Abstract
Practical relevance:
Malocclusion affecting cats, and treatment thereof, has not been widely described in the veterinary literature, yet is a condition seen in a growing number of breeds, often causing pain and discomfort to the patient. Recognising the problem, and certainly whether it is a hereditary problem (eg, a skeletal malocclusion), is important for the longer term health of pedigree breeds.
Clinical challenges:
If there is a malocclusion, the mouth may be painful and a thorough occlusal assessment of the conscious patient may be difficult. Occlusal assessment should always be accompanied by a thorough oral examination and, where necessary, further investigation under general anaesthesia, including dental radiography. Recognising what is normal, and what is not, can be challenging; so, too, can be determining the correct time to intervene.
Audience:
This article is intended to help fill the gap in dental education regarding the range of developmental and acquired malocclusions seen in cats. Treatment options are also briefly reviewed.
Evidence base:
The guidance contained in this article is based on a combination of the published literature, the author’s personal experience and that of colleagues.
What causes malocclusion?
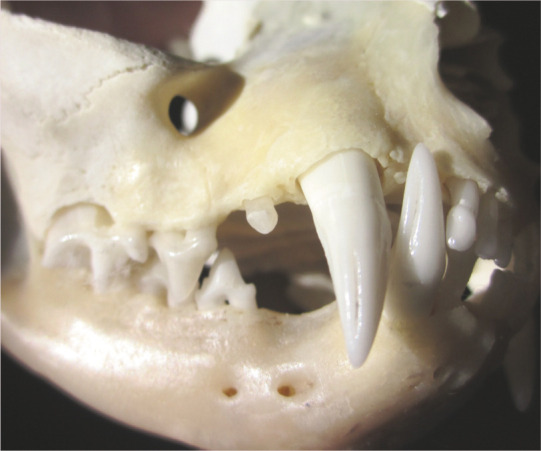
Occlusion refers to the alignment of the teeth and the relationship of the maxillary and mandibular teeth to one another. By definition, malocclusion is an abnormality in the position of the teeth. 1 Malocclusion is common in dogs, but also occurs in cats; however, this is not as extensively described in the literature. The clinical significance of a malocclusion is that it may often cause discomfort and pain to the affected animal. In some cases, it may be the direct cause of severe oral pathology (Figure 1). 2
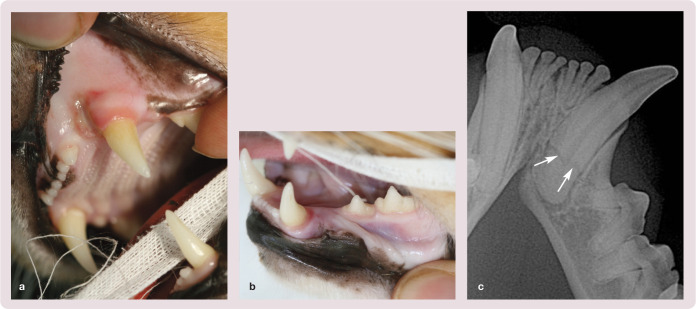
Figure 1.

Soft tissue trauma to the upper lip caused by malocclusion of the mandibular canine (404) in a 10-month-old Persian
Malocclusion can result from a discrepancy in jaw length and/or width (skeletal malocclusion), from tooth malpositioning (dental malocclusion) or a combination of the two. The development of the occlusion is determined by both genetic and environmental factors. It is known that jaw length, tooth bud position and tooth size are inherited. 3 It is also known that the development of the upper jaw, mandibles and teeth is independently regulated genetically. 3 Any change or abnormality in the regulation of these structures may result in malocclusion.
Alteration of jaw growth by a hormonal disorder (eg, acromegaly or hypersomatotropism), trauma or functional modification may result in skeletal malocclusion (Figure 2). 4 Although tooth bud position is inherited, various events during development and growth may influence the definitive tooth position. While it has been claimed that at least 50% of malocclusions are acquired and have no genetic cause, 5 there are no data to support such a claim in dogs or cats. 6 Not much research has been performed and there are no large epidemiological studies available. Specific genetic mechanisms regulating malocclusion are unknown. A polygenic mechanism is likely, however, and explains why not all siblings in successive generations are affected by malocclusion to the same degree, if at all. With a polygenic mechanism, the severity of clinical signs is linked to the number of defective genes. 2
Figure 2.
(a) Seven-month-old kitten with severe mandibular distocclusion (see page 8) and maxillary–mandibular asymmetry. The kitten had developed temporomandibular joint ankylosis after falling from a height at a young age. (b) The mandibles are too short. There is a large discrepancy between the maxillary and mandibular incisor teeth. The mandibles are also deviated to the left
The most reasonable approach suggested to evaluate whether malocclusion is hereditary or acquired is described on the right.
Evaluation of occlusion
Early recognition of a problem is essential to avoid discomfort and pain to the cat and prevent the development of further pathology.
Occlusal evaluation is part of the basic oral examination of a conscious cat. To make an evaluation, the veterinarian needs to be able to identify normal occlusion for the breed. It is important to evaluate the occlusion prior to any sedation or anaesthesia, as placement of an endotracheal tube will not allow full closure of the mouth and thus a proper occlusal assessment. It is important also to examine the whole mouth, head shape and all the teeth, and not base the judgement solely on the position of the incisor teeth. The canine and premolar relationships often give a better guide to the occlusion and also help determine whether the malocclusion is of skeletal or dental origin. 2
The shape of the head affects the position of the teeth. Malocclusion occurs in any of the three head shapes (dolichocephalic, mesocephalic, brachycephalic); it tends to be described in brachycephalic breeds (eg, Persians), 8 although the more dolichocephalic head shapes, such as the Siamese, also develop problems. The short wide muzzle of the brachycephalic breeds imposes space limitations, resulting in overcrowding or rotation of the teeth (Figure 3). Those breeds with longer, narrow muzzles usually do not have the same spatial problems as seen in the brachycephalic breeds.
