Abstract
Introduction and importance
Primary total hip arthroplasty (THA) is a procedure performed in the United States for a variety of indications, with operation rates slated to increase over 275 % by 2040 when compared to 2014 (Thilak et al., 2015). Dual-mobility (DM) implants have gained popularity in the United States since gaining approval in the early 2010s (Heckmann et al., 2020). It has been well reported that DM implants decrease the risk of dislocation after primary and revision THA (Vielpeau et al., 2011; Donovan et al., 2022; Heifner et al., 2023; Foissey et al., 2023; Schmidt et al., 2020; Neri et al., 2019).
Case presentation
We present the case of a 33-year-old male with a suspected ankylosing spondylitis (AS) diagnosis and bilateral bony ankylosis of the hips who underwent staged THA with modular dual-mobility (MDM) implants. At one year post-operatively, the patient is walking without the use of an assistive device and reports a VAS pain score of 0 at rest and 2 with activity and HHS of 90.
Clinical discussion
Implant selection is important in this patient population due to the increased risk of dislocation. Contemporary reports reveal MDM implants have demonstrated a substantial reduction in dislocation risk compared to fixed-bearing implants in patients with a high risk of dislocation. We opted to place the acetabular component inside the safe zone to improve stability and use the dual-mobility prosthesis to achieve our desired range of motion.
Conclusion
The improved stability of DM implants allows for a greater range of acetabular positions in patients who have a highly unpredictable functional outcome at the time of surgery. Our preliminary results contribute to the growing list of indications for MDM total hip arthroplasty.
Keywords: Bony ankylosis, Case report, Dual mobility, Sequential reconstruction, Total hip arthroplasty
Highlights
-
•
We present the case of a 33-year-old male with bilateral bony ankylosis of the hips.
-
•
The patient was successfully treated with bilateral THA, staged six days apart.
-
•
Patient reported improved range of motion and quality of life and decreased pain.
-
•
The acetabular component placement was placed inside of Lewinnek's safe zone.
-
•
Dual-mobility implant provided greater arc and range of motion prior to impingement.
1. Introduction
Primary total hip arthroplasty (THA) is a procedure commonly performed in the United States for a variety of indications, with operation rates slated to increase over 275 % by 2040 when compared to 2014 [9]. Most commonly indicated in older patients with end-stage arthritic conditions that lead to joint space narrowing, decreased range of motion and pain, this procedure can provide significant improvements in outcomes for patients who find their condition inhibiting to activates of daily living.
Dual-mobility (DM) implants have gained popularity in the United States since gaining approval in the early 2010s [2]. The most modern generation of DM implants have substantially decreased the risk of intraprosthetic dislocation (IPD), aseptic loosening and polyethylene (PE) wear [8,10,11] present in the older designs. Neuromuscular disorders, spinal pathologies and inflammatory arthritis are risk factors for increased rates of dislocation following primary THA [12]. It has been well reported that DM implants decrease the risk of dislocation after primary and revision THA [[3], [4], [5], [6], [7], [8]].
