Abstract
Background
Transcatheter arterial chemoembolization (TACE) combined with targeted therapy and immunotherapy can significantly improve the prognosis of patients with hepatocellular carcinoma (HCC). T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains (TIGIT) is a novel immunosuppressive molecule. This study aimed to analyze the clinical correlation between TIGIT expression on T cells and patients with HCC.
Methods
Clinical data from 140 patients with HCC were retrospectively collected, and TIGIT expression on T cells was examined in each patient. Patients were subsequently divided into high- and low-expression groups, and their prognosis was analyzed.
Results
Patients with a high TIGIT expression on their T cells at baseline had a larger tumor volume, later staging, higher proportion of regulatory T cells, higher blood concentrations of interleukin (IL)-6 and IL-10, and lower interferon-γ concentrations. Following TACE, CD155 concentration decreased; however, TACE did not affect TIGIT expression on T cells. Additionally, among patients receiving TACE combined with apatinib and camrelizumab treatment, patients with a high TIGIT expression on T cells had significantly shorter progression-free survival (PFS) and overall survival times than those of patients in the low-expression group. Patients receiving TACE combined with apatinib and camrelizumab treatment with higher TIGIT expression have shorter PFS time than those receiving TACE combined with apatinib treatment.
Conclusions
Patients with HCC that have a high TIGIT expression on their T cells exhibited poorer baseline characteristics, immunosuppressive status, and prognosis after receiving TACE combined with apatinib and camrelizumab and maybe more suited to receive TACE combined with apatinib treatment instead.
Keywords: Hepatocellular carcinoma, Transcatheter arterial chemoembolization, Immunotherapy, T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains
Background
Liver cancer is the sixth most common cancer worldwide and the third leading cause of cancer-related deaths. Hepatocellular carcinoma (HCC) accounts for the largest proportion of liver cancer cases [1]. Treatment plans for patients with advanced HCC often combine local treatment, targeted therapy, and immunotherapy. Among these options, transcatheter arterial chemoembolization (TACE) combined with apatinib and camrelizumab is associated with longer survival time than that with TACE alone or TACE with only apatinib [2–4].
The T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains (TIGIT) is a novel co-inhibitory molecule primarily located on T and natural killer (NK) cells. CD155 is a high-affinity ligand that can bind to TIGIT [5], and after binding, reactions that inhibit tumor immunity are elicited, leading to T cell dysfunction and inhibition of NK cell cytotoxicity [6]. Simultaneously blocking TIGIT and programmed cell death protein 1 (PD-1) can specifically enhance the anti-tumor effect of CD8 + T cells [7]. In non-small cell lung cancer, patients who use both PD-1 and TIGIT inhibitors have a longer progression-free survival (PFS) time compared to those who use PD-1 inhibitors alone [8]. In liver cancer, multiple immunosuppressants targeting TIGIT have been validated in multiple clinical trials [9].
Although local treatment combined with targeted immunotherapy can significantly improve the prognosis of patients with HCC, some patients are unresponsive to this treatment. Conversely, local treatment combined with targeted therapy can also benefit some patients [10]. Moreover, the relationship between TIGIT and patients with HCC receiving local treatment combined with targeted immunotherapy has not been studied. This study aimed to analyze the relationship between TIGIT expression on T cells and patient baseline characteristics and immunosuppressive status as well as determining the association between TIGIT expression and prognosis following the three different treatment methods.
Methods
Study design and patient selection
This study was approved by the Review Committee of the Science and Ethics Committee of the Cancer Hospital Affiliated to Zhengzhou University (approval number: 2017002). Data from 140 patients diagnosed with HCC and treated at Zhengzhou University Cancer Hospital between January 2019 and December 2022 were retrospectively analyzed. Written informed consent was waived. Among these patients, 20 were included in the TACE-alone treatment group (T group), 66 in the TACE combined with apatinib treatment group (T + A group), and 54 in the TACE combined with apatinib and camrelizumab treatment group (T + A + C group). Data on the patients’ clinical characteristics were collected, including age; sex; Barcelona Clinic Liver Cancer (BCLC) staging; Child–Pugh score; pathogen; tumor size and number; baseline alpha fetoprotein, alanine aminotransferase, aspartate aminotransferase, and vascular endothelial growth factor levels; and baseline lymphoid immune cell test results.
The inclusion criteria were as follows: (i) met the diagnostic and treatment criteria for HCC, with at least one measurable liver target lesion; (ii) not suitable for surgical resection or refusal of surgical treatment; (iii) aged 18–75 years; (iv) liver function suitable for TACE treatment (Child–Pugh A or B ≤ 7score); and (v) no history of liver cancer-related treatment.
The exclusion criteria were as follows: (i) Barcelona Phase A stage; (ii) received anti-tumor treatments, such as surgery, ablation, and radiotherapy; (iii) suffered from severe comorbidities, such as severe heart failure and respiratory system diseases; (iv) uncorrectable abnormalities in renal and coagulation functions; (v) severe liver dysfunction (Child–Pugh class C or D) or irreversible liver decompensation; (vi) Eastern Cooperative Oncology Group score of ˃2 points; (vii) expected life of < 3 months; and (viii) a history of other tumors.
