Abstract
Background
Ongoing conflict between multiple armed groups, including pastoralist herders in the Central African Republic (CAR) causes frequent population displacements, food insecurity and scarcity of healthcare services. The inaccessibility and insecurity of many areas of CAR limit data collection and assessments from national nutritional surveys. Community health workers (CHWs) trained by an international non-governmental organisation, The MENTOR Initiative, deliver basic healthcare to children under 5 years old living in hard-to-reach and conflict-affected areas in eight subprefectures of north-west CAR. Their nutritional status and its associations with geography, malaria, season and conflict are unknown.
Methods
CHW monthly records (October 2015–August 2021), Armed Conflict Location and Event Data project conflict data and The World Bank Group meteorological data for eight subprefectures of north-west CAR were analysed. Associations between counts of global acute malnutrition (GAM) assessed by mid-upper arm circumference and malaria, season and conflict were investigated using negative binomial regression.
Results
Of the 457,325 consultations with children aged 6–59 months, 6.2% and 0.4% were classified as moderately or severely malnourished, respectively. The negative binomial model demonstrated differences in counts of GAM by subprefecture. Counts of GAM were positively associated with the case rate of severe malaria (IRR = 1.045; 95% CI: 1.04–1.06) and the rainy season (July–September) (IRR = 1.10; 95% CI: 1.03–1.17). Conflict events coded as Battles in ACLED were associated with lower counts of GAM (IRR = 0.78; 95% CI: 0.62–0.97).
Conclusions
This analysis shows geographical differences in levels of malnutrition in north-west CAR and demonstrates clear associations between malnutrition, season and malaria. It provides evidence that levels of GAM may be underestimated in north-west CAR in areas experiencing conflict. These findings highlight the need for targeted nutritional support to reach children most at risk of malnutrition. CHWs are a proven effective means of delivering essential primary healthcare services in hard-to-reach, conflict-affected areas.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-024-03603-9.
Keywords: Central African Republic, Malnutrition, Malaria, Community health workers, Conflict
Background
The Central African Republic (CAR), land locked in the heart of Africa, gained independence from France in 1960 [1]. Subsequent political instability, civil unrest, and conflict between a growing number of armed groups and pastoralist communities using transhumance corridors across CAR have created a complex and turbulent past and present security situation for the entire population [1]. In 2024, CAR entered its third decade of armed conflict. Battles between multiple rebel groups for control of the country and its resources began soon after Francois Bozizé seized power in 2003 [2]. Conflict escalated into full-scale civil war in 2013 when Seleka, a Muslim rebel coalition, backed by Chadian and Sudanese mercenaries, attacked and took control of the capital city, Bangui, and overthrew the government [3]. Almost continuous armed conflict to date has shattered the country’s essential infrastructure and its population [4]. By 2021, CAR was one of the poorest countries in the world, ranking 188 out of 191 on the Human Development Index [5]. An estimated 71% of its population was living under the international poverty line and it had some of the lowest levels of education indicators [6].
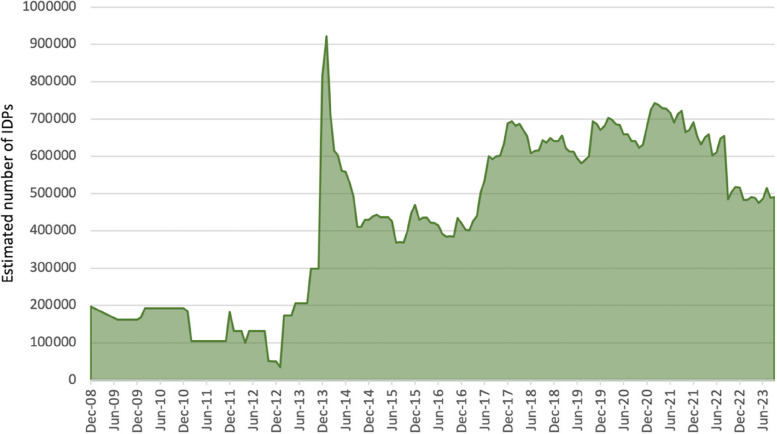
Over 1.3 million (one in every five) people have been forced to flee their homes, of which over 725,000 have sought safety as refugees in neighbouring countries, most others becoming internally displaced people (IDP) seeking refuge in other parts of the country [7]. More than 200,000 people were displaced in a 2-month period alone following violence and insecurity generated by the December 2020 presidential elections [8, 9]. In April 2021, children accounted for around half of the IDP in CAR; recent estimates (December 2023) put the number of IDP at 511,800 [10, 11] (Fig. 1). Access to healthcare services has also been severely affected and where services do exist, they are often in a poor state, with under half estimated to be fully functional [12]. Almost half (2.8 million) of the population (6.1 million) are currently in need of humanitarian assistance, yet despite having one of the highest humanitarian caseloads per capita, this ‘silent crisis’ remains one of the world’s most unreported and underfunded, currently at its lowest level in 6 years [13, 14].
Fig. 1.
Estimated number of Internally Displaced People in the Central African Republic between December 2008 and September 2023.11
Conflict, food insecurity and malnutrition
There is a growing body of evidence for a significant, negative association between conflict and child health [15]. During conflict-affected crises, many factors can increase food insecurity. Civilians’ access to agricultural fields and market places can be severely impeded as they are often targeted and forced to flee their homes, preventing timely planting or harvesting of crops; in the 2020–2021 farming season, for example, an estimated 30% or more of farmers in the Ouham and Ouham Pendé prefectures were unable to farm [16, 17]. Throughout the period of data collection for this analysis, there have been repeated reports of market closure, disrupted trade corridors and consequently increased prices of staple foods [18]. Furthermore, armed groups routinely loot homes, food stocks, livestock, local shops and warehouses; access to immediately needed food supplies is consequently severely depleted, leading to a complete loss of food security and thus poor nutrition or malnutrition amongst affected communities [19]. Both these aspects of such crises increase the dependency of displaced communities on foraging or food aid supply lines.
Limitations of nutritional surveys in conflict settings
Good nutrition is essential for the healthy development of children, yet the 2021 Global Nutrition report highlights that child malnutrition levels remain unacceptably high globally and few countries will meet the 2025 maternal, infant and young children nutrition targets [20]. Over a quarter of children worldwide are estimated to be suffering from undernutrition: around 22% of children worldwide are stunted (149.2 million) and 6.7% wasted (45.4 million) [21]. The report notes that ‘data for 194 countries shows substantial variation in terms of data availability, quality’ [21]. For CAR, nutritional data are taken from inter-agency Standardized Monitoring and Assessment of Relief and Transition (SMART) surveys and UNICEF Multiple Indicator Cluster Surveys (MICS), the most recent conducted in September–December 2019 and 2018–2019, respectively [22–24]. These are important and useful at a global level, but do not take into account populations living in hard-to-reach areas, enclaves, or having to hide in the bush due to chronic periodic conflict [25]. The 2018 MICS survey protocol for CAR clearly states that inaccessible areas would be excluded [26]. Indeed, the MICS 2018–2019 final report specified that 18% (99/550) of enumeration areas were not assessed due to inaccessibility or insecurity [24]. The unassessed sites included important rural and urban areas, 19% and 17% respectively, in Ouham and Ouham Pendé prefectures [24].
A survey conducted in Ouaka prefecture in 2020 found higher mortality rates (under-five mortality rate 1.87 [95% CI: 1.37–2.54] deaths/10,000 persons/day) than those previously estimated, raising concern that CAR may potentially have one of the highest mortality rates in the world [27]. Between 2015 and 2020, malaria prevalence in CAR increased from 68.9% to 74.71% and was reported to be the most common cause of death, followed by violence in 2020 [28]. A survey in Ouham prefecture reported a much higher birth rate than previously estimated [29]. These two surveys further highlight the need for good health indicator data in conflict-affected settings in order to improve United Nations’ modelling validity upon which policy and spending is based and prioritise funding to people most in need of assistance.
