Abstract
Objectives/Hypothesis
Socioeconomics and demographics have been shown to be determinates of healthcare in specialty clinics, in which thorough research is lacking in the setting of the United States clinical sphere. We set out to determine the impact of socioeconomic and demographic factors on patient preparedness in an otolaryngologic clinic as to highlight the need for awareness in this aspect of disparate and delayed clinical care.
Study Design
Retrospective chart review.
Methods
A chart review was conducted of 482 patients who visited our otolaryngology clinic between June 1, 2020 and June 1, 2023. Demographic data including marital status, gender, age, zip code, and race was collected.
Results
Our study found several interesting points of significance. Marital status was a significant determinant of whether patients had missing labs and/or imaging (p = .001). Age was a significant determinant of patients having their imaging (p < .0001). Patients were more likely to have all their labs and imaging at a follow‐up appointment compared to an initial appointment (p < .0001). Finally, a patient's zip code was found to be a significant determinant of whether a patient no‐showed an appointment or arrived with all their needed imaging and labs (p = .004).
Conclusions
Having the needed labs and imaging for a clinical visit is vital to providing timely and well‐informed care for all patients. This study highlighted several potential determinates of missing labs and imaging. Elderly patients were less likely to have imaging, which may be attributed to transportation issues and a weaker support system. Individuals who were married were more likely to have their imaging. Married individuals may have a stronger support system, where their spouses can provide transportation and reminders for appointments. Finally, the significance of zip code highlights the role transportation distance and living in an underserved area may have on patients being able to go to their appointments or obtain their needed imaging.
Level of Evidence
4
Keywords: determinates, follow‐up, imaging, missing labs
With prior studies noting the notable effects of socioeconomic status and demographic factors on care in specialty clinics, we set out to determine the accessory effect of these factors on patient appointment preparedness in an otolaryngologic clinic. This study specifically examines these factors in regard to patient arrival with appropriate labs and imaging, as these are crucial in lead time and providing appropriate care for the patient. Our study identified follow‐up versus initial appointment, zip code, age, sex, and marital status to be significant factors influencing patient preparedness.

1. INTRODUCTION
Every clinician has had to deal with patients who either no‐show or who arrive to clinic appointments lacking requested imaging, labs, or other work‐up. These missed opportunities for care are frustrating for both clinicians and patients and represent an inefficiency of our healthcare system. If the determinants that lead patients to no‐show or arrive at appointments missing aspects of their work‐up could be addressed, delays can be prevented, and patients can receive more timely and comprehensive care. Socioeconomic status within the United States has become a notable barrier for healthcare access and compliance, and it seems likely that it plays a driving role on no‐shows and in appointments with missing components of work‐up. Specific investigations into these factors, however, have been substantially limited in current literature, especially within the field of Otolaryngology. Prior studies have been completed outside of the United States and in universal healthcare systems. One study from Canada demonstrated associations between noncompliance and age, sex, and appointment day of the week. 1 These results, however, remain functionally very limited with an unknown application to our healthcare system.
Similar studies in the United States have been completed in varying fields of outpatient medicine, also indicating potential associations between estimated household income and distance from their home to the clinic. 2 Studies specifically investigating impact of race and ethnicity have been completed which show factors including transportation challenges, difficulty taking time off work, lack of understanding of scheduling systems, and even perceived disrespect of their beliefs have resulted in decreased rates of appointment attendance. 3 The type of appointment and clinical context have also been shown as notable factors, as patients are less likely to miss diagnostic appointments or follow‐ups after indeterminate and inconclusive findings. Primary language was also impactful, with Spanish‐speaking patients actually being less likely to miss an appointment. 4 The extreme variation of these study results, in concordance with the multiple specialties of their scope, demonstrate unknown significance and generalizability within otolaryngology. It is, however, evident that there are disparities leading to missed appointments associated with socioeconomic and demographic factors. These factors are apparent across medicine, and our goal was to determine whether these factors have an impact in the field of otolaryngology, particularly in an important, but unaddressed area of healthcare delivery in otolaryngology: patients having all appropriate material for their clinical visits.
