Abstract
Objective:
Injuries account for a large portion of the global burden of disease, representing over 10% of all disability adjusted life years (DALYs). This study analyzes the economic impact of injury for those experiencing moderate-to-severe injury in Beirut, Lebanon. It further examines the impact of different demographic and socioeconomic factors on trauma-specific quality of life 1–2 years following injury.
Methods:
This was a prospective cohort study following patients 1–2 years after being treated for injury at one of three hospitals in Beirut, Lebanon. Patients interviewed by phone. In addition to questions on financial impact, access to healthcare, and socioeconomic status, the Trauma-specific Quality of Life (TQoL) Questionnaire was used to assess quality of life following injury. Multivariable linear models were constructed to examine TQoL and demographics among institutes.
Results:
116 patients completed interviews. The average out-of-pocket cost of injury was 2975.42 USD, 65% of which was borrowed. 21% of people lost employment due to injury. Patients at Geitawi Hospital and the Rafic Hariri Governmental Hospital borrowed more on average and had higher reductions in employment than patients at the American University of Beirut Medical Center (AUBMC). There was a loss of income for those employed at the time of injury, with a mean monthly loss of 261.6 USD. The economic impact of injury was 10,329.00 USD. 25% of patients reported difficulty with accessing follow-up care, predominantly due to cost. Mean-adjusted Trauma-specific Quality of life (TQoL) was highest at AUBMC. Education was associated with functional recovery in the TQoL questionnaire; for every additional year of education there was an increase in the functional recovery domain of 0.03.
Conclusion:
Individuals that experienced moderate-to-severe injury in Beirut, Lebanon, suffered financial repercussions, including reductions in income, less employment, or unemployment. Across all patients surveyed, higher level of education was associated with better functional quality of life. More study into the intricacies of accessing healthcare care in Lebanon, especially given the current economic and political climate, are crucial to maintain the health of those experiencing injury and can help inform targeted interventions.
Keywords: Injury, Quality of Life, Access to care, Cost of care
Introduction
Injuries account for a significant portion of the global burden of disease, representing over 10% of all disability adjusted life years (DALYs) [1]. The injury burden disproportionately affects low- and middle-income countries (LMIC); over 90% of all injury-related deaths occur in LMICs, where lack of preventative measures and under-resourced healthcare systems contribute to difficulties in mitigating injury-related disabilities and healthcare impacts [2]. The Eastern Mediterranean region faces large injury-associated healthcare impacts, where unintentional injury is the leading cause of death, and the second leading contributor of DALYs [3]. Lebanon, a middle-income country in the Eastern Mediterranean Region, is no exception, with the World Health Organization (WHO) reporting that injury is the third leading cause of death and the fifth leading contributor of DALYs [4].
These injuries often contribute to dramatic and immediate reductions in the quality of life for injured individuals. A systematic review of literature pertaining to quality of life after road traffic injuries demonstrated that quality of life levels for patients experiencing moderate to severe injury never return to those of population-based controls, even in the long-term [5]. Different demographic, biological, and socioeconomic factors can impact quality of life outcomes following injury, with lower socioeconomic status (SES), female gender, older age, and post-traumatic stress disorder being associated with worse outcomes [5–11]. Though SES can impact trauma outcomes, trauma itself has substantial impacts on post-injury socioeconomic status. One follow-up study of patients who experienced moderate to severe injury reported that four years after hospital discharge roughly 20% of respondents did not return to work as a result of injury [12]. Even if able to return to work, nearly 88% of injured individuals suffer long-term financial repercussions because of injury [10]. These repercussions, including reduced income, unemployment, and increased financial burden, worsened health outcomes and decreased quality of life metrics [10], [13].
Individuals living in Lebanon are particularly vulnerable to the financial impacts of injury and the associated health consequences. It is estimated that roughly 43% of people living in Lebanon lack basic forms of health insurance, with out-of-pocket spending representing roughly 58–75% of all health-related expenses [14–16]. To date, there are few studies on the financial impact of injury to families in Lebanon, and the associated health consequences. This study aims to help fill in the knowledge gap by assessing the financial impact of injury to families and examining whether different demographic variables and SES metrics such as income and education impact patient-reported trauma-specific quality of life outcomes.
Methods
Setting and design
This study adopted a prospective cohort methodology to assess the impact of socioeconomic status (SES) on trauma-specific quality of life for patients 12–24 months after experiencing moderate to severe injury in Beirut, Lebanon. Patients were contacted by phone to complete a questionnaire in Arabic.
The study population was drawn from an actively managed research database at the American University of Beirut Medical Center (AUBMC), a major tertiary hospital located in the greater Beirut area. The database includes all patients who visited the Emergency Departments of five major hospitals in Beirut for unintentional injuries between 2017 and 2019. Of the 5 hospitals included in the database, 3 hospitals provided enrollment approval: one academic hospital (AUBMC), one private hospital—Geitawi Hospital (GH), and one public hospital—Rafic Hariri Governmental Hospital (RHGH).
Between June of 2017 and June of 2018, 3383 patients experiencing unintentional injury were treated in the Emergency Rooms of participating hospitals. Of these patients, only those who met the following inclusion criteria were enrolled in the study: patients must have been older than 18 years at the time of injury and have sustained moderate to severe injury treated in the emergency rooms of the hospitals included in the study. Injury severity was determined via documentation of functional impairment at discharge by the treating physician, classified as mild, moderate, or severe.
