Abstract
Objective
To analyze the relationship between perceived discrimination over the life course, social status, and limited health literacy (HL).
Methods
5040 adults who participated in the 2023 Survey of Racism and Public Health. We applied stratified multilevel models adjusted for sociodemographic characteristics.
Results
The average age was 47 years, 48% identified as White, 20% as Latinx, and 17% as Black. In the overall sample, we observed associations of perceived discrimination (b = 0.05, 95% CI: 0.01, 0.09), subjective social status (b = −0.16, 95% CI: −0.23, −0.10), and their interaction (b = 0.02, 95% CI: 0.01, 0.03). More perceived discrimination was associated with lower HL in the White and Multiracial participants. Higher subjective social status was associated with higher HL in the White and Latinx participants. There was a statistically significant interaction between perceived discrimination and subjective social status on HL among the White, Latinx, and Multiracial participants.
Conclusion
This analysis has implications for public health practice, indicating that multi-level interventions are needed to address limited HL.
Innovation
Our findings provide novel insights for identifying key SDOH indicators to assess in clinical settings to provide health literate care.
Keywords: Racism, Social epidemiology, Social status, Low health literacy, Marginalized populations, Race
Highlights
-
•
There is limited data on how social determinants of health are related to HL.
-
•
Perceived discrimination and subjective social status (SSS) are associated with HL.
-
•
The two social determinants of health interacted in their impact on HL.
-
•
Understanding the predictors of HL is key to developing clinical screening tools.
1. Introduction
Improving health literacy is essential across all medical specialties [1]. Patients with limited health literacy often struggle with effective health self-management, such as medication non-adherence and drug label misinterpretation [[2], [3], [4]]. Limited health literacy is associated with worse glycemic control, cardiovascular and chronic diseases, and higher all-cause mortality rates [[5], [6], [7]]. These challenges have significant implications for healthcare costs, as patients with low health literacy are more likely to visit the emergency department and require hospitalization [2,4,8]. As a result, there has been growing interest in understanding the root causes of health literacy, such as social determinants of health, which may inform health literacy skills [[9], [10], [11]].
Perceived racial discrimination and social status have long been implicated as SDOH [[12], [13], [14], [15], [16], [17]]. Perceived discrimination is a subjective measure of how often an individual experiences unfair treatment due to race, ethnicity, or color [18]. Studies have linked perceived discrimination to elevated blood pressure, low infant birthweight, and autoimmune disease severity [[12], [13], [14]]. Social status, another subjective measure, assesses an individual's perceived social standing relative to others [19]. Higher perceived social status is associated with better mental and physical health and predicts health outcomes more accurately than traditional socioeconomic indicators such as income and educational attainment [[15], [16], [17]]. Despite their potential significance, perceived discrimination and social status remain relatively unexplored in the health literacy literature.
There are several mechanisms by which perceived discrimination and subjective social status may impact health literacy. Individuals who perceive discrimination or occupy a lower subjective social status may face barriers to accessing healthcare services, obtaining accurate health information, and making informed decisions about their health. People who experience discrimination or perceive themselves to have a lower social status may be more likely to engage in unhealthy behaviors, such as smoking, excessive alcohol consumption, and lack of physical activity [20,21]. Additionally, they may have limited access to health information and resources, leading to lower health literacy levels. Experiences of discrimination and lower social status can impair cognitive processes, attention, and memory, and in turn, negatively affect comprehension of health information. Lastly, perceived discrimination and lower subjective social status can create power imbalances and communication barriers in healthcare settings. Patients who feel discriminated against or perceive a lower social status may be less likely to seek care, and, in turn, less likely to obtain health-promoting information.
Therefore, we analyzed the relationship between perceived discrimination over the life course, subjective social status, and limited health literacy among adults in the 2023 Survey of Racism and Public Health. Specifically, we used survey data from over 5000 study participants to investigate the following research questions:
-
(1)
Is perceived discrimination associated with health literacy?
-
(2)
Is subjective social status associated with health literacy?
-
(3)
Does the perceived discrimination association with health literacy vary across levels of subjective social status?
-
(4)
Do these relationships vary across racial/ethnic groups?
We hypothesize that more experiences of discrimination across the life course is associated with limited health literacy. We hypothesize that this association will be more pronounced among those who perceive themselves as having low social status and those belonging to racial/ethnic minoritized groups.
2. Methods
2.1. Participant recruitment and data collection
We used data from the Survey of Racism and Public Health. This web-based cross-sectional survey included sociodemographic questions and asked participants about their experiences with discrimination, social status, financial and food insecurity, voting, policing, and health. Study participants were sourced through Qualtrics Research Services, which collected survey data based on inclusion/exclusion criteria, sample size, and target demographics. To be eligible, participants had to be at least 18 years old, speak and read English, and reside in the following states/territories: Connecticut, Delaware, District of Columbia, Maine, Maryland, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Puerto Rico, Rhode Island, Vermont, and Virginia. The target age groups were 30% aged 18–34, 32% aged 35–54, and 38% aged 55 or older. The target racial/ethnic categories included an oversampling of minorities relative to their percentage in the US population: 50% White, 20% Black, 20% Hispanic, and 10% Other. Participants received compensation (e.g., gift cards) through Qualtrics's third-party vendors. Additional details about the study protocol can be found elsewhere [22,23]. Informed consent was obtained prior to survey participation, and the study protocol was approved by the New York University Institutional Review Board (IRB-FY2023-7408).
2.2. Analytic sample
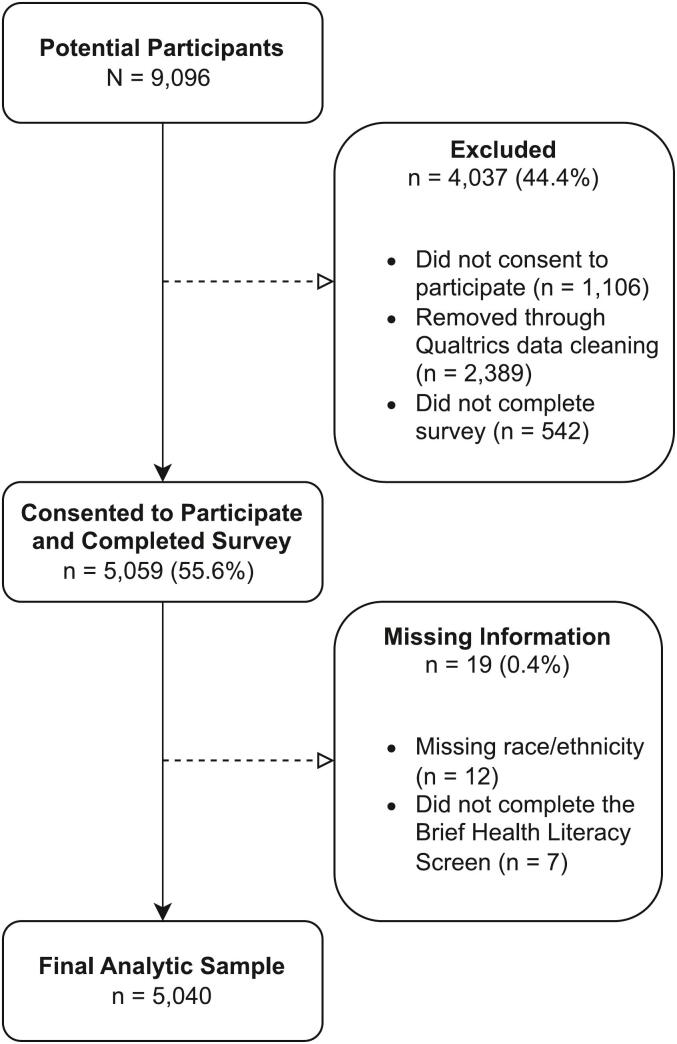
Participants were recruited from March 10 to April 12, 2023 (Fig. 1). Out of 9096 potential participants, 44.4% (n = 4037) did not consent (n = 1106), were removed through Qualtrics data cleaning services (n = 2389) or did not complete the survey (n = 542). Qualtrics removed responses for the following reasons: non-sensical answers, duplicates, responses to questions not making sense (e.g., height being too short or too tall), bots, contradictory responses, suspicious weight, suspicious race and origin, invalid IP, and gibberish. The remaining participants totaled over 5000 (n = 5059) who were eligible, agreed to participate, and completed the survey. Of these, 12 (0.2%) participants did not provide information on their race/ethnicity, and 7 (0.1%) participants did not complete the BHLS, resulting in a final analytic sample of 5040 study participants.