Social determinants of health themselves have been repeatedly shown to effect patient outcomes across all fields. Within otolaryngology specifically, it has been associated with increased rates and/or complications including olfactory dysfunction, vestibular schwannomas, thyroid cancer, laryngotracheal stenosis, and need for tracheostomy. 5 , 6 , 7 , 8 In addition to the increased stress on patients, missed appointments also add unnecessary stress to the healthcare system. Not only do missed appointments cost facilities an average of $725.42 per day for an average clinic schedule of 24 patients per day, but increasing disease severity and complication rate from this noncompliance leads to further appointments and preventable events. 9 This increased stress on clinics results in increased lead time to appointment, which has been reported in prior studies to increase missed appointment rates even further. This leads to a detrimental “loop” of redundancy between the two wherein missed appointments cause increased number of appointments, which causes further lead time which, in turn, further increases missed appointments. 10
While these studies seek to explain causes of missed appointments, this is only one category leading to these results. In addition to the multitude of variables mentioned above, arriving to the appointment without necessary components such as required labs and imaging is also a major factor interfering with timely patient care. This ultimately requires additional appointments with the proper results to achieve the appointment goal. This delays treatment and operative timelines, further adding stress and burden to the healthcare system, clinics, physicians, and patients in a similar fashion as missed appointments. Therefore, our study aimed to elucidate the knowledge gaps between these two factors by investigating which socioeconomic and demographic factors impact patient arrival to their appointment without these needed labs and imaging results.
Our study set out to examine demographic factors that have been examined in the literature such as race, gender, and insurance status, as the disparities associated with these factors have been well‐demonstrated in the literature and found to be profound. We included patient zip codes in our study to better pinpoint regional, geographic disparities. We also included both marital status and age in our study. These factors have not been well studied in other studies examining missed appointments in otolaryngology. However, married patients have been shown to have better treatment adherence and outcomes in head and neck cancer, so we aimed to see if these positive associations play a similar role in appointment attendance and having appropriate diagnostic studies and imaging. 11 , 12 , 13 Age has been shown to have additional barriers to treatment including transportation, which can very well play a significant role in older patients having appropriate diagnostic studies and imaging prior to their appointments. 14
The implications of socioeconomic status and demographic factors are wide‐ranging in health disparities, and there is a clear gap in the literature regarding their impact in patients completing necessary diagnostic studies and imaging prior to their otolaryngologic clinical appointments. Our study hypothesized that these factors play a role in this issue and aimed to determine the extent of the impact of these factors. Having a greater understanding of the impact of these factors and their effect is vital to guiding interventions and policies to address these disparities.
2. METHODS
With approval from the Texas Tech University Health Sciences Center Quality Improvement Review Board (QIRB), a retrospective chart review was conducted of 482 patients who visited our Otolaryngology clinic between June 1, 2020 and June 1, 2023. Demographic data including marital status, gender, age, zip code, and race was collected. Their clinic notes were then examined to see if the patient no‐showed their appointment, if they attended their appointment but without the requested imaging, if they attended their appointment but without other requested diagnostic testing reports and/or laboratory values, or if they attended their appointment with all requested components. Inclusion criteria included patients who were coming to either their primary or secondary otolaryngology appointment and required imaging and/or labs prior to their appointments. Patients who did not require imaging or labs for their appointments were excluded. Patients who already had two or more appointments previously were excluded. Our clinical practice is composed of five attending physicians, and we randomly selected approximately 100 patients from each attending within our date range to include in the study. Patient charts that did not contain all of the studied parameters were excluded.
With regard to sample size, a power analysis was performed, and for an α of .05 and a power (1 − β) of .80, to detect a minimum detectable effect of 2.4 years with regard to the variable of age, a minimum sample size of 474 would have been necessary, but the sample size was increased to 482 for robustness. Statistics were performed using GraphPad Prism 9.4.1 (Dotmatics, Boston, MA, USA). The D'Agostino and Pearson tests indicated that the data were not normally distributed. Therefore, appropriate nonparametric tests were selected. For univariate analyses, the Mann–Whitney test was performed. Many of the studied variables were assumed to be potentially confounding, and thus, for multivariate analysis to analyze how the variables related to each other, the Kruskal–Wallis test was performed. A chi‐square test was used to analyze categorical variables.
