Summary
Background
The design of health benefits package (HBP), and its associated payment and pricing system, is central to the performance of government-funded health insurance programmes. We evaluated the impact of revision in HBP within India’s Pradhan Mantri Jan Arogya Yojana (PM-JAY) on provider behaviour, manifesting in terms of utilisation of services.
Methods
We analysed the data on 1.35 million hospitalisation claims submitted by all the 886 (222 government and 664 private) empanelled hospitals in state of Punjab, from August 2019 to December 2022, to assess the change in utilisation from HBP 1.0 to HBP 2.0. The packages were stratified based on the nature of revision introduced in HBP 2.0, i.e., change in nomenclature, construct, price, or a combination of these. Data from National Health System Cost Database on cost of each of the packages was used to determine the cost-price differential for each package during HBP 1.0 and 2.0 respectively. A dose–response relationship was also evaluated, based on the multiplicity of revision type undertaken, or based on extent of price correction done. Change in the number of monthly claims, and the number of monthly claims per package was computed for each package category using an appropriate seasonal autoregressive integrated moving average (SARIMA) time series model.
Findings
Overall, we found that the HBP revision led to a positive impact on utilisation of services. While changes in HBP nomenclature and construct had a positive effect, incorporating price corrections further accentuated the impact. The pricing reforms highly impacted those packages which were originally significantly under-priced. However, we did not find statistically significant dose–response relationship based on extent of price correction. Thirdly, the overall impact of HBP revision was similar in public and private hospitals.
Interpretation
Our paper demonstrates the significant positive impact of PM-JAY HBP revisions on utilisation. HBP revisions need to be undertaken with the anticipation of its long-term intended effects.
Funding
Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ).
Keywords: Health benefit packages, Reimbursement rates, Health insurance, Behavioural economics, Universal health coverage, Supplier-induced demand
Research in context.
Evidence before this study
We searched the Cochrane Database for Systematic Reviews, and MEDLINE, and Embase for articles (in English language) evaluating the impact of health insurance policy interventions on claims utilisation, covering publications up to June 2024. Our search combined terms related to health insurance (e.g., ‘health insurance’ OR ‘health benefit package’ OR ‘Diagnosis-related groups’) AND policy interventions (e.g., ‘policy reforms’ OR ‘price revisions’ OR ‘fee revisions’ OR ‘insurance design’ and ‘reimbursement rate revision’) AND outcomes (e.g., ‘utilization’ OR ‘volume of services’ OR ‘claims’ OR ‘insurance claims’). No country or year restrictions were applied.
We found one systematic review from 2019 evaluating changes in Medicaid fees, including 18 studies on fee changes over time. Seven studies focused on provider participation, five on enrollee access, and fourteen on service use. All studies used quasi-experimental methods, of which five used a triple difference (DDD) design. Two studies used a difference-in-difference (DD) design, six studies used a dose–response (DR) model that examined changes in outcomes for states with larger versus smaller fee changes over time, and five studies used an interrupted time series (ITS) design without a concurrent control group. The systematic review was limited to changes in provider payment in the outpatient setting.
Most studies examined fee revisions' impact on service volume, with eight of fourteen finding positive associations with service utilization measures. However, no studies compared prices to costs or evaluated the dose–response relationship of price changes. Additionally, no studies assessed the impact of other policy interventions, such as changes in nomenclature and package constructs, on claims utilization.
Added value of this study
The findings of our study provide important evidence on the impact of various health benefit package policy (HBP) interventions introduced under India’s Pradhan Mantri Jan Arogya Yojana (PM-JAY), which is the world’s largest health insurance scheme. Overall, we found that the HBP revisions in terms of change in package nomenclature, construct and prices led to a positive impact on utilisation of services. First, all the changes in HBP package nomenclature and construct led to a positive change in provider behaviour for uptake of services. This signifies that the revision in packages led to a better understanding as well as ease for use of services. Second, the revision of package construct and nomenclature both had a higher positive effect (5.74 claim increase per package per month) on utilisation than either change in package construct (0.34 claim increase per package per month) or nomenclature (1.79 claim increase per package per month) alone. Third, the change in utilisation following either package construct or nomenclature was higher, when accompanied by a price change.
Furthermore, pricing reforms led to a significantly higher impact on those packages which were originally significantly under-priced (1.84 claim increase per package per month), or moderately under-priced (0.76 claim increase per package per month). However, within the category of packages as per the original cost-price differential, there was no dose–response relationship based on extent of price correction. A similar pattern of dose–response relationship for increase in utilisation of packages which are initially more under-priced was seen for the private sector. However, public sector showed statistically significant increase in utilisation among those packages which were moderately under-priced, appropriately priced and overpriced (0.24, 0.38, and 0.15 claims per package per month respectively).
We also found that the estimates of effect did not vary much between the analysis with and without adjustment for number of empanelled hospitals. This suggests that after a basic number of hospitals are empanelled, subsequent increase in hospital numbers does not have any significant effect on expanding access, unless it is accompanied with an appropriate health benefit package design.
Implications of all the available evidence
Understanding the drivers of differences in the outcomes of insurance reforms is critical to inform future implementations of publicly funded health insurance to achieve the broader goal of universal health coverage. Our paper makes significant contribution to the existing literature by combining the data on claims, prices and cost of health care packages, to examine the impact of HBP revisions. Our paper demonstrates the significant positive impact of PM-JAY HBP revisions in package nomenclature, construct and pricing. Such HBP revisions need to very thoughtfully undertaken, with the anticipation of its long-term intended effects. Our paper also demonstrates the importance of aligning the prices with the actual cost of care, which has also been argued by several other previous papers commenting on PM-JAY provider payment rates.
Introduction
Risk pooling and prepayment is considered as an important strategy for financing of health care services to achieve universal health coverage.1 Considering the relatively large sections of poor populations, working in informal sector, and having low willingness to pay for an insurance premium,2,3 Governments in several low-income and-middle-income countries (LMICs) are resorting to using tax revenue to finance such a risk pooling system to finance and purchase health care.4, 5, 6, 7, 8, 9 Traditionally, public healthcare financing in India was dominantly governed by supply-side funding. The supply-side financing structure entails the allocation of funds for developing health infrastructure, paying for salaries of human resources, procurement of drugs and consumables, etc. These allocations are typically guided by predefined payment norms corresponding to different levels of healthcare facilities. However, a discernible shift towards a demand-side financing system has emerged with the advent of numerous publicly funded health insurance schemes. This transition in the financing landscape signals a concerted effort to foster a more patient-centred and service-driven approach to funding healthcare services in India. Demand-side financing promotes accountability and responsiveness towards individual patient preferences, ensuring a dynamic and quality-focused healthcare system. Additionally, allowing individuals to use tax funds to purchase health services from the private sector introduces patient choice in selection of healthcare providers. This can lead to a more dynamic and responsive healthcare system, and induce competition. While the success of such endeavours is dependent on several policy levers, a critical aspect of this is its health benefits package (HBP), which is the explicit statement of who is covered, for what services, and at what price to the provider.10,11
In 2018, India launched the Pradhan Mantri Jan Arogya Yojana (PM-JAY), which is the world’s largest health assurance program. This non-contributory tax-financed health insurance program aims to provide coverage to 500 million Indians.12,13 The Punjab state initiated this scheme in 2019, covering 65% of its population. Besides the socio-economic caste census (SECC) beneficiaries (bottom 40% according to SECC 2011), the State Government of Punjab covers the National Food Security Act (NFSA) ration card holders, construction workers, small traders, and accredited and yellow card holder journalists. The insurance scheme in Punjab is directly implemented by the State Health Agency without involvement of an intermediary insurance company.