Fig. 1.
Recruitment of Survey of Racism and Public Health study participants, March 10 to April 12, 2023.
2.3. Dependent variable
2.3.1. Health literacy
We evaluated health literacy using the Brief Health Literacy Screen (BHLS), a validated subjective measure comprised of three self-reported Single Item Literacy Screeners [[24], [25], [26]]. These items gauge an individual's difficulty reading hospital materials, difficulty learning about their medical condition, and confidence in filling out medical forms. Each item was rated on a 5-point Likert scale and then summed to create a BHLS index (Cronbach's = 0.69). Lower scores indicate higher health literacy (range = 3–15).
2.4. Independent variables
2.4.1. Discrimination across the life course
We assessed perceived discrimination with an adapted version of the Major Experiences of Discrimination Scale [18]. Four items measured participants' experiences with discrimination throughout their lives. Participants indicated how often they were mistreated because of their race, color, or ethnicity during different life stages: childhood, teenage years, adulthood, and the past year. Response options ranged from never (1) to always (5) on a 5-point scale and were summed to create a composite perceived life course discrimination index (Cronbach's = 0.92). Higher values reflected more frequent experiences with discrimination across the life course (range = 4–20).
2.4.2. Social status
We used the MacArthur Scale of Subjective Social Status – Adult Version (MacArthur SSS Scale) to measure subjective social status [19]. Other researchers have employed this scale across diverse racial and ethnic groups [[27], [28], [29], [30]]. The MacArthur SSS Scale asks participants to rank themselves on a ladder compared to others in their community. Specifically, participants in the survey were asked: “Think of this ladder as representing where people stand in our society. At the top of the ladder are the people who are the best off, those who have the most money, most education, and best jobs. At the bottom are the people who are the worst off, those who have the least money, least education, and the worst jobs or no job. Where would you place yourself on this ladder? Please select the number that best represents where you would be on this ladder.” Response options range from 1 (lowest) to 10 (highest). We treated this variable as continuous in the analysis.
2.4.3. Sociodemographic factors
The survey also collected information on the participants' demographics. We recoded the categorical variables for this analysis. Demographic covariates include age (measured continuously in years), race/ethnicity, gender identity (woman, man), educational attainment (high school, some college, college degree), marital status (married/living with partner vs. other), employment status (full/part-time vs. other), number of dependents (0, 1, 2+), and zip code. Race/ethnicity was recategorized as White, Hispanic/Latinx (Latinx), Black/African American (Black), Asian American/Pacific Islander (AA/PI), Multiracial, and American Indian/Native American/Arab/Middle Eastern/North African (AI/AN/A/ME/NA). Latinx was inclusive of race as all other groups are non-Hispanic (e.g., non-Hispanic White, non-Hispanic Black). We classified “other” gender identity (n = 29) as missing due to the small sample size. The “other” marital status category includes those who were divorced, separated, widowed, or never married. The “other” employment status category consists of those on temporary leave, unemployed, not working by choice (e.g., disability, student), independent contractors, or business owners. We used rural-urban commuting area codes from the US Department of Agriculture to classify zip codes as rural or urban [31].
2.5. Analytic strategy
We calculated frequencies or means to describe the characteristics of the study sample. Next, we performed bivariate analyses using the Kruskal-Wallis rank sum test and Pearson's Chi-squared test to examine descriptive factors by race/ethnicity. We applied multilevel linear regression models to explore the relationship between perceived discrimination across the life course, social status, and limited health literacy. We nested participants by zip code to account for the correlation of health literacy outcomes among respondents residing in the same area. Covariates were determined a priori based on previous health literacy studies [[32], [33], [34], [35]]. We fit adjusted models for the overall sample and each racial/ethnic group and tabulate the estimates () with their corresponding 95% confidence intervals. In the supplementary materials, we provided additional bivariate analyses using a dichotomous health literacy measure. Consistent with other studies [3,26], we classified individuals with total BHLS scores of 6 or greater as having limited health literacy and those with scores <6 as having adequate health literacy. All statistical analyses were conducted using R [36].
3. Results
3.1. Study population characteristics
Table 1 presents the characteristics of the overall study population and stratified by racial/ethnic group. The average age was 47.0 years (SD: 17.5), with an equal gender identity distribution (man: 50.3%; woman: 49.7%). Most of the respondents identified as White (48.0%) or Latinx (20.4%), had obtained at least some college education (74.5%), were married or living with a partner (53.0%), were engaged in full- or part-time employment (57.0%), had no dependents (55.8%), and resided in an urban area (91.8%). The average health literacy score was 5.1 (SD = 2.4), and 35.4% were classified as having limited health literacy according to the BHLS (Supplemental Table 1). The mean perceived discrimination score was 8.0 (SD = 3.8), implying that, on average, individuals in this sample reported low levels of discrimination over the life course. The average subjective social status score was 5.9 (SD = 2.0), demonstrating that, on average, study participants perceived themselves a little above average within society.
Table 1.
Study participant characteristics, Survey of Racism and Public Health, 2023.
