Abstract
Background
Supportive care (SC) refers to the prevention and management of complications of cancer and its treatment. While it has long been recognized as an important cancer care delivery component, a high proportion of patients face unaddressed SC needs, calling for innovative approaches to deliver SC.
Objective
The objective of this master protocol is to evaluate the implementation of different integrated proactive SC pathways across the cancer care continuum in our institution (Gustave Roussy, Villejuif, France). Pathways studied in this master protocol may occur shortly after diagnosis to prevent treatment-related burden; during treatment to monitor the onset of toxicities and provide timely symptom management; and after treatment to improve rehabilitation, self-management skills, and social reintegration.
Methods
This study is guided by the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework. The primary objective is to evaluate the impact of SC pathways on patients’ distress and unmet needs after 12 weeks, measured by the National Comprehensive Cancer Network’s Distress Thermometer and Problem List. Secondary objectives will focus on the pathways (macrolevel) and each SC intervention (microlevel), evaluating their reach (administrative data review of the absolute number and proportion of clinical and sociodemographic characteristics of patients included in the pathways); short-term and long-term efficacy through their impact on quality of life (EQ-5D-5L and the 30-item European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire) and symptom burden (MD Anderson Symptom Inventory, Hospital Anxiety and Depression Scale, Insomnia Severity Index, and 22-item European Organization for Research and Treatment of Cancer Sexual Health Questionnaire); adoption by patients and providers (administrative data review of SC referrals and attendance or use of SC strategies); barriers to and leverage for implementation (surveys and focus groups with patients, providers, and the hospital organization); and maintenance (cost-consequence analysis). Pilot evaluations with a minimum of 70 patients per pathway will be performed to generate mean Distress Thermometer scores and SDs informing the calculation of formal sample size needed for efficacy evaluation (cohorts will be enriched accordingly).
Results
The study was approved by the ethics committee, and as of February 2024, a total of 12 patients were enrolled.
Conclusions
This study will contribute toward innovative models of SC delivery and will inform the implementation of integrated SC pathways of care.
Trial Registration
ClinicalTrials.gov NCT06479057; https://clinicaltrials.gov/study/NCT06479057
International Registered Report Identifier (IRRID)
PRR1-10.2196/52841
Keywords: care delivery, pathway of care, oncology, supportive care, quality of life, cohort study
Introduction
Background
Due to the rapid evolution of modern anticancer treatment, cancer is often considered a chronic disease. Novel treatments deliver longer survival but frequently with a range of acute toxicities and long-term side effects, which negatively impact the quality of life and necessitate ongoing health service use [1].
Supportive care (SC) is defined as the prevention and management of adverse effects of cancer and its treatment [2,3]. This includes management of physical and psychological symptoms and side effects across the continuum of cancer experience, from diagnosis through anticancer treatment to posttreatment care [2,3]. Enhancing rehabilitation, secondary cancer prevention, survivorship, and end-of-life care are integral to SC. Financial and social issues that may be associated with risk of toxicities or access to SC should also be considered [2,4-6].
While SC has long been recognized as an important component of cancer care delivery, published evidence suggests an ongoing, high burden of unaddressed needs across all SC domains for many patients, at all phases of cancer experience [7,8]. A systematic review of 57 studies quantifying patients’ unmet SC needs across different tumor types and phases of the cancer continuum reported that, although highly variable, these could reach 93% for unmet informational needs, 89% for unmet physical needs, 89% for unmet psychosocial needs, 63% for unmet sexuality needs, and 51% for unmet spiritual needs, with many of these unmet needs experienced concurrently [9]. In addition, while unmet needs appeared to be highest and most varied during treatment, a greater number of individuals were likely to express unmet needs after the end of treatment compared to any other time [9]. More specifically, long-term physical and behavioral symptoms (fatigue, neuropathy, weight management, emotional distress, insomnia, and cognition decline), intimacy-related concerns, financial and work-related concerns, and provider-communication and information needs have been highly cited as common unmet needs across the cancer care continuum [10].
A recent study aimed to identify and synthesize patient’s views about areas where they need support through cancer care [8]. Quantitative and qualitative studies were included, and the authors presented 3 lines of work for managing chronic illness (“illness-work,” “everyday-life work”, and “biographical work”), including a group of key common patient needs. For “illness-work,” the key needs identified were understanding their illness and treatment options, knowing what to expect, communication with health care professionals, and staying well. With regard to “everyday-life work”, patients wanted to maintain a sense of normalcy and look after their loved ones. For “biographical work,” patients commonly struggled with the emotional impact of illness and a lack of control over their lives. Spiritual, sexual, and financial problems were less universal. For some types of support, demographic factors influenced the level of need reported.
Importantly, there is evidence demonstrating that unmet SC needs are associated with inferior quality of life, increased symptom burden, and worse clinical outcomes such as emergency visits and hospitalizations [11-13].
Although a large body of evidence exists on interventions addressing SC needs in patients with cancer [14], implementation of effective interventions in clinical practice has been suboptimal [7,15]. The delivery of SC requires a multidisciplinary approach, involving the screening, assessment, management, treatment of side effects, symptoms, and needs of patients with cancer, carriers, and family [2]. A recent framework highlighted the importance of perceiving SC as a way of understanding, planning, delivering, and evaluating integrated cancer care, where each component of cancer care and treatment occur within a SC framework, instead of considering it as a subspecialty, discipline, or series of interventions [16]. Ideally, SC needs to be delivered in all health care settings at all steps of the cancer pathway from diagnosis to survivorship and end of life [2]. Most commonly, SC is primarily delivered in everyday practice by treating oncologists who during their routine oncological consultation may detect SC needs and refer patients to multiple multidisciplinary strategies such as palliative care, social work, rehabilitation, psycho-oncology, and integrative medicine. However, this approach can lead to heterogeneous access and fragmented care [16]. An integrated SC delivery model has been proposed to overcome these challenges [17]. In this model, longitudinal specialist SC is provided by an interdisciplinary SC team, with timely involvement of other teams (eg, cancer pain service and rehabilitation) when the need arises [17]. For patients who have completed curative treatments and are on surveillance, the survivorship care team may be the main SC service [18]. Key features of this model include universal referral, systematic SC needs screening, tailored specialist involvement and evidence-based symptom management strategies, streamlined care, and collaborative teamwork [17]. In addition, several modifiable risk factors for toxicity and quality of life deterioration have been identified across the cancer care continuum [19-23]. Therefore, an integrated preventive strategy that anticipates tailored SC services to patients at higher risk of toxicity or quality of life deterioration has been suggested [22] and requires further evaluation of its implementation and impact on patient-reported outcomes.