HCC was staged according to the BCLC standards [11]. The Child–Pugh score was calculated based on the patients’ clinical examination results, laboratory parameters, and imaging manifestations [12]. Efficacy was evaluated using the modified response evaluation criteria for solid tumors based on enhanced computed tomography or magnetic resonance imaging: (1) Complete response (CR): All target lesion activity disappeared, indicating no enhancement during the arterial phase; (2) Partial response (PR): The total diameter of active lesions is reduced by ≥ 30%; (3) Progressive disease (PD): The total diameter of active lesions increases by ≥ 20% or new lesions appear; (4) Stable disease (SD): The active lesion size neither shrinks to meet PR criteria nor increases to meet PD criteria [13]. The main endpoint of this study was PFS (the time from the start of treatment to progression or death from any cause), while the secondary endpoint was overall survival (OS) (the period from initial TACE treatment to patient death or loss to follow-up).
TACE and drug therapy
The Seldinger technique, as described in a previous report [14], was used to puncture the femoral artery and evaluate hepatic artery blood flow and tumor blood supply through angiography. The epirubicin (Haizheng Pharmaceutical, Hangzhou, China) dose was 50–75 mg/m2, and it was adjusted based on tumor size, blood vessels, liver function, and body surface area. Epirubicin was mixed with 5–20 mL lipiodol (Lipiodol Ultra-Fluid; Laboratoire Guerbet, Paris, France), the tumor supply artery was superselected through a microcatheter (Progreat; Terumo, Tokyo, Japan), and the mixture was injected at a rate of 1 mL/min until the blood flow stopped. Thereafter, gelatin sponge (Caligel; Alicon Pharmaceutical, Hangzhou, China) particles of 500–700 μm were added to block the artery supplying the tumor.
The multidisciplinary team of the hospital determined the final combination treatment plan based on the BCLC guidelines and individual patient conditions. According to the instructions, patients took targeted drugs daily, starting three days after the first TACE treatment. The patients received 250 mg oral apatinib daily [15]. Additionally, they received intravenous injection of 200 mg of camrelizumab every three weeks within 20–60 min [16]. Owing to toxicity, camrelizumab use can be temporarily interrupted, but with no dose reduction; conversely, the dose of apatinib can be reduced. Medication use was discontinued in the event of disease progression or unacceptable toxic effects, patient selection, or doctor’s recommendation.
Blood sampling and enzyme-linked immunosorbent assay (ELISA)
At the first visit, fasting peripheral venous blood samples were collected from patients at baseline in the morning. Additional post-treatment samples were collected three days after treatment in the TACE group. The samples were centrifuged at 974 × g for 10 min at 4℃, and the separated plasma was stored at -80℃. Human plasma interleukin IL-6, IL-10, PD-1, CD155, and interferon-gamma (IFN-γ) levels were measured using commercially available ELISA kits (Shanghai Enzyme-linked Biotechnology Co., Ltd., China) according to the manufacturer’s instructions.
Flow cytometry
TIGIT expression on T cells was detected at baseline in all patients. Patients who received TACE alone underwent additional testing of TIGIT expression on T cells three days after treatment. Peripheral blood mononuclear cells were isolated from blood samples using Ficoll Paque density gradient centrifugation. Total T cells were sorted using CD3 antibodies, and the TIGIT positivity rate in T cells was detected using FITC-labeled anti-TIGIT antibodies (BD Biosciences). Data were analyzed using FlowJo version 10 software (FlowJo, Ashland, OR, USA).
Statistical analysis
SPSS software (version 22.0) was used for data analysis. The comparison of quantitative data between two groups that conform to normal distribution and variance homogeneity is conducted using a two-independent sample t-test. For samples before and after treatment, which conform to a paired design, a paired t-test is used. For groups that do not follow normal distribution and variance homogeneity, the non-parametric Mann-Whitney U test is applied. The chi-square test is used for qualitative data. When the sample size is ≥ 40 and the theoretical frequency T is ≥ 5, the basic formula is applied; if the sample size is ≥ 40 but the theoretical frequency is 1 ≤ T < 5, use the continuous corrected chi square test. For sample sizes < 40 or when the theoretical frequency T < 1, Fisher’s exact probability method is employed for statistical analysis. Kaplan–Meier method was used to analyze PFS and OS, and the log-rank test was used for intergroup comparisons. P-values < 0.05 were considered statistically significant.
Results
Patient characteristics
The patients’ average age was 57.7 ± 9.6 (range: 29–72) years, most of whom were male (89.3%, 125/140). Among these patients, hepatitis B virus infection was the main cause of liver disease (93.6%, 131/140), and most had cirrhosis (93.6%, 131/140). The number of patients in the T, T + A, and T + A + C groups were 20 (14.3%), 66 (47.1%), and 54 (38.6%), respectively. The average positive expression rates of TIGIT on T cells in the T, T + A, and T + A + C groups were 11.64%, 11.57%, and 12.60%, respectively. Table 1 shows the patients’ detailed baseline demographic data.
Table 1.
