Abstract
Tuberculosis is a rare but treatable infectious disease that continues to pose a significant health issue in regions with high prevalence. Its abdominopelvic localization can mimic advanced ovarian cancer, leading to diagnostic challenges. This report describes the case of a 33-year-old woman who was admitted to the gastroenterology unit with ascites, peritoneal thickening, and an ovarian mass on imaging. The diagnosis of abdominopelvic and peritoneal tuberculosis was confirmed after laparoscopy. The patient underwent antitubercular chemotherapy and showed clinical improvement.
Keywords: Ascites, abdominal mass, ovarian neoplasm, laparotomy, tuberculosis
Introduction
Tuberculosis, an infectious disease that can be effectively treated with appropriate medical intervention, has seen a resurgence worldwide, particularly in areas with high endemicity. This increase is largely attributed to the immunosuppressive effects of HIV infection. Pelvic tuberculosis is observed in approximately 15% of cases and often presents in a pseudotumoral form that can resemble malignant ovarian tumors. 1 In this report, we present a case of pelviperitoneal tuberculosis that mimicked ovarian cancer.
Case report
A 33-year-old woman was admitted to the gastroenterology unit for the investigation of ascites. She presented with a 6-month history of lower abdominal pain, accompanied by a weight loss of 9 kg. Additionally, she had observed progressive abdominal swelling over the past 2 months and amenorrhea. Seven months prior, she had delivered a healthy male infant.
Physical examination revealed moderate ascites, but no masses or lymphadenopathy were detected. Other systemic examinations were normal.
Blood tests indicated signs of an inflammatory syndrome, with a C-reactive protein level of 138 mg/L and elevated CA-125 serum levels of 396 U/mL (normal range: <35 U/mL). All other laboratory results were within normal limits. Her chest X-ray was also normal.
Our patient did not undergo an abdominal ultrasound, but computed tomography (CT) scan revealed a multicystic, thick-walled formation measuring 155 × 168 × 80 mm. Both ovaries were found to be protruding into the lesion. The uterus, liver, spleen, pancreas, and kidneys appeared normal.
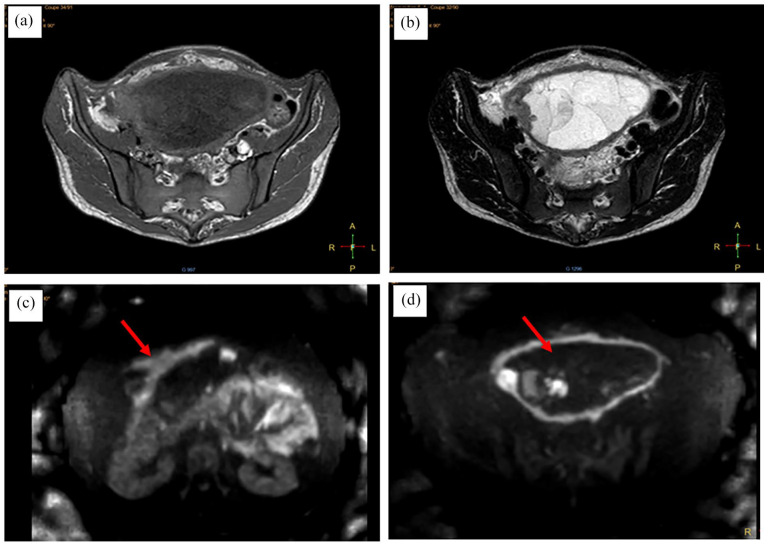
Pelvic magnetic resonance imaging (MRI) (Figure 1) showed an abdominopelvic, multi-septated cystic mass, likely originating from the left ovary. The mass had a thickened, irregular, and nodular wall with internal vegetations suggesting endocytic development. It exhibited hypointensity on T1-weighted imaging, intermediate hypointensity on T2-weighted imaging, significant diffusion hypersignal, and marked enhancement following contrast injection. The mass measured 140 × 135 × 180 mm. Suspected bilateral iliac lymphadenopathies were observed, with the largest on the left external iliac, measuring 15 × 8.5 mm. Ascites was noted along with peritoneal thickening and the presence of two regular peritoneal nodules.
Figure 1.
Pelvic magnetic resonance imaging showing an abdominopelvic multi-septated cystic mass with T1 hypointensity and a fairly intense and regular contrast enhancement of the walls of the mass and intramural budding lesions and peritoneal leaves (a). The mass exhibits a heterogeneous content showing hyperintensity on T2-weighted imaging, containing portions with hypointensity on T2 and some thin septations (b). Presence of free peritoneal nodules (red arrow) at the level of the greater omentum (c) and the diffusion sequence showed diffusion hyperintensity of the mass wall and intramural vegetating portions (red arrow) (d).
The diagnosis of ovarian cancer with peritoneal carcinomatosis was suspected, leading to a laparoscopy. This procedure revealed a large mass, exceeding 200 mm in size, adherent to the posterior wall of the uterus at the fundus and the intestinal loops at the top, with evidence of hardening and infiltration. The omentum also showed hardening and was speckled with multiple nodules, as were the uterus, fallopian tubes, and small bowel loops. Both ovaries were not visualized during the procedure.