Both GH and RHGH provided hospital ethics review approvals for their patients being contacted for follow-up directly by the research team. AUBMC performed a primary screen of patients in which an AUBMC Emergency Room Physician made initial contact with all patients treated at AUBMC to obtain consent to be conacted by the research team. Each participant was called on two different occasions by an ED provider for this primary screen. See Fig. 1 for consort diagram.
Figure 1.
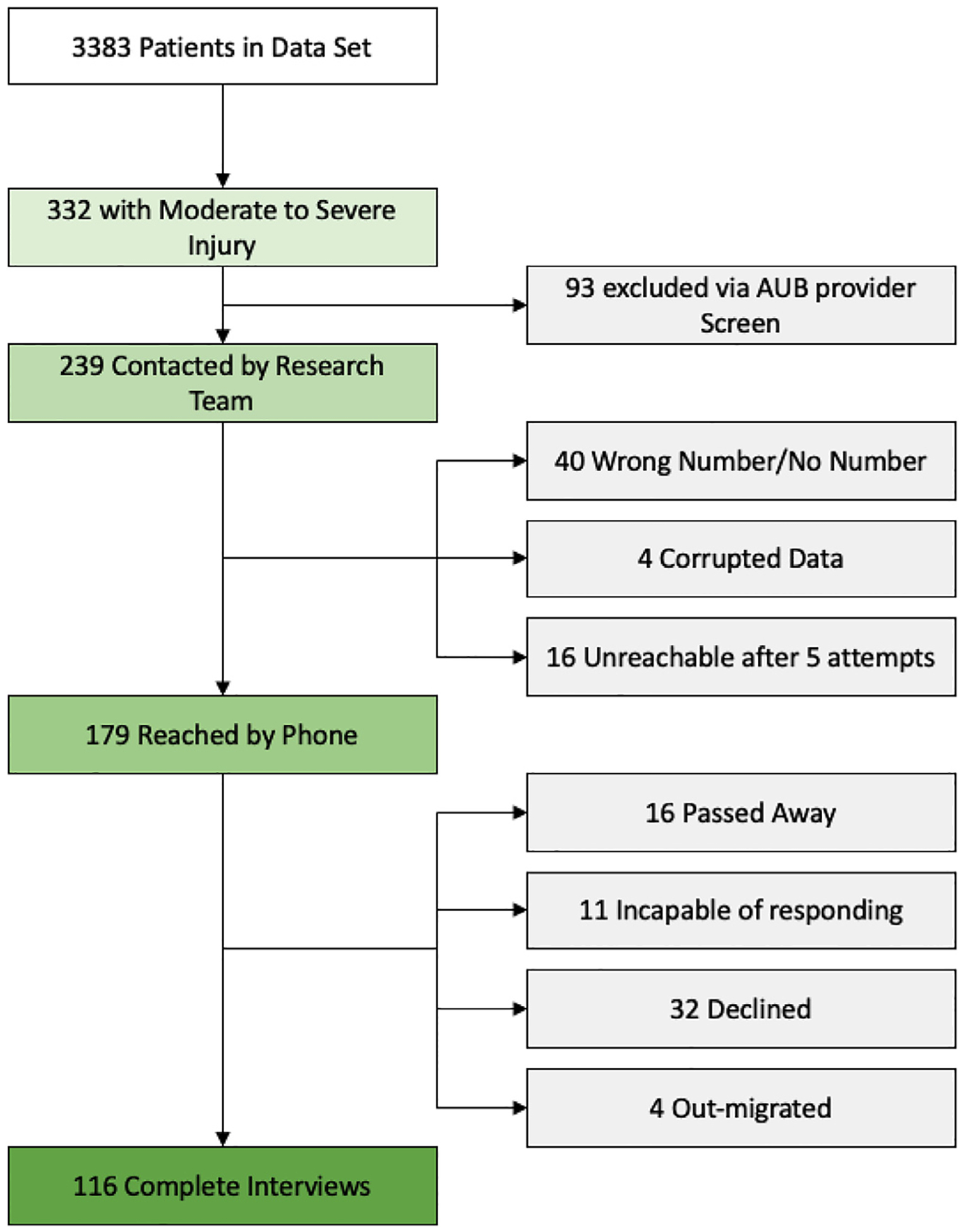
Survey response breakdown.
Per IRB-approved protocols at both Yale University and AUBMC, patients were contacted by phone to explain the purpose of the study, any risks or benefits, and to ask for consent to participate in the study, with emphasis that participation would not impact their future eligibility and access to healthcare services. In appreciation for their time, participants who completed the interview over the phone were given $10 USD through a phone transfer immediately after the interview. Each patient was called 5 times, with at least two days in between each attempt, before they were considered unreachable.
Interview and questionnaire
The phone interviews included different questions about socioeconomic status, access to care, the financial impact of injury, and quality of life as assessed through the Trauma Quality of Life Questionnaire [17].
Socioeconomic Status: The survey assessed the socioeconomic status of participants by asking questions about their educational background, including highest level of education attained, occupational status, income level, number of household members including dependents, and access to emergency funds.
Access to Care: Two questions were adapted from the Access to Healthcare Survey developed by the U.S. Department of Health and Human Services Agency for Healthcare Research and Quality [18]. These questions ask whether, and for what reasons, patients have had trouble accessing medical care, tests, treatments, or prescription medications following Emergency Department discharge.