Objectives
At our institution (Gustave Roussy, Villejuif, France), several SC resources were co-designed and deployed in clinical practice (Figure 1 and Textbox 1), including integrated SC pathways of care and specific SC referrals. In Gustave Roussy, the integrated SC pathways include a formal SC needs assessment and tailored SC referrals and resources according to patient’s needs. These pathways are offered to patients across the entire cancer care continuum: shortly after diagnosis to prevent treatment-related burden; during treatment to monitor and manage treatment-related toxicities; and after treatment to accelerate rehabilitation, social integration, and self-management. This study will evaluate the implementation of integrated and proactive SC pathways in oncology.
Figure 1.
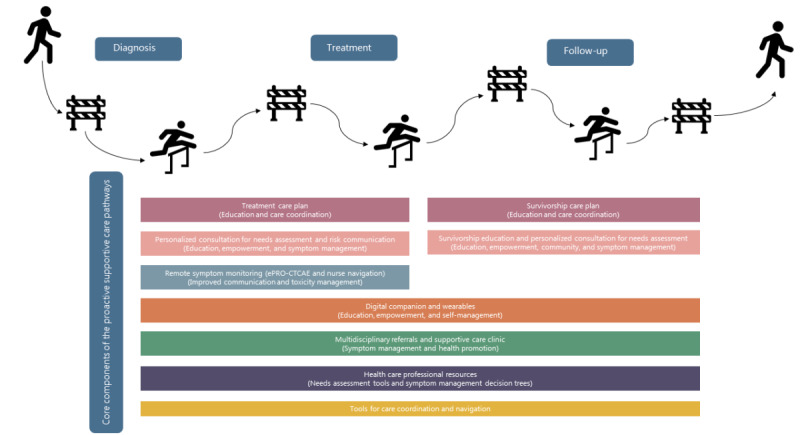
Examples of core supportive care components of supportive care pathways across the cancer care continuum. ePRO-CTCAE: electronic patient-reported outcomes version of the common terminology criteria for adverse events.
Current supportive care interventions and referrals available at Gustave Roussy.
Integrated supportive care pathways
-
Shortly after diagnosis
Supportive care pathway for preventing treatment-related burden after breast cancer (eg, cancer-related fatigue and cluster of behavioral symptoms)
Supportive care pathway to prevent treatment-related burden for patients considered vulnerable with brain, head and neck, thoracic, and neuroendocrine tumors
-
During treatment
Remote symptom monitoring pathway with weekly electronic patient-reported outcomes (ePROs) and nurse navigation (for patients during active systemic treatment with chemotherapy, immunotherapy, or targeted agents)
Immunotoxicity management pathway
-
After treatment
Proactive survivorship care pathway (breast cancer and others)
Supportive care interventions available at the institution
-
Digital health tools
Remote monitoring (ePRO system) for patients receiving active treatment (chemotherapy, target agents, and radiotherapy)
Mobile app delivering education and self-management advice (articles, videos, and podcasts)
Internet-delivered self-care programs of evidence-based validated supportive care strategies (physical activity, mindfulness, yoga, and cognitive behavioral therapy)
ePRO data collection web system for research studies
-
In-person multidisciplinary supportive care resources at the supportive care clinic
Adapted physical activity program
Mindfulness program
Acupuncture consultations
Hypnosis consultations
Sophrology program
Art-therapy program
Socioesthetician follow-up
Return-to-work educational seminars
Diet and nutrition educational seminars
Survivorship educational seminars
Individualized risk of toxicity assessment
-
Community-based survivorship resources
Nutrition follow-up
Adaptive physical activity
Psychological support
-
In-person multidisciplinary supportive care resources at the hospital
Nutritionist follow-up
Palliative care follow-up
Addiction treatment programs (tobacco and alcohol)
Social services follow-up
Organ specialists for toxicity management of cancer therapies (cardiologist, pneumologist, endocrinologist, neurologist, rheumatologist, etc)
Day hospital for acute toxicity management
Rehabilitation hospital
Psychologist or psychiatrist follow-up
Pain evaluation and management at pain clinic
Sexologist follow-up
Speech therapy
Ostomy nurses
Supportive care nurses
Thrombosis evaluation team
Bone metastases evaluation team
Methods
Study Design and Interventions
The study design is a master protocol [24] for a prospective cohort study focused on evaluating the implementation of integrated proactive pathways of SC at Gustave Roussy. This master protocol study is conducted with a collection of substudies for each SC intervention that share key design components and operational aspects. Data collection will allow the evaluation at a macro level (integrated SC pathway, including SC needs assessment and tailored multidisciplinary referrals) and at a micro level (separated for each SC intervention).
The Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework [25] was used to guide the definition of study objectives and the data collection plan. As a framework, RE-AIM has both individual-level and staff- or setting-level dimensions, including Reach and Effectiveness (individual-level), Adoption and Implementation (staff and setting levels), and Maintenance (both individual and staff or setting levels) [26].
Patients will be clinically monitored from the date of their screening visit until the date of the last visit, loss to follow-up, withdrawal of consent, disease progression, death, or end of study, whichever occurs first. There are no treatments prescribed to the patients other than those prescribed in routine practice.
Patients will be prospectively entered in the study after checking for eligibility criteria and signature of the informed consent form. Data will be collected at baseline, 4 weeks, 12 weeks, and 24 weeks. For patients participating in the immunotoxicity management pathway, data will also be collected at 1 month. Study participants will be asked to complete the study web-based questionnaires using the WeShare platform’s electronic patient-reported outcomes module [27,28]. Identifying data (personal data) are recovered at the time of the creation of the WeShare account and will be separated from the study data. The investigation plan is detailed in Table 1. In-paper questionnaires will also be available if preferable by the patient.
Table 1.
