Abstract
Practical relevance:
Tooth resorption is common in the domestic cat and the incidence has been reported to increase with increasing age. Cats with clinically missing teeth have also been found to be more likely to have tooth resorption. All types of teeth in the feline dentition may be affected, but lesions seem to be more common in certain teeth.
Clinical challenges:
Tooth resorption can be difficult to detect, with cats often masking signs of oral discomfort or pain. Routine radiography is required for timely diagnosis, as clinical (visual and tactile) methods only detect late-stage lesions – that is, when they become evident in the crown. The aetiology of many tooth resorptions is not clear. A large number of lesions appear to be idiopathic and, to date, there is no known treatment that prevents the development and/or progression of this category of tooth resorption. Tooth extraction is the gold standard treatment but teeth with resorptive lesions are notoriously difficult to extract and coronal amputation is often indicated. Determining the best treatment option in an individual case again relies on radiography.
Audience:
This review is aimed at feline and general practitioners, as well as veterinarians with expertise in dentistry.
Evidence base:
The author draws on the published literature and her clinical experience and own research to review current thinking about the epidemiology, aetiology and pathogenesis of tooth resorptions, and to offer advice on diagnosis and treatment options.
Epidemiology – what do we know?
Resorption of teeth is common in domestic cats and frequently presents clinically as a hard tissue defect at the cemento-enamel junction of the tooth. Prevalence rates ranging from 28.5–67.0% have been reported in the cat and the incidence increases with increasing age.2,7 –11 Certain breed susceptibilities have also been suggested in some studies, but differences in the mean age among different breed groups examined make meaningful comparisons difficult.
The wide variation in prevalence rates can be explained by the different populations of cats studied (random vs dental vs mixed) and by the different methods used to diagnose tooth resorption (clinical vs radiographic). The incidence has generally been higher in studies where the cats examined were presented for dental examination or treatment, as compared with studies looking at a random or mixed (ie, presented for dental or other problems) populations of cats. However, in an Australian study looking at a mixed population, 52% of cats were affected, with a mean of 3.2 lesions per affected cat. 7
All types of teeth in the feline dentition may be affected by tooth resorption, but lesions seem to be more frequent in certain teeth. 11 The common manifestation of a defect at the cemento-enamel junction can often be diagnosed clinically by visual and tactile examination. Studies that have included radiography have demonstrated that resorption can occur anywhere on the root surfaces (ie, not only at the cemento-enamel junction).11–13 Clearly, clinical methods will only detect lesions that involve the crown, while radiography will also detect lesions confined to the root. Thus, the reported prevalence of tooth resorption in studies that include radiography is higher.
An investigation of the incidence of tooth resorption in a clinically healthy population of 228 cats (mean age 4.92 years), using a combination of clinical examination and radiography, 11 provided some interesting insights:
Clinical manifestation
Tooth resorptions occur as a result of an external root resorption process (see box on page 39), wherein the hard tissues of the root surfaces are destroyed by the activity of multinucleated cells called odontoclasts. The destroyed root surface is replaced by cementum-like or bone-like tissue.
The process starts in cementum and progresses to involve the dentine, where it spreads along the dentine tubules and eventually comes to involve the dentine of the crown as well as the root. The peripulpal dentine is relatively resistant to resorption and the pulp only becomes involved late in the disease. The process extends through the crown dentine, eventually reaching the enamel. The enamel is either resorbed or it fractures off and a defect becomes clinically evident (Figures 1 and 2a).
Figure 1.