- Financial Impact of Injury: The financial impact of injury was assessed by gauging the following: capacity to return to work post-injury, number of days of work or school lost by the patient due to injury, number of days of work or school lost from immediate family members due to patient injury, and out-of-pocket costs associated with initial Emergency Department care, including the total amount of money, if any, borrowed to help cover those costs. These metrics were combined into an equation to determine the total financial impact of injury to patients in the 12 months following injury. The equation, in general terms, sums the total out of pocket cost for treatment, the income lost during recovery (if able to return to work), and any income differential resulting from injury. The following equation was used:
(1) Trauma Quality of Life Questionnaire (TQoL): The Trauma Quality of Life Questionnaire, a validated survey used to assess quality of life following trauma, was used to gauge the impact of injury [17]. The TQoL is a five-domain questionnaire assessing domains that are unique to trauma populations, including emotional well-being, functional engagement, recovery/resilience, peritraumatic experience, and physical well-being. This study’s survey used the four domains with strongest inter-item reliability, which include emotional well-being, functional engagement, recovery/resilience, and physical well-being, to assess post-traumatic quality of life, taking a similar approach to the FORTES study [7].
The tool is used to provide a snapshot of the quality of life for people following injuries, though lacks the option of incorporating disabilities that exist from prior injuries. To help control for the impact of prior injuries and disabilities on the TQoL outcome, the study team asked each question with a particular focus on the injury that was represented in the study database. For example, when asked whether they strongly disagree, disagree, agree, or strongly agree to the phrase “I need help with walking,” participants were instructed to reference whether the injury in question impacted their capacity to walk, and if it did not, they would select strongly disagree, ensuring that the phrases in question referred to the injury represented in the database.
Data analysis
Data were collected over the phone on written surveys and then transferred to a digital Qualtrics form. To increase brevity and respect the time of all those interviewed, questions that were not relevant to some individuals were omitted. For those who were unemployed or retired without pension, income was set to $0. Additionally, for those who reported no change in employment or income after injury, their post-injury income was set to their pre-injury income.
Patient demographics and characteristics, stratified by hospital, were summarized using mean and standard deviation for continuous variables and frequency and percent for categorical variables. Mean TQoL scores for the four domains were assessed with multivariable generalized linear models. The models were adjusted for participant age, research institution, education level, and household income at time of survey. Contrast statements were constructed to compare differences in TQoL between the research institutes. A paired t-test was used to evaluate difference in income before and after injury.
All statistical analyses were performed using SAS/STAT Software, version 9.4 (SAS Institute, INC., Cary, NC). The significance level was set as p<0.05, two-sided.
Results
332 patients (190 AUBMC, 81 GH, 61 RHGH) met the inclusion criteria to be included in the study (Fig. 1). Ninety-three out of the 332 individuals were excluded via the AUBMC primary screen. These individuals were excluded for several reasons including some having passed away, some being unreachable during the two separate attempts to contact, some declining contact by the study team, and some having wrong, or no phone numbers listed. Of the remaining 239 patients from all three hospitals, 40 had wrong numbers/no number listed in the database, four had corrupted data in the database making them unreachable, and 16 were unreachable after five attempts to contact, leaving 179 who were reached by phone. Of these 179 individuals, 116 responded and completed the interview, 32 declined to participate, 16 were identified as having passed away by relatives since their admission, 11 were incapable of responding to the survey, and 4 had migrated out of Lebanon. The 11 individuals who were incapable of filling out the survey included one person who spoke neither English nor Arabic, two who could not provide any information about their injury because it was related to government defense, and eight who did not have the mental capacity to respond either because of amnesia with respect to the incident [7] or being in a coma since the injury [1]. The overall response rate for the survey was 116/332 (34.9%). When only including individuals living in Lebanon with correct contact information available to the study team, 116/148 filled out the survey, for a response rate of 78.9%.
Demographics and socioeconomic status of participants
The demographics and socioeconomic characteristics of all respondents, stratified by hospital, are outlined in Table 1. The average age of the respondents was 56.5 years (AUBMC 59.4, GH 59.7, RHGH 45.8). Half of all respondents (58/116) were female. The average household size was 3.9 individuals (AUBMC 3.5, GH 3.7, RHGH 5.3).
Table 1.
