Abstract
Background
The adjunctive therapeutic potential of simvastatin in schizophrenia treatment has generated interest due to its anti-inflammatory and neuroprotective properties. This meta-analysis aims to assess the efficacy of simvastatin as an adjunct treatment for schizophrenia, synthesizing results from various controlled trials.
Methods
We performed a comprehensive search of databases including PubMed, Embase, and the Cochrane Library for randomized controlled trials (RCTs) evaluating the efficacy of simvastatin as an adjunct therapy in patients with schizophrenia. The primary outcome measures were improvements in the Positive and Negative Syndrome Scale (PANSS) scores. Secondary outcomes included changes in overall clinical condition and level of functioning. Data were pooled using random-effects models, and heterogeneity was assessed through I² statistics.
Results
The four RCTs included in the analysis represented 425 participants. The combined results demonstrated no significant advantage of simvastatin over placebo in reducing PANSS total scores with a pooled effect size (Standard Mean Difference, SMD) of −0.36 (95% Confidence Interval, CI: −0.82 to 0.11) at 1 month, and −1.80 (95% Confidence Interval, CI: −4.82 to 1.21) at 3 months, indicating minimal to no effect. Similarly, analyses of secondary outcomes showed no significant improvements in overall clinical condition and level of functioning. The studies exhibited low heterogeneity (I² = 0%).
Conclusion
This meta-analysis provides evidence that simvastatin, used as adjunctive therapy, does not significantly improve the symptomatic outcomes of schizophrenia compared to placebo. Although simvastatin is well-tolerated, its role in enhancing antipsychotic treatment efficacy in patients with schizophrenia appears limited. These findings suggest that simvastatin should not be recommended as an adjunctive treatment in the clinical management of schizophrenia. Further research may explore the potential subgroups that could benefit from such treatment or identify the biological reasons for the lack of efficacy.
Keywords: schizophrenia, simvastatin, adjunctive therapy, meta-analysis, randomized controlled trials, efficacy
Introduction
Schizophrenia is a chronic and severe mental disorder characterized by distortions in thinking, perception, emotions, language, sense of self, and behavior.1 This complex syndrome is associated with a variety of symptoms, often categorized as positive, negative, and cognitive deficits, substantially impacting the quality of life and functioning of affected individuals.2 Although the etiology of schizophrenia remains partially understood, it is widely acknowledged to be a multifactorial condition, with genetic, neurobiological, and environmental factors playing critical roles in its development and progression.3
Current treatment options for schizophrenia predominantly revolve around antipsychotic medications, which primarily target the dopaminergic system.4 Unfortunately, these conventional antipsychotics have limited efficacy against the negative and cognitive symptoms of the disorder and are frequently accompanied by significant side effects, highlighting the necessity for adjunctive treatments to address the breadth of symptoms experienced by patients.5
Emerging evidence has suggested a potential role for inflammatory processes in the pathophysiology of schizophrenia.6 Consequently, there has been growing interest in exploring anti-inflammatory agents,7,8 such as simvastatin, a lipid-lowering statin drug, for adjunctive treatment. Simvastatin has been subject to scrutiny in this context due to its neuroprotective and anti-inflammatory properties, which could hypothetically ameliorate various symptoms of schizophrenia.9,10
However, clinical trials investigating simvastatin as an adjunct to standard antipsychotic treatment have produced inconsistent and sometimes conflicting outcomes.11,12 This inconsistency presents a substantial challenge for clinicians considering simvastatin as a complementary approach in managing schizophrenia. Given the necessity for evidence-based treatments and the potential implications of employing statins adjunctively, a systematic consolidation of available data is essential to accurately assess the efficacy of simvastatin in this capacity.
This meta-analysis aims to integrate findings from various clinical trials to evaluate the overall efficacy of simvastatin as an adjunctive therapy in the treatment of schizophrenia. By reviewing and synthesizing the data from randomized controlled trials, we seek to provide a comprehensive understanding of whether simvastatin offers any tangible benefits for patients with schizophrenia when used alongside antipsychotic medications.
In addressing this question, we will examine the impact of adjunctive simvastatin therapy on various symptom domains within schizophrenia, including positive symptoms, negative symptoms, and cognitive function. In doing so, the present meta-analysis aims to offer evidence that could inform future clinical decisions and guide further research in the quest for effective treatments for this debilitating disorder.
Methods
This study is in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 statement.13 The study was not registered, and the study protocol was not applicable.
