Abstract
The authors report a rare case of pediatric tuberculous dactylitis of the thumb with flexor tendon involvement in a child with multiple failed treatment attempts. The patient was diagnosed, treated and the outcome of the one-year follow-up was excellent. Extra pulmonary tuberculosis frequently surprises clinicians with aberrant presentations, which may be missed during radiographic studies, if not considered in differential diagnosis amid its rare location in the appendicular skeleton. This has been highlighted in this rare case of a girl in her mid-childhood with a spindle-shaped swelling with discharging sinuses at the right thumb proximal phalanx. Scenarios mimicking similar presentations such as Enchondromatosis, Chronic pyogenic osteomyelitis, Brodie’s abscess and Actinomycosis, can be misleading. Several researchers have proffered up such rare cases, but after the anti-tubercular therapy era, the incidence has been exceptionally reduced. Still, a high index of suspicion can be helpful to avoid missing the diagnosis.
Keywords: Tuberculosis, tuberculous dactylitis, anti-tubercular therapy, Spina Ventosa, paediatric osteoarticular tuberculosis, Mycobacterium tuberculosis
Introduction
Tuberculous dactylitis (Spina Ventosa) of the thumb in a child beyond six years has not been reported yet [1,2]. This is a rare presentation of osteoarticular tuberculosis.
Spina Ventosa is the terminology used for metacarpals, metatarsals, and phalanges of hands and feet being infected with Mycobacterium tuberculosis. “Spina Ventosa” is an illustrative terminology referring to any destructive cortical lesion surrounding the medullary canal along with progressive subperiosteal hyperplasia resembling roentgenographically like a tumor [1]. It is rare after six years of age, once epiphyseal centers are well established [2-4]. The hand is more commonly affected with the proximal phalanx of the index and middle finger as the commonest sites of infection [1,4,5]. We report a case of a girl in her mid-childhood having tuberculous dactylitis of the right thumb proximal phalanx with involvement of flexor pollicis longus tendon sheath, which is an inculcation of a rare disease with rare site of involvement. In general, tuberculous dactylitis is treated with anti-tubercular therapy (ATT) [6].
Case presentation