The PM-JAY HBP prices pertaining to surgical and day-care packages cover costs related to medical examination, treatment and consultation, medicine and medical consumables, non-intensive and intensive care services, diagnostics and laboratory investigations, implants wherever applicable, accommodation for hospital stay, food services, management of complications arising during treatment, and pre and post hospitalisation follow-up care up-to 15 days. The PM-JAY HBP service coverage and pricing was initially developed based on review of the extant State-level Government funded, or other voluntary private insurance schemes. While the service coverage was comprehensive, comprising of several medical and surgical interventions covering nearly 24 specialities for a range of 1394 (which is currently 1949) tertiary and secondary care hospitalisations, appropriateness of pricing or provider payment rates in early years was limited due to poor quality cost data. As a result, the procedures were reported to be under-priced, which led to low provider interest in getting empanelled to provide care, or denial of services by those empanelled which can potentially affect access.14, 15, 16, 17 Besides the inappropriate nomenclature of certain packages or its construct limited its potential use by the providers for providing treatment (Table 1).
Table 1.
Description of the type of health benefit package revision under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY).
| Sr. No. | Package category | Operational definition | Examples |
|---|---|---|---|
| 1. | Change in package nomenclature | Packages whose nomenclature (package name) was revised in terms of description, from HBP 1.0 to HBP 2.0 such that package name becomes more explanatory |
|
| 2. | Change in package construct |
|
|
| 3. | Change in price | Packages whose price was revised (increased/decreased) |
|
| 4. | Change in package nomenclature and package construct | Packages whose nomenclature was changed along with their construct |
|
PDA stenting—Patent ductus arteriosus, CBD—Common bile duct, Lap.—Laparoscopic.
As a result, India’s National Health Authority (NHA) has made several subsequent revisions to the HBP, which have relied on more robust cost and utilisation data which was generated over time, as well as extensive stakeholder consultations.18 Four such revisions have been undertaken so far, where price corrections as per the actual cost of providing care have been made, besides revising the nomenclature and construct of the packages. A comprehensive assessment of the cost-price differentials showed that the extent of significantly under-priced packages was reduced to half between the HBP 1.0 (42%) and HBP 2.0 (20%).19
An important objective of such HBP revisions is to set the right provider incentives, and eventually ensure high degree of access to care. However, there is no such evidence from India, or other LMICs regarding the extent to which such changes in prices of procedures, or its nomenclature and construct, affects the utilisation of care in the context of Government funded health insurance programs. We used the data on 1.35 million claims over a period of 28 months from state of Punjab, India to determine the impact of change from HBP 1.0 to HBP 2.0 on the utilisation of surgical care services. We further evaluated the impact on utilisation, stratified by type of HBP revision undertaken, and by type of ownership of provider (public versus private).
Methods
Context and scope of analysis
The Government of India implemented the PM-JAY in 2018, with a health benefit package referred to as HBP 1.0. Four subsequent revisions of the HBP have taken place so far, including HBP 2.0, 2.1, 2.2 and 2022.20, 21, 22, 23 While the HBP 2.0 and 2022 have been major revisions comprising of changes in number of packages, package specifications and nomenclature, as well as most importantly significant change in prices, the other two HBP revisions i.e., HBP 2.1 and HBP 2.2, were minor in nature. While 76 new packages were added in HBP 2.1, only 1 additional package was incorporated in HBP 2.2. Details of HBP revisions are provided in S1 Appendix (page number 1–2). Since, HBP 2022 was launched in April 2022, and has only been introduced in a few states so far with an average implementation duration of about 6 months, it is premature to evaluate its impact.24 As a result, we evaluated the impact of the HBP 2.0 revision.
As India is a federal country, the States are free to choose the version of HBP to follow. Also, as each state may be on a different version of HBP, as well as timing of its implementation may vary significantly, it becomes logical to evaluate any impact of the HBP revision at the State level. We chose to undertake this evaluation in the north Indian state of Punjab. The state implemented the scheme in August, 2019, and shifted to HBP 2.0 in August, 2020,25 and since then has not migrated to any other version of the HBP.
The hospitals are paid for each hospitalisation claim based on a pre-specified case-based bundled rate. In case of surgical packages, it is a fixed lumpsum amount. On the other hand, in case of medical packages it is defined based on per-day rate, stratified based on setting (routine versus intensive care), and hospitals get paid based on the length of stay for each hospitalisation. As a result, irrespective of the base rate, in case of medical package, there is a possibility for hospitals to increase the length of stay to maintain incomes. Since the surgical packages are not subject to this bias, we chose to evaluate the impact of changes in price and other HBP revisions on utilisation based on analysis of surgical package claims only. Moreover, in HBP 2.0 there was no change in the per-day rate for medical packages, so it is logical to omit medical packages from analysis.
Data source
We obtained the data on 1.35 million hospitalisation claims for PM-JAY from the Punjab State Health Agency, for the period from August 2019 to December 2022. This data comprised of claims submitted by all the 886 (222 government and 664 private) empanelled hospitals for treating patients who are beneficiaries of the PM-JAY in Punjab state.26 The data included information on month-wise claims for each procedure (procedure name along with its code) in the HBP 1.0 and 2.0, by type of health care provider where the claim was booked—public or private.
The first step in data processing included matching of the similar procedures in HBP 1.0 and 2.0 (since the coding pattern was completely different between HBP 1.0 and 2.0). The details of the matching methodology followed is described in the Supplementary Appendix S1 (Supplementary Fig. S1). The first set of matching for 675 packages was done initially using the list of matched packages provided by the NHA.20 Subsequently, for the remaining 536 packages, detailed examination by the authors, followed by clinical expert consultations and discussion with the NHA HBP team was undertaken to finally match all similar packages and re-assign unique codes. New packages introduced in HBP 2.0, or those in HBP 1.0 which were discontinued, were removed from the final dataset. Therefore, a total of 1122 HBP 2.0 procedures, comprising of 863 (76.9%) surgical (880 as per HBP 1.0) and 259 (23.1%) medical packages (256 as per HBP 1.0) after excluding the package which were discontinued from HBP 1.0 or added as new packages in HBP 2.0 were included in the final analysis (Supplementary Appendix S1, page number 4).
The second step in data curation involved assigning the type of HBP revision done for a given package in HBP 1.0. The 3 revision possibilities included—change in nomenclature, change in construct, a change in price, or a combination of these (Table 1). The HBP 2.0 revision, which involved 16 surgical specialities comprised of a change in the nomenclature of 269 (30.7%) packages, revision in construct of 44 (5%) packages, both nomenclature and construct revision of 197 (22.5%) packages, and 365 (41.8%) packages had no change in package nomenclature and construct. Further, HBP 2.0 comprised of revision in prices of 597 (68.2%) packages. In terms of change in prices, while 473 (54%) packages saw an upward revision, the prices were decreased for 124 (14.2%) packages. However, price of 278 (31.8%) packages remain unchanged (Table 2).
Table 2.
Impact of redesigning of health benefit packages (HBPs) in terms of change in package nomenclature, construct and price on utilisation of claims in Punjab state.
| Scenario | Price change | Sample size | Pre slopea | Change in slopea | Post slopea | p-valuea |
|---|---|---|---|---|---|---|
| Change in Package nomenclature and construct | Change in price | 186 | −10.25 | 5.77 | −4.48 | 0.001 |
| No change | 11 | −1.82 | 0.26 | −1.56 | 0.823 | |
| Total | 197 | −9.74 | 5.74 | −4.00 | 0.001 | |
| Change in Package nomenclature | Change in price | 209 | −1.46 | 2.24 | 0.78 | 0.002 |
| No change | 60 | −0.95 | 1.48 | 0.53 | 0.003 | |
| Total | 269 | −0.35 | 1.79 | 1.44 | 0.005 | |
| Change in Package construct | Change in price | 25 | −0.24 | 0.43 | 0.19 | 0.036 |
| No change | 19 | −0.45 | 0.23 | −0.22 | 0.017 | |
| Total | 44 | −0.17 | 0.34 | 0.17 | 0.032 | |
| No change in package nomenclature and construct | Change in price | 177 | −0.09 | 0.07 | −0.02 | 0.85 |
| No change | 188 | −0.89 | 0.84 | −0.05 | 0.006 | |
| Total | 365 | −0.64 | 0.54 | −0.10 | 0.068 |
Pre-slope–number claims changing(increasing or decreasing) each month before intervention.