The MENTOR initiative and community health worker network
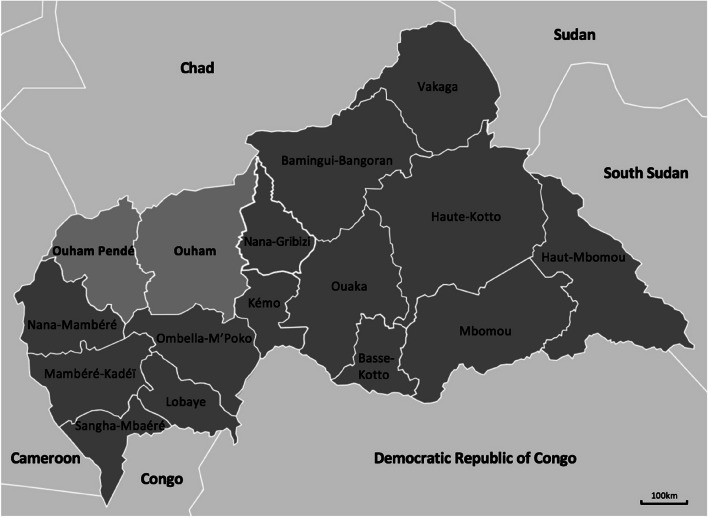
In 2008, The MENTOR Initiative, an international non-governmental organisation, established the country’s first network of community health workers (CHWs) in north-west CAR to reach isolated and conflict displaced communities [30, 31]. This network was initially based in the subprefecture of Paoua in Ouham Pendé prefecture and from 2011, also in Markounda in Ouham prefecture [31]. It was expanded in 2015 to cover six more subprefectures in north-west CAR: Bocaranga, Koui and Ngaoundaye (Ouham Pendé prefecture) and Batangafo, Nana-Bakassa and Nangha Boguila (Ouham prefecture) (Fig. 2). Population density is higher than average in these two prefectures (14.7 vs 8.8 people /km2 on average for CAR), with a high proportion of IDP, but few functioning healthcare facilities [12, 32]. Households surveyed in March–April 2020 in the Ouaka prefecture, where conditions are likely to be similar to those in Ouham and Ouham Pendé, reported facing many problems including, difficulties in accessing healthcare and fields due to insecurity and conflict, roadblocks, thefts and lootings, houses burnt down, food insecurity [27].
Fig. 2.
Map of the Central African Republic and its prefectures
The CHWs trained and supervised by The MENTOR Initiative deliver basic healthcare, including malaria diagnosis and treatment of children under 5 years old, and nutritional status assessment of children aged 6–59 months [31]. The CHWs are recruited from amongst the communities they will serve. Equipped with a bicycle and a kit consisting of essential diagnostic and case management materials, a MUAC tape and a patient record book, they hold clinics under trees or in community structures, giving populations in remote and insecure areas better access to malaria diagnosis and treatment (Fig. 3). All CHW services are provided free of charge, to ensure that cost is not a barrier to access.
Fig. 3.

MENTOR Community Health Workers in N.W. Central African Republic, 2012
This also enables access to healthcare to continue if a community is displaced, as the CHW remains with them and is reequipped by the MENTOR Initiative in the location they are displaced to [31]. Nutritional status is assessed using mid-upper arm circumference (MUAC) measurement which identifies children with moderate acute malnutrition (MAM) and severe acute malnutrition (SAM) [31]. Scales and height measuring boards, whilst used standardly in the few functioning health facilities in the area, are too large for CHWs to carry from village to village. The MUAC tape is a simple, portable tool, ideal for use in settings in which CHWs work, with evidence suggesting MUAC is better at identifying children at risk of dying from malnutrition than the weight-for-height Z-score [33–35]. CHWs routinely collect data for each patient seen, including malaria test results and nutritional status; this has resulted in a unique dataset consisting of medical data for 478,276 consultations of children under 5 years old between October 2015 and August 2021, during which period this region of CAR experienced varying levels of conflict in different locations. Young children are usually the first to suffer when food is scarce and the most severely affected if they are undernourished, leading to both short-term and long-term consequences (e.g. lasting cognitive impairment) and increased risk of mortality [36, 37]. Lack of good nutrition compromises the development and function of the immune system in children; gut barrier function is impaired, increasing susceptibility to infection and affecting its absorptive capacity [38, 39]. Children living in rural settings are at higher risk of infection from multiple communicable diseases, though malaria is the overwhelming cause of most health treatment seeking in this highly endemic area. Patients are normally treated by relatively unskilled primary health care workers, licensed only to provide orally administered drug therapy [40, 41]. Consequently, children who are malnourished and infected with a communicable disease such as malaria may deteriorate very quickly unless they can reach effective health care services which are able to administer more effective rectal or intravenous/intramuscular therapies [42, 43]. Travelling to health facilities in insecure areas, such as north-west CAR, can be dangerous or very challenging, potentially leading to higher death rates amongst malnourished children [44].
The c.
ontinuing conflict in CAR since 2008 is sporadic in time and location. It results in changes in levels of population isolation and their access to fields and other food supplies. Levels of nutritional vulnerability are consequently likely to increase and negatively impact nutritional status. We hypothesised that an increased incidence of global acute malnutrition will be associated with periods of increased conflict. In addition, there are likely to be associations amongst nutritional status, geographical location, seasonality and malaria incidence. The aims of this analysis are to assess the nutritional status of children aged 6–59 months who were seen by CHWs across eight subprefectures of CAR between October 2015 and August 2021 and to explore associations between nutritional status and malaria, seasonality and conflict.
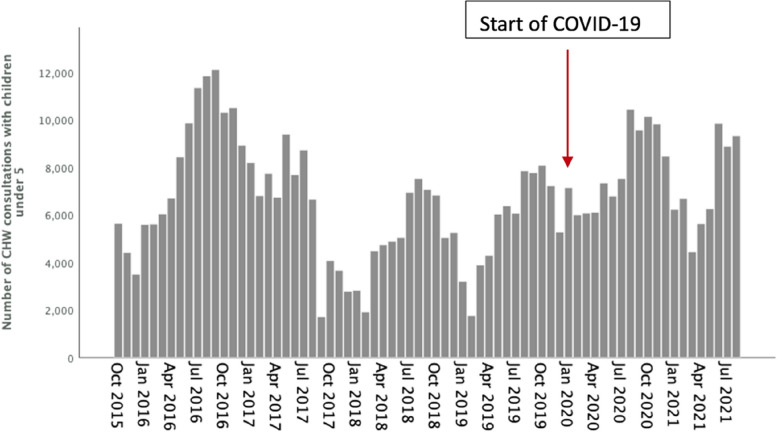
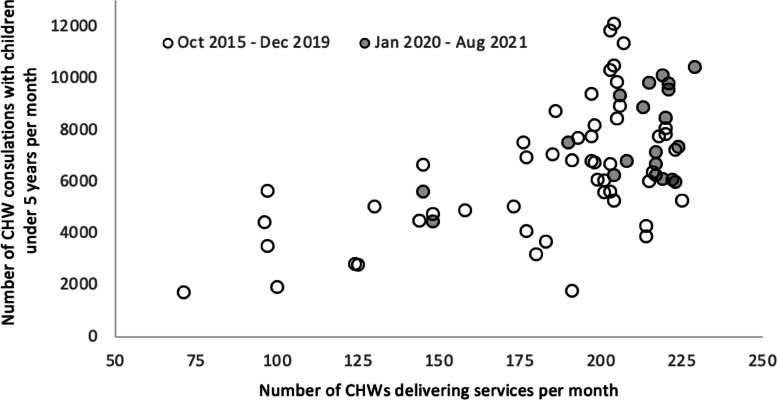
The period analysed extended into the global COVID-19 pandemic. Whilst this caused logistical challenges for international supply chains and potentially reduced access to some static health facilities, CHW services to communities were sustained and enhanced (Fig. 4) as part of the overall pandemic response in CAR, and levels of access and consultation did not suffer negatively (Fig. 5).
Fig. 4.
Number of CHW consultations with children under 5 years old between October 2015 and August 2021 across the eight subprefectures
Fig. 5.
Number of CHWs delivering services per month against the number of CHW consultations with children under 5 years old per month across the eight subprefecture pre-COVID-19 (October 2015–December 2019) and during COVID-19 (January 2020–August 2021). August 2021 across the eight subprefectures
The results provide a unique insight into the associations that could help identify communities most at risk of malnutrition and inform response planning. Limited resources are available to governments and humanitarian organisations seeking to assist communities affected by long-term chronic emergency settings, such as CAR, making allocation and planning decisions difficult. Given that humanitarian crises around the world are facing similar settings, this analysis contributes to an evidence base from which people responding to such crises can draw to help inform operational planning and resource allocation decisions that will directly affect the lives of people in humanitarian crises.