Investigation schedule.
|
|
Electronic case report form creation | Baseline visit | Follow-up month 1a week 4 (–2 weeks to +2 weeks) | Follow-up month 3 week 12 (–2 weeks to +2 weeks) | Follow-up month 6 week 24 (–2 weeks to +2 weeks) | |
| Prescreening informed consent | ✓ |
|
|
|
|
|
| Screening informed consent |
|
✓ |
|
|
|
|
| Eligibility criteria |
|
✓ |
|
|
|
|
| Clinical datab |
|
✓ | ✓ | ✓ | ✓ | |
| Supportive care resources proposedc |
|
✓ |
|
|
|
|
| Attendance and adoption data to supportive care resources proposedd |
|
|
|
✓ | ✓ | |
| Out of schedule use of hospital services (emergency visits, extra consultations, and hospitalization) |
|
|
|
✓ |
|
|
| Resilience mobile app use datae |
|
✓ | ✓ | ✓ | ✓ | |
| Electronic patient-reported outcomesf | ||||||
|
|
Sociodemographic questionnaire |
|
✓ |
|
|
|
|
|
National Comprehensive Cancer Network’s Distress Thermometer and Problem List |
|
✓ | ✓ | ✓ | ✓ |
|
|
5-level EQ-5D version |
|
✓ | ✓ | ✓ | ✓ |
|
|
MD Anderson Symptom Inventory |
|
✓ | ✓ | ✓ | ✓ |
|
|
Patient Assessment of Chronic Illness Care |
|
|
|
✓ |
|
|
|
Health Literacy Questionnaire |
|
✓ |
|
|
|
|
|
Gustave Roussy vulnerability questionnaireg |
|
✓ |
|
|
|
|
|
30-item European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaireh |
|
✓ |
|
✓ | ✓ |
|
|
Hospital Anxiety and Depression Scalei |
|
✓ |
|
✓ | ✓ |
|
|
Insomnia Severity Index j |
|
✓ |
|
✓ | ✓ |
|
|
22-item European Organization for the Research and Treatment of Cancer Sexual Health Questionnairek |
|
✓ |
|
✓ | ✓ |
|
|
Experience and satisfaction questionnairesl |
|
|
|
✓ |
|
| Qualitative research | ||||||
|
|
Focus groupsm |
|
|
|
✓ |
|
aFor patients included in the immune toxicity management pathway.
bComplete clinical data including type of cancer; stage; prior and ongoing oncological treatments; comorbidities; disease status; description and grading of treatment-related toxicities and its relationship with treatment; treatment discontinuation and reintroduction; supportive care strategies proposed and attendance log to supportive care strategies; and use of hospital services, including emergency visits, extra consultations, and hospitalizations. Oncological scores used for supportive care management included: Geriatric score G8, thrombosis score, nausea, and vomiting score.
cFor the complete list of supportive care resources, refer to Textbox 1.
dIncluding attendance data in all in-person supportive care interventions.
eResilience [29] is a mobile app used in routine care at Gustave Roussy for remote symptom monitoring, patient empowerment, and education. Data on mobile app use, including symptoms reported, alerts generated, and content used, will be evaluated.
fSpecific questionnaires can be added if pertinent to a new pathway.
gSent only for patients participating in the pathway to prevent treatment-related burden (brain, head and neck, thoracic, and neuroendocrine tumors).
hSent only for patients in the pathway for preventing treatment-related burden after breast cancer.
iSent only for patients in the pathway for preventing treatment-related burden after breast cancer or patients referred to supportive care services for emotional distress and anxiety (mindfulness meditation programs, cognitive behavioral therapy, and psychological consultation).
jSent only for patients referred for supportive care strategies for insomnia (cognitive behavioral therapy and mindfulness meditation programs).
kSent only for patients with sexual concerns referred for sexologist consultation.
lThe experience questionnaire will be specific for each supportive care intervention.
mFocus groups with participants of each supportive care intervention.
Eligibility Criteria
Patients are eligible if they have histological confirmation of cancer of any type and stage, are aged ≥18 years, and provided written informed consent. For the primary end point, all patients included in SC pathways (ie, who received a formal SC needs assessment and tailored multidisciplinary referrals) will be invited to participate. As for the secondary end points, any patient participating in SC interventions may be invited to participate. As for health care providers, those who assist the patients included in the SC pathways, care managers, and coordinators involved are eligible. If a patient withdraws consent for the study, no further study-specific evaluations will be performed, and no additional data will be collected.
Integrated SC Pathways
At Gustave Roussy, integrated pathways of SC were co-designed with patients, providers (including nurses, oncologists, radiotherapists, surgeons, and SC specialists), sociologists, care managers, technology experts, and implementation scientists. These pathways aim to provide a formal SC needs assessment and tailored multidisciplinary care referral across the entire cancer care continuum, leveraging mechanisms that ensure the inclusion of patients considered vulnerable. During the co-design phase, each pathway carefully considered the available scientific evidence and the needs of patients and providers according to tumor type and disease stage. Shortly after the moment of diagnosis, the objective of the integrated SC pathways is to anticipate and prevent treatment-related burden. An autoevaluation of patient’s symptoms and SC needs alongside a health care provider’s assessment are conducted to implement a personalized SC plan. This pathway is being implemented for patients with brain, head and neck, thoracic, and endocrine tumors and will be adapted and expanded to other tumor types, including breast cancer (long-term fatigue after breast cancer prevention of cancer-related fatigue and cluster of long-term behavioral symptoms pathway). During treatment, the goal is to continuously monitor and manage the toxicity of systemic therapies at an earlier stage, reduce symptom burden, and avoid recourse to emergency care. A total of 2 pathways are implemented: a remote patient monitoring pathway using electronic weekly patient-reported outcomes (electronic patient-reported outcomes version of the common terminology criteria for adverse events) with nurse navigation [19] and an immunotoxicity management pathway with a multidisciplinary expert team providing mobile evaluation for hospitalized and ambulatory patients and follow-up consultations. Both the remote patient monitoring pathway and the immunotoxicity management pathway are agnostic (any cancer type and stage). After treatment, the objective is to mitigate long-term treatment-related toxicities, accelerate rehabilitation, give support during long adjuvant treatments, promote healthier behaviors, and facilitate social reintegration. This pathway is implemented for breast cancer [20] and encompasses a personalized survivorship care consultation for needs assessment and SC referrals, the delivery of a survivorship care plan document, invitation to attend face-to-face survivorship educational group seminars, access to a mobile app delivering personalized education and self-management advice, and decision aids for physicians focused on SC needs. This pathway will be adapted and expanded to other tumor types in our institution.
A pathway implementation committee oversees the co-design and deployment process of the SC pathways, including the need for staff training or specific recruitments before the pathway is implemented in routine care. If staff replacements are needed, proper training is provided to new team members.
Study Objectives
Primary Objective
The primary objective of this study is to evaluate the impact of an integrated proactive SC pathway in patients’ distress and unmet needs at 12 weeks’ follow-up in difference phases of the cancer continuum (at diagnosis, during treatment, and survivorship phase). Distress and unmet needs will be measured by the National Comprehensive Cancer Network (NCCN) Distress Thermometer and Problem List, respectively [30,31]. For patients participating in the immunotoxicity management pathway, the impact of the pathway will be evaluated at 4-week follow-up.