Change in slope–number of claims (increasing or decreasing) due to intervention.
Post-slope–number claims changing(increasing or decreasing) each month after intervention.
Values in the table represents outcome in terms of number of insurance claims per package per month and bold figures represent statistically significant figures (p value < 0.05).
As the third step, we categorised the packages in both the HBP 1.0 and 2.0 according to the extent to which their price differed from the actual cost incurred in providing the set of services included in the package. This was done to examine the extent to which the change in price in HBP 2.0 corrected for the discordance between the reimbursement rate set for payment to the hospital, and the actual cost incurred. The aim of doing the same was to determine a dose–response relationship between the upward correction of price and provider behaviour in terms of provision of care or utilisation of claims. The data on cost of 618 HBP 2.0 packages (662 as per HBP 1.0) surgical packages were obtained from the Costing of Health Services in India (CHSI) study,27 which is also available in the Indian National Health System Cost Database.28,29 The CHSI study estimates on cost are based on a nationally representative sample of 14 tertiary public hospitals drawn from 14 states, 27 district public hospitals from 9 states and 22 private hospitals from 11 states.30 The methods of the study, its process evaluations, and findings on unit cost from this study are published elsewhere.30, 31, 32, 33, 34 We compared the cost of each package, as estimated through CHSI data, and the price of the package in HBP 1.0 and 2.0 respectively. Based on the comparison, we computed the ratio of price and cost for each package. Subsequently, we categorised the packages where the prices were either <50%, or 50%–75%, or 75%–110% or greater than 110% of the actual cost. This categorisation was done separately based on prices in HBP 1.0 and 2.0 respectively (Supplementary Fig. S2). We have considered two distinct scenarios for the present analysis. In the first scenario, the utilisation of PMJAY claims in different categories (stratified based on cost-price differential) was compared between the pre-intervention period (HBP 1.0) and the total number of claims in HBP 2.0, irrespective of the CPD category in HBP 2.0 [Table 3]. The second scenario evaluates the extent of price correction across all packages in different categories based on CPD in pre and post intervention periods as shown in Table 4 [S1 Appendix, page number 11].
Table 3.
Impact of price revision on utilisation of insurance claims across overall,a public and private sector in the state of Punjab, India.
| Package category |
Significantly under-priced |
Moderately under-priced |
Appropriately priced |
Overpriced |
All categories |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Cost price differential) |
(<50%) |
(50–75%) |
(75–110%) |
(>110%) |
|||||||||||
| Sector | Overalla | Public | Private | Overalla | Public | Private | Overalla | Public | Private | Overalla | Public | Private | Overalla | Public | Private |
| Sample size | 316 | 314 | 260 | 159 | 155 | 139 | 99 | 89 | 93 | 39 | 33 | 38 | 613 | 591 | 530 |
| Pre slopea | −0.55 | −0.58 | 0.23 | −0.27 | −0.27 | −0.01 | −0.79 | −0.54 | −1.44 | 0.91 | −0.34 | 1.08 | −0.36 | −0.57 | 0.12 |
| Change in slopea | 1.84 | 0.6 | 1.41 | 0.76 | 0.24 | 0.55 | 0.68 | 0.38 | 0.69 | 0.39 | 0.15 | 0.34 | 1.22 | 0.50 | 0.88 |
| Post slopea | 1.29 | 0.02 | 1.64 | 0.49 | −0.03 | 0.54 | −0.11 | −0.16 | −0.75 | 1.3 | −0.19 | 1.42 | 0.86 | −0.07 | 1.00 |
| p-valuea | 0.001 | 0.066 | 0.012 | 0.017 | 0.039 | 0.106 | 0.117 | 0.002 | 0.126 | 0.373 | 0.006 | 0.407 | 0.009 | 0.039 | 0.026 |
Pre-Slope-number claims changing (increasing or decreasing) each month before intervention.
Change in Slope-number of claims (increasing or decreasing) due to intervention.
Post-Slope-number claims changing (increasing or decreasing) each month after intervention.
Overall represents public and private sector analysis. Values in the table present outcome in terms of number of insurance claims per package per month, all bold figures represent statistically significant figures (p value < 0.05).
Table 4.
Impact of extent of price correction on utilisation of insurance claims across public and private sector in the state of Punjab, India.
| Package category (CPD)a pre intervention scenarioa | Package category post intervention scenarioa | Sample size | Pre slopea | Change in slopea | Post slopea | p-valuea | Confidence interval (change in Slope) |
|---|---|---|---|---|---|---|---|
| Significantly under-priced (0–50%) | Significantly under-priced | 201 | −1.35 | 1.49 | 0.14 | 0.003 | (0.568–2.414) |
| Moderately under-priced | 68 | 1.19 | 3.58 | 4.77 | 0.029 | (0.349–6.811) | |
| Appropriately priced | 38 | 0.14 | 0.30 | 0.44 | 0.051 | (−0.008 to 0.598) | |
| Overpriced | 9 | 0.12 | 0.64 | 0.76 | 0.130 | (−0.242 to 1.518) | |
| Moderately under-priced (50–75%) | Significantly under-priced | 12 | −0.85 | 1.64 | 0.79 | 0.005 | (0.559–2.721) |
| Moderately under-priced | 81 | −0.42 | 1.07 | 0.65 | 0.002 | (0.444–1.688) | |
| Appropriately priced | 54 | −0.02 | 0.06 | 0.04 | 0.676 | (−0.249 to 0.373) | |
| Overpriced | 12 | −0.30 | 0.08 | −0.22 | 0.407 | (−0.117 to 0.271) | |
| Appropriately priced (75–110%) | Significantly under-priced | 3 | −5.90 | 2.66 | −3.24 | 0.083 | (−0.427 to 5.749) |
| Moderately under-priced | 24 | −0.13 | 0.13 | 0.01 | 0.103 | (−0.033 to 0.301) | |
| Appropriately priced | 48 | −1.08 | 1.04 | −0.04 | 0.122 | (−0.325 to 2.411) | |
| Overpriced | 24 | 0.09 | 0.15 | 0.24 | 0.476 | (−0.292 to 0.584) | |
| Overpriced (More than 110%) | Significantly under-priced | – | – | – | – | – | – |
| Moderately under-priced | 2 | −0.15 | 0.10 | −0.05 | 0.452 | (−0.174 to 0.372) | |
| Appropriately priced | 16 | 0.11 | −0.09 | 0.02 | 0.448 | (−0.325 to 0.155) | |
| Overpriced | 21 | 1.95 | 0.64 | 2.59 | 0.599 | (−1.982 to 3.266) |
Values in the table present outcome in terms of number of insurance claims per package per month; CPD refers to Cost-price differential, Pre intervention scenario refers to HBP 1.0 and Post intervention scenario refers to HBP 2.0, all bold figures represent statistically significant figures (p value < 0.05).