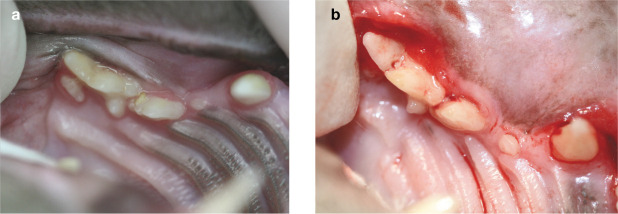
Figure 3.
(a) Space limitations in the right maxilla have led to overcrowding of the teeth in an exotic shorthair. The maxillary molar (109) is displaced to the palatal aspect of the maxillary fourth premolar (108). There is also overlap between the third and fourth maxillary premolars (107 and 108). (b) Another example of overcrowding of the maxillary premolars. This cat also has severe gingivitis; periodontal disease is more common in malaligned teeth, as these become sites of plaque stagnation and retention
Normal occlusion in the cat, which forms the basis by which feline malocclusions are classified, is described in the box on page 7.
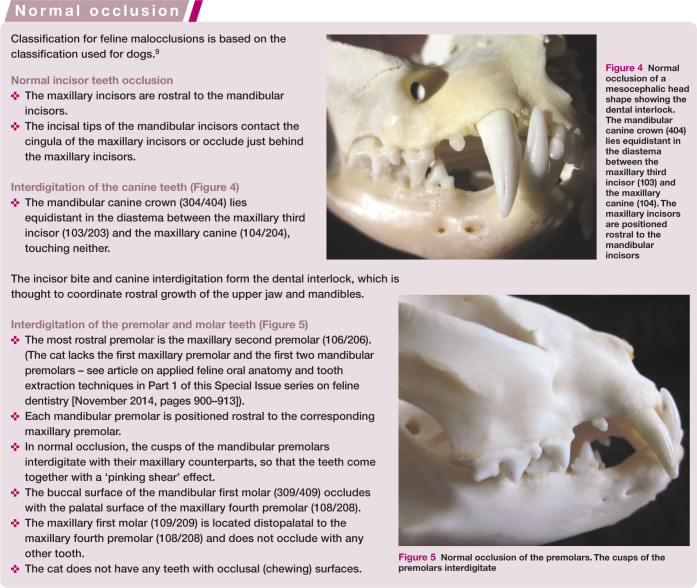
Figure 4.
Normal occlusion of a mesocephalic head shape showing the dental interlock. The mandibular canine crown (404) lies equidistant in the diastema between the maxillary third incisor (103) and the maxillary canine (104). The maxillary incisors are positioned rostral to the mandibular incisors
Figure 5.

Normal occlusion of the premolars. The cusps of the premolars interdigitate
Developmental malocclusions
Skeletal malocclusion
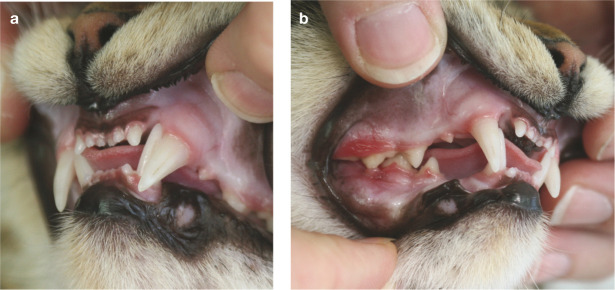
Mandibular mesiocclusion (Figure 6)
Figure 6.
Mandibular mesiocclusion. (a) The right mandibular canine (404) is trapped behind the maxillary second and third incisors (102 and 103) in this mild case. This cat also has a level incisor bite. (b) The canine teeth (304 and 404) are protruding rostral to and contacting the outer surface of the lips. (c) A more severe case where the incisors and canines are all rostral to the lips. (d) Intraoral view of the mandibular incisors of the patient in (c). The mandibles are also too narrow, causing the abnormal alignment of the incisors. Note the soft tissue indentations where the maxillary incisors are contacting the oral mucosa just distal to the mandibular canine teeth
In mandibular mesiocclusion (also referred to as mandibular prognathism, class 3 malocclusion and colloquially as ‘undershot’) the mandibles are longer than the maxillae and some or all of the mandibular teeth are rostral to their normal position. If the dental interlock prevents the mandible from growing rostrally to reach its full genetic potential, lateral or ventral bowing of the mandible may occur to accommodate the length. This results in an open bite, characterised by increased space between the premolar cusps. In addition, the caudal angle of the mandible is caudal to the temporomandibular joint to accommodate the extra length of the mandible.2,9
This type of malocclusion is most commonly seen in brachycephalic breeds such as the Persian, and is not uncommon in Maine Coons. However, any breed can be affected.
A number of variations may be seen depending on the degree of malocclusion:
Normal incisor occlusion, but the mandibular premolars are rostrally displaced, disrupting the pinking shear effect. The mandibular canine cusps (304/404) may occlude against the maxillary third incisors (103/203) (Figure 7).
Level bite: the maxillary and mandibular incisors meet at their incisal edges. The mandibular canines (304/404) may occlude against the maxillary third incisors (103/203) and the mandibular premolars are rostrally displaced. 10
Rostral crossbite (reverse scissor bite): the mandibular incisors are rostral to the maxillary incisors. The mandibular canines may be either caudal or rostral to the maxillary third incisors, and the mandibular premolars are rostrally displaced.
Figure 7.

Attrition of the right mandibular canine (404) (arrows) caused by contact from the maxillary third incisor (103). In severe cases treatment may be warranted if there is chronic pulpitis
Mandibular distocclusion
A mandibular distocclusion (also referred to as mandibular brachygnathic bite, class 2 malocclusion and colloquially as ‘overshot’) occurs when the mandibles are shorter than normal, occluding in a more caudal position relative to the maxillae.2,9 This is less common in the cat compared with the dog.