Secondary Objectives
The study’s secondary objectives are to (1) evaluate the Reach of the pathway through the absolute number, proportion, and representativeness of patients who participated in the SC needs assessment and in each SC intervention; (2) evaluate the microlevel Efficacy of the pathway and each SC intervention through the impact of the pathway and each SC intervention on patients’ quality of life, symptom burden, and distress; (3) evaluate the Adoption of the pathway through the absolute number, proportion, and representativeness of physicians and patients engaged with the pathway and each SC intervention; (4) evaluate barriers and leverages for pathway Implementation through collection of patient, health care provider, and organization experience; and (5) plan for Maintenance of the pathway through a cost-consequences analysis, with analysis of health resources and costs related to hospital services and efficacy outcomes (quality-adjusted life years [QALYs]) over a 6-month follow-up.
Study Assessments
The NCCN’s Distress Thermometer and Problem List [30] will be used to measure patients’ distress and unmet needs at baseline and after 12 weeks and 24 weeks. In addition, we will evaluate at 12 weeks the Reach as the absolute number, proportion, and representativeness of patients: offered to participate in a SC pathway, who accepted the participation in a SC pathway, and for whom each type of SC strategy was indicated.
At baseline, a socioeconomic questionnaire and a health literacy questionnaire [32] will be completed. Quality of life will be evaluated at baseline, 12 weeks, and 24 weeks with the EQ-5D-5L [33] in the overall cohort and the 30-item European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire [34] for patients with breast cancer participating in fatigue prevention pathway. Symptom burden will be evaluated at baseline, week 12, and week 24 with the MD Anderson Symptom Inventory [35] in the overall cohort and relevant questionnaires for specific patient cohorts, such as the Hospital Anxiety and Depression Scale [36] for patients in the frailty prevention pathway (breast cancer) and patients referred to SC services for emotional distress and anxiety, the Insomnia Severity Index [37] for patients referred for SC strategies for insomnia, and the 22-item European Organization for Research and Treatment of Cancer Sexual Health Questionnaire [38] for patients with sexual concerns referred for sexologist consultation. In addition, patients with brain, lung, head and neck, and neuroendocrine tumors participating in the pathway to prevent treatment-related burden will also complete a vulnerability questionnaire at baseline.
Adoption at week 12 and week 24 will include metrics focused on (1) physicians: absolute number, proportion, and representativeness of physicians referring patients to the SC pathways and (2) patients: absolute number, proportion, and of patients that fully adopted each SC intervention (eg, in the after cancer pathway: attendance to consultations, seminaries, classes, completion of a SC program, and use data). To evaluate implementation, we will look at patient, provider, and organizational experience (levers and obstacles to proper implementation) within the proactive SC pathways at week 12 of follow-up. A patient experience questionnaire, the Patient Assessment of Chronic Illness Care [39], will be applied at week 12. In addition, an ad hoc patient satisfaction questionnaire (5-point Likert scale) will also be collected at 12 weeks after pathway delivery. This questionnaire includes core common questions for all pathways (overall satisfaction, perceived usefulness of the needs assessment and supportive are services proposed, clarity of the recommendations, and ability to comply with the SC plan recommended) and specific satisfaction and perceived usefulness questions for SC services used in each pathway; a free text field for comments is also included. All these quantitative analyses will be enriched with preplanned qualitative analysis with focus groups with patients, providers, and implementation team to assess experience, satisfaction, and contextual factors that influence implementation [40]. Maintenance of the pathway will be performed through a cost-consequences analysis. Hospital costs from the perspective of the French national health insurance will be assessed during the study period. This will be calculated by administrative data review of internal allocated resources for pathway delivery and estimated costs of use of hospital services (unplanned hospitalization, consultations, and emergency visits recorded in the electronic medical records). QALYs will be measured using utility values derived from the EQ-5D-5L. QALYs will be computed combining survival time by utility values.
Assessments at week 4 will be conducted exclusively with patients participating in the immunotoxicity management pathway (Table 1).
Statistical Considerations
The NCCN’s Distress Thermometer scores are based on mean and SD values at baseline and have been used in heterogeneous populations [31,41]. To estimate the expected effect of the integrated and proactive SC pathway on Distress Thermometer scores, a pilot evaluation will be conducted to calculate the formal sample size needed for efficacy evaluation. According to the sample size requirements for pilot studies proposed by Teare et al [42], pilot evaluations with a minimum of 70 patients will be performed to generate NCCN’s Distress Thermometers mean scores and SDs before and after going through a SC pathway (70 patients for each SC pathway).
The primary analysis will compare patient distress scores by the NCCN’s Distress Thermometer measured before and after the intervention (baseline and week 12) using the Wilcoxon signed rank test.
For secondary analyses, the scores and subscores of the patient-reported outcome measurements (EQ-5D-5L, MD Anderson Symptom Inventory, Hospital Anxiety and Depression Scale, Insomnia Severity Index, 30-item European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire, and the 22-item European Organization for Research and Treatment of Cancer Sexual Health Questionnaire) and patient-reported experience measurement (NCCN Distress Thermometer) questionnaires and scales will be calculated using mixed models to take into account the repeated measures and the initial value before intervention.
All patients receiving SC interventions and referrals as well as health care providers and care coordination professionals performing activities related to the SC clinical pathways (nurses, oncologists, gynecologists, surgeons, radiation oncologists, and members from the multidisciplinary SC team) may be included in the study. For the primary end point, any patient who received a needs assessment in the context of an integrated supportive pathway will be included. For the secondary end points, any patient participating in SC activities will be included.
For the cost-consequence analysis, costs from the perspective of the French national health insurance will be assessed during the study period. This will be calculated by administrative data review of internal allocated resources for pathway delivery and estimated costs of use of hospital services (unplanned hospitalization, consultations, and emergency visits recorded in the electronic medical records). Utility values will be assessed using the EQ-5D-5L. QALYs will be computed combining survival time by utility values. Long-term efficacy will be evaluated with the same efficacy outcomes at 6-month follow-up.
All analyses will be performed using SAS (version 9.4; SAS Institute) and R (version 4.0.3). Statistical significance will be defined with a P<.05.