Methods
Data collection
The MENTOR Initiative trained CHWs to deliver basic health care across the eight subprefectures in north-west CAR. The CHWs routinely recorded each patient visit that took place between October 2015 and August 2021. Data collected included an assessment of the nutritional status of children aged 6–59 months using the MUAC measurement which classified them into three categories: well-nourished—green MUAC; moderate acute malnutrition (MAM)—yellow MUAC; severe acute malnutrition (SAM)—red MUAC. The results of malaria rapid diagnostic tests (RDT, First Response® Malaria Antigen P. falciparum (HRP2) Card Test) undertaken on children presenting to CHWs with clinical symptoms and test results were collected [45]; positive cases were recorded as severe or uncomplicated malaria depending on symptoms. Uncomplicated malaria symptoms include fever, sweats, chills, headaches, nausea and vomiting whereas severe malaria symptoms can include unconsciousness/coma, inability to walk/sit up unaided, convulsions, and failure to feed [46]. CHWs’ monthly records were collected during monthly supervisions and entered into an Excel database (one entry per village per month) for analysis and reporting.
Data used in this analysis were collected for children seeking treatment from CHWs. Data containing the records for all children under 5 years old seen by a CHW during the entire study period were cleaned and checked for data entry errors. Data consisted of 290 monthly reporting records from 97 villages across Batangafo, Markounda and Paoua between October 2015 and December 2015 and 13,139 monthly reporting records from 348 villages across the eight subprefectures between January 2016 and August 2021 of which 13,012 contained data for children aged 6–59 months. Data was anonymised for security reasons and as count data representing individual consultations, it is likely that some children may have presented for CHW consultations more than once within each year. The following were computed for each recorded entry: counts of global acute malnutrition (GAM—sum of counts of yellow and red MUAC); malaria test positivity rate (number of children under 5 years old with a positive RDT as a percentage of the total number of children under 5 years old); case rate of uncomplicated and severe malaria (number of uncomplicated or severe malaria cases as a percentage of the total number of children under 5 years old). The subprefectures were coded one to eight according to alphabetical order, starting with Batangafo, which thus became the reference subprefecture for the analysis.
Monthly rainfall data (2015–2020) for Ouham and Ouham Pendé prefectures were obtained from The World Bank Group [47]. Data collection methods were dependent upon the geographic siting of permanent weather recording stations in CAR. Access to those stations sited in NW CAR was not possible during the most insecure periods. Rainfall data for 2021 were therefore unavailable; data for 2020 were substituted for this time period. Months with rainfall over 200 mm (July to September) were coded 1 for the rainy season, the remaining months were coded 0.
Conflict data were obtained from the Armed Conflict Location & Event Data Project (ACLED) [48]. ACLED collects real-time data in more than 240 countries where political violence and protest events are recorded, including data on time, locations, actors and type of event. ACLED’s database was searched for all events involving all actors in CAR between October 2015 and August 2021. ACLED records conflict events according to six different types: violence against civilians, strategic development, battles, explosions/remote violence, riots and protests. Events were entered into the database according to event type, location and date [49].
Data analysis
Descriptive statistics were determined for all variables by indicator and subprefecture. The outcome variable, counts of GAM, was not normally distributed; non-parametric tests were therefore performed.
Manual backward stepwise negative binomial regression was performed for GAM for all entries between October 2015 and August 2021 to investigate associations between GAM and rainfall, geography, time, malaria and conflict. Initially, a full model was run with all potential covariates. New models were run, removing variables one by one, if they were not statistically significant (p > 0.05), until only variables that were statistically significant remained in the reduced model or the model with the lowest fit statistics was obtained. An offset variable (the natural log of the total number of children under 5 year olds) was included in the model to take into account children who were seen more than once by a CHW during the collection period. A total of 3.1% of entries had no data as a result of minor variations in CHW numbers during the period. These were excluded from the analysis. All data were entered and analysed using SPSS 29.01.0 [50].
Results
Study population
Trained CHWs conducted a total of 478,276 consultations across the eight subprefectures for children under 5 years old (of whom 48.5% were female) between October 2015 and August 2021 (Table 1).
Table 1.
Summary of the number of consultations for children < 5 years by subprefecture between October 2015 and August 2021
| Subprefecture | Total < 5 years | Total males | Number of CHW monthly reporting records |
|---|---|---|---|
| Batangafo | 52,735 | 26,860 (50.9%) | 1132 |
| Bocaranga | 36,945 | 19,418 (52.6%) | 1492 |
| Koui | 20,269 | 10,627 (52.4%) | 1107 |
| Markounda | 43,190 | 21,768 (50.4%) | 1419 |
| Nana-Bakassa | 39,269 | 20,633 (52.5%) | 1189 |
| Nangha Boguila | 49,466 | 25,257 (51.1%) | 1181 |
| Ngaoundaye | 38,484 | 19,667 (51.1%) | 1625 |
| Paoua | 197,918 | 101,860 (51.5%) | 3867 |
| Total | 478,276 | 246,080 (51.5%) | 13,012 |
Nutritional status
Of the 478,276 consultations, CHWs, following a standardised screening protocol, conducted an assessment of the nutritional status of 457,327 children (6–59 months old) consultations using MUAC. The majority of children (93.4%) were classified as well-nourished; however, 28,345 children (6.2%) and 1626 children (0.4%) were classified as moderately and severely malnourished, respectively (Table 2).
Table 2.
Summary of mid-upper arm circumference results for children aged 6–59 months by subprefecture between October 2015 and August 2021
| Subprefecture | Total measured |
Well-nourished (> 125 mm) |
Moderate acute Malnutrition (115–125 mm) |
Severe acute Malnutrition (< 115 mm) |
Number of CHW monthly reporting records with MUAC data |
|---|---|---|---|---|---|
| Batangafo | 49,658 | 47,254 (95.1%) | 2221 (4.5%) | 183 (0.4%) | 1126 |
| Bocaranga | 36,109 | 33,567 (93.0%) | 2425 (6.7%) | 117 (0.3%) | 1482 |
| Koui | 19,927 | 18,891 (94.8%) | 1005 (5.0%) | 31 (0.2%) | 1101 |
| Markounda | 41,410 | 38,680 (93.4%) | 2619 (6.3%) | 111 (0.3%) | 1399 |
| Nana-Bakassa | 34,993 | 31,664 (90.5%) | 3016 (8.6%) | 313 (0.9%) | 1183 |
| Nangha Boguila | 44,864 | 41,271 (92.0%) | 3434 (7.6%) | 159 (0.4%) | 1172 |
| Ngaoundaye | 37,216 | 34,759 (93.4%) | 2260 (6.1%) | 197 (0.5%) | 1612 |
| Paoua | 193,150 | 181,270 (93.8%) | 11,365 (5.9%) | 515 (0.3%) | 3841 |
| Total | 457,327 | 427,356 (93.4%) | 28,345 (6.2%) | 1626 (0.4%) | 12,916 |
Malaria burden
Of the 478,276 consultations, CHWs with a total of 466,897 RDTs for detecting P. falciparum were performed on children under 5 years old during the study period. The overall malaria test positivity rate was 91.3% (426,179/466,897); 1% (4283) of malaria-positive cases had symptoms of severe malaria (Table 3).
Table 3.
Summary of malaria rapid diagnostic test results for children < 5 years by subprefecture between October 2015 and August 2021
| Subprefecture | Total RDT performed | Total RDT positive | Total RDT negative | Uncomplicated malaria | Severe malaria | Number of CHW monthly reporting records with RDT data |
|---|---|---|---|---|---|---|
| Batangafo | 50,425 | 46,675 (92.6%) | 3750 (7.4%) | 46,260 (99.1%) | 415 (0.9%) | 1132 |
| Bocaranga | 36,796 | 34,189 (92.9%) | 2646 (7.1%) | 34,034 (99.5%) | 155 (0.5%) | 1492 |
| Koui | 20,198 | 18,480 (91.4%) | 1742 (8,6%) | 18,316 (99.1%) | 164 (0.9%) | 1107 |
| Markounda | 43,061 | 38,707 (89.9%) | 4354 (10.1%) | 38,203 (98.7%) | 505 (1.3%) | 1419 |
| Nana-Bakassa | 35,528 | 32,473 (91.4%) | 3055 (8.6%) | 32,011 (98.6%) | 462 (1.4%) | 1189 |
| Nangha Boguila | 45,578 | 41,547 (91.1%) | 4031 (8.9%) | 40,896 (98.5%) | 620 (1.5%) | 1181 |
| Ngaoundaye | 38,184 | 35,537 (93.1%) | 2647 (6.9%) | 34,823 (98%) | 714 (2.0%) | 1625 |
| Paoua | 197,127 | 178,571 (90.6%) | 18,600 (9.4%) | 177,100 (99.3%) | 1248 (0.7%) | 3867 |
| Total | 466,897 | 426,179 (91.3%) | 40,825 (0.7%) | 421,643 (99%) | 4283 (1%) | 13,012 |
Conflict data
ACLED recorded a total of 432 events between October 2015 and August 2021 across the eight subprefectures (Table 4).
