Abstract
Background
Cigarette smoking is one of the leading causes of preventable death in the world. Decisions to smoke are often made within a broad social context and therefore community interventions using coordinated, multi‐component programmes may be effective in influencing the smoking behaviour of young people.
Objectives
To determine the effectiveness of multi‐component community based interventions in influencing smoking behaviour, which includes preventing the uptake of smoking in young people.
Search methods
The Tobacco Addiction group's specialised register, Medline and other health, psychology and public policy electronic databases were searched, the bibliographies of identified studies were checked and raw data was requested from study authors. Searches were updated in August 2010.
Selection criteria
Randomized and non randomized controlled trials that assessed the effectiveness of multi‐component community interventions compared to no intervention or to single component or school‐based programmes only. Reported outcomes had to include smoking behaviour in young people under the age of 25 years.
Data collection and analysis
Information relating to the characteristics and the content of community interventions, participants, outcomes and methods of the study was extracted by one reviewer and checked by a second. Studies were combined in a meta‐analysis where possible and reported in narrative synthesis in text and table.
Main results
Twenty‐five studies were included in the review and sixty‐eight studies did not meet all of the inclusion criteria. All studies used a controlled trial design, with fifteen using random allocation of schools or communities. One study reported a reduction in short‐term smoking prevalence (twelve months or less), while nine studies detected significant long‐term effects. Two studies reported significantly lower smoking rates in the control population while the remaining thirteen studies showed no significant difference between groups. Improvements were seen in secondary outcomes for intentions to smoke in six out of eight studies, attitudes in five out of nine studies, perceptions in two out of six studies and knowledge in three out of six studies, while significant differences in favour of the control were seen in one of the nine studies assessing attitudes and one of six studies assessing perceptions.
Authors' conclusions
There is some evidence to support the effectiveness of community interventions in reducing the uptake of smoking in young people, but the evidence is not strong and contains a number of methodological flaws.
Keywords: Adolescent, Child, Female, Humans, Male, Young Adult, Health Promotion, Smoking Prevention, Age Factors, Controlled Clinical Trials as Topic
Plain language summary
Can community interventions deter young people from starting to smoke?
Some evidence is available to suggest that multi‐component community interventions are effective in influencing smoking behaviour and preventing the uptake of smoking in young people. These interventions use co‐ordinated, widespread, multi‐component programmes to try and influence young people's behaviour. Community members are often involved in determining and/or implementing these programmes. These include education of tobacco retailers about age restrictions, programmes for prevention of smoking‐related diseases, mass media, school and family‐based programmes. Changes in intentions to smoke, knowledge, attitudes and perceptions about smoking did not generally appear to affect the long‐term success of the programmes.
Summary of findings
Summary of findings for the main comparison. Community interventions for preventing smoking in young people.
| Community interventions for preventing smoking in young people | ||||||
| Patient or population: patients with preventing smoking in young people Settings: Intervention: Community interventions | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Community interventions | |||||
| Weekly smoking Follow‐up: 2‐ to 15‐years | Study population | OR 0.83 (0.59 to 1.17) | 17508 (7 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 169 per 1000 | 144 per 1000 (107 to 192) | |||||
| Medium risk population | ||||||
| 170 per 1000 | 145 per 1000 (108 to 193) | |||||
| Monthly smoking Follow‐up: 2‐ to 15‐years | Study population | OR 0.97 (0.81 to 1.16) | 27077 (9 studies) | ⊕⊝⊝⊝ very low1,2,3 | ||
| 148 per 1000 | 144 per 1000 (123 to 168) | |||||
| Low risk population | ||||||
| 140 per 1000 | 136 per 1000 (116 to 159) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval OR: Odds ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 A mixture of RCT's and CCT's were used, lack of allocation concealment, blinding and significant loss to follow‐up 2 Significant heterogeneity as determined by a combination of visual data inspection and I‐squared statistic. 3 Some studies required manual adjustment for clustering effects as this was not addressed by the original study authors
Background
The reduction of smoking prevalence among adolescents remains a key public health priority (BMA 2008). Addiction to nicotine usually begins during adolescence although the proportion of new smokers who first use cigarettes after the age of 18 has increased in the United States from around 25% in 2002 to 40% in 2009 (SAMHSA 2009). An estimated one‐in‐five young teenagers already smokes regularly and another 30 million children throughout the world will take up the habit every year (GYTSC 2002) with 19.1% of school students who had never smoked cigarettes indicating that they would initiate smoking within the next year (MMWR 2008). In England the prevalence of regular smoking amongst 11 to 15 year olds in 2009 was 6%, a decline from 13% in 1996 (NHS IC 2010). Amongst 15 year olds the prevalence was higher in girls (16%) than boys (14%) (NHS IC 2010). Current reports still indicate that globally, smoking behaviour among adolescent girls is increasing over that of boys (Mackay 2006; Warren 2009). The UMDNJ 2007 New Jersey Youth Tobacco Survey estimates that 90 million cigarettes, or 4.2 million packs of cigarettes were consumed by high‐school students annually in 2006.
There is a wide‐held theory that if smoking does not start during adolescence, it is unlikely ever to occur (USDHHS 1994). This has resulted in various attempts to reduce the number of young people taking up smoking through primary prevention programmes, which have been designed to discourage experimentation with cigarettes and to deter regular use. Most interventions have included prevention programmes delivered in school settings, however the results have been mixed and reported effects small (Rooney 1996, Wiehe 2005, Thomas 2006). Mass media interventions have been compared in another Cochrane review, Brinn 2010 also with mixed results. The most effective campaigns for the review (Brinn 2010) were based on solid theoretical grounds, used formative research in designing the campaign message, and the message broadcasts were of reasonable intensity over extensive periods of time. Recognition that decisions to smoke are made within a broad social context has led to the development and implementation of community‐wide programmes. Such interventions are based on the premise that social and environmental processes impact upon health and well‐being and contribute to health decline, disease, and mortality. It has been argued that the essence of the community approach to influence smoking behaviour, in particular smoking prevention lies in its multi‐dimensionality, in the co‐ordination of activities to maximise the chance of reaching all members, and in ongoing and widespread support for the maintenance of non‐smoking behaviour (Schofield 1991).
Interventions with multiple components such as age restrictions for tobacco purchase, tobacco‐free public places, various mass media communications and special programmes in schools are often combined to create large‐scale community‐wide initiatives, to influence the smoking behaviour of young people. Initiatives vary in the extent to which they emphasise community involvement in problem specification and planning of the intervention. Some have been conducted through community groups and organisations emphasising a principle of 'ownership' or 'partnership' in promoting health. Community members are involved in decisions about the implementation of various activities within the programme, often building on existing organisational structures.
Despite the potential of community‐wide programmes, debate continues about their effectiveness in influencing the smoking behaviour of young people. For example, a non‐systematic review of eighteen smoking prevention programmes up to 1995 concluded that community initiatives have yet to demonstrate that they can directly reduce smoking prevalence in adolescents (Stead 1996).
Objectives
To carry out a systematic review to assess the effectiveness of community interventions in influencing the smoking behaviour of young people. In particular the following issues were addressed:
a. The effectiveness of community interventions, compared with no intervention in influencing the smoking behaviour of young people;
b. The effectiveness of community interventions compared with other single component interventions (e.g. school‐based programmes) in influencing the smoking behaviour of young people.
Methods
Criteria for considering studies for this review
Types of studies
We considered studies using one of the following designs:
a. RCT: (randomized controlled trials) in which participants were assigned prospectively to one or more alternative forms of intervention using a process of random allocation;
b. CCT: (controlled clinical trials) in which participants were assigned prospectively at the level of community, geographical region or school, to one or more alternative intervention groups using a quasi‐random allocation method, or in which the method of assignment was unclear but could possibly have been random or quasi‐random;
c. CBA: (controlled before‐and‐after trial) where contemporaneous baseline and post‐intervention data was collected from the intervention group and a comparable population, (no CBA studies were identified for inclusion in this review).
Each study needed to have a minimum of two clusters in each of the intervention and control groups.
Studies which did not report baseline characteristics were excluded.
Types of participants
Young people aged less than 25 years.
Types of interventions
Interventions were considered which:
a. were targeted at entire or parts of entire communities or large areas, and;
b. had the intention of influencing the smoking behaviour of young people, and;
c. focused on multi‐component (i.e. more than one) community intervention, which could include but was not limited to: school‐based programmes, media promotion (e.g. TV, radio, print), public policy, organisational initiatives, health care provider initiatives, sports, retailer and workplace initiatives, anti‐tobacco contests and youth anti‐smoking clubs.
Community interventions were defined as coordinated widespread (multi‐component) programmes in a particular geographical area (e.g. school districts) or region or in groupings of people who share common interests or needs, which support non‐smoking behaviour.
Studies which only included single component interventions, did not have community involvement (e.g. school‐based only) or had mass media as the sole form of intervention delivery were excluded.
Types of outcome measures
Young people were classified as smokers or non‐smokers in different ways according to daily, weekly or monthly frequency of smoking, or by lifetime consumption. Where possible the strictest distinction was used, in which youths with any history of cigarette use were defined as smokers.
Primary outcomes
The primary outcome measure of smoking behaviour were objective (e.g. saliva thiocyanate levels, alveolar carbon monoxide) or self‐reported smoking. This outcome was measured in terms of:
a) the level of change in smoking behaviour observed,
b) the sustainability of the change in behaviour after the intervention ('less than' versus 'longer than' one year).
Search methods for identification of studies
Possible studies were identified from the Cochrane Tobacco Addiction Group Database which includes reports of possible trials identified from regular searches of CENTRAL, MEDLINE, EMBASE and PsycINFO (see search strategies and dates in the Tobacco Addiction Group Module). Additional searches covered a wider range of databases and combined terms related to smoking, young people and community‐wide interventions.
Electronic searches
For this update searches were limited by publication date from 2002 onwards. The search platform is that used for the present update. The following databases were searched:
Searched via OVID on 18th August 2010: Medline, EMBASE, PsycINFO, Econlit. Searched via CSA on 19th August 2010: Sociological Abstracts, British Humanities Index, PAIS, ERIC, ASSIA. Searched in the Cochrane Library issue 3, 2010: Cochrane Central Database of Controlled Trials (CENTRAL)
Other databases searched for the original review were no longer easily available, and since no original studies had been located solely from one of these sources we did not update these searches. Databases searched for earlier versions are listed in Appendix 1
The MEDLINE strategy is listed below. Other strategies are provided in the Appendix
1 exp Smoking/ 2 "Tobacco Use Disorder"/ or Tobacco/ 3 (smoking or tobacco or cigarette$).ti,ab. 4 1 or 2 or 3 5 (young adj people).ti,ab,sh. 6 (children or juveniles or girls or boys or teenagers or adolescents).ti,ab. 7 Adolescent/ 8 Child/ 9 minors.ti,ab,sh. 10 8 or 6 or 7 or 9 or 5 11 (nationwide or statewide or countrywide or citywide).ti,ab,sh. 12 (nation adj wide).ti,ab,sh. 13 (state adj wide).ti,ab,sh. 14 ((country or city) adj wide).ti,ab,sh. 15 outreach.ti,ab,sh. 16 (multi adj (component or facet or faceted or disciplinary)).ti,ab,sh. 17 (field adj based).ti,ab,sh. 18 (interdisciplinary or (inter adj disciplinary)).ti,ab,sh. 19 local.ti. 20 citizen$.ti,ab,sh. 21 (community or communities).mp. 22 11 or 21 or 17 or 12 or 20 or 15 or 14 or 18 or 13 or 16 or 19 23 22 and 4 and 10
Searching other resources
The bibliographies of papers identified in the electronic searches were checked for any additional relevant studies, and personal contact with content area specialists were made.
Data collection and analysis
Selection of studies
From the title, abstract, or descriptors, KC independently reviewed the literature searches to identify potentially relevant trials. All studies that clearly did not meet the inclusion criteria in terms of study design, population or interventions, were excluded. All potential inclusions and 'exclude but relevant' studies were confirmed by a second author (MB).
Data extraction and management
One review author (KC) completed data extraction for each included study, which was reviewed by an additional author (either MB or NL) using a tailored standardised data extraction form. All disagreements were resolved by consensus.
Assessment of risk of bias in included studies
The quality of included studies were assessed using the ‘Risk of bias’ tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) and additional criteria developed by the Cochrane EPOC Group (EPOC 2009). One review author (KC) independently assessed the risk of bias for each included study, which was independently assessed again by one of two additional authors (MB or NL). All disagreements were resolved by consensus. Risk of bias was assessed with the following seven domains: sequence generation; allocation concealment; blinding of participants and outcome assessors; incomplete outcome data; selective outcome reporting; and other potential threats to validity (Higgins 2008). Three additional domains were included that assessed design‐specific threats to validity including: imbalance of outcome measures at baseline; comparability of intervention and control group characteristics at baseline; and protection against contamination (EPOC 2009). Finally, for cluster study designs, we assessed the risk of bias associated with an additional domain; selective recruitment of participants. In studies eligible for inclusion in this review, the term ‘participant’ may refer to schools, community organisations and individual young people.
Measures of treatment effect
Outcomes
Outcome measures for RCT, CCT and CBA studies were selected in accordance with Cochrane Collaboration standards (Higgins 2008) for dichotomous outcomes, continuous outcomes (mean difference) and counts or rates (rate ratio).
Unit of analysis issues
Studies found to contain unit of analysis errors were re‐analysed if data were available. Unit of analysis errors are found in studies that allocate participants to treatment or control in clusters (e.g. schools and communities), but analyse the results by individual participants. This can result in overestimation of the statistical significance of the results by not accounting for the clustering of individuals in the data (Rooney 1996; Ukoumunne 1999). For studies that did not include adjustments for clustering the size of the trial was reduced to the effective sample size (Rao 1992) using the original sample size from each study, divided by a design effect of 1.2 which is consistent with other smoking cessation community intervention trials (Gail 1992) and as per recommendations in the Cochrane Handbook, section 16.3.4 (Higgins 2008).
Dealing with missing data
Where statistics essential for analysis were missing (e.g. group means and standard deviations for both groups are not reported) and can not be calculated from other data, we attempted to contact the authors to obtain data.
Assessment of reporting biases
Potential reporting biases would have been assessed using a funnel plot, providing the inclusion of greater than ten studies for each reported outcome. Asymmetry in the plot could be attributed to publication bias, but may well be due to true heterogeneity, poor methodological design or artefact. As there were fewer than ten studies for each outcome, the reporting biases have been extrapolated within the 'other bias' section in the risk of bias tables.
Data synthesis
Meta‐analyses were only conducted if relevant, valid data were available from at least two studies of the same design, with interventions that were conceptually similar (e.g. interventions that include school components) and measured the same outcome. The fixed‐effects model was used for meta‐analysis with the exception of data presenting significant heterogeneity as determined by a combination of the I² statistic (> 60%) and visual inspection of the data. In such instances the analysis was converted to the random‐effects model.
For smoking behaviour outcomes entered in a meta‐analysis we used outcomes reported at the longest follow up. Studies that reported a follow up at less than 12 months and after a longer period could be included in both time periods in the sub group analysis by duration of follow up. For studies with multiple outcome measures that were appropriate for inclusion in a meta‐analysis, the authors ranked the effect sizes of each measure and used the median value. Where two appropriate measures were used, the most conservative value was taken.
A tabular analysis considering the direction of observed effects and size for each study outcome is presented in Additional tables. A narrative synthesis was also conducted taking into consideration the methodological quality of each study (Results).
Subgroup analysis and investigation of heterogeneity
The effects of community interventions are complex, and may be influenced by a number of competing factors. Significant heterogeneity relating to results and study characteristics was determined by a combination of the I² statistic (> 60%) and visual inspection of the data as per recommendations in the Cochrane handbook, chapter 9.5.4 (Higgins 2008). We were unable to use a Forrest plot for visual inspection of the data due to an insufficient number of included studies for the reported outcomes. We conducted sub‐group analyses to further investigate the different aspects of community intervention programmes. Subgroup analyses were conducted only if comparable data (as outlined above) was available from two studies, which could be considered similar enough to be included in the same subgroup, (e.g. two studies conducted in rural areas), or reporting separate outcomes for different subgroups (e.g. by gender). The following characteristics were pre‐specified for possible sub‐group analysis prior to data extraction:
a) Population ‐ e.g. developed/developing countries or urban/rural populations
b) Subjects ‐ e.g. gender, age or socioeconomic status
c) Intervention ‐ e.g. number of intervention components, duration of interventions or intensity of interventions
d) Design ‐ e.g. duration of follow‐up
Sensitivity analysis
Sensitivity analysis was conducted on studies with a high risk of bias for sequence generation and allocation concealment.
Results
Description of studies
See: Characteristics of included studies and Characteristics of excluded studies tables
Results of the search
Reports relating to twenty five studies met all of the inclusion criteria from 2717 articles (see Figure 1 for PRISMA diagram). Detailed information about each included study is provided in the 'Characteristics of included studies' table. (See 'Characteristics of excluded studies' for details of the sixty eight excluded studies and reasons for exclusion.) All of the included studies used a controlled trial design with clustering.
1.
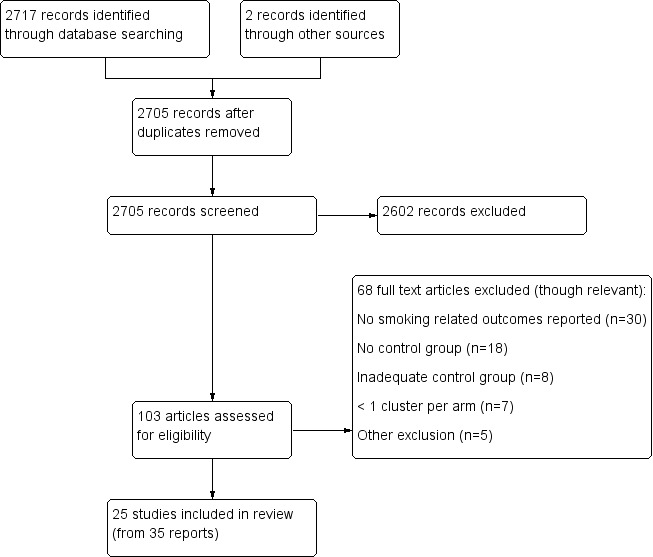
Flow diagram of literature for this review
Included studies
All 25 studies investigated the effects of multi‐component community interventions directed at young people, <25 years, using either a parallel group RCT (n=15) or CCT (n=10) design. Trials were published between 1989 and 2009, though the methodology and preliminary results for some studies were published earlier; from 1983. A total of approximately 104,000 participants were recruited from a mixture of schools (n=735), community clubs (n=92), communities/cities/towns n=49 and paediatric practices (n=12). Seventeen studies originated from the United States of America, three from Australia, two from the United Kingdom and one each from India and Finland. One study (De Vries 2003) included six countries (Denmark, Finland, Netherlands, Portugal, Spain and the United Kingdom) as a nested, cluster controlled clinical trial.
Characteristics of communities:
The communities in which the interventions took place varied across the studies. For example, in one study the populations of the communities randomised ranged from 1,700 to 13,500 (Biglan 2000) and another was based in a city of 1.3 million people (Pentz 1989), while the largest study spanned six countries (De Vries 2003). Some communities were in rural areas (Biglan 2000; Hancock 2001) whilst others were in towns or cities in predominantly urban areas (Winkleby 1993; Perry 1994; Piper 2000) and some communities were specifically targeted because of economic deprivation (St Pierre 1992; Perry 2008).
Characteristics of participants:
The participants varied across studies. Some studies targeted young people in specific high‐risk groups; for example those defined as high‐risk because they lived in a deprived area (St Pierre 1992; Perry 2008), because they attended a continuation high‐school (continuation high‐schools are alternative high‐schools in the USA for young people at risk of dropping out of the school) (Sussman 1998; Winkleby 2004), or because they were expected to have a high smoking prevalence (Elder 2000). Native American children living on reservations were targeted in one study (Schinke 2000). The age of participants ranged from 8 to 24 years across the different studies. The age of targeted participants also varied and ranged from 10 to 24 years of age.
Characteristics of interventions:
The interventions evaluated in the 25 studies were diverse and each differed in the focus of activity. Thirteen focused specifically on influencing youth smoking behaviour through tobacco prevention initiatives (St Pierre 1992; Gordon 1997; Tang 1997; Sussman 1998; Biglan 2000; Elder 2000; Piper 2000; Schinke 2000; Stevens 2002; Schofield 2003; Gordon 2008; Perry 2008; Klein 2009), five included tobacco prevention with an additional aim to reduce specific health risk factors for cancer (Hancock 2001) or cardiovascular disease (Winkleby 1993; Perry 1994; Baxter 1997; Vartiainen 1998), while the remaining seven studies combined goals through a combination of tobacco prevention with either reduction or cessation initiatives (Pentz 1989; Murray 1994; D'Onofrio 2002; De Vries 2003; Perry 2003; Winkleby 2004; Hawkins 2009). Though the interventions for all studies involved influencing smoking behaviour, nine studies also included interventions for alcohol, (Elder 2000; Stevens 2002) alcohol and marijuana (Schinke 2000) or alcohol, marijuana, other drug use and/or delinquent behaviour (Pentz 1989; St Pierre 1992; Sussman 1998; Piper 2000; Stevens 2002; Perry 2003).
The extent to which attempts were made to include community participation also varied significantly. In five studies community leaders were encouraged to become actively involved in both the development and in giving ongoing support for the community programmes (Perry 1994; Piper 2000; Hancock 2001; Perry 2003; Hawkins 2009), though the duration and intensity of involvement differed. In the 'Age Appropriate' arm of the Piper 2000 study a community organiser was employed for six months over a three year period whilst in the 'Intensive' arm the organiser was employed for one fifteen month block. They were trained to use survey data, prioritise and target risk factors for prevention actions and to choose which prevention policies and programmes addressed the communities needs. However, in the Perry 2003 study, eight community organisers were hired to create and facilitate extra‐curricular activities for the second component of the D.A.R.E. intervention. In the study by Hawkins 2009, community leaders received six training sessions delivered over six to twelve months to form a community coalition of diverse stakeholders to implement and monitor the intervention. Other studies involved multiple organisations including the national health service, city councils, social workers, business owners, voluntary organisations, sports organisations, health care providers, community organisations, media, retailers, schools, government, law enforcement or workplaces.
Specific intervention components:
The majority of studies included school components in addition to a multi‐component community intervention (twenty one of the twenty five included studies), though the duration and intensity differed. As examples, Biglan 2000 had five class sessions over a one week period for three consecutive years, and Hawkins 2009 allowed schools to choose any combination of school and community programmes which ranged from five, two‐hour weekly sessions to weekly, year‐long classroom activities; Pentz 1989 included ten school and homework sessions per year over two years, while D'Onofrio 2002 only included an optional activity to conduct a tobacco survey at school as part of an intervention run through local community 4‐Health Clubs. This intervention included education, booklets, worksheets, puzzles, stories, experiments, poster and activities to make a anti‐smoking commercial at 4‐Health Clubs. One other trial conducted an intervention with local girls' and boys' Clubs St Pierre 1992 including education, group activities and video sessions, however no school‐based interventions were included. In total four studies included no school related activities (St Pierre 1992; Elder 2000; Stevens 2002; Klein 2009). The remaining three studies involved: recruitment from a migrant education programme with an intervention focusing on parent/child communications with eight weeks of evening group meetings plus booster sessions (Elder 2000); Stevens 2002 enrolled subjects from a paediatric primary care setting, where the family would decide upon a personal tobacco prevention policy with the addition of subsequent clinician education visits, twelve mail out newsletters specific to adults and twelve specific to young people in addition to letters from their respective clinician. Finally the Klein 2009 intervention focused on the government initiated 'Clean Indoor Air' policy as their programme, with an evaluation of the subsequent smoking ban in public places, particularly in restaurants, cafes and bars.
Optional extracurricular projects were added to some interventions including organisation of a tobacco‐free day and the option of working with community agencies on tobacco use prevention (D'Onofrio 2002), non‐smoking conference attendance on National non‐smoking day (De Vries 2003), health fairs, after‐school clubs and amusement park activities (Gordon 2008), promotion of World No Tobacco Day (Schofield 2003), drug‐free parties and drug‐awareness week (Sussman 1998), amongst others (Hancock 2001; Perry 2003). Four studies used incentives for completion of tobacco prevention assignments and to improve class attendance (Piper 2000; Stevens 2002; Schofield 2003; Gordon 2008).
Sixteen trials involved parent/guardian participation which mainly included education through pamphlets or homework requiring parent/guardian involvement (Gordon 1997; Biglan 2000; Piper 2000; Hancock 2001; D'Onofrio 2002; Perry 2003; Schofield 2003; Perry 2008; Gordon 2008; Hawkins 2009). Though some studies did have stronger parental involvement with equal parent/youth attendance for group sessions (Elder 2000; Stevens 2002), requests or incentives to quit smoking as a role model (De Vries 2003; Tang 1997), or attendance at tobacco prevention information sessions (Pentz 1989; Schinke 2000). Ten studies included peers as role models, (Baxter 1997; Vartiainen 1998; Biglan 2000; Elder 2000; Piper 2000; Perry 2003;Schinke 2000; Schofield 2003; Perry 2008;Winkleby 1993), two of which used older high‐school students (Winkleby 1993; Schinke 2000). Four studies were simultaneously run with adult programmes (Winkleby 1993; Perry 1994; Baxter 1997; Vartiainen 1998).
Media advocacy components were included in nine studies, two of which included television prevention initiatives (Pentz 1989; De Vries 2003) in addition to other media. The remaining seven studies used a combination of local media publications, magazines, radio, flyers, posters and newspapers (Winkleby 1993; Perry 1994; Tang 1997; Biglan 2000; Piper 2000; Schinke 2000; Hancock 2001).
Six interventions aimed at young people included components focusing on reducing tobacco scales to minors. Some included specific activities for youth to reduce illegal tobacco sales, (Biglan 2000; De Vries 2003; Schofield 2003; Winkleby 2004) whilst the study by Gordon 1997 reminded tobacco retailers about the law before conducting retailer tests where young people attempted to purchase tobacco products. Another study (Tang 1997) provided retailer education and surveillance.
Health care professionals as intervention deliverers were a key component in four studies and a smaller component of interventions in four other studies. The study by Stevens 2002, used the paediatric primary care setting to recruit youth and implement the intervention via family/clinician meetings through individualised development of a smoke‐free policy, for each family. Other studies included training for pharmacists and dental care interventions (De Vries 2003), continuing education and utilisation of health professionals (Perry 1994; Hancock 2001), or simply provided health education through intervention components such as mass media and other health promotion activities (Pentz 1989; Piper 2000; Schofield 2003; Winkleby 2004). Further encouragement into healthy life‐style choices through smoke‐free sporting events such as roller‐skating, rock climbing, bowling, snowboarding, skiing, disc golf tourneys and skateboarding competitions, were also aspects to the Sussman 1998, De Vries 2003 and Gordon 2008 studies.
Specific control components:
Most studies used usual activities as the control groups (Baxter 1997; Tang 1997; St Pierre 1992; Winkleby 1993; Murray 1994; Perry 1994; Sussman 1998; Vartiainen 1998; Piper 2000; Schinke 2000; Hancock 2001; D'Onofrio 2002; De Vries 2003; Schofield 2003; Gordon 2008; Klein 2009; Hawkins 2009), though two studies included minimal interventions which included components to influence youth smoking behaviour ‐ Biglan 2000 opted to invest the same intensity and duration for the programme, where the intervention focused on drug use prevention, and Gordon 1997 provided control students with smoking prevention booklets which were used in schools, plus take home workbooks. Retailers were also tested for underage cigarette purchases in the control catchment areas through students attempting purchases. Three control areas were provided with delayed interventions, which were commenced after the evaluation period for the studies were completed (Pentz 1989; Perry 2003; Perry 2008). One study (Schofield 2003) offered the intervention to control schools after completion of the evaluation only if the schools requested it, however support was offered for other health related issues during the evaluation period. Other initiatives unrelated to smoking were used as controls in some studies to account for biases associated with increased resources and attention provided to intervention subjects, or as an alternative means of providing some form of benefit to the control clusters for their participation in the evaluation. The control group in Elder 2000 consisted of a first aid and home safety education programme focused on preparation for emergencies, skills and household safety concerns such as baby‐proofing a house. Education, role‐playing sessions and intensity of the programme mimicked that of the smoking prevention intervention. In Winkleby 2004 school students learned about drug and alcohol abuse prevention through a modified version of Project Toward No Drug abuse, (Sussman 1998) focusing on health motivation, social skills and decision making regarding drug and alcohol use.
Intervention delivery:
Methods for the programme message implementation varied significantly between studies with the majority of interventions delivered by multiple individuals. Teachers and other school faculty contributed to intervention delivery in sixteen studies (Pentz 1989; Murray 1994; Perry 1994; Tang 1997; Sussman 1998; Vartiainen 1998; Biglan 2000; Piper 2000; Schinke 2000; Hancock 2001; De Vries 2003; Schofield 2003; Perry 2003; Gordon 2008; Perry 2008; Hawkins 2009) and were trained by study investigators or paid research staff. The level of training varied between studies and within study clusters, for example in De Vries 2003, the largest study including six countries, training for teachers varied from two to forty‐eight hours. Adult and youth volunteers contributed as trained volunteer leaders (Sussman 1998; D'Onofrio 2002), volunteers for Big Brother and Big Sister tutoring programmes (Hawkins 2009), peer narrators for prevention information (Gordon 2008) or other roles (Biglan 2000; Elder 2000; Hancock 2001). Peers were also elected by teachers or fellow class mates and were trained to act as role models and deliver influential programme messages for seven studies (Pentz 1989; Winkleby 1993; Perry 1994; Vartiainen 1998; Perry 2003; Schofield 2003; Perry 2008). Similarly, five studies recruited parents as channels to enhance and deliver programme information (Elder 2000; Schinke 2000; De Vries 2003; Schofield 2003; Gordon 2008). Research or project staff delivered the intervention directly to individuals only in four studies (Sussman 1998; Vartiainen 1998; Winkleby 2004; Gordon 2008) whilst specialised groups were used for six studies. These groups included cancer Council health educators, (Hancock 2001) health and human services workers for community based, youth focused and family focused programmes, (Hawkins 2009) government level policies, (Klein 2009) paediatric primary care clinicians, (Stevens 2002) and law enforcement (Schinke 2000; Perry 2003).
Follow‐up:
The duration of follow up at which smoking status was assessed differed between studies and in some cases was not clear. Outcomes were measured, for example, at the end of the intervention (Baxter 1997; Gordon 1997; De Vries 2003), one year later (Sussman 1998; Baxter 1997; Hancock 2001), approximately one and a half years later (Elder 2000; D'Onofrio 2002), three and a half years later (Schinke 2000), and in the case of one study, fifteen years after the intervention (Vartiainen 1998).
Outcome collection:
Smoking behaviour was assessed in all studies by self‐report, though two studies used face‐to‐face interviews for data collection purposes. A number of different intermediate outcomes were measured, including knowledge about the effects of smoking, attitudes toward smoking and intentions to smoke in the future. Chemical validation occurred in eight studies by exhaled carbon monoxide (Pentz 1989; Winkleby 1993; Murray 1994; Sussman 1998; Biglan 2000; Elder 2000; Piper 2000; Winkleby 2004) in addition to plasma thiocyanate levels for one study (Winkleby 1993). A random number of students in half of the school classes in the Perry 1994 study were assessed for saliva thiocyanate levels, whilst in the Schinke 2000 trial only a small proportion were analysed. Researchers in the Piper 2000 study collected exhaled carbon monoxide samples for bogus pipeline measures only.
Outcome collection occurred through different methods which could also differ at various time points throughout the study and in some trials methods, were not clear. These include research staff and trained data collectors in nine studies, (Pentz 1989; St Pierre 1992; Perry 1994; Sussman 1998; Vartiainen 1998; Piper 2000; Schofield 2003; Winkleby 2004; Perry 2008) school teachers and/or other faculty in eleven (Murray 1994; Baxter 1997; Gordon 1997; Tang 1997; Biglan 2000; Hancock 2001; De Vries 2003; Perry 2003; Schofield 2003; Gordon 2008; Hawkins 2009), via telephone calls in four studies (Biglan 2000; D'Onofrio 2002; Winkleby 2004; Klein 2009), postal questionnaires in six (Pentz 1989; Tang 1997; Vartiainen 1998; Biglan 2000; D'Onofrio 2002; Stevens 2002), and face‐to‐face in two (Winkleby 1993; Elder 2000). One study (Biglan 2000) sent $10 in an envelope with the questionnaire as an incentive for parents to complete and return the survey.
Risk of bias in included studies
Key methodological features of the twenty five included studies are summarised in the table of characteristics of included studies (Figure 2).
2.
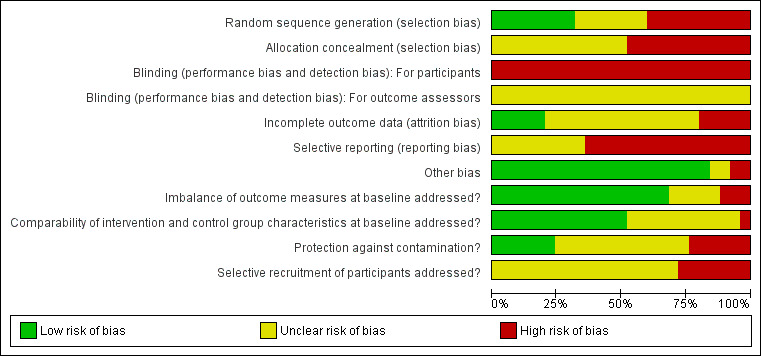
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Sequence generation:
Methods for choosing intervention and control areas varied across studies and in some cases the details provided were unclear. Some studies chose areas specifically to target particular groups of young people such as those with a high risk of substance abuse (Sussman 1998). In some studies the allocation of areas, communities or schools within particular geographical regions to either intervention or control was random (Schinke 2000), whilst for other studies allocation was random after communities or areas had been matched on a number of different factors. The investigators described a random component for sequence generation in eight studies (Gordon 1997; Biglan 2000; Hancock 2001; Schinke 2000; D'Onofrio 2002; Winkleby 2004; Gordon 2008; Hawkins 2009) which includes coin tossing or the use of computer generated random number tables. Ten studies had inadequate sequence generation (Pentz 1989; St Pierre 1992; Winkleby 1993; Perry 1994; Baxter 1997; Tang 1997; Vartiainen 1998; Piper 2000; De Vries 2003; Klein 2009), and the remaining seven studies were unclear.
Allocation concealment:
Allocation concealment was inadequate in twelve studies, i.e. the assignment of participants was not conclealed from investigators (Pentz 1989; St Pierre 1992; Winkleby 1993; Murray 1994; Perry 1994; Baxter 1997; Tang 1997; Vartiainen 1998; Piper 2000; De Vries 2003; Klein 2009), and unclear in the remaining thirteen.
Blinding for participants and outcome assessors:
All studies were inadequate in terms of blinding for participants due to the nature of a community‐delivered intervention. No authors mentioned any attempts to conceal subject allocation from outcome assessors.
Incomplete outcome data:
Complete reporting of outcome data occurred in five studies (Vartiainen 1998; De Vries 2003; Perry 2003; Perry 2008; Hawkins 2009), which accounted for attrition in the sample population and described methods of handling missing variables in data sets, such as via random imputation or removal of data sets missing 90% of the responses etc. Five other studies failed to address incomplete outcome data. Baxter 1997 had significant amounts of data missing from one of the intervention schools and three classes in the control school; Hancock 2001 failed to mention characteristics of participants unable to be followed up and mentioned the collection of weekly and ever smoking data outcomes, however the data was not presented as it was deemed 'very similar' to the results for monthly smoking. The Klein 2009 study was unable to collect data at some time points due to gaps in funding, whereas the Piper 2000 study were unable to schedule in‐school surveys for two intensive and one control school despite attempts. Both the Hancock 2001 and St Pierre 1992 studies mentioned outcome variables as being collected, which were not reported in the publications. The remaining fourteen studies had unclear reporting of incomplete outcome data.
Selective reporting:
Selective reporting was unclear in nine studies (Murray 1994; Baxter 1997; Gordon 1997; Sussman 1998; Vartiainen 1998; Schinke 2000; Perry 2003; Schofield 2003; Winkleby 2004) and was a high risk of bias for the remaining fifteen. Examples of selective reporting include outcomes reported incompletely with missing n‐values for separate intervention and control groups or as a visual representation only which can not be meta‐analysed or studies failing to include results for a key outcome which would be expected to be reported for such a study.
Imbalance of outcome measures at baseline:
Three studies (Winkleby 1993; Baxter 1997; Schofield 2003) failed to address imbalances in outcome measures at baseline, five studies were unclear (Tang 1997; Gordon 1997; Hancock 2001; Perry 2003; Winkleby 2004), whilst the remaining seventeen studies accounted for any imbalances in outcome measures at baseline through statistical measures.