Data Collection, Management, and Auditing
The Biostatistics and Epidemiology unit at Gustave Roussy implemented an electronic case report form (eCRF) to allow secure online-direct data collection using REDCap. Each user has personal identifiers (user ID and password), and data access is strictly limited according to profiles: (1) hospital clinical research assistant (CRA), allowing data entry on the eCRF; (2) data manager, allowing the first data monitoring, perform consistency checks, and edit requests for clarification addressed to the investigator or hospital CRA; and (3) investigator profile, enabled to sign and validate the data electronically. Electronic learning is mandatory to access the eCRF. The password is configured when the profile is activated and must be changed every 6 months. For each patient included, the eCRF has to be completed by hospital CRA and signed by a study investigator. An audit trail within the system tracks all the changes made to the data. Data sources of the study include the eCRF, data from the WeShare platform, and data from the technology providers of remote care interventions (Resilience Care). SC referrals and attendance will be captured in the eCRF of the study. Attendance to each of the SC strategies will be retrieved from the electronic medical records or from a specific attendance-log database in the case of integrative therapies. Usability data from technology-enabled SC interventions will also be retrieved and transferred by Resilience Care. Patient-reported outcomes data will be collected and hosted by the WeShare platform and transferred to the investigator at the end of the study. Both patient-reported outcomes data and usability data from Resilience Care are interoperable with Redcap. Data collected will be managed in the Biostatistics and Epidemiology unit at Gustave Roussy. Standard institutional practices will be followed to maintain the confidentiality and security of data collected in this study. A copy of the consent form and documentation of consent will be stored in a locked cabinet or an encrypted, password-protected computer drive. All protected health information collected from the study eCRF will be encrypted and password protected. If any questionnaire is filled out on paper, this will be stored in a locked cabinet in a secured office in Gustave Roussy. Data will be stored until data analysis is complete, and then the data will be transferred to a centralized repository. Access to the repository will be limited to the principal investigator, coinvestigators, and associates from the original study team. Future studies requesting the use of the data must either be related to the original research study or will require separate institutional review board approval. To guarantee the authenticity and the credibility of the data in conformity with good clinical practices, auditing and quality assurance systems include (1) study management in accordance with standardized procedures at Gustave Roussy and (2) quality control performed by the CRA. Particularly, it is the responsibility of the CRA to (1) check that the investigator’s file is correctly and regularly updated; (2) verify the signatures and validity of consent forms, fulfillment of eligibility criteria, validity of evaluation criteria, and adverse events; and (3) assure that reporting requirements are met. Regular meetings, held at least monthly, with the investigator team and study coordinator ensure a thorough review of study procedures, provide periodic updates on study progress (including patient enrollment numbers vs expected numbers), and address any procedural issues.
Equity, Diversity, and Inclusion
To ensure equity, diversity, and inclusion, social determinants of health and health-related social risks are screened at pathway entry. In addition, SC services targeting actionable unfavorable social determinants of health, such as social services and financial counseling, referrals to smoking and alcohol cessation programs, and nutritional counseling, are part of the actions delivered in the context of the pathways. In addition, plain language standards are applied to educational materials used to communicate pathway activities toward patients. An objective guidance on equity, diversity, and inclusion is publicly available for researchers and providers involved in this study via the WeShare platform [28], and a cultural competency training is being developed and will be recommended for all providers involved in pathway activities (screening and care delivery). Social determinants of health and demographics are collected during the study and will allow to monitor the participation of populations that have been historically excluded in SC interventions.
Patient Involvement in the Study
The SC pathways implemented in this study are co-designed with patient representatives upfront before deployment. Particularly, the study team meets with patient representatives at four key moments to foster cocreation: (1) at conceptualization to identify patient’s SC needs, (2) during development of pathway components giving input and ideas of components to prioritize and how to model them, (3) just before implementation, and (4) after implementation. In addition, a patient representative is a member of the operational team (JA). The study protocol was also discussed in detail and approved by patient representatives. Across the study, qualitative and quantitative assessments of patient experience are planned. These data will serve to continuously improve pathway components and delivery to meet the needs of the patients.
Ethical Considerations
This study received regulatory approval by the institutional review board of Gustave Roussy and by the French national review board on September 4, 2023 (ID-RCB 2023-A01225-40). All participants (patients, providers, and managers) will provide informed and signed consent before taking part in the data collection process. Information that could potentially identify participants will be securely stored in a password-protected, locked database. Whenever possible, data will be deidentified through codification. Participants will not receive any monetary compensation for taking part in the study.
Results
As of February 2024, the evaluation of the SC pathway to prevent treatment-related burden for patients considered vulnerable with brain, head and neck,
thoracic, and neuroendocrine tumors has started, and 12 patients were enrolled in the study. The evaluation of the SC pathway for preventing treatment-related burden after breast cancer and the proactive survivorship care pathway (breast cancer) is expected to start in April 2024. Data will be analyzed once at least 70 patients have completed the study evaluations for one of the pathways. Results of this study will be sent for publication in peer-reviewed journals and will also be presented to the multidisciplinary implementation team so that SC pathways can be refined accordingly to better serve the needs of patients and providers. The clinical trial is registered at ClinicalTrials.gov (NCT06479057).
Discussion
Principal Findings
The proposed study will evaluate the implementation of distinct integrated proactive pathways of SC that are offered to patients treated at Gustave Roussy. Our study has several strengths. It is a master protocol for a prospective study on patients diagnosed with any type of cancer, across different moments of the cancer care continuum, using the RE-AIM framework to guide its evaluation. Quantitative analyses will use a variety of data, including validated patient-reported outcomes measures; experience and satisfaction surveys; and administrative, sociodemographic, health literacy, and clinical data. Furthermore, these will be enriched with preplanned qualitative assessments (focus groups) with several stakeholders. This study design will allow for analysis of patterns of unmet needs that are currently difficult to generalize. In addition, it may serve as an umbrella protocol for ancillary prospective studies focusing on each SC intervention. It is expected to lead to a higher level of coordination than the one achieved by independently conducted studies.
Despite the existing literature on interventions addressing SC needs in patients with cancer, their implementation has been suboptimal due to inconsistency of empirical evidence for interventions and the difficulties experienced by policy makers and health service providers in finding and assessing the evidence for interventions [15,43]. Typical obstacles include low level of awareness among oncologist on SC services, lack of a comprehensive multidisciplinary SC team, fragmented and unclear communication and referral processes for SC interventions, nonstandardized delivery of needs assessment and tailored referrals, uneven access to SC services among patients considered vulnerable and minority groups, incorporation of nonevidence-based practices, reimbursement and care valorization issues, and lack of integration with community-based resources [7].
Conclusions and Impact
This study will provide evidence on the implementation process of integrated, proactive SC pathways and will also inform future care delivery strategies to improve the reach and adoption of SC in oncology centers. It may serve as a model for other cancer centers trying to implement such integrated pathways. The analysis of quantitative and qualitative data collected from the patient, providers, and the health care organization for this study will be used to improve the design and delivery of SC pathways so that they meet the needs of patients and are feasible to be implemented according to a provider point of view. In addition, it will provide a detailed description of patients’ unmet SC needs across the cancer care continuum in multiple cancer types.
