Abstract
Varicose veins are associated with conditions that impair venous return, such as pregnancy, physical inactivity, valve failure and post-thrombotic syndrome. We report the case of a 50-year-old female patient with history of intermittent calf pain, worsening with prolonged standing posture. She had no previous medical history of either lower extremity trauma or infection. Physical examination showed medial pretibial soft tissue swelling. CT and MRI showed images suggestive of anomalous intraosseous venous drainage with associated bone edema and periosteal reaction. Knowledge of this rare entity is fundamental for proper patient management.
Keywords: Pretibial varices, Anomalous intraosseous venous drainage, Bone marrow edema, Periosteal reaction, Musculoskeletal radiology
Introduction
Leg varices have high prevalence, affecting around 10%-40% of the world's population [1,2]. Rarely, leg varices may have an intraosseous location, i.e. anomalous intraosseous venous drainage (AIVD). The cause and clinical relevance of varicose veins with AIVD are not yet completely understood.
The anomalous communication between pretibial varices and intraosseous veins has already been reported [2]. However, to our knowledge this is the first example of AIVD associated with tibial bone marrow edema and periosteal reaction.
Case report
We report the case of a 50-year-old female patient with a history of intermittent calf pain. She had no previous history of lower extremity trauma or infection.
Physical examination revealed medial pretibial soft tissue swelling.
Radiographs and magnetic resonance of the left leg were requested, in the diagnostic workup for varicose veins. Radiograph was performed in another hospital and reported normal (images were unavailable).
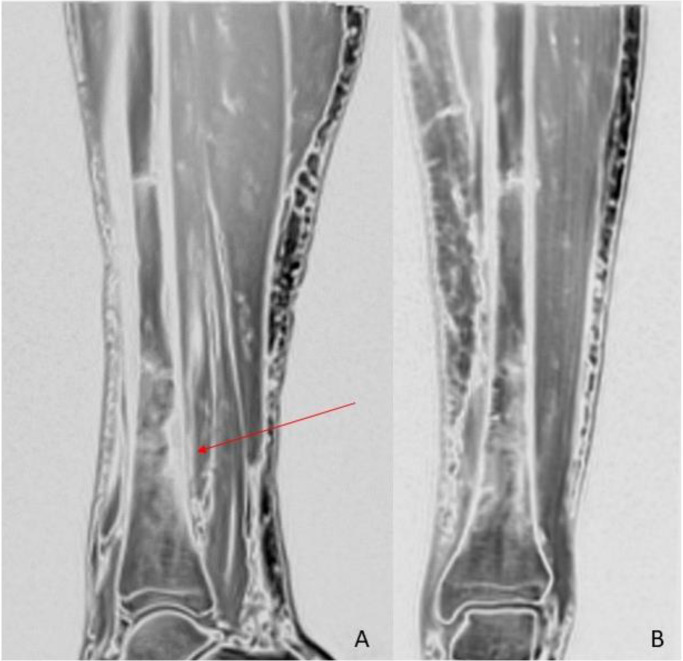
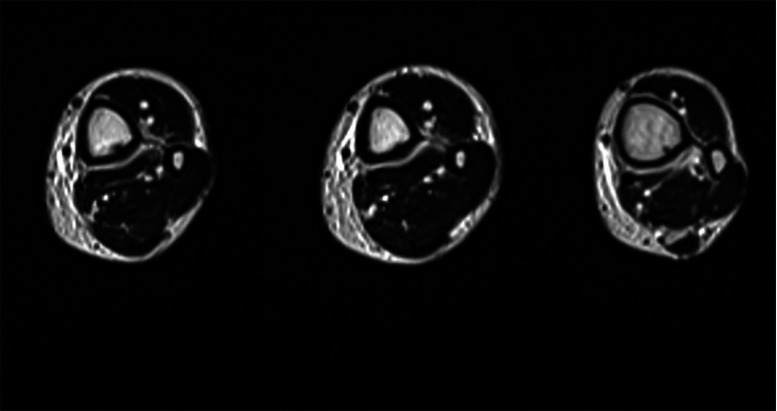
MRI of the left leg (Fig. 1, Fig. 2, Fig. 3) showed bone marrow edema extending from the middle to the distal third of the tibial diaphysis. In the posterior middle-third of the tibial diaphysis, serpiginous subcortical images with oblique course and flow-voids on T1- and T2-weighted were seen. Similar findings were visible at the distal third of the tibial diaphysis. These findings were consistent with dilated vessels connected to anomalous venous structures with an intra-osseous course. At the cortical entry point of the distal third of the tibial diaphysis, periosteal reaction on the posterior side was visible. These intraosseous venous structures were connected to deep venous branches at the middle third of tibia. Small superficial varicose veins were also visible at the medial side of the leg. Subcutaneous edema was present.