Table 4.
Summary of conflict data by subprefecture and event type between October 2015 and August 2021
| Conflict event type | |||||||
|---|---|---|---|---|---|---|---|
| Subprefecture | Violence against civilians | Battles | Strategic development | Riots | Protests | Explosions/remote violence | Total (%) |
| Batangafo | 42 | 28 | 19 | 2 | 2 | 1 | 94 (21.7) |
| Bocaranga | 26 | 22 | 14 | 1 | 0 | 1 | 64 (14.8) |
| Koui | 15 | 17 | 7 | 0 | 0 | 3 | 42 (9.7) |
| Markounda | 10 | 5 | 4 | 0 | 0 | 0 | 19 (4.4) |
| Nana-Bakassa | 7 | 2 | 3 | 0 | 0 | 0 | 12 (2.8) |
| Nangha Boguila | 1 | 4 | 3 | 0 | 0 | 0 | 8 (1.9) |
| Ngaoundaye | 22 | 15 | 21 | 2 | 0 | 3 | 63 (14.6) |
| Paoua | 61 | 34 | 28 | 6 | 1 | 0 | 130 (30.1) |
| Total (%) | 184 (42.6) | 127 (29.4) | 99 (22.9) | 11 (2.5) | 3 (0.7) | 8 (1.9) | 432 |
Interlinked associations between malaria, rainfall and GAM
Global acute malnutrition regression models
We conducted negative binomial regression analysis for counts of global acute malnutrition (GAM) (n = 12,916), including all yellow and red MUAC. The model with the best fit included the following variables: subprefecture, rainfall, conflict, case rate of uncomplicated malaria and case rate of severe malaria (Additional file 1: Table S1).
Change in GAM by subprefecture, season, conflict and rates of malaria
The final model demonstrated an association between counts of GAM and subprefecture, rainy season and year (Table 5). While holding all other variables constant, compared to Batangafo, counts of GAM were 54% higher in Bocaranga, 22% higher in Koui, 43% higher in Markounda, 107% higher in Nana-Bakassa, 68% higher in Nangha Boguila, 40% higher in Ngaoundaye and 32% higher in Paoua (Table 5).
Table 5.
Summary of the negative binomial regression model for counts of GAM (n = 12,916)
| Variable | IRR (95% CI) | p value |
|---|---|---|
| Subprefecture | ||
| Paoua | 1.32 (1.19–1.48) | < 0.001 |
| Ngaoundaye | 1.40 (1.23–1.59) | < 0.001 |
| Nangha Boguila | 1.68 (1.47–1.92) | < 0.001 |
| Nana-Bakassa | 2.07 (1.81–2.37) | < 0.001 |
| Markounda | 1.43 (1.25–1.63) | < 0.001 |
| Koui | 1.22 (1.05–1.41) | 0.008 |
| Bocaranga | 1.55 (1.36–1.77) | < 0.001 |
| Batangafo | 1 | |
| Rainfall | ||
| Rainy season (Jul-Sep) | 1.10 (1.03–1.18) | 0.004 |
| Dry season (Oct-Jun) | 1 | |
| Conflict | ||
| Violence against civilians | 0.92 (0.77–1.10) | 0.36 |
| Battles | 0.78 (0.62–0.97) | 0.029 |
| Strategic development | 0.85 (0.68–1.06) | 0.14 |
| Riots | 0.55 (0.28–1.09) | 0.088 |
| Malaria | ||
| Case rate of uncomplicated malaria | 1.007 (1.005–1.01) | < 0.001 |
| Case rate of severe malaria | 1.045 (1.04–1.06) | < 0.001 |
| χ2 (14) = 279.13, p < 0.001 | ||
IRR incidence rate ratio, CI confidence intervals
While holding all other variables constant, counts of GAM were 10% higher in the rainy season (July to September) (Table 5).
The final model demonstrated a negative association between counts of GAM and battles, 22% lower compared to no conflict (Table 5).
The final model demonstrated a positive association between GAM and both the case rate of uncomplicated malaria and the case rate of severe malaria, with an increase in counts of GAM of 0.7% and 4.5% for every one unit increase in the case rate of uncomplicated malaria and the case rate of severe malaria, respectively, while holding all other variables constant (Table 5).
IRR, incidence rate ratio; CI, confidence intervals.
Discussion
The aims of this analysis were to assess levels of malnutrition in children aged 6–59 months living in eight subprefectures of north-west CAR between October 2015 and August 2021 and to explore the association with geography, season, incidence of malaria and conflict. The dataset analysed is truly unique, having been collected in some of CAR’s least accessible and, at times, most insecure subprefectures. There are no other data available on such a large scale, either for CAR or for other similar, malaria-endemic, conflict-affected countries.
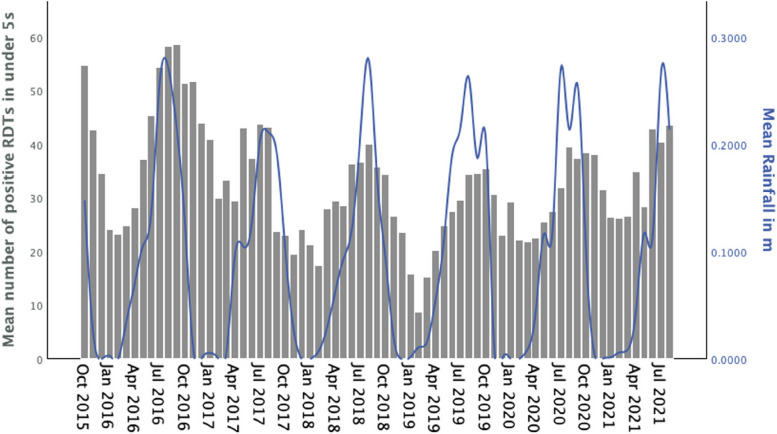
Association between malaria and seasonality
Malaria transmission patterns across Africa are markedly heterogenic. However, rainfall seasonality has been significantly associated with malaria transmission in equatorial African locations, including Bangui, the capital city of CAR, where two rainy seasons each year reinforced transmission [51, 52]. Other climatic and environmental factors such as temperature, whilst also being important are lower-level determinants of transmission [51, 52]. This analysis of malaria count data and rainfall across remote rural sub-prefectures in northwest CAR confirms that malaria transmission is strongly associated with rainfall (Fig. 6).
Fig. 6.
Confirmed malaria cases vs rainfall between October 2015 and August 2021 across the eight subprefectures
Associations between nutritional status and geography
There is evidence for an association between subprefecture and nutritional status in the GAM regression model, with differences in counts of GAM ranging from 23% (Koui) to 110% (Nana-Bakassa) more when compared to Batangafo. Geographical differences in levels of GAM are likely to be partly explained by differences in levels of rural vs urban population and accessibility to food, with many communities living in very remote conditions, far from supply roads. The population of Nana-Bakassa subprefecture is 100% rural, with the nearest market 64 km away, whereas Batangafo subprefecture is around 72% rural and Batangafo town has three markets. Another important difference between rural and urban populations is access to clean (or safe) drinking water and its decline since 2000 [53, 54]. Access to at least basic drinking water amongst rural populations has fallen from 44% in 2000 to 28% in 2020, and from 83 to 50% amongst the urban population [53, 54]. Lack of basic drinking water is accompanied by lack of basic sanitation: in 2020, 12.4% of the rural population had access to basic or safely managed sanitation compared to 25.3% of the urban population; 38% of the rural population was practising open defecation in 2020 compared to 6.7% of the urban population [55]. Lack of basic drinking water, together with poor sanitation and hygiene exposes children to multiple faecal pathogens. These include important and treatable parasitic or viral diseases, but faecal pathogens may also result in asymptomatic environmental enteropathy [56]. Characterised by blunted microvilli and inflammation in the small intestine, altered gut permeability and microbiota, environmental enteropathy leads to reduced absorptive capacity for drugs and nutrients, and micronutrient deficiencies and is thought to be a causal factor in malnutrition and stunting [57, 58].