A number of variations may be seen depending on the degree of malocclusion:
The maxillary incisors are rostral to the mandibular incisors.
The maxillary canines are just caudal to, but touching the mandibular canines, level with the lower canines or rostral to the mandibular canines (Figure 8a).
The mandibular premolars are caudally displaced relative to the maxillary premolars, disrupting the pinking shear effect.
Figure 8.
Mild case of mandibular distocclusion. (a) The mandibular canine teeth are occluding against the gingiva in the diastema between the canines, causing an indentation in the mucosa. The cusp of the left mandibular canine (304) is obscured by the maxillary canine (204) and appears distal to its normal position. (b) The right mandibular canine (404) is occluding distal to normal and in a position palatal to the upper canine (104). This will result in contact with, and potential trauma to, the palatal mucosa. (Note also the penetration of the oral mucosa on the buccal aspect of the mandibular molar by the cusp of the maxillary fourth premolar [108])
The concern with this malocclusion is that the mandibular canine contacts the palatal mucosa, causing trauma. 11 If left untreated this may lead to an oronasal communication (fistula) (Figures 8b and 9).
Figure 9.
(a) Unilateral right nasal discharge caused by oronasal communication as a result of trauma to the palate from the mandibular right canine (404). (b) Severe mandibular distocclusion evident in the space between the incisors, the distal occlusion of the mandibular canines and the malocclusion of the premolars
Maxillary–mandibular asymmetry
Colloquially known as a wry bite, this asymmetry occurs if one side of the head grows more than the other side. In its mildest form a one-sided mesiocclusion or distocclusion develops. In more severe cases, a crooked head and bite develops with a deviated midline. An open bite may also develop in the incisor region such that the affected teeth are displaced vertically and do not occlude (Figure 10).
Figure 10.

Maxillary–mandibular asymmetry. There is complete asymmetry of the maxillae and mandibles with a deviated midline (arrows). Note the absence of incisors 101 and 102
Dental malocclusion
Dental malocclusion is malpositioning of a tooth or teeth where there is no obvious skeletal abnormality (ie, no jaw length or width discrepancy). Dental malocclusion may also occur in association with skeletal malocclusion. 12 The terminology for the various forms of malocclusion is described on the left.
Malocclusion of the canine teeth (Figure 11)
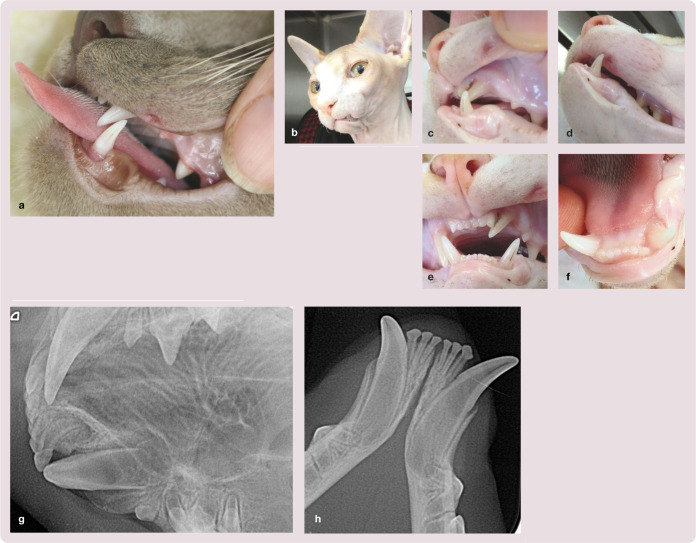
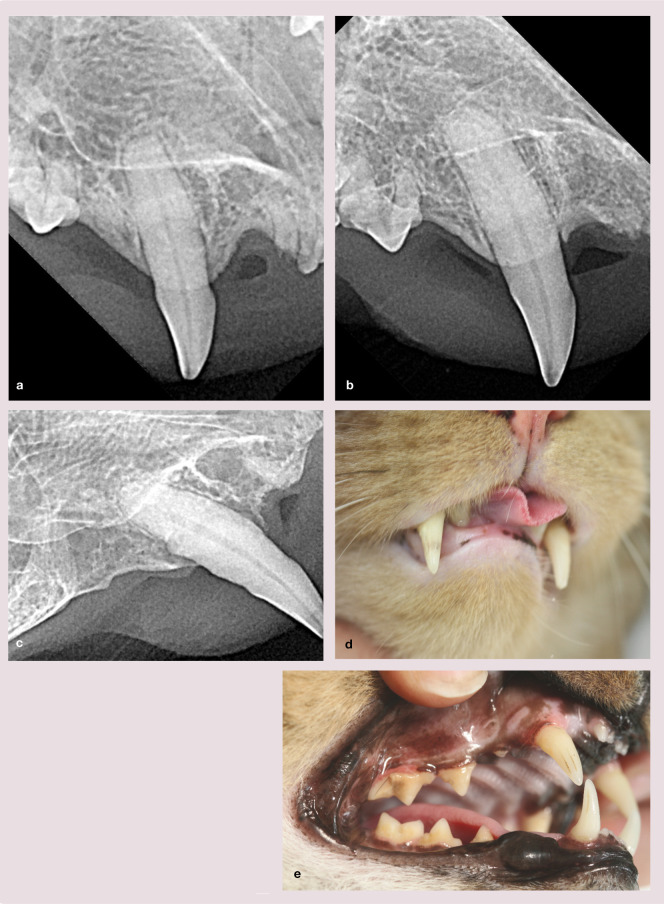
Figure 11.