Data analysis
We used an interrupted-time series analysis design to evaluate the impact of revision of HBP 1.0 to HBP 2.0. The HBP 2.0 was implemented in Punjab in August 2020.20 The period from November 2019 to August 2020 was considered as the pre-intervention, while the period from September 2020 to December 2021 was taken as the post-intervention period for the purpose of analysis. The claims data from initial 3 months (August–October 2019) of PM-JAY implementation was removed to discount for initial period of setting up and implementation of scheme. The analysis was undertaken using the software–IBM SPSS Statistics 26.
The impact of HBP changes, including nomenclature and construct, on utilisation was further stratified based on whether it was accompanied with a price change. Similarly, the impact of price change was evaluated for the category of packages, as per their original cost-price differential in HBP 1.0. The latter two approaches also allowed to measure a dose–response relationship. The impact was evaluated for 2 outcome indicators—first, the total monthly claims for a given category of packages where a specific HBP revision was undertaken, and second, the number of monthly claims per package among packages in each category of HBP change. Both the outcome indicators were evaluated to ascertain a dose–response relationship between the different revision strategies. However, claims per package per month was done to standardise, since the number of packages in various strata were different. The study findings are reported in terms of number of claims per package per month in the results section. The entire analysis was undertaken using claims for all hospitals, and separately for claims from public and private hospitals. To examine and adjust for possible supply-side confounding, we undertook each analysis, with and without the adjustment for the number of empanelled hospitals. The data on month-wise number of empanelled hospitals were obtained from the State Health Agency.
For the analysis, we first adjusted the outcome viz., number of ‘monthly claims per package’ using an appropriate auto-regressive moving average (ARMA), auto-regressive integrated moving average (ARIMA) and seasonal autoregressive integrated moving average (SARIMA), time series models to adjust non-stationarity, seasonality and auto-correlation [S3 Appendix, page number 24–30]. The second step involved multiple linear regression model to calculate the estimates of change in level and trend separately by utilising the outcome series adjusted in the step 1. The estimate of change in level gives the difference between observed level and expected value of outcome right after and before the intervention. The estimate of change in trend calculates the difference between post and pre-intervention slopes.35 The pre slope refers to the rate of change (increase/decrease) in number of claims before the HBP policy intervention. The post slope is the rate of change in number of claims after the HBP policy intervention. Finally, a positive (negative) change in level and slope would indicate an increase (reduction) in utilisation of the claims because of different HBP revision strategies. The change in slope is equal to the difference between the two slopes attributable to the intervention. The ‘change in slope’ estimate was considered to be statistically significant if p-value was found to be less than 0.05.
Role of the funding source
There is no role of any agency in study design, data analysis, data interpretation or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Overall, Table 2 shows three broad trends in findings. First, all the changes in HBP package nomenclature and construct led to a positive change in provider behaviour for uptake of services. This signifies that the revision in packages led to a better understanding as well as ease for use of services. Second, the revision of package construct and nomenclature both had a higher positive effect (5.74 claim increase per package per month, p value = 0.001) on utilisation than either change in package construct (0.34 claim increase per package per month, p value = 0.032) or nomenclature alone (1.79 claim increase per package per month, p value = 0.005). It is important to note that this category includes the ‘haemodialysis’ package, which accounts for the highest number of claims compared to all other packages. This has led to higher values in the estimates. Third, the change in utilisation following either package construct or nomenclature was higher, when accompanied by a price change. For example, while a change in construct and nomenclature of package when accompanied with a price change led to a statistically significant increase of 5.77 claim increase per package per month (p value = 0.001). However, there was no statistically significant change when there was no accompanying price change with revision in nomenclature or construct (p value = 0.823.
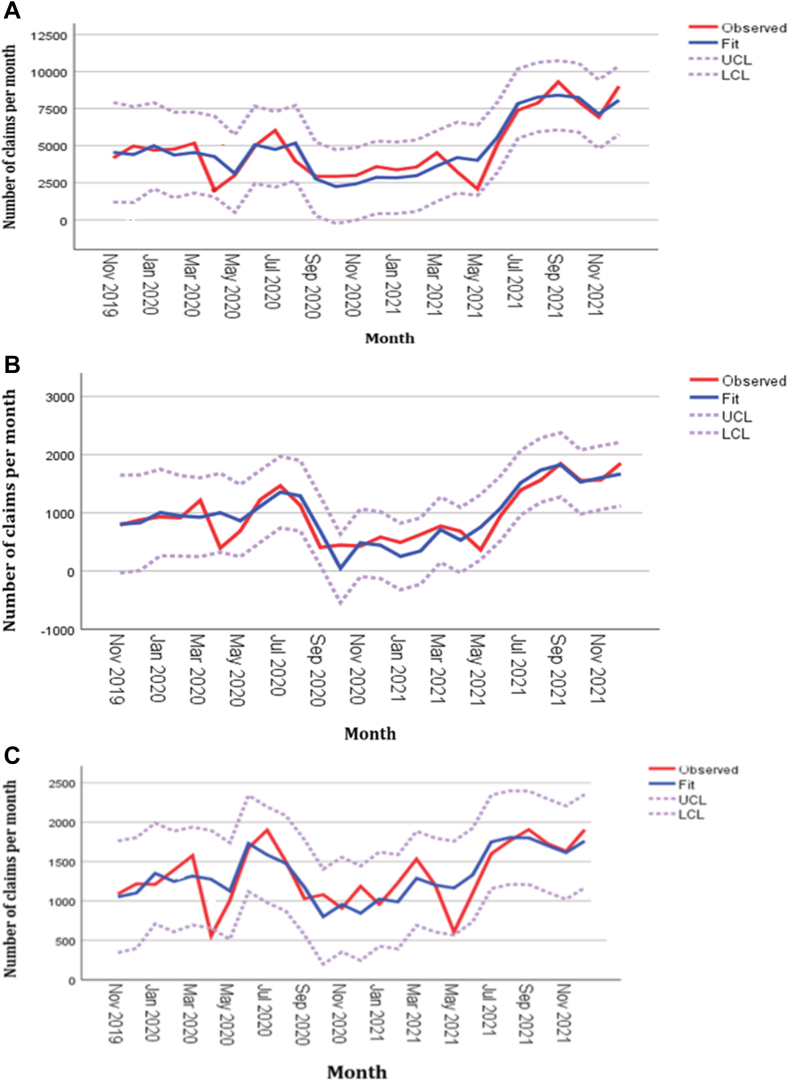
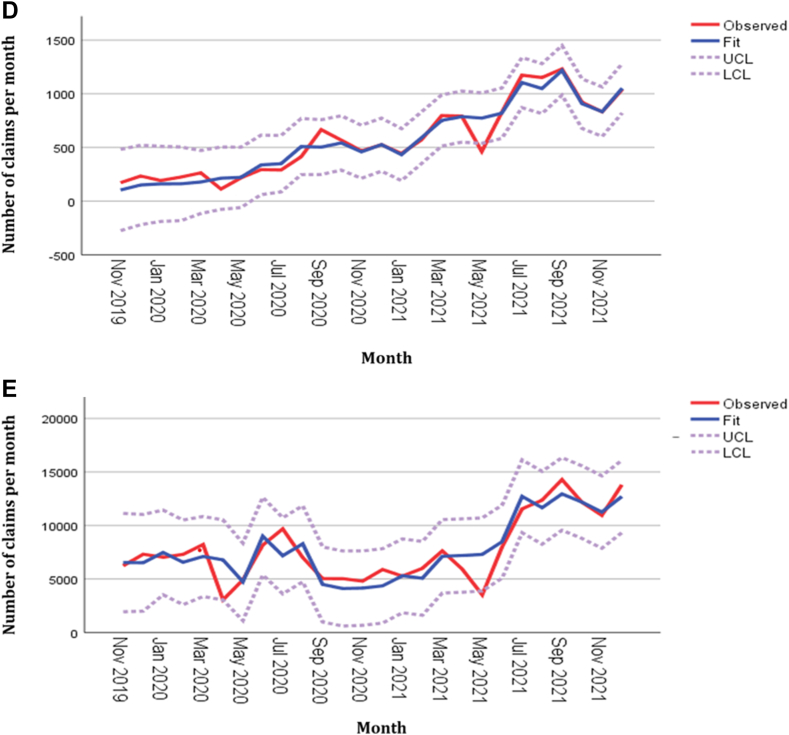
Overall, it was found that utilisation of all packages increased significantly during HBP 2.0 in both public and private sector. Further, stratifying the packages by the extent of cost-price differential during HBP 1.0, we found a statistically significant increase in utilisation of packages which were significantly under-priced (1.84 claim increase per package per month, p value = 0.001), or moderately under-priced (0.76 claim increase per package per month, p value = 0.017) (Table 3). While we do find an increase in utilisation for other packages, the latter is statistically insignificant. A similar pattern of dose–response relationship for increase in utilisation of packages which are initially more under-priced was seen for the private sector (Table 3). However, public sector showed statistically significant increase in utilisation among those packages which were moderately under-priced, appropriately priced and overpriced [0.24 (p value = 0.039), 0.38 (p value = 0.002) and 0.15 (p value = 0.006) claims per package per month respectively). Observed and predicted values of selected model for four categories of health benefit packages under HBP 1.0 in public and private sector are illustrated in Fig. 1.