Tooth resorptions first become clinically evident in the crown, often as a defect at the cemento-enamel junction. Contrary to common belief, this is a late-stage lesion. The process has extended into the crown dentine and come to involve the enamel, which in this cat has either resorbed or fractured off to reveal a small defect filled with granulation-like tissue at the buccal aspect of the gingival margin of the maxillary third premolar (107)
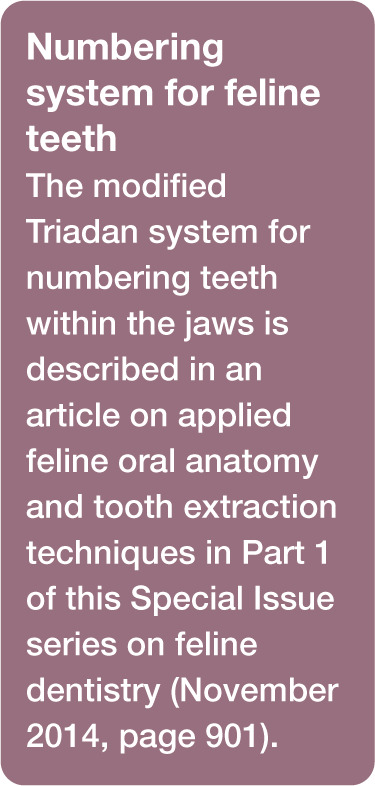
Figure 2.
Clinical and radiographic appearance of tooth resorption in the right mandibular third premolar (407). (a) There is an extensive defect at the cemento-enamel junction of the tooth. The destroyed dentine and enamel have been replaced by connective tissue in this late-stage lesion. (b) Radiography reveals that both roots of the tooth show evidence of extensive resorption – note the loss of a distinct periodontal ligament space, replacement of tooth substance by bone-like material in the distal root, and destruction of most of the crown dentine. This tooth requires treatment
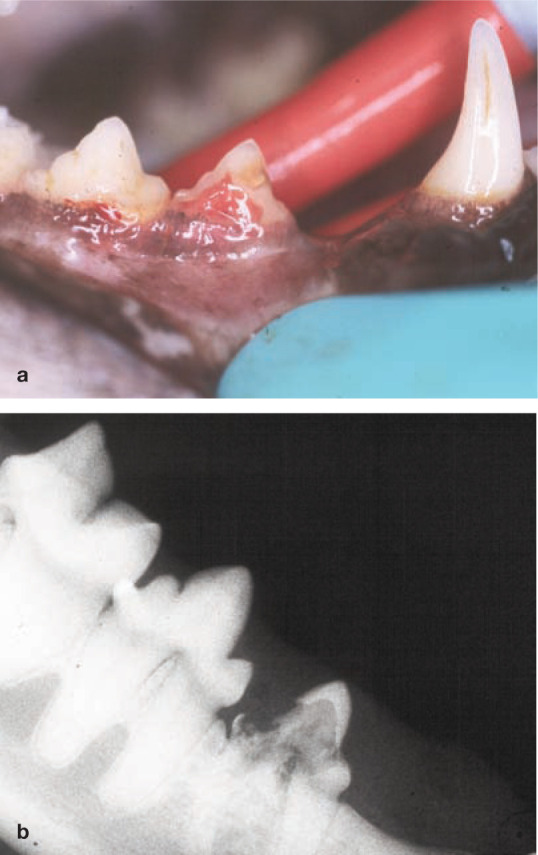
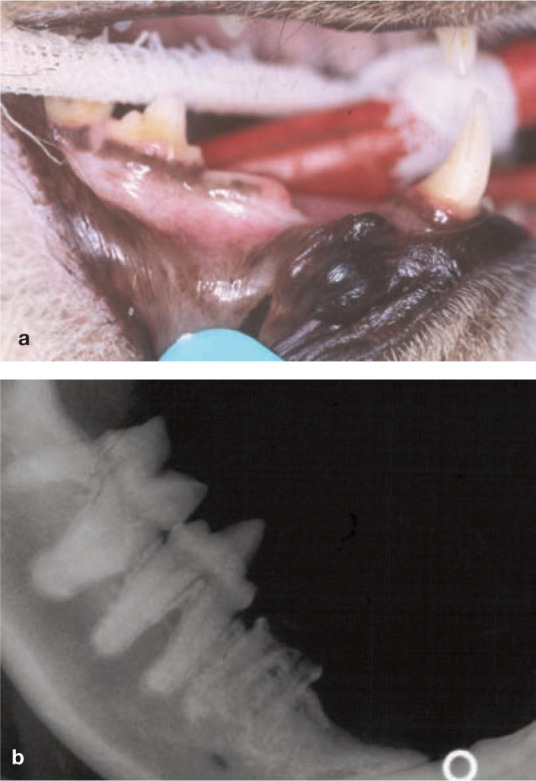
In the absence of routine radiography, the lesions are first noted clinically when they become evident in the crown, often as defects at the cemento-enamel junction. Figure 2b shows the radiographic appearance of the clinical lesion seen in Figure 2a, and amply illustrates how this first clinical manifestation represents a late-stage lesion. In many cases, progressive dentine destruction with tooth resorption weakens and undermines the crown to such an extent that minor trauma (eg, during chewing) causes the crown to fracture off, leaving the root in the alveolar bone. The resorbing root remnants are usually covered by intact gingiva (Figure 3); however, in some cases the overlying gingiva may be inflamed (Figure 4).
Figure 3.
Clinical and radiographic appearance of a missing tooth with gingival overgrowth. (a) The right mandibular third premolar (407) is absent on clinical examination. The overlying gingiva is not inflamed. (b) The roots are retained in the alveolar bone and are showing evidence of ongoing resorption. The only treatment required in this cat is clinical and radiographic monitoring (ie, there is no indication to extract the retained roots)
