Abstract
Aim: To explore the effect of a multidisciplinary team (MDT) nursing model based on enhanced recovery after surgery (ERAS) in total hip arthroplasty (THA)/total knee arthroplasty (TKA) and evaluate its application in the perioperative period of patients. Methods: A retrospective analysis was conducted on 100 patients with THA/TKA treated at Shaoxing Second Hospital Medical Community General Hospital from January 2021 to December 2023. The patients were divided into an observation group (n = 50) and a control group (n = 50) based on the nursing method employed. The control group received traditional perioperative nursing, while the observation group received an MDT nursing model intervention based on the ERAS concept. Visual analogue scale (VAS) scores were recorded at 6, 24, and 72 hours post-surgery. Additionally, postoperative activities, hospitalization duration, and postoperative complications were documented. Differences in knee joint range of motion (ROM), hip Harris score, psychological stress response score, and quality of life score between the two groups before and one month after surgery were analyzed. Results: At 6, 24, and 72 hours post-surgery, patients in the observation group had significantly lower VAS scores compared to those in the control group (all P < 0.05). The observation group had an earlier first-time mobilization (P < 0.05). The length of hospitalization and hospitalization cost were significantly lower in the observation group than in the control group (both P < 0.05). The incidence rates of postoperative adverse reactions were 22.00% in the control group and 6.00% in the observation group (P < 0.05). One month post-surgery, the observation group showed significantly greater ROM, lower psychological stress and reaction scores, and higher Harris score and quality of life score compared to the control group (all P < 0.05). Conclusion: The MDT nursing model based on ERAS concept for THA/TKA perioperative patients effectively alleviates postoperative pain, promotes early activity, shortens hospital stay, reduces hospital cost, decreases the incidence of complications, restores joint function, enhances quality of life, and reduces psychological stress.
Keywords: Knee and hip arthroplasty, rapid rehabilitation concept, multidisciplinary collaboration, perioperative period, nursing care
Introduction
Artificial arthroplasty is recognized as an effective treatment for end-stage hip and knee disorders [1]. The incidence of hip and knee injuries is increasing annually, leading to a growing demand for total hip arthroplasty (THA) and total knee arthroplasty (TKA) surgeries [2]. Studies have shown that effective postoperative nursing care for THA/TKA patients is crucial for their rehabilitation [3]. Current perioperative nursing measures for clinical THA/TKA include evidence-based nursing, enhanced recovery after surgery (ERAS), and multidisciplinary treatment (MDT) [4].
ERAS is an evidence-based and effective perioperative management program [5], with its application in joint surgery being well-established [6,7]. It aims to reduce the stress of surgical trauma, decrease the incidence of complications, enhance surgical safety, increase patient satisfaction, and promote rapid recovery [8]. MDT is essential for the effective implementation of ERAS. It involves a collaborative medical model where professionals from two or more disciplines provide specialized advice and medical services, and develop relevant programs around medical issues [9]. This model has been extensively implemented in medical education and clinical practice [10,11].
However, research on the MDT care model based on the ERAS concept in clinical settings is limited, particularly in the perioperative care of THA/TKA patients. This study aimed to analyze the effects of conventional perioperative nursing intervention and the MDT nursing model based on the ERAS concept in 100 THA/TKA cases. The goal was to provide new insight for perioperative nursing care of THA/TKA patients.
Materials and methods
Subjects
This retrospective study was conducted from January 2021 to December 2023, involving 100 patients with THA/TKA at Shaoxing Second Hospital Medical Community General Hospital.
Inclusion Criteria: Patients met the diagnostic criteria for hip and knee joint lesions [12]. Patients had indications for THA/TKA and were undergoing their first surgeries. Patients had unilateral osteoarthritic diseases.
Exclusion Criteria: Patients with fractures in other parts of the body. Patients with mental disorders. Patients with infectious diseases.
The patients were divided into a control (n = 50) and an observation (n = 50) group. In the control group, there were 21 females and 29 males, with ages ranging from 43 to 77 years (58.26±8.18). The affected joints included 27 hips and 23 knees, with the following types of surgery: 15 left THA, 12 right THA, 13 left TKA, and 10 right TKA.
In the observation group, there were 32 males and 18 females, with ages ranging from 45 to 78 years (58.42±9.79). The affected joints included 25 hips and 25 knees, with the following types of surgery: 15 left THA, 10 right THA, 14 left TKA, and 11 right TKA.
This study was approved by the Ethics Committee of Shaoxing Second Hospital Medical Community General Hospital.
Methods
The control group received routine perioperative nursing interventions as follows:
Preoperative Care: Medical staff explained to patients and their families the purpose and significance of THA/TKA and the methods of postoperative rehabilitation exercises. Patients fasted for 12 hours and abstained from water for 6 hours before surgery. Hypnotic drugs were administered as needed for patients who were tense and anxious, according to the doctor’s instructions.
Intraoperative Care: Continuous epidural anesthesia was administered.
Postoperative Care: Intravenous patient-controlled analgesia was used as prescribed by the doctor. Nausea and vomiting were managed with symptomatic treatment. Patients were forbidden from eating for 6 hours postoperatively, given semi-liquid food after 24 hours, and resumed a normal diet after 48 hours. Low molecular weight heparin was injected subcutaneously as prescribed by the doctor 12 hours postoperatively. Patients were instructed to perform passive leg-lifting exercises 6 hours after surgery, sit at the edge of the bed 1 day after surgery, actively flex their knees, and begin walking with the aid of walking devices 2 days after surgery. Patients were instructed to continue taking oral anticoagulant drugs until 35 days postoperatively.