Search Strategy and Selection Criteria
This systematic review and meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.14 The Cochrane Central Register of Controlled Trials, MEDLINE, PubMed, Embase, and PsycINFO were searched, along with ClinicalTrial.gov from the date of database inception to Mar 1, 2023. The search strategy was the combination of “simvastatin” or “statin” and “schizophrenia” or “schizoaffective disorder” or “psychosis”. No language restrictions were applied.
In the systematic review, we included randomized controlled trials that examined the effects of adjunctive therapy with simvastatin on psychiatric symptoms of patients with schizophrenia. To determine comparisons that are applicable, we used a rigorous eligibility criterion. Two authors independently browsed and selected eligible studies through titles and abstracts.
Inclusion criteria in the study were the following: (1) randomized controlled trials; (2) according to Diagnostic and Statistical Manual (DSM) diagnostic criteria; (3) subjects treated and compliant with any antipsychotic, and received simvastatin treatment; and (4) Positive and Negative Syndrome Scale (PANSS). Exclusion criteria were as follows: (1) no data reported; and (2) multiple reports of the same study. Any disagreements were resolved by consensus or discussion with the third author.
Data Extraction and Assessment of Studies
Two authors extracted data from the included studies into a spreadsheet. Authors collected trials information including study characteristics (authors, year of publication, details of the trial, diagnostic status, doses of simvastatin, duration of treatment for simvastatin, and outcomes) and patients characteristics (sample size and age).
Two authors independently evaluated risk of bias using 2011 Cochrane Handbook tool, which includes random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and other sources of bias.15 Any discrepancy was resolved through consensus.
Outcomes and Statistical Analysis
A between-group meta-analysis was performed to compare psychiatric symptoms in schizophrenia patients with simvastatin adjunctive therapy. The primary outcome was PANSS scores (Positive and Negative Syndrome Scale). It should be noted that this outcome was designated as “primary” post hoc for the purposes of this systematic review. The secondary outcomes were CGI (Clinical Global Impression) and GAF (Global Assessment of Functioning). The outcomes at 1 month and 3 months are presented, because various trials reported the data at 1 month and 3 months respectively.
Continuous outcomes were combined using mean differences (MD). All trials reported continuous outcomes as the changes from the baseline, and the differences of these values between groups were presented as the efficacy in the full articles. These outcomes were also adjusted with the least-square methods. Statistical heterogeneity was assessed visually with Galbraith plots and statistically with the I2 and Q statistics.16 All analyses were conducted with Review Manager 5 software (Version 5.3, The Nordic Cochrane Centre, Copenhagen).
Results
Overall Summary of Included Studies
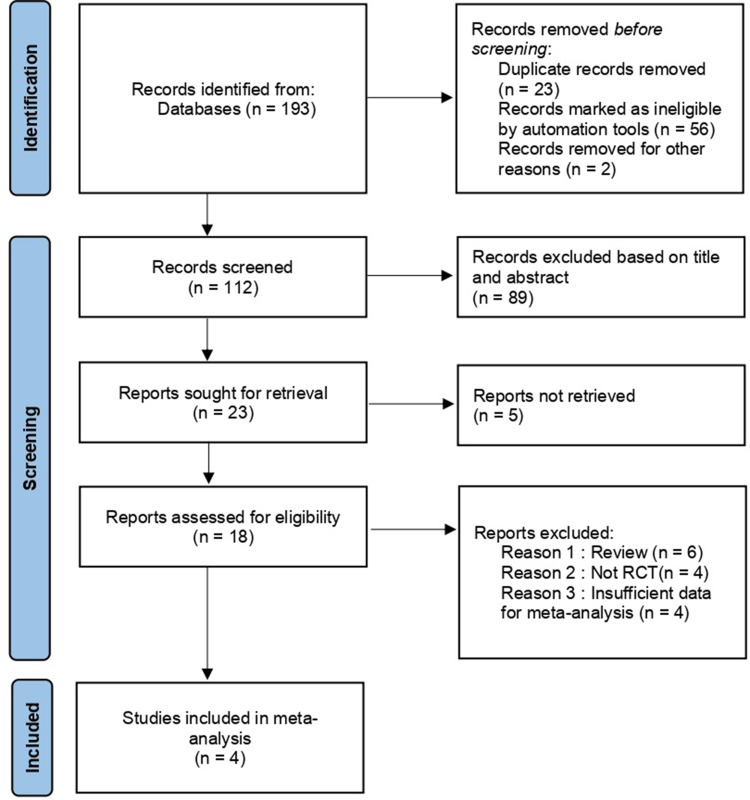
The results of the literature search and screening process are summarized in Figure 1. The literature search totaled 193 records. Of these studies, 4 randomized, placebo-controlled trials involving 425 participants met the eligibility criteria. Eligible participants were adults (aged ≥18 years), based on DMS-V criteria, were included in the analysis. The study durations varied from 2 weeks to 12 months. Key characteristics are displayed in Table 1. All trials were published in clinical journals.