Mesioversion of the maxillary canine. (a) Mesioversion of the left maxillary canine (204) in a Persian. (b–f) Mesioversion of the left maxillary canine (204) in a 6-month-old Sphynx, resulting in the lower left canine (304) flaring buccally and causing trauma to the upper lip. The tip of the maxillary canine was causing a deep indentation behind the mandibular third incisor (303). (g,h) Radiographs showing mesioversion of the maxillary canine (204) and slight rotation of the mandibular canine (304)
The most common abnormality in canine tooth position in cats is mesioversion of the maxillary canine. As a result there is often labioversion of the mandibular canine due to obliteration of the diastema between the maxillary canine and third incisor. This obliteration becomes an area of plaque stagnation, predisposing the teeth to periodontal disease. The maxillary canine may also cause trauma to the oral mucosa where it contacts the lip or, as in the case illustrated in Figure 11b–f, the mucosa around the mandibular incisors. The mandibular canine may cause trauma to the upper lip due to its abnormal angulation.
Malocclusion of the premolars and molars
Distoversion is often seen in brachycephalic breeds where there is bowing of the mandible and limited space for the premolars (Figure 12). There is often also overcrowding or rotation of the premolars and molars.
Figure 12.

Radiograph showing distoversion of the mandibular third premolar (407)
A common malocclusion resulting from impingement of the maxillary fourth premolar (108/208) on the oral mucosa around the mandibular first molar (309/409) occurs in British Shorthairs, Maine Coons and other exotic short- and longhair breeds (Figure 13). The malocclusion arises due to the slight linguoversion of the cusps of the maxillary third and fourth premolars (107 and 108; 207 and 208) and also the thicker mandibular width of the affected cat.
Figure 13.
Malocclusion of the premolars and molars. (a–c) Oral trauma resulting from impingement of the maxillary third and fourth premolars (207 and 208) on the oral mucosa around the mandibular first molar (309) in young cats. (d) The same trauma in an older cat. (e) Linguoversion of the cusps of the maxillary fourth premolars (108 and 208) (arrows). (f–h) Examples of pyogenic granulomas resulting from chronic irritation caused by the malocclusion
This impingement results in soft tissue trauma. Even in mild cases where there is gingival recession affecting the mandibular molar (309/409) or superficial ulceration, there is usually marked horizontal bone loss radiographically (Figure 14). In severe cases the ulceration may have become so chronically inflamed, that the tissue becomes more proliferative. Some cats present with a history of an oral mass that has repeatedly been excised but recurred. Histopathological diagnosis of these masses usually describes a pyogenic granuloma.
Figure 14.
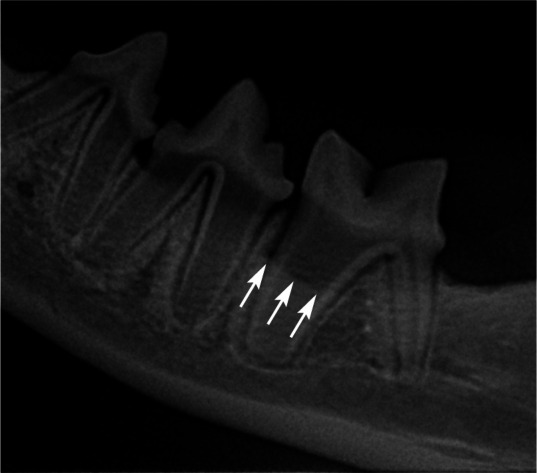
Horizontal bone loss affecting the mandibular molar (309) as a result of premolar malocclusion. The arrows indicate the edge of the bone
Pyogenic granuloma is one of the inflammatory hyperplasias seen in the oral cavity. The term is a misnomer because the lesion is unrelated to infection and in reality arises in response to various stimuli such as low-grade local irritation, traumatic injury or hormonal factors. Clinically, oral pyogenic granuloma is a smooth or lobulated exophytic lesion manifesting as small erythematous papules on a pedunculated or sometimes sessile base, which is usually haemorrhagic. The colour of the lesion may range from pink to red to purple depending on the age of the lesion (Figure 13f–h). Surgical excision and histopathology is the treatment of choice, together with elimination of the inciting cause. 13 Occlusion should always be carefully checked in cases of any caudal oral swelling.
Acquired malocclusions
An acquired malocclusion occurs as a result of a disease process or traumatic incident,4,14 and would not have been present during the cat’s development. Usually, it is a change in the cat’s appearance or inability to close its mouth, as a result of the malocclusion, that is the reason for presentation to the veterinarian.
Malocclusions resulting from trauma
Temporomandibular joint luxation (Figure 15)
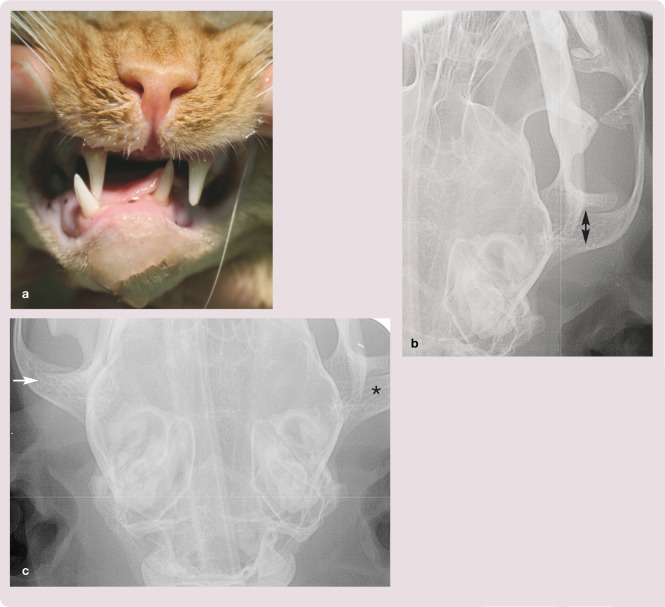
Figure 15.