The observation group received the MDT nursing model intervention based on the ERAS concept, with the following initiatives:
Formation of the MDT Intervention Team: Team Leader: 1 director of orthopedics. Surgical Plan Developer: 1 attending orthopedic physician. Quality Control Manager: 1 orthopedic nurse leader. Nursing Interventions and Coordination: 3 orthopedic nurses. Rehabilitation Plan Developer and Assessor: 1 rehabilitation physician. Pain Assessment: 1 pain specialist nurse. Nutritional Status Assessment and Dietary Protocol Developer: 1 nutritionist. Psychological Counselor: 1 counselor to intervene for patients with high psychological risk and provide psychological counseling. Anesthesia and Analgesia Protocol Developer: 1 anesthesiologist. All team members were trained and qualified for their respective roles.
Constructing the MDT Nursing Program: The MDT nursing program was developed through literature search of relevant guidelines, expert consensus, and evidence summaries on the evaluation and prevention of THA/TKA. Systematic assessment and analysis of patients were conducted after admission to formulate the MDT nursing program based on the ERAS concept. Rehabilitation goals were clarified, and targeted nursing interventions were provided to patients.
Preoperative Care: Patients were asked about smoking and alcohol consumption and advised to quit both. Anemia condition and causes were clarified; if hemoglobin levels were < 130 g/L, EPO and iron sucrose treatment was administered per the doctor’s instructions. Protein intake was forbidden for 6 hours, carbohydrates for 4 hours, and clear liquids for 2 hours before surgery. NSAIDs were taken orally for hyperalgesia before surgery. Patients were instructed in sputum expectoration training to prepare for postoperative expectoration. Videos, pictures, and teaching manuals were used to explain the ERAS concept and THA/TKA process to alleviate patient anxiety and depression. Psychological counselors used the Self-Depression Scale (SDS) and the Self-Anxiety Scale (SAS) to assess psychological status, providing timely counseling when abnormalities were found.
Intraoperative Care: Heat Preservation and Anesthesia: The operating table was equipped with cool pads, and electric blankets were used to warm the patient 1 hour before the operation. Continuous epidural anesthesia was administered, and the affected limbs were subjected to femoral nerve blocks. Inflatable heat preservation blankets were used, and the patient’s body temperature was monitored in real-time. Intraoperative rinsing fluids and medicinal fluids were warmed to 37°C in a heat preservation box before use.
Rehydration: Anesthesiologists strictly controlled the patient’s rehydration. Bleeding Control: A tourniquet was used before osteotomy, and 10 minutes before skin incision, 1 g of tranexamic acid was injected intravenously. Non-negative pressure drainage tubes were placed, and negative pressure was removed 30 minutes before removal.
Postoperative Care: Analgesia: Postoperative pain was assessed using the Visual Analogue Scale (VAS) by the pain department nurse. Multi-modal analgesic interventions were implemented based on the VAS score: For VAS scores ≤ 3, physical interventions such as listening to music were used to divert the patient’s attention. For VAS scores > 4, non-steroidal anti-inflammatory drugs were administered as appropriate.
Nausea and Vomiting Prevention: Patients were positioned with a slight head elevation. Azasetron hydrochloride was administered by IV drip for 2 days.
Eating: A nutritionist assessed the patient’s risk of malnutrition. If no abnormalities were found, patients were allowed to consume light, easily digestible liquid food rich in protein and vitamins 6 hours after surgery.
Functional Exercise: Upon returning to the ward, patients received local massages. After waking, patients were encouraged to start static quadriceps contractions, ankle pumping exercises, and active upper limb exercises. Rehabilitation doctors informed patients and their families about the nature and severity of agoraphobia, encouraging immediate mobilization. Patients in both groups received interventions until discharge and returned for follow-up 1 month after surgery.
Observation indicators
Pain Assessment: Pain levels were assessed preoperatively, and at 6, 24, and 72 hours postoperatively using the VAS, which ranges from 0 to 10. Higher scores indicate greater pain levels [13].
Postoperative Activities: The time to first mobilization, duration of the first mobilization, and distance walked during the first mobilization were recorded for both patient groups post-surgery.
Hospitalization: The length of hospital stay and hospital expenses were recorded.
Safety Evaluation: The occurrence of postoperative complications in both groups was documented.
Knee Joint Range of Motion (ROM) and Hip Joint Function: A joint mobility goniometer was used to measure knee joint ROM before and one month after surgery, with the average value taken from three measurements. Hip joint recovery was evaluated using the Harris Hip Scale, where higher scores indicate better hip function [14].
Quality of Life: The General Quality of Life Questionnaire (GQOL-74) was used to assess quality of life before and one month after surgery. The questionnaire comprises four categories, each scored out of 100 points; higher scores indicate better quality of life [15].
Psychological Stress Response: Evaluated using the Psychological Stress Response Questionnaire (SRQ) developed by Jiang Qianjin’s team, referencing the SAS, SDS, and SCL-90 scales. The SRQ includes three dimensions: physical reaction (9 items), emotional reaction (12 items), and behavioral reaction (6 items), using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). Higher scores indicate more severe psychological stress. The SRQ has a Cronbach’s alpha coefficient of 0.902 [16].