| Characteristic | N | Overall N = 5040 |
White N = 2420 |
Latinx N = 1027 |
Black N = 879 |
AA/PI N = 419 |
Multiracial N = 158 |
AI/AN/A/ME/NA N = 137 |
p-value1 |
|---|---|---|---|---|---|---|---|---|---|
| Age | 5038 | <0.001 | |||||||
| Mean (SD) | 47.0 (17.5) | 56.2 (15.9) | 34.8 (12.7) | 40.8 (15.3) | 41.9 (14.3) | 38.2 (14.6) | 41.9 (14.6) | ||
| Range | 18.0, 90.0 | 18.0, 90.0 | 18.0, 88.0 | 18.0, 83.0 | 18.0, 86.0 | 18.0, 79.0 | 18.0, 75.0 | ||
| Gender identity, No. (%) | 5010 | <0.001 | |||||||
| Man | 2519 (50.3%) | 1533 (63.5%) | 358 (35.3%) | 346 (39.5%) | 165 (39.7%) | 56 (35.9%) | 61 (44.9%) | ||
| Woman | 2491 (49.7%) | 881 (36.5%) | 655 (64.7%) | 529 (60.5%) | 251 (60.3%) | 100 (64.1%) | 75 (55.1%) | ||
| Educational attainment, No. (%) | 5016 | <0.001 | |||||||
| High School | 1280 (25.5%) | 497 (20.6%) | 329 (32.2%) | 320 (36.5%) | 52 (12.4%) | 39 (24.7%) | 43 (31.9%) | ||
| Some College | 1639 (32.7%) | 750 (31.1%) | 353 (34.6%) | 329 (37.6%) | 81 (19.4%) | 69 (43.7%) | 57 (42.2%) | ||
| College Degree | 2097 (41.8%) | 1161 (48.2%) | 339 (33.2%) | 227 (25.9%) | 285 (68.2%) | 50 (31.6%) | 35 (25.9%) | ||
| Marital status, No. (%) | 5038 | <0.001 | |||||||
| Other | 2368 (47.0%) | 909 (37.6%) | 534 (52.0%) | 589 (67.1%) | 186 (44.4%) | 80 (50.6%) | 70 (51.1%) | ||
| Married/Living with partner | 2670 (53.0%) | 1510 (62.4%) | 493 (48.0%) | 289 (32.9%) | 233 (55.6%) | 78 (49.4%) | 67 (48.9%) | ||
| Employment status, No. (%) | 5005 | <0.001 | |||||||
| Other | 2154 (43.0%) | 1179 (49.3%) | 357 (34.8%) | 350 (39.9%) | 137 (32.8%) | 75 (47.5%) | 56 (41.2%) | ||
| Full/part-time | 2851 (57.0%) | 1211 (50.7%) | 669 (65.2%) | 527 (60.1%) | 281 (67.2%) | 83 (52.5%) | 80 (58.8%) | ||
| # Children, No. (%) | 5039 | <0.001 | |||||||
| 0 | 2812 (55.8%) | 1410 (58.3%) | 515 (50.1%) | 491 (55.9%) | 240 (57.3%) | 91 (57.6%) | 65 (47.4%) | ||
| 1 | 998 (19.8%) | 473 (19.5%) | 190 (18.5%) | 198 (22.6%) | 81 (19.3%) | 28 (17.7%) | 28 (20.4%) | ||
| 2+ | 1229 (24.4%) | 537 (22.2%) | 322 (31.4%) | 189 (21.5%) | 98 (23.4%) | 39 (24.7%) | 44 (32.1%) | ||
| Residence, No. (%) | 5040 | <0.001 | |||||||
| Rural | 414 (8.2%) | 315 (13.0%) | 33 (3.2%) | 26 (3.0%) | 7 (1.7%) | 17 (10.8%) | 16 (11.7%) | ||
| Urban | 4626 (91.8%) | 2105 (87.0%) | 994 (96.8%) | 853 (97.0%) | 412 (98.3%) | 141 (89.2%) | 121 (88.3%) | ||
| Health literacy | 5040 | <0.001 | |||||||
| Mean (SD) | 5.1 (2.4) | 4.8 (2.3) | 5.7 (2.6) | 5.3 (2.6) | 5.2 (2.3) | 5.1 (2.3) | 5.9 (2.5) | ||
| Range | 3.0, 15.0 | 3.0, 15.0 | 3.0, 14.0 | 3.0, 14.0 | 3.0, 13.0 | 3.0, 11.0 | 3.0, 15.0 | ||
| Perceived discrimination | 5038 | <0.001 | |||||||
| Mean (SD) | 8.0 (3.8) | 6.3 (3.2) | 9.0 (3.8) | 9.8 (3.8) | 9.4 (3.3) | 10.4 (3.8) | 9.5 (3.9) | ||
| Range | 4.0, 20.0 | 4.0, 20.0 | 4.0, 20.0 | 4.0, 20.0 | 4.0, 20.0 | 4.0, 20.0 | 4.0, 20.0 | ||
| Subjective social status | 5040 | <0.001 | |||||||
| Mean (SD) | 5.9 (2.0) | 6.1 (1.9) | 5.7 (2.1) | 5.4 (2.1) | 6.2 (1.8) | 5.4 (2.0) | 5.5 (2.2) | ||
| Range | 1.0, 10.0 | 1.0, 10.0 | 1.0, 10.0 | 1.0, 10.0 | 1.0, 10.0 | 1.0, 10.0 | 1.0, 10.0 |
Latinx = Hispanic/Latinx, Black = Black/African American, AA/PI = Asian American/Pacific Islander, AI/AN/A/ME/NA = American Indian/Native American/Arab/Middle Eastern/North African, SD = Standard Deviation.
Kruskal-Wallis rank sum test; Pearson's Chi-squared test.
We found statistically significant differences in sociodemographic characteristics across racial/ethnic groups (all p < 0.001). White respondents were the oldest (mean age = 56.2, SD: 15.9) and had the lowest proportion of woman participants (36.5%) and participants who worked full- or part-time (50.7%). Additionally, White respondents had the highest proportion of participants who were married or living with a partner (62.4%) and had no dependents (58.3%). In contrast, Black participants had the lowest proportion of participants who were married or living with a partner (32.9%). Latinx participants were the youngest (mean age = 34.8, SD: 12.7) and had the highest proportions of woman participants (64.7%). AA/PI had the highest proportions of those living in an urban area (98.3%), those with at least some college education (87.6%), and those who worked full- or part-time (67.2%).
We observed statistically significant differences in measures of health literacy, perceived discrimination, and social status across racial/ethnic groups (all p < 0.001, Table 1). When comparing racial/ethnic groups, the mean health literacy scores ranged from 4.8 (White, SD: 2.3) to 5.9 (AI/AN/A/ME/NA, SD: 2.5). White participants had the lowest mean discrimination score (mean = 6.3, SD: 3.2), while Multiracial participants had the highest (mean = 10.4, SD: 3.8). Black (mean = 5.4, SD: 2.1) and Multiracial (mean = 5.4, SD: 2.0) participants had the lowest subjective social status score, whereas AA/PI participants had the highest (mean = 6.2, SD: 1.8).
3.2. Associations with health literacy among the study sample
Table 2 displays the adjusted associations between health literacy, perceived discrimination, and social status in the overall sample. The statistically significant association of perceived discrimination (b = 0.049, 95% CI: 0.005, 0.094) suggests that more frequent perceived discrimination experiences over the life course are associated with lower health literacy. However, this association depends on the level of subjective social status. The interaction term between perceived discrimination and subjective social status (b = 0.021, 95% CI: 0.014, 0.089) was found to be statistically significant, in addition to the independent association of subjective social status (b = −0.163, 95% CI: −0.230, −0.096).
Table 2.
Adjusted associations between health literacy, perceived discrimination, and social status among the overall sample, Survey of Racism and Public Health, 2023.
| Overall (n = 4944) |
||
|---|---|---|
| b | 95% CI | |
| Perceived discrimination | 0.049 | 0.005, 0.094 |
| Subjective social status | −0.163 | −0.230, −0.096 |
| Perceived discrimination*Subjective social status | 0.021 | 0.014, 0.028 |
CI = Confidence interval. Model adjusted for age, race/ethnicity, gender identity, educational attainment, marital status, employment status, number of children, and residence.