Population demographics, economic impact of injury, and access to care for injured patients.
| Research institute | ||||
|---|---|---|---|---|
| AUBMC | RHGH | GH | Total | |
| (N = 73) | (N = 25) | (N = 18) | (N = 116) | |
| Age (yr) | ||||
| Mean (SD) | 59.44 (20.88) | 45.76 (22.13) | 59.72 (26.06) | 56.53 (22.53) |
| Gender | ||||
| Female | 38 (52.05%) | 10 (40.00%) | 08 (44.44%) | 56 (48.28%) |
| Years of education | ||||
| Mean (SD) | 12.33 (5.58) | 7.25 (4.26) | 7.06 (5.44) | 10.44 (5.83) |
| Household size | ||||
| Mean (SD) | 3.48 (1.60) | 5.32 (2.69) | 3.72 (1.90) | 3.91 (2.05) |
| Total family combined income | ||||
| Mean (SD) | 3019.79 (2386.48) | 810.07 (504.16) | 1161.41 (987.75) | 2264.70 (2190.46) |
| Working situation one month prior to injury | ||||
| Full-time | 33 (45.21%) | 13 (52.00%) | 05 (27.78%) | 51 (43.97%) |
| Part-time | 01 (01.37%) | 01 (04.00%) | 03 (16.67%) | 05 (04.31%) |
| Employed after injury | ||||
| Yes | 30 (83.33%) | 9 (64.28%) | 06 (75.00%) | 45 (80.35%) |
| Change in employment after injury | ||||
| Yes | 04 (13.33%) | 06 (66.67%) | 01 (16.67%) | 11 (25.00%) |
| Income (one month prior to injury) | ||||
| Mean (SD) | 991.26 (1725.68) | 424.12 (471.56) | 352.72 (528.85) | 769.95 (1427.08) |
| Income (when interviewed) | ||||
| Mean (SD) | 965.82 (1761.99) | 223.44 (298.04) | 247.17 (493.15) | 694.31 (1457.58) |
| Days of work or school lost due to injury: Self | ||||
| Mean (SD) | 71.25 (63.58) | 164.66 (125.93) | 63.67 (69.93) | 86.33 (86.26) |
| Days of work or school lost due to injury: Family | ||||
| Mean (SD) | 4.14 (12.31) | 25.36 (62.92) | 14.76 (27.14) | 10.32 (33.31) |
| Cost of injury | ||||
| Mean (SD) | 3150.41 (10323.19) | 3338.53 (9819.17) | 1780.83 (3797.68) | 2975.42 (9430.75) |
| Amount borrowed for injury | ||||
| Mean (SD) | 1664.35 (8000.48) | 3061.93 (9865.18) | 1375.00 (3786.83) | 1922.88 (7928.79) |
| Emergency funds | ||||
| Mean (SD) | 6402.99 (12367.48) | 164.56 (237.78) | 894.28 (2112.30) | 4165.11 (10189.48) |
| Trouble getting medical care, tests, or treatments your Emergency Room physician or follow-up physician believed necessary | ||||
| No | 61 (83.56%) | 14 (56.00%) | 10 (55.56%) | 085 (73.28%) |
| Yes | 12 (16.44%) | 11 (44.00%) | 08 (44.44%) | 031 (26.72%) |
| Main reason you have not be able access follow-up care | ||||
| Couldn’t afford care | 03 (25.00%) | 10 (90.91%) | 02 (25.00%) | 015 (48.39%) |
| Insurance company wouldn’t approve, cover, or pay for care | 04 (33.33%) | 01 (9.09%) | 00 (0.00%) | 005 (16.13%) |
| Other | 05 (41.67%) | 00 (0.00%) | 06 (75.00%) | 011 (35.48%) |
| Trouble getting prescription medications your Emergency Room physician or follow-up physician believed necessary | ||||
| No | 01 (1.37%) | 09 (36.00%) | 02 (11.11%) | 012 (10.34%) |
| Yes | 72 (98.63%) | 16 (64.00%) | 16 (88.89%) | 104 (89.66%) |
| Main reason you have not been able to obtain prescription medications | ||||
| Couldn’t afford care | 00 (0.00%) | 08 (88.89%) | 01 (50.00%) | 009 (75.00%) |
| Insurance company wouldn’t approve, cover, or pay for care | 00 (0.00%) | 00 (0.00%) | 01 (50.00%) | 001 (8.33%) |
| Other | 01 (100.00%) | 01 (11.11%) | 00 (0.00%) | 002 (16.67%) |
AUBMC=American University of Beirut Medical Center, RHGH= Rafic Hariri Governmental Hospital, GH= Geitawi Hospital
The average number of years of education across all participants was 10.4 years (AUBMC 12.3 years, RHGH 7.3 years, GH 7.1 years) (Table 1). The average monthly household income of patients was 2264.7 USD across all participants (AUBMC 3019.8 USD, GH 1161.4 USD, RHGH 810.1 USD) (Table 1). The average total emergency funds across all participants was 4165.1 USD. Patients at AUBMC had more financial reserve than patients at GH; both had more reserve than patients at RHGH. AUBMC Patients had access to emergency reserves of an average of 6403 USD, compared to GH 894.3 USD, and 164.6 USD for RHGH (Table 1).
One month prior to injury, roughly 50% of all participants were employed either full or half-time, with the exact breakdown of work-status as follows: 51 Full-time, 5 Part-Time, 27 Keeping House or Raising children, 26 retired, 1 Looking for Work, 3 Unemployed, and 3 students.
Financial impact of injury
Most participants experienced financial repercussions associated with injury, both directly from healthcare costs and from impacts on their income and employment status. The average out of pocket cost for medical expenses across all 116 participants was 2975.4 USD (AUBMC 3150.4 USD; RHGH 3338.5 USD, GH 1780.8 USD) (Table 1). Patients borrowed an average of 1922.9 USD, or 64.6% of the total cost to help cover these bills (Table 1). The percent of total medical expenses that were borrowed varied by hospital; patients at the RHGH borrowed the most at 91.7% compared to 52.8% at AUBMC and 77.2% at GH (Table 1).
These financial costs and associated loan burdens were also exacerbated by reductions in income associated with injury. The 56 individuals employed either full or part-time at the time of injury experienced an average reduction of roughly 261.6 USD (95% CI (Confidence Interval) −383.0, 140.3) (Table 2). The average monthly income prior to injury was 1582.4 USD, and 1320.8 USD afterwards. This difference was statistically significant (p < 0.001) AUBMC patients had the lowest income reduction at 208.3 USD, or 9.8% loss in monthly income, as compared to drops of 406.8 USD, or 53.7%, at the Rafic Hariri Governmental Hospital, and 237.5 USD, or 33.7%, at Geitawi hospital (Table 2).
Table 2.