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) flow diagram.
Table 1.
Characteristics of Included Studies
| Author, year | Inclusion Criteria | Diagnostic Status | Duration | Treatment Group, (No. of Participants) | Age Range | Outcomes |
|---|---|---|---|---|---|---|
| Chaudhry, 201417 | SZ, SA, P-NOS, SF | DSM-IV | 12 weeks | Simvastatin 20–40mg/day (11)/Placebo (12) | 18–65 | PANSS total, positive, negative, and general,CGI, GAF |
| Sommer, 202111 | SZ, SA, P-NOS, SF | DSM-IV | 48 weeks | Simvastatin 40mg/day (56)/Placebo (48) | 18–50 | PANSS total, positive, negative, and general,GAF |
| Tajik-Esmaeeli, 201618 | SZ | DSM-IV-TR | 8 weeks | Simvastatin 40mg/day (33)/Placebo (33) | 18–60 | PANSS total, positive, negative, and general |
| Weiser, 202312 | SZ, SA | DSM-IV-TR | 12 weeks | Simvastatin 40mg/day (116)/Placebo (116) | 18–65 | PANSS total, positive, negative, and general,CGI |
Abbreviations: PANSS, Positive and Negative Syndrome Scale; DSM-(TR), Diagnostic and Statistical Manual of Mental Disorders (Text Revision); SZ, schizophrenia; SA, schizoaffective disorder; P-NOS, psychosis not otherwise specified; SF, schizophreniform disorder; CGI, Clinical Global Impression; GAF, Global Assessment of Functioning.
Risk of Bias in Included Studies
All studies, which adequately reported the prespecified primary outcomes in full articles, had adequate sequence generation, allocation concealment, and blinding of outcome. The results are summarized in Table 2. All included studies were assessed independently by two authors, and the risk of bias for each item was categorized as “low risk”, “unclear” or “high risk”.
Table 2.
Risk of Bias in Included Studies
| 1st Author (Year) | Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessors | Incomplete Outcome Data | Selective Outcome Reporting | Other Source of Bias |
|---|---|---|---|---|---|---|---|
| Chaudhry, 201417 | Low | Low | Low | Low | Low | Low | Low |
| Sommer, 202111 | Low | Low | Low | Low | Low | Low | Low |
| Tajik-Esmaeeli, 201618 | Low | Low | Low | Low | Low | Low | Low |
| Weiser, 202312 | Low | Low | Low | Low | Low | Low | Low |
Primary Outcome Analysis
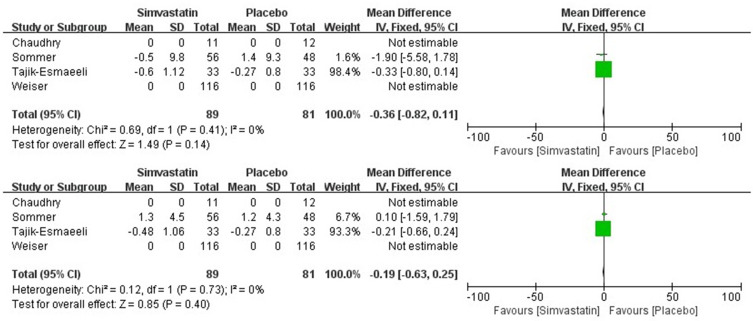
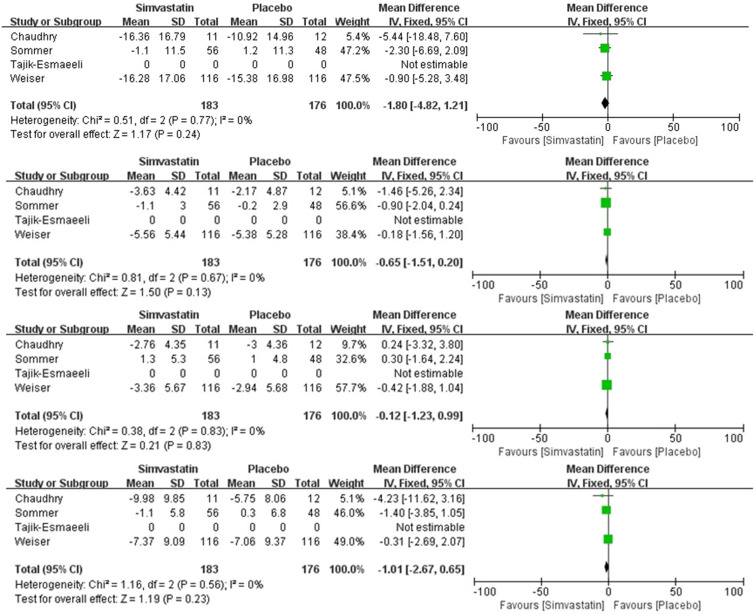