Statistical analysis
Data were analyzed using SPSS 20.0. Measured data were expressed as mean ± standard deviation (SD). The t-test was used for comparisons between the two groups, and analysis of variance (ANOVA) was used for comparisons across multiple time points. Counted data were expressed as percentages (%), and the chi-square test was performed. A significance level of α = 0.05 was used for all tests.
Results
Comparison of general information
There was nosignificant difference in general data between the two groups (all P > 0.05). See Table 1.
Table 1.
Comparison of general data between the two groups
| Group | Gender [n/(%)] | Age (x̅±SD) | Diseased joint [n/(%)] | Type of surgery [n/(%)] | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Male | Female | Articulatio coxae | Articulatio genus | Left side THA | Right side THA | Left side TKA | Right side TKA | ||
| Control group (n = 50) | 29 (58.00) | 21 (42.00) | 58.26±8.18 | 27 (54.00) | 23 (46.00) | 15 (30.00) | 12 (24.00) | 13 (26.00) | 10 (20.00) |
| Observation group (n = 50) | 32 (64.00) | 18 (36.00) | 58.42±9.79 | 25 (50.00) | 25 (50.00) | 15 (30.00) | 10 (20.00) | 14 (28.00) | 11 (22.00) |
| X2/t-value | 0.378 | 0.089 | 0.160 | 0.267 | |||||
| P-value | 0.539 | 0.930 | 0.689 | 0.966 | |||||
Comparison of pain situation
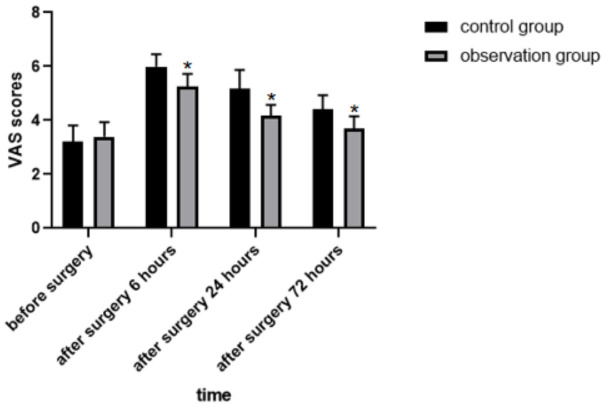
There was no significant difference in VAS scores between the two groups before surgery. The VAS scores at 6 h, 24 h, and 72 h postoperatively were higher than the preoperative scores in both groups (all P < 0.05). However, the VAS scores in the observation group at 6 h, 24 h, and 72 h postoperatively were lower than those in the control group (all P < 0.05). See Table 2 and Figure 1.
Table 2.
Comparison of VAS scores between the two groups at each time period (x±SD)
| Preoperative | 6 h postoperative | 24 h postoperative | 72 h postoperative | |
|---|---|---|---|---|
| Control group (n = 50) | 3.20±0.61 | 6.00±0.45* | 5.16±0.71* | 4.40±0.53* |
| Observation group (n = 50) | 3.40±0.53 | 5.24±0.48*,# | 4.18±0.39*,# | 3.68±0.47*,# |
| Finterblock/Pinterblock | 344.700/< 0.001 | |||
| Ftime/Ptime | 113.800/< 0.001 | |||
| Finteraction/Pinteraction | 24.350/< 0.001 | |||
Note: Compared to preoperative;
P < 0.05.
Compared to the control group;
P < 0.05.
VAS, Visual analogue scale.
Figure 1.
Comparison of VAS scores at each time period between the two groups. Note: Compared to the control group, *P < 0.05. VAS, Visual analogue scale.
Comparison of postoperative activities
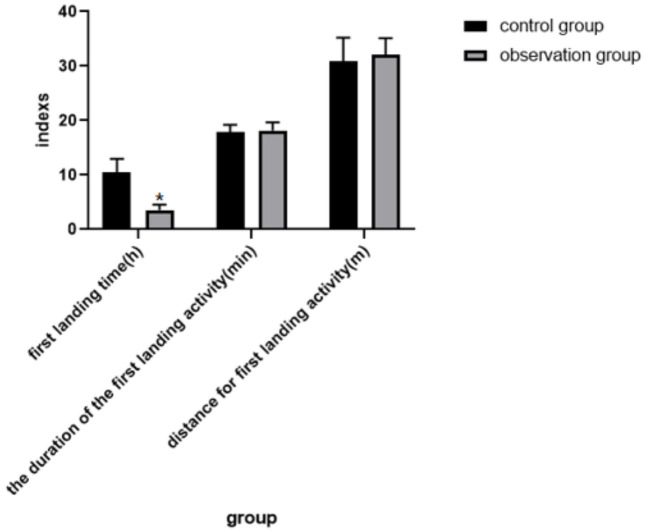
The first ambulation time of the observation group was earlier than that of the control group (P < 0.05). However, there was no significant difference in the duration or distance of the first ambulation between the two groups (all P > 0.05). See Table 3 and Figure 2.
Table 3.