Demographics and economic profile/impact of injury for employed individuals.
| Research institute | ||||
|---|---|---|---|---|
| AUBMC | RHGH | GH | Total | |
| (N = 34) | (N = 14) | (N = 8) | (N = 56) | |
| Age (yr) | ||||
| Mean (SD) | 46.65 (15.38) | 40.43 (19.01) | 45.63 (25.03) | 44.95 (17.73) |
| Gender | ||||
| Female | 10 (29.41%) | 02 (14.29%) | 02 (25.00%) | 14 (25.00%) |
| Years of education | ||||
| Mean (SD) | 14.21 (4.01) | 8.23 (3.52) | 6.63 (5.37) | 11.69 (5.20) |
| Household size | ||||
| Mean (SD) | 3.94 (1.79) | 5.07 (2.97) | 4.63 (2.07) | 4.32 (2.19) |
| Employed after injury | ||||
| Yes | 29 (85.29%) | 9 (64.2%) | 06 (75.00%) | 44 (78.57%) |
| Change in employment after injury | ||||
| Yes | 04 (13.79%) | 06 (66.67%) | 01 (16.67%) | 11 (25.58%) |
| Income (one month prior to injury) | ||||
| Mean (SD) | 2128.29 (2001.03) | 757.36 (372.47) | 706.13 (599.41) | 1582.39 (1717.61) |
| Income (when interviewed) | ||||
| Mean (SD) | 1920.74 (2123.14) | 350.57 (326.07) | 468.63 (653.24) | 1320.75 (1830.79) |
| Total family combined income | ||||
| Mean (SD) | 3148.41 (2323.42) | 703.76 (315.59) | 1355.75 (1198.20) | 2281.15 (2160.58) |
| Days of work or school lost due to injury: Self | ||||
| Mean (SD) | 71.25 (63.58) | 164.66 (125.93) | 63.67 (69.93) | 86.33 (86.26) |
| Days of work or school lost due to injury: Family | ||||
| Mean (SD) | 5.09 (16.66) | 37.00 (82.15) | 15.75 (26.84) | 14.59 (45.14) |
| Cost of injury | ||||
| Mean (SD) | 3202.33 (10483.55) | 4940.31 (13060.28) | 402.75 (640.52) | 3236.89 (10402.86) |
| Amount borrowed for injury | ||||
| Mean (SD) | 1642.15 (5631.82) | 4778.46 (13104.86) | 343.75 (640.00) | 2240.74 (7877.77) |
| Emergency funds | ||||
| Mean (SD) | 6117.06 (11134.61) | 213.07 (294.57) | 991.50 (2303.47) | 3908.84 (9100.14) |
| Economic Impact | ||||
| Mean (SD) | 13967.64 (42289.67) | 4193.22 (3138.07) | 1342.89 (1190.63) | 10329.46 (34762.33) |
AUBMC=American University of Beirut Medical Center, RHGH= Rafic Hariri Governmental Hospital, GH= Geitawi Hospital
The opportunity cost of injury also contributes to this economic impact, with both patients and their families’ losing days of work or school due to injury. Of the 56 patients employed at the time of injury, twelve patients were unable to return to work, with 5 out of 34 patients at AUBMC, 5 out of 14 patients at the RHGH, and 2 out of 8 patients at GH unable to resume work by the time of follow-up (Table 2). Eleven patients, roughly 20% of these 56 individuals, had a change in occupation because of their injury (Table 2). The exact breakdown of pre- and post-injury employment outcomes can be found in appendix B.
Of those able to resume work, 86.3 days of work were lost on average due to patient injury (AUBMC 71.3, RHGH 164.7, GH 63.7 days) (Table 2). Across all respondents, immediate family members lost an average of 10.3 days to assist with their care (AUBMC 4.1, RHGH 25.4, and GH 14.8 days) (Table 1).
For those employed at the time of injury, the average calculated economic impact (Eq. 1) in the year immediately after injury was 10,329.46 USD (AUBMC 13,967.64 USD, RHGH 4193.22 USD, and GH 1342.89 USD) (Table 2).
Access to care following injury
Thirty-one patients (26.72%) had difficulty accessing medical care, tests, or treatments deemed necessary by their clinicians following injury, (AUBMC 12 (16.44%), RHGH 11 (44.00%), and GH 8 (44.44%) patients) (Table 1). The primary obstacle to accessing care was cost with 15 (48.39%) of the 31 patients indicating they could not afford care and 5 (16.13%) indicating their insurance would not approve, cover, or pay for their care (Table 1). The remaining 11 (35.48%) indicating “other” as the reason for being unable to access care with reasons including: significant wait times [4], no hospital availability at the time of injury [2], needing government connections to receive care [5]. Twelve (10.34%) of the 116 patients reported difficulty obtaining prescribed medications (11 (91.66%) due to issues of affordability, and one (8.33%) reporting the medication was not available in Lebanon and it had to be imported from Turkey (Table 1).
Trauma quality of life regression results
TQoL regression tables can be found in Table 3. There are differences in mean adjusted TQoL between the different institutions, but there is no difference based on age of the patients. Years of education and household income are not significantly related to emotional, recovery, or physical QOL.
Table 3.
Relationship of QOL Domains with age, institute, education, household income.