Temporomandibular joint luxation. (a) Acute-onset malocclusion in a cat with a temporomandibular joint luxation. In rostrodorsal luxations, which are most common, the jaw is displaced to the side opposite the luxation. (b) Radiograph showing the luxated joint and the ‘empty’ mandibular fossa (double arrow). (c) Radiograph showing both joints, normal (arrow) and abnormal (*), for comparison
Cats typically present with an acute-onset inability to close their mouth. The condylar process is usually displaced rostrodorsally. The retroarticular process is a caudoventral extension of the mandibular fossa, which cups and prevents the caudal luxation of the condylar process. Caudal luxations can occur but usually in combination with a fracture of the retroarticular process. Luxations may be unilateral or bilateral. Unilateral joint luxation results in the mandible deviating to the side opposite the luxated joint. Diagnosis is usually confirmed radiographically.
Jaw fractures
Malocclusions can be a serious postoperative complication in cats following jaw fracture repair. Failure to properly align fracture segments, particularly in caudal mandibular fractures, results in significant deviation of the rostral segment. In severe cases the cat may not be able to close the mouth properly because of traumatically occluding maxillary and mandibular premolars and molars. If occlusion is not carefully assessed during fracture repair, serious malocclusions may not be recognised until the immediate postoperative recovery period. In less severe cases of malocclusion secondary to fracture repair there may be a traumatic occlusion between a few teeth only. These cases can be treated by selective extraction of the maloccluding teeth. This will allow the cat to close its mouth post-operatively, but is considered a significant compromise for poor surgical technique. 15
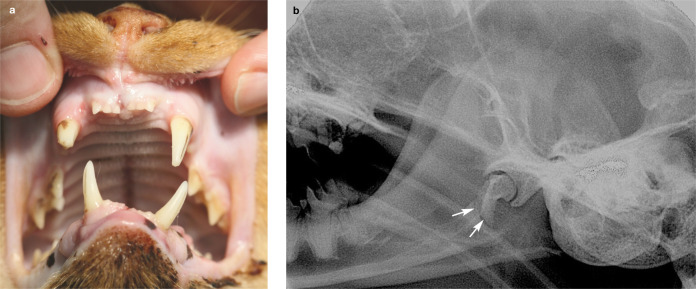
Temporomandibular joint fracture (Figure 16) Usually temporomandibular joint fractures occur in combination with other maxillofacial trauma. The jaw deviates to the side of the fracture. Radiographs are diagnostic but computed tomographic imaging is more useful in determining the extent of all the injuries.
Maxillary fractures (Figure 17) Caudal palatine bone fractures may result in the dental arch tipping palatally. If undiagnosed or untreated, this results in the maxillary premolar cusps contacting the mandibular premolars and molar, and thus inability to close the mouth. In severe cases, a caudal crossbite may result. Midline palatal fractures from high-rise falls or road traffic accidents may also result in a malocclusion.
Mandibular fractures (Figure 18) Most caudal mandibular fractures result in compression of the fracture segment and cause the rostral mandible to deviate towards the side of the fracture.
Figure 16.
Temporomandibular joint fracture. (a) Deviation of the mandibles towards the side of the fracture, resulting in a malocclusion and inability to close the mouth. (b) Lateral oblique radiograph showing a fracture (arrows) through the condylar neck
Figure 17.

Caudal palatine bone fracture resulting in the left maxillary dental arch tipping palatally
Figure 18.
Mandibular fracture. (a) Right deviation of the mandibles and soft tissue trauma of the caudal oral mucosa raises the suspicion of a caudal mandibular fracture. (b) Bilateral temporomandibular joint fractures. There is also a right caudal mandibular fracture. (c) Intraoral radiograph showing a caudal mandibular fracture extending from the distal aspect of the mandibular molar (409) (arrow)
Tooth luxation (Figure 19)
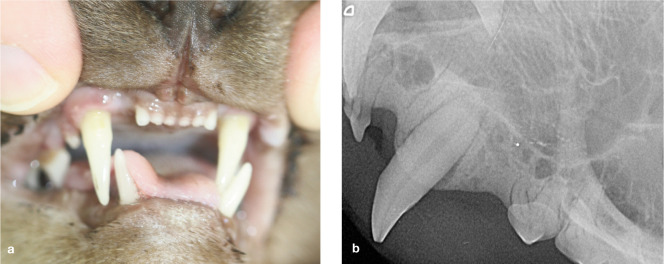
Figure 19.
(a) Acute-onset malocclusion in a 7-year-old domestic shorthair. (b) Radiograph showing lateral luxation of the mandibular canine (404) with a fracture of the alveolar socket
Tooth luxation refers to a tooth that is partially or completely displaced from its alveolar support. Luxation can occur in a horizontal, lateral or vertical direction. The cause of luxation is usually trauma, such as a road traffic accident or a fall from a height, which results in damage to the supporting apparatus of the tooth allowing it to become mobile. The tooth may appear shorter than normal or longer than normal, and may be tipped outward towards the lip or inward towards the palate or tongue.
Cats will present with an acute-onset malocclusion. Tooth luxations represent true dental emergencies. The duration of luxation is an important factor for success of treatment as the cells of the periodontal ligament need to remain viable if the tooth is to be re-implanted. For the best chances of success the tooth should be re-implanted within 60 mins of avulsion. If the tooth is stored in a suitable medium (eg, low fat milk) then it can still be successfully re-implanted provided it is within 3 h of avulsion. 16 Often the vascular supply to the pulp is severely damaged, resulting in the need for endodontic treatment following re-implantation.