Baseline demographic data of patients
| Variable | T (n = 20) | T + A (n = 66) | T + A + C (n = 54) | P value (T + A vs. T + A + C) |
|---|---|---|---|---|
| Age (≥ 55/<55) | 14/6 | 43/23 | 34/20 | 0.804 |
| Sex (F/M) | 6/14 | 6/60 | 3/51 | 0.464 |
| Etiology | ||||
|
Hepatitis B virus Hepatitis C virus Others |
18 0 2 |
63 1 2 |
50 0 4 |
0.371 |
| AFP level (ng/mL) | ||||
|
≤ 400 > 400 |
11 9 |
33 33 |
21 33 |
0.224 |
| ALT (U/L) | ||||
|
≤ 40 > 40 |
6 14 |
16 50 |
14 40 |
0.832 |
| AST (U/L) | ||||
|
≤ 40 > 40 |
3 17 |
4 62 |
4 50 |
0.769 |
|
VEGF (pg/mL) mean (SD) |
411.39 (169.33) |
456.44 (210.09) |
0.198 | |
| Cirrhosis | ||||
|
No Yes |
2 18 |
3 63 |
4 50 |
0.506 |
| Child-Pugh class | ||||
|
A B |
14 6 |
22 44 |
19 35 |
0.831 |
| ECOG Score | ||||
|
0 1 2 |
3 15 2 |
1 52 13 |
3 36 15 |
0.237 |
| Tumor size (cm) | ||||
|
≤ 5 > 5 |
9 11 |
30 36 |
21 33 |
0.469 |
| Tumor number | ||||
|
Single Multiple |
11 9 |
8 58 |
6 48 |
0.864 |
| BCLC stage | ||||
|
A B C |
10 10 0 |
0 21 45 |
0 22 32 |
0.311 |
| TIGIT positive rate | 11.64 (5.90) | 11.57 (6.52) | 12.60 (7.79) | 0.436 |
AFP: alpha fetoprotein; ALT: alanine aminotransferase; AST: aspartate aminotransferase; BCLC: Barcelona Clinic Liver Cancer; ECOG: Eastern Cooperative Oncology Group; SD: standard deviation; T group: TACE-alone treatment group; T + A group: TACE combined with apatinib treatment group; T + A + C group: TACE combined with apatinib and camrelizumab treatment group; TACE: transcatheter arterial chemoembolization; TIGIT: T-cell immune receptor with immunoglobulin and ITIM domains; VEGF: vascular endothelial growth factor
Relationship between TIGIT expression on T cells and the patients’ clinical and immune characteristics
The patients were divided into high- and low-expression groups based on the median positive expression rate (10.44%) of TIGIT in T cells (Table 2). Patients with a higher TIGIT expression in T cells had larger and more late-stage tumors, a higher proportion of regulatory and helper T/suppressor T cells, higher plasma IL-6 and IL-10 concentrations, and lower IFN-γ concentrations (Table 3).
Table 2.
Correlation between TIGIT expression on T cells and the clinical characteristics of patients TIGIT: T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains
| Variable | Low expression (n = 70) | High expression (n = 70) | P value |
|---|---|---|---|
| Age (≥ 55/<55) | 43/27 | 48/22 | 0.376 |
| Sex (F/M) | 7/63 | 8/62 | 0.784 |
| Etiology | |||
|
Hepatitis B virus Hepatitis C virus Others |
66 0 4 |
65 1 4 |
0.498 |
| AFP level (ng/mL) | |||
|
≤ 400 > 400 |
31 39 |
34 36 |
0.611 |
| ALT (U/L) | |||
|
≤ 40 > 40 |
16 54 |
20 50 |
0.439 |
| AST (U/L) | |||
|
≤ 40 > 40 |
5 65 |
6 64 |
0.753 |
|
VEGF (pg/mL) mean (SD) |
412.86 (184.54) |
451.10 (193.70) |
0.270 |
| Cirrhosis | |||
|
No Yes |
5 65 |
4 66 |
1.000 |
| Child-Pugh class | |||
|
A B |
26 44 |
29 41 |
0.604 |
| ECOG Score | |||
|
0 1 2 |
4 56 10 |
3 47 20 |
0.115 |
| Tumor size (cm) | |||
|
≤ 5 > 5 |
36 34 |
24 46 |
0.040 |
| Tumor number | |||
|
Single Multiple |
14 56 |
11 59 |
0.508 |
| BCLC stage | |||
|
A B C |
6 33 31 |
4 20 46 |
0.039 |
AFP: alpha fetoprotein; ALT: alanine aminotransferase; AST: aspartate aminotransferase; BCLC: Barcelona Clinic Liver Cancer; ECOG: Eastern Cooperative Oncology Group; SD: standard deviation; TIGIT: T-cell immune receptor with immunoglobulin and ITIM domains; VEGF: vascular endothelial growth factor
Table 3.