| Emotional QOL | Estimate | 95% CI | P-value |
|---|---|---|---|
|
Age (yr)
Research Institute: |
0.01 | (−0.01, 0.02) | 0.39 |
| AUBMC | 3.23 | (3.08, 3.39) | <0.001 |
| RHGH | 2.72 | (2.43, 3.02) | <0.001 |
| GH | 2.70 | (2.39, 3.01) | <0.001 |
| Years of education | 0.01 | (−0.01, 0.04) | 0.29 |
| Household income | 0 | (−0.00, 0.00) | 0.26 |
| Functional QOL | Estimate | 95% CI | P-value |
|
Age (yr)
Research Institute: |
−0.02 | (−0.03, 0.00) | 0.05 |
| AUBMC | 3.49 | (3.28, 3.70) | <0.001 |
| RHGH | 2.97 | (2.58, 3.36) | <0.001 |
| GH | 3.40 | (2.99, 3.81) | <0.001 |
| Years of education | 0.04 | (0.01, 0.08) | 0.01 |
| Household income | 0 | (−0.00, 0.00) | 0.82 |
| Recovery QOL | Estimate | 95% CI | P-value |
|
Age (yr)
Research Institute: |
0 | (−0.01, 0.00) | 0.3 |
| AUBMC | 2.53 | (2.42, 2.65) | <0.001 |
| RHGH | 2.33 | (2.12, 2.55) | <0.001 |
| GH | 2.24 | (2.02, 2.47) | <0.001 |
| Years of education | 0 | (−0.02, 0.02) | 0.92 |
| Household income | 0 | (−0.00, 0.00) | 0.58 |
| Physical QOL | Estimate | 95% CI | P-value |
|
Age (yr)
Research Institute: |
0 | (−0.02, 0.01) | 0.58 |
| AUBMC | 3.21 | (3.00, 3.42) | <0.001 |
| RHGH | 2.49 | (2.09, 2.89) | <0.001 |
| GH | 2.69 | (2.27, 3.12) | <0.001 |
| Years of education | 0 | (−0.03, 0.04) | 0.92 |
| Household income | 0 | (−0.00, 0.00) | 0.22 |
AUBMC=American University of Beirut Medical Center, RHGH= Rafic Hariri Governmental Hospital, GH= Geitawi Hospital
Mean adjusted Emotional TQoL for AUBMC, RHGH and GH are: 3.37 (95% CI 2.62, 4.13), 2.52 (1.80, 3.25), and 2.22 (1.37, 3.08) respectively (Table 3). The comparisons of mean scores with AUBMC & RHGH and AUBMC & GH are significantly different; patients from AUBMC have higher emotional TQoL score, on average. Mean adjusted functional TQoL for AUBMC, RHGH, and GH are: 3.49 (3.28, 3.70), 2.97 (2.58, 3.36), and 3.40 (2.99, 3.81) respectively (Table 3). For each 1-year increase in years of education, the average reported functional TQoL score increases by 0.04 (0.01, 0.08) (Table 3). Mean adjusted recovery TQoL for AUBMC, RHGH, and GH are: 2.53 (2.42, 2.65), 2.33 (2.12, 2.55), and 2.24 (2.02, 2.47) respectively. AUMBC has higher average recovery TQOL score than RHGH by 0.57 (0.01, 1.13) (Table 3). Mean adjusted physical TQoL for AUBMC, RHGH, and GH are: 3.21 (3.00, 3.42), 2.49 (2.09, 2.89), and 2.69 (2.27, 3.12) respectively (Table 3).
Discussion
The results of this study document several disparities in the impacts of trauma on patients’ long-term physical and economic health, with a myriad of social determinants of health impacting the degree to which patients were able to recover from their injuries including income, educational attainment, and access to emergency funds through personal networks.
Financial impacts
The direct financial impact of injury in Beirut often involves high out-of-pocket costs that require loans to help cover the balance. The average out-of-pocket cost across the 116 participants in this study was 2975 USD, with 1922 USD (65%), coming from loans. This burden is unevenly distributed. Patients at the AUBMC borrowed on average 53% of their total out-of-pocket costs compared to 91.7% at the RHGH and 77.2% at the GH. This difference can largely be explained by financial reserve, with patients at the AUBMC reporting higher average incomes as well as access to more emergency funds than patients at either of the other hospitals. These large out-of-pocket expenditures are consistent with previous estimates and studies demonstrating sizeable out-of-pocket costs associated with care in Lebanon [14–16]. Though the exact payment made to the hospital, including both personal and insurance-based contributions, was beyond the scope of this study, the high cost of injury in relation to individual income raises serious concerns regarding the affordability of existing healthcare options for injured patients in Beirut.
For those who were employed at the time of injury, the direct and indirect economic costs were particularly detrimental. Looking at the economic impact factor—which assesses direct and indirect costs in the 12 months following injury—costs associated with injury care represent an average of 6.5-months salary for injured patients. When factoring in existing living expenses, it could be many years, if ever, for a patient to be financially stable after injury. Roughly 21% of those who were employed at the time of injury were unable to return to work 1–2 years following injury, which is similar to the 20% reduction in employment four years after injury found in another study [12].
Even for those returning to work—either to a previous job or a new one—injured patients often experienced reductions in income. In this study, those employed at the time of injury had an average 16.3% reduction in income following injury; though similar to the trend observed with borrowing, the reduction in income was different depending on hospital. Those treated at the AUBMC, who on average had the highest level of household income, education, and access to emergency capital, had the least income reduction, at 9.78%, as compared to 53.71% and 33.65% at the RHGH and GH, respectively.
Similarly, patients at the AUBMC had fewer days of employment lost as a result of injury than either RHGH or GH. This difference in income reduction and days of work lost can likely be attributed to types of occupations of those who are treated at the AUBMC in comparison to those who are treated at RHGH and GH. Looking at the occupation breakdown in Appendix B, those treated at AUBMC were mainly employed in administrative/managerial (knowledge worker) occupations whereas those at the RHGH and HG were more likely to be employed in occupations that are more physically demanding. These occupations, along with lower SES, have been shown to negatively impact return-to-work timelines [19]. Additionally, a majority of the patients who were eventually physically able to return to work at the RHGH found themselves in new occupations with lower incomes, either as a result of new physical limitations or their old occupation being filled in their absence. The differences in financial outcomes between the three hospitals highlight how pre-injury SES can potentially influence post-injury employment and financial outcomes.