Tooth root fracture (Figure 20)
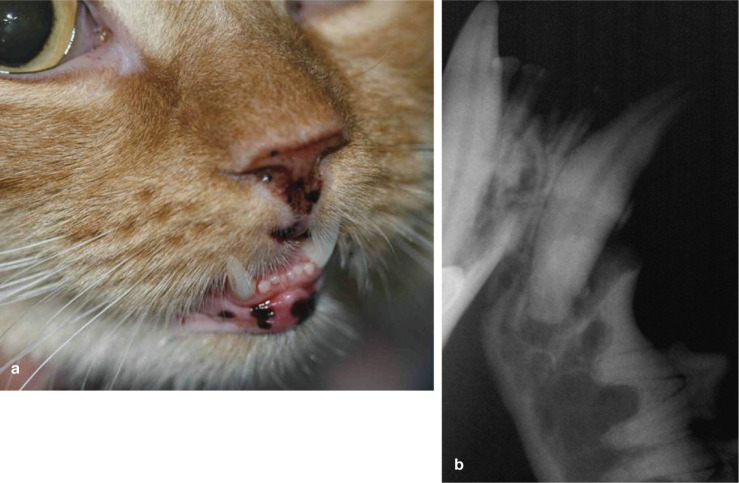
Figure 20.
Tooth root fracture. (a) Ulceration of the gingiva secondary to malocclusion of the mandibular canine in a 2-year-old Bengal that had fallen from a height. (b) Bruising of the oral mucosa just rostral and distal to the frenulum. (c) Radiograph showing a horizontal root fracture (arrows) of the mandibular canine (304) and an increase in the periodontal ligament space where the tooth has been partially luxated
Root fractures are a relatively infrequent dental injury, occurring usually as a result of trauma. When a root fractures horizontally, the coronal segment is displaced to a variable degree, but generally the apical portion of the root is not displaced. The extent of displacement usually indicates the location of the fracture and can vary from no displacement to severe displacement mimicking a luxation injury.
If a root fracture is suspected, more than one dental radiograph is usually required at differing angles to identify the fracture. 17
Malocclusions resulting from a disease process
Idiopathic extrusion of canine teeth (Figure 21)
Figure 21.
Extrusion of canine teeth. (a–c) Radiographs of the right maxillary canine (104). Radiograph (a) shows normal bone attachment. In (b) and (c) there is supereruption of the tooth. Note the increased distance between the alveolar margin and cemento-enamel junction in the absence of horizontal or vertical alveolar bone loss in (b). In (c) there is vertical and horizontal bone loss affecting the canine; this case was secondary to periodontal disease. (d) Clinical photograph showing supereruption of the maxillary canines in a geriatric domestic shorthair secondary to periodontal disease. (e) Clinical photograph of a periodontally healthy maxillary canine showing supereruption. There is an increased distance between the gingival margin and the cemento-enamel junction
Idiopathic extrusion, also referred to as supraeruption, supereruption or pathologic migration, refers to excessive extrusion of unknown origin. Extrusion describes movement of a tooth beyond its normal occlusal plane. Abnormal extrusion of canine teeth is often noted in middle-aged and geriatric domestic cats. Teeth severely affected by periodontal disease can undergo extrusion as part of the body’s response to local infection. It is also reported that tooth extrusion is linked to, or may be caused by, factors similar to those responsible for the development of tooth resorption. 18
Extrusion of the maxillary canine teeth becomes clinically apparent when there is an increased distance between the alveolar margin and cemento-enamel junction in the absence of horizontal or vertical alveolar bone loss. 18
Periodontal disease (Figure 22)
Figure 22.
(a) Acute-onset malocclusion and inability to close the mouth in an 8-year-old Burmese cat. The left maxillary canine (204) is occluding more palatally, resulting in contact on the mandibular canine and causing the mandibles to deviate. (b) Radiograph showing vertical bone loss around the maxillary canine root. This will allow slight movement of the tooth, resulting in the malocclusion
Periodontal disease results in loss of attachment of the tooth to its supporting structures. 19 Vertical bone loss and loss of the periodontal ligament of the maxillary canine tooth may result in mobility and, as a result, malocclusion of the tooth. The problem may be compounded by extrusion of the tooth, which complicates and interferes with closure of the cat’s mouth.
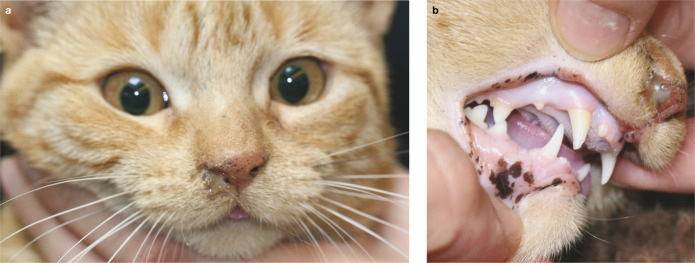
Oral neoplasia (Figure 23)
Figure 23.
(a) Sudden-onset malocclusion in a 15-year-old domestic shorthair secondary to squamous cell carcinoma. (b) Radiograph of the mandible showing bony involvement of the tumour
Space-occupying lesions or bony destructive lesions result in displacement of teeth. Cats will often present when the owner notices a change in appearance; this is usually facial swelling or asymmetry, but may sometimes involve a malaligned tooth.
Squamous cell carcinoma (SCC) is the most common oral tumour affecting the cat. 20 It primarily occurs on the tongue or gingiva but can affect any oral soft tissues. If the mass occurs on the gingiva, teeth may become mobile and displaced due to bony destruction. Feline oral SCC carries a generally poor prognosis, but longer survival times have been reported with a combination of aggressive local resection and radiation therapy. 21
Malocclusion following extraction
Canine malocclusion (Figure 24)
Figure 24.