Correlation between TIGIT expression on T cells and patient immune indicators TIGIT: T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains
| Variable | Low expression (n = 70) | High expression (n = 70) | P value |
|---|---|---|---|
| Total T lymphocytes (%) | 75.15 (11.50) | 71.33 (11.66) | 0.053 |
| Suppressor/cytotoxic cells (%) | 29.50 (10.34) | 26.82 (12.87) | 0.175 |
| Helper/inducible cells (%) | 38.31 (8.56) | 38.85 (9.09) | 0.719 |
| Natural killer cell (%) | 15.44 (9.02) | 16.94 (10.65) | 0.368 |
| B lymphocytes (%) | 8.65 (5.57) | 10.22 (6.18) | 0.118 |
| Helper T cells/Suppressor T cells | 1.56 (1.03) | 1.95 (1.21) | 0.041 |
| Regulatory cells (%) | 10.16 (2.95) | 11.36 (3.30) | 0.025 |
| Proportion of PD-1 + in Mononuclei (%) | 3.87 (7.90) | 4.99 (7.33) | 0.388 |
| Proportion of PD-1 + in CD3 + cells (%) | 4.14 (9.35) | 6.02 (10.04) | 0.254 |
| Proportion of PD-1 + in CD4 + cells (%) | 5.01 (10.35) | 7.29 (11.76) | 0.226 |
| Proportion of PD-1 + in CD8 + cells (%) | 2.91 (8.36) | 5.53 (9.28) | 0.081 |
| Absolute count of total lymphocytes (/uL) | 1481.04 (669.23) | 1428.14 (607.08) | 0.625 |
| Absolute T lymphocyte count (/uL) | 1012.99 (437.57) | 1085.39 (449.49) | 0.336 |
| CD4 + T lymphocyte absolute count (/uL) | 504.31 (282.67) | 518.37 (249.41) | 0.756 |
| CD8 + T lymphocyte absolute count (/uL) | 408.86 (248.79) | 434.09 (249.65) | 0.550 |
| Absolute NK cell count (/uL) | 231.06 (188.13) | 255.47 (198.28) | 0.456 |
| Absolute B cell count (/uL) | 135.76 (121.75) | 122.37 (94.72) | 0.469 |
|
IL-6 (pg/mL) IL-10 (pg/mL) |
85.78 (65.03) 2111.68 (844.17) |
189.15 (144.67) 3236.56 (1166.62) |
0.006 0.001 |
| PD-1 (pg/mL) | 345.6 (134.84) | 480.72 (269.98) | 0.052 |
| CD155 (ng/mL) | 115.78 (57.46) | 119.82 (42.07) | 0.636 |
| IFN-γ(pg/mL) | 2759.78 (1471.40) | 1476.34 (995.34) | 0.003 |
IFN-γ: interferon gamma; IL: interleukin; PD-1: programmed cell death protein 1; TIGIT: T-cell immune receptor with immunoglobulin and ITIM domains
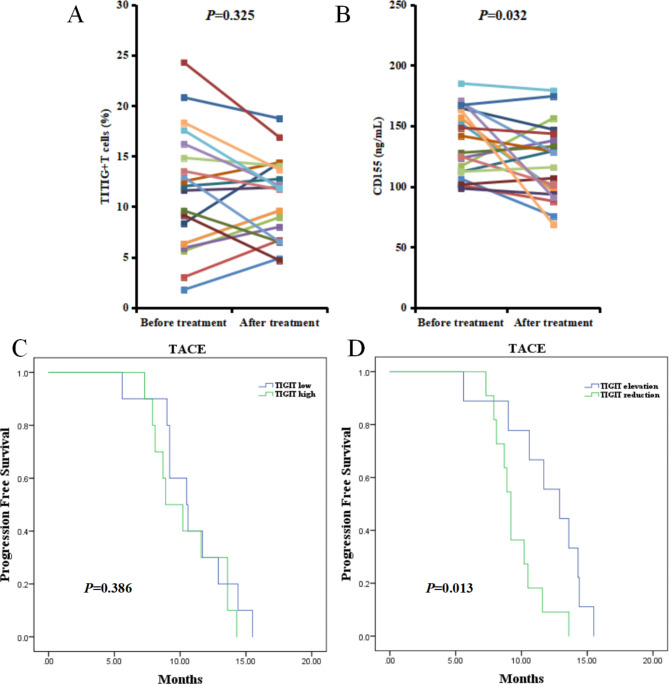
TIGIT expression and prognosis in patients in the T group
Of the 20 patients who received TACE treatment alone, no significant change was observed in the proportion of TIGIT + T cells three days after treatment compared to baseline (P = 0.325) (Fig. 1a and b). In addition, plasma CD155 expression was significantly lower at three days after treatment than before treatment (P = 0.032).
Fig. 1.
A, Changes in the proportion of TIGIT + T cells before and after TACE treatment. B, Changes in CD155 expression in the plasma before and after TACE treatment. C, PFS rates of patients in the TIGIT high- and low-expression groups who received TACE treatment alone. D, PFS rates in patients with increased and decreased TIGIT expression after TACE treatment
TACE: transcatheter arterial chemoembolization; TIGIT: T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains; PFS: progression-free survival
According to the median positive expression rate (11.60%) of TIGIT in T cells of patients receiving TACE treatment alone, the patients were divided into high- and low-expression groups. No significant difference was observed in PFS time between the two groups (TIGIT low: median PFS time, 10.5 months; 95% confidence interval [CI], 8.331–12.669 and TIGIT high: median PFS time, 8.9 months; 95% CI, 6.576–11.224; P = 0.386) (Fig. 1c).
According to the changes in TIGIT expression after TACE treatment, patients were divided into TIGIT elevation and TIGIT reduction groups (Fig. 1d). The PFS time of patients in the TIGIT elevation group was significantly longer than that of those in the TIGIT reduction group (TIGIT elevation: median PFS time, 12.9 months; 95% CI, 9.394–16.406 and TIGIT reduction: median PFS time, 9.2 months; 95% CI, 8.679–9.721; P = 0.013).
