Abstract
As the population ages and grows, health services must evolve in ways to offer versatile patient care, whilst improving patient outcomes and maintaining long-term economic viability. A facility assisting in the provision of such healthcare is the hybrid operating room (HOR): a specialised suite allowing simultaneous radiological and surgical diagnostics and therapeutics in a single episode of care. Versatile and customizable, the HOR is utilised by a broad range of subspecialties in elective and emergency settings, including (but not limited to) vascular surgery, trauma surgery and interventional radiology. Though the benefits of hybrid techniques to patient care are well known, the actual steps in operationalising the HOR can be challenging if not considered and coordinated appropriately. The intention of this narrative review is to highlight issues and suggest solutions in the design and commissioning of an HOR. Key areas in need of specific attention include stakeholder involvement, economic feasibility, suite location, workflow planning, hybrid equipment choice, and team organisation.
Keywords: Hybrid theatre, Vascular surgery, Endovascular surgery, Open surgery, Interventional radiology, HOR design
Introduction
The Hybrid Operating Room (HOR) is a cutting-edge surgical facility at the forefront of modern-day surgery and contemporary healthcare provision. It combines the traditional open theatre surgical environment, with the added multifunctional capabilities of state-of-the-art medical imaging equipment, enabling synchronous diagnostic and therapeutic care in a single location and care episode. The configuration of an HOR is far from uniform and the room layout and design is highly customisable, tailored to suit the specific needs of its intended health service.
Clinicians and hospital administration alike are increasingly recognising the applications and potential benefits of an HOR. Within vascular surgery, the rapid evolution of open and endovascular surgical techniques is a driving factor, however interventional radiology, trauma surgery, neurosurgery, cardiothoracic surgery, orthopaedic surgery and obstetrics are also seeing improvements in their own patient outcomes with the use of a hybrid operating suite, leading to an increasing demand for operating rooms with image-guidance capabilities.1,2 With an ageing population, and ever-increasing complexity in endovascular interventions, such an endovascular aortic aneurysm repair, complex arch-branched repair, cardiac valve repair, and hybrid cardiac intervention, a hybrid operating room is readily becoming a staple in modern hospitals. 3 By amalgamating diagnostic and therapeutic interventions in a single episode of care, and combining minimally invasive and traditional open surgery, an HOR omits the need for multiple medical imaging and theatre visits, thus increasing the overall efficiency in the public healthcare system. Evidence supports a reduction in perioperative risk and simultaneous improvement of patient health and safety outcomes.4,5 The potential benefits of implementing an HOR are summarised in Table 1.1,2,6
Table 1.
| Potential benefits of a hybrid operating room | |
|---|---|
| Facilitation of minimally invasive procedures | Decreased interdisciplinary transfer |
| Improved patient outcomes | Decreased intravenous or intra-arterial contrast burden |
| Decreased incidence of intensive care visits and/or reduced length of intensive care stay | Greater prospective return-on-investment/reimbursement and lower total peri-procedural and procedural cost per patient |
| Decreased total hospital length of stay | Improved use of resources and waste minimisation |
| Decreased total number of operating theatre visits for patients that would otherwise need staged surgeries or a separate diagnostic and therapeutic procedures | Acquisition and training of staff with new or improved skill sets |
While an HOR offers clear benefits to patients and organisations alike, its implementation in a hospital setting presents many challenges. This is an inevitable pitfall of its highly customisable design, resulting in a lack of standard configuration, procedure types, or protocols. The present narrative review was conducted to highlight common difficulties in interdisciplinary and financial planning, layout and design considerations, and the utilization of an HOR, with the intention of providing viable solutions that may be implemented by a well-coordinated team.
Stakeholder vision
Members of the stakeholder group need an overarching view of what it is that the organisation wishes to achieve by the construction and implementation of an HOR in their health service. This should include its subspecialty use and scope of work, and a strategic plan to service the current population health gaps. Consideration for future ambitions regarding patient care and hospital recruitment strategy should also be included in this vision.