Fig. 1.
Magnetic resonance: middle third of the tibial shaft (A) T2-weighted image of the left lower leg demonstrates a periosteal thickening due to lamellar periosteal reaction and bone marrow edema. (B and D) fat-suppressed T2-weighted image showing numerous varicose veins in the adjacent soft tissues. (C) coronal T1-weighted image showing prominent vessel with flow-void at the middle third of the tibial diaphysis (white arrow).
Fig. 2.
Magnetic resonance (A and B) sagittal and coronal high resolution isotropic VIBE images showing periosteal reaction at the distal third of the tibial diaphysis associated with bone marrow edema (red arrow).
Fig. 3.
Magnetic resonance axial T2-weighted images showing a serpiginous structure entering the bone from a cortical entry point at the distal third of the tibial shaft.
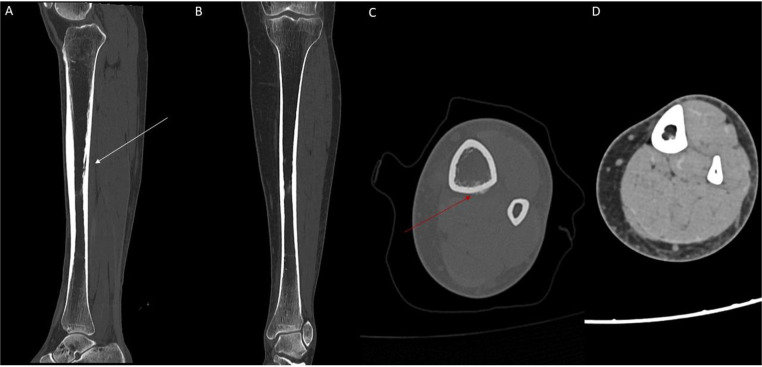
Due to the presence of bone edema, CT was performed to rule out a stress fractures (Fig. 4).
Fig. 4.
(A) sagittal CT showing linear osteolytic image with adjacent sclerosis (white arrow) (B) coronal CT (C) axial CT of the distal one-third of the tibial diaphysis showing periosteal reaction (red arrow). (D) No bone or soft tissue mass lesions were noted.
The patient underwent orthopedic and angiological evaluation, which recommended conservative treatment with physical activity, muscular exercise and weight loss. At follow-up, an improvement in symptoms was observed.
Discussion
The physiopathology of anomalous communication between pretibial varices and intraosseous venous structures is not yet completely understood. In physiologic conditions venous flow in long bones occurs in both centripetal and centrifugal ways, the former being predominant. Boutin et al. [1] postulated that centripetal transcortical venous flow could be increased due to venous insufficiency, venous hypertension, or both. These will shift the flow to mainly centrifugal, possibly being responsible for intraosseous venous anomalies [5]. Conversely, patients with intraosseous venous anomalies are at risk for varices and deep venous thrombosis [1,3].
Patients with AIVD are usually symptomatic and have peripheral venous insufficiency [2].
Management depends on the cause and site of the pathologic venous insufficiency.
The diagnosis can be achieved with imaging. Color-Doppler ultrasound confirms the presence of characteristic varices’ venous flow pattern. Conventional radiography can show tiny subcortical osteolytic lesions immediately beneath the pretibial varices, and an enlarged nutrient canal in the posterior tibial diaphysis. CT and MRI are used to confirm the diagnosis and rule out soft tissue or bone tumors as well as other vascular anomalies (e.g. arteriovenous malformation) [2,7,8]. MRI is the most sensitive and preferred technique to confirm AIVD, as it lacks ionizing radiation, is less invasive, and provides excellent contrast resolution [6]. Venography is an invasive technique that allows a detailed study of the venous system. Treatment can be either surgical or nonsurgical. Phlebectomy, ligation, stripping or percutaneous ablation are the surgical treatment options. Some authors advocate a nonsurgical approach, usually with sclerotherapy [4], as a safe alternative method [1,3].
