Abstract
Background
The proliferation of electronic cigarettes (e-cigarettes) has presented new challenges in public health, particularly among adolescents and young adults. While marketed as safer than tobacco and as cessation aids, e-cigarettes have raised concerns about their long-term health and psychosocial impacts, including potential links to increased suicidal behaviors. This study aims to evaluate the relationship between e-cigarette use and suicidal behaviors by conducting a systematic review of the current literature.
Methods
We searched PubMed, Web of Science, and EMBASE for studies up to March 10, 2024, examining the relationship between e-cigarette use and suicidal behaviors. Eligible studies included cross-sectional, longitudinal, retrospective, prospective, and case–control designs. Meta-analysis was performed to calculate pooled odds ratios (ORs). Newcastle Ottawa scale was used to assess the quality of studies. R software (V 4.3) was used to perform the meta-analysis.
Results
Our analysis included fourteen studies, predominantly from the US and Korea, with participants ranging from 1,151 to 255,887. The meta-analysis identified a significant association between e-cigarette use and an increased risk of suicidal ideation (OR = 1.489, 95% CI: 1.357 to 1.621), suicide attempts (OR = 2.497, 95% CI: 1.999 to 3.996), and suicidal planning (OR = 2.310, 95% CI: 1.810 to 2.810). Heterogeneity was noted among the studies.
Conclusion
E-cigarette use is significantly associated with the risk of suicidal behaviors, particularly among adolescents. The findings underscore the necessity for caution in endorsing e-cigarettes as a safer smoking alternative and call for more extensive research to understand the underlying mechanisms. Public health strategies should be developed to address and mitigate the risks of suicidal behaviors among e-cigarette users.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-024-06012-7.
Keywords: Electronic cigarettes, Mental health, Adolescent health, Suicide, Self-harm, Nicotine, Public health, Good health and well-being, Global health targets, Suicide prevention
Introduction
The advent of electronic cigarettes (e-cigarettes) has ushered in a new era in the landscape of tobacco consumption, offering a technological alternative to traditional smoking methods [1–4]. Marketed as a safer option and a potential tool for smoking cessation, e-cigarettes have rapidly gained popularity among various demographics, notably among teens and young adults [5]. However, this rise in e-cigarette use has been paralleled by growing concerns among health professionals and researchers regarding their long-term health implications and psychosocial outcomes [6–11].
The use of e-cigarettes, especially among adolescents and young adults, poses significant health concerns [12]. While e-cigarettes are often marketed as a safer alternative to traditional tobacco products, they are not without risks [11, 13]. Studies have shown that e-cigarette use can lead to increased exposure to harmful chemicals such as nicotine, which can adversely affect brain development in youths and lead to addiction. Additionally, there is evidence linking e-cigarette use with respiratory issues and the potential for cardiovascular harm [14]. The prevalence of e-cigarette use among adolescents and young adults has been rising, driven by factors such as appealing flavors, targeted marketing, and the perception of reduced harm compared to smoking [15]. This trend is alarming, as early exposure to nicotine can establish long-lasting addictive behaviors, potentially leading to the use of other tobacco products and sustaining a cycle of dependence that can be difficult to break.
Among the most alarming potential consequences is the impact of e-cigarette use on mental health, a subject that has recently begun to garner attention within the scientific community [16, 17]. Suicidal behaviors, encompassing suicidal ideation, planning, attempts, and completed suicide, represent a significant public health issue worldwide [18]. The World Health Organization (WHO) reports that nearly 700,000 people pass away from suicide each year, positioning it as the second most common cause of death among individuals aged 15 to 29 years. [19]. The etiology of suicidal behaviors is multifaceted, with a complex interplay of psychological, genetic, and environmental and social factors [20, 21]. Recently, substance use, including the consumption of nicotine through smoking, has been identified as a risk factor for suicidal behaviors [22–24]. Nicotine's neurobiological effects, which can influence mood and cognitive function, alongside the psychosocial aspects of substance use, may contribute to this association [23, 25].
The emergence of e-cigarettes, which deliver nicotine without the combustion of tobacco, was initially met with optimism for their potential to reduce the harm associated with traditional cigarette smoking [26, 27]. Nonetheless, the impact of e-cigarettes on mental health, and specifically their association with suicidal behaviors, remains underexplored and poorly understood. Preliminary studies have suggested a potential association between e-cigarette use and increased risk of suicidal behaviors [28–31]. Some studies have found that e-cigarette use is associated with increased suicidal ideation, suicide planning, and suicide attempts among adolescents. For instance, a study in South Korea found that among male participants, rates of suicidal ideation, suicide planning, and suicide attempts were higher among those who initially used e-cigarettes compared to those who initially used conventional cigarettes or never smoked [32]. Similarly, a scoping review of vaping and mental health found that e-cigarette use was associated with depression, suicidal ideation, and suicide attempts among adolescents [33]. Additionally, a study in the US found that the use of e-cigarettes was associated with 23% increased odds of seriously considering attempting suicide in the prior year among more than 25,000 adolescents participating in the US Youth Risk Behavior Survey [34]. These findings suggest that e-cigarette use may be a significant risk factor for suicide behaviors globally.
A systematic review has yet to be conducted to assess this issue. This systematic review and meta-analysis aimed to address this gap by evaluating the existing body of research on the association between e-cigarette use and suicidal behaviors. By aggregating data from diverse studies, this work seeks to provide a more robust understanding of the relationship. Through this analysis, we endeavor to contribute valuable insights into the potential psychosocial risks associated with e-cigarette use, offering a foundation for future research and informing policy-makers and healthcare providers in their efforts to mitigate the adverse outcomes related to e-cigarette consumption.