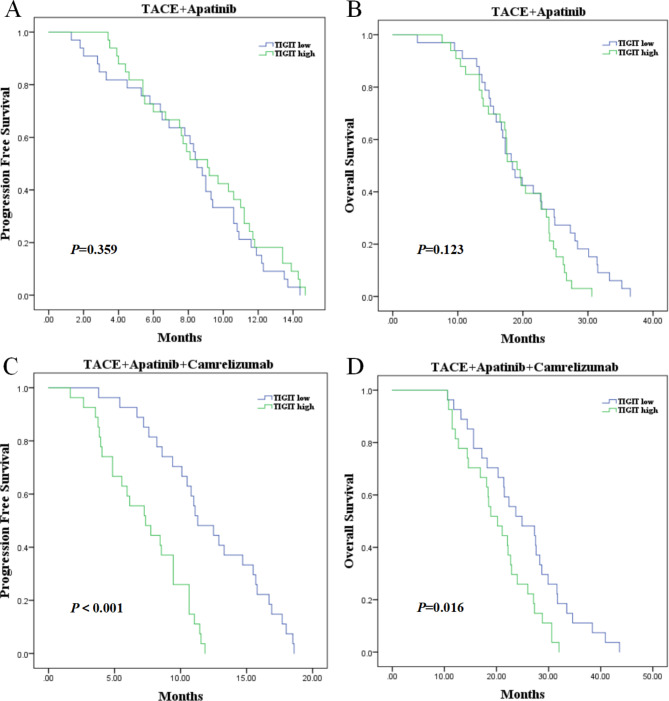
TIGIT expression and prognosis in patients in the T + A and T + A + C groups
Patients were divided into high- and low-expression groups based on the median positive expression rate of TIGIT in T cells of patients receiving TACE combined with either apatinib and or apatinib and camrelizumab treatment. No significant differences were observed in PFS (TIGIT low: median PFS time, 8.5 months; 95% CI, 7.656–9.344 and TIGIT high: median PFS time, 9.1 months; 95% CI, 6.849–11.351; P = 0.359) and OS (TIGIT low: median OS time, 18.4 months; 95% CI, 15.586–21.214 and TIGIT high: median OS time, 19.1 months; 95% CI, 16.943–21.257; P = 0.123) between the high and low TIGIT expression groups in patients treated with TACE combined with apatinib (Fig. 2a and b).
Fig. 2.
A, PFS rates of patients in the TIGIT high- and low-expression groups who received TACE combined with apatinib treatment. B, OS rates of patients in the TIGIT high- and low-expression groups who received TACE combined with apatinib treatment. C, PFS rates of patients in the TIGIT high- and low-expression groups who received TACE combined with apatinib and camrelizumab treatment. D, OS rates of patients in the TIGIT high- and low-expression groups who received TACE combined with apatinib and camrelizumab treatment
TACE: transcatheter arterial chemoembolization; TIGIT: T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains; PFS: progression-free survival; OS: overall survival
In patients treated with TACE combined with apatinib and camrelizumab, the PFS time of patients in the low TIGIT expression group was significantly longer than that of those in the high TIGIT expression group (TIGIT low: median PFS time, 11.3 months; 95% CI, 8.756–13.844 and TIGIT high: median PFS time, 7.4 months; 95% CI, 4.636–10.064; P < 0.001). The OS time of patients in the low TIGIT expression group was significantly longer than that of those in the high TIGIT expression group (TIGIT low: median OS time, 24.9 months; 95% CI, 16.588–33.212 and TIGIT high: median OS time, 20.2 months; 95% CI, 15.790–24.610; P = 0.016) (Fig. 2c and d).
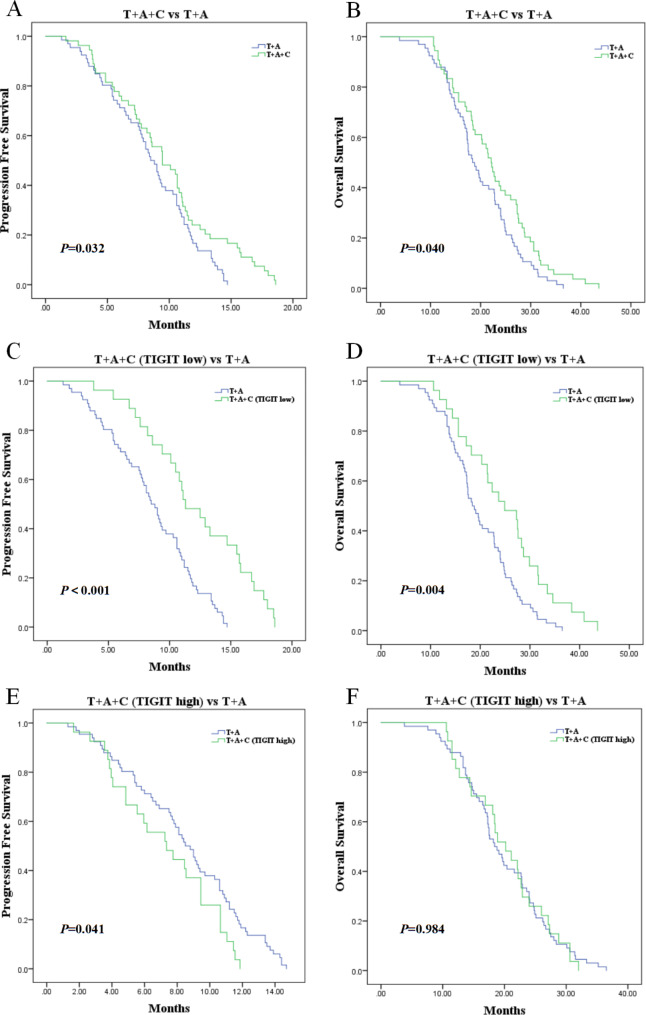
Comparison of survival prognosis between the T + A + C and T + A groups
As shown in Fig. 3a and b, patients in the T + A + C group had significantly longer PFS (T + A + C: median PFS time, 9.4 months; 95% CI, 7.171–11.729 and T + A: median PFS time, 8.5 months; 95% CI, 7.438–9.562; P = 0.032) and OS times (T + A + C: median OS time, 22.1 months; 95% CI, 20.180–24.020 and T + A: median OS time, 18.4 months; 95% CI, 16.365–20.435; P = 0.040) than those in the T + A group.
Fig. 3.
