Abstract
Hydatid disease is a common parasitic illness. The paravertebral region is rarely involved. After presenting with chronic posterior upper neck swelling, a 28-year-old male patient underwent successful surgical treatment for a primary hydatid disease of the cervical paravertebral compartment after he presented with chronic posterior neck pain. Magnetic resonance imaging was very helpful in identifying a single, well-encapsulated lesion located in the suboccipital paravertebral region. The lesions contained classic daughter cysts that were isointense to the cerebrospinal fluid on all sequences. He had no abdominal or chest hydatid diseases. Primary hydatid disease is extremely rare in this area, and to our knowledge, only 1 previous case similar to ours exists.
Keywords: Cervical hydatid disease, Hydatid disease, MRI, Paravertebral, Suboccipital
Introduction
Hydatid disease (HD) is a zoonotic infection transmitted by Echinococcus granulosus. Humans are accidental hosts [1]. HD affects the liver and lung, the most commonly affected organs [2]. Muscle and soft tissue involvement are rare, and symptoms generally depend on the location, size, and complications of the infection [3]. Paravertebral compartment involvement is rare; only a few case reports are available [4]. Radiology plays a pivotal role in diagnosis [1,2]. Uncomplicated cases have unilocular or multilocular, well-encapsulated cystic regions. The presence of daughter cysts is typical [2]. Complicated cases show a floating membrane. Imaging with ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) can establish the relationship of lesions to neighboring structures, enhancement pattern, and stage of the disease [2,5,6]. Whenever possible, surgical removal along with an anthelmintic is provided because it is associated with the best long-term outcome [3].
Clinical history
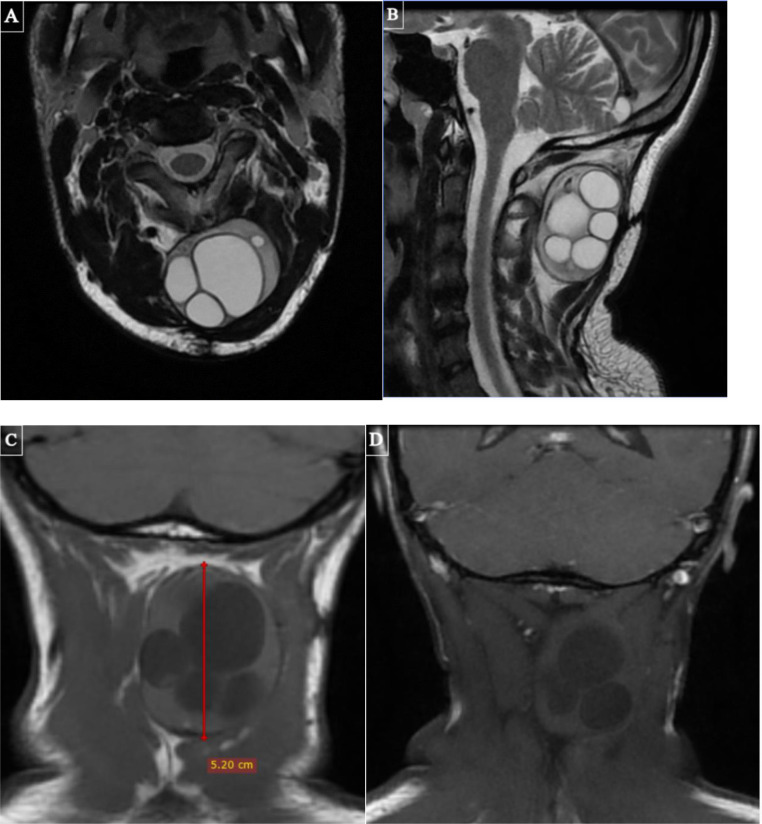
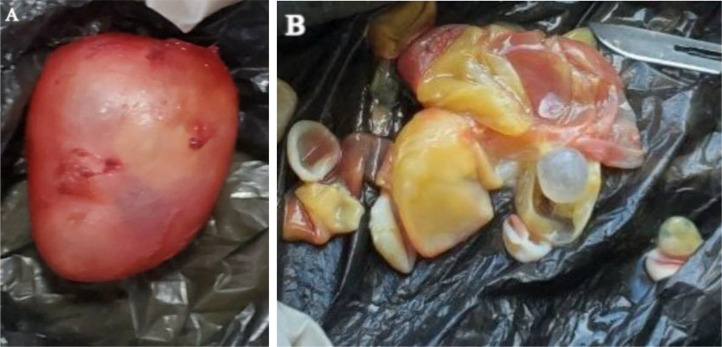
A 28-year-old male patient presented with progressively enlarging left posterior neck swelling and dull pain that lasted for 1 year. He also complained of a restricted neck motion. There was no history of trauma or surgery. On physical examination, the patient appeared well and had normal vital signs. The posterior neck showed a deep, nontender, smooth mass with unremarkable overlying skin. The patients’ sensory and motor functions were intact. The laboratory examination revealed a normal complete blood test and an erythrocyte sedimentation rate. The imaging workup was initiated with a lateral cervical radiograph, which was nonspecific and showed an ill-defined increased opacity of the suboccipital region. A pre- and postcontrast cervical MRI (Fig. 1) followed, revealing a 5.3 × 4.3 × 3.4 cm (CCxTRxAP) solitary round, well-defined lesion in the sub-occipital para-vertebral region posterior to the spinous processes of C1-C3. It has multiple different-sized daughter cysts that exhibit homogeneous T1 dark and T2 bright signal intensities. There was no noticeable enhancement or perilesional fat stranding. There was no neural foraminal extension. The lesion's characteristically multilocuted appearance suggested an imaging diagnosis of a hydatid cyst. An abdominal ultrasound and a chest radiograph were nonrevealing. Subsequently, the patient underwent a surgical excision of the lesion, which confirmed an oval reddish cyst (Fig. 2A), which revealed multiple internal daughter cysts (Fig. 2B). He was discharged from the hospital after an uneventful recovery.
