Abstract
Aneurysms of the common femoral and profunda femoris arteries are rare. Open surgical repair is the treatment of choice, even though hybrid and total endovascular repair with stent graft placement are reported in the literature. We describe a case of a successful total endovascular repair of a common femoral aneurysm extending to the profunda femoris with a bifurcated abdominal endograft placed in the common femoral artery with distal landing in profunda femoris and superficial femoral artery to preserve flow in both arteries. Endovascular repair of common femoral artery aneurysms with bifurcated endografts is a feasible alternative in complex anatomies.
Keywords: Aneurysm, Endovascular procedure, Common femoral artery
True aneurysms of the femoral arteries are rare, with an incidence of 5 per 100,000,1 representing 3% of peripheral aneurysms.2 Historically, repair of femoral aneurysms was advocated at the threshold of 2.5 to 3.0 cm,3,4 even though recent series favor repair at 3.5 cm,5 because of a low incidence of complications at smaller diameters. Although most series describe open surgical repair as the primary treatment,3,5, 6, 7 there are reports of hybrid or total endovascular repair in high-risk patients.5,7, 8, 9, 10 We present the case of a patient with a common femoral artery (CFA) aneurysm with extension to the superficial femoral artery (SFA) and profunda femoris artery (PFA) treated with a bifurcated abdominal endograft with distal landing in both the SFA and PFA through a single ipsilateral SFA approach. The patient consented to this report.
Case report
We present a 64-year-old male patient, former smoker, with a history of hypertension, dyslipidemia, thrombophilia requiring oral anticoagulants, and myocardial infarction. He had history of multiple vascular procedures, including a bilateral aortorenal bypass with occlusion of the left bypass10 years later; an open infrarenal aneurysm repair evolving with proximal neck dilatation after 5 years, requiring a suprarenal endovascular aneurysm repair (EVAR), a right iliorenal bypass and left nephrectomy; left CFA and popliteal aneurysm bypass repair that occluded after several reinterventions and led to an above-the-knee amputation; a type IIIa endoleak endovascular repair; a zone 3 to 4 thoracic EVAR owing to an intramural hematoma; and a single-vessel physician modified FEVAR owing to a 105-mm thoracoabdominal aneurysm.
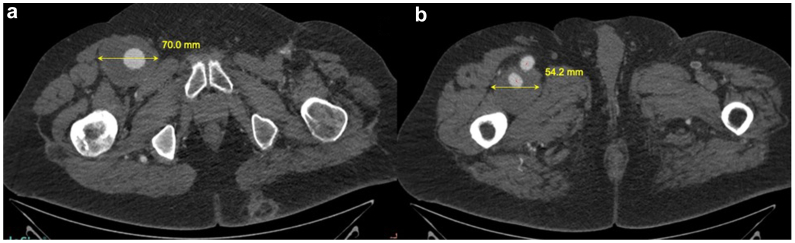
On his computed tomography follow-up 7 years after fenestrated EVAR, he was diagnosed with a 7-cm right CFA aneurysm extending to the SFA and popliteal artery and 15 cm into the PFA with a 54-mm maximum diameter at this level (Fig 1, A and B) and major PFA branches arising from a distal healthy portion. After multidisciplinary discussion, owing to multiple previous procedures and the distal extension of the aneurysm in the thigh, open repair was considered risky and an endovascular approach was planned. To preserve both femoral arteries, a bifurcated stent graft through the SFA with extension to the PFA was deemed necessary. Because contralateral access was precluded owing to left iliac occlusion and upper extremity access could compromise previous fenestrated EVAR, access to the PFA was planned from an ipsilateral approach.
Fig 1.
(A) A 70-mm common femoral artery aneurysm (yellow arrow). (B) A 54-mm profunda femoris artery (PFA) aneurysm.