A, PFS survival rates of patients receiving TACE combined with apatinib and camrelizumab and TACE combined with apatinib treatment. B, OS rates of patients receiving TACE combined with apatinib and camrelizumab or TACE combined with apatinib treatment. C, PFS rates in TIGIT low expression patients receiving TACE combined with apatinib and camrelizumab treatment and in patients receiving TACE combined with apatinib treatment. D, OS rates in TIGIT low expression patients receiving TACE combined with apatinib and camrelizumab treatment and in patients receiving TACE combined with apatinib treatment. E, PFS rates in TIGIT high expression patients receiving TACE combined with apatinib and camrelizumab treatment and in patients receiving TACE combined with apatinib treatment. F, OS rates in TIGIT high expression patients receiving TACE combined with apatinib and camrelizumab treatment and in patients receiving TACE combined with apatinib treatment
TACE: transcatheter arterial chemoembolization; TIGIT: T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains; PFS: progression-free survival; OS: overall survival
Considering the significant differences in survival between high- and low-expression TIGIT groups receiving TACE combined with apatinib and camrelizumab, we analyzed the survival prognosis of patients with high and low TIGIT expression in the T + A + C group and all patients in the T + A group, respectively. The results are shown in Fig. 3c and d. Compared with patients in the T + A group, those in the TIGIT low-expression group who received TACE combined with apatinib and camrelizumab had longer PFS (T + A + C-TIGIT-low: median PFS time, 11.3 months; 95% CI, 8.756–13.844 and T + A: median PFS time, 8.5 months; 95% CI, 7.438–9.562; P < 0.001) and OS times (T + A + C-TIGIT-low: median OS time, 24.9 months; 95% CI, 16.588–33.212 and T + A: median OS time, 18.4 months; 95% CI, 16.365–20.435; P = 0.004). As shown in Fig. 3e and f, compared with patients in the T + A group, those in the TIGIT high-expression group who received TACE combined with apatinib and camrelizumab had shorter PFS (T + A + C-TIGIT-high: median PFS time, 7.4 months; 95% CI, 4.636–10.064 and T + A: median PFS time, 8.5 months; 95% CI, 7.438–9.562; P = 0.041). However, no significant difference existed in OS time between the two groups (T + A + C-TIGIT-high: median OS time, 20.2 months; 95% CI, 15.790–24.610 and T + A: median OS time, 18.4 months; 95% CI, 16.365–20.435; P = 0.984).
Discussion
In the present study, we found that TIGIT expression on T cells positively correlated with tumor size and staging in patients with HCC, including the amount of certain immune cells and cytokines. Patients with lower TIGIT expression on their T cells had a better prognosis after receiving TACE combined with apatinib and camrelizumab treatment than those with higher TIGIT expression. Patients with high TIGIT expression who received TACE combined with apatinib and camrelizumab treatment had worse survival than those who received TACE with apatinib.
Increasing evidence suggests that the TIGIT/CD155 pathway is involved in HCC pathogenesis [17]. TIGIT and CD155 expression are both elevated in liver cancer tissue. As the degree of tumor cell differentiation increases from high to low, TIGIT expression in liver cancer tissue gradually increases [18]. The PD-1 + TIGIT + CD8 + T cell population is elevated in patients with advanced hepatitis B virus-HCC, and PD-1 + TIGIT + CD8 + T cells exhibit T cell exhaustion characteristics. Blocking the TIGIT/CD155 signaling pathway can reverse T cell failure [19], indicating that TIGIT may have clinical significance in tumor immunity and patient prognoses.
Furthermore, we found that high TIGIT expression on T cells was significantly associated with adverse baseline characteristics, such as larger tumor size and later staging in patients with HCC. Additionally, the proportion of regulatory T cells in the blood of patients with high TIGIT expression on T cells was higher. Regulatory T cells can inhibit the immune response of the body to tumor cells, and an increase in their proportion can inhibit anti-tumor immune effects, promoting tumor growth [20]. The high-expression group also exhibited higher levels of IL-6 and IL-10, which were associated with poor patient prognosis. IL-6 and IL-10 can inhibit anti-tumor immunity by blocking the synthesis of pro-inflammatory cytokines and inhibiting the expression of cell surface molecules involved in antigen presentation and co-stimulation [21, 22]. IFN-γ can promote the differentiation and proliferation of T lymphocytes, enhance the activity of immune cells, and inhibit the proliferation of tumor cells [23]. However, IFN-γ concentration in the blood of patients with high TIGIT expression was lower. Therefore, our findings indicate that patients with high TIGIT expression on T cells at baseline have poor immune status and a poor prognosis.
TACE is a commonly used local treatment method for patients with HCC that can affect the immune microenvironment of tumors in multiple aspects [24]. We found no significant change in TIGIT expression on T cells in patients receiving TACE treatment alone either before or after treatment; however, the expression of its ligand CD155 in the blood was significantly reduced. This suggests that TACE may affect the activity of the TIGIT/CD155 pathway to some extent, improving the inhibitory immune microenvironment. Although TIGIT expression was negatively correlated with patient prognosis, the PFS time in patients with increased TIGIT expression after TACE was significantly longer than that in patients with decreased TIGIT expression. This may be attributed to the lower TIGIT expression in the elevated group of patients who are more sensitive to the multi-efficacy of TACE on the immune microenvironment; however, this hypothesis requires further validation.