Pooled simvastatin add-on therapy showed no significant superiority over placebo in the improvement of PANSS total scores at 1 month (MD = −0.36; 95% CI, −0.82 to 0.11; p = 0.14; I2 = 0%). Individually, there was no association between the effect size for pooled simvastatin add-on therapy with respect to PANSS negative subscale (MD = −0.19; 95% CI, −0.63 to 0.25; p = 0.40; I2 = 0%) at 1 month (Figure 2). Similarly, Meta-regression analysis showed that there was no association between the effect size for pooled statin add-on therapy with respect to PANSS total scores (MD = −1.80; 95% CI, −4.82 to 1.21; p = 0.24; I2 = 0%), PANSS positive subscale (MD = −0.65; 95% CI, −1.51 to 0.20; p = 0.13; I2 = 0%), PANSS negative subscale (MD = −0.12; 95% CI, −1.23 to 0.99; p = 0.83; I2 = 0%) or PANSS general subscale (MD = −1.01; 95% CI, −2.67 to 0.65; p = 0.23; I2 = 0%) at 3 months (Figure 3).
Figure 2.
Summary of primary outcome analysis at 1 month (PANSS total scores and PANSS negative subscale).
Figure 3.
Summary of primary outcome analysis at 3 months (PANSS total scores, PANSS positive subscale, PANSS negative subscale and PANSS general subscale).
Secondary Outcome Analysis
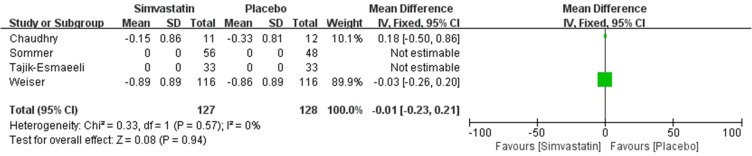
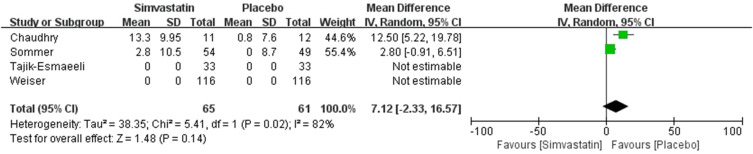
A total of 2 trials reported data on CGI and GAF at 3 months. Compared with the control group, simvastatin adjunctive therapy did not significantly affect CGI, and the pooled estimated change in CGI was −0.01 (95% CI, −0.23 to 0.21; p = 0.94; I2 = 0%) (Figure 4). Two studies provided data on GAF, and pooling the data of these studies showed that simvastatin adjunctive therapy failed to show a significant effect on GAF (MD = 7.12; 95% CI, −2.33 to 16.57; p = 0.14; I2 = 82%) (Figure 5).
Figure 4.
Summary of secondary outcome analysis at 3 months (CGI).
Figure 5.
Summary of secondary outcome analysis at 3 months (GAF).
Discussion
The primary aim of this study was to evaluate the efficacy of simvastatin as an adjunctive treatment for patients with schizophrenia. Our findings indicate that simvastatin, when used alongside standard antipsychotic medications, does not yield a significant improvement in the clinical outcomes for schizophrenia patients. These results are somewhat surprising given prior research that suggested possible anti-inflammatory and neuroprotective effects of statins, which could potentially benefit individuals with schizophrenia.