Methods
This systematic review and meta-analysis adhered to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to ensure transparency and completeness in reporting [35] (Table S1). The aim was to systematically review and synthesize existing literature on the association between e-cigarette use and suicidal behaviors, including suicidal ideation, planning, attempts, and completion. This systematic review has been registered prospectively in PROSPERO.
Search strategy
A search strategy was developed to identify studies that investigated the association between e-cigarette use and suicidal behaviors. Electronic databases, including PubMed, Web of Science, and EMBASE, were searched from their inception to March 10, 2024. The search strategy combined terms related to e-cigarettes (e.g., "electronic cigarettes," "e-cigarettes," "vaping") with terms related to suicidal behaviors (e.g., "suicide," "suicidal" AND “self-harm"). Both MeSH terms (where applicable) and free text terms were used. The search strategy is displayed in Table S2.
Eligibility criteria
For inclusion, we considered studies involving participants from the general population without any restrictions, thus allowing for a broad and inclusive analysis. The exposure of interest was clearly defined as the use of e-cigarettes, vaping products, or Electronic Nicotine Delivery Systems (ENDS), excluding studies that focused solely on traditional tobacco smoking due to its well-documented effects and distinct mechanisms compared to e-cigarettes. Regarding outcomes, we aimed to include studies that investigated suicidal ideation, suicidal planning, and suicidal attempts, explicitly excluding research that focused on non-suicidal self-harms to maintain a clear focus on suicidal behaviors directly. In terms of study design, our criteria included a wide range of observational studies, encompassing cross-sectional, longitudinal, retrospective, prospective, and case–control studies. We excluded qualitative studies, policy analyses, opinion pieces, case studies, case reports, reviews, and animal studies from our analysis, as these did not offer the empirical evidence necessary to address our research question directly (Table S3).
Study selection
Titles and abstracts were screened for eligibility independently by two reviewers, utilizing Nested-Knowledge web software for the process. Subsequently, full texts of studies that appeared potentially suitable were retrieved and assessed independently for inclusion. Any discrepancies were settled through discussion or by consulting a third reviewer.
Data extraction
Data extraction was conducted independently by two reviewers utilizing a uniform data extraction template. The information extracted encompassed characteristics of the study (such as author, publication year, country, design of the study, and size of the sample), demographics of the participants, and outcomes pertaining to suicidal behaviors. Discrepancies encountered during the data extraction process were addressed through discussions or by seeking the opinion of a third reviewer.
Quality assessment
The assessment of the quality of the included studies was carried out using the Newcastle–Ottawa Scale. This scale assesses the selection criteria of the study groups, the comparability between these groups, and the determination of the exposure or outcome of interest.
Statistical analysis
The meta-analysis employed a random-effects model (REM) to accommodate expected variability among the studies, offering a more standardized estimate of the overall effect. This approach is designed to manage the inherent differences found across studies. The relationship between the use of e-cigarettes and suicidal behaviors was measured using odds ratios (ORs) accompanied by 95% confidence intervals (CIs). The degree of heterogeneity between the studies was evaluated using the I2 statistic [36]. Additionally, a 95% prediction interval was utilized to provide deeper insight into the degree of heterogeneity. To examine publication bias, funnel plots and Egger's test were applied. The analysis was conducted using the ‘Meta’ and ‘Metafor’ packages within the R statistical software (Version 4.3) [37].
Result
Literature search
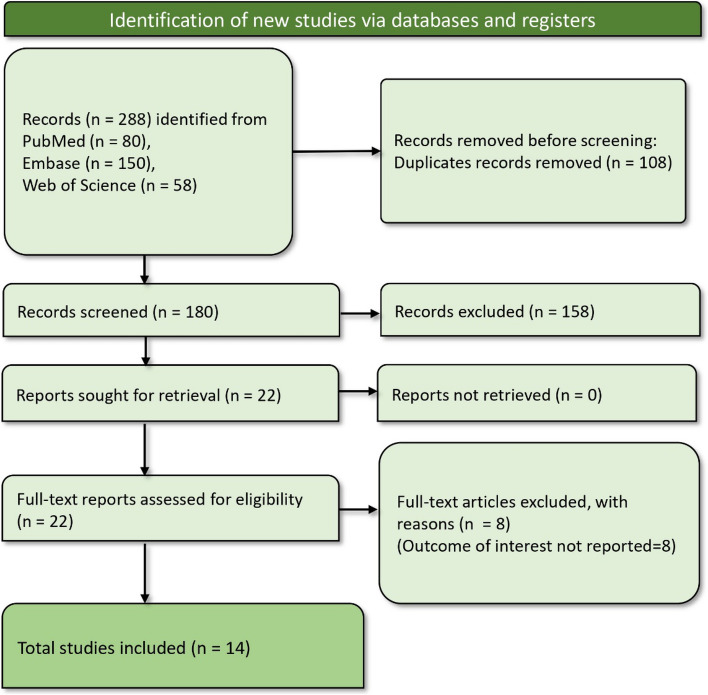
The initial search yielded 288 records, which were reduced to 180 after the removal of 108 duplicate entries. Each of these records was screened based on our predefined criteria, identifying 22 potentially relevant reports for full retrieval. Upon closer examination, eight of these were excluded due to their lack of reporting on the outcomes of interest, specifically related to suicidal behaviors in the context of e-cigarette use. The screening process culminated in selecting 14 suitable studies [28–32, 38–46] for inclusion in our systematic review and meta-analysis (Fig. 1).
Fig. 1.