Comparison of postoperative activities between the two groups (x±SD)
| Group | First time to get down to the ground (h) | Duration of first activity on the ground (min) | Distance of first activity on the ground (m) |
|---|---|---|---|
| Control group (n = 50) | 10.50±2.48 | 17.92±1.29 | 30.90±4.31 |
| Observation group (n = 50) | 3.56±0.99* | 18.18±1.49 | 30.12±3.00 |
| t-value | 18.377 | 0.933 | 1.050 |
| P-value | < 0.001 | 0.353 | 0.296 |
Note: Compared to Control group;
P < 0.05.
Figure 2.
Comparison of postoperative activities in both groups. Note: Compared to the control group, *P < 0.05.
Comparison of hospitalization
The hospitalization duration in the observation group was shorter, and the hospitalization cost was lower than that in the control group (both P < 0.05). See Table 4 and Figure 3.
Table 4.
Comparison of hospitalization in the two groups (x̅±s)
| Group | Duration of hospitalization (d) | Hospitalization expenses ($10,000) |
|---|---|---|
| Control group (n = 50) | 18.30±2.35 | 5.03±0.84 |
| Observation group (n = 50) | 13.52±2.87* | 3.77±0.43* |
| t-value | 9.112 | 9.441 |
| P-value | < 0.001 | < 0.001 |
Note: Compared to Control group;
P < 0.05.
Figure 3.
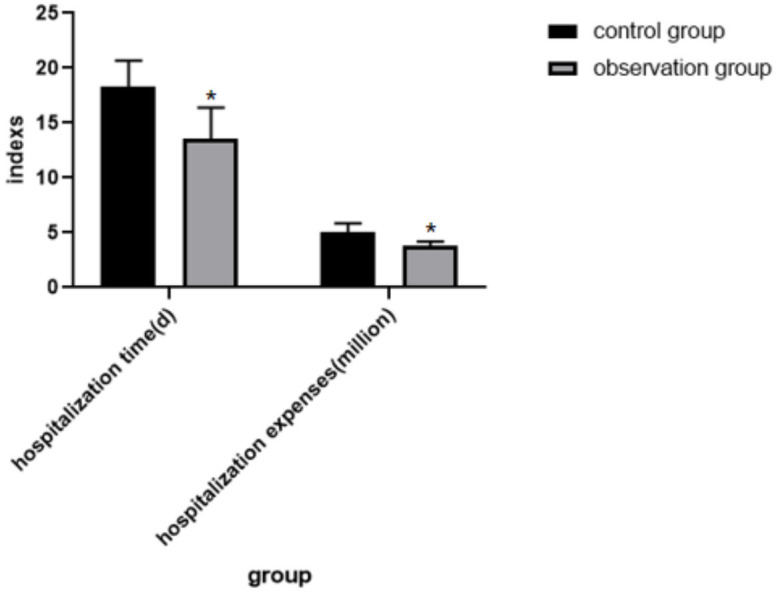
Comparison of hospitalization in the two groups. Note: Compared to the control group, *P < 0.05.
Comparison of safety evaluation
The incidence of postoperative adverse reactions was 22.00% in the control group and 6.00% in the observation group, with the observation group showing a lower incidence (P < 0.05). See Table 5 and Figure 4.
Table 5.
Comparison of the occurrence of postoperative adverse reactions in the two groups [n/(%)]
| Group | Nausea and vomiting | Poor incision healing | Deep vein thrombosis of lower limbs | Lung infection | Total |
|---|---|---|---|---|---|
| Control group (n = 50) | 5 (10.00) | 3 (6.00) | 2 (4.00) | 1 (2.00) | 11 (22.00) |
| Observation group (n = 50) | 1 (2.00) | 1 (2.00) | 1 (2.00) | 0 (0.00) | 3 (6.00)* |
| χ2-value | 5.316 | ||||
| P-value | 0.021 |
Note: Compared to Control group;
P < 0.05.
Figure 4.
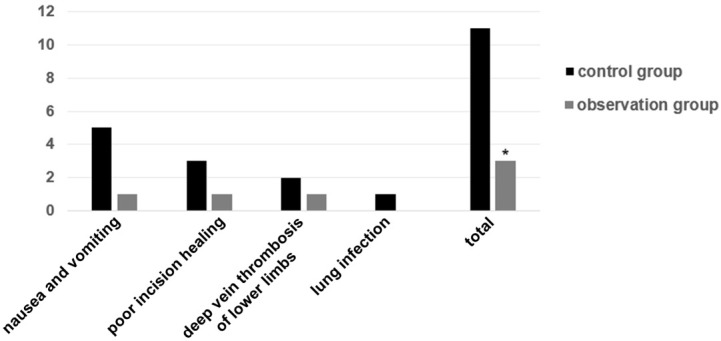
Comparison of the occurrence of adverse reactions between the two groups. Note: Compared to the control group, *P < 0.05.
Comparison of recovery of knee and hip joints
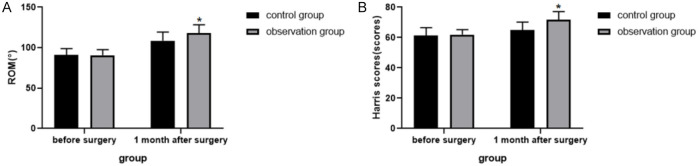
There was no significant difference in ROM or Harris score between the two groups before surgery. Compared to the preoperative values, both ROM and Harris scores increased at 1 month postoperatively in both groups (P < 0.05), with the observation group showing higher scores than the control group at 1 month postoperatively (P < 0.05). See Table 6 and Figure 5.
Table 6.