This study will also add evidence on using technology to facilitate the delivery and evaluation of SC pathways. More specifically, for care, electronic patient-reported outcomes are integrated with medical records and used for needs assessment to screen patient vulnerability status being used to perform tailored SC referrals since diagnosis. Technology is also used for remote patient monitoring where electronic patient-reported outcomes are transmitted in real time to nurse navigators during active treatment phase with chemotherapy and targeted therapies. Several digitally enabled SC strategies are also implemented, such as physical activity, meditation, yoga, and cognitive behavioral therapies. Finally, for research purposes, technology is used to collect patient-generated data and clinical data for outcomes assessment.
This study has the potential to impact policy and global SC practices in oncology through several mechanisms. First, it can serve as a model to other cancer centers to build and implement coordinated and integrated SC pathways. It will report in detail the infrastructure required in cancer centers to deliver integrated SC. It will also introduce innovative methods to facilitate implementation, such as using technology to screen patients’ needs, monitor symptoms, deliver specific SC interventions, and partner with community-based SC infrastructures. Furthermore, the proactive supportive care pathway approach is innovative as it allows to anticipate SC needs in a tentative manner to prevent treatment-related burden instead of using the standard reactive supportive care pathway approach currently used in most institutions. Finally, the presentation of this study in medical conferences and the publication of its results both in peer-reviewed journals and in lay media channels will also contribute to raise awareness among cancer care providers and policy makers to stimulate care and research initiatives of innovative models of SC delivery to improve patients’ quality of life, addressing the physical and psychosocial needs of patients while improving the organization of health services.
Acknowledgments
The authors would like to thank the members of the Interdisciplinary Department for the Organization of Patient Pathways at Gustave Roussy for their collaboration in this research protocol.
This study is funded by the Gustave Roussy Foundation (INTERVAL program to IV-L), the French Regional Health Agency (ARS-Ille de France) (Prognosis program to LP) and French Cancer Research Funding (Foundation ARC grant number ARCPGA2022010004401_4882) through the PREFACE program to ADM. MAF is funded by a Conquer Cancer—Breast Cancer Research Foundation Career Development Award for Diversity and Inclusion, supported by Breast Cancer Research Foundation. Any opinions, findings, and conclusions expressed in this paper are those of the authors and do not necessarily reflect those of the American Society of Clinical Oncology, Conquer Cancer, or the Breast Cancer Research Foundation. IV-L declares that the WeShare project is funded by the French National Health Agency (grant ANR-21-ESRE-0017).
Abbreviations
- CRA
clinical research assistant
- eCRF
electronic case report form
- NCCN
National Comprehensive Cancer Network
- QALY
quality-adjusted life years
- RE-AIM
Reach, Effectiveness, Adoption, Implementation, and Maintenance
- SC
supportive care
Data Availability
The data sets generated during and/or analyzed during this study will be available in the WeShare Data repository [28].
Footnotes
Conflicts of Interest: MAF declares receiving research funding from Resilience (for the institution) and Gilead (for the institution) and speaker honoraria from Novartis (for the institution). ADM declares expert testimony activities for Kephren, Techspert (personal; not related to this manuscript). FS declares receiving honoraria from Leo Phar, Viatris, Pharmanovia, Amgen, Gilead Sciences, BMS GmbH & Co. KG, and GlaxoSmithKline. IV-L declares receiving speaker honoraria from Amgen, AstraZeneca, Pfizer and Edimark, Novartis, Sandoz (institutional); a writing engagement from Pfizer and Edimark (institutional); research funding from Resilience Care (institutional); and travel support from Novartis. All other authors have no other conflicts to declare.
References
- 1.Vaz-Luis I, Masiero M, Cavaletti G, Cervantes A, Chlebowski RT, Curigliano G, Felip E, Ferreira AR, Ganz PA, Hegarty J, Jeon J, Johansen C, Joly F, Jordan K, Koczwara B, Lagergren P, Lambertini M, Lenihan D, Linardou H, Loprinzi C, Partridge AH, Rauh S, Steindorf K, van der Graaf W, van de Poll-Franse L, Pentheroudakis G, Peters S, Pravettoni G. ESMO expert consensus statements on cancer survivorship: promoting high-quality survivorship care and research in Europe. Ann Oncol. 2022 Nov;33(11):1119–33. doi: 10.1016/j.annonc.2022.07.1941. https://linkinghub.elsevier.com/retrieve/pii/S0923-7534(22)03792-9 .S0923-7534(22)03792-9 [DOI] [PubMed] [Google Scholar]
- 2.Olver I, Keefe D, Herrstedt J, Warr D, Roila F, Ripamonti CI. Supportive care in cancer-a MASCC perspective. Support Care Cancer. 2020 Aug;28(8):3467–75. doi: 10.1007/s00520-020-05447-4.10.1007/s00520-020-05447-4 [DOI] [PubMed] [Google Scholar]
- 3.Jordan K, Aapro M, Kaasa S, Ripamonti CI, Scotté F, Strasser F, Young A, Bruera E, Herrstedt J, Keefe D, Laird B, Walsh D, Douillard JY, Cervantes A. European Society for Medical Oncology (ESMO) position paper on supportive and palliative care. Ann Oncol. 2018 Jan 01;29(1):36–43. doi: 10.1093/annonc/mdx757. https://linkinghub.elsevier.com/retrieve/pii/S0923-7534(19)35021-5 .S0923-7534(19)35021-5 [DOI] [PubMed] [Google Scholar]
- 4.Gourret Baumgart J, Kane H, Pelletier S, André K, Barbe C, Lecomte T, Sam Y, Messai N, Rusch E, Denis F. Understanding inequalities in the uptake of supportive care to improve practices in the cancer care continuum. Cancers (Basel) 2022 Dec 08;14(24):6053. doi: 10.3390/cancers14246053. https://www.mdpi.com/resolver?pii=cancers14246053 .cancers14246053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zafar SY. Financial toxicity of cancer care: it's time to intervene. J Natl Cancer Inst. 2015 Dec 11;108(5):djv370. doi: 10.1093/jnci/djv370.djv370 [DOI] [PubMed] [Google Scholar]