Comparability of intervention and control characteristics at baseline:
Only one study failed to address comparability of intervention and control group characteristics at baseline. In Pentz 1989 the authors mentioned a possibility of non‐equivalence of study groups, since the majority of schools were assigned to programme and control conditions based on administrator flexibility. No adjustments were made in the analysis to account for these imbalances. Thirteen studies adequately addressed imbalances in intervention and control characteristics at baseline through statistical adjustments or did not have any significant imbalances (St Pierre 1992; Winkleby 1993; Murray 1994; Perry 1994; Vartiainen 1998; Piper 2000; Schinke 2000; Hancock 2001; D'Onofrio 2002; Stevens 2002; Perry 2008; Hawkins 2009; Klein 2009). The remaining 11 studies had unclear comparability between study characteristics at baseline.
Protection against contamination:
Seven studies had potential sources of contamination: A state‐wide tobacco education programme was initiated in 1990, which may have affected the control group results in the D'Onofrio 2002 study. The control group in the Netherlands for the De Vries 2003 study also underwent a national smoking prevention programme simultaneously with the evaluation for this programme. The Elder 2000 study had schools containing both intervention and control groups within them, whilst authors in the Gordon 1997 study mentioned contamination as a difficulty in their discussion. St Pierre 1992 provided the intervention to boys and girls clubs, a setting in which authors believe a natural 'booster programme' effect may have occurred for both prevention groups, thus making the two treatment groups similar. In addition, 87% of the 'SMART only' and 87% of the 'controls' reported learning about alcohol and other drugs from an intervention programme at school. For the Tang 1997 study, authors mention a possibility that little difference existed between the extent of exposure for intervention and control conditions. Furthermore, a comprehensive programme aimed at reducing the sale of cigarettes to minors was implemented in the control in Northern Sydney during the closing stages of the evaluation. Finally the Winkleby 1993 study had possible contamination due to one control city banning public smoking in 1990 which subsequently produced a large decline in smoking. One‐third of survey respondents for this study did not live in the treatment cities during the entire intervention period. Although authors adjusted for this in their analysis the results did not change. Six studies were adequately protected against contamination (Perry 1994; Vartiainen 1998; Biglan 2000; Hancock 2001; Perry 2003; Winkleby 2004), whilst the remaining 12 studies had unclear protection against contamination.
Selective recruitment of participants:
Selective recruitment of participants were unclear in 18 studies and a high risk of bias in the remaining seven (Pentz 1989; St Pierre 1992; Piper 2000; De Vries 2003; Winkleby 2004; Hawkins 2009; Klein 2009). Possible selective recruitment occurred through subjects volunteering to take part in the evaluation, subjects selected by school teachers or by study staff.
Other risks of bias:
Two studies were identified as having other possible threats to validity. In Piper 2000, authors found significant differences between the different proposed methods of analysis used for the same data. As such they presented the results with 'the least amount of bias in the estimates of the standard errors due to the design effect'. The other study, D'Onofrio 2002, had a significant gap between study completion and publication of results (12 years). In addition authors state that different interventions were delivered to each intervention group and the full intervention as it was intended was not delivered, with an average delivery of 67%. The Baxter 1997 and Elder 2000 studies provided insufficient information to permit judgement of 'yes or no', while the remaining 21 studies had no other sources of bias identified.
Effects of interventions
See: Table 1
Intervention effectiveness was assessed in all 25 included studies through smoking prevalence, in addition to a mixture of secondary outcomes including behaviours, attitudes, perceptions and knowledge. The data was analysed as per the pre‐defined methods described in 'Subgroup analysis and investigation of heterogeneity'. For a summary of intervention effectiveness for each of these outcomes see Table 2.
1. Summary of intervention effectiveness.
| Study ID/ n‐values | Outcome Results (comparing intervention to control): | ||||
| Smoking | Behavioural intention* | Attitudes | Perceptions | Knowledge | |
|
Baxter 1997 Clusters n=4 (high‐schools) plus unknown number of primary‐schools (n=13 for intervention group only) Individuals n=1503 (mean from cross‐section x2 time points) 36‐months (SI) |
Not significant | ‐ | ‐ | ‐ | ‐ |
|
Biglan 2000 Clusters n=16 (communities) Individuals n=4450 (mean from cross‐section x5 time points including baseline) 12‐months (SI) |
Favours intervention | Favours intervention | Favours intervention | Favours intervention | ‐ |
| 24‐months (SI) | Not significant | Favours intervention | Favours intervention | Not significant | ‐ |
| 36‐months (SI) | Not significant | Favours intervention | Favours intervention | Not significant | ‐ |
| 48‐months (SI) | Favours intervention | Favours intervention | Favours intervention | Favours intervention | ‐ |
|
D'Onofrio 2002 Clusters n=78 (community clubs) Individuals n=1590 (mean from cross‐section x3 time points) 9‐months (SI) |
Not significant | Favours intervention | Not significant | Favours intervention | Favours intervention |
| 24‐months (SI) | Not significant | Not significant | Not significant | Not significant | Not significant |
|
De Vries 2003 Clusters n=235 (schools) Individuals n=23531 (Also see Table 4 and footnote) 12‐months |
Overall not significant; Favours intervention 2/6 countries; Favours control 2/6 countries | Overall not significant; Favours control 2/6 countries | Overall not significant; Favours intervention 1/6 countries | ‐ | ‐ |
| 24‐months (SI) | Overall not significant; Favours intervention 2/6 countries | Overall not significant; Favours intervention 1/6 countries; Favours control 1/6 countries | Overall favours intervention; Favours intervention 3/6 countries | ‐ | ‐ |
| 30‐months (SI) | Overall favours intervention; Favours intervention 2/6 countries | Overall not significant; Favours intervention 2/6 countries | Overall not significant; Favours intervention 2/6 countries | ‐ | ‐ |
|
Elder 2000 Clusters n=25 (schools) n=17 (school districts) Individuals n=660 2‐months (SI) |
Not significant | ‐ | Not significant | ‐ | ‐ |
| 12‐months (SI) | Not significant (GEE); Favours intervention (time x treatment of 'susceptible' cohort) | ‐ | Not significant (GEE); Favours intervention (time x treatment for tobacco‐anticipated outcomes) | ‐ | ‐ |
| 24‐months (SI) | Not significant (GEE); Favours intervention (time x treatment of 'susceptible' cohort) | ‐ | Not significant (GEE); Favours intervention (time x treatment for tobacco‐anticipated outcomes) | ‐ | ‐ |
|
Gordon 1997 Clusters n=8 (schools) Individuals n=1569 6‐months (SI) |
Not significant | Favours intervention | Favours intervention | ‐ | Not significant |
|
Gordon 2008 Clusters n=40 (schools) Individuals n=6276 12‐months (SI) |
Overall and Cohort‐1: Not significant Cohort‐2: Favours intervention | Cohort‐1: Not significant ( ANCOVA); Cohort‐1&2: Favours intervention (time x treatment) | Not significant | ‐ | ‐ |
|
Hancock 2001 Clusters n=20 (towns) Individuals n=3973 36/48‐months (SI) |
Favours control | ‐ | ‐ | ‐ | ‐ |
|
Hawkins 2009 Clusters n=28 (school districts) n=88 (schools) Individuals n=4407 36‐months (SI) |
Favours intervention | ‐ | ‐ | ‐ | ‐ |
|
Klein 2009 Clusters n=9 (cities) n=60 (GPU's) (both intervention only) Individuals n=4230 24‐months (EI) |
Not significant | Not significant | ‐ | Not significant | ‐ |
|
Murray 1994 Clusters n=81 (schools) Individuals n=7180 36‐months (SI) |
Not significant | ‐ | ‐ | ‐ | ‐ |
|
Pentz 1989 Clusters n=42 (schools) Individuals n=1607 (matched cohort) n=5065 (total) 12‐months (EI) |
Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 24‐months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
|
Perry 1994 Clusters n=2 (communities) n=20 (schools) Individuals n=2401 12‐months (SI) |
Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 24‐months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 36‐months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 48‐months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 60‐months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 72‐months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
|
Perry 2003 Clusters n=24 (schools) Individuals n=6237 24‐months (SI) |
D.A.R.E. Not significant; D.A.R.E. Plus: Favours intervention for boys only, overall not significant (Combined D.A.R.E. and D.A.R.E. Plus in meta‐analyses favour intervention) |
D.A.R.E. Not significant; D.A.R.E. Plus Favours intervention for boys only, overall not significant (Combined D.A.R.E. and D.A.R.E. Plus in meta‐analyses favour intervention) |
‐ | ‐ | ‐ |
|
Perry 2008 Clusters n=32 (schools) Individuals n=8369 12 months (SI) |
Not significant | Favours intervention | Favours intervention | Favours control | Favours intervention |
| 24 months (SI) | Favours intervention | Favours intervention | Favours intervention | Favours control (see Table 3) | Favours intervention |
|
Piper 2000 Clusters n=21 (middle‐schools) Individuals n=1981 (matched cohort) n=1677 (year ten only) 24 months (SI) |
Not significant | ‐ | ‐ | Age appropriate HFL: Not significant; Intensive HFL: Favours intervention |
‐ |
| 36 months (SI) | Age appropriate HFL: Favours control; Intensive HFL: Not significant |
‐ | ‐ | Age appropriate HFL: Not significant; Intensive HFL: Favours intervention |
‐ |
|
Schinke 2000 Clusters n=10 (reservations) n=27 (schools) Individuals n=1396 6‐months (SI) |
Not significant | ‐ | ‐ | ‐ | ‐ |
| 18‐months (SI) | Not significant | ‐ | ‐ | ‐ | ‐ |
| 30‐months (SI) | Not significant for weekly smoking; Favours Skills only for smokeless tobacco use |
‐ | ‐ | ‐ | ‐ |
| 42‐months (SI) | Not significant for weekly smoking; Favours Skills only for smokeless tobacco use |
‐ | ‐ | ‐ | ‐ |
|
Schofield 2003 Clusters n=24 (schools) Individuals n=4841 24 months (SI) |
Not significant | ‐ | Not significant | ‐ | Favours intervention |
|
St Pierre 1992 Clusters n=14 (clubs) Individuals n=377 3 months (SI) |
Not significant | ‐ | ‐ | ‐ | Favours intervention |
| 15 months (SI) | Not significant | ‐ | ‐ | ‐ | Favours intervention |
| 27 months (SI) | Not significant; However on post‐hoc tests SMART Only and SMART + Boosers Favoured the intervention | ‐ | ‐ | ‐ | Favours intervention |
|
Stevens 2002 Clusters n=12 (paediatric practices) Individuals n=3145 12‐months (SI) |
Not significant | ‐ | ‐ | ‐ | ‐ |
| 24‐months (SI) | Not significant | ‐ | ‐ | ‐ | ‐ |
| 36‐months (SI) | Not significant | ‐ | ‐ | ‐ | ‐ |
|
Sussman 1998 Clusters n=21 (schools) Individuals n=1578 12 months (SI) |
Not significant | ‐ | ‐ | ‐ | ‐ |
| 24/36 months (SI) | Not significant | ‐ | ‐ | ‐ | ‐ |
| 48/60 months (SI) | Not significant | ‐ | ‐ | ‐ | ‐ |
|
Tang 1997 Clusters n=27 (schools) Individuals n=4567 12 months (SI) |
Not significant | ‐ | Favours control (on data adjusted for baseline cofounders) | Not significant | Not significant |
|
Vartiainen 1998 Clusters n=6 (schools) Individuals n=897 24 months (SI) |
Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 36 months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 48 months (SI) | Favours intervention | ‐ | ‐ | ‐ | ‐ |
| 96 months (SI) | Favours intervention; Except for monthly smoking which was not significant | ‐ | ‐ | ‐ | ‐ |
| 180 months (SI) | Not significant; However favours intervention for cohort of baseline non‐smokers | ‐ | ‐ | ‐ | ‐ |
|
Winkleby 1993 Clusters n=4 (cities) Individuals n=2605 (cross‐sectional sample of 4 cities) 12 months (from the start of the adolescent intervention) |
Not significant | ‐ | ‐ | ‐ | ‐ |
| 24 months (from the start of the adolescent intervention) | Not significant | ‐ | ‐ | ‐ | ‐ |
|
Winkleby 2004 Clusters n=10 (continuation high‐schools) Individuals n=813 2.5 months (SI) |
Favours intervention (daily smoking only); Not significant for weekly or non‐smokers | ‐ | ‐ | ‐ | ‐ |
| 6 months (EI) | Favours intervention (daily smoking only); Not significant for weekly or non‐smokers | ‐ | ‐ | ‐ | ‐ |
* Behavioural intention = intentions to smoke in the future
SI: Follow‐up commences from the start of the intervention period
EI: Follow‐up commences from the end of the intervention period
DeVries 2003: Baseline smokers excluded from analysis; Weekly smoking at 12‐months follow‐up varied: two of the six countries showed a significant difference favouring the intervention whilst authors describe Denmark and UK as producing counter productive trends; See also Table 3, Table 4 and Effects of interventions.
Overall summary of smoking behaviour:
Overall ten interventions presented in the 25 studies demonstrated intervention effectiveness in influencing smoking behaviour including prevention, at primary follow up. One programme provided statistically and clinically significant short‐term benefits (<12 months) (Winkleby 2004) and nine provided longer‐lasting effectiveness (Pentz 1989; St Pierre 1992 (only in post hoc testing); Perry 1994; Vartiainen 1998 (up until eight‐year follow up); Biglan 2000 (for 12‐ and 48‐month follow ups only); De Vries 2003 (at 30 months only); Perry 2003 (for boys only in the D.A.R.E. Plus intervention; and when combining both D.A.R.E. and D.A.R.E. Plus groups together and comparing to control for the meta‐analysis); Perry 2008; Hawkins 2009). Two interventions favoured the control group (Piper 2000; Hancock 2001), whilst the remaining 13 studies demonstrated no significant benefit.
Narrative synthesis has been used to report primary outcomes, secondary outcomes and process measures for all studies (Table 3). A combination of 16 studies were able to be included in the meta‐analyses, with eight studies being the largest number of studies available for one outcome. However these results should be interpreted with caution as outcomes are only reported for studies in which data were available for meta‐analyses. Of the studies categorised as showing evidence of clinically and statistically significant benefit, only two (Vartiainen 1998, Perry 2008) reported outcomes that could be included in the meta‐analysis. Smoking was assessed as daily (Analysis 1.1), weekly (Analysis 1.2), monthly (Analysis 1.3), ever smoked (Analysis 1.4) and smokeless tobacco use (Analysis 1.5). Sub‐group analyses were conducted based on intervention duration < 12 months and > 13 months. There were no statistically or clinically significant results for weekly, monthly or smokeless tobacco use. For daily smoking and 'ever smoked' the point estimates were consistent with a clinical benefit but the number of studies were small and the confidence intervals wide (daily smoking Analysis 1.1, two studies, OR 0.89 (95% CI 0.69 to 1.15)), (ever smoked Analysis 1.4, three studies, OR 0.82 (95% CI 0.39 to 1.74)).
2. Summary of individual study outcomes and process measures.
| Study ID/sub‐headings: | Detailed synthesis of intervention effectiveness: |
|
Baxter 1997 Smoking behaviour: |
Cohort analysis: Smoking increased in both intervention and control areas by 20% overall; in the intervention schools the number of girls smoking increased by 29% and the number of boys by 10%, and in the control school the numbers of girls smoking increased by 24% and the number of boys by 16%. Cross‐sectional analysis: There was no evidence of any difference between intervention and control schools in the change in smoking rates between 1991 and 1994 (Chi‐square =2.6; p=0.12). |
|
Baxter 1997 Intermediate outcome data: |
None reported. |
|
Baxter 1997 Process measures: |
None reported. |
|
Baxter 1997 Comments: |
NHS costs (schools component only) estimated to be £16,350. |
|
Biglan 2000 Smoking behaviour: |
Prevalence of cigarette smoking in prior month: Using a random coefficients analysis for nested cross sectional design, the effect of the interventions were not significant. Using pair‐wise analysis of the effect from time‐1 to each of the follow‐up points, the effects of the interventions were significant at times‐2 (p=0.022) and ‐5 (p=0.038) and approached significance at time‐4 (p=0.077, 2 tailed test). The effect was calculated as the difference in the change in prevalence from time‐1 to the relevant time for the control condition, minus the same change for the school‐based‐only condition. At time‐2 the net change was 4.5% (i.e., a larger decrease in community‐participation areas), at time‐4 it was 2.4%, and at time‐5, 3.8%. Prevalence of smoking in school‐based‐only communities increased significantly from time‐1 to each of the subsequent time points. There was no significant change in the community‐participation condition, suggesting that the intervention prevented an increase in prevalence. There was no evidence that the community‐participation and school‐based‐only communities differed on expired carbon monoxide at any time points. |
|
Biglan 2000 Intermediate outcome data: |
Young people in the community‐participation group reported more negative attitudes toward tobacco use (slope t(14 df)=2.31, p=0.036). Their awareness of efforts to prevent illegal sales became significantly more positive (slope t(14 df)=‐2.31, p=0.036), Intentions to smoke over 5‐years were significantly more positive for grade 9 males in school‐based‐only communities (slope t(14 df)=2.87, p=0.0124). At time‐2 parents in community‐participation communities perceived more town support for tobacco access restrictions (8 communities). By time‐3 and ‐4, parents in the community‐participation group were aware of more efforts to reduce youth access, and perceived greater town support for access restrictions. There were significant intervention effects over time on the perception of town support for tobacco prevention, and the support of business leaders. There was no evidence of an impact on perceived support from schools or government officials. |
|
Biglan 2000 Process measures: |
After the first year of intervention, the total amount of activities over the year were correlated with the amount of change in the prevalence of any tobacco use (including smokeless tobacco), r=‐0.61, p<0.10. The correlation was not significant for time‐1 to time‐3. However, the correlation between the cumulative number of activities over the 3‐years of the intervention in each community and the community’s change in the prevalence of any tobacco use between time‐1 and time‐4 was significant, r=‐0.75, p<0.05. This correlation was apparently due to the correlation of cumulative activities with changes in smoking prevalence between time‐1 and time‐4, r=‐0.73, p<0.05 (data from an unpublished draft report). |
|
Biglan 2000 Comments: |
Time‐1 smoking prevalence was higher in community‐participation groups (approximately 10%, adjusted for covariates) than in school‐based‐only groups (approximately 8%). This difference approached but did not reach significance. From time‐1 to time‐2 there was a marked drop in smoking prevalence in community‐participation groups and increase in the school‐based only communities. An analysis of the slope for prevalence (excluding the time‐2 data) showed that the slopes did differ significantly (t(14)=‐2.79, p=0.014), even when excluding the data points offering the strongest evidence for an effect. Communities had small populations and were mainly in rural areas. Only two communities had significant numbers of students from minority ethnic groups. Parents were offered a $10 incentive to complete the questionnaire. |
|
D’Onofrio 2002 Smoking behaviour: |
None of the smoking behaviour programme effect estimates were significant at post‐test 1 or post‐test 2. |
|
D’Onofrio 2002 Intermediate outcome data: |
At post‐test 1 (9‐months) programme effect coefficients (EC) with 95% confidence intervals are used to show that youth in the programme clubs had: greater knowledge of the actual prevalence of tobacco use among high‐school students (EC+0.058; +0.021, +0.095); were more likely to report that smokeless tobacco is addictive (EC+0.168; +0.062, +0.274); the first use of cigarette is harmful to one’s body (EC+0.166; +0.019, +0.313); quitting cigarettes is difficult (EC+0.154; +0.005, +0.337); tobacco companies try to sell their products to children (EC+0.194; +0.051, +0.337); and they did not intend to smoke cigarettes in the future (EC+0.084; +0.023, +0.145); By post‐test 2 (24‐months) there were no significant results for any outcome. |
|
D’Onofrio 2002 Process measures: |
Fidelity of programme implementation varied by club from 43.0% to 85.3% with an average fidelity of 67.3% (SD=9.7). programme leaders added their own anecdotes to the curriculum approximately twice per session. The 'going further' activities were reported as being completed by 5.3% of members. |
|
D’Onofrio 2002 Comments: |
None to report. |
|
De Vries 2003 Smoking behaviour: |
For time‐1/time‐2 (12‐months) no overall effects for smoking behaviour were found using logistic regression. With regards to weekly smoking at time‐3 (24‐months), 18.4% of non‐smokers in the experimental group had begun smoking on a weekly basis compared to 18.8% in the control group. A significant overall effect for weekly smoking was found at time‐4 (30‐months) with 21.9% commencing smoking in the experimental group compared to 23.4% in the control (p=0.03). (Also see Table 4). |
|
De Vries 2003 Intermediate outcome data: |
Intentions to smoke overall were not significant at any follow‐up, though individual countries demonstrated varying results (some in favour of intervention, some control) across the three time‐periods (see Table 4). In one country (Spain), subjects were significantly less convinced of the advantages of smoking at 12‐months compared to the control, however this effect was not seen in any other country as all the respondents perceived many disadvantages and believed that smoking had detrimental effects. As such there was no overall significant differences between intervention and control, which was also the case at 30‐months follow‐up. The experimental group at time‐3 (24‐months) however, were significantly less convinced of the pros of smoking than the controls (p<0.05). By time‐4 the experimental group were more confident in cigarette refusal (self‐efficacy) than the control. |
|
De Vries 2003 Process measures: |
Intervention implementation varied significantly between countries with total number of lessons being Denmark 12, Finland 14, The Netherlands 9, Spain 18, Portugal 14 and United Kingdom 9. The activities within the ESFA projects also varied though each contained some components at the school level, parental level and out‐of‐school level. |
|
De Vries 2003 Comments: |
Random assignment was not possible in the Netherlands and Spain. |
|
Elder 2000 Smoking behaviour: |
No between‐group results were significant. 30‐day smoking started and remained at very low levels throughout the 2‐years; The highest group prevalence at any measurement period was 4.7% with 2.5% being the lowest. Smoking prevalence in those susceptible (susceptibility defined as a combination of outcomes designed by the authors) to smoking reduced by nearly 40% in the attention‐control group and by 50% in the intervention group from baseline to 2‐year follow‐up. The overall reduction in subjects 'susceptible to smoking' from immediate post‐intervention to 2‐years was statistically significant (definition of susceptible subjects included those who were current smokers, did not show a firm resolve not to smoke, would accept a cigarette from a friend or intended to smoke in the next year). Older children were more likely to smoke and boys were significantly more susceptible than girls to smoking. |
|
Elder 2000 Intermediate outcome data: |
Tobacco peer norms, tobacco self‐standards and communication with parents all had no significant interactions and no significant intervention effects when the interaction terms were dropped (GEE results). Tobacco‐anticipated outcomes for the time‐by‐treatment analysis was statistically significant. Authors state this interaction was due to the discrepancy in the difference between control and intervention at time‐2 (‐0.05) compared to differences seen at time‐3 (0.19) and time‐4 (0.14). |
|
Elder 2000 Process measures: |
A significant dose‐response relationship with respect to susceptibility to smoking was seen as dose increased in the intervention group, which was not seen in the attention control group (p=0.036). |
|
Elder 2000 Comments: |
None to report. |
|
Gordon 1997 Smoking behaviour: |
At 6‐months there were no significant differences in smoking prevalence between the control group and the intervention group. After the intervention period the number of non‐smokers reduced by 13%, ever smokers increased by 5% and weekly smokers increased by 3%, however these results were not significant between groups. |
|
Gordon 1997 Intermediate outcome data: |
Number of students who did not intend to smoke fell by 8% (from 62% to 54%) in the intervention group and by 17% (from 69% to 52%) in control group (p=0.01). There were marginal increases in knowledge in both groups and significant influences on attitudes (overall attitudes toward smoking). Purchasing cigarettes from retailers was more difficult, 12‐ out of 17‐students were refused in the intervention group compared to 5‐ out of 13‐students in the control group. |
|
Gordon 1997 Process measures: |
Various anti‐smoking activities in the community were encouraged such as: community police officers reminding retailers of their obligations regarding the sale of cigarettes to minors and posters and leaflets displayed in general practitioner practices. |
|
Gordon 1997 Comments: |
In the control group compared to the intervention group at baseline there were more non‐smokers (70% vs 63%), fewer occasional smokers (17% vs 21%), and less regular smokers (0% vs 2%). It is unclear whether the pupils in the control schools might have been contaminated by community initiatives in the catchment areas of the intervention schools |
|
Gordon 2008 Smoking behaviour: |
No intervention effect was found for smoking prevalence for either cohort using the mixed‐model ANCOVA, p=0.4010 or the time‐by‐condition analysis (p=0.5716). A statistically significant effect was found for cohort‐2 (ANCOVA ‐0.042, t=‐2.59, df=18, p=0.0187), representing a 4.2% reduction in smoking prevalence in intervention schools after controlling for pre‐test smoking. Cohort‐2 exhibited an 11.2% increase in smoking prevalence in control schools and a 7.1% increase in intervention schools. There was no intervention effect on smokeless tobacco use (assessed for males only) across both cohorts (p=0.9349) or in cohort‐2 (p=0.9058). |
|
Gordon 2008 Intermediate outcome data: |
No intervention effect was found for susceptibility using a mixed model ANCOVA (p=0.1147), however the time‐by‐treatment analysis indicated a marginal reduction (‐0.072, t=2.12, df=37, p=0.041). Cohort‐2 schools however significantly differed by condition for susceptibility according to both the mixed‐model ANCOVA (‐0.08, t=‐2.45, df=18, p=0.0245, partial r=‐0.50) and the time‐by‐treatment analysis (‐0.098, t=‐2.92, df=17, p=0.0096, partial r=‐0.58). The interaction between condition and cohort was not significant (ANCOVA p=0.077 time‐by‐treatment p=0.1331). The intervention had no significant effect on smoker image (i.e., the condition did not affect student’s images of smokers), though in cohort‐2, sixth grade smoker image was significantly associated with eighth grade 30‐day smoking (0.04, t=2.93, df=1,479, p=0.0034, r=0.08) Sixth grade reports on house smoking rules were significantly related to eighth grade 30‐day cigarette use across cohorts, even after controlling for baseline smoking (‐0.019, t=‐4.87, df=3,406, p<0.0001, r=‐0.08). There was no evidence that intervention effects were mediated by effects on house rules for the combined sample or cohort‐2. |
|
Gordon 2008 Process measures: |
None reported. |
|
Gordon 2008 Comments: |
Analysis conducted on 60% Intervention and 59% Control. |
|
Hancock 2001 Smoking behaviour: |
Smoking prevalence (4‐week) increased over time in all towns, and intervention towns showed a greater increase (outcome significantly favoured control). Girls showed the greatest net difference, 5%, but this was not significant (p=0.2). |
|
Hancock 2001 Intermediate outcome data: |
None reported. |
|
Hancock 2001 Process measures: |
At time‐2 only 2588 students answered questions about anti‐smoking activities. In the past 2‐years 74.6% of intervention and 70.8% of control groups were aware of anti‐smoking activities (difference not significant, p=0.5). Of students aware of campaigns, 30.1% had smoked in the past month, of those not aware 28.6% had smoked, (relationship not significant, p=0.5). |
|
Hancock 2001 Comments: |
Sample size was reduced at time‐2, with fewer boys included. About 10% of surveys contained some nonsensical responses and were not included. The lack of difference in awareness of anti‐smoking actions may indicate that many similar activities were occurring in control towns and schools. A survey of school principals supported this for school activities. |
|
Hawkins 2009 Smoking behaviour: |
A mixed‐model analysis of covariance for smokeless tobacco use in the last 30‐days showed significantly higher prevalence rates in the eighth grade for control communities, compared to intervention communities (t8=3.23, p=0.01 [2‐tailed], adjusted odds ratio =1.79). Eighth grade student smoking prevalence (30‐day use) did not differ significantly across groups (t8=1.47). |
|
Hawkins 2009 Intermediate outcome data: |
None reported. |
|
Hawkins 2009 Process measures: |
Over the 2‐years adherence improved for most programmes with rates averaging 91% in 2004‐2005 and 94% in 2005‐2006. Only one programme decreased in adherence over the 2‐years from 93% to 54% (programme Development Education). The highest dosage scores were in the parent training and after school programmes with all programmes averaging at least a 4.0 on a 5 point quality delivery score. Average delivery scores in 2004‐2005 were 4.38 and in 2005‐2006 they were 4.59. |
|
Hawkins 2009 Comments: |
None to report. |
|
Klein 2009 Smoking behaviour: |
The intervention had no significant effect on monthly or weekly smoking compared to control. Smoking prevalence rates across both cohorts increased from 12% at baseline to 29% at 5‐year follow‐up for monthly smoking and 8% at baseline to 22% at 5‐year follow‐up for weekly smoking. |
|
Klein 2009 Intermediate outcome data: |
Parental smoking and close friend smoking increased the odds of past month smoking by 40% and nearly 100% respectively). Rules on smoking at home were significantly associated with a 12% reduction in the odds of past month smoking. Friend smoking status rendered a more powerful influence on smoking behaviour than the intervention (clean‐indoor‐air) policy with youth. Youth with close friends who smoked were more likely themselves to smoke compared to youth with no close friends that smoked. |
|
Klein 2009 Process measures: |
The number of participants living in an area with a clean‐indoor‐air policy were 1028. No other information provided. |
|
Klein 2009 Comments: |
None to report. |
|
Murray 1994 Smoking behaviour: |
Authors report no significant differences in tobacco use incidence or prevalence rates at 36‐months follow‐up, nor was there any evidence of a dose‐response relationship in the four‐group comparison study data set. There was a marginal (p=0.05) difference in favour of control when the three intervention groups were combined as one, when meta‐analysing data for this review (odds ratio 1.23 (95% CI 1.00 to 1.51). |
|
Murray 1994 Intermediate outcome data: |
Pro‐smoking messages were stable; anti‐smoking messages more frequently reported by Minnesota youth in 4 of 5 media types tested. Frequently expressed strong anti‐tobacco beliefs were stable over time. Increases in exposure to anti‐smoking messages had little effect on smoking related beliefs. |
|
Murray 1994 Process measures: |
In 1989 and 1990, 95% of participants saw or heard at least one advertisement; On average advertisements were seen or heard 50‐times per year, per person. |
|
Murray 1994 Comments: |
Minnesota students had significantly fewer peers, family or friends who smoked, which did not change over the 5‐years. |
|
Pentz 1989 Smoking behaviour: |
Smoking rates increased in both groups over time, however the intervention reported a smaller rate of increase (last month smoking) compared to the control with 15% and 22% respectively (p<0.05), at 1‐year follow‐up. Change scores in the proportion of monthly smokers were (as % (95% CI)): Intervention 3.4 (0.2 to 6.6), Control 13.1 (7.5 to 18.8). Change scores in the proportion of weekly smokers were (as % (95% CI)): Intervention 4.3 (1.7 to 6.9), Control 10.5 (5.6 to 15.5). Schools with a high level of programme implementation had a decrease (from baseline) in cigarette use within the last month (1.23%), compared to an increase (6.72%) in schools with low implementation and an increase (10.95%) within control schools (p<0.05 for difference between high implementation and control). Preliminary analyses at 2‐year follow‐up (longitudinal panel) suggested that effects were maintained (no further information provided). |
|
Pentz 1989 Intermediate outcome data: |
None reported. |
|
Pentz 1989 Process measures: |
Intervention implementation training occurred in all television station managers (n=9), and many teachers (n=65) and student leaders (n=4 per class). Teachers report that 80% of students completed homework assignments. |
|
Pentz 1989 Comments: |
Student’s results were adjusted for grade, race, urbanicity and socio‐economic status. Cross‐sectional student’s results were adjusted for grade. Students were more likely to have used cigarettes in the last month if their mother, father, or older sibling smoked. |
|
Perry 1994 Smoking behaviour: |
For the matched cohort there were significant differences for smoking prevalence and intensity (taking into account adjustments for false negatives in the 9th grade) between communities at all follow‐up years. All p‐values were significant for prevalence at 12‐months to 72‐months (p=0.005, p=0.001, p=0.002, p=0.019, p=0.034, p=0.041) and for intensity (p=0.025, p=0.004, p=0.002, p=0.009, p=0.016, p=0.011). In 1989 (the end of high‐school), 14.6% of students were weekly smokers in the intervention community compared with 24.1% in the control community. There were no significant differential programme effects between the sexes. For the cross‐sectional sample there were significant differences between communities in all follow‐up years (1983‐1989). Saliva thiocyanate levels were significantly lower in the intervention community than in the control community in both the cohort sample (54 vs. 39 ug/mL, p=0.0002) and the cross‐sectional sample (56 vs. 41 ug/mL, p=0.0009). |
|
Perry 1994 Intermediate outcome data: |
None reported. |
|
Perry 1994 Process measures: |
None reported. |
|
Perry 1994 Comments: |
Financial constraints prevented analysis of non‐responding students, however by identifying and using previous years values for students not present, the magnitude of the intervention would have been increased in 4 of the 6 follow‐up evaluations by 0.5% to 2.3%, and would have declined in the other two by 0.2% to 0.35%. |
|
Perry 2003 Smoking behaviour: |