Additionally, the relationship between TIGIT expression on T cells and the prognosis of patients receiving targeted immunotherapy was evaluated. We found that patients in the low-expression group receiving TACE combined with apatinib and camrelizumab treatment had better PFS and OS than those in the high-expression group. However, in patients receiving TACE alone and TACE combined with apatinib treatment, no significant correlation was observed between TIGIT expression and patient prognosis. This also confirms the correlation between TIGIT and PD-1 immunosuppressants. Previous studies have shown that the expression frequency of TIGIT on CD8 + T cells is positively correlated with PD-1 expression frequency. For other cancer treatments, dual blockade of TIGIT and PD-1 has shown a synergistic effect, achieving a greater-than-sum impact [25]. This indicates that TIGIT expression on T cells can relatively predict the prognosis of patients treated with TACE combined with apatinib and camrelizumab and even provide theoretical support for combining TIGIT and PD-1 dual immunosuppressive therapy in patients with HCC. In addition, further comparative studies found that patients with high TIGIT expression who received TACE combined with apatinib and camrelizumab treatment had even shorter PFS than those who received TACE combined with apatinib, but no significant difference in OS was observed between the two groups of patients. However, patients with low TIGIT expression in the T + A + C group had a better prognosis than those in the T + A group. This is very noteworthy, indicating that patients with high TIGIT expression on T cells are not suitable for TACE combined with apatinib and camrelizumab treatment. Instead, receiving TACE combined with apatinib treatment can achieve a better prognosis. This also indicates that TIGIT expression on T cells can help distinguish whether patients are suitable for immunotherapy or TACE combined with targeted immunotherapy. However, further research is required to confirm this assertion.
Despite the strengths of the study, it also has some limitations. Further mechanistic research is required to determine the impact of TACE on TIGIT expression and the immune microenvironment, as well as the biological effects produced by interleukins 6 and 10. Furthermore, a larger sample size is needed to determine the correlation between TIGIT and patient prognosis following immune combination therapy and determine more accurate threshold values.
Conclusions
Patients with HCC who had a high TIGIT expression on their T cells may have poorer baseline characteristics, immunosuppressive status, and prognosis after receiving TACE combined with apatinib and camrelizumab treatment. In addition, patients with high TIGIT expression on their T cells may not be suitable for TACE combined with apatinib and camrelizumab treatment. Instead, receiving TACE combined with apatinib treatment can lead to a better prognosis. This provides a valuable reference for HCC patients to choose the most suitable combination therapy methods.
Acknowledgements
We thank the editors for their kind work and the reviewers for their constructive comments.
Abbreviations
- BCLC
Barcelona Clinic Liver Cancer
- HCC
Hepatocellular carcinoma
- IFN-γ
Interferon-gamma
- IL
Interleukin
- NK cells
Natural killer cells
- OS
Overall survival
- PFS
Progression-free survival
- PD-1
Programmed cell death protein 1
- TACE
Transcatheter arterial chemoembolization
- TIGIT
T-cell immunoreceptor with immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domains
- ELISA
Enzyme-linked immunosorbent assay
- CI
Confidence interval
Author contributions
Conception and design: HLL, YG; Patient selection and treatment: HTH, WLX, XY, FTL, Data collection, analysis, and interpretation: WBZ; Datainterpretation: WLX; Steering committeeactivities and critical statistical processing: HLL, HTH; Manuscript writing: YG; Manuscript reviewing: HLL, HTH.All authors contributed to the article and approved thesubmitted version.
Funding
This study has received funding from the Henan Province Natural Science Foundation (212300410403), Technology Major Project of the Ministry of Science and Technology of China (2018ZX10303502), and Medical Education Research Project of Henan Province (Wjlx2021334).
Data availability
The datasets generated and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Due to the retrospective nature of this study, with the approval of the Review Committee of the Science and Ethics Committee of the Cancer Hospital Affiliated to Zhengzhou University (approval number: 2017002), written informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuan Guo and Xiong Yang are co-first authors
Contributor Information
Hong Tao Hu, Email: huhongtaogy@163.com.
Hai Liang Li, Email: lihailianggy@163.com.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. 10.3322/caac.21660. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2.Jin ZC, Zhong BY, Chen JJ, Zhu HD, Sun JH, Yin GW, et al. Real-world efficacy and safety of TACE plus camrelizumab and apatinib in patients with HCC (CHANCE2211): a propensity score matching study. Eur Radiol. 2023;33:8669–81. 10.1007/s00330-023-09754-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duan X, Li H, Kuang D, Chen P, Zhang K, Li Y, et al. Transcatheter arterial chemoembolization plus apatinib with or without camrelizumab for unresectable hepatocellular carcinoma: a multicenter retrospective cohort study. Hepatol Int. 2023;17:915–26. 10.1007/s12072-023-10519-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ju S, Zhou C, Yang C, Wang C, Liu J, Wang Y, et al. Apatinib plus camrelizumab with/without chemoembolization for hepatocellular carcinoma: a real-world experience of a single center. Front Oncol. 2022;11:835889. 