The purpose of an HOR is to provide patients with the best form of intervention in a timely fashion, be it open surgical, minimally invasive, or a hybrid combination of the two. It should simultaneously centralise care and broaden the scope of practice, resulting in improved patient outcomes and healthcare economics. To meet the demands of this new interdisciplinary environment, a clear understanding of HOR work dynamics and its integration into subspecialty practice needs to be conceptualised. Therefore, the key stakeholder working group should include surgeons, interventionalists, anaesthesiologists, radiographers, nursing staff and theatre technicians. This will need to be coupled with the financial guidance of funders (including intra- and interhospital sponsorship and leverage) and senior executives (Table 2). Of note, the suggested stakeholder list is not exhaustive, and would be highly dependent on the organisation structure, available services, and scope of the intended HOR service provision. 6 It is important that the focus remains patient-centred, where the HOR addresses the needs of healthcare providers in a single space with the intention of minimising transfer of care episodes between different clinical specialities.
Table 2.
Example of recommended potential stakeholder members in building the ideal hybrid operating room planning team.
| Recommended stakeholder members | |
|---|---|
| Chief Operating Officer/Organisation executive | Director of Interventional Radiology |
| Chief Financial Officer or delegate | Director of Trauma/Trauma Surgery |
| Director of Vascular Surgery | Director of Neurosurgery |
| Director of Anaesthetics | Director of Perioperative Services (or equivalent) |
| Director of Nursing | Director of Medical Imaging |
| Director of Cardiothoracic Surgery | Other network hospitals within district health service |
The application of an HOR should be anticipated to pose a significant budgetary challenge with reference to the scope of work. As such, the potential re-allocation of funding from within the district health service and sources of external funding from government or private funding bodies needs to be considered. In order to justify such an investment, there needs to be stakeholder group alignment regarding the primary intended use of the HOR (e.g. vascular surgery). However, the integrated use of other surgical subspecialties should be heavily considered as this adds to the estimate of anticipated interventions and potential caseload volume, all of which will drive the necessary ‘case for change’ to the hospital executives. The overall purpose of the HOR is to elevate the quality of, and access to, care for patients, and in return provide economic benefits to the healthcare organisation.
Feasibility assessment – costs and financial considerations
The implementation of a hybrid theatre in a healthcare organisation is a substantial and expensive endeavour, where the underlying demand and alignment with the hospital’s vision influences budget. This considerable financial investment should be presented to hospital administration with a clear feasibility model, accounting for initial designing, construction, and equipment expenses as well as ongoing operational and maintenance/service costs. Consequently, the business plan will need to detail the initial capital outlet for construction and ongoing operating expenses against the back-end savings reflected by the reduction in intensive care unit (ICU) dependence, reoperation, readmission, episodes of care, lengths of stay and theatre visits (a rough estimate of 1–2 financial years later). The economic feasibility assessment should also consider:
Acquisition and installation of the imaging system
Acquisition and installation of the theatre table or tables
Acquisition and installation of ancillary equipment (detailed later)
Service costs of the imaging system, tables and ancillary equipment
Cost of disposable stock (including drapes, wires, catheters, sheaths, balloons, stents, contrast)
Cost of training or acquiring suitable staff
Reimbursements from various procedures, including hybrid procedures
Details of cost monitoring plan and/or prosthetics governance group
Retrofitting an HOR into a pre-existing theatre space or catheterisation laboratory is feasible and may be more cost-effective (although there are some complexities to this). While a good idea at first glance, substantial architectural changes often need to be made to accommodate the appropriate equipment. For example, some floor-mounted imaging systems will need to be built in to a ‘cut-out’ in the floor, while others will need to be built on load-bearing pylons (many require both of these). Equally, booms, multijointed arms, movable monitors and ceiling-mounted imaging systems will require easy access to mains electricity, load-bearing rails and clever ceiling reinforcement that works around the theatre ventilation and lighting. The cost of these key structural components should not be understated. These can obviously be planned for if the build is entirely new, and it is obvious that a new build would be infinitely more flexible than working with an existing space, for the above reasons.