The D.A.R.E. project did not demonstrate any significant behavioural effects, however boys in the D.A.R.E. Plus schools were less likely than those in the control schools to show increases in past month tobacco use behaviour. When combining D.A.R.E and D.A.R.E Plus interventions together for analysis in this review, there is a borderline significant effect in favour of the intervention (OR 0.18 (95% CI 0.03 to 1.00) p=0.05) over that of the control. |
|
Perry 2003 Intermediate outcome data: |
Boys in the D.A.R.E. Plus schools were more likely to show reduced intentions to smoke than the control, and were more likely to show reduced intentions to smoke compared to D.A.R.E. only schools. When combining D.A.R.E and D.A.R.E Plus interventions together for analysis in this review, there is a borderline significant effect in favour of the intervention (OR 0.06 (95% CI 0.00 to 0.99), p=0.05) over that of the control. |
|
Perry 2003 Process measures: |
Among the first cohort of n=1033, only 11.9% or n=123 students reported receiving the D.A.R.E. programme. This rose to 51% (n=852) and 91.1% (n=1418) of students by the second and third cohorts respectively. |
|
Perry 2003 Comments: |
Tracking patterns from elementary to middle‐school showed significant mixing of D.A.R.E. exposed and non‐D.A.R.E. exposed students in the second cohort. |
|
Perry 2008 Smoking behaviour: |
At 1‐year follow‐up there were no significant differences between intervention and control in relation to tobacco use, which decreased in both conditions over time. However at the 2‐year follow‐up period significant between‐group differences were found for trajectories (rates of growth) for cigarette smoking (p<0.05), bidi smoking (p<0.01) and any tobacco use (p<0.04). There were no significant trajectories for chewing tobacco (p<0.1). Over the 2‐year study period tobacco use increased by 68% in the control group and decreased by 17% in the intervention group. |
|
Perry 2008 Intermediate outcome data: |
Significant differences were found at 1‐year follow‐up for intermediate outcomes which were maintained at 2‐year follow‐up for 'intention to smoke' with trajectories of (p<0.01) and ‘intentions to chew’ (p<0.03), in favour of the intervention. By 2‐years intentions to smoke increased by 5% in the control whilst it actually decreased by 11% in the intervention group. Intentions to chew decreased by 12% in the control and 28% in the intervention group. Between group differences were also found in favour of the intervention with respect to knowledge of the health effects of tobacco use, reasons to use and not use tobacco, rules on smoking socially (negative social consequences), normative beliefs regarding tobacco use, advocacy skills (self‐efficacy), knowledge of tobacco‐control policies and social susceptibility to chewing tobacco use (p<0.05 for all) by 2‐year follow‐up. However the trajectories of student’s perceptions were favouring the control for perceived prevalence of chewing tobacco use and perceived prevalence of smoking (p<0.05). At 1‐year follow‐up significant results in favour of the intervention were found for: knowledge of health effects of tobacco (p<0.01), social consequences toward tobacco use (p=0.04), reasons to use tobacco (p<0.01), reasons not to use tobacco (p=0.03), social susceptibility to chewing tobacco (p=0.04), social susceptibility to smoking (p=0.03), perceived fewer peer and adult smoking (p<0.01), perceived chewing tobacco (p<0.01), tobacco not acceptable (p<0.01), tobacco advocacy (p=0.03), knowledge about tobacco control policies (p<0.01) and support of policies (p=0.04). No significant differences were found for changes in refusal skills (self‐efficacy) (p=0.06) or normative expectations (p=0.25). |
|
Perry 2008 Process measures: |
The first year of MYTRI implementation was completed with 65 sixth grade and 60 eighth grade classrooms. Thirteen of 16 intervention schools were completed with all of the planned activities, 3 schools partially implemented classroom activities. Inter‐school activities were implemented with 67% of the sixth and eighth grade cohort attending the 2 out‐of‐school events (n=3569 in total). |
|
Perry 2008 Comments: |
There are generalisability concerns as significantly more tobacco users dropped‐out of the study than non‐tobacco users. |
|
Piper 2000 Smoking behaviour: |
Past month cigarette use at each grade for the Intensive HFL (Healthy‐For‐Life) group vs. control were: 6th grade 5% (pretest) /9th grade 22%/ 10th grade 28%; Age Appropriate HFL v control: 6th grade 4%/ 9th grade 24%/ 10th grade 36%; Control alone: 6th grade 5%/ 9th grade 24%/ 10th grade 30%. Time by treatment analysis showed no significant effect for the Intensive HFL, however the Age Appropriate HFL at 10th grade significantly favoured the control (p<0.01). Monthly smoking rates in the intensive condition (using hierarchical linear modelling) significantly reduced the likelihood of smoking compared to control (coefficient ‐0.38, SE 0.15, p<0.05) and in the age appropriate condition the likelihood of smoking was increased compared to control though not significantly (coefficient 0.41, SE 0.20, p=0.1). |
|
Piper 2000 Intermediate outcome data: |
Perception of Peer ATOD (Alcohol, Tobacco and Other Drug) use scale for Intensive HFL were: 6th grade 6.5 (2.3)/ 9th grade 9.5 (2.7) (p<0.001)/ 10th grade 11.3 (2.7) Age Appropriate HFL: 6th grade 6.4 (1.9)/ 9th grade 10.2 (2.7)/ 10th grade 11.6 (2.8) Control: 6th grade 6.3 (2.1)/ 9th grade 10.3 (3.0)/ 10th grade 11.6 (2.9) OLS regression results for scale of perception of peer ATOD use: standard regression (beta) coefficients and significance at 9th and 10th grades: Baseline risk from previous cohort 9th grade .20 (p<0.001)/ 10th grade .16 (p<0.001) time‐1 behavioural indicator 9th grade .21 (p<0.001)/ 10th grade .15 (p<0.001) Age appropriate treatment condition 9th grade ‐.01/ 10th grade .03 Intensive treatment condition 9th grade ‐.19 (p<0.001)/ 10th grade ‐.10 (p<0.01). |
|
Piper 2000 Process measures: |
None reported. |
|
Piper 2000 Comments: |
Tenth grade survey under‐represented students from the Intensive condition (61% vs 68% overall, p<0.001) for administrative scheduling reasons. |
|
Schinke 2000 Smoking behaviour: |
There were no significant differences in weekly smoking rates between the intervention and control groups at any follow‐up, though all rates more than trebled to 35‐40% over 3.5‐years. Rates of cigarette use were higher for females than males. At 30‐ and 42‐month follow‐up smokeless tobacco use was lower for subjects in the skills only arm compared to subjects in both the control and skills + community arms of the study. Only the skills + community intervention arm was used for the meta‐analysis compared to control in this review. |
|
Schinke 2000 Intermediate outcome data: |
None reported. |
|
Schinke 2000 Process measures: |
Field observations showed a close correspondence between implementation of skills and community intervention and written protocols (no further details given). |
|
Schinke 2000 Comments: |
The skills + community intervention tended to lie between the skills only and the control group on all substance use measures. All significant differences for outcomes other than smoking were between skills only and the control, with the exception of smokeless tobacco use at 30‐ and 42‐months. |
|
Schofield 2003 Smoking behaviour: |
The HPS (Health Promoting Schools) intervention had no significant effect on smoking behaviour over the 2‐year study period with an increase in smoking prevalence of 10% for both the intervention and control groups. Although weekly smoking was 20.5% and 17.5% for the control and intervention groups respectively at follow‐up, baseline imbalances meant that actual differences in the proportion of smokers from baseline to follow‐up were 10% and 9.7% for the control and intervention groups respectively. |
|
Schofield 2003 Intermediate outcome data: |
The programme favoured the intervention for smoking knowledge with 64% of the intervention group scoring the maximum knowledge compared with 60% in the control group, which represents an increase of 12% for the intervention group compared with 7% in the control (p=0.001). This effect was not seen for the outcome smoking attitudes with no between group differences found. Positive attitudes to smoking did however decrease from pre‐ to post‐test among smokers, though not amongst non‐smokers (p=0.01). |
|
Schofield 2003 Process measures: |
None reported. |
|
Schofield 2003 Comments: |
A higher proportion of smokers were lost‐to‐follow‐up compared to non‐smokers which may affect generalisability. |
|
St Pierre 1992 Smoking behaviour: |
Overall the three groups did not differ on the cigarette behaviour scale. However post‐hoc analysis found that intervention groups A (Stay SMART Only ) and B (Stay SMART plus boosters) reported significantly less cigarette related behaviour than group C (control). Adjusted means for cigarette behaviour were: A 1.46, B 1.48, C 1.63 (p<0.05). Marginally fewer youths in group B (Stay SMART plus boosters) reported recent (in the last year) cigarette use at 27‐month post‐test compared with group A (Stay SMART only) and the control group (not significant). |
|
St Pierre 1992 Intermediate outcome data: |
For the overall drug knowledge scale, Stay SMART only and Stay SMART plus boosters groups demonstrated significantly more knowledge about drug use than the control group (p< 0.001, and p<0.05, respectively). The Stay SMART only group showed significantly more knowledge than the Stay SMART plus booster group (p<0.05) across 27‐months. |
|
St Pierre 1992 Process measures: |
None reported. |
|
St Pierre 1992 Comments: |
Funded by the Federal Office for Substance Abuse Prevention. |
|
Stevens 2002 Smoking behaviour: |
No significant differences were found for ever smoking or smokeless tobacco use for any of the follow‐up periods. Adjusted odds ratios (AOR) and 95% confidence intervals (95% CI) for ‘ever smoking’ were 1.05 (0.80, 1.39), p=0.71 at 12‐months, 1.04 (0.82, 1.31), p=0.76 at 24‐months and 0.97 (0.79, 1.20), p=0.78 at 36‐months. For ‘smokeless tobacco use’ the AOR and 95% CI’s were 1.00 (0.39, 2.57), p=0.99 at 12‐months, 1.11 (0.52, 2.38), p=0.79 at 24‐months and 1.42 (0.77, 2.62), p=0.26 at 36‐months. |
|
Stevens 2002 Intermediate outcome data: |
None reported. |
|
Stevens 2002 Process measures: |
Audits of participant charts indicated that 99% were labelled with the research project identification sticker, 95% of participants had been seen for subsequent visits by physicians, 51% in the alcohol/tobacco arm of the study had documentation of prevention messages by physician or other staff members in their notes and 47% had documented messages for the control group (safety messages). |
|
Stevens 2002 Comments: |
None to report. |
|
Sussman 1998 Smoking behaviour: |
At post‐test there were no significant effects on cigarette use in the past 30‐days: adjusted means for cigarette use (means adjusted for baseline use) A: 34.53/ B: 33.08/ C: 30.71. Overall condition effect F (2, 18) 0.16, p=0.85. |
|
Sussman 1998 Intermediate outcome data: |
None reported. |
|
Sussman 1998 Process measures: |
Activities and lessons were delivered as planned for A and B schools. Students attended approximately two thirds of the drug abuse prevention sessions with no decrease of attendance over time. In B schools (school‐as‐community group), weekly ASB meetings involved approximately 6% of the student body of each school, and the events involved an average of 20% of the student body of each school. All schools implemented at least 6 events. |
|
Sussman 1998 Comments: |
No statistically significant differences between participants measured pre‐ and post‐intervention and those measured at pre‐test only. No evidence that the 3 groups varied on any pre‐test measures. Baseline smoking rates not given. |
|
Tang 1997 Smoking behaviour: |
Smoking prevalence rates were not significantly lower in the Intervention group after adjustment for baseline differences (OR 0.81 (95% CI 0.41, 1.33)). |
|
Tang 1997 Intermediate outcome data: |
No significant changes in children’s knowledge, attitudes or perceptions. (Perceived peer smoking could not be meta‐analysed as data adjusted for baseline imbalances were not presented). |
|
Tang 1997 Process measures: |
Fifteen of the 17 teachers responding taught 5 lessons. There was a low response to the parental information evening, to the quit number and to the follow‐up questionnaire. Twenty four parents were active in campaigning to reduce supply. No retailer prosecutions occurred. |
|
Tang 1997 Comments: |
The parental involvement was relatively weak. A programme to reduce sales to minors was implemented in the area of some comparison schools towards the end of the project, and media coverage was generated. |
|
Vartiainen 1998 Smoking behaviour: |
Individual as unit of analysis: Immediately after intervention (1980) one third fewer students reported smoking once a month in both intervention groups than in control group; results 6‐months and 2‐years later were similar; at 8‐years, effect persisted only in teacher‐led programmes. At 15‐years, differences between intervention and control schools were not significant. For baseline non‐smokers followed up to 28‐years of age, significantly fewer students in the intervention than in the control schools took up smoking: health educator‐led vs teacher‐led vs control schools (30.8% vs 29.3 vs 41.2%) p=0.02. School as unit of analysis: The preventive effect in the intervention groups vs control groups remains significant in baseline non‐smokers. The prevalence of all smokers was 28%, 30%, 30%, and 32% in intervention, and 36% and 46% in control schools (mean prevalence of all smokers was 30% in intervention and 41% in control schools (F=11.7, p=0.02)). After 15‐years, cumulative exposure to tobacco was 22% lower in the intervention groups than in the control groups (p=0.01) if missing data points were replaced, 25% lower (p=0.01) if missing data points ignored, and 27% lower (p=0.05) if only data for those who participated in all surveys were used. |
|
Vartiainen 1998 Intermediate outcome data: |
None reported. |
|
Vartiainen 1998 Process measures: |
None reported. |
|
Vartiainen 1998 Comments: |
Fewer girls in the intervention school become regular smokers. Prevalence of smokers was highest at age 21 and declined slightly thereafter. Men tended to smoke more heavily than women. The average man in the intervention group had consumed 5,500 fewer cigarettes than his counterpart in the control group between the ages of 13‐ and 28‐years. |
|
Winkleby 1993 Smoking behaviour: |
There were no statistically significant differences in smoking prevalence trends among the cities over time, indicating no overall treatment effect. There was a significant decline in smoking between the 2nd and the 4th survey for all age groups, both sexes and all cities (p<0.001). Over the 12‐year period prevalence of daily smoking declined in all cities by approximately 50% among 16‐ to 19‐year‐olds and 20‐ to 24‐year‐olds but showed little change among 12‐ to 15‐year‐olds. During each period smoking prevalence escalated most sharply between the ages of 12‐ to 15‐years and 16‐ to 19‐years. |
|
Winkleby 1993 Intermediate outcome data: |
None reported. |
|
Winkleby 1993 Process measures: |
None reported. |
|
Winkleby 1993 Comments: |
There were demographic/characteristic differences between cities at baseline e.g. race, father’s education, smoking prevalence. In one control city 20‐ to 24‐year‐olds were significantly more likely to smoke than all other age groups at all other times in all cities (p<0.001). |
|
Winkleby 2004 Smoking behaviour: |
Regular smoking (daily) decreased significantly by 3.8% in the intervention schools compared to an increase of 1.5% in control schools by end‐of‐intervention (end of semester). This produced a net change of 5.3%. Significant differences were maintained between intervention and control schools with regular smoking rates for the intervention schools of 25.1%, 21.3% and 20.3% at baseline, post‐intervention and 6‐months follow‐up respectively, compared to control schools which were similar across all 3 time points. No significant differences were found for weekly smokers or non‐smokers at either follow‐up. |
|
Winkleby 2004 Intermediate outcome data: |
There were significant net changes between groups in favour of the control for the three social constructs of perceived incentive value for creating a tobacco‐free environment, perceived self‐efficacy to perform advocacy activities, and outcome expectancies that advocacy activities would result in changes within student environments. All three measures for social constructs remained unchanged for control schools. |
|
Winkleby 2004 Process measures: |
Mean exposure time for each student within the intervention schools were 20.0‐hours and 19.2‐hours for control students. Community advocacy activity involvement 5‐months post‐intervention increased from 0.9 to 4.0 activities per student for intervention subjects and remained unchanged at 1.0 activities for control subjects. |
|
Winkleby 2004 Comments: |
Students were volunteers from 10 continuation high‐schools therefore authors indicate possible concerns over generalisability. |
1.1. Analysis.
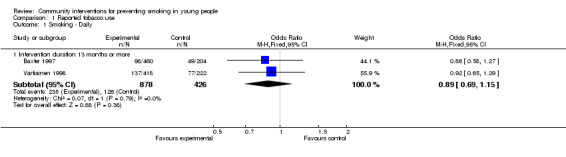
Comparison 1 Reported tobacco use, Outcome 1 Smoking ‐ Daily.
1.2. Analysis.
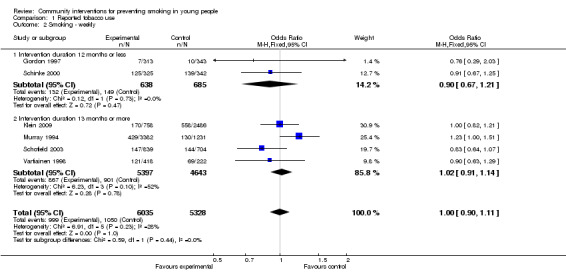
Comparison 1 Reported tobacco use, Outcome 2 Smoking ‐ weekly.
1.3. Analysis.
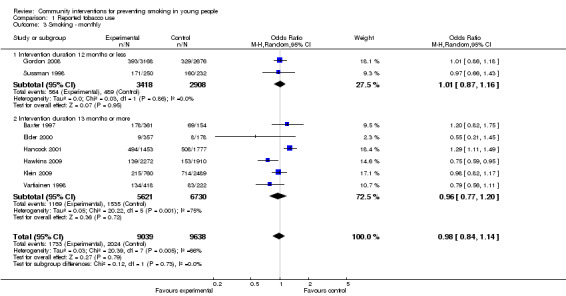
Comparison 1 Reported tobacco use, Outcome 3 Smoking ‐ monthly.
1.4. Analysis.
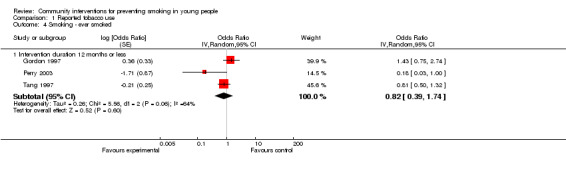
Comparison 1 Reported tobacco use, Outcome 4 Smoking ‐ ever smoked.
1.5. Analysis.
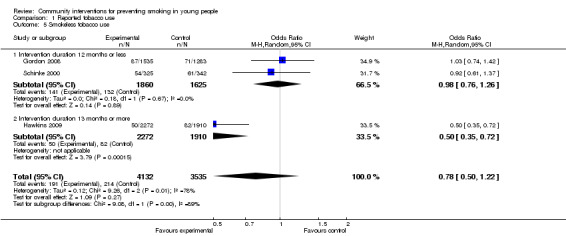
Comparison 1 Reported tobacco use, Outcome 5 Smokeless tobacco use.
An alternative subgroup analysis (Analysis 2) using length of follow up rather than duration of intervention, did not provide any evidence that this affected outcomes or explained heterogeneity. Studies could contribute to both short and long follow up groups, but there was not enough data to detect whether intervention effect might increase or decline over time.
The Pentz 1989 study reported reductions in the intervention community versus the control community, who received the media component only, whilst in post hoc analyses of the St Pierre 1992 study, both intervention groups reported significant reductions in cigarette use over that of the control group (p<0.05). Both Perry 1994 and Vartiainen 1998 programmes were initially designed as large‐scale, cardiovascular disease prevention programmes aimed at entire populations, and included a school‐based component specifically targeting young people. Although smoking outcomes in the Vartiainen 1998 study were not significant at 15‐year follow up, significant effects in favour of the intervention were seen for daily and weekly smoking up until 8‐year follow up (p=0.035 and p=0.022 respectively), and for monthly smoking up until 4‐year follow up (p=0.004). The Biglan 2000 study reported reductions in the community intervention group compared with a school based programme only. Perry 2003 compared two interventions to a control population with a statistically significant difference observed amongst boys in the 'D.A.R.E. Plus' intervention and a clinically significant difference for the combined gender population for the same intervention. For the De Vries 2003 study the results were diverse due to the large scale of the project (interventions delivered across six countries). Reductions in smoking onset were observed in two of the six countries as well as increased smoking observed in two of the six countries, being Denmark and the UK showing counterproductive trends at 12 months. At 24 months no overall significant effects were seen despite two countries significantly favouring the intervention. Whilst at 30 months an overall significant effect in favour of the interventions was seen (p=0.03) with two countries showing statistically and clinically significant benefits. De Vries 2003 was unable to be included in the meta‐analysis as authors excluded current smokers at baseline from all analyses, only following up those initiating smoking after baseline samples were collected. As such this study could not be compared to the other community trials included in this review which assessed the programme's influence on smoking behaviour in addition to prevention, rather than prevention alone. Due to the large scale of the evaluation, a separate table summarising each of the outcomes at each follow up period has been included (Table 4). In the Perry 2008 by two‐year follow up, overall tobacco use increased by 68% in the control group whilst a decrease of 17% was found in the intervention group. Significant between group differences in favour of the intervention were found for trajectories of cigarette smoking (p<0.05), bidi smoking (p<0.01) and any tobacco use (p<0.04) (Perry 2008). In both Winkleby 2004 and Hawkins 2009, community programme efforts were combined with a school based component to decrease smoking prevalence in the intervention group, whilst an increase was observed in the control population. In addition the Hawkins 2009 study demonstrated a significant reduction in smokeless tobacco use for the intervention population compared to the control.
3. Summary of intervention effectiveness for De Vries.
| Country: | Outcome Results for De Vries (comparing intervention to control): | ||
| Weekly Smoking | Behavioural intention* | Attitudes | |
|
Overall 12‐months |
Not significant | Not significant | Not significant |
| 24‐months | Not significant | Not significant | Favours intervention (p<0.05) |
| 30‐months | Favours intervention (p=0.03) | Not significant | Not significant |
|
Denmark 12‐months |
Favours control (p<0.05) | Not significant | Not significant |
| 24‐months | Not significant | Not significant | Not significant |
| 30‐months | Not significant | Not significant | Not significant |
|
Finland 12‐months |
Favours intervention (p<0.001) | Not significant | Not significant |
| 24‐months | Favours intervention (p=0.05) | Not significant | Favours intervention (p<0.05) |
| 30‐months | Not significant | Not significant | Not significant |
|
The Netherlands 12‐months |
Not significant | Not significant | Not significant |
| 24‐months | Favours intervention (p=0.01) | Favours control (p<0.05) | Not significant |
| 30‐months | Favours intervention (p=0.04) | Not significant | Not significant |
|
Spain 12‐months |
Favours intervention (p<0.05) | Favours control (p=0.001) | Favours intervention (p=0.001) |
| 24‐months | Not significant | Not significant | Favours intervention (p<0.001) |
| 30‐months | Not significant | Not significant | Not significant |
|
Portugal 12‐months |
Not significant | Not significant | Not significant |
| 24‐months | Not significant | Favours intervention (p<0.05) | Favours intervention (p<0.05) |
| 30‐months | Favours intervention (p=0.01) | Favours intervention (p<0.05) | Favours intervention (p<0.01) |
|
UK 12‐months |
Favours control (p<0.05) | Favours control (p=0.01) | Not significant |
| 24‐months | Not significant | Not significant | Not significant |
| 30‐months | Not significant | Favours intervention (p<0.01) | Favours intervention (p<0.05) |
* Behavioural intention = intentions to smoke in the future
Although Elder 2000 showed no significant effects overall for smoking prevention, the time x treatment analysis of the 'susceptible cohort' showed a significant result in favour of the intervention at 12‐ and 24 months post study commencement. Similarly, the Gordon 2008 study produced no significant effects for the population as a whole or for 'cohort 1' separately, however 'cohort 2' showed a significant effect in favour of the intervention at 12‐months follow up. Authors report data for the four group comparison study in the Murray 1994 papers as showing no significant effects. However for the purposes of this analysis the three intervention groups have been combined and compared to the control group, which subsequently produced a marginally significant finding in favour of the control (p=0.05), although the confidence intervals do touch the line of no effect (95% CI 1.00 to 1.51, odds ratio 1.23).
Overall summary of secondary outcomes:
Secondary outcomes including behaviours, (intentions to smoke, rules on smoking) attitudes, (advantages, disadvantages, peer attitudes, overall attitudes, okay for young people to smoke) perceptions (peer smoking, norms) and knowledge (total, first use harmful/mild okay) had mixed results. For a summary of the intervention effectiveness at each reported study follow‐up period see Table 2. At final follow up a total of eight studies assessed smoking behaviours of which five favoured the intervention: Gordon 1997; Biglan 2000; Perry 2003; for combined D.A.R.E and D.A.R.E Plus groups (Gordon 2008); for time x treatment analysis only (Perry 2008); one study favoured the intervention for two out of six countries (De Vries 2003), and two had no significant benefit (D'Onofrio 2002; Klein 2009). Nine studies assessed attitudes, out of which five favoured the intervention (Gordon 1997; Biglan 2000; Elder 2000 (for time x treatment analysis only on tobacco‐anticipated outcomes); De Vries 2003 (for 2/6 countries only); Perry 2008), three showed no statistical difference between groups, whilst adjusted data in the Tang 1997 study for the outcome 'okay for young people to smoke' favoured the control, despite the overall meta‐analysis for this outcome favouring the intervention (p=0.02). Perceptions were assessed in six studies of which two favoured the intervention, (Biglan 2000; Piper 2000 (for Intensive HFL only, the Age appropriate HFL produced no significant benefit)), one favoured the control (Perry 2008) and three produced no significant differences between groups (Tang 1997; D'Onofrio 2002; Klein 2009). Finally, knowledge scores favoured the intervention in three (St Pierre 1992; Schofield 2003; Perry 2008) of the six studies which assessed this outcome, whilst the remaining three studies (Gordon 1997; Tang 1997; D'Onofrio 2002) showed no significant effect.
A combination of five studies were able to be included in the meta‐analyses, with three studies being the largest number available to assess one outcome. Behaviours were assessed as rules on smoking at home (Analysis 3.1) which showed a statistically and clinically significant effect favouring the intervention (OR 1.10 (95% CI 1.02 to 1.18), p=0.009), and intentions to smoke (Analysis 3.2), which also had a statistically non‐significant but clinically significant effect favouring the intervention. Perceptions of peer smoking were also pooled from two studies which did not show a significant result (Analysis 4.1).
3.1. Analysis.
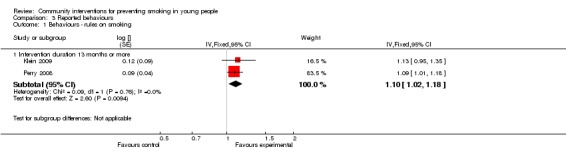
Comparison 3 Reported behaviours, Outcome 1 Behaviours ‐ rules on smoking.
3.2. Analysis.
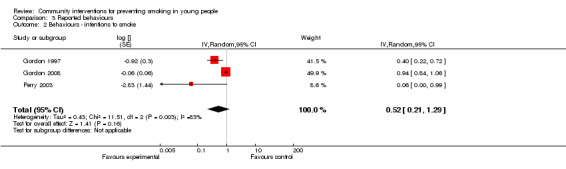
Comparison 3 Reported behaviours, Outcome 2 Behaviours ‐ intentions to smoke.
4.1. Analysis.
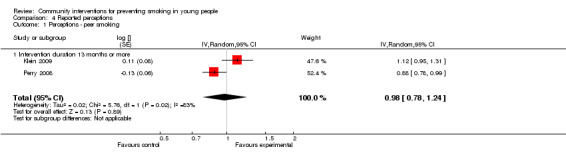
Comparison 4 Reported perceptions, Outcome 1 Perceptions ‐ peer smoking.
The De Vries 2003 study which was the largest containing six countries could not be included in the meta‐analyses due to the exclusion of baseline smokers from further follow up, as such a comparison to the other studies included in this review cannot be made. At 12‐months follow up the intervention groups from Spain and the UK reported significant results favouring the control for 'intentions to smoke in the next year', whilst the remaining four countries showed no significant effect. However at 24‐months follow up a significant effect in favour of the control was only seen in The Netherlands, while a beneficial effect was seen in Portugal. This changed again at 30‐months follow up with a beneficial effect in Portugal as well as the UK, whilst no significant differences were seen in the remaining four countries. The experimental group was significantly less convinced of the pros of smoking (or cons of not‐smoking) compared to the control group in one out of six countries at 12 months, three out of six counties at 24 months (resulting in an overall effect in favour of the intervention p<0.05) and two out of six countries at 30 months (also see Table 4).
Statistical analysis and cluster adjustments:
All studies allocated either entire countries, communities, schools or clubs to intervention or control groups. Seventeen studies accounted for the unit of allocation in their analyses, usually through hierarchical modelling or analysis of variance/covariance (Pentz 1989; Murray 1994; Perry 1994; Sussman 1998; Vartiainen 1998; Biglan 2000; Elder 2000; Piper 2000; Hancock 2001; D'Onofrio 2002; De Vries 2003; Perry 2003; Winkleby 2004; Gordon 2008; Perry 2008; Hawkins 2009; Klein 2009). Eight studies presented the results with the individual as the unit of analysis (St Pierre 1992; Winkleby 1993; Baxter 1997; Gordon 1997; Tang 1997; Schinke 2000; Stevens 2002; Schofield 2003). For these eight studies a manual adjustment for clustering was made using a design effect of 1.2 as described in the methods above under 'Unit of analysis issues'.
For the sub‐group 'Length of follow up, thirteen months or more', the longest available follow up was used for all outcomes in the data and analysis sections, the longest of which was Vartiainen 1998 with a 15‐year follow up reported. Some studies presented interim results which are not included in this meta‐analysis, however these results are discussed in more detail within the text and are documented in Table 2.
Sub‐group analyses by length of follow up:
Seven studies supplied results for follow up at twelve months or less which were able to be included in the meta‐analyses, and ten studies for follow up of thirteen months or more.
Smoking behaviour:
Smoking was assessed as daily (Analysis 2.1), weekly (Analysis 2.2), monthly (Analysis 2.3), ever smoked (Analysis 2.4) and smokeless tobacco use (Analysis 2.5). For short‐term follow up all outcomes demonstrated no significant effect. Significant heterogeneity (as assessed via multiple sources) was observed for the monthly and ever smoked outcomes with an I‐squared statistics of 70% and 64% respectively. As such these results should be interpreted with caution. For long‐term follown up (13 months or more) no statistically or clinically significant results were found for weekly or monthly tobacco use, however a statistically non‐significant but clinically significant effect was found for daily and smokeless tobacco use favouring the intervention.
2.1. Analysis.
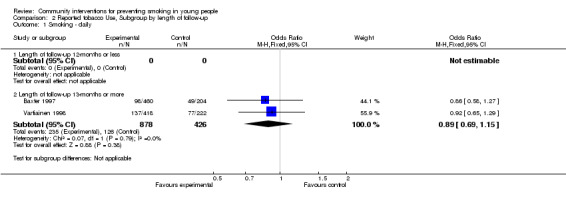
Comparison 2 Reported tobacco Use, Subgroup by length of follow‐up, Outcome 1 Smoking ‐ daily.
2.2. Analysis.
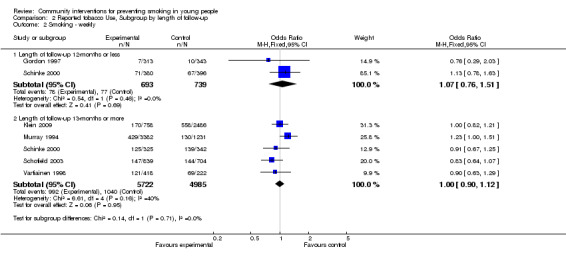
Comparison 2 Reported tobacco Use, Subgroup by length of follow‐up, Outcome 2 Smoking ‐ weekly.
2.3. Analysis.
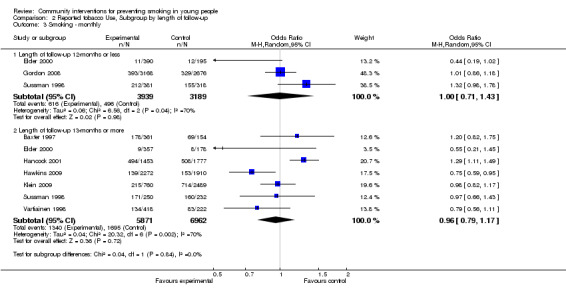
Comparison 2 Reported tobacco Use, Subgroup by length of follow‐up, Outcome 3 Smoking ‐ monthly.
2.4. Analysis.
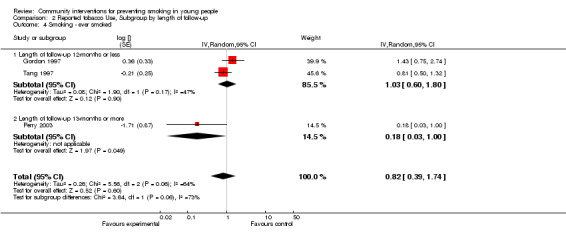
Comparison 2 Reported tobacco Use, Subgroup by length of follow‐up, Outcome 4 Smoking ‐ ever smoked.
2.5. Analysis.
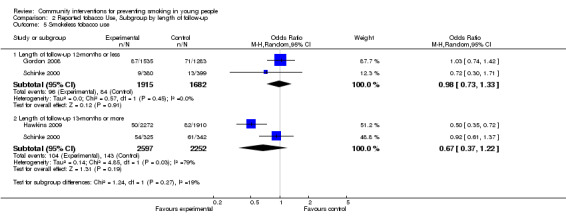
Comparison 2 Reported tobacco Use, Subgroup by length of follow‐up, Outcome 5 Smokeless tobacco use.
Secondary outcomes:
Secondary outcomes included youth attitudes (Analysis 5.1; Analysis 5.2; Analysis 5.3; Analysis 5.4; Analysis 5.5; Analysis 6.1; Analysis 6.2), behaviours (Analysis 5.6; Analysis 5.7; Analysis 6.3), knowledge (Analysis 5.8; Analysis 5.9) and perceptions (Analysis 6.4), which are presented in the relevant analyses.
5.1. Analysis.
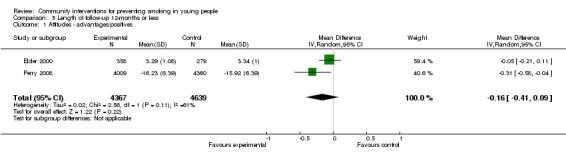
Comparison 5 Length of follow‐up 12‐months or less, Outcome 1 Attitudes ‐ advantages/positives.
5.2. Analysis.
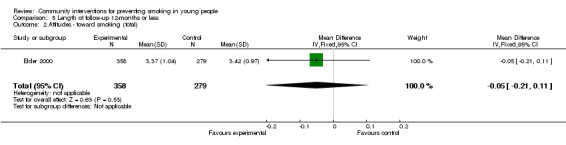
Comparison 5 Length of follow‐up 12‐months or less, Outcome 2 Attitudes ‐ toward smoking (total).
5.3. Analysis.
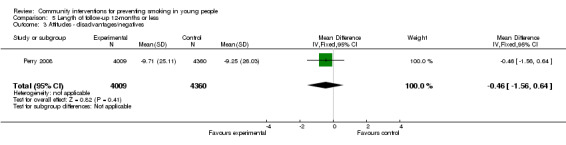
Comparison 5 Length of follow‐up 12‐months or less, Outcome 3 Attitudes ‐ disadvantages/negatives.
5.4. Analysis.
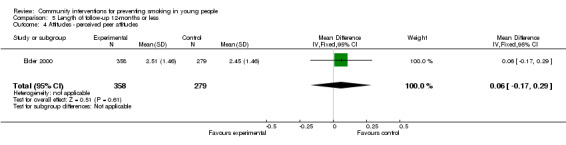
Comparison 5 Length of follow‐up 12‐months or less, Outcome 4 Attitudes ‐ perceived peer attitudes.
5.5. Analysis.
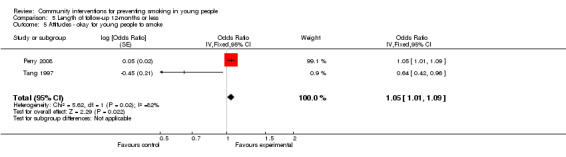
Comparison 5 Length of follow‐up 12‐months or less, Outcome 5 Attitudes ‐ okay for young people to smoke.
6.1. Analysis.
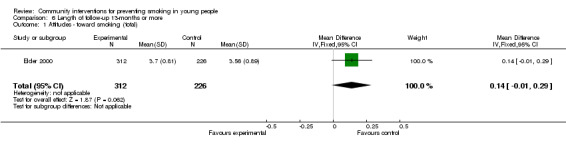
Comparison 6 Length of follow‐up 13‐months or more, Outcome 1 Attitudes ‐ toward smoking (total).
6.2. Analysis.
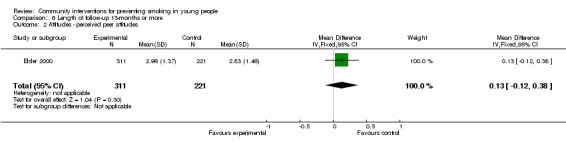
Comparison 6 Length of follow‐up 13‐months or more, Outcome 2 Attitudes ‐ perceived peer attitudes.
5.6. Analysis.
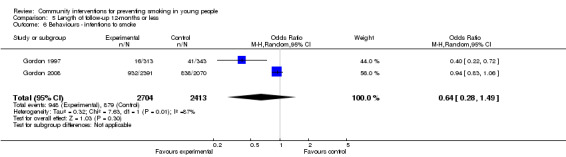
Comparison 5 Length of follow‐up 12‐months or less, Outcome 6 Behaviours ‐ intentions to smoke.
5.7. Analysis.
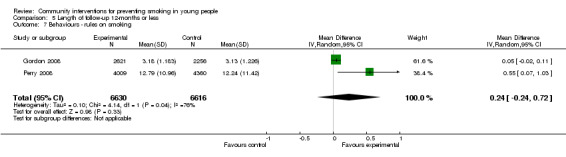
Comparison 5 Length of follow‐up 12‐months or less, Outcome 7 Behaviours ‐ rules on smoking.
6.3. Analysis.
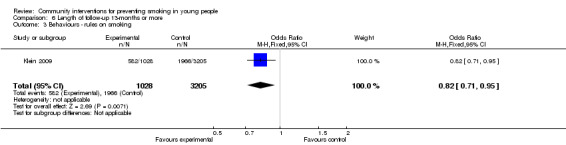
Comparison 6 Length of follow‐up 13‐months or more, Outcome 3 Behaviours ‐ rules on smoking.
5.8. Analysis.
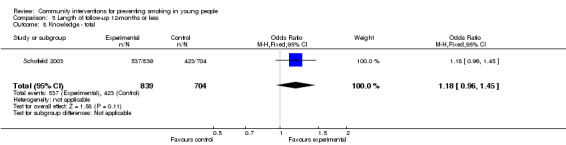
Comparison 5 Length of follow‐up 12‐months or less, Outcome 8 Knowledge ‐ total.
5.9. Analysis.
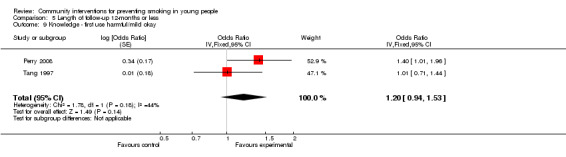
Comparison 5 Length of follow‐up 12‐months or less, Outcome 9 Knowledge ‐ first use harmful/mild okay.
6.4. Analysis.
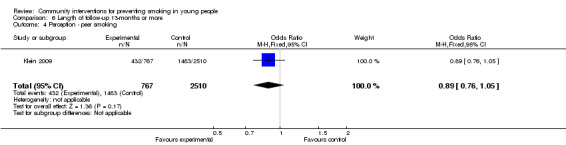
Comparison 6 Length of follow‐up 13‐months or more, Outcome 4 Perception ‐ peer smoking.
Cost effectiveness:
Costs of the interventions varied enormously amongst the few studies which provided details. One excluded study which reported the results for the UK Smokebusters programme in Wensleydale in 1992 stated that the project had cost approximately £6,000 to implement and evaluate (Davidson 1994). This was in comparison to a state wide initiative in the USA (implemented in 1985) which received a total of $2 million per year funded from higher taxes on tobacco products (Murray 1994). Through the prevention of adolescent smoking, Murray 1994 estimate the total monetary savings related to public health implications in the Kansas city area at $40 679 for each boy and $13 232 for each girl.
Process Measures
A variety of different process measures were recorded for the number of different activities participants engaged in (St Pierre 1992; D'Onofrio 2002; De Vries 2003; Schofield 2003), the percentage of students who took part in each activity (Sussman 1998; Stevens 2002; Schofield 2003; Winkleby 2004; Perry 2008; Hawkins 2009), saw media advertisements (Murray 1994), details about the actual implementation of the programme (Pentz 1989; Sussman 1998; Stevens 2002; De Vries 2003; Schofield 2003; Perry 2008; Hawkins 2009) and process measures recorded through teacher feedback questionnaires (Tang 1997). One study showing no impact on smoking prevalence also reported no significant difference in awareness of anti‐smoking campaigns or association between awareness and smoking status (Hancock 2001).
Discussion
Twenty‐five studies evaluating the effectiveness of community interventions met the inclusion criteria for this review, representing a diverse set of interventions. Five focused on reducing specific health risk factors for cancer (Hancock 2001) or cardiovascular disease (Winkleby 1993; Perry 1994; Baxter 1997; Vartiainen 1998) with influencing smoking behaviour as a secondary component of the programme, seven studies combined tobacco prevention with either reduction or cessation initiatives (Pentz 1989; Murray 1994; D'Onofrio 2002; De Vries 2003; Perry 2003; Winkleby 2004; Hawkins 2009) whilst the remaining thirteen focused exclusively on influencing smoking behaviour including prevention initiatives.