Associations between seasonality and nutritional status
There is evidence for an association between seasonality and nutritional status, with cases of GAM around 10% higher in the months with the highest rainfall (over 200 mm/month in July–September), compared to the rest of the year. This seasonal variation in levels of GAM is unsurprising: the “lean season” occurs in developing countries during the rainy season, coinciding with the time period sowing and harvesting crops, when food supplies have become low and the population has to rely on hunter-gatherer food supplies such as game, tadpoles, fish, caterpillars, forest wild fruit and vegetable (e.g. palm shoots) [59]. In northern CAR, crops are harvested between August and October, therefore an increase in the number of children with GAM is not unexpected [60]. In addition, during the rainy season, dirt roads become unusable in CAR, limiting remote communities’ ability to access markets both to sell produce and buy better food supplies [61, 62].
Associations between conflict and nutritional status
There is growing evidence of the negative impact of conflict on child nutritional status [15]; this analysis provides evidence that levels of malnutrition amongst children ages 6–59 months are likely to be underestimated in areas afflicted by conflict, particularly during events coded as battles.
There are several possible explanations for this, all of which could result in fewer cases of MAM or SAM either being seen or recorded by CHWs. The method of data collection itself could be disrupted in times of conflict since it relies on paper records of data being collected from secure locations each month, with the risk of it potentially being lost, particularly if incidents of conflict have resulted in displacement. CHWs cannot always be resupplied with materials and medications, programmes have to be paused temporarily for security reasons, or CHWs may not be able to reach their villages due to insecurity. Mothers/carers may be too afraid to venture outside to consult with a CHW during times of insecurity, with the risk of rape for women who leave the safety of their villages, camps or forest hiding places a real threat which further reduces the incentive to seek treatment for all but the worst health conditions [63]; children with MAM may be considered to be part of everyday life in this war-torn population, particularly as CHWs would not have any ‘treatment’ for MAM, only advice on how to improve diet [27]. Families who flee to the bush when their villages are attacked may remain in hiding for extended periods, with little food other than what they can forage for; consequently, children are likely to become malnourished, and those already suffering from MAM, more likely to deteriorate to SAM and possibly die before they can reach help [25].
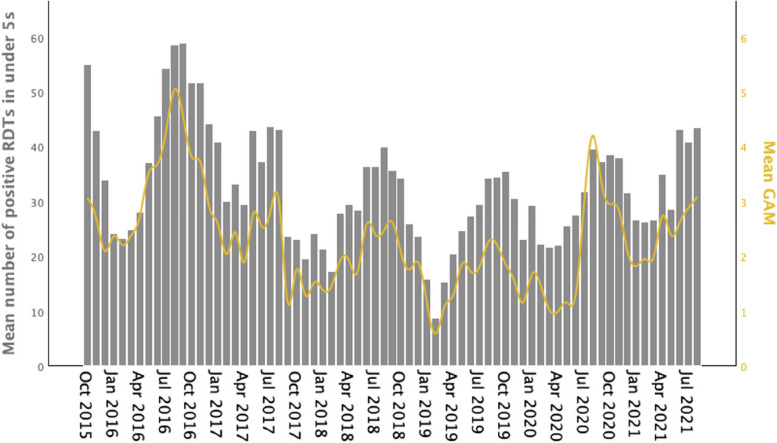
Associations between malaria infection and nutritional status
Sick children presenting to CHWs in this region have very high positivity rates for malaria, a finding consistent with previous studies [31, 52]. Confirmed malaria and GAM case counts were both highly seasonal, their patterns closely mirroring each other and rainfall seasonality (Figs. 6 and 7). The greater increase in cases of GAM with increasing levels of severe malaria (4.5%) compared to uncomplicated malaria (0.7%) is consistent with evidence that GAM impairs the immune system, weakening its ability to fight infection and thus making it more likely that uncomplicated malaria will progress to severe malaria. The immune system is a highly regulated, complex system of specialised cells and mediators which protect against external pathogens [38]. Good nutrition, including key vitamins and minerals, is essential to support the high energy demands and complexity of the immune system, particularly for optimal immunocompetence during infections, yet deficiencies of micronutrients key for immune function (e.g. vitamin A, zinc, iron) are common in low-income countries, linked to lack of dietary diversity as well as food insecurity [19, 58]. In turn, nutritional status is likely to be affected by the presence of infection, due to the interrelationship between malnutrition and immunity, either through reduced food intake, nutrient losses (e.g. diarrhoeal diseases), coupled with the increased energy demands imposed by an immune system trying to combat infection [39]. In addition, recovery from uncomplicated malaria following treatment is likely to be compromised in children with malnutrition, particularly if this is associated with environmental enteropathy; these children will have reduced absorptive capacity for drugs, decreasing the effectiveness of orally administered drugs, such as those routinely used by CHWs to treat uncomplicated malaria (artemisinin combination therapies) [64]. Consequently, treatment failure may ensue, increasing the likelihood that children with acute malnutrition will fail to clear the infection and return days later, but with worse symptoms or severe malaria [65]. Children suffering from SAM who become infected with malaria may deteriorate faster from uncomplicated to severe malaria than children suffering from MAM as SAM is associated with a severely compromised immune system [39, 66]. Children under 5 years old who develop severe malaria can die within hours, often en route to a CHW; cases of children with SAM and severe malaria may not ever be seen and therefore recorded by CHWs [27, 66].
Fig. 7.
Confirmed malaria cases vs mean GAM between October 2015 and August 2021 across the eight subprefectures
Implications of the findings
This analysis indicates that the likelihood that children aged 6–59 months suffer from GAM varies depending on where they live in north-west CAR, the degree of malaria transmission and rainfall seasonality. This is an important finding which may be missed by SMART and MICS surveys as these often do not access the more remote, conflict-affected populations. Targeted nutritional services are clearly needed to reach those in geographical areas with the highest burden and risk of GAM. In addition, it is evident that without nutritional surveys that include data from communities that are in more insecure or remote locations, communities that are most at risk of malnutrition will not always be identified.
Figures 4 and 5, when viewed together with Table 4 demonstrate the essential role of CHWs in accessing and sustaining service delivery to communities living in conflict-affected areas of CAR, without which would not be reached with essential services. CHWs have a unique ability to deliver essential primary health services to their communities, even when they are displaced. More sick children are likely to have accessed and received health care from CHWs, than would have been the case had these children been reliant on static health facilities, particularly in times of conflict. With their unique access to remote communities, it may be feasible to use CHW networks to treat cases of MAM and uncomplicated cases of SAM in their communities, particularly if conflict or distance to health care facilities is a barrier to children with SAM obtaining treatment. There is some evidence that treating uncomplicated SAM cases in the community may significantly improve nutritional recovery rates compared to treatment at inpatient facilities, in part through the improvement in early detection and treatment [67, 68].
Integration of basic nutritional surveillance and treatment services, together with bringing diagnosis and case management of malaria and other diseases to the community level in emergency settings through trained CHWs, will help save more lives; it will also inform those responsible for coordinating and delivering aid, how better to rationalise and improve targeting and increase the impact of international aid funding. At a time when international aid budgets are under great stress and numbers in need of humanitarian assistance are at record levels, never has the need to maximise the efficiency of humanitarian responses been greater.
Wider implications
This analysis reinforces understanding of the impressive geographical reach achievable by CHWs trained to deliver essential primary health care services even to the most inaccessible communities [31]. It demonstrates the ability of such community-level services to extend the scope of basic disease and nutritional surveillance [31]. This study sheds new light on the important interplay between malnutrition and malaria, the most common cause of suffering and death in this and many other similar malaria-endemic settings host to armed conflicts, natural disasters and large displaced populations. The responsibility for co-ordination and funding of resources for addressing malnutrition and malaria in such settings are siloed, as a consequence of the international Cluster mechanism, established in 2005 [69]. Inevitably, this has led to the creation of specialised aid organisations with different operational capacities, particularly for insecure settings. Whilst usually delivering good quality vertical services to some communities, they often do so in a siloed manner, due to the lack of cross-sector co-ordination mechanisms at country level. The overwhelming need to plan and deliver emergency humanitarian malnutrition and malaria control services together has been largely unrecognised, or worse, ignored.