Regarding bone marrow edema, functional studies have showed it is most likely caused by venous obstruction and intraosseous hypertension, that lead to impaired perfusion and ischemia in several models of bone marrow edema and are related to bone remodeling [9].
Concerning periosteal reaction, some models have suggested that reduced blood flow-induced interstitial fluid flow is unlikely to cause periosteal bone formation in venous stasis. Nevertheless, increased extravascular fluid pressure in response to venous stasis might increase pressure on the periosteum, thus causing new periosteal bone formation [10]. Our case of AIVD associated with bone marrow edema and periosteal reaction suggest a pathogenetic link among these conditions.
Conclusion
Intraosseous venous drainage anomaly is a rare condition in which the diagnosis can be achieved with imaging findings in combination with clinical history. Recognition of this rare entity can prevent misdiagnosis and help to choose the most appropriate treatment.
Patient consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: No funding.
References
- 1.Boutin RD, Sartoris DJ, Rose SC, Plecha EJ, Bundens WP, Haghighi P, et al. Intraosseous venous drainage anomaly in patients with pretibial varices: imaging findings. Radiology. 1997;202(3):751–757. doi: 10.1148/radiology.202.3.9051030. [DOI] [PubMed] [Google Scholar]
- 2.Kwee RM, Kavanagh EC, Adriaensen ME. Intraosseous venous drainage of pretibial varices. Skeletal Radiol. 2013;42(6):843–847. doi: 10.1007/s00256-013-1587-6. [DOI] [PubMed] [Google Scholar]
- 3.Mirault T, Lambert M, Vinckier L, Lamotte C, Cousyn M, Hatron PY. Anomalie de drainage veineux intraosseux, une cause rare de varices prétibiales [Anomalous intraosseous venous drainage: a rare cause of pretibial varicose veins] J Mal Vasc. 2010;35(6):373–376. doi: 10.1016/j.jmv.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Peh WC, Wong JW, Tso WK, Chien EP. Intraosseous venous drainage anomaly of the tibia treated with imaging-guided sclerotherapy. Br J Radiol. 2000;73(865):80–82. doi: 10.1259/bjr.73.865.10721326. [DOI] [PubMed] [Google Scholar]
- 5.Dermesropian F, Scavée V, Haxhe JP, Bodart A, Puttemans T. Bilateral pretibial varices with intraosseous venous drainage anomaly: a case report. J Belg Soc Radiol. 2015;99(2):95–97. doi: 10.5334/jbr-btr.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moraes FB, Camelo CP, Brandão ML, Fávaro PI, Barbosa TA, Barbosa RC. Intraosseous anomalous drainage: a rare case of pretibial varicose vein. Rev Bras Ortop. 2016;51(6):716–719. doi: 10.1016/j.rboe.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flors L, Leiva-Salinas C, Maged IM, Norton PT, Matsumoto AH, Angle JF, et al. MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics. 2011;31(5):1321–1340. doi: 10.1148/rg.315105213. [DOI] [PubMed] [Google Scholar]
- 8.Díaz-Candamio MJ, Lee VS, Golimbu CN, Scholes JV, Rofsky NM. Intrafibular varix: MR diagnosis. J Comput Assist Tomogr. 1999;23(2):328–330. doi: 10.1097/00004728-199903000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Littman J, Gil H, Aaron R. Spontaneous bone marrow edema: perfusion abnormalities and treatment with surgical decompression. Int J Mol Sci. 2023;24(7):6761. doi: 10.3390/ijms24076761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang L, Fritton SP, Weinbaum S, Cowin SC. On bone adaptation due to venous stasis. J Biomech. 2003;36(10):1439–1451. doi: 10.1016/s0021-9290(03)00241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]