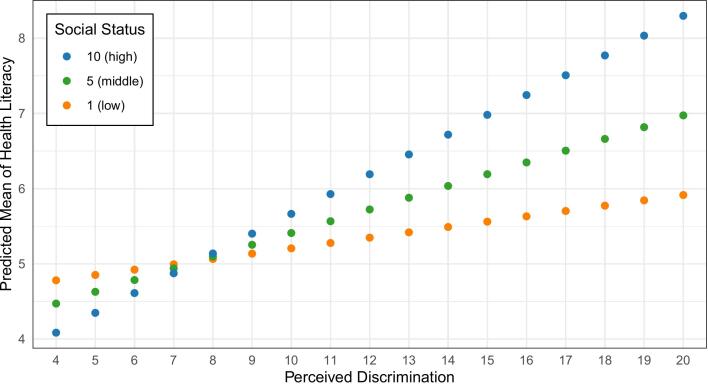
To illustrate this combined association, we plotted the predicted marginal means for subjective social status ratings of low (1), middle (5), and high (10), controlling for race/ethnicity, gender identity, education, marital and employment status, dependents, and location (Fig. 2). Among individuals who reported never experiencing discrimination throughout their lives (perceived discrimination score = 4), those who perceived themselves as high (social status = 10; predicted mean health literacy score = 4.09) on the social status ladder had better health literacy than those who perceived themselves as low (social status = 1; predicted mean health literacy score = 4.78) or middle (social status = 5; predicted mean health literacy score = 4.47) on the ladder. However, this relationship reversed among individuals who reported frequent discrimination (perceived discrimination score = 20). For instance, those who perceived themselves as low (social status = 1; predicted mean health literacy score = 5.92) on the social status ladder had better health literacy than those who perceived themselves as high (social status = 10; predicted mean health literacy score = 8.30) or middle (social status = 5; predicted mean health literacy score = 6.97) on the ladder.
Fig. 2.
Predicted marginal means from the multilevel model of the overall sample, adjusted for race/ethnicity, gender identity, education, marital and employment status, dependents, and location, Survey of Racism and Public Health, 2023.
3.3. Associations with health literacy by race/ethnicity
Table 3 compares the associations between health literacy, perceived discrimination, and social status stratified by racial/ethnic groups. The table reveals that many statistically significant associations observed in the overall sample persisted among White participants, with some strengthened associations. These associations include perceived discrimination (= 0.082, 95% CI: 0.010, 0.155; = 0.049, 95% CI: 0.005, 0.094), social status (= −0.188, 95% CI: −0.275, −0.102; = −0.163, 95% CI: −0.230, −0.096), and the interaction between perceived discrimination and subjective social status (= 0.026, 95% CI: 0.016, 0.037; = 0.021, 95% CI: 0.014, 0.028).
Table 3.
Adjusted associations between health literacy, perceived discrimination, and social status across racial/ethnic groups, Survey of Racism and Public Health, 2023.
| White |
Latinx |
Black |
AA/PI |
Multiracial |
AI/AN/A/ME/NA |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 2371 |
n = 1006 |
n = 867 |
n = 413 |
n = 155 |
n = 132 |
|||||||
| b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | |
| Perceived discrimination | 0.082 | 0.010, 0.155 | 0.008 | −0.096, 0.111 | 0.083 | −0.020, 0.186 | 0.081 | −0.133, 0.295 | 0.249 | 0.026, 0.471 | 0.030 | −0.248, 0.308 |
| Subjective social status | −0.188 | −0.275, −0.102 | −0.181 | −0.348, −0.014 | −0.024 | −0.214, 0.165 | −0.107 | −0.434, 0.220 | 0.409 | −0.067, 0.885 | −0.305 | −0.804, 0.194 |
| Perceived discrimination*Subjective social status | 0.026 | 0.016, 0.037 | 0.026 | 0.010, 0.042 | 0.008 | −0.010, 0.025 | 0.003 | −0.029, 0.035 | −0.042 | −0.082, −0.002 | 0.021 | −0.023, 0.065 |
Latinx = Hispanic/Latinx, Black = Black/African American, AA/PI = Asian American/Pacific Islander, AI/AN/A/ME/NA = American Indian/Native American/Arab/Middle Eastern/North African, CI = Confidence Interval.
Model adjusted for age, gender identity, educational attainment, marital status, employment status, number of children, and residence.
Bold font indicates 95% confidence interval does not include 0.
Similar to the overall sample results, the combined association of perceived discrimination and subjective social status on health literacy among the White sample population can be interpreted by examining the predicted marginal means (not shown). Among White individuals who reported never experiencing discrimination across their life course (perceived discrimination score = 4), those who perceived themselves as high (social status score = 10; predicted mean health literacy score = 3.92) on the social status ladder had better health literacy compared to those who perceived themselves as low (social status score = 1; predicted mean health literacy score = 4.66) or middle (social status score = 5; predicted mean health literacy score = 4.33) on the ladder. However, this relationship reversed among individuals who reported frequent discrimination (perceived discrimination score = 20). Particularly, those who perceived themselves as low (social status score = 1; predicted mean health literacy score = 6.41) on the social status ladder had better health literacy than those who perceived themselves as high (social status score = 10; predicted mean health literacy score = 9.48) or middle (social status score = 5; predicted mean health literacy score = 7.77).
Among Latinx participants, we observed statistically significant associations of subjective social status (b = −0.181, 95% CI: −0.348, −0.014) and the interaction between perceived discrimination and subjective social status (b = 0.026, 95% CI: 0.010, 0.042). Among Multiracial participants, we found statistically significant associations of perceived discrimination (b = 0.249, 95% CI: 0.026, 0.471) and the interaction between perceived discrimination and subjective social status (b = −0.042, 95% CI: −0.082, −0.002). We did not find statistically significant associations of perceived discrimination, subjective social status, and their interaction among participants identified as Black, Asian American/Pacific Islander, or American Indian/Native American/Arab/Middle Eastern/North African.
4. Discussion and conclusion
4.1. Discussion
We investigated the relationship between perceived discrimination across the life course, subjective social status, and health literacy. We observed that among the overall, White, and Multiracial participants, more perceived discrimination was associated with lower health literacy. Among the overall, White, and Latinx participants, we found that higher subjective social status was associated with higher health literacy. There was a statistically significant interaction between perceived discrimination and subjective social status on health literacy among the overall, White, Latinx, and Multiracial participants. These findings underpin the importance of examining social determinants of health literacy.
The negative relationship between perceived discrimination over the life course in the overall sample may be due to the weathering hypothesis [37,38]. This theory suggests that cumulative exposure to socioeconomic disadvantage adversely affects health outcomes [37,38]. Given the link between health literacy and health [[39], [40], [41], [42], [43], [44], [45], [46]], it is plausible that cumulative exposure to discrimination also negatively impacts health literacy. Life course discrimination may be an additional barrier to obtaining higher health literacy among populations with low income and education levels [[47], [48], [49], [50], [51]]. Our findings further suggest that subjective social status may modify the relationship between perceived discrimination and health literacy. Study participants with the most experiences of perceived discrimination and the highest self-ranking of social status tended to have limited health literacy. This may indicate that even when individuals believe they have reached the highest social level in society, their health literacy may still be plagued by internalized racism.
We observed statistically significant associations of perceived discrimination, subjective social status, and their interaction with health literacy among those racialized as White. We did not find statistically significant associations among populations racialized as Black, Asian American/Pacific Islander, and American Indian/Native American/Arab/Middle Eastern/North African. These null findings could be attributed to little variation in the frequency of interpersonal racism experienced among racially minoritized populations [52]. Despite differences in income and education levels, it is likely that no within-group variation exists because we assessed race/ethnicity using a social construct [[53], [54], [55], [56], [57], [58], [59], [60], [61]]. Future investigations should explore within-group differences based on an objective skin color measurement [[62], [63], [64], [65], [66], [67], [68], [69]].