A girl in her mid-childhood presented to the outpatient department of a tertiary care center with a complaint of dull aching pain and swelling over the right thumb for a duration of one and a half years with multiple failed treatment attempts. Previous treatment included multiple prolonged antibiotic therapies, in suspicion of osteomyelitis and frequent oncologist consultations in doubt of enchondroma.
Physical examination of the right thumb revealed two discharging sinuses at the dorsal aspect of the thumb, which was associated with bony tenderness and a painful range of motion of the proximal interphalangeal joint and metacarpophalangeal joints of the thumb. There was no local rise of temperature elicited.
Investigations
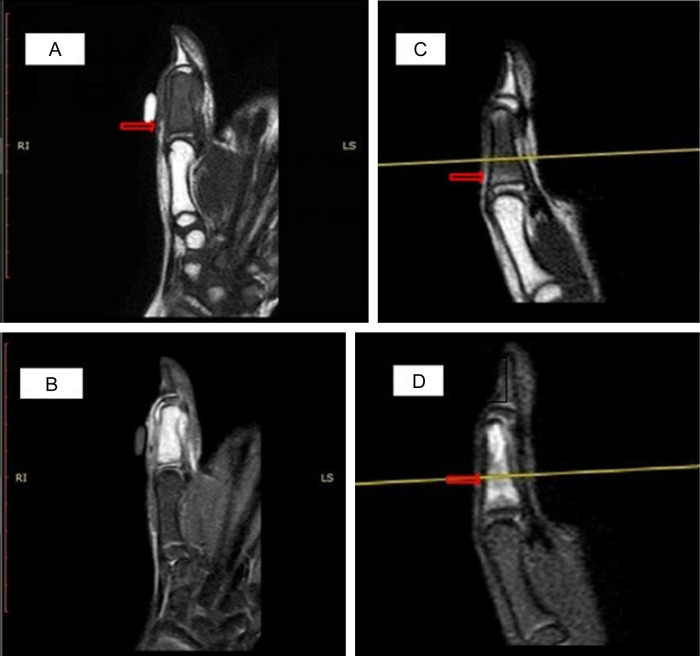
Blood investigations revealed an increased erythrocyte sedimentation rate (ESR) of 72 mm/1st hour and C-reactive protein (CRP) of 45 mg/L. There was no history of any trauma, fever, weight loss, or any contact with a tuberculosis patient in the past. The patient was fully immunized as per the national immunization schedule. Roentgenography revealed multiple concentric oval lytic lesions with thin sclerosed margins at the proximal phalanx of the right thumb with surrounding soft tissue swelling and joint sparring (Figure 1A and 1B). Based on the above findings, a differential diagnosis of enchondroma and chronic osteomyelitis was considered. Magnetic resonance imaging (MRI) was done to differentiate between the henceforth mentioned differentials, which showed marrow expansion and replacement with T1 hypointense, T2 hyperintense, and relatively homogeneously enhancing soft tissues (Figure 2A and 2B). There was evidence of a cortical breach in the medial and lateral aspects with the extension of soft tissue content through the defect measuring 15*7 mm and 8*7 mm, respectively, with minimal collection along the flexor pollicis longus tendon sheath. The above features were likely suggestive of infective etiology.
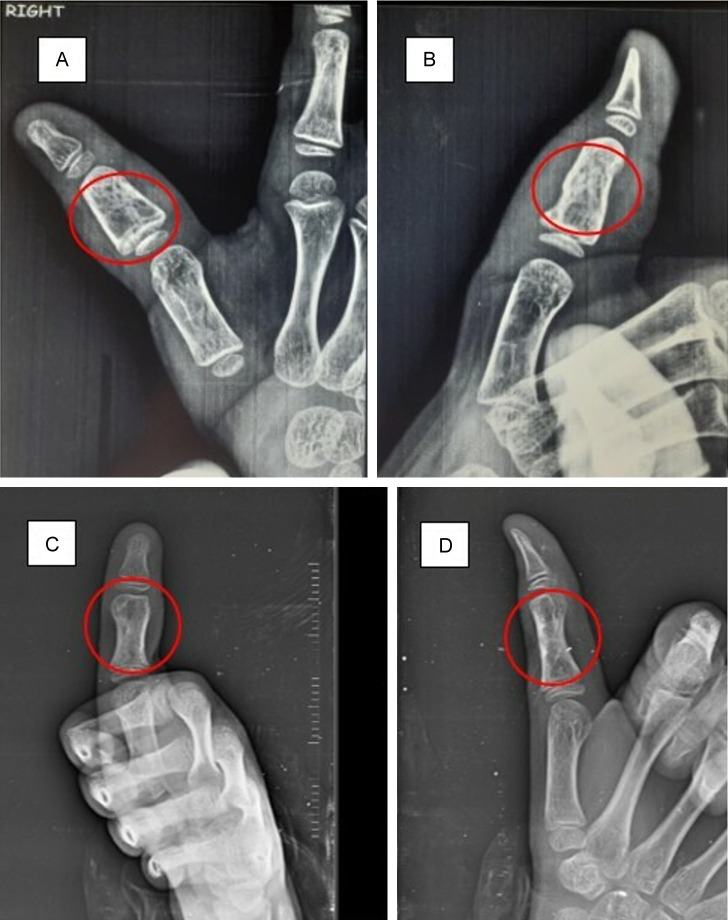
Figure 1.
Radiographs showing Antero-posterior (A) and Oblique (B) views of thumb before starting antitubercular therapy (ATT) showing multiple concentric oval lytic lesions with thin sclerosed margins at the proximal phalanx of right thumb with surrounding soft tissue swelling and joint sparring; and Radiographs showing Antero-posterior (C) and Oblique (D) views of thumb post-ATT showing healed lytic lesions with sclerosis and decreased surrounding soft tissue swelling and joint sparring.
Figure 2.