Disparities in follow-up care
After discharge, many patients experience challenges accessing follow-up care. Across the 116 participants, 26.72% had difficulty accessing medical care, tests, or treatments deemed necessary by their clinician following injury, with roughly two-thirds of individuals indicating affordability of care was the primary obstacle. The most recent estimates peg the uninsured rate in Lebanon at a staggering 43%, and even those with insurance incur significant out-of-pocket costs, with out-of-pocket costs accounting for between 58% and 75% of all health expenditure [14–16]. For those who are uninsured in Lebanon, the Ministry of Health is meant to exist as a catch-all and final line of defense for health coverage, though many find it challenging or impossible to get coverage through the ministry [20]. Interestingly, of the 11 respondents who indicated “other” as the reason for their inability to access follow-up care, 5 individuals remarked that they lacked the government connections necessary to receive care, and those who described long wait times for medical care remarked that the process would be more efficient if they knew someone in the government or had political connections. A recent study delving deeper into this phenomenon found a positive association between political activism and the probability of receiving health aid, with those with the highest political activity being four times more likely to get their healthcare covered through micro-level political institutions than those who were the least politically active [21].
Post-trauma quality of life differences
In addition to higher levels of access to care, those at the AUBMC had higher Trauma-specific Quality of Life indices. For both the emotional and recovery domains of the TQoL, AUBMC had statistically significant better outcomes, even while adjusting for age and family income. Surprisingly, family income was not significantly associated with the four TQoL domains when controlling for other variables. Previous studies using the TQoL survey in different populations have found age, sex, and education to be related to long-term trauma outcomes [7]. In this study, higher levels of education were associated with greater functional TQoL scores, but age was not. The explanation for this variation is likely multi-factorial. Though income was not associated with better outcomes, it is possible that those who go to the AUBMC for medical care are more politically connected and have access to resources via informal channels as previously mentioned. Cultural variation in interpretation of the TQoL questions also likely has a bearing. For example, in response to item number 36 of the TQoL survey, “I have to rely on others, such as family, friends, social security, or community support programs because of my current financial limitations,” five individuals, despite having little to no financial reserve, responded that they “strongly disagree” on the basis that no social safety net systems or community support networks exist for them in Lebanon. For these individuals, the question was met with strong emotional responses regarding the lack of social services, reflecting a mismatch between the standardized question within the TQoL survey and the mental models and tangible realities of those respondents.
Qualitative response data
Aside from the quantitative data collected as part of the study, the comments made by individuals with respect to their healthcare were particularly concerning. Many indicated the challenging nature of the point-of-service collections system employed in Lebanon, where you must pay the full cost of any medical care prior to receiving the service. One study in Beirut looking at individuals who left the ED without being seen found that lack of insurance and other financial reasons accounted for 66.9% and 12.8%, respectively, of all individuals leaving the emergency room before being seen by a provider [22]. This often complicates the delivery of care, with individuals having to wait to secure a loan before receiving treatment. One individual in the study commented that they had to leave the ED and spend 7 days at home before eventually securing the capital necessary for an urgent operation. One individual of Syrian nationality remarked that they could not afford the operation necessary to restore their mobility, so they went back to still war-torn Syria to see if it was possible to get the procedure done there. These anecdotes cannot be appreciably analyzed as they fall outside the scope of this study, but they do provide some perspective in addition to the quantitative data and can inform future study directions. The loan burden associated with injuries was substantial, and often leaves people in dire financial states. Further mixed qualitative and quantitative study into the relationship between injury, SES, and outcomes can help to elucidate potential areas of focus for improvement. Additionally, discerning how medical outcomes are impacted by individuals deferring care until they have the means to pay would provide further insight into the total impact of injury on individuals.
National economic & political impacts
The current political and economic climate in Lebanon in 2021 is likely only further challenging the prospects of those experiencing injury and other health problems more broadly. The Lebanese Lira has lost 80% of its value in the last calendar year 2020 [23], and estimates report that over half of the country now lives in poverty, a significantly higher portion than when the study was conducted in the summer of 2019, where the poverty rate stood at 28% [24]. With the banking industry in Lebanon pausing most loans as a result of dried-up funds [25], those individuals who would have taken a loan to continue with their care in the Lebanese point-of-service payment system are now completely vulnerable to adverse and potentially treatable health outcomes associated with injury.
Limitations and challenges
This study had many limitations including challenges in connecting with patients following injury. In addition to many having passed away at the time of contact, many individuals had no available contact information. The outcomes for individuals with no contact information could have altered the results of this study. As part of the AUBMC Primary screen requirement, many individuals were filtered out, with reasons unknown to the research team.
As the Trauma Quality of Life survey was developed in the United States and in the English language, cultural variation between the United States and Lebanon could have impacted the results. Finally, clinician gestalt at the time of injury was used to determine whether an injury was mild, moderate, or severe, which is not the most robust mechanism of determining severity. More classic metrics, such as Injury Severity Score (ISS), would have been a more robust measure of clinical severity at the time of injury if available. Despite these shortcomings, the study provides valuable insight into the economic impact of injury at the individual level and draws from the experiences of individuals attempting to navigate the Lebanese healthcare system.
Conclusion
Individuals experiencing moderate to severe injury in Beirut, Lebanon, suffer financial repercussions 1–2 years following injury, with reduced levels of employment, a significant average reduction in income for those employed at the time of injury, and high economic impact in the twelve months following injury. Patients experienced sizeable out-of-pocket expenses related to injury and borrowed on average a majority of that cost. Patients at the AUBMC, who have higher metrics of SES than both RHGH and GH, had a higher quality of life following injury as evaluated by the TQoL survey. Higher levels of education were significantly associated with better functional quality of life. More study into the intricacies of accessing care in the Lebanese Healthcare system, especially given the current economic and political climate, are crucial to maintain the health of those experiencing injury and can help inform targeted interventions.