Limited data exist on the intersection between perceived discrimination, social status, and health literacy. A study by Goodman et al. explored the association between self-reported segregation across the life course and health literacy among Suffolk County, NY health center patients [32]. The authors found that patients who reported attending predominantly White junior high schools were more likely to have adequate health literacy than those who reported attending non-predominantly White junior high schools. Additionally, this study revealed a similar association between self-reports of living in predominantly White neighborhoods and adequate health literacy. Zou et al. conducted a mediation analysis on health literacy, subjective social status, and depressive symptoms in heart failure patients [70]. In their subjective social status and health literacy model, Zou et al. found that higher perceived social status correlated with better health literacy.
Improving organizational health literacy is a viable solution for mitigating the impacts of cumulative discrimination exposure [[71], [72], [73]]. Organizational health literacy is “the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others [73].” Researchers have argued that physicians and trainees should be held more accountable for progress in increasing health literacy among minoritized patients [[71], [72], [73]]. Even though physicians and trainees take required patient communication courses, Coleman et al. contend that physicians and trainees continue to overcomplicate patient-provider communication [71]. The findings from the present study underscore the need for physicians and trainees to consider patient's past discrimination experiences. Understanding these experiences can potentially improve how providers interact with their patients, especially when socially disadvantaged patients interact with providers from historically advantaged racial backgrounds [[74], [75], [76], [77], [78]].
Several limitations should be considered when interpreting our study's findings. First, the sample was limited to online computer and mobile device users, excluding individuals without computer or mobile access. Social factors may disproportionately impact the health literacy of populations without computer or mobile access. Second, this study's findings may not be generalizable because the study recruitment strategy required participants to reside in a geographic region comprised mainly of Northeastern states/territories and be English-speaking. Participants who speak English as a second language may not fully understand English [79], which, in turn, may result in low health literacy scores. Our inferences may have been susceptible to selection bias because we oversampled Latinx participants and recruited participants from Puerto Rico but required the survey to be completed in English [80]. Future studies are needed to investigate the reliability of the BHLS in populations of varying English proficiency. Future iterations of the Survey of Racism and Public Health should be administered in multiple languages. Our results may also not be generalizable since 42% of the study sample were college graduates, a higher proportion than the US population (34%) [81]. Additionally, sample participants generally reported low levels of discrimination over the life course. As with all self-reported survey measures, there is the potential for recall and social desirability bias in participant responses [82]. We were able to discern a statistically significant association between life course discrimination and health literacy, but it will be important to examine this relationship further in a sample with greater variability in perceived discrimination.
Third, we stratified the analyses based on a social construct of race [[53], [54], [55], [56], [57], [58], [59], [60], [61]]. Fourth, we excluded participants who did not report demographic characteristics, such as race, that might marginalize them. We also classified 29 individuals in the other gender identity category as missing. Future generalizable analyses should explore associations of perceived discrimination, social status, and health literacy among gender-minoritized individuals. This would require the oversampling of gender-minoritized individuals. Fifth, assessing discrimination across the life course introduces potential recall bias and measurement error. Sixth, the BHLS does not assess other aspects of health literacy, such as visual literacy, numeracy, and oral communication [25].
Additionally, the alpha reliability coefficient for the BHLS was 0.69, slightly below the adequate level, possibly due to the difference between our sample and the BHLS validation sample [24]. Future research is needed to confirm whether our findings hold when using functional health literacy measures, such as the Test of Functional Health Literacy in Adults [83] or the Newest Vital Sign [84]. Seventh, our cross-sectional analysis prevented us from inferring causal relationships between perceived discrimination, social status, and health literacy. Lastly, we did not have access to medical records, which would have allowed us to control for factors related to health literacy, such as emergency department visits, hospitalizations, and health insurance status.
Despite its limitations, our study exhibited notable strengths and innovations. We analyzed a large sample size of over 5000 participants, which may have increased the statistical power to detect interaction effects within the overall sample and across different racial/ethnic groups. Additionally, the relatively large sample sizes within each racial/ethnic group enabled us to perform stratified analyses in a diverse study population. Our study also used validated measures of health literacy, subjective social status, and perceived discrimination. Notably, the life course measure of perceived discrimination demonstrated high reliability [85].
4.2. Innovation
This study is innovative in its focus on associations between health literacy and two SDOH (i.e., perceived discrimination over the life course and subjective social status). While conceptual frameworks have highlighted the importance of examining relationships between SDOH and health literacy [10], little empirical research has investigated this issue. The inclusion of a life-course measure of discrimination also adds to the innovation [[47], [48], [49], [50], [51],86]. The present study is also innovative in the health literacy literature with its grounding in psychosocial epidemiological theory [87,88], which informed the investigation of the interplay between two psychosocial mechanisms concerning health literacy. While much is known about how individual-level demographic factors are associated with health literacy [89,90], demographic data available in the electronic health record is often missing or unreliable [91]. There is a need to develop screening instruments for SDOH that are reliable predictors of health literacy and can be quickly collected in clinical settings. This work provides a key first step in determining how to measure SDOH.
Additionally, the present study's findings have potential implications for healthcare education and patient-provider communication. By demonstrating an association between lower health literacy and perceived discrimination in our sample, we highlight a critical area for improvement in healthcare delivery. These results suggest that healthcare providers may need enhanced education and re-education on implicit bias and its potential impact on patient understanding. If patients with lower health literacy are experiencing higher levels of perceived discrimination, it raises questions about how effectively healthcare professionals are conveying information to these patients. This insight could lead to innovations in medical education curricula and the development of more effective, culturally sensitive communication strategies in clinical settings. By addressing these issues, we may improve patient understanding, reduce perceived discrimination, and ultimately enhance health outcomes for minoritized populations.
4.3. Conclusion
After adjusting for potential confounders, we found that the impact of perceived discrimination on health literacy depends on subjective social status. Further research is necessary to confirm these associations, particularly studies that assess various household factors. In addition, further analyses of the relationships between perceived discrimination over the life course, subjective social status, and health literacy are needed among generalizable populations. Establishing evidence highlighting the social influences on health literacy can provide meaningful insights for interventions focused on patient engagement and communication.
CRediT authorship contribution statement
Jemar R. Bather: Writing – original draft, Visualization, Software, Methodology, Investigation, Formal analysis. Adolfo G. Cuevas: Writing – review & editing, Resources, Conceptualization. Adrian Harris: Writing – review & editing, Software, Investigation, Data curation. Kimberly A. Kaphingst: Writing – review & editing, Resources, Conceptualization. Melody S. Goodman: Writing – review & editing, Validation, Resources, Project administration, Methodology, Investigation, Funding acquisition, Data curation, Conceptualization.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
This work was supported by the Center for Anti-racism, Social Justice & Public Health at the NYU School of Global Public Health. We thank Arushi Chadha, Ridwan Nafiu, and Feng Liu for their valuable assistance with the secondary data analysis preparation. We greatly appreciate the editorial team and the anonymous reviewers for taking the time to review our manuscript and providing constructive comments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2024.100334.
Appendix A. Supplementary data
Supplementary material: Sample characteristics by health literacy status
Data availability
The data that support the findings of this study are available from the Center for Anti-racism, Social Justice & Public Health (gph.casjph@nyu.edu), upon reasonable request.