Figure 4.

Missing tooth with gingival inflammation. In this patient, the progressive dentine destruction has weakened and undermined the crown of the right maxillary canine (104) to such an extent that minor trauma (likely during chewing) has caused it to fracture, leaving the root in the alveolar bone. The gingiva overlying the retained root remnant is inflamed. The retained root remnant needs to be extracted
Aetiology and pathogenesis
While the ongoing or established resorptive process has been detailed,23–25 the aetiology of many tooth resorptions is not clear.
As discussed, it seems likely that at least two different types of resorption with different aetiologies are currently diagnosed as the same condition. This is supported by the findings of a study investigating the radiographic appearance of 543 feline teeth with tooth resorption. 22 Two types of roots were identified: type 1 roots had normal root radio-density and an intact periodontal ligament space; type 2 roots were radiolucent and lacked a clear periodontal ligament space.
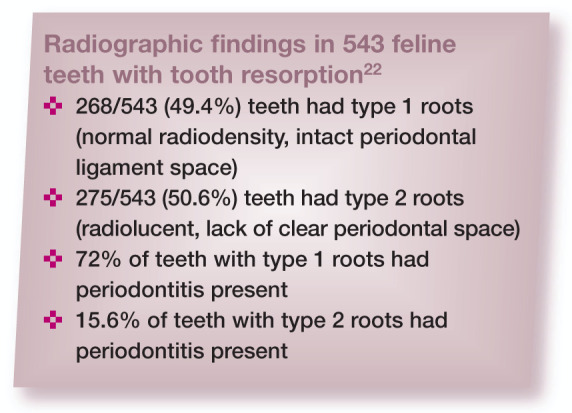
Based on these findings it seems possible that type 1 resorption is inflammatory and associated with periodontal disease while type 2 resorption is truly idiopathic.
It had been assumed that tooth resorption represented a PIRR type of lesion and was associated with periodontal disease.20,23,24,26 However, studies have shown that the histological lesion is a non-inflammatory replacement resorption, resulting in ankylosis, 27 and that there is no association between gingivitis index and the prevalence of tooth resorption. 11 These findings indicate that while a PIRR type of lesion does exist, it is not the only type of root resorption. In fact, a non-inflammatory replacement resorption is equally common. The cause of the PIRR type lesion is inflammation of adjacent tissue (ie, periodontitis), while the cause of the non-inflammatory replacement resorption is as yet unknown (ie, truly idiopathic).