We present the case of a 33-year-old male with a suspected diagnosis of ankylosing spondylitis (AS) and bilateral bony ankylosis of the hips. The patient had fixed flexion and adduction contractures of the bilateral hips which made ambulation without assistance unattainable and confined him to a wheelchair. He was successfully treated with bilateral THA, staged six days apart, using modular dual-mobility total hip arthroplasty prostheses. The presented work has been reported in line with the SCARE criteria for case reports [13]. Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
2. Case history
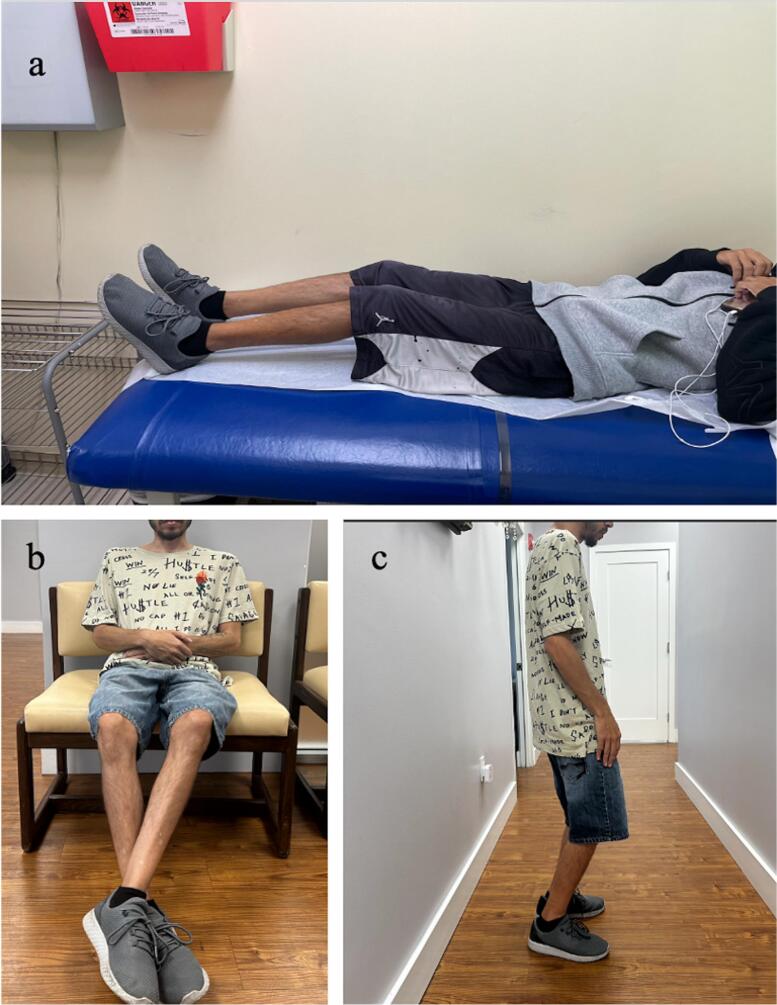
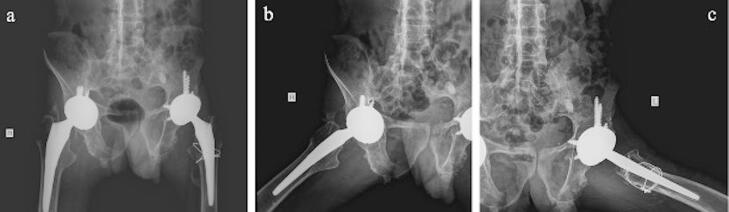
A 33-year-old male presented in the clinic with a twenty-plus year history of progressive pain and decreased range of motion (ROM) of the hips bilaterally. Upon initial interview, past medical history is significant for total nephrectomy at 1 year old for an atrophic kidney and a suspected diagnosis of AS at 3 years old. The patient is not currently receiving any additional treatment for AS. The patient ambulated with a walker and had severe restriction of extension of the hips (Fig. 1). Plain films were obtained and evaluated (Fig. 2). The patient was counseled on intervention options, with surgery recommended due to his past history of unsuccessful attempts at conservative treatments and progressive decline in ability to perform activities of daily living. The patient reported a VAS score of 6 at rest and 9 with activity and Harris Hip Score (HHS) of 29 bilaterally.
Fig. 1.
Preoperative anteroposterior radiograph of the pelvis demonstrating bilateral complete bony ankylosis of the hips.
Fig. 2.
Clinical photographs demonstrating (a) lying maximum hip extension and (b) standing max hip extension.
Preoperative planning consisted of obtaining images including X-rays of the lumbar spine, pelvis, and lower extremities and a CT scan of the pelvis and bilateral hips which was converted to 3D reconstructed images for a more accurate picture of the patient's anatomy. Results of the subsequent imaging confirmed bilateral bony ankylosis of the hips, with the hips flexed at approximately 85 degrees and adducted approximately 15 degrees.
Planning the operation in a patient such as this posed several critical issues. First, since there was no discernable delineation between the femoral head and acetabulum (best visualized by 3D reconstructed CT, Fig. 3), there would be no way to dislocate the hip joint, as is standard of care in total hip arthroplasty procedures. There was also detailed discussion in regards to the femoral neck cut and how a combination of large saw cuts and smaller, more precise bone resection utilizing a burr may be necessary if the patient's anatomy dictated so. Secondly, the chronicity of the patients' deformities raised concerns about possible distortions in anatomy over the surgical field, namely the location of the sciatic nerve as a posterior approach to the hip was planned. Consequently, it was a concern that post operatively the patient may acquire traction injuries to neurovascular structures with restoration of limb length. The greatest concern was the expectations of the surgery for the patient. Due to the fixed contracture deformities, proper hygiene was not possible. The primary goal of the operation was to improve range of motion to allow for proper hygiene with a secondary goal of restoring ambulation.