Fig. 1.
T2W axial (A) and sagittal (B), as well as precontrast (C) and postcontrast (D) coronal T1W MR Images, show a round, well-defined lesion with a sharply demarcated, thin, dark capsule in the posterior paravertebral compartment of the neck. It contains multiple homogeneously bright and different-sized daughter cysts. The T1W precontrast and postgadolinium MR images show no enhancement or adjacent perilesional fat stranding.
Fig. 2.
Postoperative photographs show the intact hydatid cyst (A) and its internal daughter cysts (B).
Discussion
Caused by E granulosus, HD is a zoonotic parasitic illness common to endemic regions like Ethiopia [7]. The life cycle of E granulosus is complex. Dogs are the definitive hosts that harbor the adult tapeworm and shed eggs. Humans are accidental intermediate hosts following ingestion of the eggs, like other intermediate hosts (sheep, cattle), but they play no role in transmitting the infection to dogs, which occurs following ingestion of the viscera of intermediate hosts [1,7]. In situ, eggs develop into embryos capable of causing duodenal damage to enter the portal vein. Next, the parasite easily reaches the liver, the most commonly affected organ at 75%, and the lung at 15% [8]. Embryos unusually enter the systemic circulation, infecting organs such as the neck, spleen, heart, muscle, and bone, which collectively account for a minority of HD. About 20%-30% of cases show multi-organ involvement, almost always in conjunction with the liver [6].
Muscle HD is rare, with reported rates of 0.5%-5% [9]. Previous studies have reported muscle involvement in the sartorius, quadriceps, adductors, pectoralis major, rectus, gluteal, and neck muscle groups [3,4]. Active contraction and muscle lactic acid content are believed to be the major reasons that prevent cyst growth, and the neck muscles are more accommodating because of reduced muscle contractions and increased vascular supply [3].
In the paravertebral region, HD is extremely rare, with only a few cases reported [4,5]. HD is also rare in the head and neck region, even in endemic areas [10]. There are 2 forms of musculoskeletal disease: primary and secondary [3,11]. The latter is much more common, followed by liver and lung involvement. The primary form is extremely rare and occurs in isolation [12]. Our case is the primary form, as he has no known HD of the liver, lung, or other body region.
The first report of a suboccipital paravertebral hydatid cyst was by Din et al. from Egypt [4], in which a 50-year-old male presented with chronic posterior neck swelling and pain. To our knowledge, this is the only case in the suboccipital area. One report [5] also showed lumbar paravertebral HD manifesting as lower back pain. In both cases, neurologic complications were absent. Magnetic resonance imaging (MRI) was the main diagnostic modality in both cases.
HD has been classified into 4 major groupings [2]. On MRI, Type 1 and 2 lesions are active and show well-capsulated unilocular or multilocular cysts with CSF intensity. In Type 3, calcification occurs. Rupture or infection can complicate type 4 lesions. Our case is classified as type 2 due to its well-capsulated nature with a T2 dark uninterrupted rim (referred to as the rim sign) and the presence of multiple daughter cysts. Experts classify Type 2 lesions into A, B, and C based on the age and morphology of the daughter cysts. Type 2A cysts exhibit a peripheral arrangement. Type 2B cysts have larger daughter cysts, which fill a much larger volume of the mother cyst and represent our case. Type 2C is a degenerating cyst with areas of calcification. The lack of enhancement makes superinfection less likely.