10.3389/fonc.2021.835889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang C, Wang Y, Xun X, Wang S, Xiang X, Hu S, et al. TIGIT can exert immunosuppressive effects on CD8 + T cells by the CD155/TIGIT signaling pathway for hepatocellular carcinoma in vitro. J Immunother. 2020;43:236–43. 10.1097/CJI.0000000000000330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heiduk M, Klimova A, Reiche C, Digomann D, Beer C, Aust DE, et al. TIGIT expression delineates T-cell populations with distinct functional and prognostic impact in pancreatic cancer. Clin Cancer Res. 2023;29:2638–50. 10.1158/1078-0432.CCR-23-0258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge Z, Zhou G, Campos Carrascosa L, Gausvik E, Boor PPC, Noordam L, et al. TIGIT and PD1 co-blockade restores ex vivo functions of human tumor-infiltrating CD8 + T cells in hepatocellular carcinoma. Cell Mol Gastroenterol Hepatol. 2021;12:443–64. 10.1016/j.jcmgh.2021.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho BC, Abreu DR, Hussein M, Cobo M, Patel AJ, Secen N, et al. Tiragolumab plus Atezolizumab versus placebo plus atezolizumab as a first-line treatment for PD-L1-selected non-small-cell lung cancer (CITYSCAPE): primary and follow-up analyses of a randomised, double-blind, phase 2 study. Lancet Oncol. 2022;23:781–92. 10.1016/S1470-2045(22)00226-1 [DOI] [PubMed] [Google Scholar]
- 9.Bicer F, Kure C, Ozluk AA, El-Rayes BF, Akce M. Advances in immunotherapy for hepatocellular carcinoma (HCC). Curr Oncol. 2023;30:9789–812. 10.3390/curroncol30110711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo Y, Hu HT, Xu SJ, Xia WL, Li Y, Lu J, et al. Correlation of serum chemokine ligand 14 with Barcelona clinic liver cancer stage, lymphocyte profile, and response to transarterial chemoembolization in patients with hepatocellular carcinoma. J Vasc Interv Radiol. 2023;34:991–8. 10.1016/j.jvir.2023.01.032 [DOI] [PubMed] [Google Scholar]
- 11.Xia WL, Xu SJ, Guo Y, Zhao XH, Hu HT, Zhao Y, et al. Plasma arginase-1 as a predictive marker for early transarterial chemoembolization refractoriness in unresectable hepatocellular carcinoma. Front Oncol. 2022;12:1014653. 10.3389/fonc.2022.1014653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xia WL, Zhao XH, Guo Y, Cao GS, Wu G, Fan WJ, et al. Transarterial chemoembolization combined with apatinib with or without PD-1 inhibitors in BCLC stage C hepatocellular carcinoma: a multicenter retrospective study. Front Oncol. 2022;12:961394. 10.3389/fonc.2022.961394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan J, Fan W, Liu T, Zhu B, Liu Y, Wang S, et al. TREM2 + macrophages suppress CD8 + T-cell infiltration after transarterial chemoembolisation in hepatocellular carcinoma. J Hepatol. 2023;79:126–40. 10.1016/j.jhep.2023.02.032 [DOI] [PubMed] [Google Scholar]
- 14.Bargellini I, Lorenzoni V, Lorenzoni G, Scalise P, Andreozzi G, Bozzi E, et al. Duration of response after DEB-TACE compared to lipiodol-TACE in HCC-naïve patients: a propensity score matching analysis. Eur Radiol. 2021;31:7512–22. 10.1007/s00330-021-07905-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Z, Lin Y, Zhang J, Zhang Y, Li Y, Liu Z, et al. Molecular targeted and immune checkpoint therapy for advanced hepatocellular carcinoma. J Exp Clin Cancer Res. 2019;38:447. 10.1186/s13046-019-1412-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao Y, Wang J, Liu WN, Fong SY, Shuen TWH, Liu M, et al. Analysis and validation of human targets and treatments using a hepatocellular carcinoma-immune humanized mouse model. Hepatology. 2021;74:1395–410. 10.1002/hep.31812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harjunpää H, Guillerey C. TIGIT as an emerging immune checkpoint. Clin Exp Immunol. 2020;200:108–19. 10.1111/cei.13407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duan X, Liu J, Cui J, Ma B, Zhou Q, Yang X, et al. Expression of TIGIT/CD155 and correlations with clinical pathological features in human hepatocellular carcinoma. Mol Med Rep. 2019;20:3773–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Li M, Wang X, Dang Z, Jiang Y, Wang X, et al. PD-1 + TIGIT + CD8 + T cells are associated with pathogenesis and progression of patients with hepatitis B virus-related hepatocellular carcinoma. Cancer Immunol Immunother. 2019;68:2041–54. 10.1007/s00262-019-02426-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iglesias-Escudero M, Arias-González N, Martínez-Cáceres E. Regulatory cells and the effect of cancer immunotherapy. Mol Cancer. 2023;22:26. 10.1186/s12943-023-01714-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tanaka T, Narazaki M, Kishimoto T. Interleukin (IL-6) immunotherapy. Cold Spring Harb Perspect Biol. 2018;10:a028456. 10.1101/cshperspect.a028456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saraiva M, Vieira P, O’Garra A. Biology and therapeutic potential of interleukin-10. J Exp Med. 2020;217:e20190418. 10.1084/jem.20190418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jorgovanovic D, Song M, Wang L, Zhang Y. Roles of IFN-γ in tumor progression and regression: a review. Biomark Res. 2020;8:49. 10.1186/s40364-020-00228-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piscaglia F, Ogasawara S. Patient selection for transarterial chemoembolization in hepatocellular carcinoma: importance of benefit/risk assessment. Liver Cancer. 2018;7:104–19. 10.1159/000485471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chiu DK, Yuen VW, Cheu JW, Wei LL, Ting V, Fehlings M, et al. Hepatocellular carcinoma cells up-regulate PVRL1, stabilizing PVR and inhibiting the cytotoxic T-cell response via TIGIT to mediate tumor resistance to PD1 inhibitors in mice. Gastroenterology. 2020;159:609–23. 10.1053/j.gastro.2020.03.074 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed in the current study are available from the corresponding author upon reasonable request.