MRI images showing marrow expansion and replacement with; T1 hypo intense and relatively homogeneously enhancing soft tissues (A) versus resolution of hypo intensity (C - After 12 months of ATT); T2 hyper intense and relatively homogeneously enhancing soft tissues (B) versus resolution of hyper intensity (D - After 12 months of ATT).
Fine needle aspiration cytology (FNAC) was performed for the definitive diagnosis, which revealed well-defined epithelioid cell granulomas along with foreign body giant cells. The background showed histiocytes with scant necrosis and hemorrhage suggestive of granulomatous inflammation with scant necrosis. No evidence of malignancy was found on cytological examination. Mantoux test elicited 20 mm diameter induration after 48 hours which was significant in the pediatric age group. Microscopic examination by Ziehl-Neelsen staining of the sputum specimen was reported to be negative. Cartridge-based nucleic acid amplification test (CBNAAT) showed presence of rifampicin sensitive Mycoba-cteria Tuberculosis.
Diagnosis
Considering the above findings, along with a strong clinical suspicion, a final diagnosis of “Tuberculous dactylitis” was made.
Treatment
Following the diagnosis, written informed consent was signed by the patient’s parents and the patient was started on anti-tubercular therapy (ATT) as per National Tuberculosis Elimination Program (NTEP) guidelines (2HRZE+10HRE) with Isoniazid 10 mg/kg/day, Rifampicin 15 mg kg/day, Pyrazinamide 30 mg/kg/day and Ethambutol 20 mg/kg/day.
Outcome and follow-up
The patient was followed up during the continuous phase treatment regimen, and repeat radiograph, ESR (18 mm/1st hour), CRP (6 mg/L), and MRI of the right thumb were obtained, which revealed healing of the disease (Figures 1C, 1D, 2C and 2D). On the assessment of the patient after 12 months of the ATT regime, both the discharging sinuses healed, swelling decreased, and pain also subsided (Figure 3). Clinically, the range of motion improved with flexion 80º and extension 5º at interphalangeal joint and flexion 50º and extension 8º at the metacarpophalangeal joint.
Figure 3.
Image showing post-ATT healed discharging sinus at the proximal phalanx of the right thumb with full range of motion.
Discussion
Tuberculosis of the thumb in a child beyond six years has not been reported so far despite the endemicity of tuberculosis in the Indian subcontinent. A clinician needs to be very vigilant in making differential diagnosis and management of cases presenting with similar manifestations.
This case is delineated because of the unusual site of presentation of the disease such as involvement of the proximal phalanx of the thumb in a pediatric age group instead of the metacarpals, index or middle finger which are the most common sites of infection [1,4,5].
Maintaining a high index of suspicion is the key in managing such cases and to restrict the inadvertent use of empirical antibiotics which adds to drug resistance. Without commencement of any empirical antibiotic for the lytic lesion of bone as seen on a radiograph, keeping in mind the endemicity of tuberculosis, essential investigations for tubercular dactylitis should be done as illustrated in Standard Treatment Workflow (STW) for management of Paediatric Osteoarticular tuberculosis [7]. Guided (CT or C-arm) biopsy for histopathological or microbiological diagnosis should be considered as secondary investigation, if and when inconclusive results are obtained after radiograph of the involved part, with chest X-ray and FNAC [7,8]. The paucibacillary nature of disease in some cases may lead to negative laboratory results, therefore, in such cases therapeutic trial of ATT can be considered on the basis of strong clinical suspicion [9].
Based on the suspicion and clinical workup in the line of Spina Ventosa, crucial time was saved in our case as a delay in diagnosis can lead to systemic manifestations which could be limb and life-threatening and even add to the increase in rate of morbidity. A case report by Ngoc et al. [10] showed a boy in his middle childhood having swelling of metacarpals, metatarsals, and phalanges of his hands and feet past six years old, that was misdiagnosed as skeletal dysplasia. Ultrasound examination revealed systemic manifestations-ascites, pleural effusion, and pericardial involvement, which was absent earlier. Laboratory investigations diagnosed the patient with Spina Ventosa. A case studied by Bhaskar et al. of a malnourished girl with tuberculous dactylitis presented after five months of symptoms with axillary scrofuloderma [2].