Fig. 3.
Preoperative anteroposterior (a) and posteroanterior (b) 3D reconstructed CT scans of the pelvis demonstrating complete bilateral bony ankylosis of the hips fixed in flexion and adduction.
The first procedure performed was a left total hip arthroplasty utilizing a posterior approach under general anesthesia. During broaching of the femur, a small crack was noted in the calcar therefore the decision to place one Luque wire was made. A dual-mobility implant with modular components was chosen for this patient due to reported improved range of motion with a press-fit femoral component and the acetabulum secured using five screws through the acetabular cup. The patient was placed in an abduction pillow in accordance with posterior hip precautions postoperatively. The patient remained impatient with adequate pain control and out of bed as tolerated while awaiting the subsequent procedure.
The second procedure performed was a right total hip arthroplasty six days after the index procedure. Great care was taken when positioning the patient in the left lateral decubitus paying respect to the existing left hip prothesis. The second procedure was conducted in the same manner as the first, utilizing an identical dual mobility implant, although only necessitating three screws to secure the acetabular cup. The patient remained impatient for 3 days prior to being discharged home. Due to evidence that patients with AS are at an elevated risk of developing heterotopic ossification (HO) [1,[14], [15], [16]], the patient was placed on Indomethacin 75 mg orally for two weeks for prophylaxis.
Throughout both procedures, the sciatic nerve was under direct visualization and tension was assessed prior to surgical dislocation, during trialing of protheses and after relocation with the final prosthesis. If inappropriate tension on the sciatic nerve was determined at any point in the procedure, leg length should be measured and great thought should be given to nerve release or if necessary, a subtrochanteric osteotomy to adequately relieve tension and avoid traction injury. Upon performing the capsulotomy and exposing the femoral neck, the anatomy was evaluated and determined that the femoral neck cut could be performed in accordance with the standard of care; starting approximately one centimeter above the lesser trochanter and at a 45-degree angle towards the tip of the greater trochanter. During trialing and final implantation of the acetabular cups, the manufacture's ante-inclination guide was used to ensure correct version and inclination.
The patient exhibited satisfactory wound healing with no evidence of infection and consistent progress in ambulation at initial follow-ups. At sequential follow-up visits, the patient reported minimal pain, significant improvement in ability to perform activities of daily living and range of motion (Fig. 4). At one year post-operatively, the patient is walking without the use of an assistive device and reports a VAS pain score of 0 at rest and 2 with activity and HHS of 90. One-year post operative radiographs demonstrate no change in component position and clinically insignificant Brooker grade 2 [17] heterotopic ossification about the tip of the greater trochanter on the right (Fig. 5).
Fig. 4.
Clinical photographs demonstrating post operative range of motion.
Fig. 5.
Anteroposterior (a), right lateral (b) and left lateral (c) radiographs of the pelvis and hip demonstrating well-fixed and appropriately positioned bilateral modular dual mobility total hip prostheses.
3. Discussion
Spontaneous bony ankylosis of the hips is a debilitating condition that significantly impacts the quality of life [16]. It has been reported that approximately 40 % of patients with AS have concomitant bony ankylosis of the hips [14]. Medical management is often insufficient to provide sustained improvements in ADLs [18]. Multimodal therapy regimens also only provide temporary relief as they do not correct the underlying deformity [19]. Total hip arthroplasty for spontaneous bony ankylosis of the hips has been often reported in the literature with favorable outcomes [[20], [21], [22]]. A recent systematic review by Lin et al. [23] reported a marked improvement in patient satisfaction, mobility and hip function following bilateral THA in AS. Jacob et al. [24] in 2022 reported a statistically significant improvement in Harris Hip Score (HSS) and ROM at a mean of 38 months follow-up that underwent primary THA for bony ankylosis. Similarly, Kumar et al. [25] reported 92 % survivorship at 10 years in 154 patients who received fixed-bearing cemented THA. Although, the authors also reported instability was the most common complication, with 50 % of those patients have more than three episodes of dislocation (3.9 %). Several studies report higher rates of dislocation, component revision and heterotopic ossification (HO) in AS patients after THA with fixed-bearing prostheses when compared to age-matched patients without AS [14,26,27].