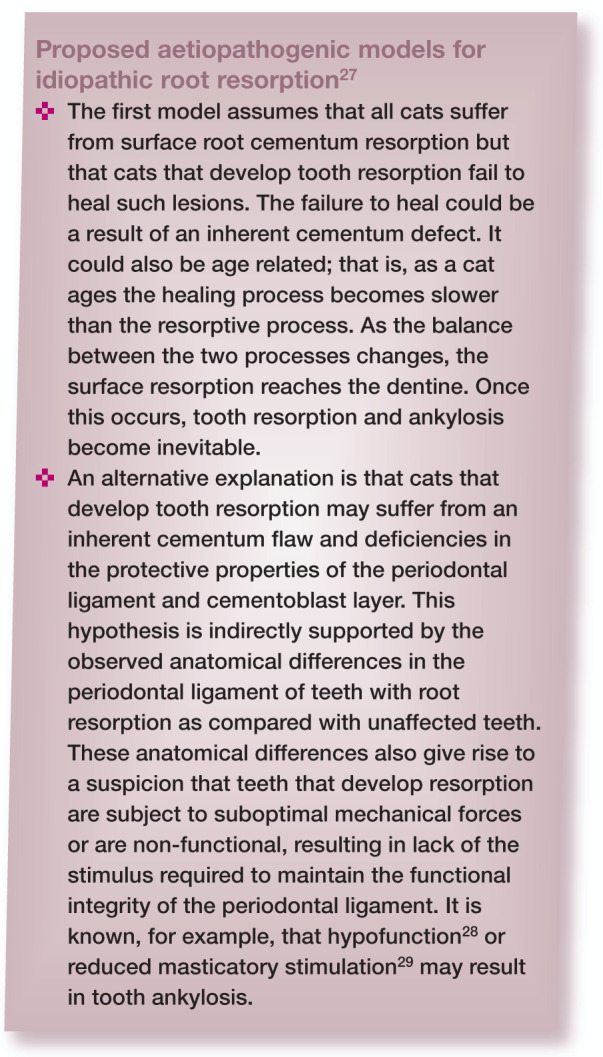
The author’s own research on the histological features of the early lesion found that surface resorptions in the root cementum were common. 27 The level along the root at which the lesions were identified varied, but they were always below the level of the alveolar crest, and were not associated with inflammation in the adjacent periodontal ligament. Therefore, in conflict with some data in the literature,7,8 this study found no evidence to support the hypothesis that resorption starts at the cemento-enamel junction or in the cervical part of the root. The conclusion was that further studies are necessary to determine exactly what causes the high incidence of this type of ‘idiopathic’ feline external root resorption. However, based on the observations, several aetiopathogenic models were suggested:
Another line of research has investigated calcium homeostasis in cats with and without tooth resorption. One study reported a link between raised circulating levels of 25-hydroxyvitamin D and odontoclastic tooth resorption, 30 and concluded that chronic excess intake of vitamin D may play an important pathogenic role. Later studies did not identify raised circulating levels of 25-hydroxyvitamin D in cats with tooth resorption and concluded that increased serum vitamin D levels as a causative factor for root resorption could not be supported.31–33
In summary, some of the tooth resorptions seen in cats are associated with inflammation of adjacent tissue, usually periodontitis, but a large number of lesions are idiopathic.
Diagnosis
Tooth resorptions can be detected by a combination of:
Visual inspection;
Examination under anaesthesia with a sharp dental explorer;
Intraoral dental radiography.
As discussed, visual inspection and tactile examination with a dental explorer will identify only end-stage lesions (ie, when the process is involving the crown and has resulted in an obvious defect; Figures 1 and 2a). Radiography, on the other hand, will additionally identify lesions that are localised to the root surfaces within the alveolar bone (Figure 5). Radiography should thus be considered an essential part of the diagnostic work-up. Moreover, it is only with the aid of radiography that the appearance and extent of a resorptive process can be identified (Figures 2b and 5), allowing the best treatment option to be selected.