Of these 25 studies, ten were associated with a reduction in the uptake of smoking amongst young people (Pentz 1989; St Pierre 1992; Perry 1994; Vartiainen 1998; Biglan 2000; De Vries 2003; Perry 2003; Winkleby 2004; Perry 2008; Hawkins 2009). Common features to these successful programmes include nine of the ten incorporating school based multi‐component interventions with intervention delivery by school teachers and other faculty members, six had parental involvement in the intervention programme, eight had intervention durations longer than 12 months and nine of the ten interventions were based on the social influences or social learning theory. The exception was Hawkins 2009 which used the social development model (Catalano 1996; Fleming 2008). However the development of programmes to influence smoking behaviour with theoretical concepts exclusively based on the social influences approach, has been criticised in the literature (Bauman 1996; De Vries 2003), with suggestions that indirect peer pressure may be just as effective to prevent peer smoking. Five of the seven studies combining tobacco prevention with either reduction or cessation initiatives were successful in influencing the smoking behaviour of young people (Pentz 1989; De Vries 2003; Perry 2003; Winkleby 2004; Hawkins 2009). Three of the five studies which included community leader participation with active involvement in both the development and ongoing support of the community programmes were also effective in reducing youth smoking (Perry 1994; Perry 2003; Hawkins 2009), however the remaining two studies, Piper 2000 (for the Age Appropriate intervention) and Hancock 2001 showed significant benefits in favour of the control. Five of the nine studies including mass‐media as additional programme components favoured the intervention (Pentz 1989; Perry 1994; Biglan 2000; De Vries 2003; Perry 2008).
Eight of the 13 unsuccessful programmes had intervention durations of 12 months or less with a mean of 2.5 years for the remaining seven studies. Community leader involvement in both the development and ongoing support for the programmes occurred in one of the 13 unsuccessful studies, with Hancock 2001 being the exception. However the primary focus of the Hancock 2001 study was cancer prevention, as such the community leader involvement was not primarily focused on influencing youth smoking behaviour. Seven of the unsuccessful programmes also used the social influences model, three used community action/organisation theory (Winkleby 1993; Hancock 2001; Schofield 2003) and five used other theories, for example office system's approach (Stevens 2002), modifiable risk factors to influence youth smoking (Baxter 1997; Klein 2009), social acceptance (Gordon 2008) or an unclear theoretical basis (Gordon 1997). Four of the thirteen unsuccessful campaigns used mass media as a programme component, four had peer involvement to act as role models and deliver programme components, thirteen involved school based intervention components and ten included parent participation. A suggestion has been made that the most substantial increases in adolescent tobacco use occur later in high school and as such, parental communication has its impact not on the age of first experimentation but rather on later regular use (Stevens 2002). Therefore, investigations of young cohorts which use parental influences for the prevention intervention, should continue follow up into high school for a more accurate example of parental influences on smoking prevention. Five of the successful studies used peers as role models, in comparison to four of the thirteen unsuccessful studies. According to current literature the perceived prevalence of smoking in the community influences youth smoking behaviours, which was confirmed in the Klein 2009 study. In this study, authors report that the influence of friends' smoking status rendered a more powerful influence on smoking behaviour that the programme policy alone. Youth with close friends who smoked were more likely to smoke than youth with no close friends who smoke, which was consistent with the De Vries 2003 study.
The lack of community leader involvement, mass media intervention components and peer influences to support the community interventions, such as those in the successful campaigns, likely attributes to the eventual failure in influencing youth smoking behaviour, in these unsuccessful programmes.
One of the two studies which produced a negative effect for smoking prevalence, (Hancock 2001), had a focus of cancer prevention; with influencing youth and adult smoking behaviour as secondary components. Methodological flaws such as small sample size, lack of biological validation for abstinence, nonsensical responses in surveys and lower consent rates in the second cross‐sectional survey are discussed, however this does not necessarily provide a reason for the failing of the intervention programme. The authors do state a concern regarding process measures through school principal reports of anti‐smoking activities in the past two years, which may provide some reasoning for the observed effect. No significant differences were found between treatment and control schools for reported activities, which suggests that many similar activities occurred in control towns and schools as happened in the intervention towns and schools. Piper 2000 reported different effects on smoking prevalence between two different versions of an intervention, compared with a control group receiving standard health education. At three‐year follow up monthly smoking in the Age Appropriate intervention was 36% (p<0.01) compared to 30% in the control and 28% in the Intensive intervention. Authors suggest a number of explanations for these findings including: insufficient time available to effect cultural change, saturation of the prevention message by 8th grade (coined the 'fatigue factor'), implementation difficulties (only in the Age Appropriate arm), insufficient time and resources for the community level interventions, lack of intervention tailoring for specific sub‐populations, multiple intervention messages which have different social meanings to different sub‐groups and inadequate control as numerous health promotion and prevention programmes were run throughout the elementary and middle‐school years.
Some dichotomy is emerging in the uptake of smoking between genders. As mentioned in the background, current reports indicate that smoking behaviour among adolescent girls is increasing over that of boys (Mackay 2006; Warren 2009). The Perry 2003 study did show a significant difference amongst boys in the D.A.R.E. Plus group compared to the controls for tobacco use, which was not present in the female population. This was also seen in the Schofield 2003 study. Authors state their findings strongly support the more widespread gender trend in which girls are nearly twice as likely as boys to be smokers in the early adolescent period. As a result consideration should be given to gender‐specific prevention and cessation programmes during early adolescence in the future. It is also worth noting that there is an increasing trend in the use of bidi smoking, especially in India as per the Perry 2008 study. There is a misinformed notion amongst youth that bidi smoking (also spelled beedis or beedies) is less harmful than regular cigarettes as they look herbal due to the leaf wrapping and they come in a variety of flavours such as vanilla, chocolate, strawberry, mango, cherry etc. However, they do not contain filters like cigarettes and contain less tobacco but more nicotine (Rahman 2000). One study found that one bidi produced more than three times the amount of carbon monoxide and five times the amount of tar than one cigarette (Watson 2003). Furthermore, they contain chemicals such as hydrogen cyanide, ammonia and phenol in greater quantities than normal cigarettes and to keep bidis lit, more frequent and deeper puffs are required in comparison to cigarettes (Gupta 2008).
Where possible we pooled pre‐specified outcomes in meta‐analyses, however these results should be considered with caution as some studies did not report in a way that allowed data to be included. Furthermore, we used the outcome at the final follow‐up periods in these meta‐analyses, with the exception of the sub‐group 'Length of follow up 12 months or less'. Many studies provided data at multiple time periods. As a result some of the studies are not represented within these analyses and the outcomes may be misleading. Most of the studies which reported significant benefits could not be included in the meta‐analysis. For this reason we recommend consideration be given to data presented in Table 2 and Table 3 when interpreting each outcome.
When combining studies in the meta‐analysis to measure smoking prevalence rates, significant heterogeneity was identified for a number of outcomes as determined via multiple sources including I‐squared statistic, visual inspection of the data and characteristics of studies. Where appropriate, the analysis methods of outcomes were changed from the fixed effect to the random effect model as outlined in the methods. It has been recognised that community‐wide programmes are especially difficult to evaluate (CART 1996a) and that many community interventions have failed to meet the criteria for rigorous scientific evaluation (CART 1996b). For example, there are particular difficulties in establishing adequate control groups (CART 1996a). Communities (or large groups) have to be assigned to either intervention or control groups rather than individuals, which means that the analysis of outcomes should be at the level of the community rather than the individual. The unit of analysis however is often presented at the individual level due to the increased power supplied to the study, which in turn gives a greater chance of finding positive programme effects. Ignoring the correct unit of analysis may lead to spurious positive findings (Altman 1997). For example one study (Murray 1992; Murray 1994) reported that if clustering had been ignored and the results had been based on the individual as the unit of analysis (without adjustment) then there would have been a spurious significant difference between the two groups, with the 2.4% net decline in smoking behaviour in the intervention state being reported as significant. One of the first community trials to employ GEE to address clustering problems was D'Onofrio 2002. They have published another paper contrasting GEE with more common analytic methods using the data from Murray 1996. Clustering was addressed in this meta‐analysis through reducing the size of the trial to the effective sample size (Rao 1992) using the original sample size from each study, divided by a design effect of 1.2 which is consistent with other smoking cessation community intervention trials (Gail 1992).
Using youth within schools as sampling units may limit the generalisability of the findings. Only six studies did not use schools as the sampling unit (St Pierre 1992; Winkleby 1993; Elder 2000; D'Onofrio 2002; Stevens 2002; Klein 2009). In one study all age‐eligible persons within randomly selected households were sampled, therefore, increasing the likelihood of including young people at high risk for smoking who may be missed when students within schools are sampled. In their sample of 19 to 24 year‐olds approximately ten per cent were high school drop‐outs and their levels of smoking were significantly higher than those students completing high school (50% versus 20%) (Winkleby 1993). As the individuals sampled in most studies were predominantly students within schools, it is unclear how the results may generalise to young people outside of the school system. As mentioned in the results, nine studies did not adjust for clustering effects within the analysis, as such a manual adjustment for clustering was made using a published design effect (Gail 1992).
Despite methodological problems common to several of the studies which met the inclusion criteria for this review, they represent the most rigorous set of studies available evaluating the effectiveness of community interventions in influencing the smoking behaviour of young people. It is important to recognise that community programmes are influenced by local factors and are likely to be difficult to replicate exactly in other settings. However, the principles and methods upon which an effective intervention was based could be useful for programme implementation in similar settings.
Authors' conclusions
Implications for practice.
Overall, there is some limited support for the effectiveness of community interventions in influencing smoking behaviour, including the prevention of smoking in young people. The following programme characteristics could be considered by individuals involved in planning future community programmes:
build upon elements of existing programmes (particularly those including multi‐component school based interventions, parental involvement, intervention duration longer than 12 months and based on the social influences or social learning theory model), that have been shown to be effective rather than repeating methods that have achieved limited success;
programmes need to be flexible to the variability between communities so that the different components of a given programme can be modified to achieve acceptability;
developmental work with representative samples of those individuals to be targeted should be carried out so that appropriate messages and activities can be implemented;
programme messages and activities should be guided by a combination of theoretical constructs about how behaviours are acquired and maintained;
community activities must reach the intended audience if they are to stand any chance of success of influencing the behaviour of that audience;
consider the use of community leader involvement in the planning, development and ongoing implementation of community programmes, mass media as a source of message delivery, the use of peers as role models and specific programme components for boys and girls separately.
Implications for research.
The evaluation of community‐wide campaigns to influence smoking behaviour is methodologically challenging, yet rigorous evaluation is required in order to demonstrate effectiveness. Careful planning of the evaluation is required, in terms of: analysis at the correct level, for example if communities are the unit of allocation then they should also be the unit of analysis or alternatively the unit of allocation should be accounted for in the analysis.
Measurement of appropriate outcomes: different levels of measurement should be planned, including behavioural, intermediate (or mediating) and process. The adequacy of implementation of each component of the intervention should also be recorded.
Feedback
Comment from Toshi Furukawa, 3 May 2013
Summary
Comment: This review is very confusing.
1) Why do you include non‐randomised studies when you already have 15 randomised ones? Moreover, you do not seem to separate the two kinds in the funnel plots?
2) The narrative summary/abstract is totally non‐congruent with your own SoF.
I agree with the conflict of interest statement below:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
Reply
Thank you for your comments.
1) Why do you include non‐randomised studies when you already have 15 randomised ones? Moreover, you do not seem to separate the two kinds in the funnel plots?
Originally when the review was conceived it was believed that the inclusion of randomised and non‐randomised controlled trials combined would offer the readers with the best summary of evidence as it is sometimes quite difficult to randomise community level studies. Controlled clinical trials still have the potential to offer useful information pertaining to tobacco outcomes and as such were included. To take these difficulties into account this pre‐specified methodology was carried out through to review completion despite the identification of a large number of randomised controlled studies so as not to introduce biases with changing approaches whilst conducting a review. However, as we are now approached another update for this review we agree with the comment and as such will be pre‐specifying the exclusion of controlled clinical trials without randomisation. The funnel plots were not used to separate the differences between randomised and non‐randomised controlled trials as again this was not a pre‐specified approach. Funnel plots were only used in an attempt to identify selective reporting of studies as a whole. There are many tests that can be added on post hoc that we and many others would perhaps find interesting once the initial analyses are complete, however this introduces issues around selective reporting, which the pre‐specified protocol aims to eliminate.
2) The narrative summary/abstract is totally non‐congruent with your own SoF.
This will be corrected in the update and a consumer representative will be utilised to ensure that all components of the review are consistent and clearly understood.
Kristin V Carson (Queen Elizabeth Hospital, Adelaide, Australia)
Contributors
Toshi Furukawa (Kyoto University School of Public Health); Kristin V Carson (Queen Elizabeth Hospital, Adelaide, Australia)
What's new
| Date | Event | Description |
|---|---|---|
| 30 May 2013 | Feedback has been incorporated | One comment received and addressed by the author. |
History
Protocol first published: Issue 3, 1997 Review first published: Issue 1, 2000
| Date | Event | Description |
|---|---|---|
| 29 April 2011 | New citation required but conclusions have not changed | New author team. No major change to conclusions but changes include updated and reformatted characteristics of included studies table; risk of bias assessment for all included studies; updated format for data and analyses; characteristics of interventions table and summary of findings table. |
| 29 April 2011 | New search has been performed | Eight new included studies; 29 new 'excluded but relevant' studies; two previously included studies now excluded; |
| 18 June 2008 | Amended | Converted to new review format |
| 24 September 2002 | New citation required but conclusions have not changed | Updated for 2003 issue 1. Two studies changed from unpublished to published. Four new studies included. No major changes to conclusions. |
Acknowledgements
Firstly, we would like to thank Lindsay Stead and Monaz Mehta for carrying out an extensive set of searches, obtaining full text for included studies, providing recommendations, ongoing support and most importantly their patience during the update.
We would also like to thank Keith Smolkowski, Judith Gordon, Steven Schinke, Joel Moskowitz and Cheryl Perry for supplying raw data and Tena St Pierre for responding to the requests for raw data.
Thank you to Veronica Pitt, Miranda Compton and all the staff at the Monash Cochrane Centre in Melbourne for their guidance and advice, and peer reviewers for their useful comments.
Laura Arblaster was an author on the first version of this review and Amanda Sowden and Lindsay Stead updated the review from issue 1, 2003.
Appendices
Appendix 1. Databases searched for previous updates of the review
Cancerlit (Dialog)1975 ‐ 1998/9, NTIS (Dialog)1964 ‐1998/9, Diogenes (Dialog)1976 ‐1998/9, Business and Industry Index (Dialog)1984 ‐1998/9, Criminal Justice Periodical Index (Dialog) 1975 ‐1998/9, Management & Marketing Abstracts (Datastar) 1975 ‐1998/9, SIGLE (Blaiseline)1980 ‐ 1998/9, Directory of Published Proceedings (Datastar) 1990 ‐ 1998/9, Dissertation Abstracts (Dialog)1861 ‐ 1998/9, Harvard Business Review (Dialog)1971 ‐ 1998/9, DH‐Data (Datastar and WinSPIRS)1983 ‐ 1998/9 Healthstar (OVID)1975 ‐ December 2001, CAB Health (Datastar)1973 ‐1998/9 (Winspirs) 1998 ‐ September 2002, ABI/INFORM (Datastar)1971 ‐1998/9 (Proquest) 1998 ‐ September 2002.
Appendix 2. ECONLIT search strategy
1 smoking.mp. [mp=heading words, abstract, title, country as subject] 2 (smoking or tobacco or cigarette$).mp. 3 1 or 2 4 (young people or child or children or juveniles or girls or boys or teenagers or adolescent$ or adolescence or minor$).mp. 5 (nationwide or statewide or countrywide or citywide).mp. 6 (nation wide or state wide or country wide or city wide).mp. 7 outreach.mp. 8 (multicomponent or multifacet or multifaceted or multidisciplinary).mp. 9 (field based or fieldbased).mp. 10 (interdisciplinary or inter disciplinary).mp. 11 local.ti. or citizen$.mp. 12 (community or communities).mp. 13 8 or 6 or 11 or 7 or 10 or 9 or 12 or 5 14 4 and 3 and 13
Appendix 3. EMBASE & PsycINFO search strategy
1 smoking.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 2 (smoking or tobacco or cigarette$).mp. 3 1 or 2 4 (young people or child or children or juveniles or girls or boys or teenagers or adolescent$ or adolescence or minor$).mp. 5 (nationwide or statewide or countrywide or citywide).mp. 6 (nation wide or state wide or country wide or city wide).mp. 7 outreach.mp. 8 (multicomponent or multifacet or multifaceted or multidisciplinary).mp. 9 (field based or fieldbased).mp. 10 (interdisciplinary or inter disciplinary).mp. 11 local.ti. or citizen$.mp. 12 (community or communities).mp. 13 8 or 6 or 11 or 7 or 10 or 9 or 12 or 5 14 4 and 3 and 13
Appendix 4. CSA Databases search strategy
Sociological Abstracts, British Humanities Index, PAIS, ERIC, ASSIA
Query: ((TI=cigarette* or smoking or tobacco) or(KW=cigarette* or smoking or tobacco) or(AB=cigarette* or smoking or tobacco)) and ((KW=young people or child or children or juveniles or girls or boys) or (TI=young people or child or children or juveniles or girls or boys) or (AB=young people or child or children or juveniles or girls or boys)) and ((KW=(nationwide or statewide or countrywide or citywide or nation wide or state wide or country wide or city wide or outreach or multicomponent or multifacet or multifaceted or multidisciplinary or field based or fieldbased or interdisciplinary or inter disciplinary or local or citizen* or community or communities)) or(TI=(nationwide or statewide or countrywide or citywide or nation wide or state wide or country wide or city wide or outreach or multicomponent or multifacet or multifaceted or multidisciplinary or field based or fieldbased or interdisciplinary or inter disciplinary or local or citizen* or community or communities)) or(AB=(nationwide or statewide or countrywide or citywide or nation wide or state wide or country wide or city wide or outreach or multicomponent or multifacet or multifaceted or multidisciplinary or field based or fieldbased or interdisciplinary or inter disciplinary or local or citizen* or community or communities)))
Appendix 5. CENTRAL search strategy
#1 (smoking or tobacco or cigarette*):ti,ab,kw and (child* or juvenile* or girls or boys or teen? or teenager? or adolescen*):ti,ab,kw and (communit* or nation* or state* or country* or city* or outreach or (multi NEXT (component or facet or faceted or disciplinary)) or interdisciplinary or (field next based)):ti,ab,kw #2 sr‐tobacco #3 (#1 AND NOT #2)
Data and analyses
Comparison 1. Reported tobacco use.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Smoking ‐ Daily | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Intervention duration 13 months or more | 2 | 1304 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.69, 1.15] |
| 2 Smoking ‐ weekly | 6 | 11363 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 2.1 Intervention duration 12 months or less | 2 | 1323 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.67, 1.21] |
| 2.2 Intervention duration 13 months or more | 4 | 10040 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.14] |
| 3 Smoking ‐ monthly | 8 | 18677 | Odds Ratio (M‐H, Random, 95% CI) | 0.98 [0.84, 1.14] |
| 3.1 Intervention duration 12 months or less | 2 | 6326 | Odds Ratio (M‐H, Random, 95% CI) | 1.01 [0.87, 1.16] |
| 3.2 Intervention duration 13 months or more | 6 | 12351 | Odds Ratio (M‐H, Random, 95% CI) | 0.96 [0.77, 1.20] |
| 4 Smoking ‐ ever smoked | 3 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 4.1 Intervention duration 12 months or less | 3 | Odds Ratio (Random, 95% CI) | 0.82 [0.39, 1.74] | |
| 5 Smokeless tobacco use | 3 | 7667 | Odds Ratio (M‐H, Random, 95% CI) | 0.78 [0.50, 1.22] |
| 5.1 Intervention duration 12 months or less | 2 | 3485 | Odds Ratio (M‐H, Random, 95% CI) | 0.98 [0.76, 1.26] |
| 5.2 Intervention duration 13 months or more | 1 | 4182 | Odds Ratio (M‐H, Random, 95% CI) | 0.50 [0.35, 0.72] |
Comparison 2. Reported tobacco Use, Subgroup by length of follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Smoking ‐ daily | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Length of follow‐up 12‐months or less | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Length of follow‐up 13‐months or more | 2 | 1304 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.69, 1.15] |
| 2 Smoking ‐ weekly | 6 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Length of follow‐up 12‐months or less | 2 | 1432 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.76, 1.51] |
| 2.2 Length of follow‐up 13‐months or more | 5 | 10707 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.12] |
| 3 Smoking ‐ monthly | 8 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Length of follow‐up 12‐months or less | 3 | 7128 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.71, 1.43] |
| 3.2 Length of follow‐up 13‐months or more | 7 | 12833 | Odds Ratio (M‐H, Random, 95% CI) | 0.96 [0.79, 1.17] |
| 4 Smoking ‐ ever smoked | 3 | (Random, 95% CI) | 0.82 [0.39, 1.74] | |
| 4.1 Length of follow‐up 12‐months or less | 2 | (Random, 95% CI) | 1.03 [0.60, 1.80] | |
| 4.2 Length of follow‐up 13‐months or more | 1 | (Random, 95% CI) | 0.18 [0.03, 1.00] | |
| 5 Smokeless tobacco use | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Length of follow‐up 12‐months or less | 2 | 3597 | Odds Ratio (M‐H, Random, 95% CI) | 0.98 [0.73, 1.33] |
| 5.2 Length of follow‐up 13‐months or more | 2 | 4849 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.37, 1.22] |
Comparison 3. Reported behaviours.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Behaviours ‐ rules on smoking | 2 | (Fixed, 95% CI) | Subtotals only | |
| 1.1 Intervention duration 13 months or more | 2 | (Fixed, 95% CI) | 1.10 [1.02, 1.18] | |
| 2 Behaviours ‐ intentions to smoke | 3 | (Random, 95% CI) | 0.52 [0.21, 1.29] |
Comparison 4. Reported perceptions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perceptions ‐ peer smoking | 2 | (Random, 95% CI) | 0.98 [0.78, 1.24] | |
| 1.1 Intervention duration 13 months or more | 2 | (Random, 95% CI) | 0.98 [0.78, 1.24] |
Comparison 5. Length of follow‐up 12‐months or less.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Attitudes ‐ advantages/positives | 2 | 9006 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.41, 0.09] |
| 2 Attitudes ‐ toward smoking (total) | 1 | 637 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.21, 0.11] |
| 3 Attitudes ‐ disadvantages/negatives | 1 | 8369 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.56, 0.64] |
| 4 Attitudes ‐ perceived peer attitudes | 1 | 637 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [‐0.17, 0.29] |
| 5 Attitudes ‐ okay for young people to smoke | 2 | Odds Ratio (Fixed, 95% CI) | 1.05 [1.01, 1.09] | |
| 6 Behaviours ‐ intentions to smoke | 2 | 5117 | Odds Ratio (M‐H, Random, 95% CI) | 0.64 [0.28, 1.49] |
| 7 Behaviours ‐ rules on smoking | 2 | 13246 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.24, 0.72] |
| 8 Knowledge ‐ total | 1 | 1543 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.96, 1.45] |
| 9 Knowledge ‐ first use harmful/mild okay | 2 | Odds Ratio (Fixed, 95% CI) | 1.20 [0.94, 1.53] |
Comparison 6. Length of follow‐up 13‐months or more.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Attitudes ‐ toward smoking (total) | 1 | 538 | Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.01, 0.29] |
| 2 Attitudes ‐ perceived peer attitudes | 1 | 532 | Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.12, 0.38] |
| 3 Behaviours ‐ rules on smoking | 1 | 4233 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.71, 0.95] |
| 4 Perception ‐ peer smoking | 1 | 3277 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.05] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baxter 1997.
| Methods |
Country: United Kingdom: England Design: Controlled Clinical Trial; Non‐equivalent control group; Pre‐/Post‐test control; Three communities matched for coronary heart disease rate and socio‐economic status and allocated to intervention or control Objectives: To evaluate a community‐wide intervention for school children aimed at reducing cardiovascular risk factors, implemented simultaneously with a cardiovascular risk reduction programme for adults Study site: Three communities in 2 electoral wards in Rotherham programmename: Action Heart Methods of Analysis: Cohort and cross‐sectional analyses; logistic regression models (allowed for differences between boys and girls, and between intervention schools) Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Clusters: n=3 secondary‐schools in intervention areas and 13 primary‐schools (Swinton and Wath); 1 secondary‐schools in control area (Maltby) (unknown number of primary‐school cluster) Individuals: (Year 7 and 10) 1991: Intervention n=1091 Control n=503; 1994: Intervention n=1344; Control n=536 Recruited: 1991: Intervention n=955 Control n=372; 1994: Intervention n=1202; Control n=476 Completed: Not matched cohort (cross‐sectional evaluation only) Age: 11‐year‐olds and 14‐yea‐ olds Gender: Ratio (boys/girls) varied from 0.52 to 1.5 Ethnicity: No data presented Recruitment means: Each school was contacted by telephone and subsequently letter to seek permission and gain commitment to the survey. All children with median ages of 11‐years and 14‐years in school years 7 and 10 were eligible |
|
| Interventions |
Theoretical basis: Risk factors chosen for which there was good research evidence that modifying them reduces the risk of coronary heart disease. Research evidence sought for health promotion interventions that could produce the desired lifestyle changes. Intervention description: Evaluated health education material; Peer‐led health education included health days; Implementation of policies such as: i) Action Heart Charter, ii) non‐smoking policies, iii) healthy eating policies; Action Heart worker; Publicity; One school had staff training; Community based activities Control description: Usual health promotion activities Duration of intervention: Three years Intervention delivered by: Not explicitly stated: project supported by health promotion officers, health visitors, project staff, dietitians, school nurses and school staff |
|
| Outcomes |
Method of outcome collection: Validated questionnaires, administered by teaching staff, used to elicit information about smoking, diet and exercise; Economic analysis of schools component of the intervention carried out Pre specified outcomes: Changes in chosen lifestyle risk factors in school children in the intervention and control areas Validation: None Follow‐up: Three years: pre‐test 1991; post‐test 1994 following completion of the intervention |
|
| Notes | No mention of sample size calculation ‐ results may not have sufficient power to determine effectiveness of intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi Experimental ‐ Chosen areas |
| Allocation concealment (selection bias) | High risk | Quasi Experimental ‐ assignment was foreseen |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large amounts of missing data from one of the intervention schools and from three classes of 10‐year‐olds in the control school; Subject survey missing data not explicitly described except that the same decision rules for coding were applied |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement of yes or no; No protocol available to detect initial outcomes. All said outcomes were addressed in this publication |
| Other bias | Unclear risk | Questionnaires not validated once changed, pilot data not presented in terms of validation; Different interventions used across the three intervention schools |
| Imbalance of outcome measures at baseline addressed? | High risk | Smoking outcome baseline imbalance, control school 11‐year‐olds in 1991 reported 10‐times the smoking rate of the intervention schools |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Unclear what the reported similarities in participant characteristics were and how the "distinctly geographically different community" would also affect the different characteristics of its population |
| Protection against contamination? | Unclear risk | Not described |
| Selective recruitment of participants addressed? | Unclear risk | Unclear if all secondary/primary‐schools in the selected communities agreed to participate |
Biglan 2000.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Pre/post control; cluster; non‐equivalent control group Objectives: To evaluate the effectiveness of a multi‐component community‐wide intervention to prevent adolescent tobacco use Study site: Sixteen communities (populations of between 1,700 to 13,500 people each) in Oregon county programmename: Project SixTeen Methods of Analysis: Random coefficients analysis for nested cross sectional design; Controlled for sex and grade and interactions with intervention; Social factors also controlled if they contributed to significant variance Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Not explicitly stated; population of Oregon communities ranged from 1700 to 13500 Recruited: Across all assessments, grades and conditions, 7% were not assessed because parents declined, 2.5% were not assessed because the student declined to participate at the time of the assessment, 4% were absent and were not available when absentee assessments were done, 0.2% were missing for unknown reasons, and 0.6% had dropped out of school Completed: Clusters: Eight communities received the school based prevention programme only (SBO), and 8 received the SBO plus community interventions Individuals: Total available only: T1 n=4438; T2 n=4515; T3 n=4425; T4 n=4708; T5 n=4165 Age: 11‐year‐old and 13‐year‐old students and their parents Gender: Baseline students Males 52%; Females 48%; parents Males 24%; Females 76% Ethnicity: Percentage of minority students ranged from 0.9% (African American) to 6.8% (Hispanic) Recruitment means: School districts that agreed to implement the school based intervention and to permit the in‐school assessment; Successive cross‐sectional surveys undertaken of all age eligible (all 7th and 9th grade) students at each time point; A 30% random sample of parents of assessed students were also surveyed |
|
| Interventions |
Theoretical basis: Social influences, including the use of multiple channels to reach people in a supportive social context Intervention description: i) School based programme consisting of 5 sessions over a one week period in grades 6 (11‐years) through 12 (17‐years) aimed at drug use prevention, (health facts, refusal skills, modelling refusal skills, public commitment and peer led discussion), ii) media advocacy, iii) youth anti‐tobacco (YAT) activities, iv) family communications (FC) about tobacco through school or civic prompted parent‐child activities v) Activities to reduce illegal sales of tobacco to young people Control description: same as i) above: School based programme consisting of 5 sessions over a one week period in grades 6 (11‐years) through 12 (17‐years) aimed at drug use prevention, (health facts, refusal skills, modelling refusal skills, public commitment and peer led discussion) Duration of intervention: Three years Intervention delivered by: Paid community coordinators and youth and adult volunteers; Teachers trained for 2‐ to 3‐hours by project staff |
|
| Outcomes |
Method of outcome collection: Annual school questionnaire survey of students; Postal questionnaire sent to parents enclosing $10; Two follow‐up mail prompts and one phone call reminder to parents Pre specified outcomes: awareness of smoking prevention and cessation activities, awareness of efforts to prevent illegal sales of tobacco, attitudes toward tobacco, friend's smoking, intentions to smoke and tobacco use; Postal questionnaire used to obtain: ratings of exposure to anti‐tobacco information, awareness of efforts to prevent youth access to tobacco, attitudes to the deleterious effects of tobacco use, interactions with other parents about adolescent tobacco use, town support for tobacco access restrictions, support of the community e.g. school, government officials, and business leaders, for tobacco use prevention programmes Validation: Samples of expired air CO from students; Community coordinators monitored weekly the number of community activities Follow‐up: Four years: T1 baseline/ T2 one year/ T3 two years/ T4 three years/ T5 four years |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin tossing described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient methodology described to permit judgement of yes or no |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Although some outcome data is missing, reasons for attrition are unlikely to produce bias however it is unclear if they are balanced between groups; Missing community coordinator weekly reports are unlikely to be related to true outcome; Subject survey missing data removed from analysis |
| Selective reporting (reporting bias) | High risk | post‐hoc analysis ‐ Authors state: “...if not significant...we dropped the interactions from the analysis”; “An effect on the slope of prevalence across time points was evident only when time‐2 data points were eliminated from the analysis" |
| Other bias | Low risk | No other biases were identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Analysis of covariance occurred for outcome measures at baseline |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Not described as separated groups, n‐values and other characteristics combined in one table |
| Protection against contamination? | Low risk | Each community shared no common high‐schools and were at least 20 miles apart |
| Selective recruitment of participants addressed? | Unclear risk | Although percentages of students taking surveys are similar across groups, it is unclear if teachers could have selected or not selected some students to take part in the surveys; Furthermore, the selection of high‐schools in each community is not detailed, i.e., some high‐schools may have been missed completely from the community |
D'Onofrio 2002.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Pre/post control group; cluster; non‐equivalent control group Objectives: To enable youth to develop personal policies about tobacco use and to participate with others in developing and implementing sound tobacco policies and programmes within the home, the 4‐H club, the school, and the community; the intervention's primary aim was preventing and reducing smokeless tobacco (ST) use among youth: the prevention and reduction of cigarette smoking became an additional objective Study site: 4‐H clubs throughout California and community agencies programmename: Project 4‐Health Methods of Analysis: GEE model using regression analysis to account and control for clustering effects; Pre‐test data also were analysed separately for each post‐test sub‐sample to determine whether the experimental conditions were affected by participant attrition: this analysis used programme condition, post‐test completion, and the interaction of these variables as factors; process variables included post‐test outcomes: fidelity of implementation, positive adaptations, programme leader characteristics (e.g. communication skills, youth vs. adult programme leaders), member's attendance, and club size; Co‐founders assessed with analysis of covariance controlling for pre‐test differences on the post‐test variable: In the individual‐level analysis, age and gender were factors along with process measures; For the club‐level analyses, individual‐level data were aggregated to the club level to create separate files for boys and girls, separate analyses were then conducted for each gender as well as for all members Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: Individual students: Interventin n=977; Control n=990 Recruited: Clusters: Seventy eight 4‐H community clubs Individuals: Intervention n=938; Control n=915 Completed: 67.8% of pre‐test youths completed both post‐tests Individuals: Intervention T1 n=938; T2 n=716; T3 n=724; Control T1 n=915; T2 n=760; T3 n=716 Age: Range 10‐ to 14‐years; Mean age of the eligible members at pre‐test was 12.11‐years (SD=1.32) Gender: Pre‐test: Males 787 (42.5) Female 1066 (57.5) Ethnicity: Pre‐test: White non‐Hispanics 89.4%; Latino 6.5%; Asian/Pacific Islander 1.1%; Native American 0.6%; African American 0.3% Missing 2.1% Recruitment means: Community‐based youth groups throughout the large and geographically diverse state of California were targeted by investigators because 4‐H community clubs enrol members between 9‐ and 19‐years of age, are led by volunteers and vary in size from fewer than 10 members to more than 100 members; Seventy eight 4‐H community clubs with a minimum enrolment of 20 members each |
|
| Interventions |
Theoretical basis: Social influences theory Intervention description: In‐club sessions comprised 'going further' activities to be completed by 4‐H members between club meetings; Each member received an illustrated, self‐guided booklet that reviewed the five club sessions and provided complete instructions and all necessary worksheets for the going‐further activities, as well as various other puzzles, stories, experiments, and activities to advance the programme’s goals; Other programme materials included a comprehensive leader’s manual, a pamphlet for parents identifying specific ways they could help, and a guide for clubs and members who wanted to from a Project 4‐Health Action Team: This latter guide provided directions and worksheets for a variety of optional group projects such as creating a tobacco use policy for the 4‐H club, conducting a tobacco survey at school, organising a poster display and contest, creating a prevention commercial, working with community agencies on tobacco use prevention, organising a tobacco‐free day, and starting a cessation group Control description: Youths attended their regular club meetings Duration of intervention: Five monthly community club meetings occurring between January and May 1988; tobacco education programme mean time spent 29.4 min (SD=10) with 5 sessions total Intervention delivered by: Implemented under real‐world conditions by trained volunteer leaders and not by project staff |
|
| Outcomes |
Method of outcome collection: Three Methods Used: CATI alone (Computer‐assisted telephone interviews); Mail survey and CATI; Small group administration in a community setting Pre specified outcomes: Tobacco‐related outcomes assessed including knowledge, attitudes, perceived social influences, intentions, behaviours; parental tobacco use, sibling tobacco use, cigarette smoking by friends, and ST use by friends Validation: None Follow‐up: Two years: T1 Baseline/ T2 nine months/ T3 two years; Pre‐test data was collected in fall 1987 and 2‐year follow‐up, was carried out in summer 1990 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table used as per contact with authors |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of yes or no |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study lost participants to attrition who were more likely to smoke and at a higher risk of smoking; Attrition addressed and was similar across groups; Authors state no bias caused by loss of study participants; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | post‐hoc data was analysed using analysis methods that were not pre‐specified and reported in text and table; Some relevant outcome data not collected but authors mention should have been |
| Other bias | High risk | Different interventions delivered to each group; The full intervention was not delivered (67% on average only); Large gap between publication of results and completion of 2‐year follow‐up (12‐years); Initiation of a state‐wide tobacco education programme in 1990 may have affected control group results |
| Imbalance of outcome measures at baseline addressed? | Low risk | Exclusions were similar in both groups; Baseline imbalances in outcome data addressed; Analysis of covariance occurred |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Groups analysed for differences using GEE analysis..."strongly suggests that the experimental conditions were initially equivalent" |
| Protection against contamination? | Unclear risk | No mention of cross over between 4‐H groups, however due to the local proximity it is possible that some contamination occurred between intervention and control groups, either through members moving or leaders |
| Selective recruitment of participants addressed? | Unclear risk | As 4‐H leaders conducted the analysis with youth, some selective recruitment may have occurred as the method of individual level recruitment was not described; Also, participant numbers for individual clusters and their subsequent percentages for survey completion was not provided |
De Vries 2003.