The hardest-to-reach communities usually have the poorest access to essential services and are often those most at risk of attack from multiple armed groups. Consequently, they are subject to the deadly combination of attacks, looting, forced displacement and increased exposure to malaria vectors when living rough. Furthermore, particularly when displaced, access to food and clean water may be severely limited. Few aid agencies have the operational capacity or cross-sectoral skill set to serve such communities on their own, with co-ordination and funding siloes creating hurdles not foreseen in 2005. CHWs have, to date, been an underutilised delivery mechanism in most humanitarian crises, often overlooked, perceived as suited only to developmental contexts and requiring multi-year funding commitment. Their proven and long-established capacity to serve people others cannot reach in insecure areas of CAR is a model that could well serve similar humanitarian crises across Africa and other parts of the world [31].
Limitations
The nutritional and malaria data used in this retrospective analysis were collected for children seeking treatment from CHWs, rather than for children selected randomly as part of a survey. CHW activity and scale varied over the study period. These variations have been accounted for in teh study analysis. However, this still remains a large and unique dataset. The number of counts of SAM was too low to allow for MAM and SAM data to be analysed separately, however, it is hypothesised that associations between SAM and severe malaria would be greater than those between MAM and severe malaria. Although all conflict events recorded by ACLED during the collection period were used in the regression analysis, some events may be missing; further research which examines data from other conflict databases may therefore be beneficial [15, 70]. It is likely that some conflict events that may have an impact on child nutritional status are not recorded in any databases, particularly when these occur in remote locations, such as many of the villages in which CHWs work [27]. Furthermore, it is difficult to capture the intensity of events in the analysis. For example, “365 homes [were] looted/burned as suspected former Seleka militiamen attacked Bowai village” is recorded as one event in the ACLED database [48]. Such events are likely to have a lasting impact on populations, causing displacement which puts children at higher risk of malnutrition. People remain hidden for long periods to avoid being raped or shot, returning to their villages and fields only when certain that the armed groups have left. This is likely to happen on a regular, cyclical basis as armed groups revolve around the areas they control, leading to regular population displacement for weeks at a time, rather than long-term displacement into formal camp settings. This type of regular displacement is unique to north-west CAR and is very difficult to record. The potential impact on the nutritional status of such conflict-induced displacements in this area is therefore difficult to assess without more detailed recording of events including timing, location, event duration and displacement numbers. Collection of a wider number of household variables, such as educational status, income levels, diet, food security, access to clean water and hygiene practices, maternal age, maternal nutritional status, family size, displacement status, and data on other morbidities, coupled with birth weight, season of birth, weight and hight measurements of children for assessment of chronic malnutrition, in addition to MUAC for assessment of acute malnutrition, combined with the other key factors measured in this analysis, would allow a more detailed analysis and improved understanding of the factors associated with chronic and acute malnutrition in this context [71–74].
Conclusions
This analysis demonstrates that there are real differences in malnutrition levels across eight subprefectures in north-west CAR. Ongoing conflict makes it difficult to access populations living in these subprefectures, particularly their rural communities. SMART and MICS nutritional surveys do not reach these communities and therefore cannot assess the differences in malnutrition levels in the very areas where this analysis has shown these may be highest. This analysis provides invaluable insight into the need for nutritional support funding to be geographically targeted to meet varying levels of support required, particularly given the current decreased funding for CAR [14]. Networks of CHWs, trained, suitably equipped, and supported for emergency contexts, offer real potential to integrate targeted nutritional support, together with essential diagnostic and treatment services for malaria and other life-threatening diseases, where most needed.
The nature of armed conflict has changed, creating long-term chronic humanitarian crises [75, 76]. The nature of the global humanitarian response must now change too, with organisations working together to ensure a more coordinated response to reach and protect those they have committed to serve.
Supplementary Information
Acknowledgements
We thank Issa Chitouissa for field support in this work and acknowledge the extraordinary dedication of the many MENTOR Initiative staff and community health workers delivering essential health and nutrition services in conflict-affected areas of the Central African Republic. We would also like to thank the Ministry of Health, and other humanitarian aid organisations working in partnership to meet the needs of the most vulnerable communities in hard-to-reach areas of the country.
Abbreviations
- ACLED
Armed Conflict Location & Event Data Project
- CAR
The Central African Republic
- CHW
Community health workers
- CI
Confidence interval
- GAM
Global acute malnutrition
- IDP
Internally displaced people
- IRR
Incidence rate ratio
- MAM
Moderate acute malnutrition
- MICS
Multiple Indicator Cluster Surveys
- MUAC
Mid-upper arm circumference
- RDT
Rapid diagnostic tests
- SAM
Severe acute malnutrition
- SMART
Standardized Monitoring and Assessment of Relief and Transition
- SPSS
Statistical Package for Social Sciences
Authors’ contributions
NS designed the study with RA and HL. NS undertook the analysis of study data with PW and RA. NS wrote the paper with assistance from RA, HL, PW, KE, EB, BAN, ML and PB. All authors read and approved the final manuscript.
Funding
This work was made possible through support provided by the UK government and by the Office of US Foreign Disaster Assistance, U.S. Agency for International Development. The opinions expressed herein are those of the author(s) and do not necessarily reflect the views of the UK government or the U.S. Agency for International Development.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
CHWs follow ethical practices and with agreement from the Ministry of Health in the CAR. Data were collected for all children under 5 years old who visited a CHW to receive diagnosis and treatment. CHWs obtained verbal consent from carers before examining or treating them and recording data. Ethical approval was obtained from the University of Surrey Ethics Committee [FHMS 21–22 161 EGA]. A data sharing agreement was set up prior to transfer of the data set.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Herbert S, Dukhan N, Debos M. State fragility in the Central African Republic: What prompted the 2013 coup? Rapid literature review. Birmingham, UK; GSDRC, University of Birmingham. 2013. https://gsdrc.org/publications/state-fragility-in-the-central-african-republic-what-prompted-the-2013-coup/. Accessed 20 Feb 2023.
- 2.BBC News. Raid on CAR town ‘leaves 20 dead’. http://news.bbc.co.uk/2/hi/africa/4035239.stm (2004). Accessed 10 Jul 2024.
- 3.Picco E. Ten Years After the Coup, Is the Central African Republic Facing Another Major Crisis? International Crisis Group. 2023. https://www.crisisgroup.org/africa/central-africa/central-african-republic/dix-ans-apres-le-coup-detat-la-republique#:~:text=In%20March%202013%2C%20Seleka%20rebels,face%20another%20violent%20power%20transfer. Accessed 14 June 2024.
- 4.United Nations Development Programme (UNDP). Fast Facts: Central African Republic. 2017. https://www.undp.org/publications/fast-facts-central-african-republic. Accessed 14 June 2024.
- 5.United Nations Development Programme (UNDP). Human Development Report 2021–2022: Uncertain Times, Unsettled Lives, Shaping our Future in a Transforming World. New York. 2022. https://hdr.undp.org/content/human-development-report-2021-22. Accessed 23 Sept 2023
- 6.The World Bank. The World Bank in Central African Republic. Overview. 2023. https://www.worldbank.org/en/country/centralafricanrepublic/overview. Accessed 13th
- 7.Internal Displacement Monitoring Centre (IDMC). Country Profile. Central African Republic. 2022. https://www.internal-displacement.org/countries/central-african-republic. Accessed 20 Feb 2023.
- 8.United Nations (UN). Central African Republic: 200,000 displaced in less than two months. 2021. https://news.un.org/en/story/2021/01/1083332. Accessed 20 Feb 2023.
- 9.Lamarche A. The Central African Republic in Crisis: Critical Measures to Address Security and Humanitarian Needs. 2021. https://www.refugeesinternational.org/reports/2021/2/3/the-central-african-republic-in-crisis-critical-measures-to-address-humanitarian-and-security-needs. Accessed 20 Feb 2022
- 10.UNICEF. Central African Republic: Nearly 370,000 children now internally displaced amidst ongoing violence – the highest number since 2014. 2021. https://www.unicef.org/press-releases/central-african-republic-nearly-370000-children-now-internally-displaced-amidst.Accessed 03 Feb 2023
- 11.Operational data portal. Central African Republic Regional Response. https://data2.unhcr.org/en/situations/car . Accessed 03 Nov 2023.
- 12.World Health Organization. HeRAMS République centrafricaine : rapport de référence 2023 – Status opérationel du système de santé. 2023. [HeRAMS Central African Republic baseline report 2023 – Operational status of health system]. https://www.who.int/publications/m/item/herams-central-african-republic-baseline-report-2023-operational-status-of-the-health-system. Accessed 03 Nov 2023.
- 13.United Nations Office for the Coordination of Humanitarian Affairs (OCHA). West and Central Africa. Central African Republic. https://www.unocha.org/central-african-republic#:~:text=In%202023%2C%203.4%20million%20people,cent%2C%20reaching%206.1%20million%20people. Accessed 03 Nov 2023.
