Abstract
Introduction and importance
Retropharyngeal abscess (RPA) represents a rare and life-threatening condition, particularly uncommon in the adult population. The simultaneous occurrence of RPA, and cervical spondylodiscitis is an exceedingly infrequent situation.
Case presentation
we reported the case of a 67-year-old male who presented to our department with complaints of sore throat, restricted neck range of motion, as well as numbness and weakness in the right arm persisting for two weeks. Cervical computed tomography identified a retropharyngeal abscess measuring 15 cm in height around C3 to D3. Subsequent cervical magnetic resonance imaging disclosed revealed infectious spondylodiscitis at C5-C6-C7 and partially collected epiduritis from C5 to C7. The abscess was promptly drained by the transoral way. Following the procedures, the patient was discharged with a cervical collar and a prescribed course of antibiotics.
Clinical discussion
Cervical retropharyngeal abscesses complicating spondylodiscitis is very rare. The clinical symptoms are variable and nonspecific. Given the potentially life-threatening nature of this condition, its management represents a real challenge.
Conclusion
The management of such complex cases necessitates a multidisciplinary approach involving otolaryngologists, neurosurgeons, and infectious disease specialists to mitigate the risk of complications and prevent any potential delays in treatment.
Keywords: Retropharyngeal abscess, Cervical pyogenic spondylodiscitis, Epiduritis, Surgery, MRI, Antibiotics
Highlights
-
•
Retropharyngeal abscesses (RPA) complicating spondylodiscitis is a rare potentially life-threatening in adults.
-
•
The recognition of RPA alongside CS presented a challenge, primarily stemming from the rarity of this syndrome.
-
•
MRI and CT scan are essential and complementary to establish the diagnosis.
-
•
The treatment approach is medico-surgical.
-
•
Therapeutic strategy must be developed as soon as such a lead is suspected.
1. Introduction
Bounded laterally by carotid sheaths, anteriorly by buccopharyngeal fascia, and posteriorly by prevertebral fascia, the retropharyngeal space stretches from the base of the skull down to the mediastinum [[1], [2], [3], [4]]. Retropharyngeal abscesses (RPA) represents 12 % of all deep neck abscesses [5]. It is a potentially life-threatening condition that affects adults quite rarely. RPA require prompt diagnosis and early management which frequently involves surgical drainage to achieve the best results. However, the appropriate timing to undergo a surgical procedure is still controversial [1].
We present an unusual case of retropharyngeal abscess revealing infectious cervical spondylodiscitis with cervical spinal epiduritis in a diabetic adult. The work has been reported in line with the SCARE criteria 2023 [6].
2. Case presentation
This concerns a 67-year-old male patient, who presented to the emergency department with a presentation of dyspnea and altered general condition. This patient is a known non-insulin-requiring diabetic on oral antidiabetic medication and hypertensive on antihypertensive drugs. His illness history dates back two weeks, marked by the onset of persistent cervicobrachialgia resistant to non-steroidal anti-inflammatory drugs for the past two weeks. The progression was characterized by the gradual development of odynophagia, dysphagia, and high dyspnea with unspecified fever. The examination noted: a clear level of consciousness, fever of 39.5 °C, with an overall unsatisfactory condition. Blood pressure was 140/80. Oxygen saturation (SAO2) in ambient air was 91 % (rising to 99 % with nasal cannula). The examination revealed pharyngeal voice, salivary stasis, and pharyngeal hyperemia with bulging of the posterior pharyngeal wall. Following the clinical examination, suspicion of a deep facial space collection arose.
An emergency CT scan revealed extensive retropharyngeal collections extending vertically from C3 to D3 in the upper and posterior mediastinum over 15 cm in height. The largest collection (around C3 and C4) measured 55 mm in the long axis, compressing the pharyngeal lumen. No vertebral bone lesions were observed (Fig. 1A.B). No foreign bodies or signs of trauma or pneumonia were identified. Laboratory tests showed elevated CRP at 452.65 mg/l, leukocytosis (26,440/μl) with neutrophilia, and hyperglycemia at 30 mmol/l. A diagnosis of retropharyngeal abscess was made.