PRISMA flow diagram showing article screening and study selection process
Characteristics of included studies
The included studies in this systematic review primarily focus on the United States (US) and Korea, with a single study from Canada (Table 1). These studies employed a cross-sectional design to investigate the association between e-cigarette use and suicidal behaviors across diverse demographic groups, including active-duty service members, adolescents, bisexual high school students, asthmatic adolescents, the general population, and middle and high school students. The sample sizes vary significantly, ranging from 1,151 to 255,887 participants, with most studies reporting a balanced gender distribution where applicable.
Table 1.
Characteristics of included studies
| Study | Country | Design | Population | Sample size | Male% | OR (95% CI) for Suicide ideation | OR (95% CI) for Suicide plan | OR (95% CI) for Suicide attempt |
|---|---|---|---|---|---|---|---|---|
| Ahmed 2023 [38] | USA | Cross-sectional | Active-duty service members from the Army, Navy, Air Force, Marine Corps, and Coast Guard | 17,166 | 83.31 | 2.00 (1.38–2.88) | NA | 2.64 (1.14–6.08) |
| Baiden 2022 [28] | USA | Cross-sectional | High school students | 14,285 | 49.7 | 1.55 (1.30–1.86) | 1.62 (1.34–1.97) | 1.75 (1.41–2.18) |
| Chadi 2019 [29] | USA | Cross-sectional | Adolescents | 26,821 | 48.7 | 1.23 (1.03–1.47) | NA | NA |
| Dunn 2023 [39] | USA | Cross-sectional | Bisexual high school students | 1151 | NA | 1.72 (1.20–2.48) | 1.59 (1.11–2.28) | NA |
| Erhabor 2023 [40] | USA | Cross-sectional | Adolescents | 12,767 | 50.50% | 1.40 (1.13–1.74) | NA | NA |
| Huh 2021 [30] | Korea | Cross-sectional | Adolescents | 57,069 | 52% | 2.29 (1.44–3.65) | 3.38 (1.81–6.33) | 4.26 (2.16–8.38) |
| Jacobs 2021 [41] | USA | Cross-sectional | High School Students | 12,578 | 48.2 | NA | NA | 1.43 (0.88–2.32) |
| Kim 2020 [31] | Korea | Cross-sectional | Asthmatic adolescents | 195,847 | NA | 1.28 (1.18–1.43) | NA | 2.11 (1.51–2.95) |
| Kim 2021 [32] | Korea | Cross-sectional | Adolescents | 255,887 | 51.20% | Male = 1.46 (1.27–1.68), Female = 1.57 (1.26–1.95) | Male = 2.15 (1.79–2.57), female = 2.38 (1.82–3.12) | Male = 2.47 (1.96–3.11), Female = 3.09 (2.31–4.15) |
| Kim 2021 [43] | Korea | Cross-sectional | General population | 39,225 | NA | 1.569 (1.839–3.588) | 3.220 (2.001–5.181) | 4.271 (2.041–8.939) |
| Kim 2021 [42] | Korea | Cross-sectional | Middle and high school students | 5405 | 81.1 | 1.58 (1.31–1.89) | 2.44 (1.94–3.08) | 2.44 (1.85–3.22) |
| Lee 2019 [44] | Korea | Cross-sectional | Adolescents | 62,276 | 50.7 | Total = 2.49 (1.82–3.42), Male = 2.11 (1.45–3.06), Female = 4.05 (2.12–7.72) | Total = 4.63 (3.22–6.67), male = 3.08(1.94–4.91), female = 11.9 (6.28–22.55) | Total = 6.17 (4.13–9.24), Male = 3.64(2.07–6.39), female = 16.42 (8.5–31.71) |
| Pham 2020 [45] | Canada | Cross-sectional | General population | 53,050 | 48.9 | Female = 2.2(0.8–6.0), Male = 2.3(1.0–5.4) | NA | NA |
| Welty 2023 [46] | USA | Cross-sectional | High school students | 10,520 | NA | NA | NA | 3.0 (2.1–3.9) |
Abbreviations: CI Confidence Interval, NA Not Available, OR Odds Ratio
Ahmed's 2023 study [38] on active-duty service members from the US military branches reports an OR of 2.00 for suicide ideation and 2.64 for suicide attempts. Baiden's 2022 [28] research on US high school students shows ORs ranging from 1.55 for suicide ideation to 1.75 for suicide attempts, with explicit data on planning as well. Chadi's 2019 study [29], Dunn's 2023 study [39], and Erhabor's 2023 study [40], all based in the US, focus on adolescents and specific groups such as bisexual students, offering varying ORs for suicide ideation and plans. Huh's 2021 study [30] stands out with its Korean adolescent population, presenting higher ORs, especially for suicide attempts, peaking at 4.26. Kim's series of studies from 2020 and 2021 in Korea explore different populations, including asthmatic adolescents and the general population, with ORs for suicide ideation and attempts indicating a considerable risk associated with e-cigarette use. Lee's 2019 [44] study from Korea provides a detailed breakdown by gender, revealing a stark contrast in ORs for suicide attempts between males and females. Pham's 2020 study [45] is the only Canadian entry offering gender-specific ORs for suicide ideation. Finally, Welty's 2023 study [46] focuses on US high school students, providing data exclusively for suicide attempts with an OR of 3.0. The quality assessment of studies is given in Table S4.