Canine malocclusion. (a) Ulceration resulting from penetration of the mandibular canine tooth (404) following extraction of the maxillary canine (104). (b) Keratinised area from a chronic lesion. Many of these cases do not need treatment if the cat seems comfortable. (c,d) Lip ulceration secondary to loss of the maxillary crown. Previously this trauma was only described post-extraction due to loss of the buccal bone plate; however, it is actually the crown of the maxillary canine that prevents contact of the mandibular canine and upper lip. Photograph (d) shows the maxillary canine (104) fractured at the gingival margin
The presence of the crown of the maxillary canine tooth keeps the upper lip away from the diastema where the mandibular canine fits into its normal occlusion. This allows the cat to close its mouth without the mandibular canine cusp becoming trapped or catching on the upper lip. In cases where the maxillary canine tooth is absent (eg, post-extraction), the mandibular canine can traumatise the lip, sometimes resulting in further treatment being required. 22 In some cases the cat learns to lick the lip out of the way so as to close the mouth without the lip becoming trapped; in other cases, ulceration and discomfort persist.
In the first instance, medical management to reduce swelling and discomfort may allow the ulceration to heal with only a small area of hair loss/scar tissue remaining. However, if the irritation persists, treatment options to resolve the problem are either to extract the lower canine or refer to a veterinary dentist for crown height reduction and endodontic therapy.
Lip entrapment is one reason why endodontic treatment for fractured maxillary canines in cats is preferable to extraction; although the problem is not always prevented if too much of the fractured tooth crown has been lost.
Premolar malocclusion (Figure 25)
Figure 25.
Premolar malocclusion. (a) Trauma to the mandibular oral mucosa caused by impingement of the maxillary third and fourth premolars (207 and 208). (b,c) Examples of cases where chronic irritation from the occlusal trauma has resulted in the development of a pyogenic granuloma
Following extraction of the mandibular molar in cats it is not uncommon to see trauma to the mandibular oral mucosa caused by impingement of the maxillary fourth premolar. The trauma may result in ulceration or, in more severe cases, a pyogenic granuloma as described earlier.
Treatment of malocclusions
Malocclusions may not always need treatment and, indeed, there may be ethical considerations involved (see box below). Generally, intervention is only required if the malocclusion is causing the cat discomfort or resulting in pathology, such as soft tissue ulceration. Certain malocclusions are considered ‘normal’ for the breed, yet still require treatment if resulting in oral trauma. If the malocclusion is an acquired malocclusion, a thorough oral assessment, together with radiography, needs to be performed to identify underlying pathology.
In dogs, primary teeth involved in malocclusion should be extracted as early as possible (ie, at 6–8 weeks of age). This will allow the maxilla and mandible to develop to their full genetic potential independently before the permanent dental interlock forms. Extracting maloccluding primary teeth before eruption of their permanent counterparts is called interceptive orthodontics. It will prevent dental interlock-induced malocclusion from developing. In the author’s experience, very few cats in the UK present with malocclusions involving the primary teeth so interceptive orthodontics is rarely performed (and is mentioned here simply for completeness).
Malocclusion of the secondary dentition that is causing discomfort and pathology needs treatment. The goal of treatment is to ensure that the cat has a comfortable, functional bite, and the options available are orthodontics (tooth movement), crown shortening or extraction. 23
Orthodontic treatment
Orthodontic movement of teeth can be described as prolonged application of intermittent or continuous pressure to the tooth, resulting in movement of the tooth as the bone around it remodels. Most orthodontic movements in cats and dogs involve mainly tipping forces. Possible complications to orthodontic movement of teeth include endodontic disease, external root resorption, tooth mobility and pain, as well as failure to move the tooth or to maintain its position once the device has been removed. In short, the outcome of an orthodontic procedure is rarely predictable and frequent monitoring based on clinical signs and radiography is needed.
The challenge with orthodontics in cats is to keep the small-base, direct-bonded brackets on the teeth without causing too much oral discomfort or trauma that could result in an anorexic patient. Certain appliances, such as an acrylic inclined bite plane, are better tolerated compared with brackets in the feline patient.
Examples of appropriate orthodontic treatment include using an inclined plane to move a maloccluding mandibular canine to avoid contact with the palatal mucosa (Figure 26), 11 or using orthodontic buttons and elastics to correct mesioversion of a maxillary canine.
Figure 26.
(a,b) The mandibular canine (404) in this 7-month-old Maine Coon is resulting in trauma to the palatal mucosa on the palatal aspect of the maxillary second and third incisors (102 and 103). (c) An acrylic inclined plane fitted to the maxillary canines is used to gently move the maloccluding mandibular canine (404) into the correct position
Crown height reduction with and without endodontic treatment
When a malpositioned tooth impinges on the opposing gingiva or contacts soft tissue, resulting in trauma, crown height reduction and restoration may be a suitable treatment option to return the cat’s mouth to comfort and maintain function. The disadvantage of this procedure is that it should be performed under strict radiographic control if pulp exposure is to be avoided. If the pulp is exposed, the best results following vital pulp therapy would be in the hands of an experienced veterinary dentist, so referral to a specialist should be considered. In a mature tooth (root formation complete) a full pulpectomy would be advised to reduce the risk of composite failure (restoration failure) or ongoing pulpitis (pulp inflammation).
An example of where crown height reduction and endodontic treatment is carried out is when there is impingement of the mandibular canine on the upper lip (Figure 27).
Figure 27.
Treatment by crown height reduction. (a) Impingement of the mandibular canine (404) on the upper lip, causing trauma. (b) Crown height reduction of a mandibular canine (404) with endodontic treatment. (c) The maxillary canine (204) has occluded in an abnormal position, causing trauma to the lower lip. (d) Crown height reduction and endodontic treatment of the canine tooth (204)
In mild cases of premolar impingement, odontoplasty (changing the tooth shape to reduce the sharp penetrating cusp), avoiding pulp exposure, followed by application of a dentinal tubule sealer can be carried out (Figure 28).
Figure 28.