Implant selection is particularly important in this patient population due to the inherent increased risk of dislocation. Chung et al. [28] reported that older patients with spontaneous bony ankylosis have higher dislocation rates following primary THA. Fixed-bearing THA implants have historically been the gold standard for these patients dating back to Charnley and Welch in the 1970s [16,29]. Recently, dual-mobility implants with modular components have increased in utilization for both primary and revision THA in the last decade [2,30]. Increased understanding of the inherent mechanics has driven an expansion of indications for DM including pathologies with increased risk of dislocation [10,[31], [32], [33]]. Contemporary results support the notion that MDM implants have demonstrated a substantial reduction in dislocation risk compared to fixed-bearing implants in patients with a high risk of dislocation [32]. The authors also considered the use of a fixed-bearing implant with a constrained liner due to the increased risk of dislocation but was ultimately decided against because of the patients age and desire for greater range of motion.
Procedural timing in bilateral disease can be adjusted to be optimize patient outcomes. It has been previously reported that bilateral synchronous THA is safe and has been effective in improving patients' quality of life [23,34]. Additionally, Mou et al. [35] reported that either synchronous or sequential operations revealed satisfactory clinical and radiographic outcomes. Several studies have reported various intervals between the index and subsequent procedure ranging from 40 days to over one year [14,25,35]. In the case presented, the decision was made to keep the patient in the hospital for the one week between operations. After discussion with the patient, we felt it was best for the patient to remain in a controlled environment where assistance with ADLs and physical therapy could be adequately provided.
Clinical outcomes for DM THA have improved due in part to a more complete understanding of the prosthesis mechanics and evolution in design [36]. Early DM constructs demonstrated elevated risk of IPD, aseptic loosening and metallosis from the additional articular surface the liner creates with the acetabular shell [5,8,10,11]. DeMartino et al. [37] noted early concerns of IPD, reporting rates of 0.7 % and 1.3 % in primary and revision THA, respectively. Neri et al. [8] determined that recent design modifications contribute to the “quasi-disappearance” of IPD. Recently, Batailler et al. [8,31] reported the midterm survivorship of MDM implants was comparable to that of fixed-bearing implants for primary THA. Similarly, Schmidt et al. [7] reported MDM implants significantly decreased the risk of postoperative dislocation without a risk of early aseptic loosening at medium term follow-up following in revision THA when compared to fixed-bearing implants. MDM constructs allow for greater effective femoral head sizes, increasing the head-neck ratio and arc of motion prior to impingement. An increase in jump distance allows for the femoral head to be seated deeper in the acetabulum, conferring additional joint stability [[38], [39], [40]].
Acetabular cup placement in the Lewinnek safe zone has historically been the guide used by surgeons when ensuring correct acetabular version and inclination, sometimes referred to as ante-inclination, during THA. Originally described as 40 ± 10- degrees of inclination and 15 ± 10 degrees anteversion [41], recent studies are providing evidence that these measurements alone do not have a reliable decrease in postoperative dislocation [42,43]. Abdel et al. [42] concluded that while these values may be useful, they do not preclude dislocation as the term “safe zone” would suggest. In this patient, concern that achieving the primary goal of improving hygiene by increasing range of motion would be accompanied by the patient remaining wheelchair bound called into question the optimal position for the acetabular component. Raphael et al. [44] reported an 8.5 % revision rate due to dislocation in their series of fixed-bearing THA for patients with cerebral palsy in which a majority were due to acetabular cup malposition. Sanders et al. [45] reported zero dislocations at midterm follow-up for patients with spastic disorders that received a dual-mobility prothesis for THA. Rather than place the acetabular component outside of Lewinnek's zone to increase range of motion, we opted to place it inside the safe zone to improve stability and utilize a dual-mobility prosthesis to achieve our desired range of motion. Riviere et al. describe a “kinematic alignment in THA” (KA-THR) where the implant is orientated in a way that respects the patients' native kinematic patterns [46,47]. The most successful guide for implantation may be a combination of generalizable principles and patient-specific tools to optimize patient outcomes measures.