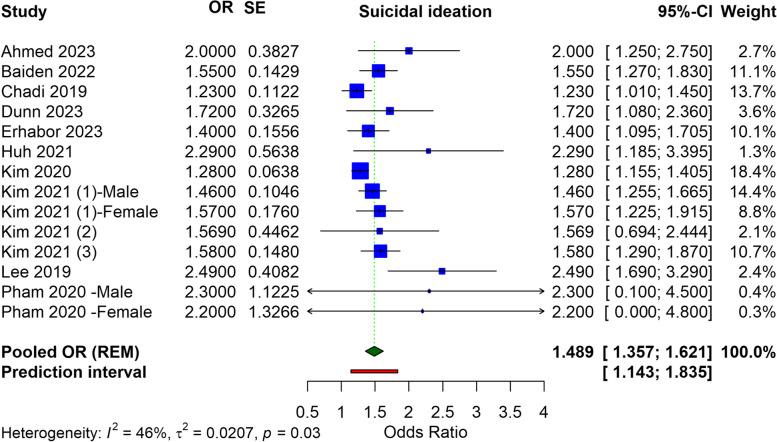
Suicide ideation
The meta-analysis for suicidal ideation associated with electronic cigarette use incorporated data from various studies, yielding pooled ORs. The pooled OR, derived using a REM, stands at 1.489 (95% CI: 1.357 to 1.621), indicating a significant relationship between e-cigarette use and an increased risk of suicidal ideation. This pooled estimate, while accounting for the variability among individual study results, underscores a nearly 50% increase in the odds of suicidal ideation among e-cigarette users versus non-users. The prediction interval (1.143 to 1.835) suggests that the true effect in an individual study is expected to lie within this range 95% of the time. The heterogeneity of the analysis, as shown by an I2 value of 46%, suggests moderate variability (Fig. 2). In adolescents or children who use e-cigarettes, the pooled OR for suicide ideation was found to be 1.46 (95% CI: 1.332 to 1.589), with a heterogeneity of I2 = 56% (Figure S1).
Fig. 2.
Forest plot illustrating the meta-analysis of association of e-cigarettes and suicidal ideation
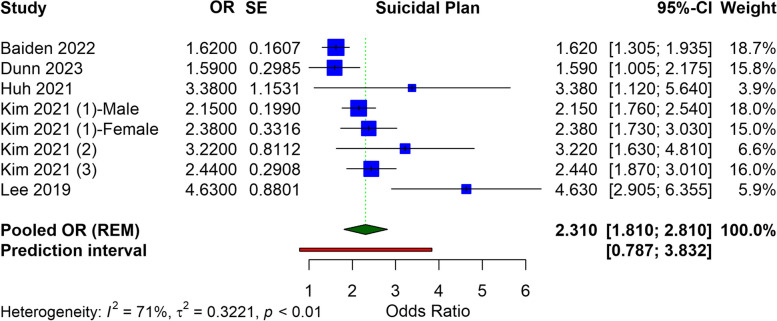
Suicidal plan
In the meta-analysis examining the relationship between e-cigarette use and suicidal planning, a pooled analysis of the selected studies was conducted. The OR for suicidal planning is calculated at 2.310 (95% CI: 1.810 to 2.810), suggesting a statistically significant relationship between e-cigarette use and a heightened risk of suicidal planning. The heterogeneity among the studies, indicated by an I2 value of 71%, is considered substantial. The prediction interval, from 0.787 to 3.832, also indicates the expected range of true effects in similar future studies, acknowledging the variability observed in the current analysis. This wide range suggests that while the overall trend points towards increased risk, individual studies may report varying degrees of association (Fig. 3). In adolescents or children who use e-cigarettes, the pooled OR for suicide planning was found to be 2.226 (95% CI: 1.739 to 2.712), with a heterogeneity of I2 = 73% (Figure S2).
Fig. 3.
Forest plot illustrating the meta-analysis of association of e-cigarettes and suicidal plan
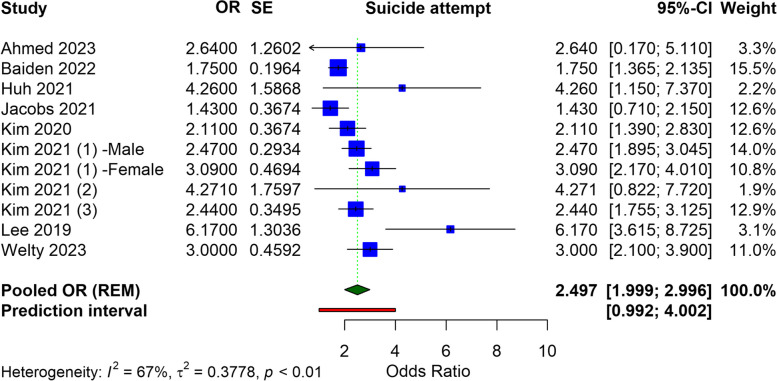
Suicidal attempt
In the meta-analysis regarding the link between e-cigarette use and suicide attempts, the selected studies encompassed a variety of populations and settings, providing a broad perspective on the issue. The ORs from individual studies point toward a relationship between e-cigarette use and an elevated risk of suicide attempts. The aggregated results yield a pooled OR of 2.497 (95% CI: 1.999 to 3.996), which indicates a significant risk of suicide attempts among e-cigarette users. The heterogeneity of the analysis is high, with an I2 value of 67%. Despite this variability, the prediction interval, ranging from 0.992 to 4.002, suggests that future studies are likely to find a true effect within this range, supporting the presence of a linkage between e-cigarette use and suicide attempts (Fig. 4). In adolescents or children who use e-cigarettes, the pooled OR for suicide attempts was found to be 2.462 (95% CI: 1.944 to 2.980), with a heterogeneity of I2 = 72% (Figure S3).
Fig. 4.
Forest plot illustrating the meta-analysis of association of e-cigarettes and suicide attempt
Sensitivity analysis
We performed a sensitivity analysis using the leave-one-out approach, and no significant variation in the results was noted for any of the outcomes. All outcomes remain significantly associated with e-cigarette use in the sensitivity analysis (Figures S4–S6).