3. RESULTS
Table 1 displays the basic demographic information of the 482 patients included in the study. The cohort was 53.1% female (n = 256) and 46.9% male (n = 226). The average age was 51.8 years old. The majority of patients were White (89.8%, n = 433), followed by Black (4.1%, n = 20), Asian (1.2%, n = 6), and Native American/Alaskan Native (0.8%, n = 4). 3.9% (n = 19) of the patients did not specify their race. In terms of marital status, 45.4% were single (n = 219), 45.4% were married (n = 219), and 9.1% did not specify (n = 44). 58.3% of appointments were subsequent visits (n = 281), while 41.7% were initial appointments (n = 201). General otolaryngology comprised of 57.3% of the appointment indications (n = 276), followed by head and neck oncology (20.1%, n = 97), facial plastics and reconstructive (3.9%, n = 19), laryngology (3.9%, n = 19), otology/neurotology/skull base surgery (3.9%, n = 19), pediatric otolaryngology (3.9%, n = 19), rhinology (2.5%, n = 12), and sleep medicine (0.6%, n = 3).
TABLE 1.
Demographics and overview of patient characteristics.
| All | No missing items | No show | Missing imaging | Missing labs | |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 53.1% (256) | 54.8% (190) | 49.5% (47) | 41.7% (10) | 56.3% (9) |
| Male | 46.9% (226) | 45.2% (157) | 50.5% (48) | 58.3% (14) | 43.8% (7) |
| Age | 51.8 (2–93, STD 21.36) | 51.1 (2–93, STD 21.0) | 49.2 (2–90, STD 21.91) | 72.5 (55–93, STD 9.02) | 52.3 (14–86, STD 24.3) |
| Race | |||||
| White | 89.8% (433) | 91.6% (318) | 81.1% (77) | 91.7% (22) | 100.0% (16) |
| Black | 4.1% (20) | 3.5% (12) | 8.4% (8) | — | — |
| Asian | 1.2% (6) | 1.4% (5) | 1.1% (1) | — | — |
| Native American | 0.8% (4) | 0.9% (3) | 1.1% (1) | — | — |
| No Reply | 3.9% (19) | 2.6% (9) | 8.4% (8) | 8.3% (2) | — |
| Marital status | |||||
| Single | 45.4% (219) | 43.2% (150) | 49.5% (47) | 45.8% (11) | 68.8% (11) |
| Married | 45.4% (219) | 50.1% (174) | 32.6% (31) | 37.5% (9) | 31.3% (5) |
| Unknown | 9.1% (44) | 6.6% (23) | 17.9% (17) | 16.7% (4) | — |
| First or subsequent appointment | |||||
| First | 41.7% (201) | 46.0% (160) | 14.7% (14) | 58.3% (14) | 43.8% (7) |
| Subsequent | 58.3% (281) | 56.2% (187) | 85.3% (81) | 41.7% (10) | 56.3% (9) |
| Subspeciality reason for appointment | |||||
| General facial plastics and reconstructive | 57.3% (276) | 54.5% (189) | 70.5% (67) | 45.8% (11) | 56.3% (9) |
| Head and neck oncology | 3.9% (19) | 4.3% (15) | 3.2% (3) | — | 6.3% (1) |
| Laryngology | 20.1% (97) | 22.2% (77) | 5.3% (5) | 37.5% (9) | 37.5% (6) |
| Otology, neurotology, and skull | 3.9% (19) | 4.3% (15) | 3.2% (3) | 4.2% (1) | — |
| Base | 3.9% (19) | 4.3% (15) | 2.1% (2) | 8.3% (2) | — |
| Pediatric | 3.9% (19) | 4.3% (15) | 4.2% (4) | — | — |
| Rhinology | 2.5% (12) | 2.6% (9) | 3.2% (3) | — | — |
| Sleep medicine | 0.6% (3) | 0.9% (3) | — | — | — |
| Most common zip code (mode) | 79424 | 79424 | 79404 | 79416 | 79424 |
Note: The table provides a demographic overview of our study population (n = 482). In addition, it stratifies our patient population based on their specific type of appointment (subspeciality vs. general otolaryngology) and whether the appointment is their first or subsequent appointment. The table highlights the relatively even distribution we have among gender and marital status.