Imaging plays an important role in preoperative diagnosis and safe surgical planning [2,4,8]. Inadvertent attempts at aspiration might cause cyst rupture, potentially leading to anaphylactic reactions [5]. Imaging choices depend on the location and stages of the disease [2]. An MRI is important for muscle and soft tissue infections because it can better assess for neurologic complications [2,3]. CT is excellent at showing calcifications and bone involvement, and ultrasound can detect hydatid sands and daughter cysts in accessible regions [2,3,11]. Abscesses or neoplasms are other lesions that we considered a differential diagnosis, but given the typical signal intensity and morphology of our patients' case, they are unlikely.
Treatment is dependent on the location, the presence of complications, and the patient's status [3,4]. For paravertebral and neck HD, surgery is the cornerstone of treatment [4]. A total cystectomy has the lowest recurrence rate, and adding a peri-surgical anthelmintic (albendazole or mebendazole) is useful to lower the chances of dissemination at surgery and further reduce postoperative recurrence [[3], [4], [5], [6]].
In conclusion, hydatid disease can involve a wide variety of body regions. Primary paravertebral disease is extremely rare, but it should be considered a plausible differential diagnosis of cystic lesions in the endemic region. Imaging plays an important role in diagnosis and preoperative planning.
Patient consent
Written informed consent was obtained from the patient to publish this case report. Personal identifiers are not used in this paper.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Bereket Girum Beyene, Email: berchgirum@gmail.com.
Michael Teklehaimanot Abera, Email: michael.thaimanot@aau.edu.et, th.miki8441@gmail.com.
Abdela Hayato Gemeda, Email: abdelactvs@gmail.com.
Abdi Alemayehu Dhuguma, Email: abdisabaa430@gmail.com.
References
- 1.Khanfar N. Hydatid disease: a review and update. Curr Anaesth Crit Care. 2004;15(3):173–183. doi: 10.1016/j.cacc.2004.06.002. [DOI] [Google Scholar]
- 2.Srinivas MR, Deepashri B, Lakshmeesha MT. Imaging spectrum of hydatid disease: usual and unusual locations. Pol J Radiol. 2016;81:190–205. doi: 10.12659/PJR.895649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tekin R, Avci A, Tekin RC, Gem M, Cevik R. Hydatid cysts in muscles: clinical manifestations, diagnosis, and management of this atypical presentation. Rev Soc Bras Med Trop. 2015;48(5):594–598. doi: 10.1590/0037-8682-0197-2015. [DOI] [PubMed] [Google Scholar]
- 4.Din DP, Anjum WA, Ahmad ML, Rehman KA, Ahmad GB, Gulshan WN. Primary para-vertebral hydatid cyst in the sub-occipital area of the neck: an unusual case of echinococcosis. Egypt J Neurosurg. 2018;33:1–5. [Google Scholar]
- 5.Sadeghian H, Motiei-Langroudi R. Hydatid cyst in the lumbar paravertebral muscle: a case report. Cureus. 2019;11(8):e5353. doi: 10.7759/cureus.5353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalifa R, Nasser F, Elsetouhy A, Farag I. Hydatid cyst of the neck. A case report and literature review. Egypt J Ear Nose Throat Allied Sci. 2016;17(2):103–105. [Google Scholar]
- 7.Fuller GK, Fuller DC. Hydatid disease in Ethiopia: clinical survey with some immunodiagnostic test results. Am J Trop Med Hyg. 1981;30(3):645–652. doi: 10.4269/ajtmh.1981.30.645. [DOI] [PubMed] [Google Scholar]
- 8.Alshoabi SA, Alkalady AH, Almas KM, Magram AO, Algaberi AK, Alareqi AA, et al. Hydatid disease: a radiological pictorial review of a great neoplasms mimicker. Diagnostics. 2023;13(6):1127. doi: 10.3390/diagnostics13061127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bulut HT, Yildirim A, Celik T, Baykan AH, Sürücü GD, Ekmekçi B. Hydatid cyst of paravertebral muscle mimicking disc herniation. Spine. 2013;38(18):E1175–E1177. doi: 10.1097/BRS.0b013e31829a8357. [DOI] [PubMed] [Google Scholar]
- 10.Katilmiş H, Oztürkcan S, Ozdemir I, AdadanGüvenç I, Ozturan S. Primary hydatid cyst of the neck. Am J Otolaryngol. 2007;28(3):205–207. doi: 10.1016/j.amjoto.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Iuliano L, Gurgo A, Polettini E, Gualdi G, De Marzio P. Musculoskeletal and adipose tissue hydatidosis based on the iatrogenic spreading of cystic fluid during surgery: report of a case. Surg Today. 2000;30(10):947–949. doi: 10.1007/s005950070052. [DOI] [PubMed] [Google Scholar]
- 12.Duncan GJ, Tooke SM. Echinococcus infestation of the biceps brachii. A case report. ClinOrthop. 1990;261:247–250. [PubMed] [Google Scholar]