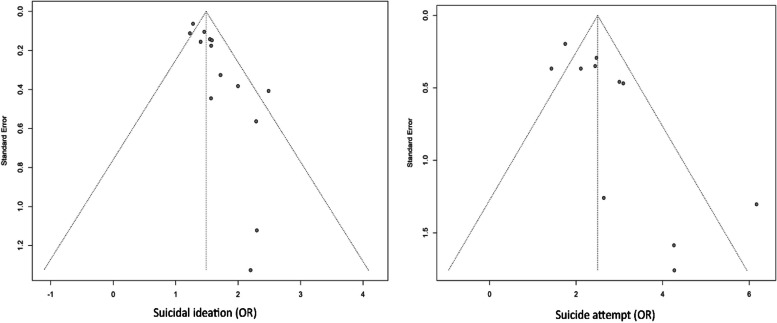
Publication bias
The assessment for publication bias in our meta-analysis was conducted through visual inspection of funnel plots and the Egger test for suicidal attempts and ideation, as presented in Fig. 5. Due to the limited number of studies available, we did not statistically evaluate publication bias for suicidal planning. Visual inspection of the funnel plots revealed asymmetry. Furthermore, the Egger test results (p = 0.0008 for suicidal ideation, p = 0.0143 for suicidal attempts) also indicated the presence of publication bias.
Fig. 5.
Funnel plot showing publication bias assessment
We further performed trim and fill analyses (Figures S7 and S8). The OR for suicide ideation was found to be 1.3865 (95% CI: 1.2459 to 1.5271), and for suicide attempts, it was 2.0404 (95% CI: 1.3660 to 2.7148). These results indicate that, even without the effects of small studies, the association between e-cigarette use and suicidal behaviors remains significant.
Discussion
The findings from our study provide strong evidence of a significant association between e-cigarette use and an increased risk of suicidal behaviors, including ideation, plan and attempts. This is particularly notable given the rising prevalence of e-cigarette use, especially among adolescents and young adults. Our analysis indicates a nearly 50% increase in the odds of suicidal ideation and more than a doubling in the risk of suicide attempts among e-cigarette users. These associations persisted in general population and adolescents, suggesting a potential universal relationship between e-cigarette use and suicidal behaviors rather than one confined to specific contexts.
The potential mechanisms underlying the relationship between e-cigarette use and suicidal behaviors could be multifactorial. Nicotine is a primary component in most e-cigarettes and is known to influence neurotransmitter activity within the brain, potentially altering mood [23]. Additionally, nicotine dependence may contribute to psychological stress, a well-documented risk factor for suicidal behaviors. This is particularly concerning as nicotine can impact neurobiological changes during critical periods of brain development among adolescents, underscoring the potential for e-cigarettes to affect mental health in this vulnerable group.
The findings of this study might also be shaped by cultural and social factors that can influence both e-cigarette usage and suicidal behaviors. Different cultural attitudes towards mental health, smoking, and the acceptance of e-cigarettes can significantly affect how individuals perceive and engage with these products [47, 48]. Social norms, the prevalence of e-cigarette advertising, and the level of awareness about mental health issues vary widely across different regions and cultures, potentially impacting the prevalence of e-cigarette use and its association with suicidal behaviors [49]. Therefore, cultural context and social dynamics variations are essential considerations when interpreting the results and could explain differences in the observed outcomes across different populations.
Prior systematic reviews have explored the impact of e-cigarettes on mental health. For example, Becker et al.'s study highlighted increased mental health issues in young e-cigarette users relative to non-users, particularly in adolescents [17]. Beyond mental health, e-cigarettes have been associated to a range of adverse health outcomes, such as addiction, poisoning, inhalation toxicity, cardiovascular alterations, and diminished lung function as indicated by an umbrella review [50]. Furthermore, the use of e-cigarettes among individuals who have never smoked is linked with an increased likelihood of tobacco smoking initiation, potentially leading to regular smoking habits [51]. A previous scoping review found that suicide attempts were notably more frequent in individuals who used e-cigarettes compared to those who did not [33]. The use of e-cigarettes was linked with depression, suicidal ideation, and suicide attempts [33]. There was a significant increase in suicide attempts among e-cigarette users relative to non-users. These results are comparable to ours.
E-cigarettes, frequently advertised as safer substitutes for conventional cigarettes and as assistance for quitting smoking, are at the centre of ongoing debates. The current evidence on their efficacy and safety is mixed, with no long-term conclusive data to confirm their effectiveness in helping individuals quit tobacco smoking. While some randomized controlled trials (RCTs) have indicated that e-cigarette might assist some smokers in reducing or quitting tobacco use, numerous observational studies have not found significant benefits in quitting tobacco through e-cigarette [52, 53]. Additionally, e-cigarette have associated health risks, such as the potential for nicotine addiction among non-smokers, particularly youth [54, 55].
The regulation of ENDS poses a complex challenge, especially in limiting youth access. The legislative approach to ENDS varies globally, with some countries implementing stringent regulations or outright bans and others having little to no controls. The WHO reports that while 34 countries have banned e-cigarette sales, 88 countries do not restrict age for purchasing these products [56]. Preventing ENDS from becoming a gateway to tobacco smoking for young people necessitates re-evaluation of their accessibility to this demographic. Effective regulation requires ongoing surveillance of ENDS use among both adults and youth, public health initiatives to inform about potential benefits for smokers and risks for non-smokers and young people, and policies mandating the reporting of adverse events.