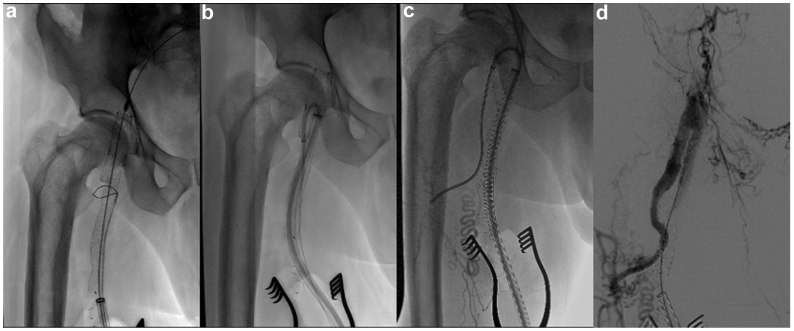
Under general anesthesia, the SFA in the mid-thigh was exposed and punctured, and a 24-Fr Dry-Seal (W. L. Gore & Associates, Flagstaff, AZ) sheath was placed over an extra-stiff wire. Over a buddy wire, a snare was inserted up to the level of the CFA. Angiography was performed, and a 28-14.5-180 mm Excluder C3 (W. L. Gore & Associates) endograft was fully deployed from the distal external iliac artery to the SFA, with the flow divider in the CFA and the contralateral gate oriented to the PFA ostium (Fig 2, A). After withdrawal of the delivery system and balloon molding, a hydrophilic guidewire was advanced from the SFA into the endograft, exteriorized through the flow divider and then snared and retrieved, establishing a through and through wire loop. Through this loop, a 45-cm 12F Dry-Seal Flex (W. L. Gore & Associates) sheath was advanced up and over the flow divider (Fig 2, B) and then PFA was cannulated. Over a 1-cm tip Amplatz super-stiff (Boston Scientific, Heredia, Costa Rica) guidewire, an 8F Flexor (Cook Medical, Bloomington, IN) sheath was advanced to the distal PFA (Fig 2, C). Then, a 7 × 79-mm balloon expandible VBX (W. L. Gore & Associates) stent graft, a 9 × 150-mm self-expandible Viabahn (W. L. Gore & Associates) stent graft, and a 12-mm Excluder IBE internal iliac component (W. L. Gore & Associates) were deployed sequentially from the healthy distal PFA to the contralateral gate of the bifurcated graft. After balloon molding at the stents overlap, angiographic control revealed a type III endoleak at the attachment site of the Viabahn and the internal iliac IBE component, so an 11 × 50-mm Viabahn (W. L. Gore & Associates) was deployed at that level. After balloon molding, sheaths and wires were withdrawn and completion angiogram showed aneurysm exclusion and patency of SFA and PFA with no endoleaks (Fig 2, D).
Fig 2.
Full endograft deployment and snare placement over a buddy wire (A). A 12F sheath up and over the flow divider (B). An 8F sheath at the distal profunda femoris artery (PFA) (C). Completion angiography showing no endoleaks and patency of superficial femoral artery (SFA) and PFA (D).
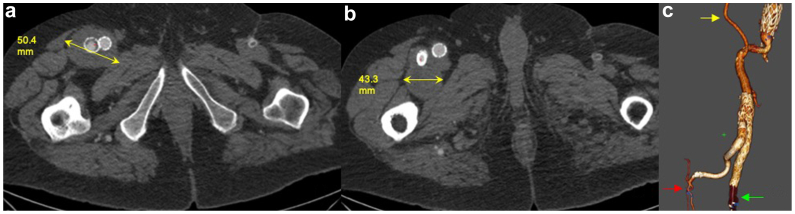
The patient recovered uneventfully and was discharged home the day after the procedure. Two months later, he presented to follow-up with no ischemic symptoms in the thigh and a CTA showing aneurysm exclusion, endograft patency, and a decrease in the CFA diameter (Fig 3, A and B). Further popliteal aneurysm exclusion with a reversed saphenous below the knee femoropopliteal bypass was planned in another stage given the complexity of the primary repair. Connective tissue disorder could not be ruled out; the patient had a visit with a geneticist, but did not undergo genetic testing owing to the additional costs.
Fig 3.
Post operative computed tomography scan showing exclusion of the aneurysm and diameter reduction of the (A) common femoral artery (CFA) and (B) profunda femoris artery (PFA). 3D volume rendering (C) showing patency of right iliac-renal bypass (yellow arrow), superficial femoral artery (SFA) (green arrow) and PFA (red arrow).
Discussion
We present a case of total endovascular repair of a CFA aneurysm preserving flow to the SFA and PFA with a bifurcated endograft through a single SFA approach.
Open, hybrid, and endovascular repairs were considered for this case. Owing to previous surgical history, a fourth open approach was deemed troublesome. In addition, retroperitoneal iliac exposure would be needed to obtain proximal cross clamping for an open or hybrid repair. Furthermore, the aneurysm extended distally 15 cm into the PFA. In this setting, preserving flow to the PFA would have required an extensive dissection deep into the thigh to reach a healthy portion of the artery where an anastomosis could be sawn, and the risk of tissue damage from such an extensive dissection was high. Therefore, a less invasive approach was favored, although it was possible that the patient had a connective tissue disorder.
The option of an inverted flared limb in the CFA was not considered because it would occlude the ostium of the PFA. Because the patient would need a femoropopliteal bypass later, we believed keeping the PFA patent was crucial in the case of future bypass failure, so preservation of both branches with a bifurcated graft was favored.