Approximately 10% to 45% of schizophrenia patients are considered treatment-resistant, and these individuals often require other antipsychotic medications or brain stimulation interventions.19–21 Nowadays, a myriad of drugs used for the targeted treatment of schizophrenia, addressing positive symptoms, negative symptoms, cognitive impairments, and other related symptoms. These include antidepressants,22–24 anticonvulsants,25–27 antihistamines,28,29 anti-inflammatory drugs,30,31 benzodiazepines,32–34 β-blockers,35,36 cholinesterase inhibitors,37,38 as well as various hormonal drugs.39,40 Strategies for the enhanced use of these medications have also emerged accordingly.41
Statins are a type of lipid-lowering medication used to treat high cholesterol, and numerous RCT studies in recent years have explored the effects of statin intensification treatment.42–44 There have been two meta-analyses regarding the use of statins as an augmentation strategy for antipsychotic treatment in schizophrenia.8,10 The two articles used similar data but arrived at different conclusions due to different analytical methods. Dr. Andrade conducted a more in-depth analysis and study of the data presented in these two meta-analyses.45 One meta-analysis concluded that statins significantly improved both positive and negative symptoms compared to placebo, showing clear improvements in total scores and general psychopathology subscale scores, while no significant differences were observed in the subscale results. Conversely, the other meta-analysis found that statins surpassed placebo in the subgroup results for positive and negative symptoms but did not show an advantage in total scores and general psychopathology subscale scores. However, the two meta-analyses suffer from the following flaws: discrepancies in disease grading across different studies, the relation of score changes within the same study and the association with key scores, and the use of erroneous data. Moreover, there are currently few RCT (Randomized Controlled Trials) studies related to intensified treatment regimens with statin drugs, and the data all show very small, even negligible, statistical differences between the experimental drug and the placebo.
Despite the exact mechanism remains unclear how statins improving psychiatric symptoms, the most common explanations are their anti-inflammatory role in the brain. Immune dysfunction and inflammation have been described not only in classical autoimmune brain diseases such as multiple sclerosis46 and autoimmune encephalitis47 but also in psychiatric disorders such as schizophrenia.48 Moreover, there is evidence of a clear link between autoimmune conditions and schizophrenia.49,50 Statins, HMG-CoA reductase inhibitors, have potent anti-inflammatory properties different than those of NSAIDs. One hypothesis is that inflammatory responses may play a certain role in the pathology of schizophrenia, and statins, being able to cross the blood-brain barrier, can reach the site of lesion and exert an anti-inflammatory effect.51 The most evident reason for the negative results in this study may lie in the fact that reducing the inflammatory state in patients with Schizophrenia Spectrum Disorders (SSD) does not itself contribute to the improvement of overall symptoms and cognition.
Some research suggested that simvastatin could significantly decrease the levels of interleukin-1β (IL-1β), tumor necrosis factor alpha (TNF-α) and C-reactive protein (CRP).52 Therefore, simvastatin may have the ability as adjuncts to improve psychiatric symptoms of schizophrenia due to the anti-inflammatory effects. Additionally, while the anti-inflammatory properties of simvastatin are well-documented, the complex pathophysiology of schizophrenia may necessitate a broader or more specialized anti-inflammatory strategy. The neurobiological underpinnings of schizophrenia are multifaceted, involving dopaminergic and glutamatergic neurotransmission, neuroinflammation, and oxidative stress. Thus, therapies targeting a single aspect, such as inflammation with simvastatin, may not suffice to produce a noticeable clinical benefit.
Statins can be classified into lipophilic and hydrophilic types based on their ability to penetrate the blood-brain barrier. Lipophilic statins, such as simvastatin, can more easily cross the blood-brain barrier to reach brain tissue.53 Simvastatin had been hypothesized to enhance cognitive functions and reduce the severity of psychotic symptoms due to its known effects on lipid metabolism and brain cholesterol synthesis.54 In contrast, hydrophilic statins (including pravastatin, rosuvastatin, and fluvastatin) have lower permeability through the barrier, which may prevent them from effectively reaching brain tissue. Therefore, we believe this may largely explain the differences in the efficacy of simvastatin in the treatment of schizophrenia compared to other statins.
In addition, several reasons may account for the lack of observed efficacy in our study. Firstly, the dosage and duration of simvastatin treatment may not have been sufficient to elicit a therapeutic response. It’s also possible that our patient cohort had differentiating characteristics that made them less responsive to the effects of simvastatin, such as the stage of illness, concurrent medical conditions, or genetic factors influencing drug metabolism. The study’s design could also have influenced the results. Though we used randomized, placebo-controlled trials, certain limitations are inherent in the study, such as sample size, follow-up duration, and a possible placebo effect. Future research with a larger participant pool, a longer study period, and possibly higher doses may yield different outcomes.