| Methods |
Country: Denmark, Finland, Netherlands, Spain, Portugal, United Kingdom Design: Controlled Clinical Trial; Cluster; Nested Objectives: The overall ESFA goal was to reduce smoking onset in the experimental group by 10% in comparison with the control group after 3‐years Study site: Schools and communities programmename: European Smoking prevention Framework Approach (ESFA) Methods of Analysis: Attrition and differences in smoking prevalence was analysed using logistics regression; Lesson exposure was measured by t‐tests; Differences between conditions for various outcomes were analysed with analysis of covariance and final models were run with multi‐level analysis Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: Not reported Recruited: Clusters: Schools ‐ Intervention n=111; Control n=124 Individuals: n=23 531 non‐smoking subjects in total (students who were smokers at baseline were not included in the analysis) Completed: Clusters: Schools ‐ Intervention n=111; Control n=124 Individuals: T2 (12‐months) n=15 422; T3 (24‐months) n=10 751; T4 (30‐months) n=9282 Age: mean=13.3‐years at baseline Gender: 49.8% male and 50.2% female at baseline Ethnicity: Not specified though recruitment occurred from six countries Recruitment means: National programme managers were asked to invite four regions from each locale to participate; Schools within these regions were subsequently asked to participate prior to enrolment |
|
| Interventions |
Theoretical basis: Attitude‐Social influence‐self‐Efficacy (ASE) model which originated from the Theory of Reasoned Action in addition to insights of various other theories such as Social Cognitive Theory, Transtheoretical Model, Precaution Adoption Model, Precede model, ABC planning model, Micro‐Macro Level Theory and Intervention Mapping Intervention description: Varied for each country and each school; School based ‐ teacher‐led school based programmes including teaching refusal skills, role‐playing, newsletters, public commitments not to smoke, education, posters, competitions and smoking cessation advice; Parent based ‐ Information, cessation advice/assistance, Quit and Win contests, guidelines distributed on how to discuss smoking with children and parent/child quizzes were implemented in some countries for parents; Community based ‐ posters were created, publications in local media, dental care intervention, youth clubs included non‐smoking education, non‐smoking TV commercials, magazines sent to home address, cards, stickers, activities to reduce cigarette sales to minors, non‐smoking conferences on National non‐smoking day, articles in local newspapers, pharmacist training, sports organisations received information and flyers and community actions for children undertaken in some countries Control description: Normal practice (varied between each country) Duration of intervention: Three years in total (individual programme durations varied between countries); School based ‐ Finland: Five 1‐hour lessons, teachers received 20‐hours training; Denmark: Six 1‐hour lessons; Netherlands: Five 1‐hour lessons; United Kingdom: Five 30‐minute lessons, teachers received 1‐day training course; Portugal: Six lessons duration not reported, teachers received a 48‐hour training course; Spain: Six lessons (Four 1‐hour and two 2‐hour), teachers received four 2‐hour training sessions Intervention delivered by: Various ‐ Primary‐school teachers, regional health coordinators, parents and community members |
|
| Outcomes |
Method of outcome collection: Self administered questionnaire Pre specified outcomes: Smoking behaviour (ever and weekly); adolescent attitudes, self‐efficacy expectations and intentions to take up smoking Validation: None Follow‐up: Three years; T1 baseline/ T2 one year/ T3 two years/ T4 thirty months |
|
| Notes | Process measures were undertaken | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Although some regions/schools within countries were said to be randomized (methods not described) others self‐selected into intervention and control groups |
| Allocation concealment (selection bias) | High risk | Spain self‐selected one city district for intervention and control schools were matched; No mention of allocation concealment for other countries in which schools were randomized |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition from T1 to T4 was significant (52.2%), however logistics regression was used; only questionnaires with 90% answered and did not have missing values in the outcome variables were included ‐ subject survey missing data removed from analysis |
| Selective reporting (reporting bias) | High risk | Subjects who were smokers at baseline were excluded from analysis |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Stastically significant differences in baseline smoking status were reported however an analysis of covariance was conducted |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Insufficient information to permit judgement of yes or no |
| Protection against contamination? | High risk | In the Netherlands schools in the control condition underwent a national smoking prevention programme |
| Selective recruitment of participants addressed? | High risk | Individual participant n‐values not specified for intervention and control groups for each country at baseline; one country (Spain) self selected one city district to receive the intervention |
Elder 2000.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Pre‐/Post‐test control group; cluster; non‐equivalent control group Objectives: To evaluate a community‐based tobacco use‐prevention programme compared with an attention‐control condition (first aid/home safety) group; A major emphasis of the intervention was on improving communication with parents and changing tobacco attitudes Study site: The Migrant Education programme in San Diego County, California; Adolescents school site; Small‐group format sessions were held in the evenings on school groups or at nearby community agencies; programmename: Sembrando Salun (sowing the seeds of health) Methods of Analysis: Logistic regression analyses with susceptibility regressed on the predictor variables; Generalised estimating equations (GEEs) were used to account for the repeated measures and for the effects of clustering that resulted when forming intervention groups within schools; For each model, covariates included the baseline value for that outcome measure, the group variable, the dose variable, and the dose by group interaction; The GEE adjusted for the clustering effect of the group leaders and schools; A dose‐response relationship was examined for several measures of dose, including youth sessions only (0 to 8); Co‐founders included Age, Gender, Acculturation, time M3/M2 and M4/M2 Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: Clusters: n=25 schools within 17 school districts in San Diego county Individuals: Not explicitly stated, however the intervention group had more eligible families (56% of the total) which was maintained through contacts, agreement to participate and enrolment Recruited: Clusters: n=22 schools within 15 school districts Individuals: n=660 adolescents and one adult care‐giver for each; Intervention n=370; Control n=290 (i.e., 56% in intervention) Completed: Individuals: Intervention: T1 n=370; T2 n=358; T3 n=326; T4 n=277; Control: T1 n=290; T2 n=279; T3 n=240; T4 n=187 Age: Range 11‐ to 16‐years Gender: Total population: male n=337 (51%) female n=323 (49%) Ethnicity: Hispanic Recruitment means: Potential subjects were identified through the Migrant Education programme in San Diego County, California; Twenty five schools within 17 school districts in San Diego County were eligible to participate in the study; Participating families came from 22 schools and 15 school districts; Schools with a large migrant education enrolment were considered for inclusion in the project; eligibility included having an adolescent (1) between 11‐ and 16‐years of age and (2) enrolled in the Migrant Education programme in Region IX, San Diego County |
|
| Interventions |
Theoretical basis: Stress and social influences model; including adult or parental support Intervention description: Components included group leader‐led discussions, videos, demonstrations, skill practice, and role playing; information about the effects of tobacco use; information about social influences on tobacco use; training in refusal skills involving parents in prevention programmes and the importance of the family (e.g. value of children, support from extended family, religious beliefs, strong parent‐child attachment, and strong sense of family loyalty; individual factors (e.g. coping, self‐esteem, self‐efficacy, risk taking, or conventionality) and situational factors (e.g. peer and parental support or availability) determine substance use; Through presentation of information, modelling, and behavioural rehearsal, the adolescents were exposed to how problems could be identified and analysed, solutions generated and decisions made, implemented, and evaluated; Parental communication skills, such as listening (e.g. verbal and nonverbal attention), confirmation (e.g. accepting messages) and re‐assurance (e.g. expressing care and concern) were developed and reinforced through behavioural methods of modelling, role playing, and behaviour rehearsal Booster: After the intervention sessions, the participants received three “booster” telephone calls at <1 month and at 14 months after the last group sessions; Three newsletters were also mailed to each participant’s home according to his/her intervention status; For participants in the tobacco and alcohol group, the contents of the newsletters repeated and reinforced information about tobacco and alcohol refusal, the health effects of smoking, and the health effects of alcohol Control description: Components included group leader‐led discussions, videos, demonstrations, skill practice, and role playing; The first aid/home safety educational programme focused on preparation for an emergency (e.g. assembling a first aid kit) and how to approach an emergency victim (e.g. check, call, and care); Specific skills required to respond to an individual presenting with physical problems (e.g. fever, burn, bleeding, fracture/dislocation, sudden illness, poisoning, and bites/stings) were modelled, role played, and rehearsed; Household safety concerns were also addressed (e.g. baby‐proofing a house) Booster: After the intervention sessions, the participants received three “booster” telephone calls at <1‐month and at 14‐months after the last group sessions; Three newsletters were also mailed to each participant’s home according to his/her intervention status. The newsletters for the participants in the attention‐control condition contained information on a first aid kit and wound care, bleeding and burn care, and home safety Duration of intervention: Eight week intervention conducted between January 1996 and December 1997; Each telephone booster lasted approximately 5‐ to 10‐minutes; Participants received three telephone booster calls at <1‐month and at 14‐months after the last group session Intervention delivered by: Group leaders: all group leaders were bilingual and bicultural Mexican Americans; Many of the group leaders were themselves former students in the Migrant Education Program; parents and peers also played a role |
|
| Outcomes |
Method of outcome collection: Trained evaluation assistants who were bilingual, bicultural, and blinded to condition conducted face‐to‐face baseline surveys; The 201‐item survey was interviewer administered and assessed Pre specified outcomes: Susceptibility to smoking, as well as smoking over the past 30‐days were the primary outcomes of interest; The 201‐item survey included standard demographic information such as age, gender, income, household size, acculturation, current smokers, firm resolve not to smoke, accept a cigarette, from a friend, intended to smoke in the next year; Attitudes assessed included anticipated outcomes for use, intentions for use, and self‐standards; Parent‐child communication included concepts of parent communication and parent monitoring Validation: Expired CO was used prior to completion of the survey, adolescents were asked to exhale twice into a Vitalograph‐Breath CO monitor, carbon monoxide monitor, 29.700 using standard protocols Follow‐up: Two year follow‐up, intervention staggered over two years: T1 baseline/ T2 two months (immediate post‐intervention)/ T3 one year post‐intervention/ T4 two years post‐intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned however sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | Some attempts were made to blind evaluation assistants, but this was not sufficient for all aspects: outcome assessors and investigators were aware of groups |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Similar attrition rates across groups for study sample; However, the one‐third of participants who declined may have had a higher smoking/drinking rate than those who took part in the study; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | 30‐day smoking data was primary outcome of interest and collected, but due to small sample size the authors did not analyse these results; Susceptibility to smoking is reported which is a combination of outcomes i.e., intentions to smoke are not reported elsewhere |
| Other bias | Unclear risk | Potential concern with language translation or information lost is translation; There were 3 additional group‐leaders in the intervention group which could have affected the overall success of intervention delivery; Some questions about the validity of the self‐reported outcome measures are raised |
| Imbalance of outcome measures at baseline addressed? | Low risk | Authors believe the smoking status in this trial population may not be indicative of the true population mean smoking levels; Baseline cohort may not be true representation of the sample due to Migrant Education Program's emphasis on healthcare access ‐ covariates adjusted for in analysis |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | More subjects were recruited in the two intervention conditions which authors attribute to randomization; however randomization methods were not described "As a result of the random assignment of schools to the two intervention conditions, the intervention group....had more eligible families....this percentage difference in the two intervention groups was maintained when looking at the number of families contacted, agreeing to participate and eventually enrolling in the study" |
| Protection against contamination? | High risk | Some schools had both intervention and control groups in them, which produces a high risk for contamination |
| Selective recruitment of participants addressed? | Unclear risk | Insufficient reporting of selection methods to permit a judgement of yes or no |
Gordon 1997.
| Methods |
Country: United Kingdom, Wales Design: Randomized Controlled Trial; Pre‐/post‐test control group; cluster; non‐equivalent control group; Eight schools randomly selected and allocated to intervention or control Objectives: Evaluation of a school based education programme and community interventions to delay the onset of smoking in young people Study site: Schools and communities of a Local Education Authority area in the city of Cardiff programmename: Stopping Them Starting Methods of Analysis: No data presented Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Cluster n=23 LEA secondary‐schools; n=19 schools agreed to participate Recruited: Clusters: n=8 schools were randomly selected and assigned to intervention and control groups Individuals: n=1569 total Completed: Clusters: n=4 Intervention schools; n=4 Control schools Individuals: Matched cohort intervention n=376; Matched cohort control n=411 (63% overall response rate) Age: Range 11‐ to 12‐years Gender: Not explicitly stated Ethnicity: No data presented Recruitment means: Schools; teachers administered questionnaires and collected completed forms from students in sealed envelopes |
|
| Interventions |
Theoretical basis: Not clear Intervention description: Includes key workers in a range of local agencies encouraged to raise smoking related issues with young people; anti‐smoking displays in public places; all tobacco retailers reminded of the law; smoking prevention booklet for use in schools and a take‐home workbook; near some schools purchases of cigarettes tested with retailers all carried out in the catchment areas of the 4 intervention schools Control description: Smoking prevention booklet for use in schools and a take‐home workbook; near some schools purchases of cigarettes tested with retailers Duration of intervention: Six months Intervention delivered by: Health promotion specialists produced the anti‐smoking booklet; key workers in local agencies raised tobacco related issues with young people |
|
| Outcomes |
Method of outcome collection: Confidential questionnaire administered by teachers to obtain students Pre specified outcomes: current and past smoking behaviour, attitudes to smoking, intentions to smoke, and knowledge about smoking; experience of purchasing cigarettes, awareness of cigarette brands and advertising. Qualitative data obtained by health promotion specialists from key workers about community based activities. Validation: None reported Follow‐up: Six months |
|
| Notes | Small scale project; Sample size can affect outcomes in this study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Eight schools were randomly selected and assigned to control and intervention groups. Randomization occurred through coin tossing |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The remaining cohort numbers (i.e., unmatched) have not been quantified; It is unclear how many were "missing data" and how may students did not have matched data; Outcome data for attitudes and smoking behaviour are missing however not quantified; Subject survey missing data not reported |
| Selective reporting (reporting bias) | Unclear risk | Unclear which outcomes are being reported as attitudes; Insufficient information to permit judgement of yes or no |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Unclear risk | Insufficient information to determine; No adjustments were made for covariance or imbalance |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Limited baseline characteristics are mentioned, unable to assess outcome |
| Protection against contamination? | High risk | Contamination mentioned as a difficulty in the discussion section |
| Selective recruitment of participants addressed? | Unclear risk | Insufficient data to determine selective recruitment of participants, through it is possible as teachers administered the questionnaires |
Gordon 2008.
| Methods |
Country: United States of America Design: Randomized Controlled Trial Objectives: To evaluate family communications (FC) and youth anti‐tobacco activities (YAT) for their effect on the onset of tobacco use among students in middle‐schools Study site: Schools programmename: Youth Anti‐tobacco Activities (YAT) and Family Communication (FC) Methods of Analysis: Nested time x condition analysis and ANCOVA. For attrition: mixed‐model ANOVA Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=128 schools (70 districts) Recruited: Clusters: Intervention n=20; Control n=20 Individuals: Intervention n=3324; Control n=2952 Completed: Clusters: Intervention n=21; Control n=19 Individuals: Intervention n=2018; Control n=1739 Age: Total for both groups: 6th grade range 11‐ to 12‐years; 8th grade 30% age 13‐years, 66% age 14‐years Gender: Total for both groups: 6th grade 50% female; 8th grade 51% female Ethnicity: Caucasian 68%; Hispanic 11%; Native American 6%; African American 2%; Asian 2%; Pacific Islander 1% Recruitment means: Schools via marketing packet delivery to schools by local prevention coordinators; The team travelled to 70 districts to explain the study and determine district interest; Recruitment into YAT by health teachers, principals and school counsellors |
|
| Interventions |
Theoretical basis: Positive association between not smoking and images or activities involving social acceptance Intervention description: Staff distributed videos and homework to sixth graders in intervention schools, requiring students to watch them with a parent/guardian; Classes and families received incentives for assignments returned; Specific activities included poster and mural contests, health fairs, after‐school clubs, scavenger hunts, school carnivals, school assemblies, “Hackademy” awards, community festival booths, roller skating, rock climbing, bowling, snowboarding/skiing, disc golf tourneys, skateboard competitions, amusement parks Control description: No‐intervention control Duration of intervention: Most events occurred within a 9‐month period, starting immediately after baseline Intervention delivered by: Research Staff, videos, teachers parents; teen narrators who were older than the study participants for the videotapes |
|
| Outcomes |
Method of outcome collection: Anonymous survey; random samples of families in each school for non‐anonymous detailed data on intervention impact and family interactions Pre specified outcomes: Smokeless tobacco (boys only); days smoked in past month, number of cigarettes per day in past month, intentions to smoke (susceptibility), home rules, smoker image, praise expected to receive for tobacco abstinence, cigarette companies target kids Validation: None reported Follow‐up: One year |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin‐flipping used to randomized schools ‐ data obtained from contact with authors |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Students without post‐test information reported higher levels of prevalence than students with post‐test data; There was also a significant interaction between condition and attrition status for susceptibility, with fewer students at high susceptibility for smoking providing data a post‐test in the intervention group; Subject survey missing data were removed from analysis |
| Selective reporting (reporting bias) | High risk | Due to very low rates of female smokeless tobacco use authors examined this outcome for males only; Due to changes in intervention for cohort 2, outcomes were tested together and separately for cohort 1 and cohort 2 (post‐hoc); No data reported for tobacco companies targeting kids; Efforts were also increased to identify and recruit youth at highest risk of starting tobacco use |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Mixed model analysis of covariance conducted |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Data not presented |
| Protection against contamination? | Unclear risk | Possible contamination due to close proximity of schools, however contamination not mentioned; One control school accidentally obtained intervention materials and was subsequently reclassified as intervention |
| Selective recruitment of participants addressed? | Unclear risk | n‐values similar across groups, the one control school which transferred to intervention adequately addressed; Insufficient information on recruitment methods to permit judgement of yes or no |
Hancock 2001.
| Methods |
Country: Australia Design: Ranomized Controlled Trial; cluster; nested; pre‐post design Objectives: To evaluate the effectiveness of a community action intervention for cancer prevention on adolescents Study site: n=20 rural towns programmename: Cancer Action in Rural Towns (CART) Methods of Analysis: Logistic regression controlling for age, gender and school year and accounting for design effects Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: n=49 town clusters and n=29 secondary‐school clusters Recruited: Clusters: Town clusters: Intervention n=10; Control n=10; School clusters: Group allocation unknown n=28 total Individuals: Intervention n=1888; Control n=2085 Completed: Clusters: Town clusters: Intervention n=10; Control n=10; School clusters: Group allocation unknown n=25 total Individuals: Intervention n=1453; Control n=1777 Age: Total: Mean 14.6‐years at T1 (range 13‐ to 16‐years) Gender: 50% female at T1 Ethnicity: Not explicitly stated Recruitment means: Towns were selected by researchers based on demographic characteristics; The community recruitment occurred with the use of a external community facilitator to act as a link between community and the research team; An extensively advertised open‐invitation community meeting was held in each town which led to the formation of the CART steering committee; All year 9 and year 10 students (13‐ to 16‐years) from all secondary‐schools were invited to participate in cross‐sectional surveys of smoking behaviours, pre‐ and post‐test data collection was staggered over 2‐years |
|
| Interventions |
Theoretical basis: Community action, using community committees and the utilization of access‐point networks to initiate and maintain intervention strategies Intervention description: Community facilitator recruited. Access points included health care providers, community organizations, media, retailers, schools and workplaces; Activities varied across towns, including surveys on smoking policies, encouragement of smoke free venues, media coverage, letters to schools (8 towns), letters to parents (5 towns) Control description: Not explicitly stated: Assumed no intervention Duration of intervention: Two to 3‐years (introduced gradually into towns) Intervention delivered by: Community facilitators: Cancer council health education officers were recruited for each intervention town; Other community members and teachers |
|
| Outcomes |
Method of outcome collection: Questionnaires completed at school under examination conditions Pre specified outcomes: Smoking in past 4‐weeks, rules about home smoking; At time‐2 also asked about perceived change in legal age signage, ease of purchase, awareness of CART, awareness of school anti‐smoking activities. Validation: None reported Follow‐up: Three to 4‐years: T1 Baseline 1993 and 1994/ T2 1997 |
|
| Notes | Baseline data collections were conducted from Febuary to March 1993 and from February to March 1994, however follow‐up only occurred at one time period being February to March 1997. As a result the final follow‐up is between 3‐ to 4‐years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random numbers list was used after town pairs were matched using a computer programme created by the researchers |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Weekly and ever smoking were also collected however results not reported in this paper as authors deemed them to be ‘very similar’ to those for monthly smoking; 25 of 28 schools from time‐1 agreed to be surveyed at time‐2 (no schools from town 4 agreed to be re‐surveyed); students who provided nonsensical responses at time‐1 and ‐2 were excluded from analysis: no further information provided about these samples; No mention of characteristics of attrition sample; Fewer boys took part in the second survey; Authors note that smoking rates did not increase as much for boys as for girls which could be an indicator that fewer boys whom smoked answered the survey or that males had a higher deception rate than a true difference |
| Selective reporting (reporting bias) | High risk | Rules on smoking were presented in text however this was not separated out for intervention and control groups |
| Other bias | Low risk | No other potential biases were identified |
| Imbalance of outcome measures at baseline addressed? | Unclear risk | No analysis of covariance for outcomes were assessed to compare treatment groups; There was no mention of comparability between intervention and control group outcomes at baseline |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Logistic regression with age, gender and school year was conducted |
| Protection against contamination? | Low risk | Proximity of towns from different matched pairs randomized into different conditions was not allowed due to the risk of contamination |
| Selective recruitment of participants addressed? | Unclear risk | It is possible that selective recruitment occurred within schools and clusters, however there is insufficient information to permit a judgement of yes or no |
Hawkins 2009.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Nested; Cluster Objectives: To test whether the Communities That Care (CTC) prevention system reduces adolescent alcohol, tobacco and other drug use and delinquent behaviour community wide Study site: Schools, homes, communities programmename: Communities That Care (CTC) Methods of Analysis: Generalised linear mixed modelling with logit or Poisson link functions; Random‐intercept models were estimated to account for variation across time within students, among students within communities, and communities within matched pairs of communities; mixed‐model analysis of covariance with student and community characteristics, respective grade 5 drug use or delinquency measures were included as pre‐intervention covariates to adjust for any potential baseline imbalances Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Clusters: Community n=41; School districts n=29 Individuals: Intervention n=3170; Control n=2621 Recruited: Clusters: Community: Intervention n=12; Control n=12; School districts total n=28; Schools total n=88 Individuals: Intervention n=2405; Control n=2002 Completed: Clusters: Community: Intervention n=12; Control n=12; School districts: not explicitly stated; Schools: Intervention n=41; Control n=36 Individuals: Year 5 Intervention n=1867, Control n=1346; Year 6 Intervention n=2368, Control n=1987; Year 7 Intervention n=2274, Control n=1921; Year 8 Intervention n=2272, Control n=1910; Age: Range 10‐ to 14‐years Gender: Total population only: Females n=2194; Males n=2213 Ethnicity: Mean percentages for all of the CYDS community (n=24): Intervention: Caucasian 89.5%; Hispanic 9.2%; African‐American 2.5%; Control: Caucasian 89.3%; Hispanic 10.1%; African‐American 2.6% Recruitment means: Communities which did not advance in the 'Diffusion Project' were eligible for the CYDS study; Recruitment occurred by mailing information packets and making in‐person phone calls to each school district superintendent and each elementary middle‐school principal asking for commitment to programme |
|
| Interventions |
Theoretical basis: Theory of change Intervention description: Intervention communities received 6 CTC training sessions delivered over 6‐ to 12‐months by certified CTC trainers; Community leaders created a community coalition of diverse stakeholders to implement CTC; They were trained to use survey data, prioritise risk factors to be targeted by prevention actions in the community, to choose tested and effective prevention policies and programmes that address the community’s targeted risk factors, to implement these interventions with fidelity, and to monitor implementation and outcomes of newly installed prevention programmes; The 12 intervention communities selected 13 different prevention programmes to implement during 2004‐2005 school year, 16 programmes in 2005‐2006 school year and 14 programmes during the 2006‐2007 school year; On average 3 programmes were implemented per community annually; These programmes included school based programmes, community‐based youth‐focused programmes and family‐focused programmes; Duration and intensity of each programme varied (also see 'Duration of intervention' below) Control description: Control communities were matched to intervention communities based on population size, racial/ethnic diversity, economic indicators and crime rates and were not thought to be using a risk‐ and protection‐focused approach Duration of intervention: 2.66‐years in total: Parent training programmes ‐ Strengthening families programme: 7, 2‐hr weekly sessions; Guiding Good Choices: 5, 2‐hr weekly sessions; Parents Who Care: 7, 2‐hr weekly sessions; Family Matters: Completion of material in 6‐months; After‐school programmes ‐ Stay SMART: 12, 60‐min weekly sessions; Participate and Learn Skills: 10, 45‐min sessions 2‐times per week; Big Brothers/Big Sisters: Matches meet 2‐times per month; Tutoring: 45‐min sessions 4‐times per week; Valued Youth: 45‐min sessions, 4‐times per week, 30 weeks; School based programmes ‐ All Stars Core: 14, 45‐min weekly sessions; Life Skills Training: 12 (Level 1) and 8 (Level 2), 45‐min weekly sessions; Lion’s Quest Skills for Adolescence: 40, 45‐min weekly sessions; Project Alert: 11, 45‐min weekly sessions; Olweus Bullying Prevention programme: Weekly, year‐long classroom sessions Intervention delivered by: CTC trainers taught community leaders; Community Youth Development Study implementation staff provided technical assistance through weekly telephone calls, e‐mails, and site visits to CTC communities at least once a year; Community leaders then implemented initiatives within their communities; local providers implemented local programmes including teachers for school programmes, health and human service workers for community‐based, youth‐focused, and family‐focused programmes and community volunteers for Big Brothers Big Sisters and tutoring programmes |
|
| Outcomes |
Method of outcome collection: Annual surveys of a panel of public school students who were in the fifth grade during the 2003‐2004 school year; self‐administered paper and pencil questionnaire Pre specified outcomes: Incidence and prevalence of tobacco use; smokeless tobacco in the past month Validation: None reported Follow‐up: Three years |
|
| Notes | Process measures reported: On average 3 programmes were implemented per community annually; P265 "...adherence improved slightly over the 2‐years for most programmes, with rates averaging 91% in 2004‐2005 and 94% in 2005‐2006. Only one programme (programme Development Evaluation) markedly decreased in adherence over the 2‐years (from 93% to 54%)."; P271 "...about 80% of families and students attended at least 60% of the parent training and after‐school sessions delivered in 2004‐2006. Nearly all children (96% in 2004‐2005 and 91% in 2005‐2006) were exposed to at least 60% of the required number of sessions in school based programmes." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | One community from within each matched pair was assigned randomly by coin toss to either the intervention (CTC) or control condition |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment methods not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition accounted for; Missing subject survey data were dealt with via multiple imputations |
| Selective reporting (reporting bias) | High risk | Results between grades 6 and 7; and 6 and 8 are only reported as visual presentation; Grades 6 to 7 for cigarette hazard favoured control |
| Other bias | Low risk | No further biases detected |
| Imbalance of outcome measures at baseline addressed? | Low risk | Mixed‐model analysis of covariance with respective grade 5 drug use as pre‐intervention covariates to adjust for any potential baseline imbalances |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Mixed‐model analysis of covariance with student and community characteristics included as pre‐intervention covariates to adjust for any potential baseline imbalances, however no data presented for these populations |
| Protection against contamination? | Unclear risk | Insufficient information to permit judgement of yes or no |
| Selective recruitment of participants addressed? | High risk | 13 pairs of communities were eligible for inclusion, however only 12 were recruited; no information provided as to the exclusion of the thirteenth pair |
Klein 2009.
| Methods |
Country: United States of America Design: Controlled Clinical Trial; Nested; Cluster; Pre‐post Objectives: To evaluate the association between local CIA (Clean Indoor Air) policies and smoking behaviours among Minnesota youth over time and subsequently discourage youth smoking Study site: Homes, and intervention delivered throughout public places e.g. restaurants, pubs, bars etc. programmename: Data drawn from the MACC study (Minnesota Adolescent Community Cohort) Methods of Analysis: A GEE (generalised estimating equation) logistic regression was used; Analysis controlled for potential cofounders at individual and community level Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: Clusters: n=129 Geopolitical units (GPU's) (Overall sample) Individuals: 58.5% response rate from eligible households (Overall sample) Recruited: Clusters: GPU's: Intervention n=60; Control not explicitly stated; Cities: Intervention n=9; Control not explicitly stated Individuals: Intervention n=1025; Control n=3205 Completed: Individuals: Intervention n=1025; Control n=3205 Age: Intervention: 11‐years: 12.8%; 12‐years: 16.4%; 13‐years: 17.7%; 14‐years: 18.3%; 15‐years: 17.0%; 16‐years: 17.7%; Control: 11‐years: 14.5%; 12‐years: 17.3%; 13‐years: 17.1%; 14‐years: 16.8%; 15‐years: 17.3%; 16‐years: 17.0% Gender: Intervention: Female 50.6%: n=520; Control: Female 51.1%: n=1631 Ethnicity: Intervention: Caucasian n=733: 71.7%; African‐American n=152: 14.9%; Native American n=24: 2.4%; Asian n=48: 4.7%; Hispanic/Latino n=31: 3.0%; Other n=34: 3.3%; Control: Caucasian n=2832: 89.1%; African‐American n=58: 1.8%; Native American n=85: 2.7%; Asian n=51: 1.6%; Hispanic/Latino n=76: 2.4%; Other n=76: 2.4% Recruitment means: Sampling frame used geopolitical units (GPUs); recruitment was conducted by telephone by Clearwater Research using modified random digit dial sampling |
|
| Interventions |
Theoretical basis: Modifiable factors to influence youth smoking Intervention description: Restriction on smoking in restaurants and/or bars (restriction in public places) Control description: No CIA policy were smoking areas were designated or not restricted; Participants who were not exposed to local CIA policies were considered to be in the control population Duration of intervention: Two years Intervention delivered by: Community level policies through the government |
|
| Outcomes |
Method of outcome collection: Telephone questionnaire conducted by Clear water research Pre specified outcomes: Parental smoking; close friend smoking, banning smoking in the home; monthly smoking Validation: None reported Follow‐up: Two years following intervention though 11‐time periods in total (across 6‐years): Baseline collection commenced in 2000 and follow‐up completed in 2006 (data collection occurred every 6‐months with the exception of survey 7); intervention was implemented in a total of 9 cities/countries by 2004 |
|
| Notes | Generalisability concerns: Targeted population may have caused bias toward null hypothesis: Authors state "The youth in the MACC sample were 16 or older at the time the first local CIA policy was established. Therefore our study may have missed the most critical period of the development of smoking behaviours between ages 10 and 15, resulting in a bias toward the null hypothesis." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention and control populations were selected based on which cities established local CIA policies commencing in 2004 |
| Allocation concealment (selection bias) | High risk | Allocation was based on who implemented CIA policies in 2004 |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Survey 7 is missing due to a gap in funding; additional 12‐year‐old cohorts were planned however they were not recruited due to funding limitations; this analysis includes data from individuals with a median of 6 surveys (max. 11) over the 6‐years of the study; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | Comparison cohort (n=604) was excluded from the analysis due to lack of local CIA policies; Authors report results form recent surveys in text which is different to those reported in the tables |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Analysis controlled for imbalances at individual and community level |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Analysis controlled for imbalances at individual and community level; Overall the demographic characteristics between intervention and control were similar with the exception of race/ethnicity and region of the state; There was a higher proportion of Caucasian youth in the control group (89% vs 72%) and more African‐Americans in the intervention group (15% vs 2%); More intervention participants lived in urban areas (47% vs 3%) or suburban areas (43% vs 33%) compared with control participants who mostly lived in rural areas (64%); Intervention communities had more college graduates (34% vs 23%) and a slightly higher median household income ($51 000 vs $48 000) All mean differences were statistically significant p<0.01 |
| Protection against contamination? | Unclear risk | Each study participant was assigned to intervention or control based on city of residence at each survey; Hence some contamination could have occurred if the control population visited cities with CIA policies in place |
| Selective recruitment of participants addressed? | High risk | n‐values are 3‐times greater in the control population in comparison to the intervention population |
Murray 1994.
| Methods |
Country: United States of America Design: Controlled Clinical Trial; Nested; Cluster Objectives: To reduce the incidence and of tobacco use in the three social influences conditions compared to that in the existing curriculum group and to reduce the prevalence rate, to be similar to that seen across Minnesota in the Two State Comparison Study. Study site: Schools, homes and communities state‐wide programmename: Minnesota‐Wisconsin Adolescent Tobacco‐Use Research Project (Four Group Comaprison Study) Methods of Analysis: Hierarchical ANOVA (to take account of the extra variation due to cluster sampling) Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: Clusters: n=112 schools Individuals: n=8992 student's enrolled in the sixth grade in April 1987 at baseline and n=7180 enrolled in seventh grade in April 1988 Recruited: Clusters: MSPP n=18; SFG n=20; MDEG n=20; EC n=23 Individuals: MSPP n=1632; SFG n=1694; MDEG n=2018; EC n=1836 Completed: Clusters: MSPP n=18; SFG n=20; MDEG n=20; EC n=23 Individuals: Year 1988 ‐ MSPP n=1542; SFG n=1631; MDEG n=1957; EC n=1744; Year 1989 ‐ MSPP n=1364; SFG n=1448; MDEG n=1784; EC n=1570; Year 1990 ‐ MSPP n=1266; SFG n=1352; MDEG n=1643; EC n=1489 Age: Mean years ‐ MSPP 11.8; SFG 11.8; MDEG 11.7; EC 11.8 Gender: % Male at baseline ‐ MSPP 50.0%; SFG 51.0%; MDEG 49.5%; EC 51.5% Ethnicity: Not explicitly defined Recruitment means: Letter to the superintendent followed by appointment to present study proposal; Once discussions complete a written agreement was signed by the PI and by the superintendent to confirm their negotiated responsibilities for the project; School based recruitment |
|
| Interventions |
Theoretical basis: Social influences model Intervention description: Intervention one:MSPP (Minnesota Smoking Prevention programme) ‐ 6‐lesson school curriculum based on the social influences model Intervention two: SFG (Smoke Free Generation) ‐ 3‐lesson school curriculum based on the Minnesota Smoking Prevention programme but shorter; it also used T‐shirts, posters and similar promotional items Intervention three MDEG (Minnesota Department of Education's Guidelines) ‐ Developed by the Department of Education and provided written guidelines and a workshop to help teachers adapt existing programmes to incorporate components of the social influences model Control description: Existing curriculum Duration of intervention: Maximum 6‐lessons over a 3‐year period Intervention delivered by: Teachers |
|
| Outcomes |
Method of outcome collection: Confidential classroom survey allowing individual members to be tracked Pre specified outcomes: demographic characteristics, weekly cigarette smoking, smokeless tobacco use, perceived tobacco use by models, exposure in schools to educational programmes related to tobacco use and other factors believed to be related to tobacco Validation: Expired air carbon monoxide Follow‐up: Three years: T1 Baseline (1987)/ T2 one year (1988)/ T3 two year (1989)/ T4 three year (1990) |
|
| Notes | Total funding approximately $2 million a year; funded from higher taxes on tobacco products as part of Minnesota State Legislation; Process measures: Most students reported exposure to between two and three of the four activities included in each measure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned but methods not described |
| Allocation concealment (selection bias) | High risk | Allocation not concealed, authors state "When a unit declined participation, the next unit on the randomized list was invited." |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Methods to account for missing outcome data not reported; Subject survey missing data not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement of yes or no |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | No significant differences among the four conditions ‐ analysis of covariance occurred |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | No significant differences among the four conditions ‐ analysis of covariance occurred |
| Protection against contamination? | Unclear risk | Possible contamination due to close proximity of intervention areas and media campaigns |
| Selective recruitment of participants addressed? | Unclear risk | Insufficient information to permit judgement of yes or no |
Pentz 1989.