Specific costs of the room-build, equipment, procedures, staffing, training, maintenance, and future-proofing are out of the scope of the present review, however, they cannot be overlooked in the initial budgeting. Nonetheless, the single most important factor in HOR financial allocation is the fluoroscopy unit - where quality cannot be compromised if hoping to achieve a sustainable return on investment. Nuances of imaging systems are discussed later, but it should be noted that the expenditure for a fixed imaging system is significantly more than a mobile image intensifier. Pertaining specifically to vascular surgery, fixed imaging is the optimal choice, with greater cost-benefits realised by pairing an HOR with a predominantly endovascular caseload. If limited by the volume and scope of vascular surgical procedures offered at the institution, interdisciplinary use of the HOR by other specialties is ideal, hence the importance of continual involvement of subspecialties within the stakeholder group. This is particularly important in the presence of a rapidly aging population, and the need for treatment of the previously untreatable - for example the generation of patients receiving transcatheter aortic valve implantation procedures. Similarly, with increasing use of minimally invasive techniques, ICU admissions and/or length of stay should theoretically decrease, along with total hospital length of stay, providing an additional means of long-term saving.
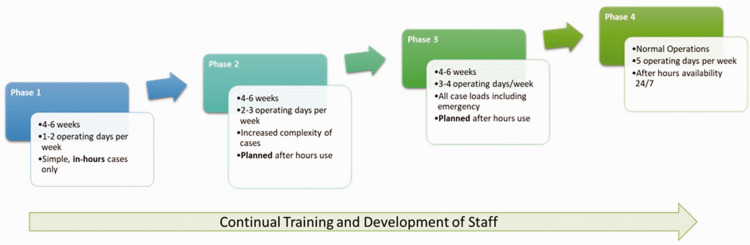
Also critical to long-term return on investment is optimising theatre utilisation. As alluded to previously, a newly established hybrid operating facility may be expected to initially run less economically per unit of time, until staff become more familiar with its navigation. Development of specific protocols and work instructions tailored to the procedure, and the individuals or teams involved in its use, is an important consideration to ensure its future efficient and economical utility. An example includes layout protocols for procedure-specific perioperative equipment set-up, with block-scheduling of procedures that would require similar orientation and equipment requirements. Furthermore, a clearly defined roll-out process that outlines gradual increases in functional operating capacities over a planned period should complement the aforementioned optimisation in workflow and logistics. This may be achieved through a ‘project implementation plan’, as depicted in Figure 1. The overarching objective should be such that the new HOR will service the relevant patient demographics of the involved surgical subspecialties, permitting more complex and greater volumes of procedures. As a result, greater reimbursements accompanied by reduced public healthcare costs, through decreased needs of staged procedures, will be realised.
Figure 1.
Example of a proposed hybrid operating room project implementation plan.
Irrespective of the construction plan, it is the responsibility of the stakeholders to ensure that by prioritising cost-effective equipment, the overall scope of procedures is not limited and still considers future population growth. Reduced spending should not impact the ability to provide high quality surgical treatment through the HOR.
Location
The current design of the hospital, building codes and government regulations may offer logistical challenges to HOR development. Co-locating the suite within the theatre complex nearby other relevant facilities may prove cost-effective, particularly in terms of operational efficiency, and better governance over the use of HOR prosthetics. Placing the HOR on the same floor as traditional surgical theatres or interventional radiology suites is advantageous, as doing so facilitates co-location with the perioperative unit, post-operative recovery bays and relevant surgical wards. This would also allow access to pre-existing surgical supplies (reducing unnecessary duplication and translocation), sterilisation facilities, surgeons, anaesthetists, and other hybrid-trained staff in the event of an emergency. Ideally, the HOR should be strategically located to allow for timely patient transfer to and from theatre in emergency situations, proximity to neighbouring operating subspecialities and services that may be required in cases where intraoperative complications arise. Other important practical considerations include strategic access to the HOR from the emergency department or helipad, and the resulting disposition to the ICU or relevant surgical wards. This will be strongly influenced by the members of the stakeholder group, and location may differ depending on the intended surgical service. For example, a high-volume dedicated trauma service may advocate integrating the HOR near emergency department resuscitation bays, the helipad, or ICUs.