It is also important to consider that the overall management of schizophrenia remains a complex endeavor that necessitates a multifaceted treatment approach, including psychosocial interventions and optimized antipsychotic therapy. The findings from this study suggest that simvastatin, while safe and well-tolerated, may not contribute meaningfully to this therapeutic array as an adjunctive measure.
In conclusion, while the results of this study challenge the potential role of simvastatin as an adjunct therapeutic in schizophrenia, they also highlight the need for continued exploration of novel treatment strategies. Future research should aim to understand the diverse biological abnormalities associated with schizophrenia and develop targeted therapies that address these complexities.
Conclusion
This study reveals that there is no sufficient evidence on the benefit of simvastatin use as an adjunctive therapy on improving psychiatric symptoms of schizophrenia.
Acknowledgments
Junyu Chen and Yupei Yuan are co-first authors for this study.
Funding Statement
This work was supported by the Distinguished Young Scholars -Natural Science Foundation of Xinjiang Uygur Autonomous Region under grant (2022D01E78).
Data Sharing Statement
The data extracted for analyses are available by the corresponding author upon reasonable requests.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sameer J, Mandy J, Peter J M. Schizophrenia. Lancet. 2022;399(10323). [Google Scholar]
- 2.Matthew L, GPA H, Christina M. Schizophrenia. N Eng J Med. 2020;382(6):1. [Google Scholar]
- 3.Eva-Maria S, et al. The genetic relationships between brain structure and schizophrenia. Nat Commun. 2023;14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masataka W, et al. Dopaminergic dysfunction and excitatory/inhibitory imbalance in treatment-resistant schizophrenia and novel neuromodulatory treatment. Mol Psychiatry. 2022;27(7):2950–2967. [DOI] [PubMed] [Google Scholar]
- 5.Kirkpatrick B, Galderisi S. Deficit schizophrenia: an update. World Psychiatr. 2008;7(3):143–147. doi: 10.1002/j.2051-5545.2008.tb00181.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.J S, et al. Inflammatory and immune response genes have significantly altered expression in schizophrenia. Mol Psychiatry. 2012;18(10):1056–1057. [DOI] [PubMed] [Google Scholar]
- 7.Willey J, Elkind MJAON. 3-Hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors in the treatment of central nervous system diseases. 2010;67(9):1062–1067. doi: 10.1001/archneurol.2010.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nomura I, et al. Statin add-on therapy in the antipsychotic treatment of schizophrenia: a meta-analysis. Psychiatry Res. 2018;260:41–47. doi: 10.1016/j.psychres.2017.11.033 [DOI] [PubMed] [Google Scholar]
- 9.Mareike A, et al. Inflammatory monocyte gene signature predicts beneficial within group effect of simvastatin in patients with schizophrenia spectrum disorders in a secondary analysis of a randomized controlled trial. Brain Behav Immun Health. 2022;26:10051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen H, Li R, Yan R, et al. Adjunctive therapy with statins in schizophrenia patients: a meta-analysis and implications. Psychiatry Res. 2018;262:84–93. doi: 10.1016/j.psychres.2018.02.018 [DOI] [PubMed] [Google Scholar]
- 11.Iris ES, et al. Simvastatin Augmentation for Patients With Early-Phase Schizophrenia-Spectrum Disorders: a Double-Blind, Randomized Placebo-Controlled Trial. Schizophr Bull. 2021;47(4):1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mark W, et al. A randomized controlled trial of add-on naproxen, simvastatin and their combination for the treatment of schizophrenia or schizoaffective disorder. Eur Neuropsychopharmacol. 2023;73:65–74. [DOI] [PubMed] [Google Scholar]
- 13.Matthew J, P. MD, Joanne ME. Introduction to preferred reporting items for systematic reviews and meta-analyses 2020 and implications for research synthesis methodologists. Res Synth Methods. 2021;13(2):153–163. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(jul21 1):b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. doi: 10.1002/14651858.ED000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Imran BC, et al. Add-on clinical effects of simvastatin and ondansetron in patients with schizophrenia stabilized on antipsychotic treatment: pilot study. Ther Adv Psychopharmacol. 2014;4(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soode T-E, et al. Simvastatin adjunct therapy for negative symptoms of schizophrenia: a randomized double-blind placebo-controlled trial. Int Clin Psychopharmacol. 2016;32(2). [DOI] [PubMed] [Google Scholar]