Our study has some limitations. The cross-sectional nature of the majority of the included studies limits the ability to establish causality. There is also significant variability in the measurement of e-cigarette use and suicidal behaviors across the studies, which could contribute to the heterogeneity of our findings. The lack of longitudinal studies prevents a more thorough examination of the temporal relationship between these variables. Additionally, the majority of the research is concentrated in the USA and Korea, which may limit the generalizability of our findings to other regions. The presence of publication bias is also a concern, as studies with non-significant findings may be underrepresented in the literature. Our analysis might not have fully considered all relevant demographic variables that could influence the relationship between e-cigarette use and suicidal behaviors, such as socioeconomic status or underlying mental health conditions. Finally, the rapid evolution of e-cigarette products and the variability in their nicotine content might not have been fully accounted for, which could affect the applicability of our results to all e-cigarette users.
Conclusion
Our analysis provided evidence of a relationship between e-cigarette use and an increased risk of suicidal ideation, plan, and attempts. The findings highlight the need for caution among health professionals and policy-makers in promoting e-cigarettes as safe alternatives to smoking. They also point to the necessity for further, high-quality research to explore the interventions aimed at reducing suicidal behaviors among e-cigarette users. Given the significant public health implications, a coordinated effort to address the mental health risks associated with e-cigarette use is warranted.
Supplementary Information
Acknowledgements
The authors acknowledge the Nested-Knowledge, MN, USA for providing the access to the software.
Name of internal review board
Not applicable.
Authors’ contributions
Substantial contribution to the conception or design of the work: RI, AMG, MNK. Acquisition of data: MS-2, SB, PB. Analysis and interpretation of data for the work: IA, MRK, AS, KP. Drafting the work: HAS, M2. AS. Revising it critically for important intellectual content: AAA, KP, MS, PB,SB, MRK. Resources: AAA, HAS, MS, KP. Final approval of the version to be published: All authors (AAA, RI, AMG, MNK, SB, PB, MS, IA, MRK, AS, KP, HAS, MS-2). Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: All authors (AAA, RI, AMG, MNK, SB, PB, MS, IA, MRK, AS, KP, HAS, MS-2).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This study received no funding.
Availability of data and materials
The data is with the authors and available on request to the corresponding author (HAS), Email: habuserhan@hamad.qa.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abdelaziz A. Awad and Ramaiah Itumalla contributed as first authors.
Contributor Information
Abdelaziz A. Awad, Email: awad.abdelaziz.0505@gmail.com
Abhay M. Gaidhane, Email: abhay.psm@dmiher.edu.in
Hashem Abu Serhan, Email: habuserhan@hamad.qa.
References
- 1.Kaisar MA, Prasad S, Liles T, Cucullo L. A decade of e-cigarettes: limited research & unresolved safety concerns. Toxicology. 2016;365:67–75. 10.1016/j.tox.2016.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamb N. E-cigarettes. Lancet. 2019;393(10174):876. 10.1016/S0140-6736(18)33196-9 [DOI] [PubMed] [Google Scholar]
- 3.Hammond S, Phillips J. E-Cigarettes and Vaping. Workplace Health Safety. 2020;68(6):301-. 10.1177/2165079920914635 [DOI] [PubMed] [Google Scholar]
- 4.Rom O, Pecorelli A, Valacchi G, Reznick AZ. Are E-cigarettes a safe and good alternative to cigarette smoking? Ann N Y Acad Sci. 2015;1340(1):65–74. 10.1111/nyas.12609 [DOI] [PubMed] [Google Scholar]
- 5.Bauld L, MacKintosh AM, Eastwood B, Ford A, Moore G, Dockrell M, et al. Young people’s use of e-cigarettes across the United Kingdom: findings from five surveys 2015–2017. Int J Environ Res Public Health. 2017;14(9):973. 10.3390/ijerph14090973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med. 2020;58(2):182–90. 10.1016/j.amepre.2019.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chatterjee S, Caporale A, Tao JQ, Guo W, Johncola A, Strasser AA, et al. Acute e-cig inhalation impacts vascular health: a study in smoking naive subjects. American J Physiol Heart Circulat Physiol. 2021;320(1):H144–58. 10.1152/ajpheart.00628.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sapru S, Vardhan M, Li Q, Guo Y, Li X, Saxena D. E-cigarettes use in the United States: reasons for use, perceptions, and effects on health. BMC Public Health. 2020;20(1):1–10. 10.1186/s12889-020-09572-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skotsimara G, Antonopoulos AS, Oikonomou E, Siasos G, Ioakeimidis N, Tsalamandris S, et al. Cardiovascular effects of electronic cigarettes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2019;26(11):1219–28. 10.1177/2047487319832975 [DOI] [PubMed] [Google Scholar]
- 10.Ebersole J, Samburova V, Son Y, Cappelli D, Demopoulos C, Capurro A, et al. Harmful chemicals emitted from electronic cigarettes and potential deleterious effects in the oral cavity. Tob Induc Dis. 2020;18:18. 10.18332/tid/116988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goel S, Shabil M, Kaur J, Chauhan A, Rinkoo AV. Safety, efficacy and health impact of electronic nicotine delivery systems (ENDS): an umbrella review protocol. BMJ Open. 2024;14(1):e080274. 10.1136/bmjopen-2023-080274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hajat C, Stein E, Shantikumar S, Niaura R, Ferrara P, Polosa R. A scoping review of studies on the health impact of electronic nicotine delivery systems. Int Emerg Med. 2022;17:1–28. 10.1007/s11739-021-02835-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asfar T, Maziak W. The risk and safety profile of electronic nicotine delivery systems (ENDS): an umbrella review. European J Public Health. 2022;32(Supplement_3):ckac129. 638. 10.1093/eurpub/ckac129.638 [DOI] [Google Scholar]
- 14.Banks E, Yazidjoglou A, Brown S, Nguyen M, Martin M, Beckwith K, et al. Electronic cigarettes and health outcomes: umbrella and systematic review of the global evidence. Med J Aust. 2023;218(6):267–75. 10.5694/mja2.51890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collins L, Glasser AM, Abudayyeh H, Pearson JL, Villanti AC. E-cigarette marketing and communication: how e-cigarette companies market e-cigarettes and the public engages with e-cigarette information. Nicotine Tob Res. 2019;21(1):14–24. 10.1093/ntr/ntx284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riehm KE, Young AS, Feder KA, Krawczyk N, Tormohlen KN, Pacek LR, et al. Mental health problems and initiation of e-cigarette and combustible cigarette use. Pediatrics. 2019;144(1):e20182935. 10.1542/peds.2018-2935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Becker TD, Arnold MK, Ro V, Martin L, Rice TR. Systematic review of electronic cigarette use (vaping) and mental health comorbidity among adolescents and young adults. Nicotine Tob Res. 2021;23(3):415–25. 10.1093/ntr/ntaa171 [DOI] [PubMed] [Google Scholar]
- 18.Bai W, Liu Z, Jiang Y, Zhang Q, Rao W, Cheung T, et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. 2021;11(1):552. 10.1038/s41398-021-01671-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suicide. World Health Organization; 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/suicide.