- 14.Financial Tracking Service. UNOCHA. République Centrafricaine Plan de Réponse humanitaire 2023. https://fts.unocha.org/plans/1130/summary. Accessed 03 Nov 2023.
- 15.Sassi M, Thakare H. Conflict and Child Malnutrition: a Systematic Review of the Emerging Quantitative Literature. Curr Nutr Rep. 2022. 10.1007/s13668-021-00386-w. 10.1007/s13668-021-00386-w [DOI] [PubMed] [Google Scholar]
- 16.Surprenant A. Rebel blockade triggers aid and food shortages in Central African Republic. 2021. https://www.thenewhumanitarian.org/news-feature/2021/2/5/central-african-republic-rebel-blockade-food-shortages#:~:text=A%20weeks%2Dlong%20rebel%20blockade%20of%20the%20main%20trade%20route,are%20fleeing%20post%2Delectoral%20conflict (2021).Accessed 15 Jan 2023.
- 17.Famine Early Warning Systems Network (FEWS NET). Higher level of food insecurity affects households in the southeast despite current harvests. https://fews.net/west-africa/central-african-republic/remote-monitoring-report/october-2021 (2021). Accessed 20 Feb 2022.
- 18.The World Bank. Rise in food prices due to escalating conflict tips more people into poverty in the Central African Republic. 2021. https://www.worldbank.org/en/news/press-release/2021/01/16/rise-in-food-prices-due- to-escalating-conflict-tips-more-people-into-poverty-in-the-central-african-republic. Accessed 15 Jan 2023.
- 19.Famine Early Warning Systems Network (FEWS NET). Resurgence of armed conflicts worsens food insecurity for poor households at the start of the lean season.2022. https://fews.net/west-africa/central-african-republic/remote-monitoring-report/february-2022 Accessed 15 Jan 2023.
- 20.World Health Organization. Global Nutrition Targets 2025: to improve maternal, infant and young child. 2014. https://www.who.int/teams/nutrition-and-food-safety/global-targets-2025. Accessed 15 Jan 2023.
- 21.2021 Global Nutrition Report:The state of global nutrition. Bristol, UK: Development Initiatives. 2021. https://globalnutritionreport.org/documents/753/2021_Global_Nutrition_Report.pdf. Accessed 15 Jan 2023.
- 22.SMART. About SMART. https://smartmethodology.org/about-smart/. Accessed 15 Jan 2023.
- 23.UNICEF. MICS. https://mics.unicef.org. Accessed 15 Jan 2023.
- 24.ICASEES. MICS6-RCA ; Enquête par grappes à indicateurs multiples 2018–2019, Rapport final des résultats de l’enquête [MICS6-CAR; Multiple Indicator Cluster Survey 2018–2019, final report of survey results]. Bangui: INCASEES. 2021. https://mics-surveys-prod.s3.amazonaws.com/MICS6/West%20and%20Central%20Africa/Central%20African%20Republic/2018-2019/Survey%20findings/French.pdf. Accessed 15 Jan 2023.
- 25.Jepson, L. Families hide in bush after attacks on villages. 2013. https://reliefweb.int/report/central-african-republic/families-hide-bush-after-attacks-villages. Accessed 15 Jan 2023.
- 26.ICASEES. Enquête Nationale sur la Situation Nutritionnelle et la Mortalité en République Centrafricaine. Protocole d’enquête [National survey on the nutritional situation and mortality in Central African Republic. Survey protocol]. 2018. https://icasees.org/nada/index.php/catalog/54/download/297. Accessed 15 Jan 2023.
- 27.Robinson E, Lee L, Roberts LF, Poelhekke A, Charles X, Ouabo A, et al. Mortality beyond emergency threshold in a silent crisis– results from a population-based mortality survey in Ouaka prefecture, Central African Republic, 2020. Confl Health. 2021. 10.1186/s13031-021-00385-2. 10.1186/s13031-021-00385-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. World malaria report 2021. 2021. https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2021 Accessed 14 June 2024.
- 29.Wol P, Kay C, Roberts L. Surveys about attended births appear to be deceptive in CAR: are the population saying what they think NGO’s want to hear? Confl Health. 2021. 10.1186/s13031-021-00381-6. 10.1186/s13031-021-00381-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The MENTOR Initiative. https://mentor-initiative.org. Accessed 14 June 2024.
- 31.Ruckstuhl L, Lengeler C, Moyen JM, Garro H, Allan R. Malaria case management by community health workers in the Central African Republic from 2009–2014: Overcoming challenges of access and instability due to conflict. Malar J. 2017. 10.1186/s12936-017-2005-7. 10.1186/s12936-017-2005-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ICASEES. Population RCA par prefecture 2021 [CAR population by prefecture 2021]. https://icasees.org/index.php/prefectures/. Accessed 27 Nov 2023.
- 33.Bliss J, Lelijveld N, Briend A, Kerac M, Manary M, McGrath M, et al. Use of mid-upper arm circumference by novel community platforms to detect, diagnose, and treat severe acute malnutrition in children: A systematic review. Global Health Science and Practice. 2018. 10.9745/GHSP-D-18-00105. 10.9745/GHSP-D-18-00105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Briend A, Maire B, Fontaine O, Garenne M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-five children. Matern Child Nutr. 2012. 10.1111/j.1740-8709.2011.00340.x. 10.1111/j.1740-8709.2011.00340.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Briend A, Alvarez J-L, Avril N, et al. Low mid-upper arm circumference identifies children with a high risk of death who should be the priority target for treatment. BMC Nutr. 2016. 10.1186/s40795-016-0101-7. 10.1186/s40795-016-0101-7 [DOI] [Google Scholar]
- 36.De Sanctis V, Soliman A, Alaaraj N, Ahmed S, Alyafei F, Hamed N. Early and Long-term Consequences of Nutritional Stunting: From Childhood to Adulthood. Acta Biomed. 2021. 10.23750/abm.v92i1.11346. 10.23750/abm.v92i1.11346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McDonald CM, Olofin I, Flaxman S, et al. The effect of multiple anthropometric deficits on child mortality: meta-analysis of individual data in 10 prospective studies from developing countries. Am J Clin Nutr. 2013. 10.3945/ajcn.112.047639. 10.3945/ajcn.112.047639 [DOI] [PubMed] [Google Scholar]
- 38.Simon AK, Hollander GA, McMichael A. Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. 2015. 10.1098/rspb.2014.3085. 10.1098/rspb.2014.3085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calder PC, Jackson AA. Undernutrition, infection and immune function. Nutr Res Rev. 2000. 10.1079/095442200108728981. 10.1079/095442200108728981 [DOI] [PubMed] [Google Scholar]
- 40.Galactionova K, Tediosi F, de Savigny D, Smith T, Tanner M. Effective coverage and systems effectiveness for malaria case management in Sub-Saharan African countries. PLoS ONE. 2015. 10.1371/journal.pone.0127818. 10.1371/journal.pone.0127818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bennett A, Bisanzio D, Yukich JO, Mappin B, Fergus CA, Lynch M, et al. Population coverage of artemisinin-based combination treatment in children younger than 5 years with fever and Plasmodium falciparum infection in Africa, 2003–2015: a modelling study using data from national surveys. Lancet Glob Health. 2017;5(4):e418–27. 10.1016/S2214-109X(17)30076-1. 10.1016/S2214-109X(17)30076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.World Health Organization (WHO). WHO guidelines for malaria. 2023. https://iris.who.int/bitstream/handle/10665/373339/WHO-UCN-GMP-2023.01-Rev.1-eng.pdf?sequence=1. Accessed 17 Nov 2023
- 43.World Health Organization. The use of rectal artesunate as a pre-referral treatment for severe Plasmodium falciparum malaria. 2023. https://iris.who.int/bitstream/handle/10665/370352/9789240075375-eng.pdf?sequence=1. Accessed 27 Nov 2023.
- 44.Médecins Sans Frontières. Medical care at arm’s length: the continuous struggle of the people of Ouaka. 2020. https://www.msf.org/barriers-accessing-healthcare-ouaka-central-african-republic. Accessed 9 Nov 2023.
- 45.World Health Organization. WHO Prequalification of In Vitro Diagnostics Public Report. 2018. https://extranet.who.int/prequal/sites/default/files/whopr_files/PQDx_0285-010-00_FirstResponseMalaria_v1.pdfAccessed 14 June 2924.