Layout and workflow planning
The collective knowledge and experience of the previously mentioned stakeholder group is imperative in the successful design layout and workflow of an HOR. There are many key pieces of equipment needed in the HOR design and future-proofing, with major fixtures including operating tables (surgical versus angiography), fixed imaging systems, a control room, an engineering/plant room, sterile airflow systems, oxygen and suction lines, cardiovascular and neurovascular monitoring systems, embedded circuitry, and ceiling-mounted equipment, such as lights, lead shields, booms, and display monitors. All of these components need to function seamlessly with each other, but also amongst ancillary theatre equipment, such as anaesthetic machines, surgical trolleys, supply carts, towers, ultrasound machines, pressure injectors and even garbage bins. Planners should collaborate early with the future staff utilisers of this space to gain a clear idea of workflow within the room, where knowing the required free space for movement is just as important as the layout of an equipment-loaded room. Though there may seem to be a lot of adjunct technologies in the HOR, it should be remembered that not all procedures require all equipment. Therefore, storage options for high-cost low-frequency instruments and consumables must be available, where HOR proximity, security and room-temperature control should all be considered.
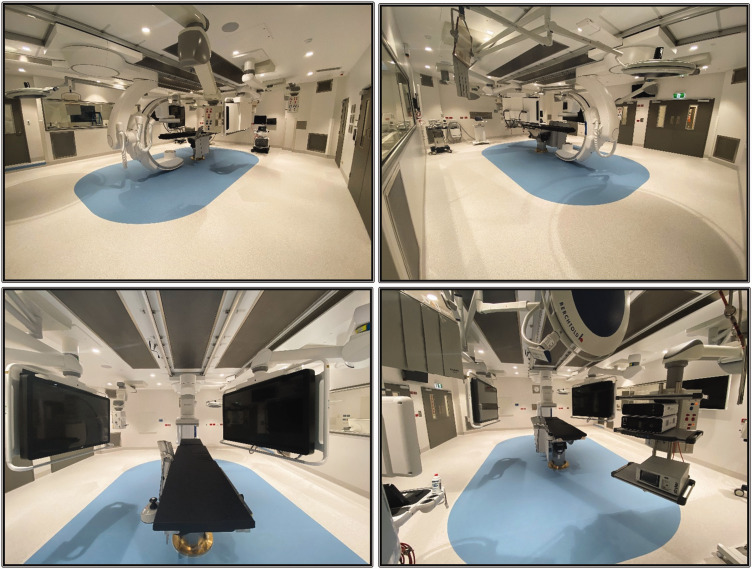
Visiting another centre with an HOR is an invaluable experience. Understanding the regrets of a previous build or installation will inform clever solutions. Given most rooms are built around an imaging system, several of the companies that produce fluoroscopy units will have lists of their previous installations. We would encourage a collegiate call to any of the centres on those lists to find out more about the planning and implementation around those particular gantries. An established HOR example is shown in Figure 2.
Figure 2.
Example of layout and pertinent equipment from an established hybrid operating room, showing a ceiling-mounted C-arm, two ceiling-mounted display panels, an operating table with control panel, overhead operating lights, anaesthetic machine, and storage for equipment and devices.
Once the required size and arrangement of the room is established, the overall workflow and patterns of traffic also need their own independent consideration. This applies to all aspects of intended procedures, including movement of the patient to and from the theatre, the intraoperative ergonomics of the room between personnel and equipment, and the interprocedural turn-over time. Policies and procedures for these patterns should be developed when designing the HOR layout. This should be periodically updated following its construction to facilitate optimal productivity. Given the vast range of equipment needed by different surgical subspecialties (for example cardiopulmonary bypass machine during cardiac surgery), and the resulting delays to workflow when making rearrangements, block scheduling specific procedures to specific days is useful. Using the example above, by scheduling cardiac surgery to dedicated days, equipment can be arranged in a timely manner, affording easier management of staffing requirements including surgeons, cardiologists, anaesthetists, perfusionists, radiographers, nursing teams and industry representatives. However, it should be noted that with extra equipment and staff comes a reduction of space for sterile fields. Though routine procedures should be planned for, ‘stress-scenarios’ need to be evaluated for their impact on workflow and the ability to maintain sterility. Some of these ‘stress-scenarios’ may include the conversion of endovascular aortic repair cases to open surgery; medical emergency responses, such as on-table cardiac arrest; or an unprecedented lack of space at the foot of the bed during certain peripheral vascular surgical interventions. Particularly during this new pandemic era, another important scenario to prepare for would be managing patients with (confirmed or suspected) highly transmissible diseases. Protocols for such situations are best developed with the implementation of simulation-based training for regular staff who would be operating in the HOR. Not only would this achieve better patient outcomes, but training for surgical and interventional registrars would be enhanced, benefiting the hospital as a patient healthcare service and staff training centre.