Several statistically significant points were found in the study. We found significance in four key areas—marital status, age, whether a patient had a primary or follow‐up appointment, and patient zip code. We did not find significance in missed imaging, labs, or appointments based on gender, race, or subspeciality. A chi‐square analysis showed that marital status was a significant determinant of whether patients had missing labs and/or imaging (p = .001). Age also significantly correlated with patients having their imaging with unmarried patients being more likely to come to appointments without required imaging (p < .0001). This is highlighted in Figure 1. Furthermore, the chi‐square test showed that patients were more likely to have all their labs and imaging at a follow‐up appointment compared to the initial appointment (p < .0001). This is demonstrated in Figure 2. Finally, utilizing Kruskal–Wallis testing, patient zip code strongly correlated with whether a patient no‐showed or arrived with all requested imaging and labs (p = .0048).
FIGURE 1.
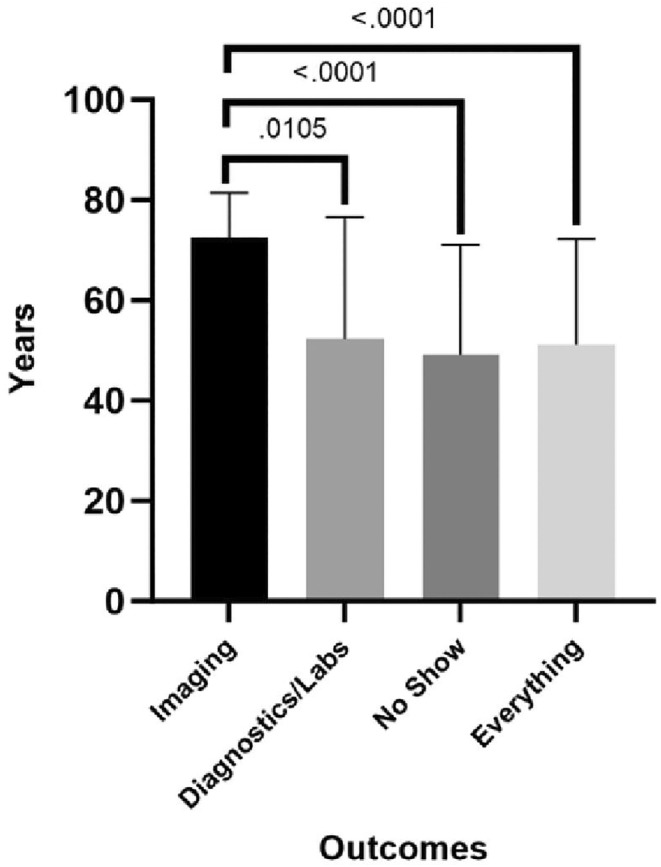
Correlation of age of patients presenting to an appointment without imaging. The figure highlights our results that showed that older patients were more likely to present to their appointments without their requested imaging. The figure also shows that no significance was found among patient age and whether a patient misses their appointment or has their required labs and diagnostic tests for their appointment. Imaging, patients presenting without imaging to appointment; Diagnostics/Labs, patients presenting without other diagnostic tests or labs to appointment; No Show, patients who missed their appointment; Everything, patients presenting with all required imaging, diagnostic testing, and/or labs to appointment.
FIGURE 2.
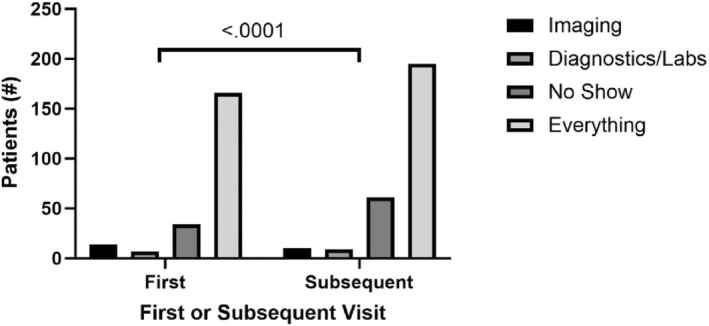
Comparison of patients presenting to primary or subsequent appointment with all requested workup. The figure highlights our results that showed that patients at subsequent appointments were more likely to present to their appointments with their requested imaging and diagnostic tests compared to patients at their primary appointment. First, a patient's primary or initial appointment; Subsequent, a patient's second appointment; Imaging, patients presenting without imaging to appointment; Diagnostics/Labs, patients presenting without other diagnostic tests or labs to appointment; No Show, patients who missed their appointment; Everything, patients presenting with all required imaging, diagnostic testing, and/or labs to appointment.