- 46.Bartoloni A, Zammarchi L. Clinical aspects of uncomplicated and severe malaria. Mediterranean Journal of Hematology and Infectious Diseases. 2012. 10.4084/MJHID.2012.026. 10.4084/MJHID.2012.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.The World Bank. Climate change knowledge portal. 2021. https://climateknowledgeportal.worldbank.org/country/central-african-republic/trends-variability-historical.Accessed 10 March 2022.
- 48.Raleigh C, Kishi R, Linke A. Political instability patterns are obscured by conflict dataset scope conditions, sources, and coding choices. Humanit Soc Sci Commun. 2023. 10.1057/s41599-023-01559-4. 10.1057/s41599-023-01559-4 [DOI] [Google Scholar]
- 49.ACLED. (2023). ACLED Codebook, 2023. Armed Conflict Location & Event Data Project (ACLED). 2023. http://www.acleddata.com. Accessed 05 May 2023.
- 50.IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp.
- 51.Mabaso, Musawenkosi & Craig, Marlies & Ross, Amanda & Smith, Thomas. Environmental predictors of the seasonality of malaria transmission in Africa: The challenge. The American journal of tropical medicine and hygiene. 2007; 10.4269/ajtmh.2007.76.33. [PubMed]
- 52.Olivier B, Eliezer M, Ngatimo E, Pierrette B, Tsalefac M, Chrysostome G. Influence of Climate Variability on the Dynamics of Malaria Transmission among Children in Bangui, Health Challenges in Central African Republic. Open Journal of Pediatrics. 2022. 10.4236/ojped.2022.123050. 10.4236/ojped.2022.123050 [DOI] [Google Scholar]
- 53.The World Bank. People using at least basic drinking water services, rural (% rural population) – Central African Republic. https://data.worldbank.org/indicator/SH.H2O.BASW.RU.ZS?end=2020&locations=CF&start=2000&view=chart. Accessed 10 Jan 2023.
- 54.The World Bank. People using at least basic drinking water services, urban (% urban population) – Central African Republic. https://data.worldbank.org/indicator/SH.H2O.BASW.UR.ZS?end=2020&locations=CF&start=2000&view=chart. Accessed 10 Jan 2023.
- 55.The WHO/UNICEF Joint Monitoring Programme (JMP). Rural and urban service levels 2015 and 2020. https://washdata.org/data/household#!/dashboard/4985. Accessed 10 Jan 2023.
- 56.Gilmartin AA, Petri WA. Exploring the role of environmental enteropathy in malnutrition, infant development and oral vaccine response. Philosophical Transactions of the Royal Society B: Biological Sciences. 2015. 10.1098/rstb.2014.0143. 10.1098/rstb.2014.0143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thompson AJ, Bourke CD, Robertson RC, Shivakumar N, Edwards CA, Preston T, et al. Understanding the role of the gut in undernutrition: What can technology tell us? Gut. 2021. 10.1136/gutjnl-2020-323609. 10.1136/gutjnl-2020-323609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kelly P. The contribution of environmental enteropathy to the global problem of micronutrient deficiency. Proceedings of the Nutrition Society. 2021. 10.1017/S0029665121000549. 10.1017/S0029665121000549 [DOI] [PubMed] [Google Scholar]
- 59.Vaitla B, Devereux S, Swan SH. Seasonal hunger: a neglected problem with proven solutions. PLoS Med. 2009. 10.1371/journal.pmed.1000101. 10.1371/journal.pmed.1000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Foreign Agricultural Service, U.S. department of Agriculture (USDA). https://ipad.fas.usda.gov/countrysummary/default.aspx?id=CT. Accessed 29 Dec 2022.
- 61.World food programme. Half of the population in the Central African Republic in the grip of dire food insecurity emergency, UN warns. 2021. https://www.wfp.org/news/half-population-central-african-republic-grip-dire-food-insecurity-emergency-un-warns. Accessed 15 Jan 2023.
- 62.Vijayakumar, S. Fixing the road to recovery in the Central African Republic. 2019. https://blogs.worldbank.org/en/nasikiliza/fixing-the-road-to-recovery-in-the-central-african-republic. Accessed 10 Jan 2023.
- 63.Office of the Special Representative of the Secretary-General on Sexual Violence in Conflict. Central African Republic. 2021. https://www.un.org/sexualviolenceinconflict/countries/central-african-republic/. Accessed 10 Jan 2023.
- 64.Chotsiri P, Denoeud-Ndam L, Baudin E, Guindo O, Diawara H, Attaher O, Smit M, Guerin PJ, Doumbo OK, Wiesner L, Barnes KI, Hoglund RM, Dicko A, Etard JF, Tarning J. Severe Acute Malnutrition Results in Lower Lumefantrine Exposure in Children Treated With Artemether-Lumefantrine for Uncomplicated Malaria. Clin Pharmacol Ther. 2019. 10.1002/cpt.1531. 10.1002/cpt.1531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.WWARN ACT Malaria and Malnutrition Study Group. Does acute malnutrition in young children increase the risk of treatment failure following artemisinin-based combination therapy? A WWARN individual patient data meta-analysis. Lancet Glob Health. 2024. 10.1016/S2214-109X(24)00003-2. 10.1016/S2214-109X(24)00003-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rafael ME, Taylor T, Magill A, Lim YW, Girosi F, Allan R. Reducing the burden of childhood malaria in Africa: the role of improved diagnostics. Nature. 2006. 10.1038/nature05445. 10.1038/nature05445 [DOI] [PubMed] [Google Scholar]
- 67.López-Ejeda N, Charle Cuellar P, Vargas A, Guerrero S. Can community health workers manage uncomplicated severe acute malnutrition? A review of operational experiences in delivering severe acute malnutrition treatment through community health platforms. Matern Child Nutr. 2019. 10.1111/mcn.12719. 10.1111/mcn.12719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dougnon AO, Charle-Cuéllar P, Toure F, Gado AA, Sanoussi A, Lazoumar RH, et al. Impact of integration of severe acute malnutrition treatment in primary health care provided by community health workers in rural Niger. Nutrients. 2021. 10.3390/nu13114067. 10.3390/nu13114067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.UNHCR. Cluster Approach. 2024 https://emergency.unhcr.org/coordination-and-communication/cluster-system/cluster-approach. Accessed 30 Aug 2024.
- 70.Dunford, E. T., Cunningham, D. E., Backer, D., Mcgrath, E. C. An integrated picture of conflict. 2019. Available online at: http://ericdunford.com/Projects/integration/dunford_et_al_2020.pdf. Accessed 15 Jan 2023.
- 71.Anato A. Severe acute malnutrition and associated factors among children under-five years: A community based-cross sectional study in Ethiopia. Heliyon. 2022. 10.1016/j.heliyon.2022.e10791. 10.1016/j.heliyon.2022.e10791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nassur A-M, Daanouni O, Luc G, Humphreys A, Blanarova L, Heymsfield G, et al. Factors associated with acute malnutrition among children aged 6–59 months in Haiti, Burkina Faso and Madagascar: A pooled analysis. PLoS ONE. 2022. 10.1371/journal.pone.0278980. 10.1371/journal.pone.0278980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ndah T, Tazoho GM, Youssa CN, Ngoufack FZ, Kuiate JR. Risk factors associated with Severe Acute Malnutrition (SAM) in children aged 6–59 months in the Mokolo Health District, Far North region of Cameroon. The North African Journal of Food and Nutrition Research. 2024. 10.51745/najfnr.8.17.76-85. 10.51745/najfnr.8.17.76-85 [DOI] [Google Scholar]
- 74.Gamit VD, Gohil JR, Nikhileshwar AB, Vagh TP. Etiological factors of severe acute malnutrition and impact of nutrition rehabilitation centre: a prospective observational study from Bhavnagar. International Journal of Contemporary Pediatrics bad. 2021. 10.18203/2349-3291.ijcp20211072. 10.18203/2349-3291.ijcp20211072 [DOI] [Google Scholar]
- 75.International Crisis Group. 10 Conflicts to Watch in 2022. 2021. https://www.crisisgroup.org/global/10-conflicts-watch-2022. Accessed 27 Nov 2023.
- 76.United Nations. ‘War’s Greatest Cost Is Its Human Toll’, Secretary-General Reminds Peacebuilding Commission, Warning of ‘Perilous Impunity’ Taking Hold. 2022. https://press.un.org/en/2022/sgsm21216.doc.htm. Accessed 27 Nov 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.