Fig. 1.
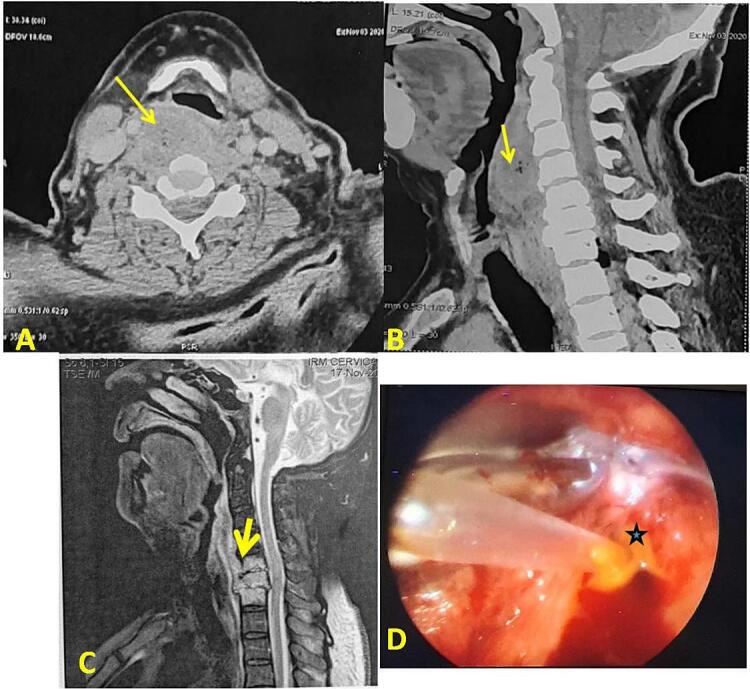
A, B: CT in axial and sagittal sections: retropharyngeal collection extending vertically from C3 to D3 in the upper and posterior mediastinum over 15 cm in height. The largest collection (around C3 and C4) measured 55 mm in the long axis, compressing the pharyngeal lumen. C. MRI in sagittal section: Extensive prevertebral collections in with approximately 25 % spinal cord compression and partially collected epiduritis from C5 to C7. D: intraoperative photo showing the release of pus during the intraoral drainage puncture.
Endoscopic exploration under general anesthesia revealed inflammatory and congestive bulging of the oropharyngeal and hypopharyngeal posterior walls. A puncture-aspiration via endobuccal route was performed, followed by surgical drainage of the retropharyngeal collection (Fig. 1D). The pus sample was sent for bacteriological examination. The patient received intravenous Cefotaxime and Metronidazole, along with analgesics and mouthwash. A protocol for correcting the ketoacidosis decompensation of his diabetes was initiated. The bacteriological analysis confirmed the presence of Gram-positive cocci on direct examination and Staphylococcus aureus in culture. The same antibiotic therapy was continued. Additionally, the patient, during acute management, reported cervical pain with right-hand paresthesia and non-systematized right cervicobrachial neuralgia. He also mentioned muscle weakness and numbness. Upon examination, right upper limb weakness was noted, while the rest of the neurological and musculoskeletal examination was unremarkable. Infectious spondylodiscitis was suspected in this scenario. A cervical MRI, conducted as part of the etiological investigation, revealed infectious spondylodiscitis at C5-C6-C7 with extensive prevertebral collections in the mediastinum with approximately 25 % spinal cord compression and partially collected epiduritis from C5 to C7 (Fig. 1C).
Following multidisciplinary consultation with neurosurgeons and infectious disease specialists, there was no indication for neurosurgical treatment. The patient continued medical treatment with cervical immobilization. The patient showed gradual improvement in clinical and laboratory signs, achieving apyrexia within 48 h. After 21 days of intravenous treatment, normalization of CRP and leukocytosis was noted. The patient was then switched to oral Ofloxacin and Rifampicin for three months. He was discharged with a follow-up radiological examination through spinal MRI in three months.
3. Discussion
Cervical retropharyngeal abscesses affects 4.10 per 100,000 children per year [3]. Only few cases of retropharyngeal abscess complicating infectious non tuberculous cervical spondylodiscitis in adults have been reported [3]. The majority of patients, including the current case, were male [1,3,7].