Figure 5.

The value of radiography for diagnosis and treatment selection is underlined by this image. The left mandibular canine (304) has a resorbing root, but the process has not yet extended into the crown dentine. In fact, there was no clinical evidence of tooth resorption in this cat. This canine could thus be treated conservatively. In contrast, in the right mandibular canine, the process has progressed to involve the crown and most of the root has been resorbed and replaced by bone-like tissue. Extraction is not possible and coronal amputation becomes the treatment of choice
A series of full mouth radiographs is recommended for all cats presented for dental therapy. If this is not possible (eg, due to financial restrictions) then one view of each mandibular premolar/molar region can be obtained in the first instance. The mandibular third premolars (307 and 407) are the most commonly affected teeth – if radiographs show resorption of these teeth, then a full mouth series must be taken. A study has shown that, in 9/10 cats with tooth resorption, the disease would be identified in these two views. 34 This technique can, therefore, be used as a rapid screening test.
Dental radiography in discussed further in Part 1 of this Special Issue series on feline dentistry (November 2014, pages 887–899). 35
Treatment approaches
The aim of any treatment is to relieve pain, prevent progression of pathology and restore function.
It remains a matter of debate as to whether tooth resorption causes discomfort or pain to the affected individual. Based on the fact that pulpal inflammation occurs late in the disease process, it seems likely that lesions that are limited to the root surfaces and do not communicate with the oral environment are asymptomatic. However, once dentine destruction has progressed to such an extent that the process invades the pulp and/or a communication with the oral cavity has been established (ie, the enamel has been resorbed or has fractured off to reveal the dentine to the oral cavity), then discomfort and/or pain are likely as the pulp becomes inflamed. Some cats show clinical signs indicating oral discomfort or pain (eg, change in food preference for a soft rather than hard diet and/or reduced food intake), though many cats do not.
To date, there is no known treatment that prevents development and/or progression of the idiopathic type of tooth resorption. It seems unlikely that such treatment can be developed without knowledge of the cause of the pathology. Currently, the suggested methods for managing tooth resorption are:
Conservative management;
Tooth extraction;
Coronal amputation.
Restoration of the tooth surface has additionally been recommended by some for the treatment of accessible lesions that extend into the dentine and do not involve pulp tissue. Several studies, however, have shown that tooth resorption continues and the restorations are lost.23–25 Consequently, the use of restoration cannot be recommended as a major treatment technique for feline tooth resorption.
Conservative management
Conservative management consists of monitoring the lesions clinically and radiographically. This approach is recommended for lesions confined to the root that are not evident on clinical examination; that is, are only seen radiographically, without any evidence of discomfort or pain.
As most lesions are only diagnosed when pathology is extensive, conservative management is rarely indicated in the general practice situation. In most cases, extraction or coronal amputation of an affected tooth is indicated, and preoperative radiographs are mandatory to allow selection of the appropriate treatment option.
Extraction
With extraction, the whole tooth is removed. This is the gold standard, and every effort should be made to entirely extract roots affected by type 1 resorption. Teeth with tooth resorption are, however, notoriously difficult to extract. In addition to preoperative radiographs to detect the lesions and determine appropriate treatment, postoperative radiographs are required to ensure that the whole tooth has been removed.