Key equipment considerations
With a wide range of novel procedures, space limitations, a demand for return on investment, and a need to deliver better patient outcomes versus traditional surgical interventions, the HOR installations require careful selection. As the standard of care is determined by the stakeholders utilising the room, clear, early and frequent communication is key. The cornerstone technology of an HOR is the imaging or angiography system. Decisions surrounding this aspect of planning are heavily influenced by the subspecialities that will be primarily utilising the room. The use of mobile C-arms is widely considered insufficient for a multitude of reasons, including (but not limited to) low image-quality, smaller field-of-view, increase in scatter radiation, and concerns surrounding hygiene, given storage, dormancy, poor integration and inter-theatre usage.4,7 Fixed angiographic systems help to address some of these issues, however, they do take up more theatre space. Such units include monoplane or biplane, which can be floor-mounted, ceiling-mounted, or both (biplane only). Many offer even more features that mobile arms cannot, including auto-mapping, smart-masking, spectral computed tomography (CT), CT fusion and perfusion analyses.
In the setting of dedicated use by cardiologists, electrophysiologists and neuro-interventionalists, a biplane system may be ideal. Nonetheless, this adds significant complexity to a space-limited room, particularly for the anaesthetic team. 8 Monoplane systems with a large detector are therefore ideal in an HOR with a predominantly surgical domain. Ceiling mounting confers total body coverage, without needing any, or minimal, movement from the table itself - a benefit of particular importance in patients with a multitude of lines and monitoring equipment from the anaesthetic team. But, ceiling-mounted systems have some pitfalls where significant ceiling space is required, potentially impacting other fixtures, such as lights, lead shields and towers. Ceiling-mounted imaging systems can, hypothetically, impair laminar airflow, raising the possibility (albeit low) of collecting dust that may fall onto the operative field and result in contamination. Another often overlooked yet important consideration with mounted imaging systems is the ability to station the machine away from the operating table. This ability clears the space to other non-imaging-guided or non-endovascular procedures, allowing the HOR to serve a multitude of other general purposes.
The operating table is a key component of the HOR. Table design selection, again, is primarily based on the involved surgical subspecialties, and will need a form of compromise to marry endovascular and open surgical procedures. In short, classical angiographic tables will provide a radiolucent carbon-fibre table that is ‘floating’. This allows effective and accurate movements as well as full-body coverage but is non-customisable to specific positioning. On the other hand, a standard operating table is ‘breakable’ and has in-built side-rails, offering the ability to alter the shape in multiple areas, allowing a high degree of optional positioning and attachment of ancillary equipment, however lacking in total radiolucency. Having additional rails and other attachments for flatter, carbon-fibre tables provides a greater degree of compatibility with open surgical devices, such as body-wall retractors, additional lead shields and side-arm tables. This proves particularly useful when multiple points of endovascular access may be required for specific cases, such as femoral and brachial access during a fenestrated endovascular aortic repair. Other key table considerations should also include multi-axis tilt, height adjustability, and total load limit, particularly in the potential setting of cardiac arrest and the added weight of the resuscitator performing chest compressions. It is important to remember that if the HOR has an imaging only table, then for some procedures patients cannot be placed in specific positions – for example lithotomy, or beach chair. This then means that the HOR cannot be used as an additional standard operating room when required. Hence, it must be rationalised if the most appropriate investment would be for either a custom tabletop creation and fittings, or alternatively, purchasing both angiographic and open surgical tables individually to be used interchangeably.
Organising the team
No guidelines currently exist that offer recommendations for HOR staffing arrangements, which would vary significantly depending on the planned procedures and specialty interest. Nevertheless, it should be recognised that in the early stages of use, on average there will be more staff required for a hybrid procedure compared with traditional open surgery versus endovascular surgery in isolation. This includes the presence of skilled radiographers, nursing staff with expertise in open-surgical and catheter-based procedures (and the challenging associated devices), and theatre technicians familiar with the movement, replacement, and storage of HOR-specific equipment. As training and familiarity within the HOR increases, this total number of in-room staffing would likely decrease. For hospitals constructing their first HOR, these members of staff are usually deployed across multiple different departments, such as medical imaging and surgery. Though exposure to cross-specialty training is essential for working in a hybrid environment, it should be noted that staff coming from separately managed departments may pose some logistical challenges, including schedule clashes, budgeting and payment of services, overtime rostering, as well as underlying departmental governance.