- 20.Stack S. Contributing factors to suicide: political, social, cultural and economic. Prev Med. 2021;152:106498. 10.1016/j.ypmed.2021.106498 [DOI] [PubMed] [Google Scholar]
- 21.Favril L, Yu R, Uyar A, Sharpe M, Fazel S. Risk factors for suicide in adults: systematic review and meta-analysis of psychological autopsy studies. BMJ Ment Health. 2022;25(4):148–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lynch FL, Peterson EL, Lu CY, Hu Y, Rossom RC, Waitzfelder BE, et al. Substance use disorders and risk of suicide in a general US population: a case control study. Addict Sci Clin Pract. 2020;15:1–9. 10.1186/s13722-020-0181-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swann AC, Graham DP, Wilkinson AV, Kosten TR. Nicotine inhalation and suicide: clinical correlates and behavioral mechanisms. Am J Addict. 2021;30(4):316–29. 10.1111/ajad.13171 [DOI] [PubMed] [Google Scholar]
- 24.Echeverria I, Cotaina M, Jovani A, Mora R, Haro G, Benito A. Proposal for the inclusion of tobacco use in suicide risk scales: results of a meta-analysis. Int J Environ Res Public Health. 2021;18(11):6103. 10.3390/ijerph18116103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orri M, Séguin JR, Castellanos-Ryan N, Tremblay RE, Côté SM, Turecki G, Geoffroy M-C. A genetically informed study on the association of cannabis, alcohol, and tobacco smoking with suicide attempt. Mol Psychiatry. 2021;26(9):5061–70. 10.1038/s41380-020-0785-6 [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y-Y, Bu F-L, Dong F, Wang J-H, Zhu S-J, Zhang X-W, et al. The effect of e-cigarettes on smoking cessation and cigarette smoking initiation: an evidence-based rapid review and meta-analysis. Tob Induc Dis. 2021;19:19. 10.18332/tid/131624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grabovac I, Oberndorfer M, Fischer J, Wiesinger W, Haider S, Dorner TE. Effectiveness of electronic cigarettes in smoking cessation: a systematic review and meta-analysis. Nicotine Tob Res. 2021;23(4):625–34. 10.1093/ntr/ntaa181 [DOI] [PubMed] [Google Scholar]
- 28.Baiden P, Szlyk HS, Cavazos-Rehg P, Onyeaka HK, Peoples JE, Kasson E. Use of electronic vaping products and mental health among adolescent high school students in the United States: the moderating effect of sex. J Psychiatr Res. 2022;147:24–33. 10.1016/j.jpsychires.2021.12.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chadi N, Li G, Cerda N, Weitzman ER. Depressive symptoms and suicidality in adolescents using e-cigarettes and marijuana: a secondary data analysis from the youth risk behavior survey. J Addict Med. 2019;13(5):362–5. 10.1097/ADM.0000000000000506 [DOI] [PubMed] [Google Scholar]
- 30.Huh Y, Cho H-J. Associations between the type of tobacco products and suicidal behaviors: a nationwide population-based study among Korean adolescents. Int J Environ Res Public Health. 2021;18(2):367. 10.3390/ijerph18020367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim CW, Jeong SC, Kim JY, Lee JS, Lee JH, Jo SH, Kim SH. Associated factors for depression, suicidal ideation and suicide attempt among asthmatic adolescents with experience of electronic cigarette use. Tob Induc Dis. 2020;18:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim SH, Jeong SH, Park EC, Jang SI. Association of cigarette type initially smoked with suicidal behaviors among adolescents in Korea from 2015 to 2018. JAMA Network Open. 2021;4(4):e218803-e. 10.1001/jamanetworkopen.2021.8803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Javed S, Usmani S, Sarfraz Z, Sarfraz A, Hanif A, Firoz A, et al. A scoping review of vaping, E-cigarettes and mental health impact: depression and suicidality. J Community Hosp Intern Med Perspect. 2022;12(3):33–9. 10.55729/2000-9666.1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Striley CW, Nutley SK, Hoeflich CC. E-cigarettes and non-suicidal self-injury: prevalence of risk behavior and variation by substance inhaled. Front Psych. 2022;13:911136. 10.3389/fpsyt.2022.911136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gandhi AP, Satapathy P, Rustagi S, Hermis AH, Sah R, Padhi BK. Comments on" Shigellosis in Southeast Asia: a systematic review and meta-analysis. Travel Med Infect Dis. 2023;102593:10–6. [DOI] [PubMed] [Google Scholar]
- 37.Shamim MA, Gandhi AP, Dwivedi P, Padhi BK. How to perform meta-analysis in R: a simple yet comprehensive guide. Evidence. 2023;1(1):60–80. [Google Scholar]
- 38.Ahmed AE, Yim MH, Dawood J, Olsen CH, Waters AJ, Singer DE, Mancuso JD. Suicidal behaviors among active-duty US service members: data from the 2018 health-related behaviors survey. Psychol Res Behav Manag. 2018;2023:4599–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dunn MS, Yannessa JF. Suicide ideation and behavior and ATOD use among bisexual high school students. J Substance Use. 2023:1–5.