It is crucial to account for dynamic changes in spinopelvic alignment during movement in patients with identified spinopelvic pathology [48]. Patients with lumbar stiffness and bony ankylosis of the hip may have an increased posterior pelvic tilt which increases native hip anteversion [49,50]. Increased native anteversion increases the risk of posterior impingement and anterior dislocation [18]. Due to increased posterior pelvic tilt and decreased pelvic incidence, care must be taken during templating and implantation of the acetabular cup to ensure it is not placed into excessive anteversion, further increasing the risk of anterior dislocation. It has been reported that ante-inclination can be predicted to change nearly one degree for every one degree of change in pelvic tilt in patients determined to have a stiff pelvis preoperatively [[51], [52], [53]]. Riviere et al. [46] recommends use of dual mobility prothesis in very high-risk patients that have a stiff lumbo-pelvic complex (LPC). Specifically, very high-risk patients are at the highest risk of edge-loading and prosthetic impingement.
4. Summary
We present a patient with suspected AS that received bilateral MDM THA for spontaneous bony ankylosis of the hips. The improved stability of DM allows for a greater range of acetabular positions in patients who have a highly unpredictable functional outcome at the time of surgery. At short term follow-up, the patient reports a significant improvement in pain, range of motion and activities of daily living. Our preliminary results contribute to the growing list of indications for MDM total hip arthroplasty.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval was not required at Larkin Community Hospital, South Miami, FL for single case reports which do not constitute research under the current guidelines.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Peter A. Falgiano, MD- study concept, data collection, initial manuscript, edits.
Robert J. Rowland, DO- study concept, data collection, initial manuscript, edits.
John J. Heifner, MD- study concept, data collection, initial manuscript, edits,
Arturo Corces, MD- study concept, data collection, initial manuscript, edits.
Guarantor
Peter A. Falgiano, MD.
Robert J. Rowland, DO.
John J. Heifner, MD.
Arturo Corces, MD.
Research registration number
N/A.
Conflict of interest statement
AC receives royalties or licenses from Arthrex and payment for lectures, presentations, speaker's bureaus, manuscript writing or educational events from Exactech. The other authors have no financial interests or personal relationships to disclose.
References
- 1.Thilak J., Panakkal J.J., Kim T.Y., Goodman S.M., Lee S.S., Salvati E.A. Risk factors of heterotopic ossification following total hip arthroplasty in patients with ankylosing spondylitis. J. Arthroplasty. 2015;30(12):2304–2307. doi: 10.1016/j.arth.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Heckmann N., Weitzman D.S., Jaffri H., Berry D.J., Springer B.D., Lieberman J.R. Trends in the use of dual mobility bearings in hip arthroplasty. Bone Joint J. 2020;102-B(7_Supple_B):27–32. doi: 10.1302/0301-620X.102B7.BJJ-2019-1669.R1. [DOI] [PubMed] [Google Scholar]
- 3.Vielpeau C., Lebel B., Ardouin L., Burdin G., Lautridou C. The dual mobility socket concept: experience with 668 cases. Int. Orthop. 2011;35(2):225–230. doi: 10.1007/s00264-010-1156-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donovan R.L., Johnson H., Fernando S., Foxall-Smith M., Whitehouse M.R., Blom A.W., et al. The incidence and temporal trends of dislocation after the use of constrained acetabular components and dual mobility implants in primary total hip replacements: a systematic review and meta-analysis of longitudinal observational studies. J. Arthroplasty. 2022;37(5):993–1001 e8. doi: 10.1016/j.arth.2022.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Heifner J.J., Keller L.M., Fox Y.M., Sakalian P.A., Corces A. The performance of primary dual-mobility total hip arthroplasty in patients aged 55 years and younger: a systematic review. Arthroplast Today. 