- 19.Stefan L, et al. The response of subgroups of patients with schizophrenia to different antipsychotic drugs: a systematic review and meta-analysis. Lancet Psychiatry. 2022;9;11:884–893. [DOI] [PubMed] [Google Scholar]
- 20.Georgi P. Comparative Analysis of Lateral Preferences in Patients With Resistant Schizophrenia. Front Psychiatr. 2022;13:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kun Y, et al. A multimodal study of a first episode psychosis cohort: potential markers of antipsychotic treatment resistance. Mol Psychiatry. 2021;27(2):1184–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jari T, et al. Polypharmacy with antipsychotics, antidepressants, or benzodiazepines and mortality in schizophrenia. Arch Gen Psychiatry. 69;5:476–483. [DOI] [PubMed] [Google Scholar]
- 23.REB T, Carol P. Do antidepressants improve negative symptoms in schizophrenia? BMJ. 2011;342:1. [DOI] [PubMed] [Google Scholar]
- 24.Christoph CU, KJ C, John SM. Developments in pediatric psychopharmacology: focus on stimulants, antidepressants, and antipsychotics. J Clin Psychiatry. 2011;72(5):4361. [DOI] [PubMed] [Google Scholar]
- 25.Leslie C. Adjunctive lithium and anticonvulsants for the treatment of schizophrenia: what is the evidence? Expert Rev Neurother. 2008;9(1):55–71. [DOI] [PubMed] [Google Scholar]
- 26.CGR H. The effectiveness of anticonvulsants in psychiatric disorders. Dialogues Clin Neurosci. 2008;10(1):77–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.C R, et al. Anticonvulsants as adjuncts for the neuroleptic treatment of schizophrenic psychoses: a clinical study with beclamide. Acta Psychiatr Scand. 1990;81(2):162–167. [DOI] [PubMed] [Google Scholar]
- 28.Xueru W, et al. Correlation between desynchrony of hippocampal neural activity and hyperlocomotion in the model mice of schizophrenia and therapeutic effects of aripiprazole. CNS Neurosci Ther. 2024;30(5):e14739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Archana M, et al. Augmentation Strategies for Partial or Non-responders to Clozapine in Patients with Schizophrenia: a Bayesian Network Meta-analysis of Randomized Controlled Trials. Clin Psychopharmacol Neurosci. 2024;22(2):232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buchanan R, Werkheiser AE, Michel H, et al. Prebiotic Treatment in People With Schizophrenia. J Clin Psychopharmacol. 2024. doi: 10.1097/JCP.0000000000001899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fond G, Mallet J, Urbach M, et al. Adjunctive agents to antipsychotics in schizophrenia: a systematic umbrella review and recommendations for amino acids, hormonal therapies and anti-inflammatory drugs. BMJ Mental Health. 2023;26(1):e300771. doi: 10.1136/bmjment-2023-300771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gibson R, Walcott G. Benzodiazepines for catatonia in people with schizophrenia and other serious mental illnesses. Cochrane Database Syst Rev. 2008;2008(4):CD006570. [DOI] [PubMed] [Google Scholar]
- 33.Volz A, Khorsand V, Gillies D, et al.Benzodiazepines for schizophrenia.. Cochrane Database Syst Rev. 2007;(1):CD006391. doi: 10.1002/14651858.CD006391 [DOI] [PubMed] [Google Scholar]
- 34.Stimmel G. Benzodiazepines in schizophrenia. Pharmacotherapy. 1996;16(6P2):148S–151S. doi: 10.1002/j.1875-9114.1996.tb03669.x [DOI] [PubMed] [Google Scholar]
- 35.Wahlbeck K, Cheine MV, Gilbody S, et al. Efficacy of beta-blocker supplementation for schizophrenia: a systematic review of randomized trials. Schizophr Res. 2000;41(2):341–347. doi: 10.1016/S0920-9964(99)00069-9 [DOI] [PubMed] [Google Scholar]
- 36.Sorgi P, Ratey J, Polakoff S. Beta-adrenergic blockers for the control of aggressive behaviors in patients with chronic schizophrenia. Am j Psychiatry. 1986;143(6):775–776. [DOI] [PubMed] [Google Scholar]