References
- 1.Institute of Medicine . The National Academies Press; 2015. Vital Signs: Core Metrics for Health and Health Care Progress, Washington, DC. [PubMed] [Google Scholar]
- 2.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann. Intern. Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [PMID:21768583] [DOI] [PubMed] [Google Scholar]
- 3.Fan J.H., Lyons S.A., Goodman M.S., Blanchard M.S., Kaphingst K.A. Relationship between health literacy and unintentional and intentional medication nonadherence in medically underserved patients with type 2 diabetes. Diabetes Educ. 2016;42(2):199–208. doi: 10.1177/0145721715624969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hibbard J.H., Peters E., Dixon A., Tusler M. Consumer competencies and the use of comparative quality information: it Isn’t just about literacy. Med. Care Res. Rev. 2007;64(4):379–394. doi: 10.1177/1077558707301630. [PMID:17684108] [DOI] [PubMed] [Google Scholar]
- 5.Schillinger D., Grumbach K., Piette J., Wang F., Osmond D., Daher C., et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [PMID:12132978] [DOI] [PubMed] [Google Scholar]
- 6.Paasche-Orlow M.K., Parker R.M., Gazmararian J.A., Nielsen-Bohlman L.T., Rudd R.R. The prevalence of limited health literacy. J. Gen. Intern. Med. 2005;20(2):175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [PMID:15836552] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Viera A., Crotty K., et al. Health literacy interventions and outcomes: an updated systematic review. Evid. ReportTechnol. Assess. 2011;199:1–941. [PMID:23126607] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffey R.T., Kennedy S.K., D’Agostino McGowan L., Goodman M., Kaphingst K.A. Is low health literacy associated with increased emergency department utilization and recidivism? Acad. Emerg. Med. 2014;21(10):1109–1115. doi: 10.1111/acem.12476. [PMID:25308133] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2030. 2024. https://health.gov/healthypeople/objectives-and-data/browse-objectives Available from. accessed Jun 8, 2023.
- 10.Schillinger D. Social determinants, health literacy, and disparities: intersections and controversies. Health Lit. Res. Pract. 2021;5(3):e234–e243. doi: 10.3928/24748307-20210712-01. [PMID:34379549] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schillinger D. The intersections between social determinants of health, health literacy, and health disparities. Stud. Health Technol. Inform. 2020;25(269):22–41. doi: 10.3233/SHTI200020. [PMID:32593981] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krieger N., Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am. J. Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [PMID:8876504] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mustillo S., Krieger N., Gunderson E.P., Sidney S., McCreath H., Kiefe C.I. Self-reported experiences of racial discrimination and black-White differences in preterm and low-birthweight deliveries: the CARDIA study. Am. J. Public Health. 2004;94(12):2125–2131. doi: 10.2105/ajph.94.12.2125. [PMID:15569964] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chae D.H., Martz C.D., Fuller-Rowell T.E., Spears E.C., Smith T.T.G., Hunter E.A., et al. Racial discrimination, disease activity, and organ damage: the black Women’s experiences living with lupus (BeWELL) study. Am. J. Epidemiol. 2019;188(8):1434–1443. doi: 10.1093/aje/kwz105. [PMID:31062841] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh-Manoux A., Marmot M.G., Adler N.E. Does subjective social status predict health and change in health status better than objective status? Psychosom. Med. 2005;67(6):855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [PMID:16314589] [DOI] [PubMed] [Google Scholar]
- 16.Tan J.J.X., Kraus M.W., Carpenter N.C., Adler N.E. The association between objective and subjective socioeconomic status and subjective well-being: a Meta-analytic review. Psychol. Bull. 2020;146(11):970–1020. doi: 10.1037/bul0000258. [PMID:33090862] [DOI] [PubMed] [Google Scholar]
- 17.Garza J.R., Glenn B.A., Mistry R.S., Ponce N.A., Zimmerman F.J. Subjective social status and self-reported health among US-born and immigrant Latinos. J. Immigr. Minor. Health. 2017;19(1):108–119. doi: 10.1007/s10903-016-0346-x. [PMID:26895151] [DOI] [PubMed] [Google Scholar]
- 18.Williams D.R., Yu Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J. Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 19.Adler N.E., Epel E.S., Castellazzo G., Ickovics J.R. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy White women. Health Psychol. 2000;19(6):586–592. doi: 10.1037//0278-6133.19.6.586. [PMID:11129362] [DOI] [PubMed] [Google Scholar]
- 20.Finch K.A., Ramo D.E., Delucchi K.L., Liu H., Prochaska J.J. Subjective social status and substance use severity in a young adult sample. J. Soc. Psychol. Addict. Behav. 2013;27(3):901–908. doi: 10.1037/a0032900. [PMID:23915371] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manuck S.B., Phillips J.E., Gianaros P.J., Flory J.D., Muldoon M.F. Subjective socioeconomic status and presence of the metabolic syndrome in midlife community volunteers. Psychosom. Med. 2010;72(1):35–45. doi: 10.1097/PSY.0b013e3181c484dc. [PMID:19933505] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bather J.R., McSorley A.-M.M., Rhodes-Bratton B., Cuevas A.G., Rouhani S., Nafiu R.T., et al. Love after lockup: examining the role of marriage, social status, and financial stress among formerly incarcerated individuals. Health Justice. 2024;12(1):7. doi: 10.1186/s40352-024-00264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bather J.R., Robinson T.J., Goodman M.S. Bayesian kernel machine regression for social epidemiologic research. Epidemiology. 2024 doi: 10.1097/EDE.0000000000001777. [DOI] [PubMed] [Google Scholar]
- 24.Chew L.D., Griffin J.M., Partin M.R., Noorbaloochi S., Grill J.P., Snyder A., et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J. Gen. Intern. Med. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [PMID:18335281] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goodman M.S., Griffey R.T., Carpenter C.R., Blanchard M., Kaphingst K.A. Do subjective measures improve the ability to identify limited health literacy in a clinical setting? J am board fam med American board of. Fam. Med. 2015;28(5):584–594. doi: 10.3122/jabfm.2015.05.150037. [PMID:26355130] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpenter C.R., Kaphingst K.A., Goodman M.S., Lin M.J., Melson A.T., Griffey R.T. Feasibility and diagnostic accuracy of brief health literacy and numeracy screening instruments in an urban emergency department. Acad. Emerg. Med. 2014;21(2):137–146. doi: 10.1111/acem.12315. [PMID:24673669] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bullock H.E., Limbert W.M. Scaling the socioeconomic ladder: low-income women’s perceptions of class status and opportunity. J. Soc. Issues. 2003;59(4):693–709. doi: 10.1046/j.0022-4537.2003.00085.x. [DOI] [Google Scholar]
- 28.Franzini L., Fernandez-Esquer M.E. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Soc. Sci. Med. 2006;63(3):788–804. doi: 10.1016/j.socscimed.2006.01.009. [PMID:16580107] [DOI] [PubMed] [Google Scholar]
- 29.Ostrove J.M., Adler N.E., Kuppermann M., Washington A.E. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychol. 2000;19(6):613–618. doi: 10.1037//0278-6133.19.6.613. [PMID:11129365] [DOI] [PubMed] [Google Scholar]
- 30.Odumegwu J.N., Chavez-Yenter D., Goodman M.S., Kaphingst K.A. Associations between subjective social status and predictors of interest in genetic testing among women diagnosed with breast Cancer at a young age. Cancer Causes Control. 2024 doi: 10.1007/s10552-024-01878-0. [DOI] [PubMed] [Google Scholar]
- 31.US Department of Agriculture Rural-Urban Commuting Area Codes. 2024. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx Available from. accessed Jun 12, 2023.