2023;24 doi: 10.1016/j.artd.2023.101241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foissey C., Batailler C., Rajput V., Premkumar A.B.J., Servien E., Lustig S. No dislocation and low complication rate for a modern dual mobility cup with pre-impacted femoral head in primary hip replacement: a consecutive series of 175 hips at minimum 5-year follow-up. SICOT J. 2023;9:1. doi: 10.1051/sicotj/2022050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt A., Batailler C., Fary C., Servien E., Lustig S. Dual mobility cups in revision total hip arthroplasty: efficient strategy to decrease dislocation risk. J. Arthroplasty. 2020;35(2):500–507. doi: 10.1016/j.arth.2019.08.060. [DOI] [PubMed] [Google Scholar]
- 8.Neri T., Boyer B., Geringer J., Di Iorio A., Caton J.H., PhiIippot R., et al. Intraprosthetic dislocation of dual mobility total hip arthroplasty: still occurring? Int. Orthop. 2019;43(5):1097–1105. doi: 10.1007/s00264-018-4054-0. [DOI] [PubMed] [Google Scholar]
- 9.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020-2040 using the National Inpatient Sample. J. Rheumatol. 2019;46(9):1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 10.Ciolli G., Mesnard G., Deroche E., Gunst S., Batailler C., Servien E., et al. Is cemented dual-mobility cup a reliable option in primary and revision total hip arthroplasty: a systematic review. J. Pers. Med. 2022;13(1) doi: 10.3390/jpm13010081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Darrith B., Courtney P.M., Della Valle C.J. Outcomes of dual mobility components in total hip arthroplasty: a systematic review of the literature. Bone Joint J. 2018;100-B(1) doi: 10.1302/0301-620X.100B1.BJJ-2017-0462.R1. (11-9) [DOI] [PubMed] [Google Scholar]
- 12.Kunutsor S.K., Barrett M.C., Beswick A.D., Judge A., Blom A.W., Wylde V., et al. Risk factors for dislocation after primary total hip replacement: a systematic review and meta-analysis of 125 studies involving approximately five million hip replacements. Lancet Rheumatol. 2019;1(2) doi: 10.1016/S2665-9913(19)30045-1. (e111-e21) [DOI] [PubMed] [Google Scholar]
- 13.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhan S., Eachempati K.K., Malhotra R. Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J. Arthroplasty. 2008;23(6):859–866. doi: 10.1016/j.arth.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 15.Sundaram N.A., Murphy J.C. Heterotopic bone formation following total hip arthroplasty in ankylosing spondylitis. Clin. Orthop. Relat. Res. 1986;207:223–226. [PubMed] [Google Scholar]
- 16.Putnis S.E., Wartemberg G.K., Khan W.S., Agarwal S. A literature review of total hip arthroplasty in patients with ankylosing spondylitis: perioperative considerations and outcome. Open Orthop. J. 2015;9:483–488. doi: 10.2174/1874325001509010483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brooker A.F., Bowerman J.W., Robinson R.A., Riley L.H., Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J. Bone Joint Surg. Am. 1973;55(8):1629–1632. [PubMed] [Google Scholar]
- 18.Oommen A.T., Hariharan T.D., Chandy V.J., Poonnoose P.M., AS A., Kuruvilla R.S., et al. Total hip arthroplasty in fused hips with spine stiffness in ankylosing spondylitis. World J. Orthop. 2021;12(12):970–982. doi: 10.5312/wjo.v12.i12.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hou L.Q., Jiang G.X., Chen Y.F., Yang X.M., Meng L., Xue M., et al. The comparative safety of TNF inhibitors in ankylosing spondylitis-a meta-analysis update of 14 randomized controlled trials. Clin Rev Allergy Immunol. 2018;54(2):234–243. doi: 10.1007/s12016-017-8623-6. [DOI] [PubMed] [Google Scholar]