Cervical spondylodiscitis (CS), a seldom encountered and severe condition, leads to enduring neurological impairments. The development of complications such as cervical spine epidural abscess and retropharyngeal abscess is certainly explained in CS by the close proximity of these anatomical structures. Although less prevalent in the cervical region compared to the thoracic or lumbar regions, the associated mortality and morbidity rates are higher [4,8].
The clinical symptoms are variable and nonspecific. The signs of infection may be lacking in certain situations of immune suppression such as diabetes [1]. The principal symptoms in adults are sore throat, fever, dysphagia, odynophagia, neck pain and dyspnea. Patients with RPA may present signs of airway obstruction. The most common physical presentation is posterior pharyngeal edema (37 %), nuchal rigidity, cervical adenopathy, drooling, and stridor; and also the emergence of new neurological deficits, particularly in conjunction with CS or cervical spine epiduritis (CSE) as observed in the presented case [1,3].
A neurological deficit is found in 68 to 80 % of cases in CS and it may develop insidiously [9]. The microbial composition of deep neck abscesses is characterized by a polymicrobial nature, wherein both anaerobic and aerobic organisms play predominant roles. In a retrospective analysis of 183 cases conducted by Almutairi et al., Streptococcus pyogenes emerged as the most prevalent pathogen, accounting for 39.3 %, followed by Staphylococcus aureus at 21.3 % [10]. Conversely, other authors identified Staphylococcus aureus as the primary non-tuberculosis pathogen associated with pyogenic spondylodiscitis in 15–84 % of cases [8,11]. Cervical CT stands out as the most valuable radiological modality for diagnosing RPA. However, it is imperative to complement this with MRI to ensure a definitive diagnosis of RPA, CS, and CSEA. This combined approach is crucial for promptly revealing spinal cord compression, mitigating the risk of severe complications such as mediastinitis, sepsis and persistent neurological deficits [3,4,12].
Depending on the patient's clinical presentation, both surgical and non-surgical approaches may be considered as viable options for managing of CS.
Surgical intervention for RPA involving abscess drainage may be considered, particularly in cases with compromised airways or when the abscess size exceeds 30 mm. The transoral route predominates among the majority of medical teams in addressing this condition [[13], [14], [15]]. Tracheotomy could also be contemplated in the presence of uncontrolled acute dyspnea not responsive to transoral abscess drainage [13].
Regarding medical treatment, it is advisable to initiate broad-spectrum empirical antibiotic therapy while awaiting culture isolation [14]. Additionally, the necessity of incorporating long-term antibiotic usage aligned with culture results is not to be debated [4]. Antibiotic treatment typically entails a minimum duration of 6 weeks and the choice of antibiotic depends on the specific organism involved [11].
Other measures, such as neck stabilization using a cervical collar, were recommended and close monitoring due to the potential risk of sudden neurological deterioration [16].
Surgical intervention is often recommended for advanced spondylodiscitis cases, particularly when there is evidence of neurological deficits, spinal instability, new or worsening kyphosis, failure of conservative management, the necessity for controlling the infectious source, or the absence of a diagnostic organism. And the primary objectives of surgical intervention are debridement of infected tissue, spinal stabilization, and decompression of neural elements [11].
4. Conclusion
In our case, the expeditious recognition of RPA alongside CS presented a challenge, primarily stemming from the rarity of this infection entity. Given its potentially life-threatening nature, healthcare providers must contemplate a diagnosis of RPA resulting from CS when patients present with concurrent oropharyngeal and neck-related symptoms.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Not applicable (data and figure included does not compromise the identity of the patient).
Funding
None.
Author contribution
Bouatay Rachida: study conception, writing and correcting the paper.
Belhadj Miled Heyfa: writing the paper.
Koubaa Jamel: revising the manuscript.
Guarantor
Rachida Bouatay.
Research registration number
Not applicable
Conflict of interest statement
None.