Fig. 1.
Observed and predicted values of selected model for four categories of health benefit packages under HBP1.0 in public and private sector: A) Packages having CPD less than 50%. B) Packages having CPD between 50 and 75%. C) Packages having CPD between 75 and 110%. D) Packages having CPD more than 110%. E) All packages. Footnote: Cost-price differential is ratio of price to cost; where cost refers to the mean health system cost of delivering the service for a package in public or private healthcare facilities in India and price refers to the amount set by the government (National Health Authority) to be reimbursed for the same service.
Table 4 shows the change in utilisation among packages as per their cost-price differential during HBP 1.0, further stratified by the extent of correction in their prices in HBP 2.0. Our analysis shows that the increase in utilisation of significantly under-priced and moderately under-priced packages, was more for those packages which had a minimal price correction, rather than those with significant upward shift in prices. For example, among the significantly under-priced packages in HBP 1.0, a significant increase in utilisation in HBP 2.0 was seen among those packages where the price correction led to a marginal change within the same category (increase of 1.49 cases per package per month, p value = 0.003), or these became moderately under-priced (increase of 3.58 cases per package per month, p value = 0.029). Conversely, packages that received significant price corrections, making them appropriately priced or overpriced, did not show a statistically significant increase in utilisation (an increase of 0.30 and 0.64 claims per package per month, with p-values of 0.051 and 0.130 respectively).
Similar trends in findings are seen for utilisation in private sector providers (Table 5). We also found that the estimates of effect did not vary much between the analysis with and without adjustment for number of empanelled hospitals. However, in case of public hospitals, the adjustment for number of empanelled hospitals had a significant impact on findings for changes implying that the increase in empanelment of public hospitals led to an increase in utilisation. The unadjusted results are given in S2 Appendix, page number 14–20 (Supplementary Tables S3–S6).
Table 5.
Impact of extent of price correction on utilisation of insurance claims across private sector in the state of Punjab, India.
| Package category (CPD)a pre intervention scenarioa | Package category post intervention scenarioa | Sample size | Pre slopea | Change in slopea | Post slopea | p-valuea | Confidence interval (change in Slope) |
|---|---|---|---|---|---|---|---|
| Significantly under-priced (0–50%) | Significantly under-priced | 170 | −0.11 | 0.56 | 0.46 | 0.013 | (0.129–0.999) |
| Moderately under-priced | 55 | −2.13 | 5.70 | 3.57 | 0.006 | (1.762–9.628) | |
| Appropriately priced | 29 | 0.40 | 0.22 | 0.62 | 0.221 | (−0.157 to 0.597) | |
| Overpriced | 6 | 0.43 | 0.21 | 0.64 | 0.429 | (−0.351 to 0.773) | |
| Moderately under-priced (50–75%) | Significantly under-priced | 12 | −0.45 | 1.30 | 0.85 | 0.005 | (0.440–2.162) |
| Moderately under-priced | 76 | −0.42 | 0.95 | 0.53 | 0.031 | (0.084–1.810) | |
| Appropriately priced | 45 | 0.12 | −0.11 | 0.01 | 0.530 | (−0.482 to 0.262) | |
| Overpriced | 6 | −0.23 | −0.01 | −0.24 | 0.928 | (−0.271 to 0.249) | |
| Appropriately priced (75–110%) | Significantly under-priced | 3 | −3.90 | 1.31 | −2.59 | 0.417 | (−2.086 to 4.706) |
| Moderately under-priced | 24 | 0.19 | −0.04 | 0.15 | 0.557 | (−0.169 to 0.097) | |
| Appropriately priced | 45 | −0.32 | 0.48 | 0.16 | 0.404 | (−0.723 to 1.689) | |
| Overpriced | 21 | 0.15 | 0.04 | 0.19 | 0.842 | (−0.392 to 0.472) | |
| Overpriced (More than 110%) | Significantly under-priced | – | – | – | – | – | |
| Moderately under-priced | 2 | 0.15 | 0.04 | 0.19 | 0.666 | (−0.164 to 0.250) | |
| Appropriately priced | 16 | 0.20 | −0.16 | 0.03 | 0.293 | (−0.487 to 0.163) | |
| Overpriced | 20 | 2.16 | 0.71 | 2.88 | 0.349 | (−0.875 to 2.303) |
Values in the table present outcome in terms of number of insurance claims per package per month; CPD refers to Cost-price differential, Pre intervention scenario refers to HBP 1.0 and Post intervention scenario refers to HBP 2.0, all bold figures represent statistically significant figures (p < 0.05).
Discussion
The design of the health benefits package in any publicly funded health insurance program is the central to the success of such schemes aimed to achieve universal health coverage. Any revision in HBP, besides adding and deleting services based on some criteria for priority setting, aims to eventually set the right incentives for achievement of long-term objectives of access, quality, and efficiency. In this paper, we evaluated the impact of HBP revision under India’s PM-JAY on provider behaviour manifesting in terms of utilisation of services. The PMJAY scheme is completely funded by the government and shared between central and state governments. At the time of inception of the scheme, national ceiling amount of ₹ 1052 per family was used to determine the central and state government share of the contribution. For states except North-Eastern States (Arunachal Pradesh, Assam, Manipur, Meghalaya, Mizoram, Nagaland and Tripura) and three Himalayan States (Jammu and Kashmir, Himachal Pradesh and Uttarakhand) and Union territories (UTs), the ratio of Central and State Government contribution is 60:40. The ratio for North-Eastern States and three Himalayan states is 90:10 and for UTs without legislatures, the Central Government may provide up to 100% on a case-to-case basis. More recently, with scheme maturity and increase in utilisation, it is proposed that the ceiling amount could be increased to ₹ 1500 per family. The issue of states bearing the full cost of scheme for population coverage beyond the SECC beneficiary base, or additional packages, or changes in prices at State level is important. However, given the fact that current utilisation of overall budget of NHA has not exceeded the allocation,36 it is not of immediate concern, and hence does not affect our study findings.
Overall, we found that the HBP revision led to a positive impact on utilisation of services. While changes in HBP nomenclature and construct had a positive effect, incorporating price corrections further accentuated the impact. Second, pricing reforms led to a significantly higher impact on those packages which were originally significantly under-priced. However, within the category of packages as per the original cost-price differential, there was no dose–response relationship based on extent of price correction. Third, the impact of provisioning in private sector hospitals was not different from the overall trends. Fourth, after a basic number of hospitals are empanelled, subsequent increase in hospital numbers does not have any significant effect on expanding access, unless it is accompanied with an appropriate health benefit package design.