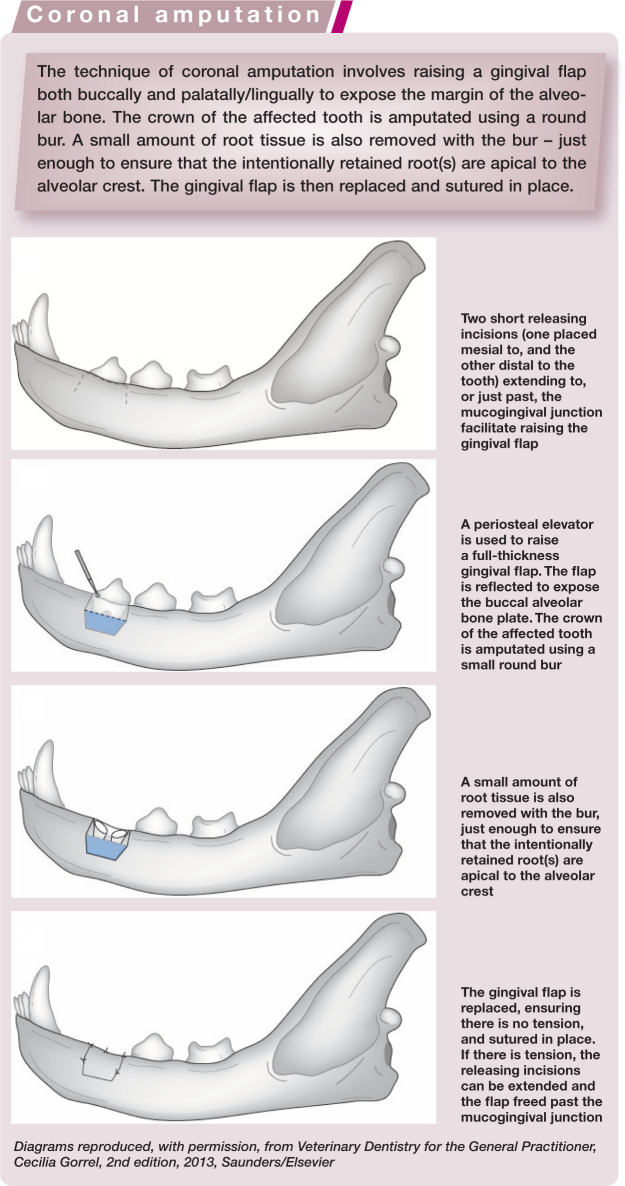
Coronal amputation
When the root has been extensively resorbed (Figure 5) it is often not possible to extract all tooth substance. Coronal amputation is then the treatment of choice. The indications for and outcome of coronal amputation have been well documented, 36 and the technique is briefly described in the box on the left. Radiographic monitoring is required at regular intervals postoperatively to ensure that the root is resorbing and that healing is uneventful.
It is important to note that coronal amputation is not indicated for type 1 tooth resorption or for teeth affected by endodontic pathology. Moreover, it cannot be recommended for cats that test positive for feline leukaemia virus or feline immunodeficiency virus.
Key Points
Tooth resorption is common in the domestic cat.
The resorptive process starts on the root surfaces and extends to involve the crown.
In the absence of routine radiography, the lesions are first noted clinically when they become obvious in the crown, often as defects at the cemento-enamel junction. This is a late-stage lesion.
Diagnosis and choice of appropriate treatment requires radiography.
The goal of treatment is relief of discomfort or pain.
In most instances, extraction of the affected tooth or coronal amputation remain the preferred treatment options.
Successful extraction and uncomplicated healing requires clinical 1 and radiographic monitoring.
Footnotes
Funding: The author received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this article.
The author does not have any potential conflicts of interest to declare.