4. DISCUSSION
This study set out to evaluate the socioeconomic and demographic factors that lead to missing appointments in otolaryngology in west Texas. This region serves as a microcosm of disparities in the United States, with sizeable rural, migrant, and underserved minority populations. Our findings build on existing literature and also demonstrate novel factors at play in missing appointments or coming to an otolaryngology appointment with missing labs or imaging.
Our study found a patient's marital status to be a significant factor in whether patients had missing labs or imaging. Patients who are married have, on average, a stronger support system, and their significant other can assist in coordinating and traveling to appointments, labs, and imaging. Several studies have identified improved survival rates in married patients with head and neck cancer. 11 , 12 , 13 Moreover, married patients have been shown to have better adherence to treatment and to seek definitive treatment. 11 , 13 The social support that a spouse provides plays a significant role in going through the difficult process of diagnosing and treating head and neck cancer. 11 , 12 , 13 The social support system that a spouse provides in these instances are likely at play in our study. Patients who listed their marital status as single were less likely to have their appropriate labs and imaging for appointment. Again, navigating a more serious otolaryngologic problem that requires extensive imaging and labs would be difficult to navigate without familial support that a spouse often provides. It would be important to identify a patient's support system regardless of marital status and to refer them to support groups and appropriate resources, such as social workers, when faced with pathology that would require extensive workup and treatment.
Our study also found age to be a significant determinant for patients to have their imaging completed before their appointment. The average age of patients who had all their needed labs and imaging was 51, while the average age of those who were missing imaging was 73. Elderly patients disproportionally face greater barriers in transportation and pursuing care. 14 Geriatric patients have barriers to seeking care that have been demonstrated in other areas of medicine. A systematic review in geriatric patients seeking mental health identified secondary barriers to seeking mental health care such as cost, transportation, and reliance on caregivers. 15 These barriers were likely faced by many of our geriatric patients and played a role in their ability to get needed imaging for the visit. Meanwhile, children may have parents or other caregivers who are motivated to ensure that pediatric patients obtain all of their requested work‐up and attend all of their appointments. To our knowledge, there is no existing literature that examines the connection between age and having requisite imaging at otolaryngology visits.
Patients were more likely to have all their required imaging and labs at follow‐up appointments compared to initial appointments. There are several factors to consider for this result. Patients who had follow‐up appointments that required imaging or labs were inherently more likely to have issues that required more extensive work‐up. Providers had the ability to counsel patients on the reasonings and necessity of the required labs and imaging and motivate the patient through discussion and shared decision‐making. In addition, it is of high likelihood that follow‐up patients received such workups via on‐site facilities versus external sources, thus eliminating the need to have the testing results faxed or copied by the referring facility. Patients who need required imaging and/or labs prior to an initial visit should receive communication from the clinic prior to the visit outlining what requisite imaging and labs are required and the reasoning for them.
Finally, patient zip code was found to significantly correlate with whether a patient missed an appointment or arrived with all their requested imaging and labs. The majority of our patients were from the zip code 79424, which is an area in Lubbock that is among the wealthiest in the region with a median household income of $87,476 (USD). 16 Nearly half of the residents in this zip code have at least some college education, and less than 10% are uninsured or below the poverty line. 15 Patients from this zip code were the most likely to show up for their appointments and have all required imaging. Patients from the zip code 79404 were the most likely to no‐show an appointment, and patients from the zip code 79416 were most likely to not have required imaging at their appointments. Both of these zip codes are areas in Lubbock with significant underserved populations, with a higher proportion of residents at or below the poverty line (24% and 20.3%, respectively), a lower median household income (40,110 and 61,627, respectively), and a higher uninsured population (18.9% and 10.8%, respectively). 17 , 18 Several studies have factors such as race, socioeconomic status, insurance status, and rurality playing a large role in disparities across the disciplines of otolaryngology. 19 These well‐established disparities can likely explain our findings that patients from certain zip codes were more likely to miss their appointment and not have their required imaging.