Bandyopadhyay et al. published a case report of a toddler who presented with swelling of a right middle metacarpal which was earlier diagnosed with enchondroma but later histopathology revealed tuberculous dactylitis [11]. Agarwal et al. [12] published a case report of a female in her early adolescence with swelling over the dorsum of the right hand near the base of the middle finger for five months with discharging sinus. Considering the case of abscess, empirical antibiotics were given to the patient, but the condition was not resolved. Microbiological examination of the abscess by fluorescent auramine staining confirmed the diagnosis to be Spina Ventosa and patient was started on ATT. One of the classical characteristic features of “Spina Ventosa” is the involvement of flexor tendon sheaths sparing the joint synovium and bones in adults which was also presented in our case report finding [1].
One limitation of our report can be that there is no culture proof of Mycobacterium Tuberculosis and this can be mislaid with a Non Tubercular Mycobacterium (NTM) which would also respond to prolonged ATT. However, CBNAAT was done to confirm the diagnosis of the case.
Thus, in order to avoid missing such cases, one should evaluate the patient thoroughly as guided by standard treatment workflow (STW). Being endemic in the Indian subcontinent, the government has started an anti-tubercular therapy (ATT) regime under the National Tuberculosis Elimination Program in 1997 which proves to be the game changer in the outcome of the treatment. The paediatric cases reported so far have been summarized along with the treatment outcomes in the tabular form below (Table 1). In all the paediatric cases documented, authors reported good treatment outcomes in patients after a course of ATT.
Table 1.
A literature review of Paediatric Spina Ventosa over the past 20 years
| Researcher (Year) | No. of cases included | Age/Site of involvement | Treatment outcome |
|---|---|---|---|
| Ankur Agarwal et al. (2021) [12] | One | 12 years old/Proximal phalanx middle finger | ATT was started with volar plaster followed by functional bracing. Lesion healed with slight shortening due to bony destruction |
| Sang Nguyen Ngoc et al. (2021) [10] | One | Seven-year-old/Metacarpals, Metatarsals, and phalanges of hands and feet later having pleural and pericardial effusion | Despite the delay in diagnosis, fully recovered after ATT |
| Cansu DU et al. (2021) [13] | One | 19 years old/Right wrist spreading to fifth finger | Successfully treated with ATT |
| Abebe W et al. (2016) [14] | One | Four-year old/Left index finger | Successfully treated with ATT, with good functional outcome |
| Sharma S et al. (2015) [1] | One | Eight-year-old/Ring finger metacarpal, Diagnosed with lupus vulgaris with lymphadenopathy along with Spina Ventosa | Patient treated with ATT |
| Bhasker et al. (2013) [2] | One | Eight-year old/Left index finger proximal phalanx with draining axillary ulcer with Lymphadenopathy | Healing of lesion with ATT without any surgery |
| Bandyopadhyay R et al. (2012) [11] | One | Two-year old/Right Bony hard swelling over middle metacarpal | Treated with Excision followed by strut grafting with fibula, post-op ATT with successful outcome |
| Patra SR (2009) [15] | One | 17 years old/middle phalanx of right middle finger | Swelling healed after ATT completion but with terminal restriction in finger movements |
| Gyanshankar PM et al. (2009) [16] | One | 15 years old/swelling with discharging sinus in Left foot Third digit | Swelling disappeared with healing of discharging sinus after course of ATT |
| Andronikou S et al. (2002) [17] | One | Nine-year old/Fourth finger of Right hand | Successfully treated with ATT |
Disclosure of conflict of interest
None.