References
- 1. Clarke DE, Cameron A. Feline dental resorptive lesions in domestic and feral cats and the possible link with diet. Proceedings of the 5th World Veterinary Dental Congress; Birmingham, UK, 1997, pp 33–34. [Google Scholar]
- 2. Verstraete FJM, Aarde Van RJ, Nieuwoudt BA, et al. The dental pathology of feral cats on Marion Island. Part II: periodontitis, external odontoclastic resorptive lesions and mandibular thickening. J Comp Pathol 1996; 115: 283–297. [DOI] [PubMed] [Google Scholar]
- 3. Levin J. Tooth resorption in a Siberian tiger. Proceedings of the 10th Annual Veterinary Dental Forum; Houston, USA, 1996, pp 212–214. [Google Scholar]
- 4. Berger M, Schawalder P, Stich H, et al. Feline dental resorptive lesions in captive and wild leopards and lions. J Vet Dent 1996; 13: 13–21. [DOI] [PubMed] [Google Scholar]
- 5. Arnbjerg J. Idiopathic dental root replacement resorption in old dogs. J Vet Dent 1996; 13: 97–99. [PubMed] [Google Scholar]
- 6. Crossley D, Dubielzig R, Benson K. Caries and odontoclastic resorptive lesions in a chinchilla (Chinchilla lanigera). Vet Ree 1997; 141: 337–339. [DOI] [PubMed] [Google Scholar]
- 7. Coles S. The prevalence of buccal cervical root resorptions in Australian cats. J Vet Dent 1990; 7: 14–16.2073359 [Google Scholar]
- 8. van Wessum R, Harvey CE, Hennet P. Feline dental resorptive lesions. Prevalence patterns. Vet Clin North Am Small Anim Pract 1992; 22: 1405–1416. [DOI] [PubMed] [Google Scholar]
- 9. Lund EM, Bohacek LK, Dahlke JL, et al. Prevalence and risk factors for odontoclastic resorptive lesions in cats. J Am Vet Med Assoc 1998; 212: 392–395. [PubMed] [Google Scholar]
- 10. Lommer MJ, Verstraete FJM. Prevalence of odontoclastic resorption lesions and periapical radiographic lucencies in cats: 265 cases (1995–1998). J Am Vet Med Assoc 2000; 217:1866–1869. [DOI] [PubMed] [Google Scholar]
- 11. Ingham KE, Gorrel C, Blackburn JM, et al. Prevalence of odontoclastic resorptive lesions in a clinically healthy cat population. J Small Anim Pract 2001; 42: 439–443. [DOI] [PubMed] [Google Scholar]
- 12. Lindskog S, Hammarström L. Evidence in favour of an anti-invasion factor in cementum or periodontal membrane. Scand J Dent Res 1980; 88: 161–163. [DOI] [PubMed] [Google Scholar]
- 13. Verstraete FJM, Kass PH, Terpak CH. Diagnostic value of full mouth radiography in cats. Am J Vet Res 1998; 59: 692–695. [PubMed] [Google Scholar]
- 14. Andreasen JO. Review of root resorption systems and models. Etiology of root resorption and the homeostatic mechanisms of the periodontal ligament. Proceedings of the International Conference on the Biological Mechanisms of Tooth Eruption and Root Resorption; Birmingham, UK, 1988, Ebesco Media, pp 9–21. [Google Scholar]
- 15. Lindskog S, Blomlöf L, Hammarström L. Repair of periodontal tissues in vitro and in vivo. J Clin Periodontal 1983; 10:188–205. [DOI] [PubMed] [Google Scholar]
- 16. Lindskog S, Blomlöf L, Hammarström L. Cellular colonization of denuded root surfaces in vivo: cell morphology in dentin resorption and cementum repair. J Clin Periodontal 1987; 14: 390–395. [DOI] [PubMed] [Google Scholar]
- 17. Andreasen JO. External root resorption: its implications in dental traumatology, paedodontics, periodontics, orthodontics and endodontics. Int Endod J 1985; 18:109–118. [DOI] [PubMed] [Google Scholar]