Biopsies were taken from the peritoneal surface, pelvic mass, and omentum for frozen-section analysis. All specimens showed epitheliod granulomas with central caseous necrosis and no evidence of malignancy (Figure 2). These findings strongly suggested pelviperitoneal tuberculosis.
Figure 2.
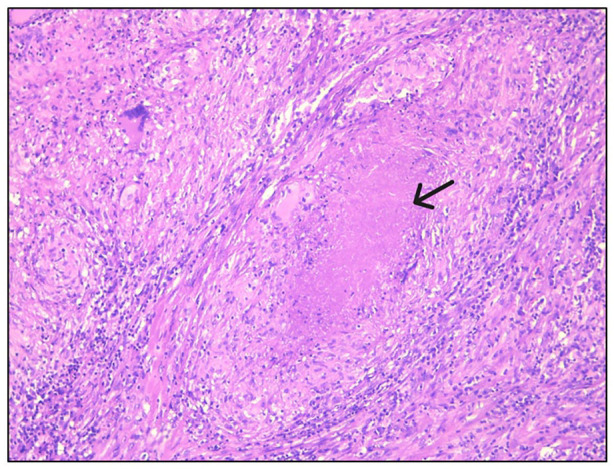
Results of the histological study of pelvic mass specimen. Ovarian tissue contains numerous epithelioid granulomas with giant cells. Some granulomas show central necrosis (black arrow) (HE stain 100×).
A four-drug regimen for tuberculosis was prescribed, consisting of isoniazid, rifampicin, pyrazinamide, and ethambutol for an initial 2-month phase, followed by a continuation phase of isoniazid and rifampicin for an additional 4 months. During follow-up, clinical improvement was observed, marked by the resolution of symptoms and the normalization of the biological inflammatory markers.
Discussion
The incidence of genital tuberculosis varies significantly across countries, with estimates ranging from less than 1% in the United States to 19% in India. 2 Female genital tuberculosis is most commonly diagnosed in patients aged 20–40 years. 3 The most frequently affected sites are the endometrium (72%), followed by the fallopian tubes (34%), ovaries (12.9%), and cervix (2.4%). 4 Pelvic localization primarily occurs through hematogenous spread.
Pseudotumoral abdominopelvic tuberculosis is a rare clinical form that can mimic advanced ovarian cancer, presenting significant diagnostic challenges. It often manifests with symptoms such as abdominal pain, ascites, an abdominopelvic mass, and weight loss, which can resemble peritoneal carcinomatosis of ovarian origin. Infertility is observed in approximately 15% of cases. 4 Other associated signs may include menstrual irregularities, dyspareunia, and bowel or urinary symptoms. Pulmonary and digestive symptoms are absent in 30%–50% of cases. 5
When peritoneal tuberculosis broadly affects the ovaries and fallopian tubes, tubo-ovarian lesions often appear minimal on CT scans. MRI is particularly useful for identifying these lesions, as it can reveal thickened fallopian tubes or nodularities on the surfaces of the ovaries and fallopian tubes. Calcifications in adnexal masses observed on CT scans may suggest tuberculosis. However, findings from both CT and MRI are nonspecific. 6
A gynecological ultrasound performed by an experienced examiner can help differentiate a malignant ovarian tumor from a benign cause, such as tuberculosis, with a sensitivity of 100% and a specificity of 86%. 7 These findings could enable conservative, fertility-preserving surgery for young women with this condition. In fact, transvaginal ultrasound has identified specific features of female pelvic tuberculosis, including thickened omentum, septate ascites, and solid, sausage-like lesions of the fallopian tubes. 8 On the other hand, a sausage-shaped cystic structure with solid tissue protruding into it like a papillary projection, a sausage-shaped cystic structure with a large solid component filling part of the cyst cavity, and an ovoid or oblong completely solid mass were recognized as characteristic of tubal carcinoma. 9 Ultrasound can also differentiate between various subclasses of malignant serous ovarian tumors. 10
CA-125 is a tumor biomarker commonly used for ovarian cancer diagnosis. However, elevated levels can also occur during pregnancy and in pelvic inflammatory conditions such as tuberculosis. Therefore, CA-125 testing alone cannot distinguish between pelvic tuberculosis and ovarian cancer, making differential diagnosis challenging. This often necessitates surgical intervention, either through laparotomy or laparoscopy, with a diagnostic success rate of 97%. 11
Peritoneal biopsies can reveal granulomatous inflammation with caseation necrosis, which are characteristic of tuberculosis. However, bacteriological examination of ascites is rarely positive. 11 The treatment for pelvic tuberculosis is medical and involves a combination of isoniazid, rifampicin, ethambutol, and pyrazinamide for an initial 2 months, followed by isoniazid and rifampicin for an additional 4 months. 12 A randomized controlled trial involving 175 women with female genital tuberculosis found no significant difference between 6 and 9 months of antituberculous therapy. 13
Surgical interventions, such as salpingectomy, may be considered to enhance fertility outcomes. 12 The prognosis of pelvic tuberculosis is significantly affected by infertility in young women, with an estimated risk of tubo-ovarian infertility at 39%. 4
Other cases of tuberculosis that mimic intra-abdominal neoplasms, such as pancreatic cancer, intestinal tumors, or carcinomatosis, have also been described.14,15 In all cases, the diagnosis was confirmed through histological examination of the mass specimen, and treatment was based on antitubercular drugs.