Based on the technique described by Stern et al11 for the deployment of iliac branched devices through an ipsilateral single access, we planned to deploy a bifurcated endograft at the CFA to preserve flow in the PFA in the same way as flow is preserved in the internal iliac artery during iliac aneurysms repair. In this case, as the proximal landing zone diameter was 23 mm and the distal SFA was 13 mm, a bifurcated graft through a 24F sheath was deployed. Therefore, access through the distal SFA and the upper extremity are preserved in case future device-related reinterventions are needed. Because this endograft does not have a precannulated gate, we had to advance a wire through the flow divider and snare it from the ipsilateral port to establish a stable looped wire access. This looped wire allowed for stable sheath placement up and over the flow divider, so further cannulation and stent deployment into the PFA were accomplished easily.
Importantly, the diameter of femoral arteries allowed the placement of a bifurcated graft; otherwise, this option would have not been feasible.
Conclusions
Total endovascular repair of CFA aneurysms is feasible. A single access approach with bifurcated grafts to preserve flow into SFA and PFA is an alternative to avoid extensive dissection. Longer follow-up is needed to assess graft patency and endoleaks.
Disclosures
M.A.C. is consultant for Boston Scientific and Medtronic and a proctor for W. L. Gore Associates and Medtronic. I.D. is consultant for Medtronic.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Lawrence P.F., Lorenzo-Rivero S., Lyon J.L. The incidence of iliac, femoral and popliteal artery aneurysms in hospitalized patients. J Vasc Surg. 1995;22:409–416. doi: 10.1016/s0741-5214(95)70008-0. [DOI] [PubMed] [Google Scholar]
- 2.Sokhal B.S., Ma Y., Rajagopalan S. Femoral artery aneurysms. Br J Hosp Med. 2022;83:1–10. doi: 10.12968/hmed.2022.0258. [DOI] [PubMed] [Google Scholar]
- 3.Graham L.M., Zelenock G.B., Whitehouse W.M., Jr., et al. Clinical significance of arteriosclerotic femoral artery aneurysms. Arch Surg. 1980;115:502–507. doi: 10.1001/archsurg.1980.01380040124022. [DOI] [PubMed] [Google Scholar]
- 4.Anderson J.L., Halperin J.L., Albert N.M., et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:1425–1443. doi: 10.1161/CIR.0b013e31828b82aa. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence P.F., Harlander-Locke M.P., Oderich G.S., et al. The current management of isolated degenerative femoral artery aneurysms is too aggressive for their natural history. J Vasc Surg. 2014;59:343–349. doi: 10.1016/j.jvs.2013.08.090. [DOI] [PubMed] [Google Scholar]
- 6.Baird R.J., Gurry J.F., Kellam J., Plume S.K. Arteriosclerotic femoral artery aneurysms. Can Med Assoc J. 1977;117:1306–1307. [PMC free article] [PubMed] [Google Scholar]
- 7.Piffaretti G., Mariscalco G., Tozzi M., Rivolta N., Anonni M., Castelli P. Twenty-year experience of femoral artery aneurysms. J Vasc Surg. 2011;53:1230–1236. doi: 10.1016/j.jvs.2010.10.130. [DOI] [PubMed] [Google Scholar]
- 8.Rancic Z., Pecoraro F., Pfammatter T., Mayer D., Veith F.J., Lachat M. Less invasive (common) femoral artery aneurysm repair using endografts and limited dissection. Eur J Vasc Endovasc Surg. 2013;45:481–487. doi: 10.1016/j.ejvs.2013.01.038. [DOI] [PubMed] [Google Scholar]
- 9.Wolthuis A.M., Watkinson A.F., Kinsella D.C., Thompson J.F. Complex iliac and bilateral common femoral artery aneurysms: a novel hybrid procedure. Surgeon. 2006;4:111–113. doi: 10.1016/s1479-666x(06)80041-7. [DOI] [PubMed] [Google Scholar]
- 10.Moriuchi H., Maeda T., Koide M., Kunii Y., Watanabe K. Surgical, endovascular, and hybrid treatment of deep femoral artery aneurysm: three case reports. Clin Case Rep. 2023;11 doi: 10.1002/ccr3.7853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stern J.R., Lyden S.P., Agrusa C.J., Schneider D.B. Ipsilateral iliac branch repair using a looped wire, precannulated gate technique. J Endovasc Ther. 2021;28:373–377. doi: 10.1177/1526602821989335. [DOI] [PubMed] [Google Scholar]