- 18. Andreasen JO, Kristerson L. The effect of limited drying or removal of the periodontal ligament. Periodontal healing after replantation of mature incisors in monkeys. Acta Odontol Scand 1981; 39: 1–13. [DOI] [PubMed] [Google Scholar]
- 19. Hammarström L, Blomlöf L, Lindskog S. Dynamics of dentoalveolar ankylosis and associated root resorption. Endod Dent Traumatol 1989; 5:163–175. [DOI] [PubMed] [Google Scholar]
- 20. Gold SI, Hasselgren G. Peripheral inflammatory root resorption. A review of the literature with case reports. J Clin Periodontal 1992; 19: 523–534. [DOI] [PubMed] [Google Scholar]
- 21. Ne RF, Witherspoon DE, Gutmann JL. Tooth resorption. Quintessence Int 1999; 30: 9–25. [PubMed] [Google Scholar]
- 22. DuPont G, DeBowes L. Comparison of periodontitis and root replacement in cat teeth with resorptive lesions. J Vet Dent 2002; 19: 71–75. [DOI] [PubMed] [Google Scholar]
- 23. Hopewell-Smith A. The process of osteolysis and odontolysis, or so-called ‘absorption’ of calcified tissues: a new and original investigation. The evidences in the cat. Dental Cosmos 1930; 72: 1036–1048. [Google Scholar]
- 24. Okuda A, Harvey CE. Etiopathogenesis of feline dental resorptive lesions. Vet Clin North Am Small Anim Pract 1992; 22: 1385–1404. [DOI] [PubMed] [Google Scholar]
- 25. Shigeyana Y, Grove TK, Strayhorn C, et al. Expression of adhesion molecules during tooth resorption in feline teeth: a model system for aggressive osteoclastic activity. J Dent Res 1996; 75: 1650–1657. [DOI] [PubMed] [Google Scholar]
- 26. Reichart PA, Durr U-M, Triadan H, et al. Periodontal disease in the domestic cat. J Periodont Res 1984; 19: 67–75. [DOI] [PubMed] [Google Scholar]
- 27. Gorrel C, Larsson Å. Feline odontoclastic resorptive lesions: unveiling the early lesion. J Small Anim Pract 2002; 43: 482–488. [DOI] [PubMed] [Google Scholar]
- 28. King GN, Hughes FJ. Effects of occlusal loading on ankylosis, bone and cementum formation during morphogenetic protein-2-stimulated periodontal regeneration in vivo. J Periodont 1999; 70: 1125–1135. [DOI] [PubMed] [Google Scholar]
- 29. Andersson L, Lindskog S, Blomlöf L, et al. Effect of masticatory stimulation on dentoalveolar ankylosis after experimental tooth replantation. Endod Dent Traumatol 1985; 1: 13–16. [DOI] [PubMed] [Google Scholar]
- 30. Reiter A, Mendoza KA. Feline odontoclastic resorptive lesions: an unsolved enigma in veterinary dentistry. Vet Clin North Am Small Anim Pract 2002; 32: 791–837. [DOI] [PubMed] [Google Scholar]
- 31. Zhang G, Cupp C, Kerr W. Vitamin D status in cats with and without feline odontoclastic resorptive lesions. Comp Contin Educ Pract Vet 2006; 28: 77. [Google Scholar]
- 32. Booij-Vrieling HE. Tooth resorption in cats: contribution of vitamin D and inflammation. PhD Thesis, Utrecht, The Netherlands, 2009. [Google Scholar]
- 33. Girard N, Servet E, Hennet P, et al. Tooth resorption and vitamin D3 status in cats fed premium dry diets. J Vet Dent 2010; 27: 142–147. [DOI] [PubMed] [Google Scholar]
- 34. Heaton M, Wilkinson J, Gorrel C, et al. A rapid screening technique for feline odontoclastic resorptive lesions. J Small Anim Pract 2004; 45: 598–601. [DOI] [PubMed] [Google Scholar]
- 35. Niemiec B. Feline dental radiography and radiology. A primer. J Feline Med Surg 2014; 16: 887–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. DuPont G. Crown amputation with intentional root retention for advanced feline resorptive lesions – a clinical study. J Vet Dent 1995; 12: 9–13. [PubMed] [Google Scholar]