This study adds novel, important findings to the literature, particularly about marital status and age. These findings should influence and further guide interventions to prevent missed appointments and imaging in these populations, particularly those with time‐sensitive diagnoses such as oropharyngeal cancer. Patients who are at risk for missing appointments or necessary labs and imaging should be provided with resources to combat these disparities. This should include, but is not limited to, transportation assistance, more frequent reminders of appointments and necessary labs and imaging, and financial assistance for uninsured populations.
We recommend that all patients are provided with comprehensive and frequent reminders of their upcoming appointments along with instructions on receiving the needed imaging and diagnostic labs prior to their appointments. In addition, patients should be given the opportunity to express whether they may have difficulties attaining the required labs or imaging prior to their appointment. This will allow for appropriate interventions and resource allocations. Unmarried patients, particularly those facing more debilitating or permanent conditions such as oropharyngeal cancer or deafness, should be with provided access to support groups and have a social worker involved in their multidisciplinary care. Building a solid support system for these patients is critical. Patients from elderly and/or socioeconomically disadvantaged populations should be questioned on any access to care issues they may have in both receiving pertinent imaging and labs prior to their appointments and attending their appointments outright. Interventions such as transportation assistance may be necessary among many patients from these populations. It is, however, important to note that each patient may face different barriers, and a more personalized approach guided by a multidisciplinary care team may provide the most effective interventions. Lastly, a future direction may be to develop a predictive model of the likelihood of a patient missing or not completing a requested work‐up and then testing specific interventions to improve care for these at‐risk patients.
5. LIMITATIONS
The main limitation of this study is sample size. While our study encompassed over 400 patients, we had a smaller sample size for patients who had missed labs and imaging. Another important limitation to point out is that these patients are from an area of the country that has a sizable rural, minority, and migrant populations. West Texas, and subsequently our academic practice, comprises a large geographic area. We serve many rural counties and have a sizeable rural patient base; our region also has industries, such as energy and agriculture, that draw a significant migrant population. In addition, we serve a sizeable urban and suburban patient base, as Lubbock is home to over 300,000 people. There are many areas across the country that serve populations similar to ours, but populations such as dense urban communities may differ significantly from our own. Other areas with different demographic distributions may have different results. It is important to note this limitation, as issues pertaining to access to care, such as transportation barriers, may be mitigated in large cities with robust public transportation.
6. CONCLUSION
This study points out novel, important findings in disparities that lead to missed appointments and accompanying imaging in otolaryngology. The objective of this study was to determine if socioeconomic and demographic determinants play in role, as demonstrated in other facets of healthcare, in patients missing imaging and other diagnostic labs for their otolaryngologic appointments. It also adds to existing literature that highlights the role socioeconomic status plays in missing appointments. Our data further highlights the role these determinants have in health disparities in otolaryngology and the need for interventions to address them. Clinicians should provide additional support to patients who are at greater risk of having missed imaging and labs, particularly when this can delay intervention.