The findings hold significance in the context of achieving the best outcomes of government funded health insurance programs. Improving the description of the package, i.e., nomenclature and construct improves its uptake, implying that it is advisable to keep the package updated with recent medical knowledge and practice. Our findings also imply that the price levels are the most important aspect of the HBP revision, which is likely to have the largest impact on its utilisation. An interesting finding of our study was the lack of any dose–response relationship between the extent of correction of pricing and utilisation. However, at an overall level, there is a positive relationship between increase in prices and utilisation. This implies that the price signals operate at an overall level, rather than package by package. This is justified considering a lack of robust cost-accounting system in hospitals, especially majority of small and medium-sized hospitals.37,38 This implies that while these hospitals recognise whether the overall revenue being earned through the patients treated under government funded insurance programs is meeting their costs, they do not have very good cost data for each intervention or service to compare intervention specific revenue and costs. So, any increase in the price gives a general signal which decreases the probability of denial of care or increases the probability for increased utilisation. Another reason which may explain the lack of a dose–response relationship is the ability of hospitals to be able to cross-subsidise the relatively under-priced packages, with those which are appropriately or relatively-generously priced. As a result, while the hospitals may implicitly demonstrate a certain degree of agreement for supply-side cost sharing for certain packages, they are able to breakeven and make some profit at the overall hospital revenue given the case-mix. Our findings can also be explained based on the fact that several hospitals consider empanelment in government-funded insurance schemes important for branding and improving patient footfalls.39,40 This is indirect effect on the overall hospital revenue, through which relatively under-priced packages are cross-subsidised.
The lack of any significant effect of increase in hospital numbers is because initial empanelment of hospitals is based on willingness to join the scheme and provide services. Subsequent increase in empanelment is either due to a government policy to simply empanel a particular category of health facilities directly, or based on a hospital’s decision to get empanelled for branding to attract other non-PMJAY patients, and hence these additional hospitals do not contribute much to expand access. This is also reflected from the PMJAY reports which shows a limited proportion of hospitals account for the predominant share of overall claims.41 Together, this implies that the policy makers in such government-funded insurance programmes need to focus more on the quality of a basic minimum hospitals than unnecessary focus on expanding the hospital numbers.
Published evidence globally also suggests that the effect of changes in regulated prices on volume of care provided is a manifestation of a change in relative prices among different groups of services,42 and an overall change in price level or the income effect. Our findings suggest a mix of the two operating together. While the findings of Table 3 suggest the former effect, lack of a dose response relationship, reported in Table 4 and is an indication of the latter. Hence, our findings agree with international literature on provider behaviour. Several other studies have found mixed effect of changes in utilisation with changes in base rate for reimbursement.43, 44, 45, 46, 47 Even within the same context, a 10% price increase corresponded to a 0.8–1.3% rise in number of medical cases, while no price effect was observed in surgical cases. The rise may be attributed to physician induced demand either to maximise the profit margins or enhance care to attract more patients in a competitive market.45 Further, patients admitted for medical treatment are more open to discretion compared with surgical treatment. We did not make any assessment of the medical packages since there was no price change among those, besides owing to this fact that the medical packages are prone to more supplier discretion for maintaining incomes.
To the best of our knowledge, this is the first comprehensive assessment of a large government funded health insurance program in terms of impact of HBP revisions. Majority of the previous evaluations have mainly focussed on how prices or reimbursement rates impact on provider behaviour.48, 49, 50 Moreover, majority of these assessments have been reported from high-income country context of either the USA or the Western European countries or Australia, and several of those evaluations were in the context of fee-for-service schedules whereas most of the countries globally are moving towards case-based bundled payments. More importantly, due to absence of comparison of prices with cost, none of the previous papers have evaluated a dose–response relationship with the impact of price changes on either the original price (relative to its cost), or the extent of subsequent price correction. We bridge this important limitation by using the nationally representative cost data from India,27,28,33 which is a major strength of our study. Moreover, we take a comprehensive view of various potential HBP revisions, and consider evaluating various combinations of these HBP policy reforms.
Any such time-series analysis design to evaluate the impact of policy changes in HBP is likely to be confounded by other concurrent demand and supply-side factors in the health system. For example, increase in the population coverage, improvements in awareness among patients about benefits of government funded insurance, increase in the number of hospitals getting empanelled and providing care, increase in services included in the HBP, or other strategies to improve quality of care or patient satisfaction can independently result in an increase in utilisation. In the context of present evaluation, first, we used a matched dataset of common procedures for analysis, and hence there is no effect in change of service coverage. Second, an important supply-side confounding variable, i.e., number of hospitals empanelled was adjusted in our regression analysis. Third, there was only 4.2% increase in population coverage for PM-JAY in Punjab state during the post intervention period, which is unlikely to affect the utilisation as much as observed in our study. Fourth, the changes in demographic and epidemiological parameters can also confound the analysis, however, these are unlikely to change over the short time-horizon of present analysis. Fifth, we introduced a dose–response stratification for packages in our evaluation design, based on the level of original cost-price differential in HBP 1.0, as well as subsequently, another stratification based on extent of cost-price correction in HBP 2.0. If there had been an increase in utilisation across all sub-groups, it would have been difficult to refute the role of these potential confounders. However, since we did not find any significant increase for half of the sub-groups, there is little reason to believe any confounding unless either of demand or supply side factors were specifically changing for those originally significantly under-priced packages. The latter was an unlikely possibility. Moreover, given the relatively short time horizon of evaluation, several of these potential confounders are less likely to change significantly. Hence, we believe that our findings are valid.
We do acknowledge certain limitations of our analysis. First, while we evaluate the impact on utilisation, we are unable to distinguish whether the increase was a fulfilment of genuine ‘need’, or induced by providers. We analysed the data comprising of month-wise pooled number of claims, rather than patient level claims data with clinical information. Hence, we could not examine patient level characteristics to assess the need for treatment. However, since the provider behaviour of private sector was not significantly different from the overall, or public sector providers specifically—which may not have any significant incentives to induce demand, this indirectly indicates that the increased utilisation is unlikely to be supplier-induced. Second, we could not measure any changes in quality of care. This is an important intended outcome of HBP revision of change in construct. However, due to absence of data on patient reported outcomes after treatment in the claims data, we could not evaluate the same. This is an important area of future research, especially considering the PM-JAY’s recent advancements towards value-based care.51 Third, as the study time overlapped with COVID-19 pandemic, it may have influenced the overall value of the pre-slope and post-slope coefficients. However, it is important that given the timeline, COVID-19 should have impacted the post intervention period of HBP reforms much more. Since the overall utilisation was found to be higher in post HBP intervention period, it is likely that the impact of HBP reforms would have been even higher without COVID-19. Further, it is important to note that the degree to which COVID-19 pandemic influenced the utilisation trends would have been similar for packages which had a change in nomenclature, construct, pricing, any combination of these revisions, or no change. Moreover, it would have been similar among packages with different levels of the price correction which was another level of stratification. Hence, the presence of control group (no change in HBP 2.0), and the dose–response relationship through creation of multiple stratifications of packages, helps to examine the role of any potential confounder, including COVID-19 pandemic. Since, the rate of change is different in different groups, it indicates that there was no significant effect of COVID-19 on the validity of our study findings. Lastly, the impact of HBP revisions would vary across different states owing to differences in demographic transitions, care-seeking pattern, population coverage, number of hospitals empanelled under the scheme, service provision (number of packages) based on the type of HBP version implemented in the state. Currently, all states are operating at different HBP versions in India. All these factors will contribute to differences in impact of the same HBP version implemented in different states. Therefore, our findings may not be generalisable across other states of the country. Hence, future research is recommended to compare the extent of impact across states and examine the role of these contextual factors.