- 32.Goodman M.S., Gaskin D.J., Si X., Stafford J.D., Lachance C., Kaphingst K.A. Self-reported segregation experience throughout the life course and its association with adequate health literacy. Health Place. 2012;18(5):1115–1121. doi: 10.1016/j.healthplace.2012.04.010. [PMID:22658579] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sentell T., Zhang W., Davis J., Baker K.K., Braun K.L. The influence of community and individual health literacy on self-reported health status. J. Gen. Intern. Med. 2014;29(2):298–304. doi: 10.1007/s11606-013-2638-3. [PMID:24096723] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith S.G., Curtis L.M., O’Conor R., Federman A.D., Wolf M.S. ABCs or 123s? The independent contributions of literacy and numeracy skills on health task performance among older adults. Patient Educ. Couns. 2015;98(8):991–997. doi: 10.1016/j.pec.2015.04.007. [PMID:25936579] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McNaughton C.D., Cawthon C., Kripalani S., Liu D., Storrow A.B., Roumie C.L. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J. Am. Heart Assoc. 2015;4(5) doi: 10.1161/JAHA.115.001799. [PMID:25926328] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.R Core Team . R Foundation for Statistical Computing; 2024. R: A Language and Environment for Statistical Computing, Vienna, Austria.https://www.R-project.org/ Available from: [Google Scholar]
- 37.Forde A.T., Crookes D.M., Suglia S.F., Demmer R.T. The weathering hypothesis as an explanation for racial disparities in health: a systematic review. Ann. Epidemiol. 2019;33:1–18.e3. doi: 10.1016/j.annepidem.2019.02.011. [PMID:30987864] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geronimus A.T. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn. Dis. 1992;2(3):207–221. [PMID:1467758] [PubMed] [Google Scholar]
- 39.Hickey K.T., Masterson Creber R.M., Reading M., Sciacca R.R., Riga T.C., Frulla A.P., et al. Low health literacy: implications for managing cardiac patients in practice. Nurs. Pract. 2018;43(8):49–55. doi: 10.1097/01.NPR.0000541468.54290.49. [PMID:30028773] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fan Z.-Y., Yang Y., Zhang F. Association between health literacy and mortality: a systematic review and Meta-analysis. Arch. Public Health. 2021;79(1):119. doi: 10.1186/s13690-021-00648-7. [PMID:34210353] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.King A. Poor health literacy: a “hidden” risk factor. Nat. Rev. Cardiol. 2010;7(9):473–474. doi: 10.1038/nrcardio.2010.122. [PMID:20725102] [DOI] [PubMed] [Google Scholar]
- 42.Yin H.S., Jay M., Maness L., Zabar S., Kalet A. Health literacy: an educationally sensitive patient outcome. J. Gen. Intern. Med. 2015;30(9):1363–1368. doi: 10.1007/s11606-015-3329-z. [PMID:26173523] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dewalt D.A., Berkman N.D., Sheridan S., Lohr K.N., Pignone M.P. Literacy and health outcomes: a systematic review of the literature. J. Gen. Intern. Med. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [PMID:15610334] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berkman N.D., Davis T.C., McCormack L. Health literacy: what is it? J. Health Commun. 2010;15(Suppl. 2):9–19. doi: 10.1080/10810730.2010.499985. [PMID:20845189] [DOI] [PubMed] [Google Scholar]
- 45.Paasche-Orlow M.K., Wolf M.S. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007;31(Suppl. 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [PMID:17931132] [DOI] [PubMed] [Google Scholar]
- 46.Rudd R.E. Improving Americans’ health literacy. N. Engl. J. Med. 2010;363(24):2283–2285. doi: 10.1056/NEJMp1008755. [PMID:21142532] [DOI] [PubMed] [Google Scholar]
- 47.White K., Borrell L.N. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17(2):438–448. doi: 10.1016/j.healthplace.2010.12.002. [PMID:21236721] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams D.R., Lawrence J.A., Davis B.A. Racism and health: evidence and needed research. Annu. Rev. Public Health. 2019;40(1):105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gilbert K.L., Elder K., Lyons S., Kaphingst K., Blanchard M., Goodman M. Racial composition over the life course: examining separate and unequal environments and the risk for heart disease for African American men. Ethn. Dis. 2015;25(3):295–304. doi: 10.18865/ed.25.3.295. [PMID:26673460] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gee G.C., Ford C.L. Structural racism and health inequities: old issues, new directions. Bois. Rev. Soc. Sci. Res. Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [PMID:25632292] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gee G.C., Walsemann K.M., Brondolo E. A life course perspective on how racism may be related to health inequities. Am. J. Public Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [PMID:22420802] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Willis H.A., Sosoo E.E., Bernard D.L., Neal A., Neblett E.W. The associations between internalized racism, racial identity, and psychological distress. Emerg. Adulthood. 2021;9(4):384–400. doi: 10.1177/21676968211005598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adkins-Jackson P.B., Chantarat T., Bailey Z.D., Ponce N.A. Measuring structural racism: a guide for epidemiologists and other health researchers. Am. J. Epidemiol. 2022;191(4):539–547. doi: 10.1093/aje/kwab239. [PMID:34564723] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Braveman P., Parker Dominguez T. Abandon “race.” Focus on racism. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.689462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Groos M., Wallace M., Hardeman R., Theall K. Measuring inequity: a systematic review of methods used to quantify structural racism. J. Health Dispar. Res. Pract. 2018;11(2) https://digitalscholarship.unlv.edu/jhdrp/vol11/iss2/13 Available from: [Google Scholar]
- 56.LaVeist T.A. Beyond dummy variables and sample selection: what health services researchers ought to know about race as a variable. Health Serv. Res. 1994;29(1):1–16. [PMID:8163376] [PMC free article] [PubMed] [Google Scholar]
- 57.Lett E., Asabor E., Beltrán S., Cannon A.M., Arah O.A. Conceptualizing, contextualizing, and operationalizing race in quantitative health sciences research. Ann. Fam. Med. 2022;20(2):157–163. doi: 10.1370/afm.2792. [PMID:35045967] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martinez R.A.M., Andrabi N., Goodwin A.N., Wilbur R.E., Smith N.R., Zivich P.N. Conceptualization, operationalization, and utilization of race and ethnicity in major epidemiology journals, 1995-2018: a systematic review. Am. J. Epidemiol. 2023;192(3):483–496. doi: 10.1093/aje/kwac146. [PMID:35938872] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Swilley-Martinez M.E., Coles S.A., Miller V.E., Alam I.Z., Fitch K.V., Cruz T.H., et al. “We adjusted for race”: now what? A systematic review of utilization and reporting of race in American journal of epidemiology and epidemiology, 2020-2021. Epidemiol. Rev. 2023;45(1):15–31. doi: 10.1093/epirev/mxad010. [PMID:37789703] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wizentier M.M., Stephenson B.J.K., Goodman M.S. The measurement of racism in health inequities research. Epidemiol. Rev. 2023;45(1):32–43. doi: 10.1093/epirev/mxad004. [PMID:37147182] [DOI] [PubMed] [Google Scholar]
- 61.White K., Lawrence J.A., Tchangalova N., Huang S.J., Cummings J.L. Socially-assigned race and health: a scoping review with global implications for population health equity. Int. J. Equity Health BioMed Central. 2020;19(1):1–14. doi: 10.1186/s12939-020-1137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Borrell L.N., Kiefe C.I., Williams D.R., Diez-Roux A.V., Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc. Sci. Med. 2006;63(6):1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [PMID:16750286] [DOI] [PubMed] [Google Scholar]