Comparison of ROM and Harris score between the two groups (x̅±s)
| Group | ROM (°) | Harris score (Score) | ||
|---|---|---|---|---|
|
|
|
|||
| Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | |
| Control group (n = 50) | 90.86±8.13 | 108.58±10.72* | 61.40±5.12 | 64.82±5.44* |
| Observation group (n = 50) | 90.50±7.10 | 118.24±10.12*,# | 61.94±3.30 | 71.62±5.48*,# |
| t-value | 0.236 | 4.633 | 0.627 | 6.227 |
| P-value | 0.814 | < 0.001 | 0.532 | < 0.001 |
Note: Compared to preoperative;
P < 0.05.
Compared to control group;
P < 0.05.
ROM, range of motion.
Figure 5.
Comparison of ROM and Harris scores in the two groups. A. ROM; B. Harris scores. Note: Compared to the control group, *P < 0.05. ROM, range of motion.
Comparison of quality of life
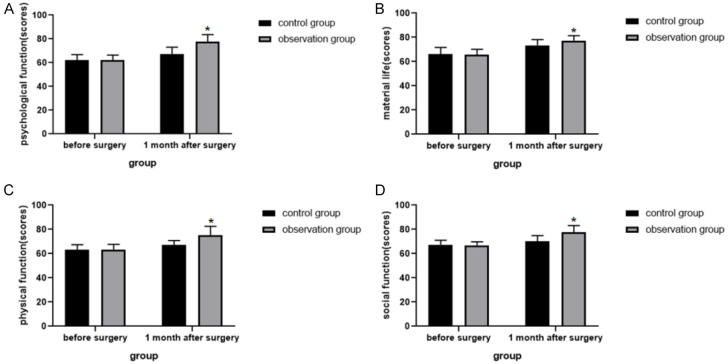
There was no significant difference in quality of life scores between the two groups before surgery. Compared to preoperative values, all quality of life indices improved at 1 month postoperatively in both groups (all P < 0.05), with the observation group showing higher scores than the control group at 1 month postoperatively (all P < 0.05). See Table 7 and Figure 6.
Table 7.
Comparison of quality of life scores between the two groups (x̅±s, Score)
| Group | Psychological functioning | Physical life | Somatic functioning | Social functioning | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | |
| Control group (n = 50) | 62.22±4.57 | 67.48±4.67* | 66.08±5.58 | 73.40±4.79* | 63.30±4.08 | 67.18±4.51* | 67.38±3.65 | 70.10±4.81* |
| Observation group (n = 50) | 62.18±4.16 | 77.60±6.00*,# | 65.78±4.43 | 77.42±4.04*,# | 63.48±4.12 | 75.10±7.43*,# | 66.98±2.77 | 77.58±5.59*,# |
| t-value | 0.046 | 9.412 | 0.298 | 4.536 | 0.220 | 6.443 | 0.617 | 7.172 |
| P-value | 0.964 | < 0.001 | 0.767 | < 0.001 | 0.827 | < 0.001 | 0.539 | < 0.001 |
Note: Compared to preoperative;
P < 0.05.
Compared to the control group;
P < 0.05.
Figure 6.
Comparison chart of the quality of life scores of the two groups. A. Psychological function; B. Material life; C. Somatic function; D. Social function. Note: Compared to the control group, *P < 0.05.
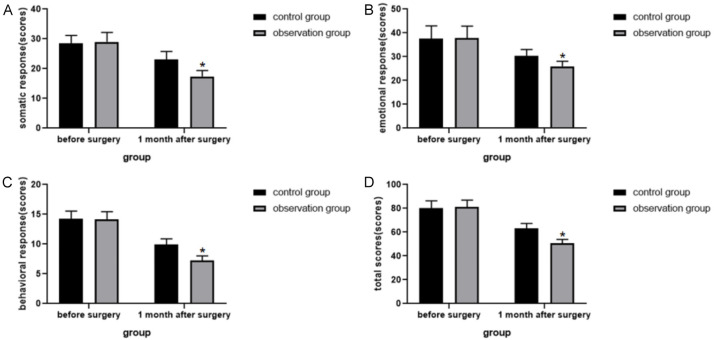
Comparison of psychological stress reaction
There was no significant difference in psychological stress reaction scores between the two groups before surgery. Compared to preoperative values, all indices of psychological stress reaction increased at 1 month postoperatively in both groups (all P < 0.05), with the observation group showing higher scores than the control group at 1 month postoperatively (all P < 0.05). See Table 8 and Figure 7.
Table 8.
Comparison of psychological stress reaction scores between the two groups (x̅±s, Score)
| Group | Somatic response | Emotional response | Behavioral response | Total score | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | Preoperative | 1 month postoperative | |
| Control group (n = 50) | 28.48±2.65 | 23.00±2.76* | 37.60±5.34 | 30.38±2.63* | 14.22±1.30 | 9.90±0.97* | 80.30±5.98 | 63.28±4.02* |
| Observation group (n = 50) | 28.96±3.23 | 17.38±2.00*,# | 37.76±5.09 | 25.92±2.19*,# | 14.12±1.30 | 7.22±0.79*,# | 81.18±5.68 | 50.52±3.32*,# |
| t-value | 0.812 | 11.659 | 0.153 | 9.215 | 0.385 | 15.148 | 0.754 | 17.306 |
| P-value | 0.419 | < 0.001 | 0.878 | < 0.001 | 0.701 | < 0.001 | 0.452 | < 0.001 |
Note: Compared with preoperative;
P < 0.05.