- 20.Bangjian H., Peijian T., Ju L. Bilateral synchronous total hip arthroplasty for ankylosed hips. Int. Orthop. 2012;36(4):697–701. doi: 10.1007/s00264-011-1313-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang W., Huang G., Huang T., Wu R. Bilaterally primary cementless total hip arthroplasty in patients with ankylosing spondylitis. BMC Musculoskelet. Disord. 2014;15:344. doi: 10.1186/1471-2474-15-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feng D.X., Zhang K., Zhang Y.M., Nian Y.W., Zhang J., Kang X.M., et al. Bilaterally primary cementless total hip arthroplasty for severe hip ankylosis with ankylosing spondylitis. Orthop. Surg. 2016;8(3):352–359. doi: 10.1111/os.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin D., Charalambous A., Hanna S.A. Bilateral total hip arthroplasty in ankylosing spondylitis: a systematic review. EFORT Open Rev. 2019;4(7):476–481. doi: 10.1302/2058-5241.4.180047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacob M.K., Reddy P.K., Kuruvilla R.S., John C.V., Poonnoose P.M., Oommen A.T. Functional and clinical outcome with modified lateral approach total hip arthroplasty in stiff hips with ankylosing spondylitis. World J. Orthop. 2022;13(8):714–724. doi: 10.5312/wjo.v13.i8.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kumar A., Nagai H., Oakley J., Luu B., Hussain M.M., Gaba R. Short to long term outcomes of 154 cemented total hip arthroplasties in ankylosing spondylitis. J. Clin. Orthop. Trauma. 2021;14:34–39. doi: 10.1016/j.jcot.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim Y.H., Oh S.H., Kim J.S., Lee S.H. Total hip arthroplasty for the treatment of osseous ankylosed hips. Clin. Orthop. Relat. Res. 2003;414:136–148. doi: 10.1097/01.blo.0000081935.75404.7f. [DOI] [PubMed] [Google Scholar]
- 27.Blizzard D.J., Penrose C.T., Sheets C.Z., Seyler T.M., Bolognesi M.P., Brown C.R. Ankylosing spondylitis increases perioperative and postoperative complications after total hip arthroplasty. J. Arthroplasty. 2017;32(8):2474–2479. doi: 10.1016/j.arth.2017.03.041. [DOI] [PubMed] [Google Scholar]
- 28.Chung B.C., Stefl M., Kang H.P., Hah R.J., Wang J.C., Dorr L.D., et al. Increased dislocation rates following total hip arthroplasty in patients with ankylosing spondylitis. Hip Int. 2023;33(6):1026–1034. doi: 10.1177/11207000221126968. [DOI] [PubMed] [Google Scholar]
- 29.Welch R.B., Charnley J. Low-friction arthroplasty of the hip in rheumatoid arthritis and ankylosing spondylitis. Clin. Orthop. Relat. Res. 1970;72:22–32. [PubMed] [Google Scholar]
- 30.(AAOS) AAoOS AmericanJointReplacementRegistry(AJRR).2021. 2021. https://www.aaos.org/registries/publications/ajrr-annual-report/ Available from:
- 31.Batailler C., Fary C., Verdier R., Aslanian T., Caton J., Lustig S. The evolution of outcomes and indications for the dual-mobility cup: a systematic review. Int. Orthop. 2017;41(3):645–659. doi: 10.1007/s00264-016-3377-y. [DOI] [PubMed] [Google Scholar]
- 32.Blakeney W.G., Epinette J.A., Vendittoli P.A. Dual mobility total hip arthroplasty: should everyone get one? EFORT Open Rev. 2019;4(9):541–547. doi: 10.1302/2058-5241.4.180045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Assi C., Barakat H., Mansour J., Samaha C., Yammine K. Primary total hip arthroplasty: mid-term outcomes of dual-mobility cups in patients at high risk of dislocation. Hip Int. 2021;31(2):174–180. doi: 10.1177/1120700019889031. [DOI] [PubMed] [Google Scholar]
- 34.Han L., Quan R., Pei Z., Cao G., Hu Y., Liu J. Mid-term results of bilateral synchronous total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J. Orthop. Surg. Res. 2021;16(1):104. doi: 10.1186/s13018-021-02258-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mou P., Zeng W.N., Chen Y., Zhou Z. Synchronous or sequential cementless bilateral total hip arthroplasty for osseous ankylosed hips with ankylosing spondylitis. BMC Musculoskelet. Disord. 2021;22(1):302. doi: 10.1186/s12891-021-04142-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McArthur B.A., Nam D., Cross M.B., Westrich G.H., Sculco T.P. Dual-mobility acetabular components in total hip arthroplasty. Am. J. Orthop. (Belle Mead N.J.) 2013;42(10):473–478. [PubMed] [Google Scholar]
- 37.De Martino I., D’Apolito R., Soranoglou V.G., Poultsides L.A., Sculco P.K., Sculco T.P. Dislocation following total hip arthroplasty using dual mobility acetabular components: a systematic review. Bone Joint J. 2017;99-B(ASuppl1):18–24. doi: 10.1302/0301-620X.99B1.BJJ-2016-0398.R1. [DOI] [PubMed] [Google Scholar]