- 63.Dixon A.R., Telles E.E. Skin color and colorism: global research, concepts, and measurement. Annu. Rev. Soc. 2017;31(43):405–424. doi: 10.1146/annurev-soc-060116-053315. [DOI] [Google Scholar]
- 64.Hochschild J.L., Weaver V. The skin color paradox and the American racial order. Soc. Forces. 2007;86(2):643–670. doi: 10.1093/sf/86.2.643. [DOI] [Google Scholar]
- 65.Krieger N., Sidney S., Coakley E. Racial discrimination and skin color in the CARDIA study: implications for public Health Research. Coronary artery risk development in young adults. Am. J. Public Health. 1998;88(9):1308–1313. doi: 10.2105/ajph.88.9.1308. [PMID:9736868] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lawrence J.A., Kawachi I., White K., Bassett M.T., Williams D.R. Instrumental variable analysis of racial discrimination and blood pressure in a sample of young adults. Am. J. Epidemiol. 2023;192(12):1971–1980. doi: 10.1093/aje/kwad150. [PMID:37401004] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Louie P. Revisiting the cost of skin color: discrimination, mastery, and mental health among black adolescents. Soc. Ment. Health. 2020;10(1):1–19. doi: 10.1177/2156869318820092. [DOI] [Google Scholar]
- 68.Monk E.P. The cost of color: skin color, discrimination, and health among African-Americans. Am. J. Sociol. 2015;121(2):396–444. doi: 10.1086/682162. [DOI] [PubMed] [Google Scholar]
- 69.Perreira K.M., Wassink J., Harris K.M. Beyond race/ethnicity: skin color, gender, and the health of young adults in the United States. Popul. Res. Policy Rev. 2019;38(2):271–299. doi: 10.1007/s11113-018-9503-3. [PMID:31595099] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zou H., Chen Y., Fang W., Zhang Y., Fan X. The mediation effect of health literacy between subjective social status and depressive symptoms in patients with heart failure. J. Psychosom. Res. 2016;91:33–39. doi: 10.1016/j.jpsychores.2016.10.006. [PMID:27894460] [DOI] [PubMed] [Google Scholar]
- 71.Coleman C., Birk S., DeVoe J. Health literacy and systemic racism-using clear communication to reduce health care inequities. JAMA Intern. Med. 2023;183(8):753–754. doi: 10.1001/jamainternmed.2023.2558. [PMID:37358860] [DOI] [PubMed] [Google Scholar]
- 72.Chen K.A., Kapadia M.R. Health literacy disparities: communication strategies to narrow the gap. Am. J. Surg. 2022;223(6):1046. doi: 10.1016/j.amjsurg.2021.11.035. [PMID:34887018] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Santana S., Brach C., Harris L., Ochiai E., Blakey C., Bevington F., et al. Updating health literacy for healthy people 2030: defining its importance for a new decade in public health. J. Public Health Manag. Pract. 2021;27(Suppl. 6):S258–S264. doi: 10.1097/PHH.0000000000001324. [PMID:33729194] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Persky S., Kaphingst K.A., Allen V.C., Senay I. Effects of patient-provider race concordance and smoking status on lung Cancer risk perception accuracy among African-Americans. Ann. Behav. Med. 2013;45(3):308–317. doi: 10.1007/s12160-013-9475-9. [PMID:23389688] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shen M.J., Peterson E.B., Costas-Muñiz R., Hernandez M.H., Jewell S.T., Matsoukas K., et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J. Racial Ethn. Health Disparities. 2018;5(1):117–140. doi: 10.1007/s40615-017-0350-4. [PMID:28275996] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Strumpf E.C. Racial/ethnic disparities in primary care: the role of physician-patient concordance. Med. Care. 2011;49(5):496–503. doi: 10.1097/MLR.0b013e31820fbee4. [PMID:21430577] [DOI] [PubMed] [Google Scholar]
- 77.Takeshita J., Wang S., Loren A.W., Mitra N., Shults J., Shin D.B., et al. Association of Racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw. Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.24583. [PMID:33165609] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Traylor A.H., Schmittdiel J.A., Uratsu C.S., Mangione C.M., Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J. Gen. Intern. Med. 2010;25(11):1172–1177. doi: 10.1007/s11606-010-1424-8. [PMID:20571929] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bigelow M., Schwarz R.L. National Institute for Literacy; 2010. Adult English Language Learners With Limited Literacy.https://eric.ed.gov/?id=ED512297 Available from: accessed Jun 17, 2024. [Google Scholar]
- 80.Heckman J. Varieties of selection Bias. Am. Econ. Rev. 1990;80(2):313–318. [Google Scholar]
- 81.United States Census Bureau QuickFacts: United States. 2020. https://www.census.gov/quickfacts/fact/table/US/PST045223 Available from: accessed May 19, 2024.
- 82.Groves R.M., Fowler F.J., Jr., Couper M.P., Lepkowski J.M., Singer E., Tourangeau R. 2nd ed. Wiley; Hoboken, NJ: 2009. Survey Methodology. ISBN:978–0–470-46546-2. [Google Scholar]
- 83.Parker R.M., Baker D.W., Williams M.V., Nurss J.R. The test of functional health literacy in adults: a new instrument for measuring Patients’ literacy skills. J. Gen. Intern. Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [PMID:8576769] [DOI] [PubMed] [Google Scholar]
- 84.Weiss B.D., Mays M.Z., Martz W., Castro K.M., DeWalt D.A., Pignone M.P., et al. Quick assessment of literacy in primary care: the newest vital sign. Ann. Fam. Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [PMID:16338915] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tavakol M., Dennick R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [PMID:28029643] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bather J.R., Goodman M.S., Kaphingst K.A. Racial segregation and genomics-related knowledge, self-efficacy, perceived importance, and communication among medically underserved patients. Genet. Med. Open. 2024;2 doi: 10.1016/j.gimo.2023.100844. [DOI] [Google Scholar]
- 87.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int. J. Epidemiol. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668. [PMID:11511581] [DOI] [PubMed] [Google Scholar]
- 88.Cassel J. The contribution of the social environment to host resistance: the fourth Wade Hampton frost lecture. Am. J. Epidemiol. 1976;104(2):107–123. doi: 10.1093/oxfordjournals.aje.a112281. [PMID:782233] [DOI] [PubMed] [Google Scholar]
- 89.Keene Woods N., Ali U., Medina M., Reyes J., Chesser A.K. Health literacy, health outcomes and equity: a trend analysis based on a population survey. J. Prim. Care Community Health. 2023;14 doi: 10.1177/21501319231156132. [PMID:36852725] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stormacq C., Van den Broucke S., Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integr. Rev. Health Promot. Int. 2019;34(5):e1–e17. doi: 10.1093/heapro/day062. [PMID:30107564] [DOI] [PubMed] [Google Scholar]
- 91.Chavez-Yenter D., Goodman M.S., Chen Y., Chu X., Bradshaw R.L., Lorenz Chambers R., et al. Association of disparities in family history and family cancer history in the electronic health record with sex, race, hispanic or latino ethnicity, and language preference in 2 large US health care systems. JAMA Netw. Open. 2022;5(10) doi: 10.1001/jamanetworkopen.2022.34574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: Sample characteristics by health literacy status
Data Availability Statement
The data that support the findings of this study are available from the Center for Anti-racism, Social Justice & Public Health (gph.casjph@nyu.edu), upon reasonable request.