Compared to the control group;
P < 0.05.
Figure 7.
Graph of psychological stress response scores for both groups. A. Somatic response; B. Emotional response; C. Behavioral response; D. Total score. Note: Compared to the control group, *P < 0.05.
Discussion
With advancements in healthcare and the pursuit of better living conditions, the demand for arthroplasty has significantly increased, particularly among the elderly. THA and TKA have a great impact on patients’ short-term mobility, requiring them to be bedridden during the postoperative period. This immobility can lead to a decline in gastrointestinal and lung function, decubitus ulcers, venous thrombosis of the lower extremities, loss of myosin, insulin resistance, and impaired tissue oxygenation, all of which hinder postoperative recovery.
The ERAS concept, proposed by the European Surgeons’ Group in 2001, aims to reduce hospital stay length, promote a rapid return to normal activities, reduce complications, and lower surgery-related costs [17]. ERAS has been widely and successfully applied in liver surgery [18,19], pancreaticoduodenectomy [20], gynecological surgery [21], and other surgical procedures. It involves various perioperative interventions that require collaboration among surgery, anesthesiology, intensive care, and specialist nursing departments to achieve optimal results.
The MDT approach is an emerging therapeutic care model that emphasizes multidisciplinary cooperation and scientific collaboration among various disciplines [22]. This model effectively integrates healthcare resources and maximizes therapeutic outcome [23]. Previous studies have confirmed that MDT promotes the integrated allocation of medical resources [24], reduces healthcare costs [25], and improves the quality and efficiency of clinical work [26].
In this study, the ERAS concept-based MDT nursing model intervention was implemented for THA/TKA patients. It was found that, compared to conventional perioperative nursing, individuals in the observation group mobilized earlier, had shorter hospital stays, and incurred lower hospital expenses. This indicates that the ERAS concept-based MDT nursing model effectively promotes early mobilization, shortens hospital stays, and reduces hospital expenses. This effectiveness may be attributed to the comprehensive intervention covering multiple aspects of the patients’ rehabilitation.
Preoperatively, factors such as smoking, alcohol consumption, anemia, and nutrition are significant risk factors leading to complications and prolonged hospital stays in patients undergoing arthroplasty [27]. Screening and intervening in these preoperative risk factors can reduce the number of patients experiencing delayed recovery and lay a solid physical foundation for the subsequent THA/TKA. Postoperative nutritional support and encouraging early mobilization can promote recovery, shorten hospital stays, and reduce hospitalization costs.
The study also found postoperative adverse response rates of 22.00% in the control group and 6.00% in the observation group. The lower incidence of postoperative complications in the observation group suggests that the MDT nursing model based on the ERAS concept can reduce this incidence rate. This reduction may be attributed to the successful prevention of various adverse events through the measures included in the MDT nursing intervention based on the ERAS concept.
Preoperative disease education and psychological counseling for patients and their families provide accurate information, alleviating anxiety, depression, and other adverse moods. The administration of non-steroidal anti-inflammatory drugs (NSAIDs) as over-the-counter analgesics to postoperative patients has been shown to significantly decrease the occurrence of complications, including nausea and vomiting [28]. Additionally, allowing patients to consume clear liquids 2 hours before surgery and providing oral feeding after surgery helps alleviate postoperative pain [29]. By preheating and humidifying anesthetic gases, warming rinsing fluids, using heating blankets, and warming infused fluids, the accelerated metabolism due to hypothermia and the incidence of related complications were effectively avoided [30]. The administration of tranexamic acid effectively reduces intraoperative blood loss [31,32], contributing to a lower complication rate. Pain management is crucial for facilitating early discharge, promoting rehabilitation, and increasing patient satisfaction after THA/TKA [33]. Kugelman et al. [34] noted that pain management in THA and TKA patients promotes postoperative functional recovery. Simpson et al. [35] found that pain management in ERAS benefits postoperative pain relief and recovery.
At 6, 24, and 72 hours postoperatively, patients in the observation group showed significantly lower VAS scores than those in the control group. Additionally, one month postoperatively, the observation group had higher Harris scores and ROM compared to the control group. These results suggest that MDT nursing intervention based on the ERAS concept effectively reduces postoperative pain and promotes joint function recovery. This may be related to postoperative multimodal analgesia and early mobilization. Studies have shown that local infiltration of narcotic analgesics around joint replacements helps relieve pain and reduce the incidence of postoperative delirium [36]. Post-arthroplasty, non-steroidal anti-inflammatory drugs and intermittent ice packs were used to reduce swelling and pain, providing multimodal analgesia throughout the perioperative period. This enabled patients to get out of bed early with assistance, aiding joint functionality restoration.
This study revealed that the observation group had higher quality of life scores and lower psychological stress scores compared to the control group. These results suggest that the MDT nursing model intervention used in this research improves patients’ well-being and reduces emotional distress.
Limitations of the study include that its sample size was small, and the follow-up period was only one month. Future studies should include larger sample sizes and longer follow-up periods for more in-depth exploration.
In summary, MDT nursing intervention based on the ERAS concept effectively relieves postoperative pain in THA/TKA patients, shortens hospitalization time, reduces hospitalization expense, lowers the risk of complications, improves joint function, enhances quality of life, and reduces psychological stress. This approach shows high practicality for clinical practice.
