagi HC, Patzakis MJ. Evolution in the acute management of open fracture treatment?Part 2. J Orthop Trauma. 2021;35:457–64. doi: 10.1097/BOT.0000000000002095. [DOI] [PubMed] [Google Scholar]
- 4.Dirschl DR, Almekinders LC. Osteomyelitis. Common causes and treatment recommendations. Drugs. 1993;45:29–43. doi: 10.2165/00003495-199345010-00004. [DOI] [PubMed] [Google Scholar]
- 5.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 6.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–6. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 7.Court-Brown CM, Caesar B. Epidemiology of adult fractures:A review. Injury. 2006;37:691–7. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 8.Gottschalk HP, Dumont G, Khanani S, Browne RH, Starr AJ. Open clavicle fractures:Patterns of trauma and associated injuries. J Orthop Trauma. 2012;26:107–9. doi: 10.1097/BOT.0b013e31821c0b7f. [DOI] [PubMed] [Google Scholar]
- 9.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–32. [PubMed] [Google Scholar]
- 10.Mouzopoulos G, Morakis E, Stamatakos M, Tzurbakis M. Complications associated with clavicular fracture. Orthop Nurs. 2009;28:217–24. doi: 10.1097/NOR.0b013e3181b579d3. [DOI] [PubMed] [Google Scholar]
- 11.Wolf S, Chitnis AS, Manoranjith A. Surgical treatment, complications, reoperations, and healthcare costs among patients with clavicle fracture in England. BMC Musculoskelet Disord. 2022;23:135. doi: 10.1186/s12891-022-05075-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury. 1999;30:497–500. doi: 10.1016/s0020-1383(99)00140-0. [DOI] [PubMed] [Google Scholar]
- 13.Sliepen J, Hoekstra H, Onsea J, Bessems L, Depypere M, Noppe N, et al. Treatment and outcome of fracture-related infection of the clavicle. Injury. 2023;54:110910. doi: 10.1016/j.injury.2023.110910. [DOI] [PubMed] [Google Scholar]
- 14.Hull PD, Johnson SC, Stephen DJ, Kreder HJ, Jenkinson RJ. Delayed debridement of severe open fractures is associated with a higher rate of deep infection. Bone Joint J. 2014;96-B:379–84. doi: 10.1302/0301-620X.96B3.32380. [DOI] [PubMed] [Google Scholar]
- 15.Strauss EJ, Kaplan KM, Paksima N, Bosco JA 3rd. Treatment of an open infected type IIB distal clavicle fracture:Case report and review of the literature. Bull NYU Hosp Jt Dis. 2008;66:129–33. [PubMed] [Google Scholar]
- 16.Novak PJ, Bach BR, Jr, Romeo AA, Hager CA. Surgical resection of the distal clavicle. J Shoulder Elbow Surg. 1995;4:35–40. doi: 10.1016/s1058-2746(10)80006-0. [DOI] [PubMed] [Google Scholar]