- 38.Chalmers B.P., Perry K.I., Hanssen A.D., Pagnano M.W., Abdel M.P. Conversion of hip hemiarthroplasty to total hip arthroplasty utilizing a dual-mobility construct compared with large femoral heads. J. Arthroplasty. 2017;32(10):3071–3075. doi: 10.1016/j.arth.2017.04.061. [DOI] [PubMed] [Google Scholar]
- 39.Abdel M.P. Dual-mobility constructs in revision total hip arthroplasties. J. Arthroplasty. 2018;33(5):1328–1330. doi: 10.1016/j.arth.2018.01.030. [DOI] [PubMed] [Google Scholar]
- 40.Hartzler M.A., Abdel M.P., Sculco P.K., Taunton M.J., Pagnano M.W., Hanssen A.D. Otto aufranc award: dual-mobility constructs in revision THA reduced dislocation, rerevision, and reoperation compared with large femoral heads. Clin. Orthop. Relat. Res. 2018;476(2):293–301. doi: 10.1007/s11999.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint Surg. Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 42.Abdel M.P., von Roth P., Jennings M.T., Hanssen A.D., Pagnano M.W. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin. Orthop. Relat. Res. 2016;474(2):386–391. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Riviere C., Harman C., Logishetty K., Van Der Straeten C. In: Personalized Hip and Knee Joint Replacement. Cham (CH) Riviere C., Vendittoli P.A., editors. 2020. Hip replacement: its development and future; pp. 23–32. [Google Scholar]
- 44.Raphael B.S., Dines J.S., Akerman M., Root L. Long-term followup of total hip arthroplasty in patients with cerebral palsy. Clin. Orthop. Relat. Res. 2010;468(7):1845–1854. doi: 10.1007/s11999-009-1167-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sanders R.J., Swierstra B.A., Goosen J.H. The use of a dual-mobility concept in total hip arthroplasty patients with spastic disorders: no dislocations in a series of ten cases at midterm follow-up. Arch. Orthop. Trauma Surg. 2013;133(7):1011–1016. doi: 10.1007/s00402-013-1759-9. [DOI] [PubMed] [Google Scholar]
- 46.Riviere C., Harman C., Boughton O., Cobb J. In: Personalized Hip and Knee Joint Replacement. Cham (CH) Riviere C., Vendittoli P.A., editors. 2020. Kinematic alignment technique for total hip arthroplasty; pp. 113–132. [Google Scholar]
- 47.Legaye J., Duval-Beaupere G., Barrau A., Boulay C., Hecquet J., Montigny J.P., et al. Relationship between sacral pelvic incidence and acetabular orientation. Hip Int. 2011;21(1):87–97. doi: 10.5301/hip.2011.6283. [DOI] [PubMed] [Google Scholar]
- 48.Lum Z.C., Giordani M., Meehan J.P. Total hip instability and the spinopelvic link. Curr. Rev. Musculoskelet. Med. 2020;13(4):425–434. doi: 10.1007/s12178-020-09648-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bukowski B.R., Clark N.J., Taunton M.J., Freedman B.A., Berry D.J., Abdel M.P. Primary total hip arthroplasty in patients with ankylosing spondylitis. J. Arthroplasty. 2021;36(7S) doi: 10.1016/j.arth.2021.01.054. (S282-S9) [DOI] [PubMed] [Google Scholar]
- 50.Sariali E., Lazennec J.Y., Khiami F., Gorin M., Catonne Y. Modification of pelvic orientation after total hip replacement in primary osteoarthritis. Hip Int. 2009;19(3):257–263. doi: 10.1177/112070000901900312. [DOI] [PubMed] [Google Scholar]
- 51.Lazennec J.Y., Charlot N., Gorin M., Roger B., Arafati N., Bissery A., et al. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg. Radiol. Anat. 2004;26(2):136–144. doi: 10.1007/s00276-003-0195-x. [DOI] [PubMed] [Google Scholar]
- 52.Shon W.Y., Gupta S., Biswal S., Hur C.Y., Jajodia N., Hong S.J., et al. Validation of a simple radiographic method to determine variations in pelvic and acetabular cup sagittal plane alignment after total hip arthroplasty. Skeletal Radiol. 2008;37(12):1119–1127. doi: 10.1007/s00256-008-0550-4. [DOI] [PubMed] [Google Scholar]
- 53.Kanawade V., Dorr L.D., Wan Z. Predictability of acetabular component angular change with postural shift from standing to sitting position. J. Bone Joint Surg. Am. 2014;96(12):978–986. doi: 10.2106/JBJS.M.00765. [DOI] [PubMed] [Google Scholar]