References
- 1.Sharma S, Sood S, Gupta M. Spina ventosa with lupus vulgaris and lymphadenopathy: multifocal tuberculosis. Indian Dermatol Online J. 2015;6(Suppl 1):S40–2. doi: 10.4103/2229-5178.171042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhaskar, Khonglah T, Bareh J. Tuberculous dactylitis (spina ventosa) with concomitant ipsilateral axillary scrofuloderma in an immunocompetent child: a rare presentation of skeletal tuberculosis. Adv Biomed Res. 2013;2:29. doi: 10.4103/2277-9175.107993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albornoz MA, Mezgarzedeh M, Neumann CH, Myers AR. Granulomatous tenosynovitis: a rare musculoskeletal manifestation of tuberculosis. Clin Rheumatol. 1998;17:166–9. doi: 10.1007/BF01452268. [DOI] [PubMed] [Google Scholar]
- 4.Sunderamoorthy D, Gupta V, Bleetman A. TB or not TB: an unusual sore finger. Emerg Med J. 2001;18:490–1. doi: 10.1136/emj.18.6.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Vuyst D, Vanhoenacker F, Gielen J, Bernaerts A, De Schepper AM. Imaging features of musculoskeletal tuberculosis. Eur Radiol. 2003;13:1809–19. doi: 10.1007/s00330-002-1609-6. [DOI] [PubMed] [Google Scholar]
- 6.Jensen CM, Jensen CH, Paerregaard A. A diagnostic problem in tuberculous dactylitis. J Hand Surg Br. 1991;16:202–3. doi: 10.1016/0266-7681(91)90177-p. [DOI] [PubMed] [Google Scholar]
- 7.Training Module on Extrapulmonary TB [Internet] Available from: https://tbcindia.gov.in/WriteReadData/l892s/7702334778Training_Module_on_Extrapulmonary_TB_-_Book_24032023.pdf.
- 8.Paediatric Osteoarticular TB [Internet] Available from: https://stw.icmr.org.in/images/Paediatric_Tuberculosis/4_Paediatric_Osteoarticular_TB.pdf.
- 9.Vardhan V, Yanamandra U. Diagnosis of osteoarticular tuberculosis. Indian J Rheumatol. 2011;6:87–94. [Google Scholar]
- 10.Nguyen Ngoc S, Nguyen Thai H, Vu Van Q, Vu Tung L, Nguyen Ngoc R, Nguyen Van H. Late discovering Spina Ventosa: a case report. Int Med Case Rep J. 2021;14:449–53. doi: 10.2147/IMCRJ.S318003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandyopadhyay R, Mukherjee A, Mondal RK. Case report: “Spina Ventosa” tuberculous dactylitis in a 2 year old boy - a very rare disease. Open Orthop J. 2012;6:118–20. doi: 10.2174/1874325001206010118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agarwal A, Agarwal S, Singh S, Nandwani S. Spina Ventosa: an often missed diagnosis. J Glob Infect Dis. 2021;13:36–37. doi: 10.4103/jgid.jgid_198_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cansu DÜ, Bodakçi E, Canaz F, Çalişir C, Korkmaz C. A challenge of tuberculosis for rheumatologists: a case of Spina Ventosa developing during anti-tumor necrosis factor treatment. J Clin Rheumatol. 2021;27:e186–e187. doi: 10.1097/RHU.0000000000001333. [DOI] [PubMed] [Google Scholar]
- 14.Abebe W, Abebe B, Molla K, Alemayehu T. Tuberculous dactylitis: an uncommon presentation of skeletal tuberculosis. Ethiop J Health Sci. 2016;26:301–3. doi: 10.4314/ejhs.v26i3.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patra SR. Tubercular dactylitis (spina ventosa) Postgrad Med J. 2009;85:699–700. doi: 10.1136/pgmj.2009.087197. [DOI] [PubMed] [Google Scholar]
- 16.Gyanshankar PM, Dhamgaye TM, Amol BF. Spina Ventosa discharging tubercle bacilli--a case report. Indian J Tuberc. 2009;56:100–3. [PubMed] [Google Scholar]
- 17.Andronikou S, Smith B. “Spina ventosa”--tuberculous dactylitis. Arch Dis Child. 2002;86:206. doi: 10.1136/adc.86.3.206. [DOI] [PMC free article] [PubMed] [Google Scholar]