References
- 1.Harkani A., Hassani R., Ziad T., Aderdour L., Nouri H., Rochdi Y., et al. Retropharyngeal abscess in adults: five case reports and review of the literature. Scientific World Journal. 2011;11:1623–1629. doi: 10.1100/2011/915163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sideris G., Nikolopoulos T., Papadimitriou N. Spontaneous, non-traumatic retropharyngeal abscess complicated by spinal osteomyelitis and epidural abscess in immunocompetent adult: management and proposal pathophysiological mechanism. Cureus. 2020;12(7) doi: 10.7759/cureus.9028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epstein N. Diagnosis, and treatment of cervical epidural abscess and/or cervical vertebral osteomyelitis with or without retropharyngeal abscess; a review. Surg. Neurol. Int. 2020;11:160. doi: 10.25259/SNI_294_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.İsayev N., Yücel L., Akyıldız H.S., Mammadkhanlı O., Başak H., Doğan İ. A rare case as different cause of retropharyngeal and spinal epidural abscess: spondylodiscitis. Egypt J. Otolaryngol. 2021;37(1):117. [Google Scholar]
- 5.Tollard E., Choussy O., Bertrand M., Thiébot J., Dacher J.N., Marie J.P. Prevertebral abscess mimicking a retropharyngeal abscess and revealing a double-location spondylodiscitis: case report. J. Neuroradiol. 2007;34(2):141–143. doi: 10.1016/j.neurad.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faidas A., James V., Jr Ferguson, Nelson J.E., Baddour L.M. Cervical vertebral osteomyelitis presenting as a retropharyngeal abscess. Clin. Infect. Dis. 1994;18(6):992–994. doi: 10.1093/clinids/18.6.992. [DOI] [PubMed] [Google Scholar]
- 8.Almansour H., Pepke W., Akbar M. Pyogenic spondylodiscitis: the quest towards a clinical-radiological classification. Orthopäde. 2020;49(6):482–493. doi: 10.1007/s00132-019-03836-0. [DOI] [PubMed] [Google Scholar]
- 9.Sakaguchi A., Ishimaru N., Ohnishi H., Kawamoto M., Takagi A., Yoshimura S., et al. Retropharyngeal abscess with cervical discitis and vertebral osteomyelitis caused by Escherichia coli in a patient with liver cirrhosis. Infez. Med. 2017;25:169–173. [PubMed] [Google Scholar]
- 10.Almutairi D., Alqahtani R., Alshareef N., Alghamdi Y.S., Al-Hakami H.A., Algarni M. Deep neck space infections: a retrospective study of 183 cases at a tertiary hospital. Cureus. 2020;12(2):6841. doi: 10.7759/cureus.6841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Treffy R.W., Laing B., Eraky A.M., Shabani S. Cervical spine spondylodiscitis: review of literature on current treatment strategies. Heliyon. 2023;9(7) doi: 10.1016/j.heliyon.2023.e17875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoang J.K., Branstetter B.F., Eastwood J.D., Glastonbury C.M. Multiplanar CT and MRI of collections in the retropharyngeal space: is it an abscess? AJR Am. J. Roentgenol. 2011;196(4):426–432. doi: 10.2214/AJR.10.5116. [DOI] [PubMed] [Google Scholar]
- 13.Keïta A., Diallo I., Fofana M., Diallo M.A., Ramata Diallo M.M., Balde O., et al. Abcès rétropharyngé et la revue de la littérature: à propos de 5 observations. Pan Afr. Med. J. 2020:36. doi: 10.11604/pamj.2020.36.360.24282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martins J., Lucas A. Deep neck infection: a case of retropharyngeal abscess. Cureus. 2023:15. doi: 10.7759/cureus.48293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brook I. Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. J. Oral Maxillofac. Surg. 2004;62(12):1545–1550. doi: 10.1016/j.joms.2003.12.043. [DOI] [PubMed] [Google Scholar]
- 16.Cunha L., Almeida M., Cordeiro I., Baptista A. Spontaneous cervical spondylodiscitis with retropharyngeal abscess and bacteremia: a case report. Cureus. 2023;15(6) doi: 10.7759/cureus.40246. [DOI] [PMC free article] [PubMed] [Google Scholar]