Conclusion
Pseudotumoral pelviperitoneal tuberculosis is a rare but treatable infectious condition. Its clinical, radiological, and biological presentations can closely mimic those of malignant ovarian tumors, leading to diagnostic challenges. The prognosis of this condition is closely linked to tubo-ovarian infertility.
Acknowledgments
ChatGPT was used for English correction.
Footnotes
Author contributions: M.Z. conception; L.R. writing the manuscript; B.R. investigation; B.A. data collection; G.A. design; G.S. data collection;
J.I. literature review; C.N. critical review; Z.A. supervision; L.M.H. critical review; L.S. supervision.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases.
Consent: The patient provided written informed consent for the publication of this case report and the related images.
ORCID iD: Zakhama Mejda  https://orcid.org/0000-0003-3127-527X
https://orcid.org/0000-0003-3127-527X
References
- 1. Kefi A, Daoud F, Aydi Z, et al. Granulomatose ovarienne tuberculeuse simulant un cancer de l’ovaire. Rev Méd Interne 2015; 36: A181. [Google Scholar]
- 2. World Health Organization. Global tuberculosis report 2020. Geneva: World Health Organization, 2020. [Google Scholar]
- 3. Shrivastava I, Bhatambare GS, Deshmukh AB, et al. Genital tuberculosis: evaluating microscopy, culture, histopathology and PCR for diagnosis all play their role. Int J Curr Microbiol Appl Sci 2014; 3(4): 439–445. [Google Scholar]
- 4. Namavar Jahromi B, Parsanezhad ME, Ghane-Shirazi R. Female genital tuberculosis and infertility. Int J Gynecol Obstet 2001; 75(3): 269–272. [DOI] [PubMed] [Google Scholar]
- 5. Adsuar N, Blanchette H, Kilchevsky E. Tuberculosis peritonitis mimicking ovarian cancer in a 20-year-old woman. A case report. J Reprod Med 2004; 49(1): 52–54. [PubMed] [Google Scholar]
- 6. Kim SH, Kim SH, Yang DM, et al. Unusual causes of tubo-ovarian abscess: CT and MR imaging findings. Radiographics 2004; 24(6): 1575–1589. [DOI] [PubMed] [Google Scholar]
- 7. Di Legge A, Pollastri P, Mancari R, et al. Clinical and ultrasound characteristics of surgically removed adnexal lesions with largest diameter ⩽ 2.5 cm: a pictorial essay. Ultrasound Obstet Gynecol 2017; 50(5): 648–656. [DOI] [PubMed] [Google Scholar]
- 8. Ludovisi M, Bruno M, Capanna G, et al. Sonographic features of pelvic tuberculosis mimicking ovarian-tubal-peritoneal carcinoma. Ultrasound Obstet Gynecol 2023; 61(4): 536–538. [DOI] [PubMed] [Google Scholar]
- 9. Ludovisi M, De Blasis I, Virgilio B, et al. Imaging in gynecological disease (9): clinical and ultrasound characteristics of tubal cancer. Ultrasound Obstet Gynecol 2014; 43(3): 328–335. [DOI] [PubMed] [Google Scholar]
- 10. Moro F, Baima Poma C, Zannoni GF, et al. Imaging in gynecological disease (12): clinical and ultrasound features of invasive and non-invasive malignant serous ovarian tumors. Ultrasound Obstet Gynecol 2017; 50(6): 788–799. [DOI] [PubMed] [Google Scholar]
- 11. Volpi E, Calgaro M, Ferrero A, et al. Genital and peritoneal tuberculosis: potential role of laparoscopy in diagnosis and management. J Am Assoc Gynecol Laparosc 2004; 11(2): 269–272. [DOI] [PubMed] [Google Scholar]
- 12. Tjahyadi D, Ropii B, Tjandraprawira KD, et al. Female genital tuberculosis: clinical presentation, current diagnosis, and treatment. Infect Dis Obstet Gynecol 2022; 2022: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sharma JB, Singh N, Dharmendra S, et al. Six months versus nine months anti-tuberculous therapy for female genital tuberculosis: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 2016; 203: 264–273. [DOI] [PubMed] [Google Scholar]
- 14. Siddeek RAT, Gupta A, Singla T, et al. Pancreatic tuberculosis mimicking as pancreatic malignancy: surgeon’s dilemma. Indian J Pathol Microbiol 2023; 66(3): 614. [DOI] [PubMed] [Google Scholar]
- 15. Suárez-Noya A, González-Bernardo O, Riera-Velasco JR, et al. Intestinal tuberculosis mimicking colon cancer. Rev Gastroenterol México Engl Ed 2023; 88(2): 183–186. [DOI] [PubMed] [Google Scholar]