| Methods |
Country: United States of America Design: Controlled Clinical Trial; Cluster; Nested; 8 schools randomly assigned to intervention or control, 20 schools assigned to intervention and 14 to control (based on school commitments) Objectives: To evaluate the effectiveness of a comprehensive community‐based drug prevention programme in reducing the prevalence of gateway drug use in adolescents Study site: Schools and communities in the greater Kansas City SMSA (population 1.3 million) programmename: Midwestern Prevention Project (MPP) Methods of Analysis: Logistic regression; School unit of analysis with all schools pooled for analysis; For parent data set individual was unit of analysis Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=15000 Recruited: Clusters: Cross‐sectional: Schools n=34; Remaining sample: Schools total n=42; Intervention n=24; Control n=18 (8‐schools were assigned randomly to programme or control conditions, 20 could reschedule existing programming and were assigned to the programme condition, and 14 did not have the flexibility to reschedule existing programming and were assigned to control condition) Individuals: 25% cross‐sectional sample of students selected randomly by classroom (n=3,371 average); Total sample size n=5065; Individually tracked n=1607 Completed: Individuals: n=5008 (1‐year); Individually tracked n=1350 (approximately) Age: Range 11 to 15‐years (plus parents) Gender: Females 83%; Males 17% Ethnicity: Students: 79% white; Parents 88% white Recruitment means: Population screened through SMSA's then recruited via school clusters |
|
| Interventions |
Theoretical basis: Social learning theory, transactional & systems theories of environmental change & communication theories Intervention description: Mass media coverage of drug prevention, included 16 television spots, 10 radio and 30 print media events throughout study period: Year‐1: 10 school & homework sessions; Year‐2: same as year‐1 plus a parent organisation, communication, and prevention practice programme; Year‐3: same as year‐2 plus community organisation training and networking; Year‐4: same as year‐3 plus promotion of local health policy change Control description: Delayed intervention control plus usual health education Duration of intervention: Two years Intervention delivered by: Teachers of science or health education and 4 student leaders for each class all given training |
|
| Outcomes |
Method of outcome collection: Self reported survey administered to students by trained data collectors; Self report survey for parents distributed to students in school in sealed envelopes, with a return envelope provided for posting Pre specified outcomes: Demographic characteristics, gateway drug use (cigarettes), and psychosocial variables related to drug use; prevalence rates; frequency of cigarette use ‐ last week, month; Cigarettes were rescaled to no use or any use in lifetime, last week and last month; Parent survey asked for reported cigarettes smoked in last week and last month by self, spouse, target child and next older child; rated importance of parent role, personal involvement, and discussion with child about preventing smoking Validation: Measure of CO in expired air Follow‐up: Baseline and one year post completion of final intervention programme 1984 ‐ 1986; The delayed intervention control was implemented in 1987 ‐ 1991 |
|
| Notes | Authors mentioned some concerns regarding reliance of self‐report measures to estimate programme effects | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Eight schools were randomly assigned, however due to scheduling flexibility after the start of the school year the remaining schools were assigned to programme or control |
| Allocation concealment (selection bias) | High risk | Most schools were assigned rather than randomized to programme or control condition |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | Data collection was performed by trained data collectors who were independent of the programme. However attempts to blind outcome assessors not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Smokers in both experimental conditions were more likely overall to be absent after baseline compared with nonusers p<0.05 ‐ logistics regression analysis was used; Missing outcome data likely to be related to true outcome; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | Lifetime cigarette use only reported as ‘individual mean percentages of lifetime drug use by demographic predictors at baseline’ ‐ as such they can not be meta‐analysed |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Demographic variables were used as covariates to adjust for potential imbalances; Initial regression analyses indicated no baseline differences in prevalence rates of lifetime drug use or demographic characteristics between the 42 schools and the additional 8 schools; Potential imbalances between intervention and control schools have not been clearly reported; No statistically significant baseline differences between random and scheduled schools |
| Comparability of intervention and control group characteristics at baseline addressed? | High risk | "...possibility of non‐equivalence of study groups, since the majority of schools were assigned to programme or control conditions based on administrator flexibility..." |
| Protection against contamination? | Unclear risk | It is unclear what intervention the controls received; Those schools that were unable to reschedule existing conditions were assigned to control, which would assume ‘usual practice’ however it is likely that they received the mass media component of the intervention |
| Selective recruitment of participants addressed? | High risk | Imbalance in number of clusters between experimental and control groups, (intervention n=24; control n=18); Schools selected into intervention and control based on scheduling flexibility |
Perry 1994.
| Methods |
Country: United States of America Design: Controlled Clinical Trial; Nested; Cluster; Cross‐sectional design Objectives: To evaluate the effect on adolescent smoking prevalence of combining a schools based health education programme with a community‐wide, population‐wide, cardiovascular disease risk factor reduction intervention Study site: Schools and communities in 2‐north central USA cities (population approximately 100,000 each) programmename: Class of 1989 study: a sub‐study of the Minnesota Heart Health Program (MHHP) Methods of Analysis: ANCOVA; Regression adjustments within and between communities to address variance; covariance adjustment for age and sex, and in 1987‐1989, for parental occupation & for pre‐intervention differences; Communities assigned to study conditions, schools unit of analysis; Intervention effect tested against school variance Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: Six Minnesota communities; All students in each community were eligible to participate ‐ no other information provided Recruited: Cluster: n=2 Minnesota communities; Schools n=13 between 1883‐86 and n=7 between 1987‐89 Individuals: n=2401 at baseline Completed: Cluster: Not explicitly stated; assumed n=2 Minnesota communities; Schools n=13 between 1883 to 1986 and n=7 between 1987 to 1989 Individuals: Matched cohort ‐ 1983 n=2401; 1984 n=2103; 1985 n=1943; 1986 n=1640; 1987 n=1578; 1988 n=1421; 1989 n=1080 Age: mean= 11‐years Gender: Not explicitly stated Ethnicity: Not explicitly stated Recruitment means: All eleven year‐olds from the 13 schools within the 2 communities were eligible for recruitment |
|
| Interventions |
Theoretical basis: Social Learning theory and theory developed for the MHHP Intervention description: School ‐ education on short term consequences, reasons, alternative options, influences of advertising, peer and adult role models, skills to resist social influences; public commitment to abstain; Community ‐ Population‐wide community organisation & education on cardiovascular risks including population risk factors, community organisation and citizen task forces, adult education, health education using mass media and continuing education of health professionals Control description: No school based programmes and no community education Duration of intervention: Education programme 3‐years; Community‐wide intervention 5‐years Intervention delivered by: School activities led by trained peer (same‐age) leaders, elected by classmates and who were effective communicators of the social and psychological messages of the programme |
|
| Outcomes |
Method of outcome collection: Project staff, trained in classroom administration, administered the survey during a class period; Standardised questions with acceptable reliability and validity, used to obtain information including prevalence of weekly smoking and self‐reported smoking history Pre specified outcomes: A smoking intensity score was created from the self‐reported measures ‐ It related the average daily and weekly smoking, and smoking history (test‐retest correlation was .99) Validation: Saliva thiocyanate levels were measured in a random sample of students in half the classes (n=1076) in 1986 Follow‐up: Five years; Pre‐test 1983; Follow‐up between 1984 ‐ 1989 |
|
| Notes | Funded by the National Heart, Lung & Blood Institute; Encouraged community leaders to become involved in the development & support of the programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Groups selected not randomized |
| Allocation concealment (selection bias) | High risk | Groups selected |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of smoking status for those students missing from follow‐up cohort or cross‐sectional surveys; 55% of the intervention community compared with 32% of the comparison community were available for follow‐up; higher level of smoking in the reference community as a result of those missing at the time of measurement; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | Authors report a post‐hoc decision to report data as pooled for gender; daily smoking mentioned as being collected, but no data was presented |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | No differences at baseline for either weekly smoking prevalence or smoking intensity |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | At baseline both smoking prevalence and intensity were slightly higher in control community; separate analyses of covariance in the cohort sample adjusting for these differences (age, gender, parental job class) required no changes in the interpretation of the data |
| Protection against contamination? | Low risk | Communities were selected to be a certain distance from each other to control for contamination |
| Selective recruitment of participants addressed? | Unclear risk | n‐values not presented between groups |
Perry 2003.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Nested; Cluster Objectives: To evaluate whether the middle and junior high‐school D.A.R.E. curriculum and an expanded D.A.R.E. Plus at the middle and junior high‐school level would reduce and prevent tobacco, alcohol, and marijuana use and violent behaviour among seventh and eighth grade students Study site: Schools and neighbourhoods, primarily in Minneapolis‐St Paul programmename: D.A.R.E. (Drug Abuse Resistance Education) and D.A.R.E. PLUS (Plus programmes on drug use and violence) Methods of Analysis: Growth curve analysis Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: n=6728 individuals Recruited: Clusters: Intervention one n=8; Intervention two n=8; Control n=8 Individuals: Intervention one n=2226; Intervention two n=2221; Control n=1790 Completed: Clusters: Intervention one n=8; Intervention two n=8; Control n=8 Individuals: Intervention one n=2108; Intervention two n=2518; Control n=2635 Age: Not explicitly stated: Seventh grade (baseline) Eighth grade (follow‐up) Gender: Total sample only: 51.6% male Ethnicity: White 67.3%, African American 7.5%, Asian American 12.7%, Hispanic 3.6%, American Indian, 4.0%, mixed/other racial groups 4.9% Recruitment means: School districts in Minnesota that had middle and junior high‐schools with a seventh grade population of at least 200 were targeted for sufficient statistical power; If a school was interested in participating, the appropriate police department was contacted |
|
| Interventions |
Theoretical basis: Social influences model Intervention description: Intervention one: D.A.R.E. ‐ 10‐session curriculum providing skills in resisting influences to use drugs and handling violent situations taught by trained police officers Intervention two: D.A.R.E. Plus ‐ classroom based peer‐led, parental involvement programme entitled “On the VERGE”: Once per week for 4‐weeks, designed as a teen magazine; This programme was led by peer leaders and students completed ‘home team’ work with their parents; Students also participated in a theatre production in their classrooms; 10‐postcards were sent out to parents every 6 to 8‐weeks, and 3 during the intervention period; 8 community organisers were hired to create and facilitate the extracurricular activities for the second component of D.A.R.E.; The final component involved neighbourhood action teams to address neighbourhood and school‐wide issues relating to drug use and violent behaviour Control description: Delayed programme commenced at end of study period (2001) i.e., usual practice control Duration of intervention: Ten weeks for D.A.R.E. and an additional 4‐weeks of classroom activities for D.A.R.E. Plus, plus extracurricular activities and 10‐postcards mailed to parents every 6‐ to 8‐weeks; September /October 1999 to April/May 2001 (2‐years) Intervention delivered by: Taught by trained police officers; Officers who were teaching D.A.R.E. in the D.A.R.E. Plus condition were provided an extra 2‐hour training by the research team on interactive teaching methods; VERGE delivered by trained teachers; classroom activities were primarily led by elected and trained peer leaders; students completed home team work with their parents; 8 extensively trained community organisers were hired to create and facilitate the extracurricular activities and neighbourhood action teams for the second and final components of D.A.R.E. |
|
| Outcomes |
Method of outcome collection: Self‐administered questionnaire Pre specified outcomes: Self‐reported tobacco use, amount of current use; behaviours and intentions related to the use of tobacco; outcome expectations concerning tobacco use; social support Validation: None reported Follow‐up: Two years |
|
| Notes | Generalisability concerns ‐ more effect for boys than girls | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned but not described |
| Allocation concealment (selection bias) | Unclear risk | Aallocation concealment not reported |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Students excluded from analysis due to contamination and drop‐out attrition had no outcome data reported on pre or post study completion; There is a potential for those subjects who did not complete follow‐up to be more likely to smoke; Adjustments were made in the statistical analysis for other missing data |
| Selective reporting (reporting bias) | Unclear risk | Some post‐hoc separation for gender in final analysis may have occurred however insufficient information to permit judgement of yes or no |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Unclear risk | Schools were matched at recruitment to have similar socioeconomic measures, drug use and size however no information provided for the recruited sample |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Schools were matched at recruitment to have similar socioeconomic measures, drug use and size; Authors state baseline ethnicity showed equivalency between study conditions however no information on other baseline characteristics provided for the recruited sample |
| Protection against contamination? | Low risk | n=92 students were identified as relocating between study conditions, as such they were excluded from analysis |
| Selective recruitment of participants addressed? | Unclear risk | Schools were targeted based on population size, followed by contact with the relevant police department; Most schools came from one area, the Minneapolis‐St Paul metropolitan region |
Perry 2008.
| Methods |
Country: India Design: Randomized Controlled Trial; Cluster Objectives: To examine whether and to what extent the psychosocial risk factors medicated the relationship between intervention components and participants tobacco‐use intentions; In other words, statistical mediation analysis was performed to investigate a) whether Project MYTRI altered the psychosocial risk factors as intended (action theory), and b) whether the changes in psychosocial risk factors were, in turn, responsible for altering students' tobacco‐use intentions (conceptual theory); The Satterthwaite method was used to compute the denominator degrees of freedom for the tests of the fixed effects; An unstructured covariance matrix was specified for defining random effects Study site: Schools (32 total) programmename: MYTRI (Mobilizing Youth for Tobacco‐Related Initiatives in India) Methods of Analysis: Series of regression equations; ANCOVA for baseline mediator and outcome measures as covariates in predicting the 1‐year follow‐up scores; Each model was adjusted for gender, grade, school type and region; ANCOVA was also used to handle repeated measures; The Akaike Information Criteria (AIC) and the chi‐square statistic were used to evaluate the overall fit of the model Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Clusters: n=93 schools available; n=68 schools approached Individuals: n=12484 at baseline; n=12075 at 1‐year; n=12752 at 2‐years Recruited: Clusters: n=32 schools (Intervention n=16; Control n=16); n=125 classrooms Individuals: Matched cohort n=8369 (31.5% attrition) (baseline and 1‐year) Completed: Clusters: At 1‐year: n=30 schools; At 2‐years n=30, however an additional 3 schools would not allow 10th graders to participate due to exams Individuals: At 1‐year: Individuals ‐ Control n=4360; Intervention n=4009; At 2‐year matched cohort for combined control and intervention n=3780 (26.9% of original cohort) Age: Mean sixth grade =11‐years; Mean eighth grade=12.8‐years Gender: Total population only: 51.6% male Ethnicity: Total population only: Indian (43.5% northern and 56.5% southern India) Recruitment means: Schools were selected based on their representativeness of the range of schools in Delhi and Chennai in terms of socioeconomic level, school type (Private versus Government), and gender (co‐ed, boys only, and girls only) |
|
| Interventions |
Theoretical basis: Social Cognitive Theory and other theories of youth health promotion: Action theory; conceptual theory; Social influences programme Intervention description: Four components: 7 Classroom sessions, 6 school posters, 6 parent postcards and peer‐led health activism; Peer leaders were involved in inter‐ and intra‐school activities at the school and community levels to make changes in those environments to reinforce the messages in the classroom and home; One component included creating tobacco free norms at school, in the home and in surrounding neighbourhoods Control description: Delayed intervention control Duration of intervention: Two years in total; intervention lasted for 4‐months with over 15‐hours of activities Intervention delivered by: Teachers and peer leaders who received prior training |
|
| Outcomes |
Method of outcome collection: Student survey data; Two‐person team conducted the survey ‐ self‐administered in pencil‐and‐paper Pre specified outcomes: Current tobacco use and intentions to use tobacco in the future; intentions to smoke tobacco and intentions to chew tobacco Validation: None reported Follow‐up: Two years: T1 baseline/ T2 one year/ T3 two years |
|
| Notes | Process measures were performed for the intervention ‐ extent and quality of intervention implementation varied between schools and classes; Three of 16 schools only partially implemented the classroom activities; 67% of the sixth and eighth grade cohort attended the inter‐school activities; Significantly higher attrition by tobacco users compared with non‐users possibly affecting generalisability | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned but not described |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Methods to account for missing outcome data (adjusted scale scores) were described; Attrition rates did not differ between study arms; Subject survey missing data were removed from analysis; |
| Selective reporting (reporting bias) | High risk | Two year follow‐up data reported in a way which could not be meta‐analysed (change scores) and final n‐values for intervention and control groups not reported separately |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Only one marginally significant difference between the two study conditions ‐ intervention condition had more reasons to use tobacco than the control condition (p=0.060) |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Analysis of covariance occurred to adjust for baseline differences |
| Protection against contamination? | Unclear risk | Distance of intervention and control schools or movement of teachers/students between schools not discussed |
| Selective recruitment of participants addressed? | Unclear risk | Method of recruitment/inclusion within schools not discussed (i.e., unclear if all classes within school and all students participated in the survey) |
Piper 2000.
| Methods |
Country: United States of America Design: Controlled Clinical Trial with randomization of the control group only; Cluster; Nested; Non‐equivalent control group Objectives: To evaluate the effectiveness of an in‐school health promotion programme supplemented with family and community components, on adolescent behaviour (alcohol, tobacco, marijuana use, nutrition and sexuality); For tobacco use the aim was to prevent the onset Study site: Suburbs, small cities and towns in Wisconsin; Suburban areas 69% and non‐farm country settings 27% programmename: Healthy for Life Project (HFL) Methods of Analysis: ANCOVA or multiple regression equivalent; Individual group adjusted ANOVA, aggregation of scores to the classroom level and hierarchical modelling Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Not explicitly stated (22 middle‐schools initially recruited ‐ 1 released at last minute due to space restraints) Recruited: Clusters: n=21 middle‐schools; Intervention one Intensive n=6; Intervention two Age appropriate n=7; Control n=8 Individuals: n=2483; Intervention one: Intensive n=758; Intervention two: Age appropriate n=827; Control n=898 Completed: Individuals ‐ matched cohort: n=1981 at both grade six and nine (80% retention rate); Tenth grade response lower (68% of the original six grade sample); Tenth grade n=1677 (not matched cohort) Age: Range 11‐ to 15‐years Gender: Females 52%; Males 48% Ethnicity: White 92% Recruitment means: Schools |
|
| Interventions |
Theoretical basis: Social influences model of health promotion and prevention Intervention description: Intervention one: (age appropriate) ‐ School: 43‐minute lessons delivered daily for 4‐weeks in each of 3‐years; 54‐lesson curriculum involving: inoculation, use of peer leaders, family values, health advocacy, short term health effects, incentives to attend classes and complete assignments; Advertising and media influences; Public commitment; Peer norms; Parent orientation session prior to programme starting; Community: HFL community organiser for 6‐months of each of the 3‐years Intervention two: (intensive) ‐ School: as above for 'age appropriate' except that the 54‐lesson curriculum was delivered in one sequential 12‐week block to 7th grade students; Community: as above for 'age appropriate' except that HFL community organiser assisted the community for 15‐months Control description: Standard health education Duration of intervention: Intervention one: HFL programme 54‐lesson curriculum: 43‐minute lessons delivered daily for 4‐weeks in each of the 3‐years Intervention two: HFL programme 54‐lesson curriculum: 43‐minute lessons delivered in one sequential 12‐week block to 7th grade students Intervention delivered by: HFL was team taught by a teacher hired, trained and supervised by the research team; This teacher was paired with a teacher from participating schools |
|
| Outcomes |
Method of outcome collection: Annual self‐report survey administered in classroom setting by research staff with teachers present, of students' health related behaviour Pre specified outcomes: Substance use behaviour; past month tobacco use; several proximal outcomes related to the social milieu of substance use were also examined; perceptions of peers use/norms Validation: Measurements of CO in expired air; Bogus pipeline measures Follow‐up: Three years: annually from grade 6 to grade 10 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 'Cluster randomized control group design nested within two self‐selected treatment options'; Schools chose between age appropriate & intensive intervention, randomized to that intervention or control; Schools blocked on level of baseline substance use |
| Allocation concealment (selection bias) | High risk | Intervention arms self‐selected, control group randomized, however methods not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analysis of survey data in grades 7 and 8 not reported as authors state these are intermediate to the Age Appropriate treatment conditions; Tenth grade samples under‐represented subjects from the intensive condition due to an inability to schedule in‐school surveys in 2 intensive and 1 control school; The subsequent mail out surveys returned lower response rates; Authors decided not to measure knowledge change, however no further information provided; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | Three "intensive schools" were added after baseline measures taken; Post‐hoc analysis conducted due to high attrition rate in the tenth grade cohorts ‐ authors decided to treat these as separate samples |
| Other bias | High risk | Authors state they found significant differences between the different methods of analysis used for the same data; As such they have presented the data with "...the least amount of bias in the estimates of the standard errors due to the design effect" |
| Imbalance of outcome measures at baseline addressed? | Low risk | Blocking design used which ensured that schools at the extreme levels of substance use were proportionately assigned to treatment and control conditions |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Analysis of covariance occurred; Small but significant between‐group differences existed in percentage of students living with 2‐parents, parental education, and mother's full‐time work status (p<0.05); Authors state that the 3‐groups of schools were equivalent on most demographic characteristics; Of the 7‐variables presented in table 1, 4 had statistically significant differences |
| Protection against contamination? | Unclear risk | Authors state the control schools were provided the opportunity to receive the HFL programme for a subsequent cohort of students; Hence, potential contamination as the study was over 3‐years, teachers could distribute the curriculum within other classes and/or students could move between schools |
| Selective recruitment of participants addressed? | High risk | Authors present only unadjusted data (raw data) though their protocol includes adjustment; Three different analysis methods were conducted for all data; Authors present only the significant results obtained by the different methods of analysis |
Schinke 2000.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Cluster, Non‐equivalent control group; Nested Objectives: To evaluate the effect on Native American youth of school or school and community based interventions for preventing substance abuse (alcohol, tobacco, smokeless tobacco and marijuana) Study site: n=27 tribal or public schools on 10‐reservations in 5‐states programmename: None reported Methods of Analysis: ANOVA, no correction for intra‐class correlation. Scheffe post‐hoc multiple comparison tests Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Clusters: n=10 reservations in North and South Dakota; n=27 tribal and public schools Recruited: Clusters: n=10 reservations in North and South Dakota; n=27 tribal and public schools Indivuals: n=1396 Completed: Total population only ‐ Individuals: T1 n=1396; T2 n=1374; T3 n=1329; T4 n=1268; T5 n=1199 Age: Mean 10‐years at baseline Gender: Female 49% Ethnicity: Native American Recruitment means: Schools |
|
| Interventions |
Theoretical basis: Social influences/ resistance skills training with cultural tailoring Intervention description: Intervention one:School only ‐ Culturally tailored instruction with skills modelling by older peers, and rehearsal; Problem solving, personal coping and interpersonal communication; Emphasis on local cultural traditions counter to substance abuse Intervention two: School and community ‐ As 1 + mobilization of Native American constituents including families, teachers, school guidance counsellors, neighbourhood residents, law enforcement, commercial establishments; Activities to raise awareness of substance abuse prevention, e.g. media releases, flyers and posters, meetings for parents and others, poster‐making, mural painting, skits Control description: No intervention Duration of intervention: 15 x50min sessions during one school term and semi annual two session boosters Intervention delivered by: Not explicitly stated: assumed teachers, parents, school counsellors, law enforcement and commercial establishments |
|
| Outcomes |
Method of outcome collection: Questionnaires (no further details) Pre specified outcomes: Use of cigarettes (Smoking defined as 7 or more cigarettes in prior week); smokeless tobacco Validation: Saliva samples collected for cotinine; Only a small proportion analysed; Correlation only 0.53 but no information about levels of misreporting Follow‐up: Three years post‐intervention (or 3.5‐years post recruitment): T1 baseline/ T2 six months/ T3 one year/ T4 two years/ T5 three years |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized using a random numbers table on a spreadsheet ‐ data obtained from contact with authors |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Cotinine measurements collected but not all were tested, however those that were tested were not reported in this paper; Subject survey missing data were removed from analysis |
| Selective reporting (reporting bias) | Unclear risk | Post‐hoc analysis for self‐reported substance use was conducted to assess differences by study arm using the Scheffe multiple comparison test; It is unclear if this method of testing was pre‐determined at the protocol stage |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Students did not differ among the 3‐arms for ‘subject’s use of cigarettes’ |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Analysis of covariance occurred for imbalances |
| Protection against contamination? | Unclear risk | Authors state the likelihood of contamination between and among intervention and control arms is small; However this can not be ruled out |
| Selective recruitment of participants addressed? | Unclear risk | Eligible individuals prior to recruitment not stated; Methods of recruitment not stated |
Schofield 2003.
| Methods |
Country: Australia Design: Randomized Controlled Trial; Nested; Cluster Objectives: To demonstrate whether the HPS intervention led to lower uptake of smoking, and improved knowledge and attitudes among the cohort of students in intervention schools compared with control schools, after controlling for pre‐test smoking and other confounders Study site: Public secondary‐schools in the Hunter Region of New South Wales, Australia programmename: The Hunter HPS Project (Health Promoting Schools) Methods of Analysis: Exploratory factor analysis using principal components method and varimax rotation was performed; factor loading of 0.5; Cronbach's alpha coefficients for standardised variables; Kaiser's measure of sampling adequacy (MSA) estimated the degree of inter‐correlations among items Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=31 school clusters Recruited: Clusters: Intervention n=12 schools; Control n=12 schools Individuals: Intervention n=2573; Control n=2268 Completed: Clusters: Intervention n=12; Control n=10 schools Individuals: Intervention n=1007; Control n=845 Age: Total sample only: Year 7 n=965; Year 8 n=980 Gender: Total sample only: Female n=1011; Male n=841 Ethnicity: Total sample only for parents ethnicity: Both Australian n=1361; One Australian n=204; Other n=287 Recruitment means: Schools ‐ No further details |
|
| Interventions |
Theoretical basis: Community organisation theory; Peer influences model Intervention description: Formal school curriculum; information leaflets and bi‐weekly school newsletters for parents, letters to tobacco retailers, smoke‐free policy development, encouragement of non‐smoking parents, peers and teachers as role models, peer influences programmes and incentive programmes; Plus additional health promotion activities including drama skit performed by students and poster competitions to promote World No Tobacco Day; Training workshops, regular newsletters, quarterly reports and information resources such as computer interactive programmes were also available to schools Control description: Control schools were not offered any of the resources or actions to reduce smoking; however if they requested assistance, then the project team offered support for other health‐related issues and promised smoking‐specific support at the completion of the study period Duration of intervention: Two year duration; Intensity not specified Intervention delivered by: Each school had a liaison officer responsible for introducing a minimum set of actions; Teachers, parents and peers also delivered interventions |
|
| Outcomes |
Method of outcome collection: Surveys were completed in classrooms under supervision of teaching and research staff. Surveys were anonymous and matched on gender, age and school Pre specified outcomes: Smoking behaviour; smoking of significant others, influences on smoking, knowledge about smoking, attitudes toward smoking Validation: None reported Follow‐up: Two years |
|
| Notes | Process measures reported: Range between 8% ‐ 100% (n=1 to 12) of schools implemented the various intervention programmes; Some concerns about efficacy of intervention delivery | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned but not described |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Two control schools refused to participate ‐ time of drop out unclear; higher proportion of smokers were lost to follow‐up compared with non‐smokers |
| Selective reporting (reporting bias) | Unclear risk | All tabular data presented as combined intervention and control or not in a way that can be meta‐analysed; Statistical analysis for intervention effectiveness changed based on preliminary analysis of results; Subject survey missing data not reported |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | High risk | Control group had a higher smoking rate at baseline compared to intervention group with 10.5% versus 7.8% respectively |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Baseline characteristics not separated for intervention and control groups |
| Protection against contamination? | Unclear risk | Authors state “...some schools who may have been enthusiastic and committed to the HPS approach may have been randomized to the control group, thus potentially contaminating the study.” |
| Selective recruitment of participants addressed? | Unclear risk | Methods of recruitment not described |
St Pierre 1992.
| Methods |
Country: United States of America Design: Controlled Clinical Trial; Pre‐/Post‐test, non‐equivalent group design with multiple post‐tests Objectives: To evaluate the effectiveness of a drug abuse prevention programme (alcohol, cigarette, smokeless tobacco, marijuana, sexual activity and cocaine) modified for use in Boys and Girls Clubs, with and without 2 year booster programmes Study site: Boys and Girls Clubs in economically deprived cities (populations 17,000 to 630,000) or in rural areas programmename: Stay SMART Methods of Analysis: ANCOVA and logistic regression; Clubs unit of allocation, young person unit of analysis; Analyses controlled for initial differences and attrition Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=150‐clubs Recruited: Clusters: Intervention one: n=5; Intervention two: n=5; Control n=4 Individuals: Intervention one: n=129; Intervention two: n=121; Control n=127 Completed: Clusters: Intervention one: n=5; Intervention two: n=5; Control n=4 Individuals: Intervention one: n=52; Intervention two: n=54; Control n=55 Age: Range 13‐ to 16‐years Gender: Total population only: Males 78%; Females 25% Ethnicity: Total population only: White 45%; Black 42%; Hispanic 14% Recruitment means: Boys and Girls Clubs in both prevention groups were purposely selected from the 10‐clubs that were demonstration sites in Boys and Girls Clubs of America's original pilot testing of its SMART Moves prevention programme immediately prior to this study; Each Boys and Girls Club in the two treatment groups extended an invitation to all the 13‐year‐old members in their Clubs until they reached a total of approximately 24 youths for the programme |
|
| Interventions |
Theoretical basis: Social learning theory; Botvin's (1983) Life Skills Training Program adapted for use in youth clubs from a schools based programme Intervention description: Intervention one: Stay SMART only ‐ adapted from a school based curriculum with 12‐sessions covering drug prevention, resistance skills, decision making, social and communication skills Intervention two: Stay SMART plus booster ‐ SMART Leaders I and SMART Leaders II for those completing the Stay SMART programme Control description: No prevention programme Duration of intervention: Intervention one: Stay SMART 3‐months; Intervention two: Stay SMART plus booster programmes 27‐months Intervention delivered by: Prevention programme leaders trained annually |
|
| Outcomes |
Method of outcome collection: Self reported confidential questionnaires administered by prevention project staff or club staff members, measured multiple items relating to drug use Pre specified outcomes: Cigarette‐related behaviour; knowledge concerning drug use; attitudes ‐ social benefits of using (positives); frequency of drug use (1 indicated never having tried the drug and 6 indicated engaging in the drug behaviour frequently); intention to use; knowledge of health consequences; prevalence by teenagers; prevalence by adults; chewing tobacco/snuff use Validation: None reported Follow‐up: Two years three months: T1 baseline/ T2 three months/ T3 fifteen months/ T4 twenty seven months |
|
| Notes | Clubs in intervention groups were chosen from clubs which were demonstration sites for the pilot testing of SMART Moves, a prevention programme delivered immediately prior to this study; Some process measures reported; Some generalisability concerns as those more at risk of experimenting with cigarettes are more likely to opt out of the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Clubs were “...purposely selected...” not randomized |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed; Potential influence due to geographical randomization non‐concealed in a community setting |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Pre‐specified outcome data not reported (e.g. intention to use, prevalence of peers and adults and attitudes) Items were deleted from the attitude scales as authors state “...they had relatively low adjusted item‐total correlations and the alpha would increase if the item was deleted. However, for these scales, the reported results are not substantially changed if the deleted items are included in the scales.” Smoking status in attrition subjects said not to be significant in comparison to retained subjects, however no other data presented; No attrition mentioned for those participants approached by the clubs but declined participation in the research; Subject survey missing data were deleted if lacking in correlation |
| Selective reporting (reporting bias) | High risk | Analyses reported with only the significant covariates included; It is unclear if the decision to set the alpha at .10 for significance was decided pre or post‐hoc; Post‐hoc methods were used to evaluate cigarette‐related behaviour; Data presented in a way which could not be meta‐analysed (means not reported with standard deviations) |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Analysis of covariance occurred (ANCOVA), with condition as the independent variable, scores for the 3 post‐tests as the levels of repeated measures and pre‐test score, gender, age and race/ethnicity as the covariates |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | A significant difference was observed between groups, for the participants present at all four measurements for age and ethnicity however these were adjusted in the analysis |
| Protection against contamination? | High risk | Authors state that the Boys and Girls Club setting in which the programmes were implemented may its self have produced a ‘booster programme’ effect for both prevention groups, thus making the two treatment groups similar; 87% of the SMART Only and 87% of the controls reported they learned about alcohol and other drugs from some type of prevention programme at school; Boys and Girls clubs in both prevention groups were purposely selected from the 10 clubs that were demonstration sites in Boys and Girls Clubs of America’s original pilot testing of its SMART Moves prevention programme immediately prior to this study; As such the intervention group’s ‘pre‐test’ results may have been contaminated through receiving the pilot intervention |
| Selective recruitment of participants addressed? | High risk | Intervention clubs were selected based on organisational capabilities; Control clubs were selected by investigators to be similar in demographic characteristics and socioeconomic factors to that of the treatment clubs; The intervention clubs extended the invitation to 13‐year‐old members until they reached a total of approximately 24 youths and 30 youths in the control ‐ potential for the clubs to selectively recruit participants in the evaluation, imbalance in cluster sizes between intervention and control |
Stevens 2002.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Cluster; Nested Objectives: To prevent early adolescent health risk behaviours and to maintain or improve safety behaviours, we compared the effects of 2 interventions, delivered through paediatric primary care practices Study site: Paediatric primary care practices in Massachusetts, New Hampshire, and Vermont programmename: Dartmouth Prevention Project Methods of Analysis: Logistics regression analysis to control for baseline factors including child's age, parental education, family income, gender of child, parent's marital status, child's having friends who drink, parental high stress and low self‐esteem, and parental drinking problems; unadjusted t‐tests and chi‐squared tests Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=4096 families Recruited: Clusters: n=12 paediatric practices Individuals: n=3496 agreed to participate and met the grade eligibility requirements and n=3145 completed both the children's and parents baseline questionnaires Completed: n=2183 completed all surveys: baseline, 12‐months, 24‐months and 36‐months Age: Intervention mean n=11 (+0.9); Control mean n=11 (+0.8) Gender: Intervention female 46%; Control female 50% Ethnicity: Not explicitly stated Recruitment means: Paediatric clinicians in 12 primary care practices attempted to recruit all families with fifth and sixth grade children who visited their practices for well‐child care during a 21‐month period |
|
| Interventions |
Theoretical basis: Office system's approach ‐ can enhance implementation of preventive health and screening activities in adult primary care practices; Based on the premise that the office as a whole delivers preventive health services; Actions by physicians are consistently reinforced with the activities of other office staff and written materials over time Intervention description: Alcohol and tobacco use: the family would talk and develop a family policy about alcohol and tobacco use; letter from clinician; subsequent office visits to clinicians to educate further; brochures, pens, card games, magnets carrying an intervention message; newsletters mailed (n=12 for parents and n=12 for children) including games, puzzles and quizzes Control description: Gun safety, bicycle helmet and seatbelt use: the family would talk and develop a family policy about safety issues; letter from clinician; subsequent office visits to clinicians to educate further; brochures, pens, card games, magnets carrying an intervention message; newsletters mailed (n=12 for parents and n=12 for children) including games, puzzles and quizzes Duration of intervention: Three years: Initiated during a health supervision visit Intervention delivered by: Paediatric primary care clinicians whom were supported through study staff via site visits, telephone calls, newsletters, and informational materials to the clinical sites and with regular scheduled visual and printed materials mailed to the families; Dr Olsen trained all alcohol/tobacco sites and Dr Boyle trained safety sites with 3‐hour sessions on site |
|
| Outcomes |
Method of outcome collection: Children and parents received self‐administered, 21‐page surveys to complete independently of each other and return by mail Pre specified outcomes: Tobacco use, school health programmes, child's perception of peer behaviours, and of parental support and control, ever smoking, and ever using smokeless tobacco Validation: None reported Follow‐up: Three years: T1 baseline/ T2 one year/ T3 two years/ T4 three years |
|
| Notes | Process Measures: Research staff conducted monthly audits of 10% or at least 20 participants’ medical charts; The number of office visits documented in the progress notes was compared with the number of office visits documented on the research project flow sheet; Parents and children were surveyed as the whether they read the newsletter; 95% of participating children had been seen for subsequent visits in the office; A random subgroup of 400 parents and 400 children from both intervention arms were interviewed individually after 12‐, 24‐ and 36‐months to determine changes in topics discussed by families, policy setting and recall of clinician advice; In the annual survey, children were asked to recall whether they had visited the doctor in the past year and whether the doctor or nurse had discussed any prevention topics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Assigned within matched pairs using computer‐generated pseudo‐random numbers; Pseudo‐random unclear |
| Allocation concealment (selection bias) | Unclear risk | Sequence generation not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The institutional review board did not allow data to be collected on potentially eligible families who did not sign an informed consent; 53% of approached families completed all time points in the study (n=2183 of n=4096); Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | No n‐values provided for separate intervention arms for follow‐up outcomes; Outcomes reported incompletely so that they can not be meta‐analysed |
| Other bias | Low risk | No other risks of bias identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | There were no notable differences across intervention groups |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | The alcohol and tobacco intervention group of children was slightly more female (50% vs 46%; p=0.04). However gender was adjusted for in all subsequent analyses |
| Protection against contamination? | Unclear risk | Insufficient information presented to permit a judgement of yes or no |
| Selective recruitment of participants addressed? | Unclear risk | As participants were recruited by clinicians in cluster settings, it is unclear if recruitment biases occurred |
Sussman 1998.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Cluster Objectives: To evaluate the effectiveness of a school based programme, including school‐as‐community component, to prevent drug abuse (cigarette, alcohol, marijuana and hard drugs) in older, high‐ risk youth Study site: Continuation high‐schools (see notes) from a 5‐county region in southern California programmename: Project Towards No Drug Abuse (PTND) Methods of Analysis: ANCOVA, with pre‐test used as covariate and condition as the grouping factor ‐ trend analysis; Issues of cluster randomization addressed (fixed random & interclass correlation components) Adjustment made for clustering: Yes |
|
| Participants |
Eligible for study: n=3813 students from 29 school districts within 5 country regions of Southern California Recruited: Clusters: n=21; Intervention school plus community n=7; Intervention school only n=7; Control n=7 Individuals: n=1578; Intervention school plus community n=533; Intervention school only n=571; Control n=474 Completed: Clusters: n=21; Intervention school plus community n=7; Intervention school only n=7; Control n=7 Individuals: Totals ‐ T1 n=1074; T2 n=1047; T3 n=725 Age: Total ‐ Range 14‐ to 19‐years (mean 16.7) Gender: Total ‐ Male 62%; Female 38% Ethnicity: White 37%, Latino 46%, Asian Americans 4%, African Americans 8%, Native Americans 3% Recruitment means: Co‐operating districts from 5‐country regions in Southern California: schools with atypical student enrolment size (fewer than 50 or more than 500) were excluded |
|
| Interventions |
Theoretical basis: Aspects of social influences (self‐control, effective listening, effective communication), improve decision making; Motivational activities (attitudinal perspective taking, stereotyping, and health as a value) Intervention description: Intervention one: School based ‐ 9 lesson drug abuse prevention curriculum, of 3 x 50‐minute sessions per week for 3 consecutive weeks; Continuation community newsletter to intervention schools Intervention two: School plus community ‐ Same as for 'intervention one' plus weekly Associated Student Body Core (ASB) group meetings for 6‐months (6‐events per school) included job training, sports participation, drug‐free parties, and drug awareness week Control description: Standard care Duration of intervention: Three week programme for school intervention consisting of 9 lesson drug abuse prevention curriculum, of 3 x 50‐minute sessions per week; 'Intervention two' also included group meetings for 6‐months Intervention delivered by: Nine project staff health educators delivered the curriculum in the programme schools; they were trained by the project manager and approximately 2.5 hrs of training were completed for each session; School‐as‐community component delivered by a volunteer staff member under project‐created guidelines |
|
| Outcomes |
Method of outcome collection: Pre‐test data obtained through confidential questionnaires of self reported drug use, and demographic and psychosocial variables; Questionnaire administered by project staff not known to students; Post‐test data obtained by questionnaire(23%) or telephone survey (77%) Pre specified outcomes: Monthly smoking Validation: CO content of expired air Follow‐up: Five years; T1 one year/ T2 two or three years/ T3 four or five years |
|
| Notes | Generalisability concerns: continuation high‐schools are alternative high‐schools for young people up to age 18‐years, who are at risk of drop‐out of the school system because of functional reasons such as substance abuse; In continuation schools cigarette use is 57% compared to 24% in the comprehensive (usual) high‐schools in the area; The Associated Student Body, under teacher supervision is the student governmental body that (if it exists in the school) organises most student social events, service and political involvement in the local community | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned but methods not described |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Significant attrition ‐ Of n=3813 students on the roll at continuation schools, n=1578 (41%) were consented, as such by final follow‐up only n=725 (19%) were analysed; Subject survey missing data not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement of yes or no |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Analysis of covariance conducted |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Schools were blocked by characteristics, however data was not presented for intervention and control groups separately at baseline |
| Protection against contamination? | Unclear risk | Insufficient information to permit judgement of yes or no |
| Selective recruitment of participants addressed? | Unclear risk | Insufficient information to permit judgement of yes or no |
Tang 1997.