To conclude, our paper makes significant contribution to the existing literature by combining the data on volume of claims, prices, and cost of health care packages, to examine the impact of HBP revisions. Our paper demonstrates the significant positive impact of PM-JAY HBP revisions in package nomenclature, construct and pricing. Such HBP revisions need to very thoughtfully undertaken, with the anticipation of its long-term intended effects. Our paper also demonstrates the importance of aligning the prices with the actual cost of care, which has also been argued by several other previous papers19,27,28,33,34 commenting on PM-JAY provider payment rates.
Contributors
Conceptualisation: SP; Data curation: SP, JD, RN, RK; Formal analysis: RN, JD, RK, SP; Funding acquisition: SP, AP; Investigation: SP, JD, RN, RK; Methodology: SP, JD, RN,RK; Project administration: SP, JD; Resources, software: SP, JD, RN; Supervision: SP; Validation: SP, JD, BG, AP, AKG, RN, RK; Visualisation: SP, JD, BG, AP, AKG, RN, RK; Writing–original draft, and writing: SP,JD, RK, RN; Review & editing: SP, JD, RK, RN, BG, AP, AKG.
Data sharing statement
The datasets and analysis will be available upon request. The study investigators retain ownership of their data. Any requests for access to data should be made directly to study investigator.
Declaration of interests
The present manuscript was written as part of a project funded by ‘The Deutsche Gesellschaft für Internationale Zusammenarbeit’, also known as GIZ. The project funding was made to the institution –Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. We would like to note that the lead author—Shankar Prinja, has formerly served as the Executive Director at the National Health Authority (NHA), while Basant Garg is currently the Additional CEO of the NHA. The authors declare no other conflicts of interest.
Acknowledgements
We would like to express our sincere gratitude to the Department of Health Research (DHR), Ministry of Health and Family Welfare, New Delhi, for funding the data collection for the estimation of the cost of delivering various health benefit packages included in the present study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2024.100462.
Appendix A. Supplementary data
References
- 1.The World Health Report: Health Systems Financing: the path to universal coverage. World Health Organization; 2010. https://apps.who.int/iris/handle/10665/44371 [cited 2023 Aug 17]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muttaqien M., Setiyaningsih H., Aristianti V., et al. Why did informal sector workers stop paying for health insurance in Indonesia? Exploring enrollees' ability and willingness to p ay. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0252708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miti J.J., Perkio M., Metteri A., Atkins S. Factors associated with willingness to pay for health insurance and pension scheme among informal economy workers in low- and middle-income countries: a systematic review. Int J Soc Econ. 2021;48(1):17–37. doi: 10.1108/IJSE-03-2020-0165. [DOI] [Google Scholar]
- 4.RSBY. Ministry of Health and Family Welfare, Government of India; 2008. http://www.rsby.gov.in/how_works.html [cited 2023 Aug 18]. Available from: [Google Scholar]
- 5.PM-JAY . National Health Authority; 2021. Official website of pradhan Mantri jan Arogya Yojana (PM-JAY)https://pmjay.gov.in/ [cited 2023 Aug 18]. Available from: [Google Scholar]
- 6.Maritim B., Koon A.D., Kimaina A., et al. “It is like an umbrella covering you, yet it does not protect you from the rain”: a mixed methods study of insurance affordability, coverage, and financial protection in rural western Kenya. Int J Equity Health. 2023;22(1):27. doi: 10.1186/s12939-023-01837-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chakraborty Sarbani. UNICO studies series;No. 22. World Bank; Washington DC: 2013. Philippines' government sponsored health coverage program for poor households.http://hdl.handle.net/10986/13295 License: CC BY 3.0 IGO. [Google Scholar]
- 8.Obermann K., Jowett M., Kwon S. The role of national health insurance for achieving UHC in the Philippines: a mixed methods analysis. Glob Health Action. 2018;11(1) doi: 10.1080/16549716.2018.1483638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szigeti S., Evetovits T., Kutzin J., Gaál P. Tax-funded social health insurance: an analysis of revenue sources, Hungary. Bull World Health Organ. 2019;97(5):335–348. doi: 10.2471/BLT.18.218982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glassman A., Giedion U., Sakuma Y., Smith P.C. Defining a health benefits package: what are the necessary processes? Health Syst Reform. 2016;2(1):39–50. doi: 10.1080/23288604.2016.1124171. [DOI] [PubMed] [Google Scholar]
- 11.Glassman A., Giedion U., Smith P.C., editors. What’s in, what's out: designing benefits for universal health coverage. Brookings Institution Press; 2017. [Google Scholar]
- 12.Ayushman Bharat –Pradhan Mantri jan AarogyaYojana (AB-PMJAY) to be launched by Prime Minister Shri Narendra Modi in Ranchi, Jharkahnd on September 23, 2018. Government of India, Ministry of Health and Family Welfare; 2018. https://pib.gov.in/Pressreleaseshare.aspx?PRID=1546948 [cited 2023 Aug 17]. Available from: [Google Scholar]
- 13.Lahariya C. ‘Ayushman Bharat’ program and universal health coverage in India. Indian Pediatr. 2018;55(6):495–506. [PubMed] [Google Scholar]
- 14.Agarwal P. 2019. Govt to revise ayushman Bharat rates as several hospitals back off.https://www.thequint.com/news/india/ayushman-bharat-pmjay-rates-to-be-hiked-to-get-big-hospitals-on-board#read-more [cited 2023 Aug 17]. Available from: [Google Scholar]
- 15.Ayushman reimbursement for private hospitals short of costs incurred: FICCI/EY Report. 2019. https://www.thehindubusinessline.com/money-and-banking/ayushman-reimbursement-for-private-hospitals-short-of-costs-incurred-ficciey-report/article29183285.ece [cited 2023 Aug 17]. Available from: [Google Scholar]
- 16.Sharma P. 2022. Private hospitals avoid Ayushman Bharat PMJAY, citing low charges.https://www.livemint.com/news/india/private-hospitals-avoid-ayushman-bharat-pmjay-citing-low-charges-11662050592878.html [cited 2023 Aug 17]. Available from: [Google Scholar]
- 17.Saxena A., Trivedi M., Shroff Z.C., Sharma M. Improving hospital-based processes for effective implementation of Government funded health insurance schemes: evidence from early implementation of PM-JAY in India. BMC Health Serv Res. 2022;22(1):73. doi: 10.1186/s12913-021-07448-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Journey from HBP 1.0 to HBP 2.0. Pmjay.gov.in. 2020. https://pmjay.gov.in/sites/default/files/2020-01/Journey-from-HBP-1.0-to-HBP-2.0.pdf [cited 17 August 2023]. Available from: [Google Scholar]
- 19.Prinja S., Singh M.P., Rajsekar K., et al. CHSI Study Group Translating research to policy: setting provider payment rates for strategic purchasing under India’s national publicly financed health insurance scheme. Appl Health Econ Health Policy. 2021;19(3):353–370. doi: 10.1007/s40258-020-00631-3. doi: 10.1007/s40258-020-00631-3. Epub 2021 Jan 19. Erratum in: Appl Health Econ Health Policy. 2021 May;19(3):451. [DOI] [PubMed] [Google Scholar]
- 20.Health benefit package - 2.0. National Health Authority; 2019. https://pmjay.gov.in/hospital/hbc [cited 2023 Aug 17]. Available from: [Google Scholar]
- 21.National master health benefit packages 2.1. National Health Authority; 2020. https://pmjay.gov.in/hospital/hbc [cited 2023 Aug 17]. Available from: [Google Scholar]