Having a dedicated team carries significant benefits, where professional familiarity between personnel leads to improvements in both patient outcomes as well as overall intraoperative efficiency. 9 Though HOR functionality should commence with several months of carefully planned and scheduled procedures during daylight-hours to facilitate training and develop the team, the team pool needs to be large enough to offer an around-the-clock roster when eventually running at full capacity. However, in a region with workforce limitations, this may never be possible. If implementing an HOR and team for the first time, there are certainly some key character traits for desirable staff members that will promote sustainability and future-proofing of the service. There is a steep learning curve required in radiation training, and the simultaneous management of open and endovascular procedures; teachability certainly cannot be overlooked. Furthermore, collegiality is of utmost importance, where staff should be confident in their ability to communicate and collaborate clearly within the new HOR environment, as well as cope with the added stress imposed by the changes in protocols and procedure brought about. Finally, staff must be engaged in the vision for the department, and in acquiring the skills associated with its fruition. Having a dedicated nursing coordinator responsible for rostering, education and workflow helps guide this new team and the blooming trajectory of the HOR program – ensuring the team maintains a willingness to challenge fundamental theatre processes that may be traditional, but outdated. As the team and service grows, maintaining excellence in working relationships between multiple clinical disciplines will be sure to attract expert medical staff wishing to participate in a hospital with such a service.
Conclusion
The HOR is a highly complex and customisable facility paving the future for surgical and trauma services. With hybrid operative techniques rapidly evolving the standard model of care, a multidisciplinary approach is essential when conceptualising and building a technologically advanced service aimed at offering world class patient care. Through experience, an understanding of the challenges and complexities faced by a new hybrid surgical service can be shared, providing guidance in its effective implementation. Although the initial capital outlay serves as a barrier to the construction of an HOR, a clear objective envisioned by the stakeholder group with careful consideration of location, layout, equipment, workflow, and team organisation will serve to positively impact the health service through improved patient outcomes and healthcare, whilst providing a positive return on investment.
Author contributions: All authors contributed to the research and preparation of this manuscript.
The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Tahmid Zaman https://orcid.org/0000-0002-5226-6172
Data availability statement
Data are available from the corresponding author upon reasonable request.
References
- 1.Loftus TJ, Croft CA, Rosenthal MD, et al. Clinical impact of a dedicated trauma hybrid operating room. J Am Coll Surg 2021; 232: 560–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin H, Liu J. Application of the hybrid operating room in surgery: a systematic review. J Invest Surg 2022; 35: 378–389. [DOI] [PubMed] [Google Scholar]
- 3.Kaneko T, Davidson MJ. Use of the hybrid operating room in cardiovascular medicine. Circulation 2014; 130: 910–917. [DOI] [PubMed] [Google Scholar]
- 4.Sikkink CJ, Reijnen MM, Zeebregts CJ. The creation of the optimal dedicated endovascular suite. Eur J Vasc Endovasc Surg 2008; 35: 198–204. [DOI] [PubMed] [Google Scholar]
- 5.Singh A, Mehta Y, Parakh R, et al. Role of hybrid operating room in surgery for the right atrial thrombus, pulmonary thrombi, and ventricular septal rupture after myocardial infarction. Ann Card Anaesth 2016; 19: 717–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Attigah N, Demirel S, Hakimi M, et al. Hybrid operating rooms versus conventional operating rooms: Economic comparisons in vascular surgery using the example of endovascular aneurysm repair. Chirurg 2017; 88: 587–594 [In German, English abstract]. [DOI] [PubMed] [Google Scholar]
- 7.Nollert G, Hartkens T, Figel A, et al. The hybrid operating room. In: Narin C. (ed) Special Topics in Cardiac Surgery, London: IntechOpen; 2012, pp. 73–107. [Google Scholar]
- 8.Singh A. Hybrid operating room: clinical applications. The Indian Anaesthetists' Forum 2016; 17: 35–36. [Google Scholar]
- 9.Mathis MR, Yule S, Wu X, et al. The impact of team familiarity on intra and postoperative cardiac surgical outcomes. Surgery 2021; 170: 1031–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.