| Methods |
Country: Australia Design: Controlled Clinical Trial; Cluster Objectives: To evaluate a school and community intervention to prevent adolescent smoking Study site: Local government areas in Sydney programmename: Kickbutts Methods of Analysis: Logistic regression used for cohort of matched students Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=20 schools (for intervention only) unknown number for control group Recruited: Clusters: Intervention n=13; Control n=14 Individuals: Matched cohort ‐ Intervention n=2969; Control n=1598 Completed: Clusters: Intervention n=13; Control n=14 Individuals: Matched cohort ‐ Intervention n=2061; Control n=1009 Age: Not explicitly stated, year 7 and 8 Gender: Not explicitly stated, mixture of males and females Ethnicity: 5% intervention/ 17% control spoke language other than English at home Recruitment means: Schools within a single local government area invited to participate; Control schools selected with similar socio‐demographic profiles |
|
| Interventions |
Theoretical basis: Cognitive and behavioural skills and social influences Intervention description: School ‐ Five lesson package within 8‐weeks of baseline; parental support ‐ information, meetings, quit kit; Community ‐ Supply reduction: retailer education, surveillance and prosecutions, media, community forum Control description: Usual smoking prevention activities Duration of intervention: One year: Two months of school programme Intervention delivered by: Teachers and others |
|
| Outcomes |
Method of outcome collection: Self‐reported questionnaire; Parents also sent pre‐ and post questionnaires Pre specified outcomes: Smoking behaviour, attitudes and perceived benefits Validation: None Follow‐up: One year (differences in timing a baseline assessment for intervention and control schools adjusted for in analysis |
|
| Notes | Process measures: Some collected in teacher feedback ‐ 17 of 13 schools completed teacher feedback questionnaires. Only 2 teachers reported giving less than 5 lessons to teach the topic areas that should be covered; Inconsistency in delivery of the intervention components between schools ‐ 2 schools reported delivery of less than 5 components; authors state “The contribution of the retailer education strategy is not clear” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The LGA in Sydney was chosen for the intervention group by the investigators for geographical reasons; Groups with similar demographic profiles were selected for control |
| Allocation concealment (selection bias) | High risk | Study groups were selected by investigators for demographic reasons |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details provided regarding characteristics or smoking status for those subjects lost‐to‐follow‐up; 67.2% of the initial sample were maintained at follow‐up to become the matched cohort; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | Some post‐hoc adjustments made as the data for intervention schools were collected some months before data for the control schools, due to the rapid maturation effects of tobacco uptake in adolescence, dates of pre‐test and post‐test were later adjusted for in the analyses |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Unclear risk | Insufficient information presented to permit judgement of yes or no |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Insufficient information presented to permit judgement of yes or no |
| Protection against contamination? | High risk | Authors state that there was a possibility that “...there was little difference in the extent of exposure to the intervention components in the comparison and intervention group schools.” A comprehensive programme aiming to reduce the sale of cigarettes to minors was implemented in the control in northern Sydney during the closing stages of the study |
| Selective recruitment of participants addressed? | Unclear risk | Insufficient information presented to permit judgement of yes or no |
Vartiainen 1998.
| Methods |
Country: Finland Design: Controlled Clinical Trial; Cluster Objectives: To evaluate the long term effectiveness of a school and community based smoking prevention programme for young people, implemented simultaneously as an adult community‐wide cardiovascular disease prevention programme Study site: Schools and communities in North Karelia and in an adjoining province programmename: North Karelia Youth Project Methods of Analysis: Both individuals and schools used as units of analysis; ANOVA for differences between schools at outset, follow‐up and changes; Changes in intervention school pairs compared using t‐test and chi square test; analyses of covariance with baseline values as covariant Adjustment made for clustering: No |
|
| Participants |
Eligible for study: n=967 in seventh grade between 1978 ‐ 1982 Recruited: n=3 pairs of matched schools (1 urban, 1 rural) selected from 1 intervention and 1 control community Completed: Intervention one (Direct): T1 n=311 T2 n=294 T3n=260 T4 n=281; Intervention two (Community‐wide): T1 n=296 T2 n=283 T3 n=266 T4 n=268; Control: T1 n=290 T2 n=274 T3 n=260 T4 n=266 Age: 12‐ to 13‐years at baseline, aged 28‐years at follow‐up Gender: At T1 boys n=464; girls n=433 Ethnicity: Not explicitly defined Recruitment means: All 13‐year‐old students enrolled in 7th grade in participating recruitment sites and responding to baseline survey. Ten pupils from each school were chosen by one or more teachers to serve as positive role models to those who are likely to start smoking. Peers are given approximately 10‐hours of training. |
|
| Interventions |
Theoretical basis: Social influences model Intervention description: Intervention one: Community wide ‐ Cardiovascular risk reduction activities plus school programme ‐ 10 x 45‐minute smoking prevention sessions Intervention two: Direct Intervention ‐ Same as 'community wide' intervention plus a school programme of 5 sessions (in 8th grade) led by class teachers trained to disseminate new curriculum in North Karelia (local youth were also involved) Control description: No special intervention Duration of intervention: Two years of school educational interventions (1978‐1980); adult smoking cessation programme implemented 6‐years prior to youth project (1972), and continued throughout the 2‐year youth programme Intervention delivered by: Project team members carried out most of the intervention. Peer leaders given 10‐hours training to deliver anti‐smoking messages in classroom setting; teachers had 5‐hours training |
|
| Outcomes |
Method of outcome collection: Surveys undertaken by trained project nurse; Self‐reported questionnaire used in schools to obtain information including smoking behaviour and number of cigarettes smoked; Third, 4th and 5th post‐test surveys used postal questionnaires Pre specified outcomes: Smoking status including monthly, weekly and daily consumption; questionnaire for parents asking about health, health behaviour, knowledge, attitudes and problems at home; project nurse or local school nurse carried out physical examinations of students to assess cardiovascular risk Validation: None reported Follow‐up: Fifteen years: Pre‐test 1978; post‐test school surveys in 1980 & 1981; postal surveys 1982 & 1986 & 1993 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | No randomization occurred; block assignment used |
| Allocation concealment (selection bias) | High risk | Participants were assigned |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Matched cohorts; missing data accounted for by replacing data points with data from the preceding survey for smoking status outcomes |
| Selective reporting (reporting bias) | Unclear risk | Unmatched cohorts not included in publications |
| Other bias | Low risk | No other bias identified |
| Imbalance of outcome measures at baseline addressed? | Low risk | Baseline outcome data were balanced between groups |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Baseline characteristics for all groups were reported and similar |
| Protection against contamination? | Low risk | Contamination was unlikely |
| Selective recruitment of participants addressed? | Unclear risk | Insufficient information to permit judgement of yes or no |
Winkleby 1993.
| Methods |
Country: United States of America Design: Randomized Controlled Trial (for individuals); Cities not random Objectives: Examination of the trends in smoking prevalence in cities with and without a multi‐component cardiovascular disease prevention intervention, and, to evaluate if there is a diffusion effect to adolescents from community based adult anti‐smoking education interventions Study site: Four cities in California (population 35,000 ‐145,000) programmename: Part of the Stanford Five‐City Project Methods of Analysis: Not explicitly stated Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Not explicitly stated; however a mean response rate of 61% was achieved among 12‐ to 24‐year‐olds across the 4‐surveys Recruited: n=2605 for all surveys (64, 72, 52 and 56% response rates) Completed: Clusters: n=4 cities Individuals: Cross‐sectional sample only: Salinas n=612; Monterey n=457; Modesto n=590; San Luis Obispo n=946 Age: Range 12‐ to 24‐years; 12‐ to 15‐years n=651; 16‐ to19‐years n=629; 20‐ to 24‐years n=1,325; All individuals aged 12‐ to 74‐years eligible, separate results given for 12‐ to 24‐year‐olds Gender: Not explicitly stated Ethnicity: White 78%; Hispanic 15%; Other 7% Recruitment means: Households were randomly chosen from commercial directories. Individuals were recruited by mail, telephone, and when needed, in person and were invited to attend survey centres located in the four communities |
|
| Interventions |
Theoretical basis: learning theories of community based health education, community organisational change, and diffusion effect to adolescents from adult smoking prevention, cessation and maintenance intervention Intervention description: Young people: All 7th and 8th grade students (12‐ to 13‐years) had 7‐session smoking prevention programme, school based & peer led; multifactor cardiovascular disease risk reduction curricula; Adults: six year education intervention 1980‐1986, using media and direct education Control description: No intervention Duration of intervention: One year student education programme implemented in 4th year of adult education programme; Media/education intervention aimed at adults occurred over 6‐years Intervention delivered by: Older high‐school students employed to guide younger peers in school based programme |
|
| Outcomes |
Method of outcome collection: One hour long interview at study centre in which a trained nurse collected information about smoking in addition to other health information Pre specified outcomes: Prevalence of daily smoking Validation: Plasma thiocyanate and expired‐air CO level measured following interview Follow‐up: Two years ‐ intervention for young people administered in the 4th year of the adult evaluation ‐ Adult study ‐ Six year community organisation and education programme with 12‐year follow‐up period; Baseline and biennial cross‐sectional surveys, 1979 to 1990 |
|
| Notes | Main Stanford Five‐City Project was an adult orientated general cardiovascular disease risk reduction intervention Of the sample 10% of 19‐ to 24‐year‐olds were high‐school dropouts; smoking prevalence was significantly higher in this group (50%) compared to that of students completing high‐school (20%) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Cities selected however individuals are said to be ‘randomly chosen'; methods not described |
| Allocation concealment (selection bias) | High risk | Cities selected, individual participant allocation concealment not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Due to ‘cost constraints’ no adolescents or young adults were included in the third survey; No mention of how missing outcome data were addressed; Low response rate to surveys ‐ 61%; Subject survey missing data not reported |
| Selective reporting (reporting bias) | High risk | A cohort sample was also followed, but is not included in the analysis because of the small number of smokers who participated in all cohort surveys; Some possible post‐hoc analyses occurred for the analytical approach due to significant differences between cities and small number of minority respondents for ethnicity |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | High risk | Different levels of smoking prevalence were seen in the four cities at baseline |
| Comparability of intervention and control group characteristics at baseline addressed? | Low risk | Cities differed in racial composition and father’s level of education. Both coastal communities served as treatment cities; Analysis of covariance occurred to address these issues |
| Protection against contamination? | High risk | One control city banned public smoking in 1990, and subsequently had a large decline in smoking; The four cities are located within a 160km radius of Stanford University, possible contamination; One third of respondents did not live in the treatment cities during the entire intervention period, but adjusting for this did not change the results |
| Selective recruitment of participants addressed? | Unclear risk | Recruitment methods not described in detail. Cities were selected |
Winkleby 2004.
| Methods |
Country: United States of America Design: Randomized Controlled Trial; Cluster Objectives: To test whether high‐school students participation in advocacy activities related to the advertising, availability, and use of tobacco in their communities would prevent or reduce their own tobacco use Study site: Ten continuation high‐schools in northern California programmename: Intervention ‐ no name provided; Control ‐ PTND (Project Toward No Drug abuse) Methods of Analysis: Two‐tailed 2‐sample t‐tests Adjustment made for clustering: No |
|
| Participants |
Eligible for study: Not explicitly stated Recruited: Clusters: Intervention n=5; Control n=5 Individuals: Intervention n=375; Control n=438 Completed: Clusters: Intervention n=5; Control n=5 (continuation high‐schools) Individuals: Intervention n=367; Control n=431 Age: Intervention 17.0 (+0.2); Control 17.1 (+0.1) Gender: Intervention female 56.5%; Control female 43.7% Ethnicity: Intervention: Latino 43.5%; White 20.9%; Mixed ethnicity 15.3%; Asian/Pacific Islander 12.6%; African American 4.0%; Other ethnicity 3.7%; Control: Latino 40.8%; White 22.6%; Mixed ethnicity 16.0%; Asian/Pacific Islander 11.4%; African American 6.5%; Other ethnicity 2.7% Recruitment means: Schools |
|
| Interventions |
Theoretical basis: Social cognitive theory; Social learning and the empowerment theory Intervention description: Advocacy activities to counter environmental‐level smoking influences in their community; education, class room and community based sessions engaging students in activities to assess advertising, availability, and access to tobacco in their community; daylong advocacy institute to foster team building and develop advocacy skills; Advocacy activities conducted by the students included conducting surveys and gathering and analysing data, developing educational materials e.g. handouts about tobacco promotion to minors or descriptions of smoking laws for store owners, talking with people in power e.g. school administrators, store owners, physicians, or city council members and evaluating progress Control description: Learned about drug and alcohol abuse prevention; Modified version of 'Toward No Drug Abuse'; curriculum focuses on health motivation, social skills, and decision making regarding drug and alcohol use; video‐tapes, audio‐tapes, role‐playing, open discussions, and outside speakers Duration of intervention: Semester‐long programme, over 4 semesters; classes taught once per week during regular school hours for 60‐ to 90‐minutes Intervention delivered by: Staff of the Stanford Prevention Research Centre, Stanford, California |
|
| Outcomes |
Method of outcome collection: Survey administered by support staff who were not affiliated with teaching the curriculum; Administered during class time for baseline and post‐intervention (end of semester) surveys, but over the phone for 6‐month surveys Pre specified outcomes: Self‐reported smoking ‐ non‐smokers, light smokers, regular smokers; demographic background, level of involvement in community advocacy Validation: CO level readings Follow‐up: One year six months: 2000 through 2002; One year of intervention with six months follow‐up post‐intervention |
|
| Notes | Some process measures: intervention n=375 recruited, attended > 1 session n=367; control n=438 recruited, attended > 1 session n=431; Average exposure time 20.0‐hours for the treatment students and 19.2‐hours for the control students; During the second semester, the intervention was provided to only 6 continuation high‐schools (3 treatment, 3 control) because of the emergency sick leave of 2 main staff members; Only 1 class was offered each semester at each school: Lack of intervention intensity may have effected results; Some generalisability concerns as this population volunteered involvement | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Clusters were assigned by toss of a coin |
| Allocation concealment (selection bias) | Unclear risk | Toss of coin, but allocation methods not described |
| Blinding (performance bias and detection bias) For participants | High risk | Due to the nature of the intervention it is not possible to blind participants to allocation; however participants may not have been aware they were taking part in an evaluation where they were receiving the intervention |
| Blinding (performance bias and detection bias) For outcome assessors | Unclear risk | No mention of blinding for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Constructs related to social cognitive theory were not asked during the 6‐month follow‐up telephone survey because of their length; Non‐smoking and weekly‐smoking rates were different between participants and non‐participants; Subject survey missing data not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement of yes or no |
| Other bias | Low risk | No other biases identified |
| Imbalance of outcome measures at baseline addressed? | Unclear risk | Authors state that there were slight differences in baseline smoking between the treatment and control high‐schools ‐ extent not reported |
| Comparability of intervention and control group characteristics at baseline addressed? | Unclear risk | Authors state that there were slight differences in baseline socio‐demographic characteristics between the treatment and control high‐schools ‐ extent not reported |
| Protection against contamination? | Low risk | Unlikely that the control group received the intervention |
| Selective recruitment of participants addressed? | High risk | Students within the clusters were recruited on a voluntary basis from each continuation high‐school during the first week of each semester by study staff ‐ those who are smokers or more likely to be non‐compliant are less likely to take part |
Additional details of intervention components for each study is given in the table 'Description of the community intervention'
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aguirre‐Molina 1995 | Multicomponent community intervention ‐ the PACPY (Perth Amboy Community Partnership for Youth); Only one cluster per arm (Intervention Perth‐Amboy; Control Jersey City) |
| Aldinger 2008 | Multicomponent evaluation of 'health promoting schools' (HPS) in China; No control group |
| American Lung Assoc 2008 | Multicomponent community based intervention for prevention and cessation among 12‐ to 16‐year‐olds; No control group |
| Andrade e Silva 1991 | Multicomponent community based smoking prevention programme for young people; No smoking related outcomes for young people reported |
| Arora 2010 | Multicomponent community based prevention programme HRIDAY (Health Related Information Dissemination Amongst Youth) in disadvantaged urban slums in India. Community level had one cluster per arm. Once blocked within community intervention group had nine clusters, however control group only had one cluster |
| Baudier 1991 | Multicomponent community based smoking prevention and cessation programme for the whole population; No smoking related outcomes for young people reported |
| Berenson 2010 | Multicomponent community based Cardiovascular Health Promotion programme for a Parish County; No control group |
| Bowen 2002 | Multicomponent community based intervention (COMMIT) for adults, which was hypothesised to have ancillary impacts on the prevalence of youth smoking; No control group |
| Brownson 1996 | Multicomponent countywide community‐based cardiovascular disease risk reduction intervention; No smoking related outcomes reported for young people |
| Cain 1992 | Multicomponent statewide smoking prevention intervention; No smoking related outcomes reported for young people |
| Campion 1994 | Multicomponent, including mass media, nationwide smoking cessation campaign targeted at pregnant 15‐ to 24‐year‐olds; No control group |
| Carleton 1995 | Multicomponent citywide cardiovascular risk reduction programme; No smoking related outcomes reported for young people |
| Charlier 2009 | Multicomponent community trial to reduce the uptake of smoking among pre‐adolescents in a majority Maori and Pacific Isalnder population; No control group |
| Chen 2006 | Multicomponent intervention with 14 randomized communities to determine the long‐term effect of local youth access laws and policies; Four separate cohorts ‐ not matched |
| Clarke 1993 | Community based smoking cessation clinics, not young people specific, No smoking related outcomes reported for young people |
| Cruz 2008 | Three year smoking prevention programme created by the educational community in two secondary‐schools in Spain; Only 1‐cluster (school) per arm of study |
| Davidson 1994 | Multicomponent community intervention ‐ Smokebuster Club working through an existing youth organisation; Only one cluster per arm |
| Elder 1996 | Multicomponent community based tobacco education programme; No control group |
| Elder 1996b | Multicomponent, multi‐state cardiovascular disease risk reduction intervention for school children: No smoking behaviour related outcome measures reported for young people |
| Farquhar 1991 | Multicomponent community based cardiovascular disease risk factor reduction intervention; No smoking related outcomes reported for young people |
| Fawcett 1997 | Multicomponent community based coalitions to prevent alcohol, tobacco and other drug use in young people: No control group |
| Forster 1998 | Not a multicomponent intervention as defined for this review |
| Frith 1997 | Multicomponent nationwide smoking prevention intervention; no smoking related outcomes reported for young people |
| Harvey 1990 | Multicomponent community based smoking cessation intervention; No smoking related outcomes reported for young people |
| HEA 1994a | Assertiveness training provided for women youth workers, which would increase adolescent women's self‐esteem and allow girls to chose more responsibly whether or not to smoke: No smoking related outcomes reported |
| HEA 1994b | Intervention consisted of promoting dance/aerobics at youth centres in order to increase youth self‐esteem and thereby improve the ability of adolescents not to start smoking or to reduce tobacco use; The comparison group was not assigned ‐ it consisted of those not attending sessions ‐ inadequate control |
| HEA 1994c | That by attending "Health Drop‐in" centres young people would develop self‐confidence, assertiveness and increased self‐esteem and would thereby respond more effectively to their own health needs; The "comparison" group was selected after the intervention was started |
| Higgs 2000 | Multicomponent community based smoking intervention (Breathe Easy!); Only 1 cluster per arm, per follow‐up time period |
| Hunkeler 1990 | Multicomponent community based smoking cessation intervention; Not young people specific, no smoking related outcomes reported |
| Hymowitz 1995 | Multicomponent community based smoking cessation and prevention intervention; No smoking related outcomes for young people reported |
| Jason 2010 | Multicomponent community based tobacco prevention programme in 24 towns using PUP (possession‐use‐purchase) law enforcement compared with low‐levels of law enforcement; No true control group ‐ both contained the intervention but at different levels of intensity |
| Kaufman 1994 | Multicomponent culturally relevant programme amongst inner city African American adolescents in Chicago; Only 1 school cluster in the control group |
| Lazenbatt 1997 | Multicomponent smoking prevention intervention in young people; Retrospective comparison between Smokebuster club members and non‐members, of smoking related outcomes five years after enrolment in club; Inadequate control |
| Marin 1994 | Multicomponent, community based smoking cessation intervention for Spanish speaking Hispanics in San Francisco; Not young people specific, no separate smoking related outcomes reported for young people |
| Meshack 2004 | Multicomponent, media and community based anti‐smoking programme in 8 study communities assigned to varying intervention conditions; No baseline characteristics reported for intervention cohort; Not a matched cohort of students |
| Morgan 1994 | Multicomponent smoking prevention intervention for young people; Reports post‐test data only |
| Mudde 1995 | Multicomponent community based smoking cessation intervention, not young people specific; No smoking related outcomes reported for young people |
| Nater 1985 | Multicomponent community based cardiovascular disease risk reduction intervention with smoking cessation component; No smoking related outcomes reported for young people |
| Nilsson 2006 | Multicomponent, school and community based tobacco use prevention that targets adolescents (Tobacco Free Duo). Not a matched cohort of students |
| O'Loughlin 1995 | Multicomponent community intervention to reduce cardiovascular disease risk; Not young people specific, no smoking related outcomes reported for young people |
| Pentz 1989B | Multicomponent community based programme directed toward delaying the onset of cigarette smoking in adolescents in 8 schools in Kansas City; No true control group ‐ both contained the intervention but at different levels of intensity |
| Pierce 1998 | Multicomponent community based tobacco control programme; No smoking related outcomes reported for young people |
| Pomrehn 1995 | School based multi‐component smoking prevention intervention, including behavioural competitions between schools, student activation in one town and community activation in another town; Regular surveys of cohorts of children, no control group |
| Ramirez 1988 | Multicomponent community based intervention to prevent and reduce smoking; No smoking related outcomes reported for young people |
| Ramirez 1997 | Community based substance abuse prevention programme; No smoking related outcomes reported for young people |
| Reinert 2004A | Multicomponent media campaign and other sources of anti‐tobacco advertising to prevent smoking in youth including family, sports and other community events, advertisements, and the Internet; No baseline (pre‐intervention) results reported; No control group |
| Reinert 2004B | Multicomponent evaluation using the Youth Tobacco Survey (YTS) in three private, southern high‐schools in Mississippi, one intervention included teacher training in tobacco prevention and curriculum‐integrated materials only, the second using the same teacher training plus clubs after school involving health promotion activities and the third had classes as usual; Only one cluster (school) per arm of trial |
| Rigotti 2002 | Evaluation of the Massachusetts Tobacco Control programme (MTCP) in 11‐public colleges and universities (age 18‐ to 24‐years); No baseline characteristics reported pre‐intervention; No true control group ‐ (controls were students attending the colleges, but whom attended high‐school outside of Massachusetts ‐ only make up 15% of the total population) |
| Rohrbach 1994 | Part of Midwestern Prevention project; Results not compared with control |
| Schinke 1996 | Multicomponent smoking prevention intervention amongst Native American young people; No smoking related outcomes reported for young people |
| Shea 1990 | Description of five multi‐component community based cardiovascular disease risk reduction interventions; No smoking related outcomes reported for young people |
| Shipley 1995 | Community based smoking prevention contests; Not young people specific, no smoking related outcomes reported for young people |
| Sigfusdottir 2008 | Multicomponent community based Icelandic Model of Adolescent Substance Use Prevention; No control group |
| Slater 2006 | Multicomponent in‐school and community‐based media prevention project involving 16 communities over 2‐years; Seven of the 16 communities self‐selected to receive the school based intervention or no intervention. |
| Smith 2008 | Multicomponent tobacco prevention programme using ToPIC (Tobacco Prevention programme for Children) in students from Boys and Girls Clubs in 5 rural counties; No control group |
| Stein 1997 | School based tobacco use prevention programme and community‐based smoking cessation programme; No smoking related outcomes reported for young people |
| Stevenson 1998 | Multicomponent culturally appropriate alcohol, tobacco and other drug abuse prevention programme with Latino youth; No control group |
| Steyn 1997 | Multicomponent community wide cardiovascular risk reduction intervention; No separate results for young people |
| Tingen 2005 | Multicomponent community and school based tobacco prevention programme with children combined with a family tobacco cessation component by school nurses in conjunction with the initiation of a statewide toll‐free Quit Line; No control group; No outcome measures for 6th grade students reported |
| Tudor‐Smith 1998 | Multicomponent community based cardiovascular disease behavioural risk factor reduction intervention; No separate results for young people |
| van Teijlingen 1996 | Multicomponent, region‐wide intervention to prevent smoking in young people; No control group |
| Vicary 1996 | Multicomponent community based intervention to prevent alcohol, tobacco and other drug problems; No smoking related outcomes reported for young people |
| Wheeler 1988 | Community based smoking cessation programme using self‐help manuals, not young people specific; No smoking related outcomes reported for young people |
| Wickizer 1993 | Multicomponent health promotion interventions in 11 geographical areas; No smoking related outcomes reported |
| Wilson 2008 | Multicomponent community based Youth Empowerment Strategies (YES!) Project in 5 elementary schools; No control group |
| Wood 2009 | Multicomponent statewide youth smoking intervention (Smarter Than Smoking) including mass media, Internet, sponsorship, school initiatives, publications and advocacy in 10‐ to 15‐year‐olds in Western Australian Schools; No control group |
| Wu 2003 | Intervention multi‐component not specific to smoking prevention; No true control group |
| Yoffe 1994 | Multicomponent community based smoking prevention programme; No smoking related outcomes reported for young people |
Contributions of authors
Kristin Carson updated the protocol, reviewed the literature, identified studies for inclusion, performed data extraction on all included studies, entered and analysed data and updated the text of the manuscript.
Malcolm Brinn and Nadina Labiszewski performed second author data extraction, analysed data and updated the text of the manuscript.
Adrian Esterman directed the data analysis and also reviewed the manuscript.
Anne Chang reviewed the manuscript.
Brian Smith reviewed the manuscript and supervised the completion of the review.
Sources of support
Internal sources
Respiratory Medicine Unit, The Queen Elizabeth Hospital, Australia.
External sources
Australasian Cochrane Airways Group Network Scholarship, Australia.
Declarations of interest
None known
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Baxter 1997 {published data only}
- Baxter AP, Milner PC, Hawkins S, Leaf M, Simpson C, Wilson KV, et al. The impact of heart health promotion on coronary heart disease lifestyle risk factors in schoolchildren: Lessons learnt from a community‐based project. Public Health 1997;111:231‐7. [PubMed] [Google Scholar]
Biglan 2000 {published and unpublished data}
- Biglan A, Ary DV, Duncan TE, Black C, Smolkowski K. A randomized control trial of a community intervention to prevent adolescent tobacco use (Draft report 1998). Oregon: Oregon Research Institute. [DOI] [PMC free article] [PubMed]
- Biglan A, Ary DV, Smolkowski K, Duncan T, Black C. A randomised controlled trial of a community intervention to prevent adolescent tobacco use. Tobacco Control 2000;9:24‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Onofrio 2002 {published data only}
- Braverman MT, Moskowitz JM, D'Onofrio CN, Foster V. Project 4‐health develops program to curb youth tobacco use. California Agriculture 1994;48:39‐43. [Google Scholar]
- D'Onofrio CN, Moskowitz JM, Braverman MT. Curtailing Tobacco Use Among Youth: Evaluation of Project 4 Health. Health Education Behaviour 2002;29:656‐682. [DOI] [PubMed] [Google Scholar]
De Vries 2003 {published data only}
- Ariza C, Nebot M, Tomas Z, Gimenez E, Valmayor S, Tarilonte V, DeVries H. Longitudinal effects of the European smoking prevention framework approach (ESFA) project in Spanish adolescents. European Journal of Public Health 2008;18(5):491‐7. [DOI: 10.1093/eurpub/ckn050] [DOI] [PubMed] [Google Scholar]
- Connelly J, Green J, Lechner L, Mittelmark MB, Rigby AS, Roberts C. The European Smoking Prevention Framework Approach (ESFA) project: Observations by Six Commentators. Health Education Research 2003;18(6):664‐77. [DOI: 10.1093/her/cyg052] [DOI] [Google Scholar]
- Vries H, Dijk F, Wetzels J, Mudde A, Kremers S, Ariza C, Vitoria PD, Fielder A, Holm K, Janssen K, Lehtovuori R, Candel M. The European Smoking prevention Framework Approach (ESFA): effects after 24 and 30 months. Health Education Research 2006;21(1):116‐32. [DOI: 10.1093/her/cyh048] [DOI] [PubMed] [Google Scholar]
- Vries H, Engels R, Kremers S, Wetzels J, Mudde A. Parents' and friends' smoking status as predictors of smoking onset: findings from six European countries. Health Education Research 2003;18(5):627‐36. [DOI: 10.1093/her/cyg032] [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Leijs I, Charlton A, Vartiainen E, Buijs G, Clemente MP, Storm H, Navarro AG, Nebot M, Prins T, Kremers S. The European Smoking prevention Framework Approach (ESFA): an example of integral prevention. Health Education Research 2003;18(5):611‐26. [DOI: 10.1093/her/cyg031] [DOI] [PubMed] [Google Scholar]
- Vries J, Mudde A, Kremers S, Wetzels J, Uiters E, Ariza C, Vitoria PD, Fielder A, Holm K, Janssen K, Lehtuvuori R, Candel M. The European Smoking Prevention Framework Approach (ESFA): short‐term effects. Health Education Research 2003;18(6):649‐63. [DOI: 10.1093/her/cyg033] [DOI] [PubMed] [Google Scholar]
- Nahit E, Fielder A, Charlton A, Povey A. Smoking behaviour in year 8 pupils: Baseline characteristics of the UK ESFA longitudinal study. International Journal of Health Promotion and Education 2003;41(1):4‐13. [Google Scholar]
- Vartiainen E, Pennanen M, Haukkala A, Dijk F, Lehtovuori R, Vries H. The effects of a three‐year smoking prevention programme in secondary schools in Helsinki. European Journal of Public Health 2007;17(3):249‐56. [DOI: 10.1093/eurpub/ckl107] [DOI] [PubMed] [Google Scholar]
Elder 2000 {published data only}
- Elder JP, Campbell NR, Litrownik AJ, Ayala GX, Slymen DJ, Parra‐Medina D, Lovato CY. Predictors of Cigarette and Alcohol Susceptibility and Use among Hispanic Migrant Adolescents. Preventive Medicine 2000;31:115‐123. [DOI] [PubMed] [Google Scholar]
- Elder JP, Litrownik AJ, Slymen DJ, Campbell NR, Parra‐Medina D, Choe S, et al. Tobacco and alcohol use‐prevention program for Hispanic migrant adolescents. American Journal of Preventive Medicine 2002;23:269‐75. [DOI] [PubMed] [Google Scholar]
- Litrownik AJ, Elder JP, Campbell NR, Ayala GX, Slymen DJ, Parra MD, et al. Evaluation of a tobacco and alcohol use prevention program for Hispanic migrant adolescents: promoting the protective factor of parent‐child communication. Preventive Medicine 2000;31(2 (Pt 1)):124‐33. [DOI] [PubMed] [Google Scholar]
Gordon 1997 {published data only}
- Gordon I, Whitear B, Guthrie D. Stopping them starting: evaluation of a community‐based project to discourage teenage smoking in Cardiff. Health Education Journal 1997;46:42‐50. [Google Scholar]
Gordon 2008 {published data only}
- Gordon J, Biglan A, Smolkowski K. The Impact on tobacco use of branded youth anti‐tobacco activities and family communications about tobacco. Prevention Science 2008;9:73‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hancock 2001 {published data only}
- Hancock L, Sanson‐Fisher R, Perkins J, Girgis A, Howley P, Schofield M. The effect of a community action intervention on adolescent smoking rates in rural Australian towns: the CART project. Cancer Action in Rural Towns. Preventive Medicine 2001;32:332‐40. [DOI] [PubMed] [Google Scholar]
Hawkins 2009 {published data only}
- Fagan AA, Hanson K, Hawkins JD, Arthur MW. Implementing effective community‐based prevention programs in the Community Youth Development Study. Youth Violence and Juvenile Justice 2008;6(3):256‐78. [DOI: 10.1177/1541204008315937] [DOI] [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Arthur MW, Abbott RD, Fagan AA, Catalano RF. Results of a Type 2 Translational Research Trial to Prevent Adolescent Drug Use and Delinquency. Archives of Pediatric and Adolescent Medicine 2009;163(9):789‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klein 2009 {published data only}
- Klein EG, Forster JL, Erickson DJ, Lytle LA, Schillo B. The relationship between local clean indoor air policies and smoking behaviours in Minnesota youth. Tobacco Control 2009;18:132‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 1994 {published data only}
- Murray DM, Hannan PJ. Planning for the Appropriate Analysis in School‐Based Drug‐Use Prevention Studies. Journal of Consulting and Clinical Psychology 1990;58(4):458‐68. [DOI] [PubMed] [Google Scholar]
- Murray DM, Jacobs DR, Perry CL, Pallonen U, Harty KC, Griffin G, Mon ME, Hanson G. A Statewide Approach to Adoelscent Tobacco‐Use Prevention: the Minnesota‐Wisconsin Adolescent Tobacco‐Use Research Project. Preventive Medicine 1988;17:461‐74. [DOI] [PubMed] [Google Scholar]
- Murray DM, Perry CL, Griffin G, Harty KC, Jacobs DR, Schmid L, et al. Results from a statewide approach to adolescent tobacco use prevention. Preventive Medicine 1992;21:449‐72. [DOI] [PubMed] [Google Scholar]
- Murray DM, Prokhorov AV, Harty KC. Effects of a Statewide Antismoking Campaign on Mass Media Messages and Smoking Beliefs. Preventive Medicine 1994;23:54‐60. [DOI] [PubMed] [Google Scholar]
- Murray DM, Rooney BL, Hannan PJ, Peterson AV, Ary DV, Biglan A, Botvin GJ, Evans RI, Flay BR, Futterman R, Getz JG, Marek PM, Orlandi M, Pentz MA, Perry CL, Schinke SP. Intraclass Correlation among Common Measures of Adolescent Smoking: Estimates, Correlates, and Applications in Smoking Prevention Studies. American Journal of Epidemiology 1994;140(11):1038‐50. [DOI] [PubMed] [Google Scholar]
Pentz 1989 {published data only}
- Pentz MA, Dwyer JH, Mackinnon DP, Flay BR, Hansen WB, Wang EY, Johnson CA. A multicommunity trial for primary prevention of adolescent drug abuse. Effects on drug use prevalence. JAMA 1989;261:3259‐66. [PubMed] [Google Scholar]
Perry 1994 {published data only}
- Perry CL, Kelder SH, Klepp K. Community‐wide cardiovascular disease prevention in young people: long‐term outcomes of the Class of 1989 Study. European Journal of Public Health 1994;4:188‐194. [Google Scholar]
Perry 2003 {published data only}
- Ennett ST, Tobler NS, Ringwalt CL, Flewelling RL. How Effective Is Drug Abuse Resistance Education? A Meta‐Analysis of Project DARE Outcome Evaluations. American Journal of Public Health 1994;84(9):1394‐401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen WB, McNeal RB. How D.A.R.E. Works: An Examination of Program Effects on Mediating Variables. Health Education & Behavior 1997;24:165‐76. [DOI: 10.177/109019819702400205] [DOI] [PubMed] [Google Scholar]
- Perry CL, Komro KA, Veblen‐Mortenson S, Bosma L, Munson K, Stigler M, Lytle LA, Forster JL, Welles SL. The Minnesota DARE Plus Project: Creating Community Partnerships to Prevent Drug Use and Violence. Journal of School Health 2000;70(3):84‐8. [DOI] [PubMed] [Google Scholar]
- Perry CL, Komro KA, Veblen‐Mortenson S, Bosma LM, Farbakhsh K, Munson KA, Stigler MH, Lytle LA. A Randomized Controlled Trial of the Middle and Junior High School D.A.R.E. and D.A.R.E. Plus Programs. Archives of Pediatric and Adolescent Medicine 2003;157:178‐84. [DOI] [PubMed] [Google Scholar]
- Rosenbaum DP, Flewelling RL, Bailey SL, Ringwalt CL, Wilkinson DL. Dops in the Classroom: A Longitudinal Evaluation of Drug Abuse Resistance Education (Dare). Journal of Research in Crime and Delinquency 1994;31:3‐31. [DOI: 10.1177/0022427894031001001] [DOI] [Google Scholar]
Perry 2008 {published data only}
- Bate SL, Stigler MH, Thompson MS, Arora M, Perry CL, Reddy KS, MacKinnon DP. Psychosocial Mediators of a School‐Based Tobacco Prevention Program in India: Results from the First Year of Project MYTRI. Preventive Schience 2009;10:116‐28. [DOI: 10.1007/s11121-008-0113-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Stigler MH, Arora M, Reddy KS. Prevention in Translation: Tobacco Use Prevention in India. Health Promotion Practice 2008;9(4):378‐86. [DOI: 10.1177/1524839906289222] [DOI] [PubMed] [Google Scholar]
- Perry CL, Stigler MH, Arora M, Reddy S. Preventing Tobacco Use Among Young People inIndia: Project MYTRI. American Journal of Public Health 2009;99(5):899‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Arora M, Reddy KS. Why are urban Indian 6th graders using more tobacco than 8th graders? Findings from Project MYTRI. Tobacco Control 2006;15(Suppl1):i54‐60. [DOI: 10.1136/tc.2005.014480] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Arora M, Shrivastav R, Mathur C, Reddy KS. Intermediate Outcomes from Project MYTRI: Mobilizing Youth for Tobacco‐Related Initiatives in India. Cancer Epidemiol Biomarkers Prev 2007;16(6):1050‐6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Piper 2000 {published data only}
- Moberg DP. Personal communication 1999.