Supplementary Material
Acknowledgments
Thank you to the Yale School of Medicine Medical Student Fellowship for providing financial support in the form a stipend to the primary author.
Role of Funding
Yale School of Medicine Medical Student Fellowship provided a stipend to the primary author. No funding source was involved with study design, data collection, data analysis, or manuscript drafting.
Footnotes
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.injury.2022.08.014.
References
- [1].Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Injury Prev 2016;22(1):3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Org 2009;87:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Obermeyer CM, Bott S, Sassine AJ. Arab adolescents: health, gender, and social context. J Adolesc Health 2015;57(3):252–62. [DOI] [PubMed] [Google Scholar]
- [4].Country Profile — Lebanon World Health Organization [cited 2020 Jun 4]; Available from: http://www.who.int/countries/lbn/en/.
- [5].Rissanen R, Berg HY, Hasselberg M. Quality of life following road traffic injury: a systematic literature review. Accid Anal Prev 2017;108:308–20. [DOI] [PubMed] [Google Scholar]
- [6].Gudmundsdottir B, Beck JG, Coffey SF, Miller L, Palyo SA. Quality of life and post trauma symptomatology in motor vehicle accident survivors: the mediating effects of depression and anxiety. Depress Anxiety 2004;20(4):187–9. [DOI] [PubMed] [Google Scholar]
- [7].Haider AH, Herrera-Escobar JP, Al Rafai SS, Harlow AF, Apoj M, Nehra D, et al. Factors associated with long-term outcomes after injury: results of the Functional Outcomes and Recovery After Trauma Emergencies (FORTE) multicenter cohort study. Ann Surg 2020;271(6):1165–73. [DOI] [PubMed] [Google Scholar]
- [8].Holbrook TL, Hoyt DB. The impact of major trauma: quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. J Trauma Acute Care Surg 2004;56(2):284–90. [DOI] [PubMed] [Google Scholar]
- [9].Ioannou L, Cameron PA, Gibson SJ, Ponsford J, Jennings PA, Georgiou-Karistianis N, et al. Financial and recovery worry one year after traumatic injury: a prognostic, registry-based cohort study. Injury 2018;49(5):990–1000. [DOI] [PubMed] [Google Scholar]
- [10].Murphy PB, Severance S, Savage S, Obeng-Gyasi S, Timsina LR, Zarzaur BL. Financial toxicity is associated with worse physical and emotional long-term outcomes after traumatic injury. J Trauma Acute Care Surg 2019;87(5):1189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Rissanen R, Ifver J, Hasselberg M, Berg HY. Quality of life following road traffic injury: the impact of age and gender. Qual Life Res 2020;29(6):1587–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Collie A, Simpson PM, Cameron PA, Ameratunga S, Ponsford J, Lyons RA, et al. Patterns and predictors of return to work after major trauma: a prospective, population-based registry study. Ann Surg 2019;269(5):972–8. [DOI] [PubMed] [Google Scholar]
- [13].Gabbe BJ, Sleney JS, Gosling CM, Wilson K, Sutherland A, Hart M, et al. Financial and employment impacts of serious injury: a qualitative study. Injury 2014;45(9):1445–51. [DOI] [PubMed] [Google Scholar]
- [14].Ammar W Health beyond politics. Beirut, Lebanon: World Health Organization Country Office; 2009.
- [15].Kronfol N Access and barriers to health care delivery in Arab countries: a review. EMHJ-Eastern Mediterr Health J 2012;18(12):1239–46 2012. [DOI] [PubMed] [Google Scholar]
- [16].Salti N, Chaaban J, Raad F. Health equity in Lebanon: a microeconomic analysis. Int J Equity Health 2010;9:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wanner JP, deRoon-Cassini T, Kodadek L, Brasel K. Development of a trauma-specific quality of life measurement. J Trauma Acute Care Surg 2015;79(2):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Access to Care Supplement US Department of Health and Human Services AfHRaQ. US Department of Health and Human Services, Agency for Healthcare Research and Quality; 2020. [citedJun 4]; Available from: https://meps.ahrq.gov/survey_comp/hc_survey/2016/Ac-111416.pdf.
- [19].Cancelliere C, Donovan J, Stochkendahl MJ, Biscardi M, Ammendolia C, Myburgh C, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap 2016;24(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kronfol NM. Rebuilding of the Lebanese health care system: health sector reforms. EMHJ-Eastern Mediterr Health J 2006;12(3–4):459–73 2006. [PubMed] [Google Scholar]
- [21].Chen B, Cammett M. Informal politics and inequity of access to health care in Lebanon. Int J Equity Health 2012;11:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hitti E, Hadid D, Tamim H, Al Hariri M, El Sayed M. Left without being seen in a hybrid point of service collection model emergency department. Am J Emerg Med 2020;38(3):497–502. [DOI] [PubMed] [Google Scholar]
- [23].Watch HR. Lebanon: events of 2020. Human Rights Watch; 2020 [cited 2021 2021]; Available from: https://www.hrw.org/world-report/2021/country-chapters/lebanon.
- [24].United Nations Economic and Social Commission for Western Asia (ESCWA). Poverty in Lebanon: solidarity is vital to address the impact of multiple over-lapping shocks. 2020.
- [25].Francis TAE. As Lebanon’s banks struggle to raise capital, a deadline looms. 2021. February 15, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