- 22.National master health benefit packages 2.2. National Health Authority; 2021. https://pmjay.gov.in/hospital/hbc [cited 2023 Aug 17]. Available from: [Google Scholar]
- 23.HBP 2022 package master and OM. National Health Authority; 2022. https://pmjay.gov.in/hospital/hbc [cited 2023 Jun 17]. Available from: [Google Scholar]
- 24.Bhatt R. The Hindu; 2022. NHA launches new version of Health Benefit Package under AB-PMJAY adding 365 new procedures.https://www.thehindu.com/news/national/nha-launches-new-version-of-health-benefit-package-under-ab-pmjay-adding-365-new-procedures/article65303372.ece The Hindu. [cited 2023 Aug 17]; Available from: [Google Scholar]
- 25.Government Orders regarding allowing 25 packages out of 180 Government reseverd 180 Packages (HBP2.0) in private hospitals. State Health Agency, Government of Punjab; 2020. https://www.sha.punjab.gov.in/shapunjab/downloadfiles/letters/Order_reagrding_25_packages_HBP20.pdf [cited 2023 Aug 17]. Available from: [Google Scholar]
- 26.PMJAY - NHA | Setu dashbaord. National Health Authority; 2023. https://dashboard.pmjay.gov.in/ [cited 2023 Aug 17]. Available from: [Google Scholar]
- 27.Singh M.P., Prinja S., Rajsekar K., et al. Cost of surgical care at public sector district hospitals in India: implications for universal health coverage and publicly financed health insurance schemes. Pharmacoecon Open. 2022;6(5):745–756. doi: 10.1007/s41669-022-00342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prinja S., Chauhan A.S., Rajsekhar K., et al. Addressing the cost data gap for universal healthcare coverage in India: a call to action. Value Health Reg Issues. 2020;21:226–229. doi: 10.1016/j.vhri.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 29.National health system cost Database for India. https://www.healtheconomics.pgisph.in/costing_web/ [cited 2023 Aug 17]. Available from:
- 30.Prinja S., Singh M.P., Guinness L., Rajsekar K., Bhargava B. Establishing reference costs for the health benefit packages under universal health coverage in India: cost of health services in India (CHSI) protocol. BMJ Open. 2020;10(7) doi: 10.1136/bmjopen-2019-035170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prinja S., Brar S., Singh M.P., et al. Process evaluation of health system costing - experience from CHSI study in India. PLoS One. 2020;15(5) doi: 10.1371/journal.pone.0232873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh M.P., Popli R., Brar S., et al. CHSI costing study-Challenges and solutions for cost data collection in private hospitals in India. PLoS One. 2022;17(12) doi: 10.1371/journal.pone.0276399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bahuguna P., Guinness L., Sharma S., Chauhan A.S., Downey L., Prinja S. Estimating the unit costs of healthcare service delivery in India: addressing information gaps for price setting and health technology assessment. Appl Health Econ Health Policy. 2020;18(5):699–711. doi: 10.1007/s40258-020-00566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prinja S., Chauhan A.S., Bahuguna P., Selvaraj S., Muraleedharan V.R., Sundararaman T. Cost of delivering secondary healthcare through the public sector in India. Pharmacoecon Open. 2020;4(2):249–261. doi: 10.1007/s41669-019-00176-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramsay C.R., Matowe L., Grilli R., Grimshaw J.M., Thomas R.E. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. Int J Technol Assess Health Care. 2003;19(4):613–623. doi: 10.1017/s0266462303000576. [DOI] [PubMed] [Google Scholar]
- 36.https://cag.gov.in/uploads/download_audit_report/2022/Executive-Summary-063fdee41243906.10069496.pdf [cited 2024 Jan 28]. Available from:
- 37.Demystifying healthcare costs: A scientific approach- India’s rst scientic study on costing of medical procedures across public and private hospitals. Federation of Indian Chambers of Commerce and Industry (FICCI); 2018. https://ficci.in/api/study_details/23028 [cited 2023Mar30]. Available from: [Google Scholar]
- 38.Assessment of the healthcare delivery market in India. Credit Rating Information Services of India Limited (CRISIL); Mumbai, Maharashtra: 2022. pp. 1–111. [Google Scholar]
- 39.Yadav V., Kumar S., Balasubramaniam S., et al. Facilitators and barriers to participation of private sector health facilities in government-led schemes for maternity services in India: a qualitative study. BMJ Open. 2017;7(6) doi: 10.1136/bmjopen-2017-017092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dave H.S., Patwa J.R., Pandit N.B. Facilitators and barriers to participation of the private sector health facilities in health insurance & government-led schemes in India. Clin Epidemiol Global Health. 2021;10 doi: 10.1016/j.cegh.2021.100699. [DOI] [Google Scholar]
- 41.Kaur S., Jain N., Bhatnagar P.C. Early trends from utilization of oncology services: insights from ayushman Bharat pradhan Mantri jan Arogya Yojana (PMJAY). National Health Authority. https://pmjay.gov.in/sites/default/files/2021-05/Working%20paper%20004-%20Utilization%20of%20Oncology%20services.pdf (no date) [cited 2023 Sep 03] Available at:
- 42.McGuire T.G., Pauly M.V. Physician response to fee changes with multiple payers. J Health Econ. 1991;10(4):385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- 43.Melberg H.O., Beck Olsen C., Pedersen K. Did hospitals respond to changes in weights of Diagnosis Related Groups in Norway between 2006 and 2013? Health Policy. 2016;120(9):992–1000. doi: 10.1016/j.healthpol.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 44.Callison K., Nguyen B.T. The effect of Medicaid physician fee increases on health care access, utilization, and expenditures. Health Serv Res. 2018;53(2):690–710. doi: 10.1111/1475-6773.12698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Januleviciute J., Askildsen J.E., Kaarboe O., Siciliani L., Sutton M. How do hospitals respond to price changes? Evidence from Norway. Health Econ. 2016;25(5):620–636. doi: 10.1002/hec.3179. Epub 2015 Apr 30. [DOI] [PubMed] [Google Scholar]
- 46.Wei W., Ulyte A., Gruebner O., et al. Degree of regional variation and effects of health insurance-related factors on the utilization of 24 diverse healthcare services - a cross-sectional study. BMC Health Serv Res. 2020;20(1):1091. doi: 10.1186/s12913-020-05930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huitfeldt I. Hospital reimbursement and capacity constraints: evidence from orthopedic surgeries. Health Policy. 2021;125(6):732–738. doi: 10.1016/j.healthpol.2021.02.004. [DOI] [PubMed] [Google Scholar]
- 48.Gosden T., Forland F., Kristiansen I.S., et al. Impact of payment method on behaviour of primary care physicians: a systematic review. J Health Serv Res Policy. 2001;6(1):44–55. doi: 10.1258/1355819011927198. [DOI] [PubMed] [Google Scholar]
- 49.Hennig-Schmidt H., Selten R., Wiesen D. How payment systems affect physicians' provision behaviour--an experimental investigation. J Health Econ. 2011;30(4):637–646. doi: 10.1016/j.jhealeco.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 50.Feldhaus I., Mathauer I. Effects of mixed provider payment systems and aligned cost sharing practices on expenditure growth management, efficiency, and equity: a structured review of the literature. BMC Health Serv Res. 2018;18(1):996. doi: 10.1186/s12913-018-3779-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Volume-based to value-based care: Ensuring better health outcomes and quality healthcare under AB PM-JAY. National health authority | official website ayushman Bharat digital mission. https://abdm.gov.in:8081/uploads/VBHC_Policy_Document_For_Upload_a20f871a55.pdf [cited 2023 Aug 18]. Available from:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.