- 6.Berman R, Davies A, Cooksley T, Gralla R, Carter L, Darlington E, Scotté F, Higham C. Supportive care: an indispensable component of modern oncology. Clin Oncol (R Coll Radiol) 2020 Nov;32(11):781–8. doi: 10.1016/j.clon.2020.07.020. https://europepmc.org/abstract/MED/32814649 .S0936-6555(20)30314-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Popescu RA, Roila F, Arends J, Metro G, Lustberg M. Supportive care: low cost, high value. Am Soc Clin Oncol Educ Book. 2021 Mar;41:1–11. doi: 10.1200/EDBK_320041. https://ascopubs.org/doi/10.1200/EDBK_320041?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PubMed] [Google Scholar]
- 8.Evans Webb M, Murray E, Younger ZW, Goodfellow H, Ross J. The supportive care needs of cancer patients: a systematic review. J Cancer Educ. 2021 Oct;36(5):899–908. doi: 10.1007/s13187-020-01941-9. https://europepmc.org/abstract/MED/33492650 .10.1007/s13187-020-01941-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009 Aug;17(8):1117–28. doi: 10.1007/s00520-009-0615-5. [DOI] [PubMed] [Google Scholar]
- 10.Paterson C, Toohey K, Bacon R, Kavanagh PS, Roberts C. What are the unmet supportive care needs of people affected by cancer: an umbrella systematic review. Semin Oncol Nurs. 2023 Jun;39(3):151353. doi: 10.1016/j.soncn.2022.151353.S0749-2081(22)00130-9 [DOI] [PubMed] [Google Scholar]
- 11.Cochrane A, Woods S, Dunne S, Gallagher P. Unmet supportive care needs associated with quality of life for people with lung cancer: a systematic review of the evidence 2007-2020. Eur J Cancer Care (Engl) 2022 Jan;31(1):e13525. doi: 10.1111/ecc.13525. [DOI] [PubMed] [Google Scholar]
- 12.Penedo FJ, Natori A, Fleszar-Pavlovic SE, Sookdeo VD, MacIntyre J, Medina H, Moreno PI, Crane TE, Moskowitz C, Calfa CL, Schlumbrecht M. Factors associated with unmet supportive care needs and emergency department visits and hospitalizations in ambulatory oncology. JAMA Netw Open. 2023 Jun 01;6(6):e2319352. doi: 10.1001/jamanetworkopen.2023.19352. https://europepmc.org/abstract/MED/37342038 .2806320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miniotti M, Bassino S, Fanchini L, Ritorto G, Leombruni P. Supportive care needs, quality of life and psychological morbidity of advanced colorectal cancer patients. Eur J Oncol Nurs. 2019 Dec;43:101668. doi: 10.1016/j.ejon.2019.09.009. http://hdl.handle.net/2318/1730023 .S1462-3889(19)30128-0 [DOI] [PubMed] [Google Scholar]
- 14.Edney LC, Roseleur J, Gray J, Koczwara B, Karnon J. Mapping a decade of interventions to address the supportive care needs of individuals living with or beyond cancer: a scoping review of reviews. Support Care Cancer. 2022 May;30(5):3793–804. doi: 10.1007/s00520-021-06713-9.10.1007/s00520-021-06713-9 [DOI] [PubMed] [Google Scholar]
- 15.Hack TF, Carlson L, Butler L, Degner LF, Jakulj F, Pickles T, Dean Ruether J, Weir L. Facilitating the implementation of empirically valid interventions in psychosocial oncology and supportive care. Support Care Cancer. 2011 Aug;19(8):1097–105. doi: 10.1007/s00520-011-1159-z. [DOI] [PubMed] [Google Scholar]
- 16.Krishnasamy M, Hyatt A, Chung H, Gough K, Fitch M. Refocusing cancer supportive care: a framework for integrated cancer care. Support Care Cancer. 2022 Dec 14;31(1):14. doi: 10.1007/s00520-022-07501-9. https://europepmc.org/abstract/MED/36513841 .10.1007/s00520-022-07501-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hui D, Hoge G, Bruera E. Models of supportive care in oncology. Curr Opin Oncol. 2021 Jul 01;33(4):259–66. doi: 10.1097/CCO.0000000000000733. https://europepmc.org/abstract/MED/33720070 .00001622-202107000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jefford M, Howell D, Li Q, Lisy K, Maher J, Alfano CM, Rynderman M, Emery J. Improved models of care for cancer survivors. Lancet. 2022 Apr 16;399(10334):1551–60. doi: 10.1016/S0140-6736(22)00306-3. https://europepmc.org/abstract/MED/35430022 .S0140-6736(22)00306-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franzoi MA, Ferreira AR, Lemaire A, Rodriguez J, Grosjean J, Ribeiro JM, Polastro L, Grellety T, Artignan X, Du KL, Pagliuca M, Nouhaud E, Autheman M, André F, Basch E, Metzger O, Ferté C, Di Palma M, Scotté F, Vaz-Luis I. Implementation of a remote symptom monitoring pathway in oncology care: analysis of real-world experience across 33 cancer centres in France and Belgium. Lancet Reg Health. 2024 Jul 31;:101005. doi: 10.1016/j.lanepe.2024.101005. https://www.thelancet.com/journals/lanepe/article/PIIS2666-7762(24)00172-8/fulltext . [DOI] [Google Scholar]
- 20.Franzoi MA, Degousée L, Martin E, Semedo PM, Aupomerol M, Soldato D, Di Meglio A, Chiodi C, Barbier A, Chaouachi H, Renvoisé N, Boinon D, Fasse L, Ribeiro J, Le-Provost JB, Arvis J, Lazorthes C, di Palma M, de Jesus A, Raynard B, Pagès A, Delaloge S, Pistilli B, Scotté F, Vaz-Luis I. Implementing a PROACTive care pathway to empower and support survivors of breast cancer. JCO Oncol Pract. 2023 Jun;19(6):353–61. doi: 10.1200/OP.23.00016. https://europepmc.org/abstract/MED/37307673 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaz-Luis I, Di Meglio A, Havas J, El-Mouhebb M, Lapidari P, Presti D, Soldato D, Pistilli B, Dumas A, Menvielle G, Charles C, Everhard S, Martin AL, Cottu P, Lerebours F, Coutant C, Dauchy S, Delaloge S, Lin N, Ganz P, Partridge A, André F, Michiels S. Long-term longitudinal patterns of patient-reported fatigue after breast cancer: a group-based trajectory analysis. J Clin Oncol. 2022 Jul 01;40(19):2148–62. doi: 10.1200/JCO.21.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Meglio A, Havas J, Soldato D, Presti D, Martin E, Pistilli B, Menvielle G, Dumas A, Charles C, Everhard S, Martin AL, Coutant C, Tarpin C, Vanlemmens L, Levy C, Rigal O, Delaloge S, Lin NU, Ganz PA, Partridge AH, André F, Michiels S, Vaz-Luis I. Development and validation of a predictive model of severe fatigue after breast cancer diagnosis: toward a personalized framework in survivorship care. J Clin Oncol. 