Disclosure of conflict of interest
None.
References
- 1.Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the United States: future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019;46:1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 2.Sabeh KG, Hernandez VH, Cohen-Levy WB, Ong A, Orozco F, Bennett V, Post Z. The effects of patient occupation, hobbies, and body mass index on kneeling after total knee arthroplasty. J Knee Surg. 2021;34:772–776. doi: 10.1055/s-0039-3400740. [DOI] [PubMed] [Google Scholar]
- 3.Kimball CC, Nichols CI, Nunley RM, Vose JG, Stambough JB. Skilled nursing facility star rating, patient outcomes, and readmission risk after total joint arthroplasty. J Arthroplasty. 2018;33:3130–3137. doi: 10.1016/j.arth.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 4.Specht K, Kjaersgaard-Andersen P, Kehlet H, Pedersen BD. Nursing in fast-track total hip and knee arthroplasty: a retrospective study. Int J Orthop Trauma Nurs. 2015;19:121–130. doi: 10.1016/j.ijotn.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. 2022;11:121–129. doi: 10.2217/cer-2021-0258. [DOI] [PubMed] [Google Scholar]
- 6.Debono B, Wainwright TW, Wang MY, Sigmundsson FG, Yang MMH, Smid-Nanninga H, Bonnal A, Le Huec JC, Fawcett WJ, Ljungqvist O, Lonjon G, de Boer HD. Consensus statement for perioperative care in lumbar spinal fusion: enhanced recovery after surgery (ERAS®) society recommendations. Spine J. 2021;21:729–752. doi: 10.1016/j.spinee.2021.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Naftalovich R, Singal A, Iskander AJ. Enhanced recovery after surgery (ERAS) protocols for spine surgery - review of literature. Anaesthesiol Intensive Ther. 2022;54:71–79. doi: 10.5114/ait.2022.113961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bogani G, Sarpietro G, Ferrandina G, Gallotta V, DI Donato V, Ditto A, Pinelli C, Casarin J, Ghezzi F, Scambia G, Raspagliesi F. Enhanced recovery after surgery (ERAS) in gynecology oncology. Eur J Surg Oncol. 2021;47:952–959. doi: 10.1016/j.ejso.2020.10.030. [DOI] [PubMed] [Google Scholar]
- 9.St-Louis J, Chowdary P, Dolan G, Goodyear D, Strike K, Pollard D, Teitel J. Multidisciplinary team care of patients with hemophilic arthropathy: a qualitative assessment of contemporary practice in the UK and Canada: Canada/UK: MDT practices for hemophilia. Clin Appl Thromb Hemost. 2022;28:10760296211070002. doi: 10.1177/10760296211070002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whalen E, Ely E, Brown A. The role of a multidisciplinary team in a pediatric pulmonary hypertension center. Pediatr Pulmonol. 2021;56:630–635. doi: 10.1002/ppul.24761. [DOI] [PubMed] [Google Scholar]
- 11.Janssen A, Donnelly C, Kay J, Thiem P, Saavedra A, Pathmanathan N, Elder E, Dinh P, Kabir M, Jackson K, Harnett P, Shaw T. Developing an intranet-based lymphedema dashboard for breast cancer multidisciplinary teams: design research study. J Med Internet Res. 2020;22:e13188. doi: 10.2196/13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conklin MJ, Kishan S, Nanayakkara CB, Rosenfeld SR. Orthopedic guidelines for the care of people with spina bifida. J Pediatr Rehabil Med. 2020;13:629–635. doi: 10.3233/PRM-200750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain. 2019;20:245–263. doi: 10.1016/j.jpain.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Ganzer D, Forke L, Irlenbusch U. Two-year follow-up of revision total hip arthroplasty using a ceramic revision head with a retained well-fixed femoral component: a case series. J Med Case Rep. 2014;8:434. doi: 10.1186/1752-1947-8-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong Y, Yan H, Wurichayihu, Zhang G. The effects of comprehensive nursing interventions on the negative emotions, quality of life, and nursing satisfaction in intracerebral hemorrhage patients. Am J Transl Res. 2021;13:4860–4867. [PMC free article] [PubMed] [Google Scholar]
- 16.Janssen A, Donnelly C, Kay J, Thiem P, Saavedra A, Pathmanathan N, Elder E, Dinh P, Kabir M, Jackson K, Harnett P, Shaw T. Developing an intranet-based lymphedema dashboard for breast cancer multidisciplinary teams: design research study. J Med Internet Res. 2020;22:e13188. doi: 10.2196/13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–641. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal V, Divatia JV. Enhanced recovery after surgery in liver resection: current concepts and controversies. Korean J Anesthesiol. 2019;72:119–129. doi: 10.4097/kja.d.19.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joliat GR, Kobayashi K, Hasegawa K, Thomson JE, Padbury R, Scott M, Brustia R, Scatton O, Tran Cao HS, Vauthey JN, Dincler S, Clavien PA, Wigmore SJ, Demartines N, Melloul E. Guidelines for perioperative care for liver surgery: enhanced recovery after surgery (ERAS) society recommendations 2022. World J Surg. 2023;47:11–34. doi: 10.1007/s00268-022-06732-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, Wellge EB, Kunzler F, Besselink MG, Asbun H, Scott MJ, Dejong CHC, Vrochides D, Aloia T, Izbicki JR, Demartines N. Guidelines for perioperative care for pancreatoduodenectomy: enhanced recovery after surgery (ERAS) recommendations 2019. World J Surg. 2020;44:2056–2084. doi: 10.1007/s00268-020-05462-w. [DOI] [PubMed] [Google Scholar]