- Moberg DP, Piper DL, Serlin RC, Wu J. When total randomization is impossible‐ nested randomization assignment. Evaluation Review 1993;17:271‐91. [Google Scholar]
- Piper DL, Moberg DP, King MJ. The Healthy for Life Project: behavioral outcomes. Journal of Primary Prevention 2000; Vol. 21:47‐73.
Schinke 2000 {published data only}
- Schinke SP, Tepavac L, Cole KC. Preventing substance use among native American youth: Three‐year results. Addictive Behaviors 2000;25:387‐97. [DOI] [PubMed] [Google Scholar]
Schofield 2003 {published data only}
- Lynagh M, Knight J, Schofield MJ, Paras L. Lessons Learned from the Hunter Region Health Promoting Schools Project in New South Wales, Australia. Journal of School Health 1999;69(6):227‐32. [DOI] [PubMed] [Google Scholar]
- Schofield MJ, Lynagh M, Mishra G. Evaluation of a Health Promoting Schools program to reduce smoking in Australian secondary schools. Health Education Research 2003;18(6):678‐92. [DOI: 10.1093/her/cy048] [DOI] [PubMed] [Google Scholar]
Stevens 2002 {published data only}
- Stevens MM, Olson AL, Gaffney CA, Tosteson TD, Mott LA, Starr P. A Pediatric, Practice‐Based, Randomized Trial of Drinking and Smoking Prevention and Bicycle Helmet, Gun, and Seatbelt Safety Promotion. Pediatrics 2002;109(3):490‐7. [DOI] [PubMed] [Google Scholar]
St Pierre 1992 {published data only}
- Pierre TL, Kaltreider DL, Mark MM, Aikin KJ. Drug prevention in a community setting: A longitudinal study of the relative effectiveness of a 3‐year primary prevention program in boys and girls clubs across the nation. American Journal of Community Psychology 1992;20:673‐706. [PubMed] [Google Scholar]
Sussman 1998 {published data only}
- Sussman S, Dent CW, Stacy AW, Craig S. One‐year outcomes of Project Towards No Drug Abuse. Preventive Medicine 1998;27:632‐42. [DOI] [PubMed] [Google Scholar]
Tang 1997 {published data only}
- Tang KC, Rissel C, Bauman A, Dawes A, Porter S, Fay J, et al. Evaluation of Kickbutts ‐ a school and community‐based smoking prevention program among a sample of year 7 and 8 students. Health Promotion Journal of Australia 1997;7:122‐7. [Google Scholar]
Vartiainen 1998 {published data only}
- Paavola M, Vartiainen E, Haukkala A. Smoking, Alcohol Use, and Physical Activity: A 13‐Year Longitudinal Study Ranging from Adolescence into Adulthood. Journal of Adolescent Health 2004;35:238‐44. [DOI: 10.1016/j.jadohealth.2003.12.004] [DOI] [PubMed] [Google Scholar]
- Puska P, Vartiainen E, Pallonen U, Ruotsalainen P, Tuomilehto J, Koskela K, Lahtinen A, Norppa J. A Community‐Based Intervention Study on CVD Risk Factors among 13‐ to 15‐Year‐Old Children: Study Design and Preliminary Findings. Preventive Medicine 1983;10:133‐48. [DOI] [PubMed] [Google Scholar]
- Vartiainen E, Fallonen U, McAlister AL, Puska P. Eight‐Year Follow‐up Results of an Adolescent Smoking Prevention Program: The North Karelia Youth Project. American Journal of Public Health 1990;80(1):78‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartiainen E, Paavola M, McAlister A, Puska P. Fifteen‐year follow‐up of smoking prevention effects in the North Karelia Youth Project. American Journal of Public Health 1998;88(1):81‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartiainen E, Pallonen U, McAlister A, Koskela K Puska P. Effect of two years of educational intervention on adolescent smoking (The North Karelia Youth Project). Bulletin of the World Health Organization 1983;61(3):529‐32. [PMC free article] [PubMed] [Google Scholar]
- Vartiainen E, Pallonen U, McAlister A, Koskela K, Puska P. Four‐Year Follow‐Up Results of the Smoking Prevention Program in the North Karelia Youth Project. Preventive Medicine 1986;15:692‐8. [DOI] [PubMed] [Google Scholar]
- Vartiainen E, Tossavainen K, Viri L, Niskanen E, Puska P. The North Karelia Youth Programs. Annals New York Academy of Sciences 1991;623:332‐49. [DOI] [PubMed] [Google Scholar]
Winkleby 1993 {published data only}
- Winkleby MA, Fortmann SP, Rockhill B. Cigarette smoking trends in adolescents and young adults: the Stanford Five‐City Project. Preventive Medicine 1993;22:325‐34. [DOI] [PubMed] [Google Scholar]
Winkleby 2004 {published data only}
- Winkleby MA, Feighery E, Dunn M, Kole S, Ahn D, Killen JD. Effects of an Advocacy Intervention to Reduce Smoking Among Teenagers. Archives of Pediatric and Adolescent Medicine 2004;158:269‐75. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aguirre‐Molina 1995 {published data only}
- Aguirre‐Molina M, Gorman DM. The Perth Amboy Community Partnership for Youth: Assessing its effects at the environmental and individual levels of analysis. International Quarterly of Community Health Education 1995;15(363):378. [DOI] [PubMed] [Google Scholar]
Aldinger 2008 {published data only}
- Aldinger C, Xin‐Wei Z, Li‐Qun L, Jun‐Xiang G, Hai YS, Jones J. Strategies for implementing Health‐Promoting Schools in a province in China. IUHPE ‐ Promotion and Education 2008;15(1):24‐9. [DOI: 10.1177/1025382307088095] [DOI] [PubMed] [Google Scholar]
- Aldinger C, Xin‐Wei Z, Li‐Qun L, Xue‐Dong P, Sen‐Hai Y, Jones J, Kass J. Changes in attitudes, knowledge and behavior associated with implementing a comprehensive school health program in a province of China. Health Education Research 2008;23(6):1049‐67. [DOI: 10.1093/her/cyn022] [DOI] [PubMed] [Google Scholar]
American Lung Assoc 2008 {published data only}
- American Lung Association, Division of Public Health's Tobacco Prevention Community contract, Delaware Health Fund. Practice Notes: Strategies in Health Education; A Program of Life. Health Education & Behavior 2008;35(2):153‐57. [DOI: 10.1177/1090198108315800] [DOI] [Google Scholar]
Andrade e Silva 1991 {published data only}
- Andrade e Silva MI. La Prevention du Tabagisme par la Promotion de la Sante [Smoking prevention through health promotion. A novel experience in schools of the northern region of Portugal]. Hygie 1991;10(4):26‐31. [PubMed] [Google Scholar]
Arora 2010 {published data only}
- Arora M, Tewari A, Tripathy V, Nazar GP, Juneja NS, Ramakrishnan L, Reddy KS. Community‐based model for preventing tobacco use among disadvantaged adolescents in urban slums of India. Health Promotion International 2010;25(2):143‐52. [DOI] [PubMed] [Google Scholar]
Baudier 1991 {published data only}
- Baudier F, Henry Y, Marchais M, Dorier J, Lombardet A, Llaona P, et al. The "Besancon smoke‐free" programme. Concepts, measures and evaluation. Hygie 1991;10(4):18‐25. [PubMed] [Google Scholar]
Berenson 2010 {published data only}
- Berenson GS. Cardiovascular Health Promotion for Children: A Model for a Parish (County) ‐ Wide Program (Implementation and Preliminary Results). Preventive Cardiology 2010;Winter:23‐28. [DOI: 10.1111/j.1751-7141.2009.00049.x] [DOI] [PubMed] [Google Scholar]
Bowen 2002 {published data only}
- Bowen DJ, Orlandi MA, Lichtenstein E, Cummings KM, Hyland A. Intervention effects on youth tobacco use in the community intervention trial (COMMIT). Tobacco Control 2002;11:382. [DOI: 10.1136/tc.11.4.382] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brownson 1996 {published data only}
- Brownson RC, Smith CA, Pratt M, Mack NE, Jackson‐Thompson J, et al. Preventing cardiovascular disease through community‐based risk reduction: the Bootheel Heart Health Project. American Journal of Public Health 1996;86:206‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cain 1992 {published data only}
- Cain JJ, Dudley TE, Wilkerson MK. Tar wars: Community‐based tobacco education project. Journal of Family Practice 1992;34:267‐68. [PubMed] [Google Scholar]
Campion 1994 {published data only}
- Campion P, Owen L, McNeill A, McGuire C. Evaluation of a mass media campaign on smoking and pregnancy. Addiction 1994;89:1245‐1254. [DOI] [PubMed] [Google Scholar]
Carleton 1995 {published data only}
- Carleton RA, Lasater TM, Assaf AR, Feldman HA, McKinlay S. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. American Journal of Public Health 1995;85:777‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Charlier 2009 {published data only}
- Charlier N, Glover M, Robertson J. Keeping Kids Smokefree: lessons learned on community participation. Health Education Research 2009;24(6):949‐56. [DOI: 10.1093/her/cyp047] [DOI] [PubMed] [Google Scholar]
Chen 2006 {published data only}
- Chen V, Forster JL. The long‐term effect of local policies to restrict retail sale of tobacco to youth. Nicotine and Tobacco Research June 2006;8(3):371‐77. [DOI: 10.1080/14622200600670249] [DOI] [PubMed] [Google Scholar]
Clarke 1993 {published data only}
- Clarke V, Hill D, Murphy M, Borland R. Factors affecting the efficacy of a community‐based quit smoking program. Health Education Research 1993;8:537‐46. [DOI] [PubMed] [Google Scholar]
Cruz 2008 {published data only}
- Cruz GG, Ferrero MG, Coca IA, Maderuelo JA, Garcia MT. Program for the Prevention of Smoking in Secondary School Students [Programa de prevencion del tabaquismo en alumnos de ensenanza secundaria]. Archivos de Bronconeumologia 2008;45(1):16‐23. [DOI] [PubMed] [Google Scholar]
Davidson 1994 {published data only}
- Davidson JE. Smokebusters: the experience of a Smokebusters intervention in a youth club in North‐East England. Edinburgh University MSc Dissertation 1994.
- Davidson L. Wensleydale Smokebusters Project Report. Northallerton: Northallerton Health Authority 1992.
Elder 1996 {published data only}
- Elder JP, Edwards CC, Conway TL, Kenney E, Johnson CA, Bennett ED. Independent evaluation of the California Tobacco Education Program. Public Health Reports 1996;111:353‐8. [PMC free article] [PubMed] [Google Scholar]
Elder 1996b {published data only}
- Elder JP, Perry CL, Stone EJ, Johnson CC, Yang MH, Edmundson EW, et al. Tobacco use measurement, prediction, and intervention in elementary schools in 4 states ‐ the CATCH study. Preventive Medicine 1996;25:486‐94. [DOI] [PubMed] [Google Scholar]
Farquhar 1991 {published data only}
- Farquhar JW. The Stanford Cardiovascular Disease Prevention Programs. Annals of the New York Academy of Science 1991;623:327‐31. [DOI] [PubMed] [Google Scholar]
Fawcett 1997 {published data only}
- Fawcett SB, Lewis RK, Paine‐Andrews A, Francisco VT, Richter KP, Williams EL, et al. Evaluating community coalitions for prevention of substance abuse: the case of Project Freedom. Health Education & Behavior 1997;24:812‐28. [DOI] [PubMed] [Google Scholar]
Forster 1998 {published data only}
- Forster JL, Murray DM, Wolfson M, Blaine TM, Wagenaar AC, Hennrikus DJ. The effects of community policies to reduce youth access to tobacco. American Journal of Public Health 1998;88:1193‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frith 1997 {published data only}
- Frith C, Roberts C, Kingdon A, Tudor‐Smith C. An evaluation of the 1996 No Smoking Day in Wales. Health Education Journal 1997;56:287‐95. [Google Scholar]
Harvey 1990 {published data only}
- Harvey M, Tuffin A, Tuffin K. An evaluation of a community based antismoking campaign. New Zealand Medical Journal 1990;103:243‐45. [PubMed] [Google Scholar]
HEA 1994a {published data only}
- Health Education Authority. Health skills for girls. London: HEA, 1994. [Google Scholar]
HEA 1994b {published data only}
- Health Education Authority. `Hi‐Energy': a final report and evaluation findings. London: HEA, 1994. [Google Scholar]
HEA 1994c {published data only}
- Health Education Authority. Choices about health for Ashfield teenagers (CHAT). London: HEA, 1994. [Google Scholar]
Higgs 2000 {published data only}
- Higgs PE, Edwards D, Harbin RE, Higgs PC. Evaluation of a Self‐Directed Smoking Prevention and Cessation Program. Pediatric Nursing March‐April 2000;26(2):150‐5. [PubMed] [Google Scholar]
Hunkeler 1990 {published data only}
- Hunkeler DF, Davis EM, Neil B, Powell JW, Polen. Richmond quits smoking: a minority community fights for health. In: Bracht N editor(s). Health promotion at the community level. Newbury Park, CA: Sage, 1990. [Google Scholar]
Hymowitz 1995 {published data only}
- Hymowitz N. Paterson COMMIT: a smoke‐free community initiative. New Jersey Medicine 1995;92:22‐4. [PubMed] [Google Scholar]
Jason 2010 {published data only}
- Jason LA, Pokorny SB, Adams M, Nihls A, Kim HY, Hunt Y. Cracking Down on Youth Tobacco May Influence Drug Use. Journal of Community Psychology 2010;38(1):1‐15. [DOI: 10.1002/jcop.20347] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaufman 1994 {published data only}
- Kaufman JS, Jason LA, Sawlski LM, Halpert JA. A comprehensive multi‐media program to prevent smoking among Black students. Journal of Drug Education 1994;24:95‐108. [DOI] [PubMed] [Google Scholar]
Lazenbatt 1997 {published data only}
- Lazenbatt A. Protecting young people from tobacco: an evaluation of the Ulster Cancer Foundation's "Smokebusters" campaign in primary schools in Northern Ireland. Ulster Cancer Foundation; Belfast 1997.
Marin 1994 {published data only}
- Marin BV, Perez Stable EJ, Marin G, Hauck WW. Effects of a community intervention to change smoking behavior among Hispanics. American Journal of Preventive Medicine 1994;10:340‐7. [PubMed] [Google Scholar]
Meshack 2004 {published data only}
- Meshack AF, Hu S, Pallonen UE, McAlister AL, Gottlieb N, Huang P. Texas Tobacco Prevention Pilot Initiative: processes and effects. Health Education Research 2004;19(6):657‐68. [DOI: 10.1093/her/cyg088] [DOI] [PubMed] [Google Scholar]
Morgan 1994 {published data only}
- Morgan M, Doorley P, Hynes M, Joy S. An evaluation of a smoking prevention programme with children from disadvantaged communities. Irish Medical Journal 1994;87:56‐8. [PubMed] [Google Scholar]
Mudde 1995 {published data only}
- Mudde AN, Vries H, Dolders MGT. Evaluation of a Dutch community‐based smoking cessation intervention. Preventive Medicine 1995;24:61‐70. [DOI] [PubMed] [Google Scholar]
Nater 1985 {published data only}
- Nater B, Junod B, Gutzwiller F, Wietlisbach V. [The influence of family environment on the evolution of tobacco consumption in 2 trial towns and 2 control towns in Switzerland]. Revue d'Épidémiologie et de Santé Publique 1985;33:90‐6. [PubMed] [Google Scholar]
Nilsson 2006 {published data only}
- Nilson M, Stenlund H, Bergstrom E, Weinehall L, Janlert U. It Takes Two: Reducing Adolescent Smoking Uptake Through Sustainable Adolescent ‐ Adult Partnership. Journal of Adolescent Health 2006;39:880‐6. [DOI: 10.1016/j.jadohealth.2006.07.004] [DOI] [PubMed] [Google Scholar]
- Nilsson M, Stenlund H, Weinehall L, Bergstrom E, Janlert U. "I would do anything for my child, even quit tobacco": Bonus effects from an intervention that targets adolescent tobacco use. Scandinavian Journal of Psychology 2009;50:341‐5. [DOI: 10.1111/j.1467-9450.2009.00716.x] [DOI] [PubMed] [Google Scholar]
O'Loughlin 1995 {published data only}
- O'Loughlin J, Paradis G, Kishchuk N, Gray‐Donald K, Renaud L, Fines P, et al. Coeur en sante St‐Henri ‐ a heart health promotion programme in Montreal, Canada: design and methods for evaluation. Journal of Epidemiology & Community Health 1995;49:495‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pentz 1989B {published data only}
- Johnson CA, Pentz MA, Weber MD, Dwyer JH, Baer N, MacKinnon DP, Hansen WB. Relative Effectiveness of Comprehensive Community Programming for Drug Abuse Prevention With High‐Risk and Low‐Risk Adolescents. Journal of Consulting and Clinical Psychology 1990;58(4):447‐56. [DOI: ] [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Johnson CA, Pentz MA, Dwyer JH. Mediating Mechanisms in a School‐Based Drug Prevention Program: First‐Year Effects of the Midwestern Prevention Project. Health Psychology 1991;10(3):164‐72. [DOI: ] [DOI] [PubMed] [Google Scholar]
- Pentz MA, Johnson CA, Dwyer JH, MacKinnon DM, Hansen WB, Flay BR. A Comprehensive Community Approach to Adolescent Drug Abuse Prevention: Effects on Cardiogascular Disease Risk Behaviors. Annals of Medicine 1989;21:219‐22. [DOI: 10.3109/07853898909149937] [DOI] [PubMed] [Google Scholar]
- Pentz MA, MacKinnon DP, Dwyer JH, Wang EYI, Hansen WB, Flay BR, Johnson CA. Longitudinal Effects of the Midwestern Prevention Project on Regular and Experimental Smoking in Adolescents. Preventive Medicine 1989;18:304‐21. [DOI] [PubMed] [Google Scholar]
- Pentz MA, MacKinnon DP, Flay BR, Hansen WB, Johnson CA, Dwyer JH. Primary Prevention of Chronic Diseases in Adolescence: Effects of the Midwestern Prevention Project on Tobacco Use. American Journal of Epidemiology 1989;130(4):713‐24. [DOI] [PubMed] [Google Scholar]
Pierce 1998 {published data only}
- Pierce JP, Gilpin EA, Emery SL, White MM, Rosbrook B, Berry CC. Has the California tobacco control program reduced smoking?. JAMA 1998;280:893‐9. [DOI] [PubMed] [Google Scholar]
Pomrehn 1995 {published data only}
- Pomrehn PR, Jones MP, Ferguson KJ, Becker SL. Tobacco use initiation in middle school children in three IOWA communities: Results of the Iowa program against smoking (I‐PAS). Journal of Health Education 1995;26:92‐100. [Google Scholar]
Ramirez 1988 {published data only}
- Ramirez AG, McAlister AL. Mass media campaign‐‐A Su Salud. Preventive Medicine 1988;17:608‐21. [DOI] [PubMed] [Google Scholar]
Ramirez 1997 {published data only}
- Ramirez AG, Gallion KJ, Espinoza R, McAlister A, Chalela P. Developing a media‐ and school‐based program for substance abuse prevention among Hispanic youth: a case study of Mirame!/Look at me!. Health Education & Behavior 1997;24:603‐12. [DOI] [PubMed] [Google Scholar]
Reinert 2004A {published data only}
- Reinert B, Carver V, Range LM. Anti‐Tobacco Messages From Different Sources Make a Difference With Secondary School Students. Journal of Public Health Management Practice 2004;10(6):518‐23. [DOI] [PubMed] [Google Scholar]
Reinert 2004B {published data only}
- Reinert B, Carver V, Range LM. Tobacco use prevention in private high schools. Quarterly of Community Health Education 2004;22(1 & 2):47‐58. [Google Scholar]
Rigotti 2002 {published data only}
- Rigotti NA, Regan S, Majchrzak NE, Knight JR, Wechsler H. Tobacco use by Massachusetts public college students: long term effect of the Massachusetts Tobacco Control Program. Tobacco Control 2002;11:ii20‐4. [DOI: 10.1136/tc.11.suppl_2.ii20] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rohrbach 1994 {published data only}
- Rohrbach LA. Hodgson CS. Broder BI. Montgomery SB. Flay BR. Hansen WB, et al. Parental participation in drug abuse prevention: Results from the Midwestern Prevention Project. Journal of Research on Adolescence 1994;4:295‐317. [Google Scholar]
Schinke 1996 {published data only}
- Schinke SP, Singer B, Cole K, Contento IR. Reducing cancer risk among Native American adolescents. Preventive Medicine 1996;25:146‐55. [DOI] [PubMed] [Google Scholar]
Shea 1990 {published data only}
- Shea S, Basch CE. A review of five major community‐based cardiovascular disease prevention programs. Part I: Rationale, design, and theoretical framework. American Journal of Health Promotion 1990;4:203‐13. [DOI] [PubMed] [Google Scholar]
Shipley 1995 {published data only}
- Shipley RH, Hartwell TD, Austin WD, Clayton AC, Stanley LC. Community stop‐smoking contests in the COMMIT trial: relationship of participation to costs. Community Intervention trials. Preventive Medicine 1995;24:286‐92. [DOI] [PubMed] [Google Scholar]
Sigfusdottir 2008 {published data only}
- Sigfusdottir ID, Thorlindsson T, Kristjansson AL, Roe EM, Allegrante JP. Substance use prevention for adolescents: the Icelandic Model. Health Promotion International 2008;24(1):16‐25. [DOI: 10.1093/heapro/dan038] [DOI] [PubMed] [Google Scholar]
Slater 2006 {published data only}
- Slater MD, Edwards RW, Plested BA, Thurman PJ, Kelly KJ, Comello MLG, Keefe TJ. Using community readiness key informant assessments in a randomized group prevention trial: Impac of a participatory community‐media intervention. Journal of Community Health 2005;30(1):39‐53. [DOI: 10.1007/s10900-004-6094-1] [DOI] [PubMed] [Google Scholar]
- Slater MD, Kelly KJ. Testing Alternative Explanations for Exposure Effects in Media Campaigns: The Case of a Community‐Based, In‐School Media Drug Prevention Project. Communication Research 2002;29(4):367‐89. [DOI: 10.1177/0093650202029004001] [DOI] [Google Scholar]
- Slater MD, Kelly KJ, Edwards RW, Thurman PJ, Plested BA, Keefe TJ, Lawrence FR, Henry KL. Combining in‐school and community‐based media efforts: reducing marijuana and alcohol uptake among younger adolescents. Health Education Research 2006;21(1):157‐67. [DOI: 10.1093/her/cyh056] [DOI] [PubMed] [Google Scholar]
Smith 2008 {published data only}
- Smith TM, Talley B, Hubbard M, Winn C. Evaluation of a Tobacco Prevention Program for Children:ToPIC. Journal of Community Health Nursing 2008;25:218‐28. [DOI: 10.1080/07370010802421210] [DOI] [PubMed] [Google Scholar]
Stein 1997 {published data only}
- Stein J, Glass K, Coburn K, Sisson J, Birnkrant J, Bravo A, et al. A medical school's plan for anti‐tobacco‐use education in community schools and hospitals. Journal of Cancer Education 1997;12:157‐60. [DOI] [PubMed] [Google Scholar]
Stevenson 1998 {published data only}
- Stevenson JF, McMillan B, Mitchell RE, Blanco M. Project HOPE: Altering risk and protective factors among high risk Hispanic youth and their families. Journal of Primary Prevention 1998;18:287‐317. [Google Scholar]
Steyn 1997 {published data only}
- Steyn K, Steyn M, Swanepoel AS, Jordaan PCJ, Jooste PL, Fourie JM, et al. Twelve‐year results of the Coronary Risk Factor Study (CORIS). International Journal of Epidemiology 1997;26:964‐71. [DOI] [PubMed] [Google Scholar]
Tingen 2005 {published data only}
- Tingen MS, Waller JL, Smith TM, Baker RR, Reyes J, Treiber FA. Tobacco prevention in children and cessation in family members. American Academy of Nurse Practitioners 2006;18:169‐79. [DOI] [PubMed] [Google Scholar]
Tudor‐Smith 1998 {published data only}
- Tudor‐Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme over five years on behavioural risks for cardiovascular disease: quasi‐experimental comparison of results from Wales and a matched reference area. BMJ 1998;316:818‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Teijlingen 1996 {published data only}
- Teijlingen ER, Friend JA, Twine F. Evaluation of Grampian Smokebusters: a smoking prevention initiative aimed at young teenagers. Journal of Public Health Medicine 1996;18:13‐8. [DOI] [PubMed] [Google Scholar]
- Teijlingen E, Friend J. Smoking habits of Grampian school children and an evaluation of the Grampian Smoke Busters campaign. Health Education Research 1993;8:97‐108. [DOI] [PubMed] [Google Scholar]
Vicary 1996 {published data only}
- Vicary JR, Doebler MK, Bridger JC, Gurgevich EA. A community systems approach to substance abuse prevention in a rural setting. Journal of Primary Prevention 1996;16:303‐18. [DOI] [PubMed] [Google Scholar]
Wheeler 1988 {published data only}
- Wheeler RJ. Effects of a community‐wide cessation program. Social Science & Medicine 1988;27:1387‐92. [DOI] [PubMed] [Google Scholar]
Wickizer 1993 {published data only}
- Wickizer TM, Von‐Korff M, Cheadle A, Maeser J, Wagner EH, Pearson D, et al. Activating communities for health promotion: a process evaluation method. American Journal of Public Health 1993;83:561‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2008 {published data only}
- Wilson N, Minkler M, Dasho S, Wallerstein N, Martin AC. Getting to Social Action: the Youth Empowerment Strategies (YES!) Project. Health Promotion Practice 2008;9(4):395‐403. [DOI: 10.1177/1524839906289072] [DOI] [PubMed] [Google Scholar]
Wood 2009 {published data only}
- Wood LJ, Rosenberg M, Clarkson J, Phillips F, Donovan RJ, Shilton T. Encouraging Young Western Australians to Be Smarter Than Smoking. American Journal of Health Promotion 2009;23(6):403‐11. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wu 2003 {published data only}
- Stanton B, Cole M, Galbraith J, Li X, Pendleton S, Cottrel L, Marshall S, Wu Y, Kaljee L. Randomised Trial of a Parent Intervention: Parents Can Make a Difference in Long‐term Adolescent Risk Behaviors, Perceptions, and Knowledge. Archives of Pediatric and Adolescent Medicine 2004;158:947‐55. [DOI] [PubMed] [Google Scholar]
- Wu Y, Stanton BF, Galbraith J, Kaljee L, Cottrell L, Li X, Harris CV, D'Alessandri D, Burns JM. Sustaining and Broadening Intervention Impact: A Longitudinal Randomized Trial of 3 Adolescent Risk Reduction Approaches. Pediatrics 2003;111(1):e32‐8. [DOI] [PubMed] [Google Scholar]
Yoffe 1994 {published data only}
- Yoffe SJ, Boren JB. Follow‐up study of a field‐based campaign against tobacco usage for children in grades six through eight. Texas Medicine 1994;90:71‐4. [PubMed] [Google Scholar]
Additional references
Altman 1997
- Altman DG, Bland JM. Statistics Notes: Units of analysis. BMJ 1997;314:1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauman 1996
- Bauman KE, Ennett SE. On the importance of peer influence for adolescent drug use: commonly neglected considerations. Addiction 1996;91:185‐98. [PubMed] [Google Scholar]
BMA 2008
- Hastings G, Angus K. Forever cool: the influence of smoking imagery on young people. British Medical Association Science and Education Department and the Board of Science, July 2008. [Google Scholar]
Brinn 2010
- Brinn MP, Carson KV, Esterman AJ, Chang AB, Smith BJ. Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews 2010, Issue 11. [DOI: 10.1002/14651858.CD001006.pub2] [DOI] [PubMed] [Google Scholar]
CART 1996a
- CART Project Team. Developing methodologies for evaluating community‐wide health promotion. Health Promotion International 1996;11:227‐236. [Google Scholar]
CART 1996b
- CART Project Team. Community action for cancer prevention: overview of the Cancer Action in Rural Towns (CART) project, Australia. Health Promotion International 1996;11:277‐290. [Google Scholar]
Catalano 1996
- Catalano RF, Kosterman R, Hawkins JD, Newcomb MD, Abbott RD. Modeling the etiology of adolescent substance use: A test of the social development model. Journal of Drug Issues 1996;26(2):429‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
EPOC 2009
- Cochrane EPOC Group 2009 . Cochrane EPOC Group. Cochrane Effective Practice and Organisation of Care Group.. Available from: http://www.epoc.cochrane.org (accessed 1 November 2009).
Fleming 2008
- Fleming CB, Catalano RF, Mazza JJ, Brown EC, Haggerty KP, Harachi TW. After‐school activities, misbehaviour in school, and delinquency from the end of elementary school through the beginning of high school: a test of social development model hypotheses. Journal of Early Adolescence 2008;28:277‐303. [DOI: 10.1177/0272431607313589] [DOI] [Google Scholar]
Gail 1992
- Gail MH, Byar DP, Pechacek TF, Corle DK. Aspects of Statistical Design for the Community Intervention Trial for Smoking Cessation (COMMIT). Controlled Clinical Trials 1992;13:6‐21. [DOI] [PubMed] [Google Scholar]
Gupta 2008
- Gupta PC, Asma S. Bidi Smoking and Public Health. Ministery of Health and Family Services, Government of India 2008; Vol. [accessed 03/02/2011].
GYTSC 2002
- The Global Youth Tobacco Survey Collaborative Group. Tobacco use among youth: a cross country comparison. Tobacco Control 2002;11:252‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. Chichester (UK): The Cochrane Collaboration; John Wiley & Sons, 2008. [Google Scholar]
Mackay 2006
- Mackay J, Eriksen M, Shafey O. The Tobacco Atlas. Second Edition. Georgia, USA: American Cancer Society, 2006. [ISBN: 0‐944235‐58‐1] [Google Scholar]
MMWR 2008
- Warren CW, Jones NR, Peruga A, Chauvin J, Baptiste J, Costa de Silva V, Awa F, Tsouros A, Rahman K, Fishburn B, Bettcher DW, Asma S. Global Youth Tobacco Surveillance. Morbidity Mortality Weekly Review ‐ CDC 25 Jan 2008;57(SS01):1‐21. [PubMed] [Google Scholar]
Murray 1992
- Murray DM, Perry CL, Griffin G, Harty KC, Jacobs DR, Schmid L, et al. Results from a statewide approach to adolescent tobacco use prevention. Prev Med 1992;21:449‐72. [DOI] [PubMed] [Google Scholar]
Murray 1996
- Murray DM, Moskowitz JM, Dent C. Design and analysis issues in a community‐based drug‐use prevention trial. American Behavioral Scientist 1996;39(7):853‐67. [Google Scholar]
NHS IC 2010
- Elizabeth Fuller, Marie Sanchez (Editors). Smoking, drinking and drug use among young people in England in 2009. www.ic.nhs.uk/pubs/sdd09fullreport: NHS Information Centre for Health and Social Care, 2010. [Google Scholar]
Rahman 2000
- Rahman M, Fukui T. Bidi Smoking and Health. Public Health 2000;114:123‐7. [DOI] [PubMed] [Google Scholar]
Rao 1992
- Rao JNK, Scott AJ. A simple method for the analysis of cluster binary data. Biometrics 1992;48:577‐85. [PubMed] [Google Scholar]
Rooney 1996
- Rooney BL, Murray DM. A meta‐analysis of smoking programs after adjustment for errors in the unit of analysis. Health Education Quarterly 1996;23:48‐64. [DOI] [PubMed] [Google Scholar]
SAMHSA 2009
- Subtance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Office of Applied Studies, SAMHSA, U.S. Department of Health and Human Services, 2010. [Google Scholar]
Schofield 1991
- Schofield MJ, Redman S, Sanson‐Fisher RW. A community approach to smoking prevention: a review. Behaviour Change 1991;8:17‐25. [Google Scholar]
Stead 1996
- Stead M, Hastings G, Tudor‐Smith C. Preventing adolescent smoking: a review of options. Health Education Journal 1996;55:31‐54. [Google Scholar]
Thomas 2006
- Thomas RE, Perera R. School‐based programmes for preventing smoking. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD001293.pub2] [DOI] [PubMed] [Google Scholar]
Ukoumunne 1999
- Ukoumunne OC, Guilliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area‐wide and organisation based intervention health and health care: a systematic review. Health Technology Assessment 1999;3(5):1‐108. [PubMed] [Google Scholar]
UMDNJ 2007
- UMDNJ‐School of Public Health. Tobacco Surveillance Data Brief: Youth Consumption of Cigarettes. http://www.state.nj.us/health/as/ctcp/documents/youth_consumption_of_cigarettes.pdf [accessed 09/07/2010] 2007; Vol. 2, issue 1.
USDHHS 1994
- US Department of Health and Human Services. Preventing Tobacco Use among Young People. A Report of the Surgeon General. Rockville, Maryland: US DHHS, 1994. [Google Scholar]
Warren 2009
- Warren C, Lea V, Lee J, Jones N, Asma S, McKenna M. Change in tobacco use among 13 15 year olds between 1999 and 2008: findings from the Global youth Tobacco Survey. Global Health Promotion 2009;16:38‐90. [DOI] [PubMed] [Google Scholar]
Watson 2003
- Watson CH, Polzin GM, Calafat AM, Ashley DL. Determination of the Tar, Nicotine, and Carbon Monoxide Yields in the Smoke of Bidi Cigarettes. Nicotine and Tobacco Reasearch 2003;5(5):747‐53. [DOI] [PubMed] [Google Scholar]
Wiehe 2005
- Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Rivara FP. A systematic review of school‐based smoking prevention trials with long‐term follow‐up. Journal of Adolescent Health 2005;36(3):162‐9. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Sowden 2000a
- Sowden A, Arblaster L. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews 2000, Issue 1. [DOI: 10.1002/14651858.CD001291] [DOI] [PubMed] [Google Scholar]
Sowden 2003
- Sowden AJ, Stead LF. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD001291] [DOI] [PubMed] [Google Scholar]