2022 Apr 01;40(10):1111–23. doi: 10.1200/JCO.21.01252. https://europepmc.org/abstract/MED/35061509 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Meglio A, Havas J, Gbenou AS, Martin E, El-Mouhebb M, Pistilli B, Menvielle G, Dumas A, Everhard S, Martin AL, Cottu PH, Lerebours F, Coutant C, Lesur A, Tredan O, Soulie P, Vanlemmens L, Joly F, Delaloge S, Ganz PA, André F, Partridge AH, Jones LW, Michiels S, Vaz-Luis I. Dynamics of long-term patient-reported quality of life and health behaviors after adjuvant breast cancer chemotherapy. J Clin Oncol. 2022 Sep 20;40(27):3190–204. doi: 10.1200/JCO.21.00277. https://europepmc.org/abstract/MED/35446677 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woodcock J, LaVange LM. Master protocols to study multiple therapies, multiple diseases, or both. N Engl J Med. 2017 Jul 06;377(1):62–70. doi: 10.1056/NEJMra1510062. [DOI] [PubMed] [Google Scholar]
- 25.Holtrop JS, Estabrooks PA, Gaglio B, Harden SM, Kessler RS, King DK, Kwan BM, Ory MG, Rabin BA, Shelton RC, Glasgow RE. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Transl Sci. 2021 May 14;5(1):e126. doi: 10.1017/cts.2021.789. https://europepmc.org/abstract/MED/34367671 .S2059866121007895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shelton RC, Chambers DA, Glasgow RE. An extension of RE-AIM to enhance sustainability: addressing dynamic context and promoting health equity over time. Front Public Health. 2020 May 12;8:134. doi: 10.3389/fpubh.2020.00134. https://europepmc.org/abstract/MED/32478025 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Franzoi MA, Gillanders E, Vaz-Luis I. Unlocking digitally enabled research in oncology: the time is now. ESMO Open. 2023 Oct;8(5):101633. doi: 10.1016/j.esmoop.2023.101633. https://linkinghub.elsevier.com/retrieve/pii/S2059-7029(23)00868-2 .S2059-7029(23)00868-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.What is WeShare? WeShare. [2024-08-06]. https://weshare.unicancer.com/
- 29.Resilience homepage. Resilience. [2024-08-06]. https://www.resilience.care/
- 30.Riba MB, Donovan KA, Andersen B, Braun I, Breitbart WS, Brewer BW, Buchmann LO, Clark MM, Collins M, Corbett C, Fleishman S, Garcia S, Greenberg DB, Handzo RG, Hoofring L, Huang CH, Lally R, Martin S, McGuffey L, Mitchell W, Morrison LJ, Pailler M, Palesh O, Parnes F, Pazar JP, Ralston L, Salman J, Shannon-Dudley MM, Valentine AD, McMillian NR, Darlow SD. Distress management, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019 Oct 01;17(10):1229–49. doi: 10.6004/jnccn.2019.0048. https://europepmc.org/abstract/MED/31590149 .jnccnGLsDistress1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cutillo A, O'Hea E, Person S, Lessard D, Harralson T, Boudreaux E. The distress thermometer: cutoff points and clinical use. Oncol Nurs Forum. 2017 May 01;44(3):329–36. doi: 10.1188/17.ONF.329-336. https://europepmc.org/abstract/MED/29493167 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ) BMC Public Health. 2013 Jul 16;13:658. doi: 10.1186/1471-2458-13-658. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-658 .1471-2458-13-658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.EQ-5D-5L. EuroQol. [2023-09-06]. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/
- 34.Quality of life of cancer patients. EORTC Quality of Life. [2023-09-06]. https://qol.eortc.org/questionnaire/eortc-qlq-c30/
- 35.The MD Anderson symptom inventory. The University of Texas MD Anderson Cancer Center. [2023-09-06]. https://www.mdanderson.org/research/departments-labs-institutes/departments-divisions/symptom-research/symptom-assessment-tools/md-anderson-symptom-inventory.html .
- 36.Stern AF. The hospital anxiety and depression scale. Occup Med (Lond) 2014 Jul;64(5):393–4. doi: 10.1093/occmed/kqu024.kqu024 [DOI] [PubMed] [Google Scholar]
- 37.Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011 May 01;34(5):601–8. doi: 10.1093/sleep/34.5.601. https://europepmc.org/abstract/MED/21532953 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oberguggenberger AS, Nagele E, Inwald EC, Tomaszewski K, Lanceley A, Nordin A, Creutzberg CL, Kuljanic K, Kardamakis D, Schmalz C, Arraras J, Costantini A, Almont T, Wei-Chu C, Dehandschutter S, Winters Z, Greimel E. Phase 1-3 of the cross-cultural development of an EORTC questionnaire for the assessment of sexual health in cancer patients: the EORTC SHQ-22. Cancer Med. 2018 Mar;7(3):635–45. doi: 10.1002/cam4.1338. https://europepmc.org/abstract/MED/29436144 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gensichen J, Serras A, Paulitsch MA, Rosemann T, König J, Gerlach FM, Petersen JJ. The patient assessment of chronic illness care questionnaire: evaluation in patients with mental disorders in primary care. Community Ment Health J. 2011 Aug;47(4):447–53. doi: 10.5167/uzh-35895. doi: 10.5167/uzh-35895. [DOI] [PubMed] [Google Scholar]
- 40.Tenny S, Brannan JM, Brannan GD. Qualitative Study. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar]
- 41.Ma X, Zhang J, Zhong W, Shu C, Wang F, Wen J, Zhou M, Sang Y, Jiang Y, Liu L. The diagnostic role of a short screening tool--the distress thermometer: a meta-analysis. Support Care Cancer. 2014 Jul;22(7):1741–55. doi: 10.1007/s00520-014-2143-1. [DOI] [PubMed] [Google Scholar]
- 42.Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials. 2014 Jul 03;15:264. doi: 10.1186/1745-6215-15-264. https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-15-264 .1745-6215-15-264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mitchell SA, Chambers DA. Leveraging implementation science to improve cancer care delivery and patient outcomes. J Oncol Pract. 2017 Aug;13(8):523–9. doi: 10.1200/JOP.2017.024729. https://europepmc.org/abstract/MED/28692331 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated during and/or analyzed during this study will be available in the WeShare Data repository [28].