(a) Premolar malocclusion resulting in soft tissue trauma. (b) Clinical photograph taken following an odontoplasty procedure which has been performed to remove the sharp cusps from the third and fourth premolars (207 and 208)
Extraction
Extractions can be carried out by the veterinarian, as opposed to the need for referral to a veterinary dentist. Referral may still, however, be required for complex cases or where there is an unknown underlying cause for the malocclusion. An advantage of extraction as a treatment option for malocclusion, compared with orthodontic or endodontic treatment, is that fewer anaesthetic procedures are required and there is usually not a need for long term follow-up.
Key Points
Early intervention is key to preventing soft tissue trauma and discomfort in cats with malocclusion.
Any potential underlying cause(s) should be identified.
Breeds in which malocclusions occur more commonly should be recognised and continued breeding from cats that present with skeletal malocclusion discouraged.
An understanding of the potential complications of procedures such as extraction or jaw fracture repair is required. Referral to a specialist should be considered where necessary.
Footnotes
Funding: The author received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
The author does not have any potential conflicts of interest to declare.
References
- 1. Wiggs RV, Lobprise HB. Glossary of terms. In: Gorrel C. (ed). Veterinary dentistry, principles and practice. Philadelphia: Lippincott-Raven, 1997, pp 653–658. [Google Scholar]
- 2. Gorrel C. Occlusion and malocclusion. In: Veterinary dentistry for the general practitioner. Philadelphia: Saunders, 2004, pp 35–46. [Google Scholar]
- 3. Stockard CR. The genetic and endocrinic basis for differences in form and behaviour. In: The American anatomical memoirs no. 19. Philadelphia: The Wistar institute of Anatomy and Biology, 1941, pp 150–153. [Google Scholar]
- 4. Hennet PR, Harvey CE. Craniofacial development and growth in the dog. J Vet Dent 1992; 9: 11–18. [PubMed] [Google Scholar]
- 5. Shipp AD, Fahrenkrug P. Orthodontics. In: Practitioner’s guide to veterinary dentistry. Beverley Hills: Dr Shipp’s Laboratories, 1992, pp 117–147. [Google Scholar]
- 6. Hennet PR. Orthodontics in small carnivores. In: Crossley DA, Penman S. (eds). Manual of small animal dentistry. Cheltenham: BSAVA, 1995, pp 182–192. [Google Scholar]
- 7. Hennet PR, Harvey CE. Diagnostic approach to malocclusions in dogs. J Vet Dent 1992; 9: 23–26. [PubMed] [Google Scholar]
- 8. Frost P, Williams CA. Feline dental disease. Vet Clin North Am Small Anim Pract 1986; 16: 851–873. [DOI] [PubMed] [Google Scholar]
- 9. American Veterinary Dental College. Classification of dental occlusion in dogs. AVDC Nomenclature Committee. http://www.avdc.org/nomenclature.html#occlusion. (2012, accessed February 2014).
- 10. Sarkiala-Kessel E. Malocclusion in a cat. J Vet Dent 2001; 18: 76–77. [DOI] [PubMed] [Google Scholar]
- 11. Wetering A. Orthodontic correction of base narrow mandibular canine tooth in a cat. J Vet Dent 2007; 24: 22–28. [DOI] [PubMed] [Google Scholar]
- 12. Bellows J. Oral pathology. In: Feline dentistry – oral assessment, treatment and preventative care. Iowa: Wiley Blackwell, 2010, pp 131–135. [Google Scholar]
- 13. Jafarzadeh H, Sanatkhani M, Mohtashan N. Oral pyogenic granuloma: a review. J Oral Sci 2006; 48: 167–175. [DOI] [PubMed] [Google Scholar]
- 14. Eisner E. Malocclusions in cats and dogs: recognizing dental alignments. Vet Med 1998; 83: 1006–1032. [Google Scholar]
- 15. Manfra Marretta S. Maxillofacial fracture complications. In: Verstraete F, Lommer M. (eds). Oral and maxillofacial surgery in dogs and cats. Philadelphia: Saunders Elsevier, 2012, p 338. [Google Scholar]
- 16. Gracis M. Management of periodontal trauma. In: Verstraete F, Lommer M. (eds). Oral and maxillofacial surgery in dogs and cats. Philadelphia: Saunders Elsevier, 2012, pp 201–213. [Google Scholar]
- 17. Trope M, Blanco L, Chivian N, et al. The role of endodontics after dental traumatic injuries. In: Cohen S, Hargreaves K. (eds). Pathways of the pulp. 9th ed. Missouri: Elsevier, 2006, pp 625–627. [Google Scholar]
- 18. Lewis JR, okuda A, Shofer F, et al. Significant association between tooth extrusion and tooth resorption in domestic cats. J Vet Dent 2008; 25: 86–95. [DOI] [PubMed] [Google Scholar]
- 19. Carranza FA, Camargo PM. Periodontal response to external forces. In: Newman MG, Takei HH, Carranza FA. (eds). Carranza’s clinical periodontology. Philadelphia: WB Saunders, 2002, pp 371–383. [Google Scholar]
- 20. Withrow SJ, Vail DM. Cancer of the gastrointestinal tract. In: Small animal clinical oncology. 4th ed. Missouri: Saunders Elsevier, 2007, pp 455–473. [Google Scholar]
- 21. McEntee M. Clinical behavior of nonodontogenic tumours. In: Verstraete F, Lommer M. (eds). Oral and maxillofacial surgery in dogs and cats. Philadelphia: Saunders Elsevier, 2012, pp 388–392. [Google Scholar]
- 22. Verstraete F. Exodontics. In: Slatter DG. (ed). Textbook of small animal surgery. 3rd ed. Philadelphia: WB Saunders, 2003, pp 2696–2709. [Google Scholar]
- 23. Bellows J. Treatment of occlusion disorders. In: feline dentistry – oral assessment, treatment and preventative care. Iowa: Wiley Blackwell, 2010, pp 269–279. [Google Scholar]