- 37.Sinkeviciute I, Begemann M, Prikken M, et al. Efficacy of different types of cognitive enhancers for patients with schizophrenia: a meta-analysis. NPJ Schizoph. 2018;4(1):22. doi: 10.1038/s41537-018-0064-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deutsch S, Schwartz BL, Schooler NR, et al. Targeting alpha-7 nicotinic neurotransmission in schizophrenia: a novel agonist strategy. Schizophr Res. 2013;148:138–144. doi: 10.1016/j.schres.2013.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu J, Song R, Pan R, et al. Extreme temperatures, PM and trajectories of impaired thyroid hormone sensitivity: a longitudinal study of patients with schizophrenia. Environ Int. 2024;191:108961. doi: 10.1016/j.envint.2024.108961 [DOI] [PubMed] [Google Scholar]
- 40.Hyun S, Ka M. Bisphenol A (BPA) and neurological disorders: an overview. Int J Biochem Cell Biol. 2024;173:106614. doi: 10.1016/j.biocel.2024.106614 [DOI] [PubMed] [Google Scholar]
- 41.Howes O, et al. New Drug Treatments for Schizophrenia: A Review of Approaches to Target Circuit Dysfunction. Biol Psychiatry. 2024. [DOI] [PubMed] [Google Scholar]
- 42.Greethurst A, et al. The Use of Statins as an Adjunctive Periodontal Disease Treatment. Syst Rev Meta Anal Dent J. 2024;12(6):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kashour T, Halwani R, Arabi YM, et al. Statins as an adjunctive therapy for COVID-19: the biological and clinical plausibility. Immuno Immunotoxicol. 2021;43(1):37–50. doi: 10.1080/08923973.2020.1863984 [DOI] [PubMed] [Google Scholar]
- 44.Ambrósio L, Rovai ES, Sendyk DI, et al. Does the adjunctive use of statins provide additional benefits to nonsurgical periodontal treatment? A systematic review and meta-analysis. J Periodontal Res. 2018;53(1):12–21. doi: 10.1111/jre.12480 [DOI] [PubMed] [Google Scholar]
- 45.Andrade C. The Use of Statins for Antipsychotic Augmentation in Schizophrenia: examination of Meta-Analyses With Flawed Methods and Conclusions. J Clini Psych. 2018;79(5). doi: 10.4088/JCP.18f12562 [DOI] [PubMed] [Google Scholar]
- 46.Wiley C, Johnson R, Reingold S. Neurological consequences of immune dysfunction: lessons from HIV infection and multiple sclerosis. J Neuroimmunol. 1992;40(1):115–119. doi: 10.1016/0165-5728(92)90219-B [DOI] [PubMed] [Google Scholar]
- 47.Fominykh V, Brylev L, Gaskin V, et al. Neuronal damage and neuroinflammation markers in patients with autoimmune encephalitis and multiple sclerosis. Metab Brain Dis. 2019;34(5):1473–1485. doi: 10.1007/s11011-019-00452-x [DOI] [PubMed] [Google Scholar]
- 48.Gangadin S, Enthoven AD, van Beveren NJM, et al. Immune Dysfunction in Schizophrenia Spectrum Disorders. Annual review of clinical psychology. Annual Review of Clinical Psychology. 2024;20(1):229–257. doi: 10.1146/annurev-clinpsy-081122-013201 [DOI] [PubMed] [Google Scholar]
- 49.Soderlund J, Schröder J, Nordin C, et al. Activation of brain interleukin-1β in schizophrenia. Mol Psychiatry. 2009;14(12):1069–1071. doi: 10.1038/mp.2009.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Potvin S, et al. Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry. 2008;63(8):801–808. doi: 10.1016/j.biopsych.2007.09.024 [DOI] [PubMed] [Google Scholar]
- 51.Çakici N, van Beveren NJM, Judge-Hundal G, et al. An update on the efficacy of anti-inflammatory agents for patients with schizophrenia: a meta-analysis. Psychological Medicine. 2019;49(14):2307–2319. doi: 10.1017/S0033291719001995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosendo AB, Lima LO, Dal-Pizzol F, et al. Lipid and C-reactive protein levels, cardiovascular disease risk factors and simvastatin treatment in Brazilian individuals. Inflammation. 2010;33(4):244–250. doi: 10.1007/s10753-009-9178-3 [DOI] [PubMed] [Google Scholar]
- 53.Béziaud T, Ru Chen X, El Shafey N, et al. Simvastatin in traumatic brain injury: effect on brain edema mechanisms. Crit Care Med. 2011;39(10):2300–2307. doi: 10.1097/CCM.0b013e3182227e4a [DOI] [PubMed] [Google Scholar]
- 54.Nomura I, Kishi T, Ikuta T, et al. Statin add-on therapy in the antipsychotic treatment of schizophrenia: a meta-analysis. Psychiatry Res. 2018;260:41–47. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data extracted for analyses are available by the corresponding author upon reasonable requests.