- 40.Erhabor J, Boakye E, Osuji N, Obisesan O, Osei AD, Mirbolouk H, et al. Psychosocial stressors and current e-cigarette use in the youth risk behavior survey. BMC Public Health. 2023;23(1):1080. 10.1186/s12889-023-16031-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacobs W, Idoko E, Montgomery L, Smith ML, Merianos AL. Concurrent E-cigarette and marijuana use and health-risk behaviors among US high school students. Prev Med. 2021;145:106429. 10.1016/j.ypmed.2021.106429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim JS, Kim K. Electronic cigarette use and suicidal behaviors among adolescents. J Public Health. 2021;43(2):274–80. 10.1093/pubmed/fdz086 [DOI] [PubMed] [Google Scholar]
- 43.Kim JY, Kang HS, Jung J-W, Jung SY, Park HJ, Park JS, et al. Nicotine dependence and stress susceptibility in E-cigarette smokers: The Korea national health and nutrition examination survey 2013–2017. Tuber Respir Dis. 2021;84(2):159. 10.4046/trd.2020.0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee Y, Lee K-S. Association of depression and suicidality with electronic and conventional cigarette use in South Korean adolescents. Subst Use Misuse. 2019;54(6):934–43. 10.1080/10826084.2018.1552301 [DOI] [PubMed] [Google Scholar]
- 45.Pham T, Williams JV, Bhattarai A, Dores AK, Isherwood LJ, Patten SB. Electronic cigarette use and mental health: a Canadian population-based study. J Affect Disord. 2020;260:646–52. 10.1016/j.jad.2019.09.026 [DOI] [PubMed] [Google Scholar]
- 46.Welty CW, Gerald LB, Nair US, Haynes PL. Vaping and sleep as predictors of adolescent suicidality. Am J Health Promot. 2023;37(1):39–46. 10.1177/08901171221112027 [DOI] [PubMed] [Google Scholar]
- 47.Nazzal Z, Maraqa B, Azizeh R, AbuAlrub I, Hmeidat M, Al-Jabari F. Exploring the prevalence, knowledge, attitudes and influencing factors of e-cigarette use among university students in Palestine: a cross-sectional study. BMJ Open. 2024;14(2):e080881. 10.1136/bmjopen-2023-080881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oyapero A, Erinoso O, Osoba M, Kareem S. Predictors of electronic cigarettes use and its association with mental health in Nigeria: A community survey. Population Med. 2023;5(December):1–11. 10.18332/popmed/175938 [DOI] [Google Scholar]
- 49.Yazidjoglou A, Watts C, Joshy G, Banks E, Freeman B. Electronic cigarette social norms among adolescents in New South Wales, Australia. Health Promot Int. 2024;39(2):daae018. 10.1093/heapro/daae018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Asfar T, Jebai R, Li W, Oluwole OJ, Ferdous T, Gautam P, Schmidt M, Noar SM, Lindblom EN, Eissenberg T, Bursac Z, Vallone D, Maziak W. Risk and safety profile of electronic nicotine delivery systems (ENDS): an umbrella review to inform ENDS health communication strategies. Tob Control. 2022:tobaccocontrol-2022-057495. 10.1136/tc-2022-057495. IF: 4.0 Q1. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 51.Baenziger ON, Ford L, Yazidjoglou A, Joshy G, Banks E. E-cigarette use and combustible tobacco cigarette smoking uptake among non-smokers, including relapse in former smokers: umbrella review, systematic review and meta-analysis. BMJ Open. 2021;11(3):e045603. 10.1136/bmjopen-2020-045603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hartmann-Boyce J, McRobbie H, Lindson N, Bullen C, Begh R, Theodoulou A, Notley C, Rigotti NA, Turner T, Butler AR, Fanshawe TR, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2021;4(4):CD010216. 10.1002/14651858.CD010216.pub5. [DOI] [PMC free article] [PubMed]
- 53.Hedman L, Galanti MR, Ryk L, Gilljam H, Adermark L. Electronic cigarette use and smoking cessation in cohort studies and randomized trials: a systematic review and meta-analysis. Tob Prev Cessat. 2021;7:62. 10.18332/tpc/142320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vogel EA, Cho J, McConnell RS, Barrington-Trimis JL, Leventhal AM. Prevalence of electronic cigarette dependence among youth and its association with future use. JAMA Network Open. 2020;3(2):e1921513-e. 10.1001/jamanetworkopen.2019.21513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kechter A, Cho J, Miech RA, Barrington-Trimis JL, Leventhal AM. Nicotine dependence symptoms in US youth who use JUUL E-cigarettes. Drug Alcohol Depend. 2021;227:108941. 10.1016/j.drugalcdep.2021.108941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tan AS, Bigman CA. Misinformation about commercial tobacco products on social media—implications and research opportunities for reducing tobacco-related health disparities. Am J Public Health. 2020;110(S3):S281–3. 10.2105/AJPH.2020.305910 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data is with the authors and available on request to the corresponding author (HAS), Email: habuserhan@hamad.qa.