- 21.Chao L, Lin E, Kho K. Enhanced recovery after surgery in minimally invasive gynecologic surgery. Obstet Gynecol Clin North Am. 2022;49:381–395. doi: 10.1016/j.ogc.2022.02.014. [DOI] [PubMed] [Google Scholar]
- 22.Staudt MD. The multidisciplinary team in pain management. Neurosurg Clin N Am. 2022;33:241–249. doi: 10.1016/j.nec.2022.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Nagaoka E, Arai H, Ugawa T, Masuda T, Ochiai K, Tamaoka M, Kurashima N, Oi K, Fujiwara T, Yoshida M, Shigemitsu H, Otomo Y. Efficacy of multidisciplinary team approach with extracorporeal membrane oxygenation for COVID-19 in a low volume ECMO center. Artif Organs. 2021;45:1061–1067. doi: 10.1111/aor.13947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDermott L, Kalluri M, Fox K, Richman-Eisenstat J. Redesigning interstitial lung disease clinic care through interprofessional collaboration. J Interprof Care. 2022;36:64–74. doi: 10.1080/13561820.2021.1884051. [DOI] [PubMed] [Google Scholar]
- 25.Iskander J, Ari M, Chen B, Hall S, Ghiya N, Popovic T. Public health grand rounds at the centers for disease control and prevention: evaluation feedback from a broad community of learners. J Public Health Manag Pract. 2014;20:542–50. doi: 10.1097/PHH.0b013e3182aa6560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu C, Liu X, Wu F, Xie M, Feng Y, Hu C. Using artificial intelligence (watson for oncology) for treatment recommendations amongst chinese patients with lung cancer: feasibility study. J Med Internet Res. 2018;20:e11087. doi: 10.2196/11087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hansen TB, Bredtoft HK, Larsen K. Preoperative physical optimization in fast-track hip and knee arthroplasty. Dan Med J. 2012;59:A4381. [PubMed] [Google Scholar]
- 28.Xuan C, Yan W, Wang D, Li C, Ma H, Mueller A, Chin V, Houle TT, Wang J. Efficacy of preemptive analgesia treatments for the management of postoperative pain: a network meta-analysis. Br J Anaesth. 2022;129:946–958. doi: 10.1016/j.bja.2022.08.038. [DOI] [PubMed] [Google Scholar]
- 29.Awad S, Stephenson MC, Placidi E, Marciani L, Constantin-Teodosiu D, Gowland PA, Spiller RC, Fearon KC, Morris PG, Macdonald IA, Lobo DN. The effects of fasting and refeeding with a ‘metabolic preconditioning’ drink on substrate reserves and mononuclear cell mitochondrial function. Clin Nutr. 2010;29:538–544. doi: 10.1016/j.clnu.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Li J, Zhao F, Gao J, Dong W, Yu X, Zhu C, Liu S, Jiang X, Liu G. Enhanced recovery after surgery (ERAS) protocol in geriatric patients underwent unicompartmental knee arthroplasty: a retrospective cohort study. Medicine (Baltimore) 2023;102:e32941. doi: 10.1097/MD.0000000000032941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chambers S, Tidwell L, Kerkhof A, Smith R, Mihalko WM. Topical tranexamic acid is effective in cementless total knee arthroplasty. Orthop Clin North Am. 2020;51:7–11. doi: 10.1016/j.ocl.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Denry I, Nédélec JM, Holloway JA. Tranexamic acid-loaded hemostatic nanoclay microsphere frameworks. J Biomed Mater Res B Appl Biomater. 2022;110:422–430. doi: 10.1002/jbm.b.34918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Latijnhouwers DAJM, Martini CH, Nelissen RGHH, Verdegaal SHM, Vliet Vlieland TPM, Gademan MGJ Longitudinal Leiden Orthopaedics Outcomes of Osteoarthritis Study (LOAS) Group. Acute pain after total hip and knee arthroplasty does not affect chronic pain during the first postoperative year: observational cohort study of 389 patients. Rheumatol Int. 2022;42:689–698. doi: 10.1007/s00296-022-05094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kugelman DN, Mahure SA, Feng JE, Rozell JC, Schwarzkopf R, Long WJ. Total knee arthroplasty is associated with greater immediate post-surgical pain and opioid use than total hip arthroplasty. Arch Orthop Trauma Surg. 2022;142:3575–3580. doi: 10.1007/s00402-021-03951-8. [DOI] [PubMed] [Google Scholar]
- 35.Simpson JC, Bao X, Agarwala A. Pain management in enhanced recovery after surgery (ERAS) protocols. Clin Colon Rectal Surg. 2019;32:121–128. doi: 10.1055/s-0038-1676477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klingberg G, Ridell K, Brogårdh-Roth S, Vall M, Berlin H. Local analgesia in paediatric dentistry: a systematic review of techniques and pharmacologic agents. Eur Arch Paediatr Dent. 2017;18:323–329. doi: 10.1007/s40368-017-0302-z. [DOI] [PMC free article] [PubMed] [Google Scholar]