FUNDING INFORMATION
This research received no specific grant or funding from any funding agency in the public, commercial, or not‐for‐profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Zeitouni J, Millsap J, Jang W, et al. Demographic and socioeconomic determinants of missing labs and imaging for otolaryngologic clinical visits. Laryngoscope Investigative Otolaryngology. 2024;9(5):e70013. doi: 10.1002/lio2.70013
REFERENCES
- 1. Zirkle MS, McNelles LR. Nonattendance at a hospital‐based otolaryngology clinic: a preliminary analysis within a universal healthcare system. Ear Nose Throat J. 2011;90(8):E32‐E34. [PubMed] [Google Scholar]
- 2. Chen AM. Socioeconomic and demographic factors predictive of missed appointments in outpatient radiation oncology: an evaluation of access. Front Health Serv. 2023;3:1288329. doi: 10.3389/frhs.2023.1288329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst. 2002;94(5):334‐357. doi: 10.1093/jnci/94.5.334 [DOI] [PubMed] [Google Scholar]
- 4. Sotudian S, Afran A, LeBedis CA, Rives AF, Paschalidis IC, Fishman MDC. Social determinants of health and the prediction of missed breast imaging appointments. BMC Health Serv Res. 2022;22(1):1454. doi: 10.1186/s12913-022-08784-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stein E, Chern A, Chen H, et al. Association between social determinants of health and olfactory dysfunction in older adults: a population‐based analysis. Int Forum Allergy Rhinol. 2023;13(5):910‐923. doi: 10.1002/alr.23088 [DOI] [PubMed] [Google Scholar]
- 6. Ellsperman SE, Bellile E, Fryatt R, et al. The impact of social determinants of health on vestibular schwannoma management: a single institution review. Otol Neurotol. 2023;44(5):507‐512. doi: 10.1097/MAO.0000000000003883 [DOI] [PubMed] [Google Scholar]
- 7. Gruszczynski NR, Low CM, Choby G, Meister KD, Smith BH, Balakrishnan K. Effects of social determinants of health care on pediatric thyroid cancer outcomes in the United States. Otolaryngol Head Neck Surg. 2022;166(6):1045‐1054. doi: 10.1177/01945998211032901 [DOI] [PubMed] [Google Scholar]
- 8. Dang S, Shinn JR, Campbell BR, Garrett G, Wootten C, Gelbard A. The impact of social determinants of health on laryngotracheal stenosis development and outcomes. Laryngoscope. 2020;130(4):1000‐1006. doi: 10.1002/lary.28208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berg BP, Murr M, Chermak D, et al. Estimating the cost of no‐shows and evaluating the effects of mitigation strategies. Med Decis Making. 2013;33(8):976‐985. doi: 10.1177/0272989X13478194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Drewek R, Mirea L, Adelson PD. Lead time to appointment and no‐show rates for new and follow‐up patients in an ambulatory clinic. Health Care Manag. 2017;36(1):4‐9. doi: 10.1097/HCM.0000000000000148 [DOI] [PubMed] [Google Scholar]
- 11. Inverso G, Mahal BA, Aizer AA, Donoff RB, Chau NG, Haddad RI. Marital status and head and neck cancer outcomes. Cancer. 2015;121(8):1273‐1278. doi: 10.1002/cncr.29171 [DOI] [PubMed] [Google Scholar]
- 12. Li Y, You D, Hu C. Impact of age, race, and gender on the association between marital status and treatment outcomes in Oral tongue squamous cell carcinomas. Ear Nose Throat J. 2023. doi: 10.1177/01455613231191010 [DOI] [PubMed] [Google Scholar]
- 13. Xu C, Chen YP, Liu X, et al. Socioeconomic factors and survival in patients with non‐metastatic head and neck squamous cell carcinoma. Cancer Sci. 2017;108(6):1253‐1262. doi: 10.1111/cas.13250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wolfe MK, McDonald NC, Holmes GM. Transportation barriers to health care in the United States: findings from the National Health Interview Survey, 1997–2017. Am J Public Health. 2020;110(6):815‐822. doi: 10.2105/AJPH.2020.305579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lavingia R, Jones K, Asghar‐Ali AA. A systematic review of barriers faced by older adults in seeking and accessing mental health care. J Psychiatr Pract. 2020;26(5):367‐382. doi: 10.1097/PRA.0000000000000491 [DOI] [PubMed] [Google Scholar]
- 16. SimpleMaps . 79424. October 2023. Accessed May 6, 2024. https://simplemaps.com/us-zips/79424/
- 17. SimpleMaps . 79404. October 2023. Accessed May 6, 2024. https://simplemaps.com/us-zips/79404/
- 18. SimpleMaps . 79416. October 2023. Accessed May 6, 2024. https://simplemaps.com/us-zips/79416/
- 19. Batool S, Burks CA, Bergmark RW. Healthcare disparities in otolaryngology. Curr Otorhinolaryngol Rep. 2023;11(2):95‐108. doi: 10.1007/s40136-023-00459-0 [DOI] [PMC free article] [PubMed] [Google Scholar]


